Abstract
Background
Periprosthetic joint infection (PJI) is one of the most serious and debilitating complications that can occur after total joint arthroplasty. Therefore, early diagnosis and appropriate treatment are important for a good prognosis. Recently, molecular diagnostic methods have been widely used to detect the causative microorganisms of PJI sensitively and rapidly. The Multiplex Loop-Mediated Isothermal Amplification (LAMP) method eliminates the complex temperature cycling and delays caused by temperature transitions seen in polymerase chain reaction (PCR) methods, making it faster and easier to perform compared to PCR-based assays. Therefore, this study developed a multiplex LAMP assay for diagnosing bacterial PJI using LAMP technology and evaluated its analytical and clinical performance.
Methods
We developed a multiplex LAMP assay for the detection of five bacteria: Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus agalactiae, Pseudomonas aeruginosa, and Escherichia coli, frequently observed to be the causative agents of PJI. The method of analytical sensitivity and cross-reactivity were determined by spiking standard strains into the joint synovial fluid. The analytical sensitivity of the multiplex LAMP assay was compared with that of a quantitative real-time PCR (qPCR) assay. Clinical performance was evaluated using 20 joint synovial fluid samples collected from patients suspected of having bacterial PJI.
Results
The analytical sensitivity of the gram-positive bacterial multiplex LAMP assay and qPCR were 105/104 CFU/mL, 103/103 CFU/mL, and 105/104 CFU/mL against S. agalactiae, S. epidermidis, and S. aureus, respectively. For P. aeruginosa and E. coli, the analytical sensitivity of the multiplex LAMP and qPCR assays were 105/104 and 106/104 CFU/mL, respectively. The multiplex LAMP assay detects target bacteria without cross-reacting with other bacteria, and exhibited 100% sensitivity and specificity in clinical performance evaluation.
Conclusions
This multiplex LAMP assay can rapidly detect five high-prevalence bacterial species causing bacterial PJI, with excellent sensitivity and specificity, in less than 1 h, and it may be useful for the early diagnosis of PJI.
Introduction
Periprosthetic joint infection (PJI) is one of the most severe and devastating complications that can occur after total joint arthroplasty (TJA). PJI is associated with high morbidity and is responsible for severe transient or permanent disabilities such as arthrodesis or leg amputation [1, 2]. The incidence of PJI is estimated to be approximately 1% for shoulder and hip TJA and 2% for knee TJA [3]. Recently, as the number of patients receiving TJA has increased due to an aging society, the incidence of PJI has increased [4].
PJI was precisely defined in 2011 by a group of specialists from the Musculoskeletal Infection Society (MSIS). The task group proposed two major and five minor criteria for defining infections following prosthesis implantation [5, 6]. To diagnose PJI, a physical examination must meet one of two major criteria and at least three minor criteria [5]. Bacteria account for 97–99% of the causative agents of PJI. The two most common are gram-positive bacteria, coagulase-negative Staphylococcus (CoNS) and Staphylococcus aureus. Gram-negative bacteria are less common; however, the two most common are Escherichia coli and Pseudomonas aeruginosa [7].
PJI is diagnosed based on clinical, serological, and radiographic findings. However, clinical manifestations and serological test results are not always reliable. Preoperative inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), can be helpful and are not specific for PJI [8]. Cultures using tissue or synovial fluid are still considered the gold standard for diagnosing PJI. However, this method can be inaccurate because of several factors, such as using an inappropriate medium, short incubation time, loss of microbial load due to storage conditions, or prior antimicrobial therapy [9]. An accurate diagnosis of PJI is essential to avoid unnecessary surgical procedures and inappropriate antibiotic treatments.
Research is being conducted to detect the causative pathogens of PJI using molecular diagnostic tools, such as broad-range 16S rRNA gene polymerase chain reaction (PCR) analysis and next-generation sequencing [1, 10, 11], to overcome the limitations of culture and improve sensitivity. However, these molecular methods have only partially overcome the limitations of culture testing, such as low sensitivity, poor detection of slow-growing bacteria, and long turnaround times. The methods have limitations in routine clinical laboratories, such as the need for expensive equipment, extended reaction times, and well-trained technicians [4].
