Abstract
Introduction
Models of care (MoCs) describe evidence-informed healthcare that should be delivered to patients. Several MoCs have been implemented for low back pain (LBP) to reduce evidence-to-practice gaps and increase the effectiveness and sustainability of healthcare services.
Objective
To synthesise research evidence regarding core characteristics and key common elements of MoCs implemented in primary healthcare for the management of LBP.
Design
Scoping review.
Data sources
Searches on MEDLINE (PubMed), EMBASE, Cochrane Central Register of Controlled Trials, PEDro, Scopus, Web of Science and grey literature databases were conducted.
Eligibility criteria
Eligible records included MoCs implemented for adult LBP patients in primary healthcare settings.
Data extraction and synthesis
Data extraction was carried out independently by two researchers and included a summary of the studies, the identification of the MoCs and respective key elements, concerning levels of care, settings, health professionals involved, type of care delivered and core components of the interventions. Findings were investigated through a descriptive qualitative content analysis using a deductive approach.
Results
29 studies reporting 11 MoCs were included. All MoCs were implemented in high-income countries and had clear objectives. Ten MoCs included a stratified care approach. The assessment of LBP patients typically occurred in primary healthcare while care delivery usually took place in community-based settings or outpatient clinics. Care provided by general practitioners and physiotherapists was reported in all MoCs. Education (n=10) and exercise (n=9) were the most common health interventions. However, intervention content, follow-ups and discharge criteria were not fully reported.
Conclusions
This study examines the features of MoCs for LBP, highlighting that research is in its early stages and stressing the need for better reporting to fill gaps in care delivery and implementation. This knowledge is crucial for researchers, clinicians and decision-makers in assessing the applicability and transferability of MoCs to primary healthcare settings.
Keywords: back pain, musculoskeletal disorders, pain management, primary health care, health services, organisation of health services
STRENGTHS AND LIMITATIONS OF THIS STUDY.
To the best of our knowledge, this is the first study aiming to map the available evidence regarding the core characteristics and key elements of models of care (MoCs) implemented in primary healthcare for the management of low back pain (LBP).
To aid the transparency and methodological rigour of this study, it followed the Joanna Briggs Institute Methodological Guidelines and Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews.
One limitation of this review is potential selection bias due to search strategies and language restrictions, as well as heterogeneity in MoC terminologies.
Strategies to overcome potential limitations included the use of a broad search strategy across databases, an overinclusion approach during article screening and regular team discussions during data extraction and analysis.
This study offers a comprehensive understanding of key characteristics of the MoCs implemented for LBP patients in primary healthcare, which may help clinicians and decision-makers to plan the implementation of MoCs in real-world settings, as well as researchers defining avenues to overcome the current evidence-to-practice gaps.
Introduction
Low back pain (LBP) is a significant global public health concern, acknowledged as the leading contributor to disability worldwide. In 2020, 619 million (95% Uncertainty Interval (UI) 554 to 694) people reported having this health condition and prevalence projections suggest it will escalate to 843 million (95% UI 759 to 933) by 2050, an increase in total cases of 36.4%.1 It is recognised that the burdensomeness of LBP is related to long-term disability and poor health-related quality of life,2–4 associated with more medical costs and utilisation of healthcare resources, such as medication, medical appointments, imaging and physiotherapy.2 5–7 Thus, LBP represents a growing burden for individuals, society and healthcare systems.
Although care delivery may vary between health systems, primary healthcare is recognised as the appropriate setting to manage LBP,8 9 which is already one of the most common reasons for general practice consultations worldwide.8 10 Accompanying the estimates of the rising prevalence of LBP, it is also expected a significant increase in primary healthcare workload in the upcoming years,9 so there is an urgent need to develop efficient and sustainable solutions to face these healthcare challenges.
Additionally, evidence shows there is a present gap between the recommended practice for LBP and the care provided in real-world contexts.9 Current patterns of care may vary between settings and lack alignment with clinical practice guideline recommendations, which succinctly endorse the delivery of non-pharmacological interventions, such as education and exercise, and manual therapy as an adjuvant treatment.8 11–14 However, many LBP patients receive unnecessary low-value care, which does not align with quality standards,14 15 leads to poor clinical outcomes4 16 and wastes healthcare resources.17–19 Therefore, system-level reform strategies are necessary to overcome these evidence-to-practice gaps and to promote the delivery of high-quality care to LBP patients.9 17 20
The implementation of models of care (MoCs) is one of the most promising strategies suggested to increase the responsiveness of health systems to the impact of LBP. A MoC is a person-centred approach that outlines evidence-informed best practices for managing specific health conditions.21–23 It details the optimal care that should be provided and the methods for its implementation. MoCs are built on clinical guidelines—drawing from up-to-date recommendations—and they primarily serve to translate these recommendations into actionable strategies.23 While clinical pathways focus on the integrated delivery of care to patients with a specific condition, MoCs go beyond this aspect, focusing much of their attention on the factors that determine a successful implementation.22 23
The principles of MoCs are in line with the quadruple aim of value-based care, targeting better health outcomes, better patient and health professional experiences and improved use of healthcare resources.17 21 MoCs usually reflect regional or national health policies that are implemented as health services in local settings.22 24 When implemented locally, a MoC includes the key core components from the system-level framework, but other elements should be adapted to meet the specific context and needs.17 The operationalisation of a MoC for local service delivery is usually designated as a model of service delivery.17
Several MoCs have been implemented for LBP patients over the last few years in different countries. Commonly, these MoCs deliver care through stepped or stratified approaches, supporting the decision-making process. In stepped care, all patients are initially offered the same treatment options and more complex care is only proposed if they have not recovered sufficiently, while, in risk-stratified MoCs, patients are stratified according to their prognosis at initial assessment and treatment is targeted to patient subgroups, with more comprehensive care offered to those at risk of poor outcomes.25
Although some MoCs reveal promising results regarding their effectiveness and cost-effectiveness,9 23 they are very heterogeneous in terms of their characteristics, making it difficult to assess the suitability of a MoC to a given context over another. These characteristics include but are not limited to, the target population, clinical pathways, levels of care and health professionals involved, type of care (stepped/stratified approaches), health interventions and context features.
Two recent reviews26 27 have analysed the evidence on initiatives for implementing LBP management. One review focuses specifically on MoCs implemented in Australia.26 The other, a systematic review,27 aims to describe clinical pathways and care integration across different levels of care, without focusing on the details of care delivery and implementation. Therefore, our work seeks to expand on these contributions by providing a broader overview of the diversity, content and resource requirements of MoCs for LBP patients. This is important information to support policy-makers, managers, clinicians in the development and implementation planning of MoCs, as well as pinpoint evidence gaps related to implementation in real-world settings.
Methods
A scoping review was deemed the most appropriate study design to answer the research questions as it aims to map the available evidence and identify characteristics or factors related to an emerging and complex concept.28 29 The uncertainty regarding the evidence sources, methodologies and amount and quality of available data determined the choice of this approach.
This study was conducted in accordance with the Joanna Briggs Institute (JBI) scoping review guidance and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA) (online supplemental file 1). The protocol was registered within the Open Science Framework Registries (https://osf.io/rsd8x) and it was published elsewhere.30
bmjopen-2023-079276supp001.pdf (36.6KB, pdf)
Patient and public involvement
Patients and public were not included in the design, conduct or reporting of this research as it is targeted at researchers, clinicians, managers and policy-makers.
Research question and aims
The research question of this review is ‘What are the key characteristics of MoCs implemented in primary healthcare for patients with LBP?’ Our objectives are to identify which MoCs have been implemented for LBP management, describe their main characteristics and similarities in care delivery, and highlight any gaps in knowledge regarding their real-world implementation.
