Abstract
Background:
A notable shift in healthcare policy is healthcare privatization, which refers to the transfer of ownership, management, or provision of healthcare services from the public sector to private entities.
Objectives:
To provide a narrative examination of the impact of privatization on various dimensions of healthcare, including quality, equity, accessibility, and cost-effectiveness. Policymakers can utilize the findings of this study to make well-informed decisions regarding privatization strategies.
Materials and Methods:
A systematic review was implemented using the following databases: PubMed, Scopus, and Google Scholar. Studies conducted from January 2000 to January 2023 in developing or developed countries that assessed the impact of healthcare privatization on population health within public sector institutions were included.
Results:
Eleven studies were included. The findings revealed diverse perspectives on the impact of healthcare privatization, with four studies (36.4%) supporting privatization (two of these were conducted in Saudi Arabia), six studies (54.5%) opposing it (three of these were conducted in European countries), and one study (9.1%) taking a neutral stance. Two studies investigated the impact on healthcare quality, and both revealed that privatization negatively impacts uninsured patients and low-income populations. In addition, five studies investigated the healthcare access and equity dimensions following privatization: one was in favor, one was neutral, and three were opposing it. Four studies investigated the cost-effectiveness dimension, with three in favor and one study opposing it.
Conclusion:
This review highlights different perspectives on healthcare privatization. While studies, as those from Saudi Arabia, suggest benefits in terms of efficiency and innovation, others, particularly from European countries, emphasize negative consequences such as inequity and reduced quality. This emphasizes the need for more investigations to understand privatization’s impact on healthcare.
Keywords: Access to care, healthcare, healthcare delivery, impact, private sector, privatization, quality of health care, system
INTRODUCTION
The global healthcare landscape has undergone significant transformations in response to the growing demand for healthcare services, budget constraints, and the pursuit of efficiency and quality.[1] One of the notable shifts in healthcare policy and delivery is the privatization of healthcare systems. Privatization in healthcare refers to the transfer of ownership, management, or provision of healthcare services from the public sector to private entities, such as for-profit corporations, non-profit organizations, or individual practitioners.[2] This change in ownership and management structure has generated extensive discourse among policymakers, healthcare professionals, and the public.[1] The context of healthcare privatization is shaped by various factors, including economic, political, and social considerations.[3] Several countries have implemented privatization initiatives in their healthcare systems,[1] often driven by the belief that private involvement can lead to efficiency improvements, cost savings, and enhanced service quality.[2] However, the impact of healthcare privatization is complex and context-dependent.
Privatization has been linked to increased growth and profitability in public firms, but its impact on consumers is not well-explored.[4] In the US hospital sector, public control (the degree of government or public influence and management over hospitals) decreased by 42% between 1983 and 2019, raising concerns about potential trade-offs.[4] The decline in public control implies an increase in privatization or a shift toward private ownership and management of hospitals. In addition, private operators enhance hospitals’ financial performance by increasing mean revenue per patient. However, this is achieved, in part, by selectively reducing the intake of low-income patients, leading to an aggregate decline in their utilization and suggesting a potential decrease in access to care.[4] Thus, there is a need to consider both the financial benefits and the impact on healthcare access when assessing hospital privatization.
The aim of this systematic review was to provide an exhaustive examination of the impact of healthcare system privatization on various dimensions of healthcare, including quality, equity, accessibility, and cost-effectiveness. Policymakers, healthcare administrators, and stakeholders can utilize the findings to make well-informed decisions regarding privatization strategies.
MATERIALS AND METHODS
The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines.[5]
Information sources and search strategy
A comprehensive literature review was conducted using the following databases: PubMed, Scopus, and Google Scholar. Studies published between January 2000 and January 2023, when the final search was carried out for all databases, were included. Appendix A provides the complete search strategy.
Eligibility criteria
The included studies adhered to the following criteria: were published in English, the full text was available, had an observational or interventional study design, and assessed the impact of healthcare privatization. Conversely, only abstracts, conference abstracts, letters to the editor, short communications, and meta-analyses were excluded. In addition, studies published before 2000 were excluded because the healthcare landscape and policies are dynamic and subject to continuous changes,[1] and thus the time-based inclusion criteria allowed capturing the most recent and relevant information regarding healthcare privatization.