Loop-mediated isothermal amplification (LAMP) is a well-established isothermal technique used to detect target nucleic acid sequences. The approach is a highly sensitive, low-cost, single-tube method that uses six primers to amplify specific gene regions [12]. Bst DNA polymerase, a strand-displacement DNA polymerase, enables the formation of a loop structure for inner primers, resulting in LAMP’s unique rapid self-priming amplification [13]. The LAMP assay is widely used to detect microbial pathogens [14]. In addition, LAMP has the advantage of multiplexed detection, allowing the simultaneous detection of multiple targets. A diverse range of multiplex Loop-Mediated Isothermal Amplification (LAMP) detection methods has been developed to date, enhancing application and efficiency of this technique [15]. These include the use of fluorescent probes, lateral flow devices, and multi-channel devices for detection. Specifically, the repertoire of multiplex LAMP methods employing probes encompasses methylation-specific LAMP (MS-LAMP) [16], FRET-based assimilating probe-LAMP [17], fluorescence of loop primer upon self-enriching LAMP (FLOS-LAMP) [18], detection of Amplification by Release of Quenching (DARQ) [19], quenching of Unincorporated Amplification Signal Reporters (QUASR) [20], and Molecular Beacon LAMP (MB-LAMP) [21]. Particularly, FRET-based assimilating probe that signal the presence of target DNA by increasing fluorescence upon target amplification, thereby offering precise and sensitive detection in multiplex LAMP assays.
To our knowledge, limited number of studies have developed LAMP based detection for PJI. In this study, we developed a multiplex LAMP assay to detect the five most common bacteria in PJI [4, 22]—S. aureus, S. epidermidis, S. agalactiae, E. coli, and P. aeruginosa. We compared our results with quantitative real-time PCR (qPCR) and performed a limit-of-detection analysis to evaluate the analytical performance of the developed multiplex LAMP assay.
Materials and methods
American Type Culture Collection (ATCC) standard bacteria strains, clinical samples, and DNA extraction
The analytical and cross-reactivity evaluations of gram-positive and gram-negative bacteria multiplex LAMP assays were performed with standard strains, including S. epidermidis (ATCC 12228), S. agalactiae (ATCC 13813), S. aureus (ATCC 29213), P. aeruginosa (ATCC 27853), E. coli (ATCC 25922), Enterobacter aerogenes (ATCC 13048), Enterococcus faecalis (ATCC 29212), Streptococcus pneumoniae (ATCC 49619), and Klebsiella pneumoniae (ATCC 13883). Among the ATCC strains stored in our laboratory, we selected strains that were reported to cause PJI with high frequency, including the LAMP target strain, and used them for cross-reactivity studies.
Clinical performance evaluation was conducted using archived joint synovial fluid specimens stored for quality control purposes in the laboratory at Korea University Guro Hospital from October 1st to 15th, 2023. All information that could identify the patient, except for the test results, was removed from these archived specimens. Additionally, specimens stored for quality control purposes in the laboratory were used in the study after IRB approval, in accordance with the IRB policy that written consent is waived. This study was approved by the Institutional Review Board of the Korea University Guro Hospital, Seoul, Republic of Korea (IRB No. 2023GR0356). The clinical samples were confirmed to contain bacterial infections by bacterial culture. A total of 20 clinical samples were used in this study, including four S. aureus, one S. epidermidis, one S. agalactiae, and 14 negative samples. All clinical specimens were stored in a -70°C deep freezer and used for LAMP assays without additional culture tests.
For DNA extraction, the AdvanSure™ E3 system (LG Chem, Seoul, Republic of Korea) was used for all samples, following the manufacturer’s manual. Briefly, 200 μL of samples were loaded into the DNA/RNA extraction cartridge, and DNA was eluted in 100 μL of elution buffer. Residual samples and DNA were stored at -70°C.