Inclusion criteria
Eligibility criteria were defined through the Population, Concept, Context framework.28 29 The target population are LBP patients, with or without radicular pain, of any duration, excluding specific causes or serious pathologies. Records including broader populations, such as ‘musculoskeletal pain’ or ‘spinal pain’, were also excluded. MoC was defined as the provision and delivery of care in a local setting, including service planning, care coordination and management of services.21 22 31 Operational criteria were defined to differentiate a MoC from intervention programmes.22 30 Regarding the context, MoCs were included if they were developed in primary healthcare or other levels of healthcare delivery, as long as they included primary care interventions in the clinical pathway.31
Search strategy
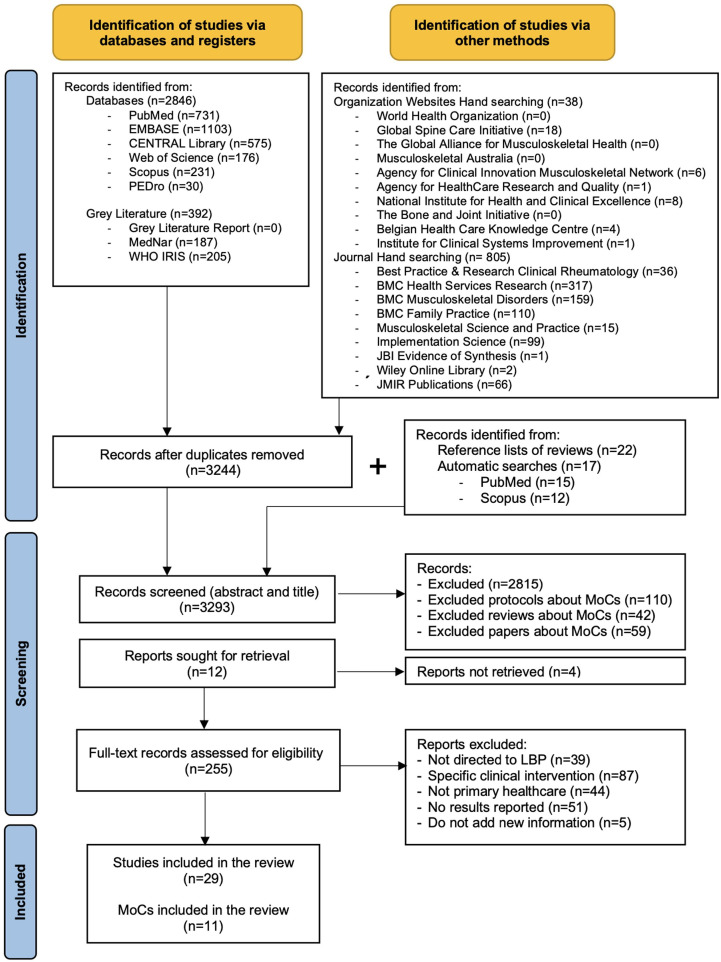
A comprehensive search was conducted on MEDLINE (PubMed), EMBASE, Cochrane Central Register of Controlled Trials, PEDro, Scopus and Web of Science, as well as grey literature sources (figure 1). Handsearching was performed in peer-reviewed journals and relevant organisation websites.32 Additional studies were identified through reference list screening. Initial searches conducted in May 2021 used key terms such as “low back pain,” “model of care” and “primary care”. Subsequent tailored searches across all databases were performed (online supplemental file 2). Only records published since 2000 were considered as we aim to examine evidence-based and coordinated healthcare delivery for LBP, reflecting the current concept of MoC. Language restrictions for English, Portuguese or Spanish were established due to practical constraints related to the availability of translation resources. The search commenced in January 2022 and was last updated in December 2022, with search strategies reviewed and conducted by an experienced information scientist (HD).
Figure 1.
PRISMA flow diagram showing the identification, screening, eligibility and inclusion process of the articles. LBP, low back pain; MoCs, models of care; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
bmjopen-2023-079276supp002.pdf (63.2KB, pdf)
Study selection
Records were imported to EndNote V.X9 (Clarivate Analytics, USA) for screening and duplicate removal. Two reviewers independently screened titles and abstracts (STD and DC). Eligibility criteria were tested with a random sample of 25 records. Afterwards, full-text screening was performed by two researchers (STD and AM), with a pilot test on 10 studies for consistency. Disagreements were discussed with a third reviewer (DC).
Data charting
To ensure data extraction transparency,28 a standardised form (online supplemental file 3) was developed and piloted, covering a summary of the studies, the identification and description of the MoC (name, country, target population and main objectives) and respective key elements (levels of care and settings, health professionals involved, type of care delivered and core components of health interventions). Two researchers (STD and AM) extracted data independently and resolved uncertainties with the research team. Only relevant data to the research question were extracted, and when necessary, the authors were contacted for clarification. Regular video meetings were held for data review and process updates.
bmjopen-2023-079276supp003.pdf (84KB, pdf)
Synthesis and presentation of results
Findings were synthesised through deductive content analysis in three phases: preparation, organisation and reporting.33 Data are presented in narrative, tabular and chart formats for each MoC for LBP management. Descriptive results include the identification of the MoCs, their general description and key elements while quantitative results refer to frequency counts of the data.
Protocol deviations
Four research questions were framed in the protocol of this study.30 However, during the processes of data extraction and analysis, it became clear that the complexity of the topic and richness of the available data justified a rigorous description and interpretation of the findings. Therefore, findings on patient-related, system-related and implementation-related outcomes of MoCs and context-specific factors (macro, meso, micro and multiple levels) contemplated in their implementation will be reported in a subsequent paper. Additionally, one criterion was added to those published in the protocol, which is the MoC is not digital (eg, telemedicine, telerehabilitation, web-based programmes and/or mobile apps).
Results
Search results
The PRISMA flow diagram (figure 1) outlines the search and selection process. From the 4081 records yielded in first instance, 29 studies,34–62 published between 2011 and 2022, were included. They portray 11 MoCs implemented in primary healthcare.
Characteristics of the included studies
Table 1 identifies each MoC and their corresponding studies. Quantitative studies (n=19) mainly consisted of randomised controlled trials (n=9) and observational cohorts (n=9). These studies assessed the clinical effectiveness and efficacy of nine MoCs34 39 42 44 46 48 49 51 55 57 58 60–62 and healthcare resources utilisation of seven MoCs.34 39 46 52–54 56–58 60–62 Only BetterBack☺ was evaluated for healthcare quality43 and economic evaluations were solely performed for three MoCs.34 35 46 58 60 61 Qualitative studies (n=5; 5 MoCs) focused on implementation outcomes and strategies36 37 41 45 59 while mixed-methods studies (n=5; 3 MoCs) investigated patient and organisational outcomes, as well as the experiences of different stakeholders.38 47 50 Detailed characteristics of the studies, including eligibility criteria, sample sizes, outcomes and outcome measures, can be found in online supplemental file 4.
Table 1.