Selection and data extraction process
In terms of selection, studies of any populations (in developed or developing countries) whose health might be affected by privatization were included to avoid findings confounded by the more fundamental socioeconomic or political transformations accompanying privatization policies. Two investigators (T.M.A.) and (R.T.A.) independently screened the titles and abstracts of the studies retrieved in the searches. Then, another two reviewers (A.S.A. and I.A.A.) individually examined the titles and abstracts of articles that broadly matched the inclusion criteria. Subsequently, the two initial investigators (T.M.A. and R.T.A.) assessed the full text of the identified articles to ascertain their eligibility for the study. Any disagreements between the investigators were resolved through discussions.
Data were extracted using a standard data extraction sheet. This study was particularly focused on the effect of healthcare privatization on the various dimensions of healthcare, including quality, equity, accessibility, and cost-effectiveness. Data were extracted based on the PICO framework,[6] as follows:
Population (P): The population encompassed individuals, patients or consumers, in developing and/or developed countries who benefit from the healthcare systems.
Intervention (I): The focal intervention was the privatization of healthcare services. Privatization was defined as the transfer (either complete or partial) of public assets and shares to private ownership as well as the facilitation of substantial private-sector investment in a healthcare business.[7]
Comparison (C): The studies evaluated or assessed the impact of healthcare privatization on healthcare.
Outcome (O): Outcome measures comprised both routinely collected and self-reported data, which gauged the effects of healthcare privatization on various aspects. These included physical health, mental health, injuries, absenteeism, financial burden, patient influx, patient access, patient and healthcare provider satisfaction, and staff satisfaction.
Assessment of study quality
The quality assessment of the included studies was independently evaluated by two reviewers (T.M.A. and I.A.A.) using the quality assessment tools for observational cohort and cross-sectional studies developed by the National Institutes of Health.[8] Then, with agreement between all the authors, each study’s quality rating was labeled as poor (i.e., a score of 0–4 of 14), fair (5–10), and good (11–14).
Data synthesis
Meta-analysis was not possible due to various reasons, including lack of homogeneity in the interventions and outcomes. Therefore, this systematic review uses a narrative synthesis, which allows inclusion of diverse study designs (qualitative and quantitative) without requiring data homogeneity for statistical pooling, thereby enabling a comprehensive exploration of the impact of privatization of the healthcare system.
RESULTS
In the initial searches, 175 papers were retrieved from PubMed, 200 from Google Scholar, and 25 from Scopus. After removing duplicates and applying the inclusion/exclusion criteria, 11 studies were included in the narrative synthesis [Figure 1]. The study encompassed different study designs, with a significant focus on cross-sectional and multi-model surveys. For the risk of bias, six studies received a fair rating, while five received a good rating [Table 1].
Figure 1.
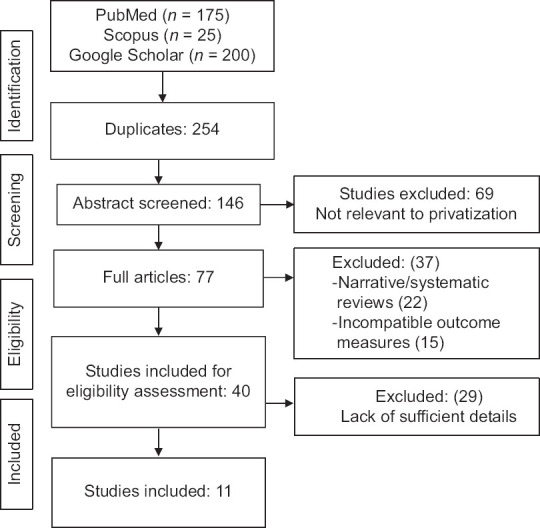
The PRISMA flow diagram depicts the flow of information through the different phases of a systematic review
Table 1.