LAMP primer design
The LAMP primer sets for S. epidermidis, P. aeruginosa, and E. coli were designed to target conserved regions of NUT42_08370, fecI3 and malB gene, respectively. All LAMP primer sets were designed using Primer Explorer software (version 5; Eiken Chemical Co., Tokyo, Japan). We used previously published LAMP primer sets for S. agalactiae and S. aureus [23, 24]. For the multiplex probe design, two types of additional synthetic oligonucleotide sequences were designed and added to the 5′ end of the LB primer of each LAMP primer set. The 5′ end of the multiplex probe was tagged with a fluorescent marker. In a gram-positive bacteria LAMP assay, the 5′ end of S. epidermidis, S. agalactiae, and S. aureus LAMP probes was tagged with FAM, HEX, and CY5. For the gram-negative bacteria LAMP assay, the 5′ end of P. aeruginosa and E. coli LAMP probes were tagged with FAM and CY5, respectively. As in previous studies [25, 26], two types of complementary synthetic oligonucleotide sequences tagged with BHQ1 or BHQ2 at the 3′ end, named quencher probes 1 and 2, were used for quenching FAM/HEX and CY5 fluorophore, respectively. All LAMP primers and probes were synthesized by Macrogen, Inc. (Seoul, Korea; 1).
Table 1. Gram positive/negative bacteria multiplex LAMP assay primer sets.
| Target (gene) | Name | Sequence (5’-3’) | μM | Reference | |
|---|---|---|---|---|---|
| S. epidermidis (NUT42_08370 gene) | SEP_F3 | TGGATATGAAGAAAGTGATGC | 4 | In this study | |
| SEP_B3 | TCTTCAAATAAAGGCATGACG | 4 | |||
| SEP_FIP | GCGGAATCATGGTACTGTTACTTTGCTCTCAAATGATTCTTCCCCT | 32 | |||
| SEP_BIP | TCCTTTCCAATCAATTGGATCTTGCGTAAATGTGTTTCCCGTTCT | 32 | |||
| SEP_LB | /LNA-T//LNA-C//LNA-A//LNA-C/TGAATTTACTCCTGTG | 4 | |||
| SEP_LBP | FAM-CGGGCCCGTACAAAGGGAACACCCACACTCCG/LNA-T//LNA-C//LNA-A//LNA-C/TGAATTTACTCCTGTG | 6 | |||
| S. agalactiae (sodA gene) | SAG_F3 | ATATGATGCGCTTGAGCC | 4 | [24] | |
| SAG_B3 | ACCACCGTTATTGATGACTG | 4 | |||
| SAG_FIP | GAGCAGCATTTGCATTAGCAACATATTTTGATGCTGAGACAATGACAC | 32 | |||
| SAG_BIP | ACATCCTGAAATTGGAGAAGACTTTTTTCCTGACGAATATCTTCTGGAAT | 32 | |||
| SAG_LF | TGCATGGTGCTTATCATGATGT | 10 | |||
| SAG_LB | AGGCGCTCTTAGCTGATGT | 4 | |||
| SAG_LBP | HEX-CGGGCCCGTACAAAGGGAACACCCACACTCCGAGGCGCTCTTAGCTGATGT | 6 | |||
| S. aureus (nuc gene) | SAU_F3 | GAAGTGGTTCTGAAGATCCAA | 4 | [23] | |
| SAU_B3 | CCAAGCCTTGACGAACTAA | 4 | |||
| SAU_FIP | AGGATGCTTTGTTTCAGGTGTCGATTGATGGTGATACGGTTA | 32 | |||
| SAU_BIP | AATATGGTCCTGAAGCAAGTGCGCTAAGCCACGTCCATAT | 32 | |||
| SAU_LF | TCTGAATGTCATTGGTTGACCT | 10 | |||
| SAU_LB | GAAGTCGAGTTTGACAAAGGTC | 4 | |||
| SAU_LBP | Cy5-GTCAGTGCAGGCTCCCGTGTTAGGACGAGGGTAGGGAAGTCGAGTTTGACAAAGGTC | 6 | |||
| P. aeruginosa (fecI3 gene) | PAE_F3 | GCTTCCGTGGTTCCGTCTC | 4 | In this study | |
| PAE_B3 | GGTTGCGGGCGATCTG | 4 | |||
| PAE_FIP | TGCCCAGGTGCTTGCGCAGCATGCCTATCAGGCGTTC | 32 | |||