MoCs identification and corresponding studies
| MoC designation | Country | Study | Objective | Type of study |
| STarT Back Subgroups for targeted treatment |
UK | Hill et al (2011)34 | To compare the clinical effectiveness and cost-effectiveness of stratified primary care with non-stratified current best practice (STarT Back trial) | RCT |
| Whitehurst et al (2012)35 | To determine the economic implications of providing stratified care compared with non-stratified current best practice for each specific risk-defined subgroup (STarT Back trial) | RCT (cost–utility) | ||
| Foster et al (2014)46 | To determine the effects of implementing risk stratified in family practice on physician’s clinical behaviour, patient outcomes and costs (IMPaCT Back trial) | Observational cohort, before–after | ||
| Whitehurst et al (2015)56 | To explore the cost–utility of implementing stratified care in general practice, compared with usual care, within risk-defined patient subgroups (IMPaCT Back trial) | RCT (cost–utility) | ||
| Ireland | Murphy et al (2016)57 | To explore the effectiveness of group-based (high-risk group) stratified care in primary care | Non-randomised controlled trial | |
| Denmark | Morsø et al (2021)58 | To evaluate the clinical efficacy and cost-effectiveness of stratified care compared with current practice in Danish primary care | RCT | |
| SCOPiC SCiatica outcomes in primary care |
UK | Saunders et al (2020)59 | To explore patients’ and clinicians’ perspectives on the acceptability of the ‘fast-track’ pathway | Qualitative |
| Konstantinou et al (2020)60 | To investigate the clinical and cost-effectiveness of stratified care vs non-stratified usual care for patients presenting with sciatica in primary care | RCT | ||
| Foster et al (2020)61 | To compare the clinical effectiveness and cost-effectiveness of the SCOPiC care versus non-SCOPiC care in primary care | Mixed methods | ||
| MATCH Matching appropriate treatment to consumers’ healthcare needs |
USA | Cherkin et al (2018)62 | To evaluate the effect of implementing an adaptation of the STarT Back strategy in a US primary care setting | Cluster RCT |
| Hsu et al (2019)36 | To describe the implementation strategies and uptake of an intervention that incorporated the STarT Back stratified care model into several primary care clinics | Qualitative | ||
| TARGET Targeted Interventions to prevent chronic low back pain in high-risk patients |
USA | Beneciuk et al (2019)37 | To describe the training developed and delivered to prepare PTs for providing treatment in the TARGET trial | Qualitative |
| Middleton et al (2020)38 | To examine variation in risk stratification and referral of high-risk patients to psychologically informed physical therapy (PIPT) and to identify barriers and facilitators related to the risk stratification and referral processes. | Mixed methods | ||
| Delitto et al (2021)39 | To test if implementation of a risk-stratified approach to care would result in lower rates of chronic LBP and improved self-reported disability; and if the stratified approach supplemented with referral to PIPT is superior to stratified care alone | Cluster RCT | ||
| BETTERBACK☺ Model of Care | Sweden | Schröder et al (2020)40 | To evaluate PTs’ confidence, attitudes and beliefs in managing patients before and after a multifaceted implementation of the BetterBack☺ and to evaluate determinants of implementation behaviours among PTs | Observational cohort, before–after |
| Enthoven et al (2021)41 | To describe patient experiences of received primary care according to the BetterBack☺ in primary care | Qualitative | ||
| Schröder et al (2021)42 | To evaluate the effectiveness and a sustained multifaceted implementation strategy of the BetterBack☺ compared with routine PT care; To compare patient outcomes based on the fidelity of clinical practice quality index adherence regarding PT care. | Cluster RCT | ||
| Schröder et al (2022)43 | To evaluate if PT’s adherence to clinical practice guideline recommendations improves after a multifaceted implementation of the BetterBack☺ | Cluster RCT | ||
| Low back and radicular pain pathway | UK (National) |
Greenough (2017)44 | To produce and use a generic pathway for the management of LBP and radicular pain in adults, from the general practitioner’s surgery to specialised care | Report (grey literature) |
| Ryan et al (2020)45 | To explore how people experience being managed for sciatica within a National Health Service pathway | Qualitative | ||
| UK (North) |
Martin et al (2018)47 | To evaluate what changes are seen in patient outcomes and experiences, and in the performance of the health service following the implementation of the pathway | Mixed methods (grey literature) | |
| UK (North East) |
Jess et al (2018)48 | To investigate the association between the duration of pain at baseline and the clinical outcomes of patients with LBP enrolled on NERBPP | Observational cohort | |
| Jess et al (2021)49 | To evaluate the association between baseline pain duration and medium-to-long term clinical outcomes in LBP patients enrolled on the NERBPP | Observational cohort | ||
| Beating Back Pain Service (BBPS) | UK | Cheshire et al (2013)50 | To report patient outcomes and experiences of the BBPS | Mixed methods |
| North East Essex Primary Care Trust manual therapy service | UK | Gurden et al (2012)51 | To describe and evaluate a community-based musculoskeletal service in terms of patient-reported outcomes and satisfaction | Observational cohort |
| Interprofessional Spine Assessment and Education Clinics (ISAEC) | Canada | Zarrabian et al (2017)52 | To determine the effect of ISAEC on access for surgical assessment, referral appropriateness and efficiency for patients meeting a priori referral criteria in rural, urban and metropolitan settings | Observational cohort |
| Saskatchewan Spine Pathway (SSP) | Canada | Kindrachuk and Fourney (2014)53 | To determine how the SSP pathway affects utilisation of MRI and spine surgery | Retrospective study, registry based |
| Wilgenbusch et al (2014)54 | To determine if outpatient referrals through a multidisciplinary spine care pathway were more likely to be candidates for surgery than conventional physician referrals; to compare clinical differences wait times for MRI and surgical assessment. | Retrospective study, registry based | ||
| Back Pain Assessment Clinic (BAC) | Australia | Moi et al (2018)55 | To report on the design, implementation and evaluation of the safety and effectiveness of the BAC model | Observational cohort pilot study |
LBP, low back pain; MoC, model of care; NERBPP, North East Low Back and Radicular Pain Pathway; PTs, physiotherapists; RCT, randomised controlled trial; SCOPiC, Sciatica Outcomes in Primary Care.
bmjopen-2023-079276supp004.pdf (195.4KB, pdf)
General description
The 11 MoCs implemented in primary healthcare for the management of LBP patients are the STarT Back,34 35 46 56–58 SCOPiC,59–61 MATCH,36 62 TARGET,37–39 BetterBack☺ MoC,40–43 Low Back and Radicular Pain Pathway,44 45 47–49 Beating Back Pain Service (BBPS),50 North East Essex Primary Care Trust (PCT) manual therapy service,51 Interprofessional Spine Assessment and Education Clinics (ISAEC),52 Saskatchewan Spine Pathway (SSP)53 54 and Back Pain Assessment Clinic (BAC).55
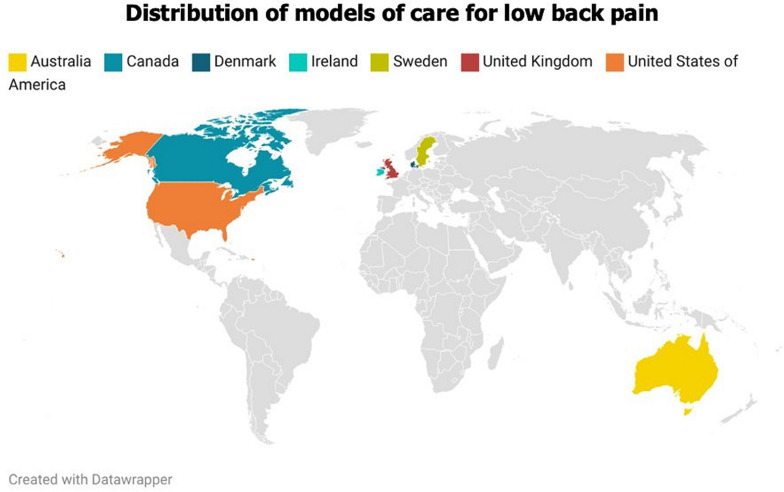
All MoCs were implemented in high-income countries from Europe, North America and Australia (figure 2). Most implementations (n=5) were set in the UK, followed by the USA (n=2) and Canada (n=2). STarT Back34 35 46 56–58 was the only MoC implemented in three countries (the UK, Ireland and Denmark). However, adaptations of this MoC, with significant adjustments to its core characteristics, were also implemented in the USA (MATCH and TARGET)36–39 62 and Sweden (BetterBack☺).40–43
Figure 2.
Geographical representation of the MoCs (n=11) implemented for LBP in primary healthcare worldwide. LBP, low back pain; MoCs, models of care.
The target population of the MoCs involved adults with LBP, with or without radicular pain, or radiculopathy. North East Essex PCT manual therapy service51 and BAC55 also included patients with neck pain. BBPS50 and Irish STarT Back57 were the only MoCs that established the duration of pain as an eligibility criterion, namely, the presence of LBP for more than 6 weeks and 3 months, respectively (online supplemental file 4).
Most MoCs (n=8) aimed to promote evidence-informed practice to improve clinical effectiveness. They were informed by national or international clinical practice guidelines to design the service delivery and health interventions for the management of LBP. Only Canadian MoCs, ISAEC52 and SSP,53 54 did not specify the guidelines they followed, although the studies mentioned the need to provide care in line with current recommendations.