Characteristics of the included studies (N=11)
| Study | Year | Objectives | Settings | Study design | Quality rating |
|---|---|---|---|---|---|
| Al-Jazaeri et al.[9] | 2017 | To assess the difference after cholecystectomy surgery within private and public healthcare facilities in Saudi Arabia | University hospital (Department of Surgery, College of Medicine, King Saud University) in Riyadh, Saudi Arabia | Cross-sectional study | Fair |
| Alkhamis et al.[10] | 2017 | To investigate the personal and workplace characteristics of uninsured expatriate males in Saudi Arabia | Male expatriate employees in businesses/companies in Riyadh, Saudi Arabia | Cross-sectional study | Fair |
| Yip and Hsiao[11] | 2014 | To assess the effects of privatization on all healthcare facilities in China | Healthcare facilities in China | Database analysis | Fair |
| Dahlgren[12] | 2014 | Examining the main effect of the first two phases of health-care reform in Sweden | Private hospitals in Sweden | Comparative study (before and after privatization) | Good |
| Villa and Kane[13] | 2013 | To analyze the impact of privatization on different dimensions: Efficiency, profitability and benefits to the community | Privatized hospitals in three American states (California, Florida, and Massachusetts) | Longitudinal analysis | Good |
| Davari et al.[14] | 2012 | To evaluate issues related to financing of healthcare system and relevant government policies in Iran | Public hospitals in Iran | Interview-based, qualitative study | Fair |
| Tiemann and Schreyögg[15] | 2012 | To assess technical efficacy and changes within hospitals after privatization | Privatized hospitals in Germany | Observational, prospective analysis | Good |
| Waitzkin et al.[16] | 2007 | To provide an empirical response to the World Bank and Wharton School’s proposals regarding the privatization of health services in less developed countries | Private hospitals in the United States, Argentina, Chile, and Mexico | Multi-method study design | Good |
| Maarse[17] | 2006 | To evaluate the effects of privatization on public and private healthcare setups | The public-private mix in health care in eight European countries: Germany, France, Belgium, Spain, Italy, Sweden, Hungary, and The Netherlands | Longitudinal analysis | Good |
| Ovretveit[18] | 2003 | To evaluate the impact of privatization and private healthcare in Nordic countries, specifically in terms of healthcare financing and service quality | The raw data were provided by statistical sources in each country. The Nordic countries include Denmark, Norway, Sweden, Finland, Iceland, the Faroe Islands, Greenland, and Åland Islands | Multi-methods, survey-based quantitative study | Fair |
| Shen[19] | 2003 | To evaluate the effects of ownership conversion on hospital financial conditions, administration, staffing, capacity, and unprofitable care | The study utilized hospital-level data from the American Hospital Association Annual Surveys, Medicare hospital cost reports, and Frank Sloan of Duke University in the United States | Cross-sectional study | Fair |
Table 2 provides a summary of the included studies. The findings reveal diverse perspectives on the impact of healthcare privatization, with four studies (36.4%) supporting privatization,[9,10,13,15] six studies (54.5%) opposing it,[12,14,16,17,18,19] and one study (9.1%) taking a neutral stance[11] [Figure 2].
Table 2.
Summary of the included studies (N=11)
| Study | Results | Comments | Country classification by the United Nations | Conclusion |
|---|---|---|---|---|
| Al-Jazaeri et al.[9] | Public sector hospitals have shorter symptom duration but longer waiting times and hospital stays compared to private hospitals, suggesting private hospitals have quicker surgery access | The study’s title and objective are not matched, and it failed to identify financial issues among participants or compare public and private hospitals to interpret results | Saudi Arabia: Developing country (high-income) | Favor privatization |
| Alkhamis et al.[10] | Private hospitals had shorter hospitalization durations (1 day) compared to public hospitals (2 days), and patients in private hospitals were more likely to be admitted on the same day of diagnosis | Private provider’s samples were from a specific medical facility, not representing the entire uninsured expatriate population, and it did not compare two similar populations (private and public hospitals), making interpretation challenging | Saudi Arabia: Developing country (high-income) | Favor privatization |
| Yip and Hsiao[11] | Countries with higher gross domestic product, such as Taiwan, Hong Kong, Singapore, and Japan, had better access to healthcare services. Additionally, it was observed that some facilities in China adopted stringent policies, like “hospital zero drug policies,” which helped maintain safety and high-quality care | The study does not explicitly take a position either in favor of or against privatization. Instead, it emphasizes that no single policy would provide a magic solution to improving China’s healthcare system. It suggests measures like improved public hospital accountability, better care coordination, and performance-based purchasing to achieve a cost-effective and high-quality system | China: Developing country (upper middle income) | Neutral toward privatization |