| PAE_BIP | GCCGACCTCGCCCAGGATAGCTCGACCGATTGCCG | 32 | |||
| PAE_LF | CGCAGCAACTCGCCATG | 10 | |||
| PAE_LB | GCCCAGTGGCTGAAATGGC | 4 | |||
| PAE_LBP | FAM-CGGGCCCGTACAAAGGGAACACCCACACTCCGGCCCAGTGGCTGAAATGGC | 6 | |||
| E. coli (malB gene) | ECO-F3 | GGCGCGAAAAAAGAAGTGAT | 4 | In this study | |
| ECO-B3 | AGGTTGGAGAGCGGTTCAT | 4 | |||
| ECO-FIP | GGTTTGCGATCCAGCAAATGCGAACCAGCGAGTTAACCAGG | 32 | |||
| ECO-BIP | GTGGTCAGCGTCAGCGTGTGCGAGCAAAAATACGCTTGGC | 32 | |||
| ECO-LF | CCAGTTGCAGCACTTCCG | 10 | |||
| ECO-LB | CGATTGGCCGTACGCTGGTG | 4 | |||
| ECO-LBP | Cy5-GTCAGTGCAGGCTCCCGTGTTAGGACGAGGGTAGGCGATTGGCCGTACGCTGGTG | 6 | |||
| Quencher probe 1 | GAGTGTGGGTGTTCCCTTTGTACGGGCCCG-BHQ1 | 9 | |||
| Quencher probe 2 | CCTACCCTCGTCCTAACACGGGAGCCTGCACTGAC-BHQ2 | 9 | |||
LAMP: Loop-mediated isothermal amplification; F3: forward primer; B3: backward primer; FIP: forward inner primer; BIP: backward inner primer; LF: loop forward primer; LB: loop backward primer; LBP: loop backward probe.
The gram-positive/negative bacteria multiplex LAMP assay
The multiplex LAMP assay for gram-positive and gram-negative bacteria was performed using an ELPIS Biotech LAMP kit (ELPIS Biotech, Daejeon, South Korea). The gram-positive LAMP reaction mixture consisted of 12.5 μL of 2× reaction buffer, 1 μL of S. epidermidis LAMP primer mix, 1 μL of S. agalactiae LAMP primer mix, 1 μL of S. aureus LAMP primer mix, 2 μL of 9 μM quencher probe 1, 1 μL of 9 μM quencher probe 2, 1.5 μL of DNase/RNase-free distilled water, and 5 μL of sample DNA (final reaction volume: 25 μL). The gram-negative LAMP reaction mixture consisted of 12.5 μL of 2× reaction buffer, 1 μL of P. aeruginosa LAMP primer mix, 1 μL of E. coli LAMP primer mix, 1 μL of 9 μM quencher probe 1, 1 μL of 9 μM quencher probe 2, 3.5 μL of DNase/RNase-free distilled water, and 5 μL of sample DNA (final reaction volume: 25 μL). Each bacterial LAMP primer mix was composed of 4 μM of two outer primers (F3 and B3), 32 μM of two inner primers (FIP and BIP), 10 μM of forward loop primer (FLP), 4 μM of backward loop primer (BLP), and 6 μM of BLP probe. The LAMP assay was run on a CFX 96 Touch Real-Time PCR Detection System (Bio-Rad Laboratories, Hercules, CA, USA) at 64°C for 30 min.
Quantitative real-time PCR
The performance of the gram-positive and gram-negative bacterial multiplex LAMP assays for S. aureus, S. epidermidis, S. agalactiae, P. aeruginosa, and E. coli strains was compared and evaluated using qPCR. This study used the S. aureus, S. epidermidis, S. agalactiae, P. aeruginosa, and E. coli previously reported qPCR primer sets (Table 2) [27–32]. The thermocycling parameters of all qPCR were as follows: initial denaturation at 50°C for 3 min, 45 cycles of denaturation at 95°C for 15 s, annealing and extension with fluorescence detection at 60°C for 30 s.