MoCs comprising more than one level of care, such as interface services and/or secondary care,44 45 48 49 52–55 59–61 were especially concerned with reducing waiting times and optimising referral behaviours for imaging, care delivery and specialist review. Goals related to equitable access to care were only identified for the LBP and Radicular Pain Pathway44 and the North East Essex PCT manual therapy service.51
The majority of MoCs were implemented within the National Healthcare Systems through local (n=3) and regional (n=7) pathways. Only the LBP and Radicular Pain Pathway refers to a national MoC44 45. MATCH36 62 and TARGET37–39 were implemented in integrated healthcare delivery systems of the USA. Additionally, only four MoCs (Danish STarT Back, SCOPiC, TARGET and ISAEC)39 52 58 60 were implemented in different geographical areas, covering urban, inner city and rural settings.
Table 2 presents detailed information on the general characteristics of the different MoCs, including target population, goals, type of care, settings and health professionals involved in care delivery.
Table 2.
General characteristics of the MoCs
| MoC | Study | MoC goals | Population | Type of care | Settings | Health professionals | Context |
| STarT Back | STarT Back34 35 | Implement stratified care; promote EBP and/or guideline-concordant care; improve care effectiveness; reduce costs; optimise referral behaviour for care and/or imaging | LBP, radiculopathy | Stratified (by prognosis) | PHC (general practices and PT-led back pain clinic) | GPs, nurses and PTs | NHS (PCT); general practices within the Keele GP Research Partnership (network of practices); Clinical manifestation of the guidelines of the Royal College of General Practitioners (1996), Working Group on Guidelines for the Management of Acute LBP in Primary Care (2006) and Arthritis and Musculoskeletal Alliance (2004). |
| IMPaCT Back46 56 | PHC (general practices and community-based PT practices) | GPs and PTs | NHS (PCT); Clinical manifestation of the NICE guidelines (2009) | ||||
| Ireland57 | Implement stratified care; improve care effectiveness; Promote EBP and/or guideline-concordant care; reduce healthcare resources use | LBP, radicular pain | Stratified (by prognosis) | PHC (PT-led spinal triage clinic—Back Pain Clinic) | GPs and PTs | NHS (Waterford City Primary Care); Clinical manifestation of the NICE guidelines for LBP (2009) | |
| Denmark58 | Implement stratified care; improve care effectiveness; Promote EBP and/or guideline-concordant care; reduce costs; optimise referral behaviour for care and/or imaging | LBP, radicular pain | Stratified (by prognosis) | PHC (general practices and PT clinics) | GPs and PTs | PHC from different geographical areas of the Regions of Southern and Central Denmark. | |
| SCOPiC | 59–61 | Reduce wait times for imaging and/or specialist review; Ppromote EBP and/or guideline-concordant care; improve care effectiveness; Implement stratified care | LBP, radicular pain (suspected sciatica) |
Stratified (by prognosis and pattern diagnosis) | PHC (general practices, community PT services), primary/ secondary care interface services and secondary care | GPs, PTs, spinal specialist PTs and spinal surgeons | NHS (Trusts); general practices localised in a mix of urban, inner city, semirural and rural areas; spinal specialist services include specialist clinics at the primary/secondary care interface, spinal orthopaedic and pain clinic teams (treatments offered are part of NHS care). |
| MATCH | 36 62 | Implement stratified care; improve care effectiveness; reduce healthcare utilisation; optimise referral behaviour for care and/or imaging | LBP | Stratified (by prognosis) | PHC (clinics with onsite PT departments) | Medical doctors, physician assistants/nurse practitioners and PTs | Integrated healthcare delivery system (group health); adaptation of the STarT Back approach: major differences concern the delivery of care, which follows the Group Health treatment guidelines. |
| TARGET | 37–39 | Implement stratified care; improve care effectiveness; reduce healthcare resources use; optimise referral behaviour for care and/or imaging | LBP | Stratified (by prognosis) | PHC (clinics) | PHC physicians and PTs | Five healthcare systems (University of Pittsburgh Medical Centre, Boston Medical Centre, Johns Hopkins Medicine, Intermountain Health, Medical University of South Carolina)—network of PHC clinics in both urban and rural environments; MoC directed to manage high-risk patients (according to SBST stratification). |
| BETTERBACK☺ | 40–43 | Promote EBP and/or guideline-concordant care; Iimprove care effectiveness; promote integrated care | LBP, radiculopathy | Hybrid - stratified/ stepped | PHC (PT clinics) | PTs | Adaptation of best practice clinical guidelines. developed by the Danish Health and Medicines Authority (2016) and the English NICE (2016) to the Swedish context |
| Low back and radicular pain pathway | National44 45 | Improve care effectiveness; promote timely and/or equitable access to care; promote EBP and/or guideline-concordant care; promote integrated care; reduce wait times for care, imaging and/or specialist review; optimise referral behaviour for care and/or imaging | LBP, radicular pain | Hybrid – Stratified/ stepped | PHC, community services, secondary care and specialist pain management services | GPs, PTs, chiropractors, osteopaths, pharmacists, TTPs, specialist spinal surgeon, multidisciplinary staffing | NHS; The implementation of the National Pathway is a decision of the Clinical Commissioning Groups, considering services and provision within their commissioning area; TTPs play a core role in the pathway. |
| North47 | Not reported | PHC (outpatient PT service) | GPs and TTPs (specialised nurses and PTs) | NHS (community trust); Part of the national pathway (UK Low Back and Radicular Pain Pathway); Clinical manifestation of the NICE guidelines for LBP (2009) | |||
| North East48 49 | Hybrid—stratified/stepped | PHC, primary/ secondary care interface services and secondary care | Clinical manifestation of the NICE guidelines for LBP (2009) | ||||
| Beating back pain service | 50 | Promote EBP and/or guideline-concordant care; reduce wait times for care, imaging and/or specialist review | LBP | Hybrid—stepped/stratified (by patient preference) | PHC and community care | GPs, occupational therapists, acupuncturists, psychotherapists | NHS (PCT); Clinical manifestation of the NICE guidelines for LBP (2009) |
| North East Essex PCT service | 51 | Improve care effectiveness; promote timely and/or equitable access to care; reduce wait times for care, imaging and/or specialist review; optimise referral behaviour for care and/or imaging; reduce healthcare resources use | Back or neck pain | Hybrid—stepped/stratified (by patient preference) | PHC and community care (chiropractic, osteopathic and PT clinics) | GPs, chiropractors, osteopaths and PTs | NHS (North East Essex PCT); Clinical manifestation of the NICE guidelines for LBP (2009) |
| ISAEC | 52 | Promote EBP and/or guideline-concordant care; reduce wait times for care, imaging and/or specialist review; optimise referral behaviour for care and/or imaging; promote integrated care | LBP | Stratified (by pattern diagnosis) | PHC and ISAEC clinics | Doctors, nurse practitioners, PTs, chiropractors, surgeons, pain specialists and rheumatologists | Funded by the Ontario Ministry of Health and Long-Term Care to enable shared-care management of LBP; Implemented in rural, urban and metropolitan settings. |
| Saskatchewan Spine Pathway (SSP) | 53 54 | Promote EBP and/or guideline-concordant care; promote integrated care; improve care effectiveness and efficiency; reduce variations in practice patterns; reduce wait times for care, imaging and/or specialist review; optimise referral behaviour for care and/or imaging | LBP, radicular pain | Stratified (by pattern diagnosis) | PHC and SSP clinics | Physicians, spine surgeons and specialised PTs | Pathway developed by spine surgeons; It uses a multidisciplinary triage process and treatment algorithms based on the SSP classification; The SSP classification defines four clinical patterns of symptoms and signs determined by history and physical examination. |
| Back pain Assessment Clinic (BAC) | 55 | Promote EBP and/or guideline-concordant care; promote integrated care; optimise referral behaviour for care and/or imaging; reduce wait times for care, imaging and/or specialist review | LBP or neck pain | Stepped | PHC, tertiary neurosurgery and orthopaedic referral centre | Practice PTs, rheumatology registrars, rheumatologists, neurosurgeons, orthopaedic spinal surgeons | BAC is a community-based specialist service for assessing and managing neck and LBP; Pathway developed by health professionals of the Royal Melbourne Hospital, which serves as a tertiary neurosurgery and orthopaedic referral centre; Rheumatologist coordinate BAC care. |
EBP, evidence-based practice; GPs, general practitioner; ISAEC, Interprofessional Spine Assessment and Education Clinics; LBP, low back pain; MoC, model of care; NERBPP, North East Low Back and Radicular Pain Pathway; NHS, National Health System; NICE, National Institute of Health and Care Excellence; PCT, Primary Care Trust; PHC, primary healthcare; PT, physiotherapy; PTs, physiotherapists; SBST, STarT Back Screening Tool; TTPs, triage and treat practitioners.