| Dahlgren[12] | Privatization has led to increased inequity in healthcare access, shifting patient care priorities, and compromising accessibility and quality of care, especially for patients with minor health issues compared to those with multiple health problems | The findings might not be directly applicable to healthcare systems in other countries with different contexts. The study did not examine the long-term impacts of privatization, and the observed effects on equity and quality may have evolved over time | Sweden: Developed country (high-income) | Oppose privatization |
| Villa and Kane[13] | The study revealed that the conversion of public hospitals to private ownership resulted in a slight decrease in overall profitability, with a total margin difference of−0.18%. Yet, the conversion resulted in a 6.6% increase in the operating margin, indicating enhanced efficiency and profitability | The study, primarily focusing on the US context, may not be applicable to other countries and may not explore potential consequences for access to care, service quality, or equity | US: Developed country (high-income) | Favor privatization |
| Davari et al.[14] | Privatization led to a decrease in healthcare services utilization, limited financial resources, and negative impacts on healthcare outcomes due to under-the-table fees and informal payments | The study, primarily focusing on Iran, provides valuable insights into the potential drawbacks of healthcare privatization in Iran, but its findings may not be universally applicable due to variations in healthcare structures and policies | Iran: Developing country (upper middle income) | Oppose privatization |
| Tiemann and Schreyögg[15] | Privatized hospitals showed significant improvements in efficiency metrics (2.9%–4.9%), including changes in bed numbers, efficiency of nonprofit and profit-based hospitals, and bed allocation, with for-profit hospitals showing increased efficiency and patient satisfaction | The study’s findings are limited to a specific context and may not be applicable to other healthcare systems. It primarily focused on efficiency measures and did not address potential impacts of privatization on healthcare quality, access, or costs | Germany: Developed country (high-income) | Favor privatization |
| Waitzkin et al.[16] | The results of the study indicated that the benefits of privatization, as advocated by these institutions, were less pronounced than expected. Access to healthcare did not substantially improve, especially for vulnerable populations, despite the push for privatization | The study’s limitations include its focus on specific countries and contexts, and its reliance on World Bank and Wharton School proposals, suggesting a need for further research to understand the effects of health service privatization in less developed countries | Developed: US (high-income) Developing: Chile (high-income) Mexico and Argentina (upper middle income) | Oppose privatization |
| Maarse[17] | The study found that privatization negatively impacts healthcare quality and equality, especially for financially dependent populations, and may worsen disparities in access and care | The study’s findings, based on specific policies and approaches in eight European countries, may vary in their impact on privatization and healthcare systems, highlighting potential regional variations | All developed countries: Germany, France, Belgium, Spain, Italy, Sweden, and the Netherlands (high-income) But Hungary (upper middle income) | Oppose privatization |
| Ovretveit[18] | Privatization led to increased patient service fees and a decline in healthcare quality, with insured patients receiving lower care than private patients, potentially causing negative consequences | The study’s findings may not be universally applicable due to its specificity to the Nordic context and its potential influence on other regions with different healthcare systems and policies | Developed: Denmark, Norway, Sweden, Finland, Iceland (high-income) Developing: Faroe Islands, Greenland, and Åland Islands (high-income) | Oppose privatization |
| Shen[19] | Privatized hospitals faced lower staffing levels and budgetary challenges compared to non-privatized hospitals | The study’s limitations include unaddressed confounding variables and potential universal applicability due to the potential varying impact of ownership conversions on hospital performance | US: Developed country (high-income) | Oppose privatization |
Figure 2.
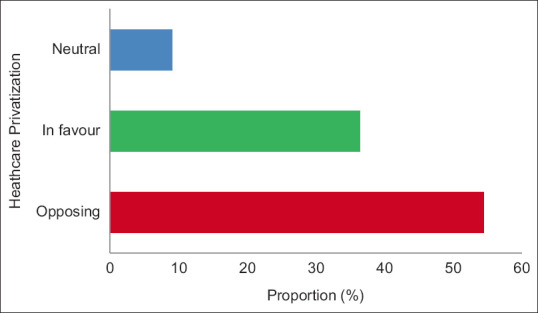
Categorization of the included studies’ conclusion toward healthcare privatization
Impact of privatization on healthcare quality
Maarse’s examination of healthcare privatization in European nations revealed negative effects on healthcare quality and equality, particularly impacting financially vulnerable populations.[17] Ovretveit’s study on Nordic privatization indicated increased patient service fees and declining healthcare quality, particularly for insured patients.[18]
Effect of privatization on healthcare access and equity
Al-Jazaeri et al.’s study on cholecystectomy surgery in Saudi Arabia found that patients in public-sector hospitals have shorter symptom duration but longer waiting times and hospital stays compared with those attending private hospitals, suggesting that private hospitals provide quicker surgery access and shorter waiting times and hospitalization periods.[9]