Table 2. Gram-positive/negative bacteria quantitative real-time PCR primer sets.
| Target (gene) | Name | Sequence (5’-3’) | μM | Reference |
|---|---|---|---|---|
| S. epidermidis (atlE gene) | SEP_atlE_F | GGAGGAACTAATAATAAGTTAACTG | 10 | [28] |
| SEP_atlE_R | GTCATAAACAGTTGTATATAAGCC | 10 | ||
| SEP_atlE_P | FAM-CTGCTAATCGTGGTGTTGCTCAAATTAAA-BHQ1 | 10 | ||
| S. agalactiae (sodA gene) | SAG_sip_F | GTTCCAGCAGCTAAAGAGGAAG | 10 | [29] |
| SAG_sip_R | CCGGTGCTACTTTAGCTACTGG | 10 | ||
| SAG_sip_P | HEX-CACCAGCTTCTGTTGCCGCTGAAACACCAGC-BHQ1 | 10 | ||
| S. aureus (nuc gene) | SAU_nuc_F | CACCTGAAACAAAGCATCCTAAA | 10 | [30] |
| SAU_nuc_R | CGCTAAGCCACGTCCATATT | 10 | ||
| SAU_nuc_P | CY5-TGGTCCTGAAGCAAGTGCATTTACGA-BHQ2 | 10 | ||
| P. aeruginosa (gyrB gene) | PAE_gyrB_F | GGCGTGGGTGTGGAAGTC | 10 | [31] |
| PAE_gyrB_R | TGGTGGCGATCTTGAACTTCTT | 10 | ||
| PAE_gyrB_P | FAM-TGCAGTGGAACGACA-BHQ1 | 10 | ||
| E. coli (16s rRNA gene) | ECO_16s_F | CATGCCGCGTGTATGAAGAA | 10 | [32] |
| ECO_16s_R | CGGGTAACGTCAATGAGCAAA | 10 | ||
| ECO_16s_P | CY5-TATTAACTTTACTCCCTTCCTCCCCGCTGAA-BHQ2 | 10 |
Analytical sensitivity tests
For the analytical sensitivity tests of gram-positive and gram-negative bacteria multiplex LAMP assays, all five standard ATCC bacteria (S. aureus, S. epidermidis, S. agalactiae, P. aeruginosa, and E. coli) were cultured; a colony count assay confirmed cell concentrations. The five bacteria were spiked into a normal joint fluid (107 CFU/mL) and serially diluted 10-fold with normal joint fluid from 107 to 100 CFU/mL. DNA was extracted from the samples using an AdvanSure E3 system (LG Chem, Seoul, Republic of Korea). The analytical sensitivity of the gram-positive and gram-negative bacterial multiplex LAMP assays were compared to the qPCR assay. All tests were repeated three times and the minimum concentration was determined as the concentration at which all three tests were positive.
Results
Temperature optimization of the gram-positive/negative bacteria multiplex LAMP assay
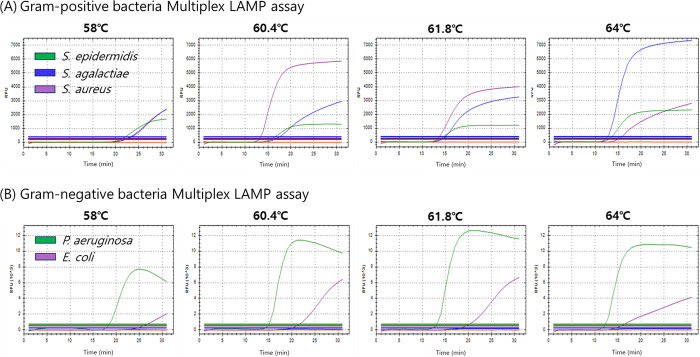
Temperature gradient tests (58–64°C) were conducted to determine the optimal temperature for the gram-positive and gram-negative bacteria in multiplex LAMP assays. The gram-positive bacteria multiplex LAMP assay was tested with DNA samples extracted from joint fluid samples spiked with ATCC S. agalactiae, S. epidermidis, and S. aureus (at a concentration of 107 CFU/mL in a 1:1:1 ratio). In contrast, the gram-negative bacteria multiplex LAMP assay was tested with DNA samples extracted from joint fluid samples spiked with ATCC P. aeruginosa and E. coli (at a concentration of 107 CFU/mL in a 1:1 ratio) (Table 3; Fig 1). Among the four temperatures assessed (64°C, 61.8°C, 60.4°C, and 58.0°C), both the gram-positive and gram-negative multiplex LAMP assays exhibited the lowest Tt values across all fluorescence channels at 64°C, except for the S. aureus signal, which was delayed slightly. However, the Tt values for signals from other bacterial strains were considerably delayed at other temperatures. Therefore, based on the overall results, the optimal temperature for conducting multiplex LAMP analysis of gram-positive and gram-negative bacteria was 64°C.