Settings and healthcare professionals
Most MoCs (n=10) for LBP encompass multiple healthcare setting. General practices serve as the entry point for eight MoCs, being important in the initial management of LBP patients. These MoCs ensure continuity of care in outpatient physiotherapy clinics and community care settings, where patients receive the main health interventions. SCOPiC,59–61 Low Back and Radicular Pain Pathway44 45 47–49 and BAC55 also include other settings, such as interface, secondary and tertiary care services. MATCH,36 62 TARGET37–39 and BetterBack☺40–43 were exclusively implemented in primary healthcare clinics featuring onsite physiotherapy departments.
The health professionals who most commonly deliver care in MoCs are general practitioners and physiotherapists. General practitioners are primarily involved in the initial assessment and referral of patients receiving health services, whereas physiotherapists oversee the rehabilitation process. Four models also include osteopaths, chiropractors and acupuncturists,44 45 50–52 depending on the integration of these professionals within the specific healthcare system of each country. MoCs that incorporate more than one level of care44 45 53–55 59–61 comprise consultations of medical specialties with surgeons and rheumatologists. Four MoCs44 45 47–49 52–54 59–61 also include advanced practice clinicians, usually physiotherapists specialised in triage processes and identification and management of red flags and emergency conditions.
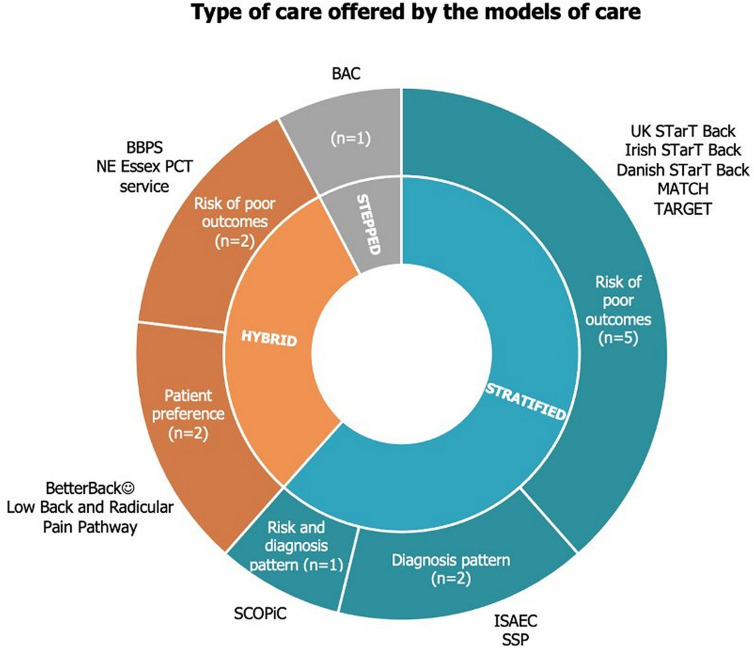
Type of care
The majority of MoCs (n=7) use a stratified care approach, targeting health intervention to patients’ subgroups based on their prognostic profile and/or pattern diagnosis. Less treatment is given to those who are at low risk or whose signs and symptoms are less severe while high-risk patients receive more specialised treatment or are referred to secondary care. The only MoC that is characterised by a stepped approach is the BAC,55 being essentially a health service dedicated to the screening and referral of LBP patients.
Hybrid care, combining stratified and stepped approaches, was identified in four MoCs. BetterBack☺40–43 and Low Back and Radicular Pain Pathway44 45 47–49 stratify patients based on clinical prognosis. If there are no improvements after the main health intervention, patients are referred to additional group care in BetterBack☺40–43 and to Pain Management Services and specialist spinal surgical options in the Low Back and Radicular Pain Pathway.44 45 47–49 In BBPS50 and North East Essex PCT service,51 the stepped care occurs first through education sessions and usual general practitioner care, respectively. Patients are stratified a posteriori based on their treatment preferences, such as care provided by physiotherapists, osteopaths or chiropractors. Figure 3 and table 2 summarise the type of care provided in each MoC.
Figure 3.
Sunburst chart representing the different approaches of care delivered by the MoCs. BAC, Back Pain Assessment Clinic; BBPS, Beating Back Pain Service; ISAEC, Interprofessional Spine Assessment and Education Clinics; MoCs, models of care; PCT, Primary Care Trust; SCOPIC, Sciatica Outcomes in Primary Care; SSP, Saskatchewan Spine Pathway.
Core components of MoCs
To facilitate the reporting, core components were separated into five moments, which correspond to referral, assessment, health interventions, follow-ups and discharge. These elements are presented in online supplemental file 5.
bmjopen-2023-079276supp005.pdf (150.3KB, pdf)
Referral and assessment
As aforementioned, the initial consultation with a general practitioner is an entry point on the pathway in all MoCs. In three MoCs,34 35 40–45 self-referral through direct access to services is possible, as well as a referral by other health professionals (MATCH, TARGET and ISAEC). Surgeons are the main referrers in SSP53 54 and BAC.55
The assessment of LBP patients concerns mainly the exclusion of red flags, physical assessment and stratification. Physiotherapists are the most common health professionals (n=9) to carry out the assessment, followed by the GP and triage specialists. The only model that does not carry out an assessment before an intervention is the BBPS,50 which is only performed after a group education session.
Health interventions
Education (n=10), exercise (n=9) and manual therapy (n=7) were the key core elements of MoCs reported by most studies. With the exception of North East Essex PCT service51 and BAC,55 all MoCs included at least a minimal education intervention, focusing on the reassurance about the benign nature of LBP and self-management strategies. These messages were communicated directly by the health professionals or through support tools, such as written information, DVDs and online content.
In MoCs that include a stratified approach, patients receive appropriate matched treatments, with different doses of education, exercise and manual therapy, according to their prognosis, pattern diagnosis or treatment preference. More complex interventions, such as interventions for high-risk patients34–41 43 45 46 48 56–58 60 62 and community-based spinal rehabilitation programmes,44 45 47–49 55 combine physical and psychological therapies, adding cognitive-behavioural approaches and support for long-term self-management. However, these are poorly described in the included studies.
The majority of MoCs include a health intervention that may vary from a single session (for low-risk patients in stratified approaches according to prognosis profile) to several weeks of multifaceted rehabilitation programmes. However, not all models establish a specific duration for these interventions. Individualised treatments are the chosen format for healthcare delivery in most MoCs, except for Irish STarT Back.57 Group interventions appear to be a second treatment option in BetterBack☺40–43 and Low Back and Radicular Pain Pathway44 45 47–49 when the main health intervention did not result in benefits for LBP patients.
Other interventions, such pain medication prescription or review, were usually delivered by GP or other medical doctor in the initial consultation (STarT Back, TARGET, Low Back and Radicular Pain Pathway and SSP). None of the MoCs included occupational interventions or treatments focused on the adoption of healthy lifestyles.
Follow-up and discharge
Follow-up management and criteria for discharge were not well-defined in the included studies. When there are no improvements in the health condition, follow-ups may combine referral to additional group interventions, interface or secondary/tertiary care services. Irish57 and Danish58 STarT Back, TARGET37–39 and BBPS55 did not report how and when follow-ups are conducted.
Concerning discharges, it seems they occur at the end of health interventions, but the reporting is not clear. In risk-stratified models, such as STarT Back, patients attend a preset number of appointments to receive treatments. However, it is poorly described if patients are discharged after this period, with six MoCs not mentioning any criteria or timing. In TARGET,37–39 Low Back and Radicular Pain Pathway44 45 47–49 and North East Essex PCT service51 patients can be discharged at any point along the pathway on improvement of the LBP.