Conversely, Dahlgren’s assessment of healthcare reforms in Sweden found a connection between privatization and increased healthcare access inequality. Privatization resulted in a shift in patient care priorities, favoring minor health issues over complex ones, ultimately compromising access and overall care quality.[12] Davari et al.’s study in Iran identified adverse outcomes of privatization, including decreased healthcare service utilization and financial resources as well as negative impact on healthcare outcomes due to under-the-table fees and informal payments.[14] Waitzkin et al.’s research on healthcare privatization in less-developed countries reported that privatization did not substantially improve access to healthcare, especially for vulnerable populations.[16]
However, Yip’s and Hsiao’s study in China offers a nuanced perspective, emphasizing the link between higher gross domestic product (GDP) and enhanced healthcare access in privatized systems without explicitly endorsing or opposing privatization.[11]
Cost-effectiveness of privatization
Three studies demonstrated a positive impact on this dimension. Alkhamis et al.’s study in Saudi Arabia emphasized on the effectiveness in private hospitals, where shorter hospitalization durations and same-day admissions were observed.[10] Tiemann and Schreyögg’s analysis of hospital efficiency after privatization showed significant improvements in various efficiency metrics, including changes in number of beds, the efficiency of non-profit and for-profit hospitals, and bed allocation. Notably, for-profit hospitals displayed increased efficiency and higher patient satisfaction.[15] A study by Villa and Kane in the United States suggests that converting public hospitals to private ownership can enhance efficiency and profitability, supporting the argument that privatization can improve the sustainability of universal health coverage systems.[13] In contrast, the study by Shen raised concerns about the cost-effectiveness of privatization, as it was found that privatized hospitals faced lower staffing levels and budgetary challenges compared with non-privatized hospitals.[19]
DISCUSSION
This systematic review, based on an analysis of 11 selected studies, provides a comprehensive examination of the impact of healthcare privatization. The review’s findings offer significant insights into the ongoing debate on healthcare privatization. Notably, the results indicate a diversity of perspectives on the effects of privatization in healthcare as specified below.
Impact on healthcare quality
Maarse[17] and Ovretveit[18] demonstrated that privatization has a negative impact on healthcare quality, particularly affecting uninsured patients and low-income populations. Similarly, Basu et al. expressed concerns about privatization’s impact on healthcare quality, highlighting reduced quality in privatized healthcare settings, especially regarding safety and equitable care delivery.[20]
On the other hand, a study by Passalent et al. demonstrated that privatization was associated with higher patient satisfaction scores, suggesting that the private sector may excel in delivering quality care.[21] However, the heterogeneity of findings across studies underscores the context-specific nature of the impact of privatization on healthcare quality.
Effect on healthcare access and equity
Equity and access to healthcare services are central concerns in the healthcare privatization debate, and the literature presents mixed findings on these issues.
For positive impact, only Al-Jazaeri et al.’s study in this review clearly demonstrated that privatization leads to more efficient healthcare delivery by shorter waiting times, shorter hospitalization periods, and quicker surgery access.[9] Similarly, Passalent et al.’s reported shorter waiting times in privatized settings, indicating improved access.[21]
Conversely, Dahlgren,[12] Davari et al.,[14] and Waitzkin et al.[16] reported negative impact on this dimension. They emphasized that privatization compromises healthcare access and overall care quality, especially for vulnerable populations. In addition, Dahlgren’s assessment of healthcare reforms in Sweden found a connection between privatization and increased healthcare access inequality.[12] Similarly, Basu et al. found reduced equitable access in privatized healthcare systems, particularly for marginalized populations.[20] These findings suggest that privatization may not consistently align with the goal of achieving equitable healthcare access and outcomes.
Nevertheless, Yip and Hsiao’s study in China offers a nuanced perspective, emphasizing the link between higher GDP and enhanced healthcare access in privatized systems without explicitly endorsing or opposing privatization. Instead, the study advocates for a multifaceted approach, including improved public hospital accountability, enhanced care coordination, and the implementation of performance-based purchasing, as strategies to establish a cost-effective and high-quality healthcare system.[11]
These diverse findings underscore the need for a nuanced examination of access, considering factors like affordability, geographic distribution, and the needs of vulnerable populations.