Table 3. Temperature optimization for gram-positive/negative bacteria multiplex LAMP assay.
| Temp (°C) | Gram-positive bacteria multiplex LAMP assay (Tt values) | Gram-negative bacteria multiplex LAMP assay (Tt values) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| S. epidermidis | S. agalactiae | S. aureus | P. aeruginosa | E. coli | ||||||
| Tt | RFU | Tt | RFU | Tt | RFU | Tt | RFU | Tt | RFU | |
| 64.0°C | 13.1 | 2307 | 12.7 | 7296 | 15.4 | 2622 | 12.2 | 10662 | 15.6 | 3744 |
| 61.8°C | 13.9 | 1209 | 15.0 | 3171 | 13.5 | 3955 | 13.6 | 11815 | 19.4 | 5935 |
| 60.4°C | 15.58 | 1312 | 17.5 | 2724 | 13.2 | 5819 | 15.1 | 10197 | 21.0 | 5490 |
| 58.0°C | 21.1 | 1576 | 23.4 | 1910 | 22.5 | 1938 | 18.5 | 6830 | 25.8 | 1432 |
LAMP: Loop-mediated isothermal amplification, RFU: relative fluorescence unit, Tt: threshold time.
Fig 1. Temperature optimization for the gram-positive/negative bacteria multiplex LAMP primer set.
A temperature gradient from 58 to 64°C was performed. (A) The Multiplex LAMP assay for gram-positive bacteria was designed to detect three bacterial species, namely, S. epidermidis (FAM), S. agalactiae (HEX), and S. aureus (CY5). In parallel, (B) the Multiplex LAMP assay for gram-negative bacteria was designed to target two bacterial species, P. aeruginosa (FAM) and E. coli (CY5).
Analytical sensitivity of the gram-positive/negative bacteria multiplex LAMP assay
Using the analytical sensitivity test for five strains: S. epidermidis, S. agalactiae, S. aureus, P. aeruginosa, and E. coli, the analytical performance of the multiplex LAMP assay for gram-positive and gram-negative bacteria was evaluated and compared with that of the qPCR assay (Table 4). Each DNA sample extracted from the joint fluid spiked with ATCC bacteria, diluted 10-fold in seven levels, was used for analytical sensitivity testing of the gram-positive and gram-negative bacteria multiplex LAMP and qPCR assays. The analytical sensitivity of the gram-positive bacterial multiplex LAMP assay and qPCR were 105/104 CFU/mL, 103/103 CFU/mL, and 105/104 CFU/mL against S. agalactiae, S. epidermidis, and S. aureus, respectively. For P. aeruginosa and E. coli, analytical sensitivities of the multiplex LAMP assay and qPCR were 105/104 CFU/mL and 106/104 CFU/mL, respectively. In all test samples, except for S. epidermidis, the gram-positive and gram-negative bacteria multiplex LAMP assay showed 10 to 100-fold higher analytical sensitivity compared to the qPCR assay.