Discussion
This study mapped the available evidence regarding the core characteristics and key elements of MoCs implemented in primary healthcare for the management of LBP. 11 MoCs were found, all of them implemented in high-income countries with strong primary healthcare services, where general practitioners and physiotherapists serve as the main referrers. The majority of MoCs involve complex interventions delivered by physiotherapists, showing great variability in the reporting of core components, including unclear duration, follow-up and discharge criteria.
First, MoCs for LBP are in various stages of research and integration into health systems. While the LBP and Radicular Pain Pathway44 45 are implemented nationwide, other MoCs are in trial phases regionally or locally. This reflects a growing emphasis on adopting MoCs for LBP, recognised for their potential to enhance care quality through evidence-based practices.63 However, given the inconsistent outcomes observed with these MoCs, they are not yet suitable for implementation beyond research environments.
Recent studies show that LBP patients receiving treatments aligned with guidelines see better clinical outcomes and less healthcare usage.64 Although the reviewed MoCs align with these guidelines, only BetterBack☺40–43 65 has been assessed for its adherence to quality standards in care delivery. The reports suggest guideline-compliant designs, yet often lack detail on ensuring the intended delivery of interventions. The gap between research findings and practical application in clinical settings remains,9 66 as the current evidence does not fully explore this transition. Future research should more thoroughly document care delivery assessment and monitoring processes.
Ten MoCs included stratified care approaches. Considering the successful implementation of the STarT Back34 in the UK on clinical and cost-effectiveness,34 35 46 56 adaptations of this MoC were developed in other countries. Recently, a systematic review found that a stratified care approach provides substantial clinical, economic and health-related cost benefits in the medium and high-risk subgroups compared with usual care in short-term and medium-term follow-ups.67 This may explain why MoCs tend to follow a stratified or hybrid approach to deliver care using the STarT Back Screening Tool. However, evidence shows that some adaptations of the MoC in other countries, such as in the USA, failed to show its clinical effectiveness. Moreover, despite there being no current evidence favouring stratified over stepped approaches for LBP management, the stepped care has demonstrated efficacy for other musculoskeletal conditions, such as osteoarthritis.25 The development of future MoCs may involve research on stepped care solutions as both strategies are endorsed by guidelines for treating LBP.11 13 68 69
This review found that many MoCs for managing LBP align with recommended practices, emphasising primary and community care as initial contact points22 involving specialised health professionals, and focusing on education and exercise interventions.8 11–14 However, there was significant variability in how health interventions were reported over time, with many studies lacking detailed documentation on follow-up procedures, discharge criteria and specialised interventions across care levels. Accurate and detailed reporting of these interventions is essential for their replication and adaptation, critical for successful implementation in clinical settings.
MoCs aim to streamline and enhance healthcare efficiency through effective coordination across care sectors. Such coordination is key to delivering integrated, patient-centred care.17 22 Despite this emphasis, our review found that only 436–38 45 47 48 60 61 of the 11 MoCs provided clear details on achieving this coordination, often only mentioning clinical pathways and electronic health records. This gap suggests a potential underprioritisation of or challenges in implementing effective care integration, echoing broader findings of limited care integration for LBP patients between primary and secondary settings.27 70 Future research should focus on detailing strategies to improve healthcare provider collaboration, shared decision-making and treatment plan adjustments to foster better care integration.71
This review intended to inform clinicians and decision-makers on the current stage of MoCs implementation worldwide. We intend to continue this reflection through the synthesis of context-specific factors and outcomes used to evaluate the implementation of MoCs for LBP in primary healthcare. A subsequent paper will provide a comprehensive understanding of how implementation processes and strategies may have influenced outcomes.
Strengths and limitations
The major strength includes adherence to JBI recommendations28 29 32 and ensuring a robust and systematic methodology, right from protocol design to the presentation of results. Critical aspects such as the development of the search strategy, screening of records by two independent reviewers and regular team discussions during data extraction and analysis were conducted under this guidance. However, the study also faced challenges such as potential evidence selection bias due to search strategies and language restrictions, possibly excluding some pertinent studies on MoCs. Variations in MoC terminologies in literature, the inclusive definition of MoC and the ambiguity between specific evidence-based interventions and MoCs posed additional issues. Despite a focus on LBP-related MoCs, other relevant studies concerning spinal disorders may have been missed. To mitigate these issues, a broad and sensitive search strategy, an overinclusion approach during screening, several adjustments to the extraction form and regular reviewer discussions were employed. Yet, the diversity in MoC reporting possibly led to the omission of certain information, even though specific frameworks and a continuously adapted data form were utilised to tackle this challenge.
Implications
Throughout this process, it became evident that most of the MoCs implemented for LBP in primary healthcare are still under investigation and require further testing to produce robust estimates of their effectiveness, as well as guidance for optimal implementation. Future research should focus on effectiveness-implementation studies with pragmatic designs to reproduce the challenges of implementing MoCs in real-world clinical settings, such as integration across care sectors and differences in funding models, context features and teams of healthcare providers.70
Additionally, in line with the recommendations for conducting scoping reviews,28 29 a quality or risk of bias assessment was not performed in this study. Systematic reviews and meta-analyses are needed to assess the methodological quality of the studies and provide stronger conclusions on their findings. This knowledge may contribute to inform health policies, interventions and infrastructures favouring the implementation of a MoC that promotes the delivery of high-quality care for LBP patients in the most efficient and sustainable way for health systems.
Finally, this scoping review sheds light on features shared by MoCs for LBP, offering a detailed insight into their foundations, content and resource requirements. However, the heterogeneity in reporting reveals the need for guidelines on the development and the implementation of MoCs. This guidance will facilitate their transferability and adaptation to primary healthcare settings.
Conclusion
This study provides a broad overview of the key common elements of eleven MoCs implemented for LBP patients in primary healthcare worldwide. These MoCs are aligned with clinical practice guideline recommendations. Primary healthcare is the entry point for patients into the health system and they are offered stratified care approaches, based on education, exercise and manual therapy. More complex interventions or referrals to secondary and tertiary care are feasible options when first approaches fail. However, most studies were very heterogeneous in reporting care coordination and its delivery over time. Additionally, most MoCs are not integrated into health systems and are still in the early stages of research. These findings highlight the need for guidelines to support the research, development and implementation of MoCs in real-world settings.
Supplementary Material
Acknowledgments
The authors gratefully thank the late Professor Carla Nunes for considerable help and inspiration in the design and development of this study.
Footnotes
@donato_h, @bruno_m_heleno, @EBCRUZ64
Contributors: STD, EBC, PA and DC conceived the study. HD supported the formulation of search strategies and the literature search. Title and abstract screening were performed by STD and DC. Full-text screening and data extraction were carried out by STD and AM with the support of DC to solve disagreements. Data analysis was performed by STD and discussed with EBC, PA and BH throughout the process. STD is the guarantor of the study and drafted this manuscript. All authors revised and approved the final version of the manuscript.
Funding: This project is supported by FCT—Fundação para a Ciência e a Tecnologia, I.P., under the PhD grant awarded to STD (UI/BD/150882/2021) and the MyBack project (PTDC/SAU-SER/7406/2020), in which EBC is the principal investigator.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable as no datasets were generated for this study. All relevant data were included in the article or as online supplemental file. Additional data are not available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
As this study involves a secondary analysis of previously published data, ethical approval is not required.