Cost-effectiveness of privatization
Three studies (Alkhamis, et al.,[10] Villa and Kane,[13] and Tiemann and Schreyögg[15]) highlight the potential cost savings, shorter hospitalization durations, and efficiency gains associated with healthcare privatization. This supports the argument that converting public hospitals to private ownership can improve the sustainability of universal health coverage systems. Correspondingly, Wallin reported that privatization was associated with lower administrative costs in healthcare systems.[22] These findings suggest that privatization may help optimize resource allocation and control expenses.
However, Shen’s study has raised concerns about the cost-effectiveness of privatization, as privatized hospitals faced lower staffing levels and budgetary challenges compared with non-privatized hospitals.[19] Similarly, an article by Rao indicated that privatization did not consistently lead to cost savings and efficiency improvements in healthcare delivery.[23] Thus, the cost-effectiveness of privatization may vary depending on the specific healthcare context, market structure, and regulatory framework.
Economic context
The majority of studies conducted in developed countries,[24] particularly in Europe, express opposition to privatizing the health sector due to adverse consequences such as inequity, reduced quality, and limited access to care,[12,17,18] whereas developing countries, exemplified by Saudi Arabia,[9,10] tend to support privatization, as it increases efficiency and improves healthcare quality. In addition, economic factors likely influence this dichotomy, as Saudi Arabia perceives privatization as an avenue to attract investment, diversify their economy, and introduce innovative practices in healthcare.[10] The economic context, thus, plays a pivotal role in shaping the differing attitudes toward healthcare privatization in developed and developing regions.
Limitations
This systematic review has several limitations that should be considered. Firstly, the review only includes studies published in English, which might introduce language bias, potentially excluding relevant research in other languages. Secondly, the included studies exhibited heterogeneity in methodology and study design, which could impact the comparability of results across different contexts. Finally, the studies found in the literature were mainly conducted in high-income or upper middle-income countries, which could have limited the generalizability of this review. Therefore, it is essential to acknowledge that the conclusions of this review represent a specific point in time and might not capture the most recent developments in healthcare privatization.
CONCLUSION
The findings of this systematic review underscore the complexity and diversity of the privatization debate in healthcare. While some studies conducted in developing countries, exemplified by Saudi Arabia, provide evidence supporting the potential benefits of privatization in terms of efficiency, innovation, and profitability, others, such as those conducted in European countries, emphasize adverse consequences, including inequity, reduced quality, and limited access to care. The variations in findings across different studies highlight the need for a balanced and context-specific assessment of the impact of privatization on healthcare systems. This comprehensive review contributes to a more informed and nuanced understanding of the multifaceted implications of healthcare privatization.
Peer review
This article was peer-reviewed by two independent and anonymous reviewers.
Data availability statement
Data sharing is not applicable for this article, as no new data were created or analyzed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix A.
Electronic search terms
| Database | PubMed |
|---|---|
| Search terms | (“finance “[MeSH Terms] OR “ invest”[MeSH Terms] OR “national”[MeSH Terms] OR “private”[MeSH Terms] AND (“healthcare “[MeSH Terms] |
| Limitations | Title/Abstract and MeSH Terms as noted above. Years selected (2000 – 2023). |
| Results | 175 |
|
| |
| Database | Google Scholar |
|
| |
| Search terms | “finance “ OR “ invest” OR “national” OR “private” OR “privatization” AND “healthcare” |
| Limitations | Years selected (2000–2023) |
| Results | 200 |
|
| |
| Database | Scopus |
|
| |
| Search terms | “finance “ OR “ invest” OR “national” OR “private” OR “privatization” AND “healthcare” OR “system” |
| Limitations | Abstract/Title/Keyword. Years selected (2000–2023) |
| Results | 25 |
REFERENCES
- 1.Saltman RB, Durán A, Dubois HF. Governing public hospitals: Reform strategies and the movement towards institutional autonomy. [[Last accessed 2023 Sept 24]];Health Policy. 2019 123:827–32. Available from: https://iris.who.int/handle/10665/326425 . [Google Scholar]
- 2.Himmelstein DU, Woolhandler S. Public health's falling share of US health spending. Am J Public Health. 2016;106:56–7. doi: 10.2105/AJPH.2015.302908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levi B, Zehavi A. Religious and ethnic identities influence on public views of privatization: The case of Israel. Policy Stud. 2023;44:236–57. [Google Scholar]
- 4.Duggan M, Gupta A, Jackson E, Templeton ZS. The Impact of Privatization: Evidence from the Hospital Sector. Cambridge, MA: National Bureau of Economic Research; 2023. [Google Scholar]
- 5.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: A key to evidence-based decisions. ACP J Club. 1995;123:A12–3. [PubMed] [Google Scholar]
- 7.Hemming MR, Mansoor MA. Privatization and Public Enterprises. International Monetary Fund. 1998. [[Last accessed 2023 Sept 24]]. Available from: https://www.elibrary.imf.org/display/book/9781557750051/9781557750051.xml .