Table 4. Comparison of analytical sensitivity of the gram-positive bacteria multiplex LAMP assay and qPCR assay using ATCC strains.
| A. Gram-positive bacteria | ||||||||||
| CFU/mL | S. agalactiae | S. epidermidis | S. aureus | |||||||
| LAMP | qPCR | LAMP | qPCR | LAMP | qPCR | |||||
| Tt (SD) | Tt (SD) | Tt (SD) | Tt (SD) | Tt (SD) | Tt (SD) | |||||
| 1 × 107 | 18.5 ± 0.7 | 24.0 ± 0.4 | 13.3 ± 0.4 | 27.2 ± 1.0 | 15.3 ± 0.8 | 27.1 ± 0.1 | ||||
| 1 × 106 | 20.3 ± 0.2 | 27.8 ± 1.5 | 14.0 ± 0.5 | 30.5 ± 0.6 | 17.6 ± 2.1 | 30.8 ± 0.3 | ||||
| 1 × 105 | 26.2 ± 0.6 | 32.3 ± 0.1 | 15.9 ± 0.4 | 32.8 ± 1.0 | 21.3 ± 1.1 | 34.2 ± 0.2 | ||||
| 1 × 104 | N/A | 34.2 ± 0.5 | 17.8 ± 1.1 | 35.3 ± 0.9 | N/A | 36.5 ± 0.9 | ||||
| 1 × 103 | N/A | N/A | 20.7 ± 0.7 | 37.6 ± 1.1 | N/A | N/A | ||||
| 1 × 102 | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| 1 × 101 | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| 1 × 100 | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| 0 | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| B. Gram-negative bacteria | ||||||||||
| CFU/mL | P. aeruginosa | E. coli | ||||||||
| LAMP | qPCR | LAMP | qPCR | |||||||
| Tt (SD) | Tt (SD) | Tt (SD) | Tt (SD) | |||||||
| 1 × 107 | 12.1 ± 0.4 | 27.4 ± 0.4 | 15.1 ± 0.6 | 19.0 ± 0.2 | ||||||
| 1 × 106 | 13.7 ± 0.5 | 30.8 ± 0.5 | 17.8 ± 0.8 | 23.0 ± 0.3 | ||||||
| 1 × 105 | 16.9 ± 1.1 | 35.1 ± 1.6 | N/A | 29.1 ± 0.3 | ||||||
| 1 × 104 | N/A | 39.9 ± 2.2 | N/A | 32.8 ± 1.5 | ||||||
| 1 × 103 | N/A | N/A | N/A | N/A | ||||||
| 1 × 102 | N/A | N/A | N/A | N/A | ||||||
| 1 × 101 | N/A | N/A | N/A | N/A | ||||||
| 1 × 100 | N/A | N/A | N/A | N/A | ||||||
| 0 | N/A | N/A | N/A | N/A | ||||||
LAMP: Loop-mediated isothermal amplification, qPCR: quantitative real-time PCR, ATCC: American Type Culture Collection, Tt: threshold time, SD: standard deviation, N/A: not available.
Clinical performance of the gram-positive/negative bacteria multiplex LAMP assay
We compared the sensitivity and specificity of the LAMP assay with those of qPCR for clinical synovial fluid samples (Table 5) to validate the clinical performance of the gram-positive and gram-negative bacterial multiplex LAMP assays. The gram-positive/negative bacterial multiplex LAMP assay demonstrated 100% specificity when tested against normal joint fluid clinical samples (n = 14). For six clinical samples, including S. agalactiae (n = 1), S. epidermidis (n = 1), and S. aureus (n = 4), the gram-positive bacteria multiplex LAMP assay exhibited 100% sensitivity without cross-reaction with other target bacteria; the multiplex LAMP assay showed 100% specificity.
Table 5. Performance comparison between the gram-positive/negative bacteria multiplex LAMP assay and qPCR for clinical samples.