References
- 1. GBD 2021 Low Back Pain Collaborators . Global, regional, and national burden of low back pain, 1990 – 2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol 2023;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wasiak R, Kim JY, Pransky G. Work disability and costs caused by recurrence of low back pain: longer and more costly than in first episodes. Spine 2006;31:219–25. 10.1097/01.brs.0000194774.85971.df [DOI] [PubMed] [Google Scholar]
- 3. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. The Lancet 2018;391:2356–67. 10.1016/S0140-6736(18)30480-X [DOI] [PubMed] [Google Scholar]
- 4. Gouveia N, Canhão H, Branco JC. The Burden of Chronic Low Back Pain in the Adult Portuguese Population: An Epidemiological Population-Based Study Under the Scope of Epireumapt. Faculdade de Ciências Médicas da Universidade Nova de Lisboa, 2015. [Google Scholar]
- 5. Gouveia N, Rodrigues A, Eusébio M, et al. Prevalence and social burden of active chronic low back pain in the adult Portuguese population: results from a national survey. Rheumatol Int 2016;36:183–97. 10.1007/s00296-015-3398-7 [DOI] [PubMed] [Google Scholar]
- 6. Lemmers GPG, van Lankveld W, Westert GP, et al. Imaging versus no imaging for low back pain: a systematic review, measuring costs, Healthcare utilization and absence from work. Eur Spine J 2019;28:937–50. 10.1007/s00586-019-05918-1 [DOI] [PubMed] [Google Scholar]
- 7. Kim LH, Vail D, Azad TD, et al. Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA Netw Open 2019;2:e193676. 10.1001/jamanetworkopen.2019.3676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018;27:2791–803. 10.1007/s00586-018-5673-2 [DOI] [PubMed] [Google Scholar]
- 9. Dziedzic KS, French S, Davis AM, et al. Implementation of musculoskeletal models of care in primary care settings: theory, practice, evaluation and outcomes for musculoskeletal health in high-income economies. Best Pract Res Clin Rheumatol 2016;30:375–97. 10.1016/j.berh.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 10. Beyera GK, O’Brien J, Campbell S. Health-care utilisation for low back pain: a systematic review and meta-analysis of population-based observational studies. Rheumatol Int 2019;39:1663–79. 10.1007/s00296-019-04430-5 [DOI] [PubMed] [Google Scholar]
- 11. National Institute for Health and Care Excellence . Low back pain and sciatica in over 16S: assessment and management: full guideline: assessment and noninvasive treatments. Royal College of Physicians 2016. [Google Scholar]
- 12. Chenot JF, Greitemann B, Kladny B, et al. Clinical practice guideline: non-specific low back pain. Dtsch Arztebl Int 2017;114:883–90. 10.3238/arztebl.2017.0883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American college of physicians. Ann Intern Med 2017;166:514–30. 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- 14. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med 2020;54:79–86. 10.1136/bjsports-2018-099878 [DOI] [PubMed] [Google Scholar]
- 15. Buchbinder R, Underwood M, Hartvigsen J, et al. The lancet series call to action to reduce low value care for low back pain: an update. Pain 2020;161 Suppl 1:S57–64. 10.1097/j.pain.0000000000001869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Powell AC, Rogstad TL, Elliott SW, et al. Health care utilization and pain outcomes following early imaging for low back pain in older adults. J Am Board Fam Med 2019;32:773–80. 10.3122/jabfm.2019.06.190103 [DOI] [PubMed] [Google Scholar]
- 17. Speerin R, Needs C, Chua J, et al. Implementing models of care for musculoskeletal conditions in health systems to support value-based care. Best Pract Res Clin Rheumatol 2020;34:S1521-6942(20)30065-6. 10.1016/j.berh.2020.101548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet 2018;391:2368–83. 10.1016/S0140-6736(18)30489-6 [DOI] [PubMed] [Google Scholar]
- 19. Hall AM, Scurrey SR, Pike AE, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: A systematic review and synthesis of qualitative studies using the theoretical domains framework. Implementation Sci 2019;14:1–19. 10.1186/s13012-019-0884-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Traeger AC, Buchbinder R, Elshaug AG, et al. Care for low back pain: can health systems deliver Bull World Health Organ 2019;97:423–33. 10.2471/BLT.18.226050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Briggs AM, Chan M, Slater H. Models of care for musculoskeletal health: moving towards meaningful implementation and evaluation across conditions and care settings. Best Practice & Research Clinical Rheumatology 2016;30:359–74. 10.1016/j.berh.2016.09.009 [DOI] [PubMed] [Google Scholar]
- 22. Briggs AM, Jordan JE, Jennings M, et al. A Framework to Evaluate Musculoskeletal Models of Care. Cornwall, UK, 2016. Available: http://bjdonline.org/a-framework-to-evaluate-musculoskeletal-models-of-care/ [Google Scholar]
- 23. Speerin R, Slater H, Li L, et al. Moving from evidence to practice: models of care for the prevention and management of musculoskeletal conditions. Best Pract Res Clin Rheumatol 2014;28:479–515. 10.1016/j.berh.2014.07.001 [DOI] [PubMed] [Google Scholar]
- 24. Chehade MJ, Yadav L, Kopansky-Giles D, et al. Innovations to improve access to musculoskeletal care. Best Pract Res Clin Rheumatol 2020;34:101559. 10.1016/j.berh.2020.101559 [DOI] [PubMed] [Google Scholar]
- 25. Kongsted A, Kent P, Quicke JG, et al. Risk-stratified and stepped models of care for back pain and osteoarthritis: are we heading towards a common model PAIN Rep 2020;5:e843. 10.1097/PR9.0000000000000843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Costa N, Blyth FM, Amorim AB, et al. Implementation initiatives to improve low back pain care in Australia: A Scoping review. Pain Medicine 2022;23:1979–2009. 10.1093/pm/pnac102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Murphy C, French H, McCarthy G, et al. Clinical pathways for the management of low back pain from primary to specialised care: a systematic review. Eur Spine J 2022;31:1846–65. 10.1007/s00586-022-07180-4 [DOI] [PubMed] [Google Scholar]
- 28. Pollock D, Peters MDJ, Khalil H, et al. Recommendations for the extraction, analysis, and presentation of results in Scoping reviews. JBI Evid Synth 2023;21:520–32. 10.11124/JBIES-22-00123 [DOI] [PubMed] [Google Scholar]
- 29. Peters MDJ, Godfrey C, McInerney P, et al. Best practice guidance and reporting items for the development of Scoping review protocols. JBI Evid Synth 2022;20:953–68. 10.11124/JBIES-21-00242 [DOI] [PubMed] [Google Scholar]
- 30. Duarte ST, Nunes C, Costa D, et al. Models of care for low back pain patients in primary Healthcare: a Scoping review protocol. BMJ Open 2022;12:e053848. 10.1136/bmjopen-2021-053848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. World Health Organization . Operational framework for primary health care. 2020. Available: https://www.who.int/publications/i/item/9789240017832
- 32. Peters MD, Godfrey C, McInerney P, et al. Chapter 11: Scoping reviews. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. 2021. [Google Scholar]
- 33. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 34. Hill JC, Whitehurst DGT, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (start back): A randomised controlled trial. Lancet 2011;378:1560–71. 10.1016/S0140-6736(11)60937-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Whitehurst D, Bryan S, Lewis M, et al. Exploring the cost-utility of stratified primary care management for low back pain compared with current best practice within risk-defined subgroups. Ann Rheum Dis 2012;71:1796–802. 10.1136/annrheumdis-2011-200731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hsu C, Evers S, Balderson BH, et al. Adaptation and implementation of the start back risk stratification strategy in a US health care organization: A process evaluation. Pain Medicine 2019;20:1105–19. 10.1093/pm/pny170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Beneciuk JM, George SZ, Greco CM, et al. Targeted interventions to prevent Transitioning from acute to chronic low back pain in high-risk patients: development and delivery of a pragmatic training course of psychologically informed physical therapy for the TARGET trial. Trials 2019;20:256. 10.1186/s13063-019-3350-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Middleton A, Fitzgerald GK, Delitto A, et al. Implementing stratified care for acute low back pain in primary care using the start back instrument: a process evaluation within the context of a large pragmatic cluster randomized trial. BMC Musculoskelet Disord 2020;21:776. 10.1186/s12891-020-03800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Delitto A, Patterson CG, Stevans JM, et al. Stratified care to prevent chronic low back pain in high-risk patients: the TARGET trial. A multi-site pragmatic cluster randomized trial. EClinicalMedicine 2021;34:100795. 10.1016/j.eclinm.2021.100795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schröder K, Öberg B, Enthoven P, et al. Confidence, attitudes, beliefs and determinants of implementation Behaviours among Physiotherapists towards clinical management of low back pain before and after implementation of the Betterback model of care. BMC Health Serv Res 2020;20:443:443. 10.1186/s12913-020-05197-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Enthoven P, Eddeborn F, Abbott A, et al. Patients’ experiences of the Betterback model of care for low back pain in primary care - a qualitative interview study. Int J Qual Stud Health Well-Being 2021;16:1861719. 10.1080/17482631.2020.1861719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schröder K, Öberg B, Enthoven P, et al. Effectiveness and quality of implementing a best practice model of care for low back pain (Betterback) compared with routine care in Physiotherapy: A hybrid type 2 trial. J Clin Med 2021;10:1230. 10.3390/jcm10061230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schröder K, Öberg B, Enthoven P, et al. Improved adherence to clinical guidelines for low back pain after implementation of the Betterback model of care: A stepped cluster randomized controlled trial within a hybrid type 2 trial. Physiother Theory Pract 2023;39:1376–90. 10.1080/09593985.2022.2040669 [DOI] [PubMed] [Google Scholar]
- 44. Greenhough C. National back pain and Radicular pain pathway 2017 - including implementation of NICE guidance Ng59. Trauma Program Care NHS Engl 2017. [Google Scholar]
- 45. Ryan C, Pope CJ, Roberts L. Why managing sciatica is difficult: patients’ experiences of an NHS sciatica pathway. A qualitative, interpretative study. BMJ Open 2020;10:e037157. 10.1136/bmjopen-2020-037157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Foster NE, Mullis R, Hill JC, et al. Effect of stratified care for low back pain in family practice (impact back): a prospective population-based sequential comparison. Ann Fam Med 2014;12:102–11. 10.1370/afm.1625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Martin D, Ryan C, Wellburn S, et al. The north of England regional back pain and Radicular pain pathway: evaluation. 2018;1–26.