- 8.Study Quality Assessment Tools. U. S. Department of Health and Human Services. 2021. [[Last accessed on 2023 Jun 18]]. Available from: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort .
- 9.Al-Jazaeri A, Ghomraoui F, Al-Muhanna W, Saleem A, Jokhadar H, Aljurf T. The impact of healthcare privatization on access to surgical care: Cholecystectomy as a model. World J Surg. 2017;41:394–401. doi: 10.1007/s00268-016-3739-z. [DOI] [PubMed] [Google Scholar]
- 10.Alkhamis A, Cosgrove P, Mohamed G, Hassan A. The personal and workplace characteristics of uninsured expatriate males in Saudi Arabia. BMC Health Serv Res. 2017;17:56. doi: 10.1186/s12913-017-1985-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yip W, Hsiao W. Harnessing the privatisation of China's fragmented health-care delivery. Lancet. 2014;384:805–18. doi: 10.1016/S0140-6736(14)61120-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dahlgren G. Why public health services?Experiences from profit-driven health care reforms in Sweden. Int J Health Serv. 2014;44:507–24. doi: 10.2190/HS.44.3.e. [DOI] [PubMed] [Google Scholar]
- 13.Villa S, Kane N. Assessing the impact of privatizing public hospitals in three American states: Implications for universal health coverage. Value Health. 2013;16:S24–33. doi: 10.1016/j.jval.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Davari M, Haycox A, Walley T. Health care financing in Iran;is privatization a good solution? Iran J Public Health. 2012;41:14–23. [PMC free article] [PubMed] [Google Scholar]
- 15.Tiemann O, Schreyögg J. Changes in hospital efficiency after privatization. Health Care Manag Sci. 2012;15:310–26. doi: 10.1007/s10729-012-9193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waitzkin H, Jasso-Aguilar R, Iriart C. Privatization of health services in less developed countries: An empirical response to the proposals of the World Bank and Wharton School. Int J Health Serv. 2007;37:205–27. doi: 10.2190/A1U4-7612-5052-6053. [DOI] [PubMed] [Google Scholar]
- 17.Maarse H. The privatization of health care in Europe: An eight-country analysis. J Health Polit Policy Law. 2006;31:981–1014. doi: 10.1215/03616878-2006-014. [DOI] [PubMed] [Google Scholar]
- 18.Ovretveit J. Nordic privatization and private healthcare. Int J Health Plann Manage. 2003;18:233–46. doi: 10.1002/hpm.712. [DOI] [PubMed] [Google Scholar]
- 19.Shen YC. Changes in hospital performance after ownership conversions. Inquiry. 2003;40:217–34. doi: 10.5034/inquiryjrnl_40.3.217. [DOI] [PubMed] [Google Scholar]
- 20.Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low- and middle-income countries: A systematic review. PLoS Med. 2012;9:e1001244. doi: 10.1371/journal.pmed.1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Passalent LA, Landry MD, Cott CA. Exploring wait list prioritization and management strategies for publicly funded ambulatory rehabilitation services in Ontario, Canada: Further evidence of barriers to access for people with chronic disease. Healthc Policy. 2010;5:e139–56. [PMC free article] [PubMed] [Google Scholar]
- 22.Wallin BA. Public Budgeting. New York, NY: Routledge; 2015. [[Last accessed on 2024 Jan 06]]. The need for a privatization process: Lessons from development and implementation; pp. 406–20. Available from: https://www.taylorfrancis.com/chapters/edit/10.4324/9781315701431-44/need-privatization-process-bruce-wallin . [Google Scholar]
- 23.Rao S. Is The Private Sector More Efficient? A Cautionary Tale. 2015. [[Last accessed on 2024 Jan 06]]. Available from: https://www.undp.org/sites/g/files/zskgke326/files/publications/GCPSE_Efficiency.pdf .
- 24.United Nations. World Economic Situation and Prospects. 2014. [[Last accessed on 2024 Jan 07]]. Available from: https://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_country_classification.pdf .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable for this article, as no new data were created or analyzed.