- 48. Jess M-A, Ryan C, Hamilton S, et al. Does duration of pain at baseline influence clinical outcomes of low back pain patients managed on an evidence-based pathway? spine Spine 2018;43:E998–1004. 10.1097/BRS.0000000000002612 [DOI] [PubMed] [Google Scholar]
- 49. Jess M-A, Ryan C, Hamilton S, et al. Does duration of pain at baseline influence longer-term clinical outcomes of low back pain patients managed on an evidence-based pathway? spine Spine 2021;46:191–7. 10.1097/BRS.0000000000003760 [DOI] [PubMed] [Google Scholar]
- 50. Cheshire A, Polley M, Peters D, et al. Patient outcomes and experiences of an Acupuncture and self-care service for persistent low back pain in the NHS: A mixed methods approach. BMC Complement Altern Med 2013;13:1:300. 10.1186/1472-6882-13-300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gurden M, Morelli M, Sharp G, et al. Evaluation of a general practitioner referral service for manual treatment of back and neck pain. Prim Health Care Res Dev 2012;13:204–10. 10.1017/S1463423611000648 [DOI] [PubMed] [Google Scholar]
- 52. Zarrabian M, Bidos A, Fanti C, et al. Improving spine surgical access, appropriateness and efficiency in metropolitan, urban and rural settings. Can J Surg 2017;60:342–8. 10.1503/cjs.016116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kindrachuk DR, Fourney DR. Spine surgery referrals redirected through a Multidisciplinary care pathway: effects of Nonsurgeon triage including MRI utilization. J Neurosurg Spine 2014;20:87–92. 10.3171/2013.10.SPINE13434 [DOI] [PubMed] [Google Scholar]
- 54. Wilgenbusch CS, Wu AS, Fourney DR. Triage of spine surgery referrals through a Multidisciplinary care pathway: A value-based comparison with conventional referral processes. Spine (Phila Pa) 1976;39:S129–35. 10.1097/BRS.0000000000000574 [DOI] [PubMed] [Google Scholar]
- 55. Moi JHY, Phan U, de Gruchy A, et al. Is establishing a specialist back pain assessment and management service in primary care a safe and effective model? twelve-month results from the back pain assessment clinic (BAC) prospective cohort pilot study. BMJ Open 2018;8:e019275. 10.1136/bmjopen-2017-019275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Whitehurst DGT, Bryan S, Lewis M, et al. Implementing stratified primary care management for low back pain: cost-utility analysis alongside a prospective, population-based, sequential comparison study. Spine (Phila Pa 1976) 2015;40:405–14. 10.1097/BRS.0000000000000770 [DOI] [PubMed] [Google Scholar]
- 57. Murphy SE, Blake C, Power CK, et al. Comparison of a stratified group intervention (start back) with usual group care in patients with low back pain: A Nonrandomized controlled trial. SPINE 2016;41:645–52. 10.1097/BRS.0000000000001305 [DOI] [PubMed] [Google Scholar]
- 58. Morsø L, Olsen Rose K, Schiøttz-Christensen B, et al. Effectiveness of stratified treatment for back pain in Danish primary care: A randomized controlled trial. Eur J Pain 2021;25:2020–38. 10.1002/ejp.1818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Saunders B, Konstantinou K, Artus M, et al. “Patients’ and Clinicians’ perspectives on a “fast-track” pathway for patients with sciatica in primary care: qualitative findings from the Scopic stratified care trial”. BMC Musculoskelet Disord 2020;21:469. 10.1186/s12891-020-03483-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Konstantinou K, Lewis M, Dunn KM, et al. Stratified care versus usual care for management of patients presenting with sciatica in primary care (Scopic): a randomised controlled trial [with consumer summary]. Lancet Rheumatol 2020;2:e401–11. 10.1016/S2665-9913(20)30099-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Foster NE, Konstantinou K, Lewis M, et al. Stratified versus usual care for the management of primary care patients with sciatica: the Scopic RCT. Health Technol Assess 2020;24:1–130. 10.3310/hta24490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Cherkin D, Balderson B, Wellman R, et al. Effect of low back pain risk-stratification strategy on patient outcomes and care processes: the MATCH randomized trial in primary care. J Gen Intern Med 2018;33:1324–36. 10.1007/s11606-018-4468-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet 2018;391:2384–8. 10.1016/S0140-6736(18)30488-4 [DOI] [PubMed] [Google Scholar]
- 64. Hanney WJ, Masaracchio M, Liu X, et al. The influence of physical therapy guideline adherence on Healthcare utilization and costs among patients with low back pain: A systematic review of the literature. PLoS One 2016;11:e0156799. 10.1371/journal.pone.0156799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Schröder K. Implementing BetterBack – a Best Practice Physiotherapy Healthcare Model for Low Back Pain Clinician and Patient Evaluation. Linköping: Linköping University Medical Dissertations, Available: https://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-179586 [Google Scholar]
- 66. Lau R, Stevenson F, Ong BN, et al. Achieving change in primary care-causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci 2016;11:40. 10.1186/s13012-016-0396-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Ogbeivor C, Elsabbagh L. Management approach combining Prognostic screening and targeted treatment for patients with low back pain compared with standard Physiotherapy: A systematic review & meta-analysis. Musculoskeletal Care 2021;19:436–56. 10.1002/msc.1541 [DOI] [PubMed] [Google Scholar]
- 68. Agency for Clinical Innovation . Management of people with acute low back pain - model of care. Rev Prat 2016;58. [Google Scholar]
- 69. Wambeke P, Desomer A, Ailliet L, et al. Low back pain and Radicular pain: assessment and management 2017. 2017.
- 70. Coeckelberghs E, Verbeke H, Desomer A, et al. International comparative study of low back pain care pathways and analysis of key interventions. Eur Spine J 2021;30:1043–52. 10.1007/s00586-020-06675-2 [DOI] [PubMed] [Google Scholar]
- 71. Schultz EM, McDonald KM. What is care coordination. Int J Care Coordination 2014;17:5–24. 10.1177/2053435414540615 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-079276supp001.pdf (36.6KB, pdf)
bmjopen-2023-079276supp002.pdf (63.2KB, pdf)
bmjopen-2023-079276supp003.pdf (84KB, pdf)
bmjopen-2023-079276supp004.pdf (195.4KB, pdf)
bmjopen-2023-079276supp005.pdf (150.3KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable as no datasets were generated for this study. All relevant data were included in the article or as online supplemental file. Additional data are not available.