| Clinical Sample | Gram-positive bacteria multiplex LAMP assay | Gram-negative bacteria multiplex LAMP assay | qPCR | ||||
|---|---|---|---|---|---|---|---|
| S. agalactiae | S. epidermidis | S. aureus | P. aeruginosa | E. coli | |||
| S. agalactiae (n = 1) | P/N | 1/0 | 0/1 | 0/1 | 0/1 | 0/1 | 1/0 |
| Sensitivity | 100 | - | - | - | - | 100 | |
| Specificity | - | 100 | 100 | 100 | 100 | - | |
| S. epidermidis (n = 1) | P/N | 0/1 | 1/0 | 0/1 | 0/1 | 0/1 | 1/0 |
| Sensitivity | - | 100 | - | - | - | 100 | |
| Specificity | 100 | - | 100 | 100 | 100 | - | |
| S. aureus (n = 4) | P/N | 0/4 | 0/4 | 4/0 | 0/4 | 0/4 | 4/0 |
| Sensitivity | - | - | 100 | - | - | 100 | |
| Specificity | 100 | 100 | - | 100 | 100 | - | |
| Negative Sample (n = 14) | P/N | 0/14 | 0/14 | 0/14 | 0/14 | 0/14 | 0/14 |
| Sensitivity | - | - | - | - | - | - | |
| Specificity | 100 | 100 | 100 | 100 | 100 | 100 | |
“P” and “N” indicate the positive and negative reactions, respectively.
LAMP: Loop-mediated isothermal amplification, qPCR: quantitative real-time PCR.
Cross-reactivity tests
In addition to the five target bacteria for the LAMP assay developed in this study, cross-reactivity tests were performed using an additional 4 ATCC strains: E. aerogenes (ATCC 13048), Enterococcus faecalis (ATCC 29212), S. pneumoniae (ATCC 49619), and K. pneumoniae (ATCC 13883) (Table 6). In target bacteria, including S. agalactiae, S. epidermidis, S. aureus, P. aeruginosa, and E. coli, the gram-positive and gram-negative bacteria multiplex LAMP assay detected the target bacteria without cross-reaction with other signals targeting other target bacteria. The gram-positive and gram-negative bacteria multiplex LAMP assays exhibited no cross-reactivity for the other four infectious bacteria, including E. aerogenes, E. faecalis, S. pneumoniae, and K. pneumoniae. These results indicate that the LAMP assay can accurately detect the target bacteria without producing false-positive results, even in the presence of other bacteria.
Table 6. Cross-reactivity of the gram-positive/negative bacteria multiplex LAMP assay against infectious bacteria.
| Test bacteria (ATCC strains) | Gram-positive bacteria multiplex LAMP assay | Gram-negative bacteria multiplex LAMP assay | |||
|---|---|---|---|---|---|
| S. agalactiae | S. epidermidis | S. aureus | P. aeruginosa | E. coli | |
| S. agalactiae | P | N | N | N | N |
| S. epidermidis | N | P | N | N | N |
| S. aureus | N | N | P | N | N |
| P. aeruginosa | N | N | N | P | N |
| E. coli | N | N | N | N | P |
| E. aerogenes | N | N | N | N | N |
| E. faecalis | N | N | N | N | N |
| S. pneumoniae | N | N | N | N | N |
| K. pneumoniae | N | N | N | N | N |
“P” and “N” indicate the positive and negative reactions, respectively.
LAMP: Loop-mediated isothermal amplification, qPCR: quantitative real-time PCR.
Discussion
Recently, molecular diagnostic methods for PJI diagnosis were introduced to increase detection sensitivity and shorten turnaround times [33]. However, molecular diagnostic methods like real-time PCR require expensive equipment and trained personnel. Additionally, the test takes at least 2–3 h and can only be performed in the central laboratories of hospitals with all the necessary equipment [4]. Methods for identifying causative microorganisms using isothermal nucleic acid amplification have attracted renewed attention to overcome these limitations. Among the isothermal amplification methods, LAMP is most actively studied for the development of new diagnostic kits for detecting microorganisms [12, 14].
In this study, we developed a multiplex LAMP assay that can detect five bacterial species that account for many PJI-causing bacteria. We validated the performance of our developed LAMP assay by comparing it against published qPCR assays for each bacterium, whose performance has been verified, using bacterial analysis samples prepared identically. Our multiplex LAMP assay detects five bacteria in two reactions. The gram-positive assay detected three gram-positive bacteria: S. epidermidis, S. agalactiae, and S. aureus, and the gram-negative assay detected two: P. aeruginosa and E. coli. Previously, attempts were made to use LAMP to detect bacteria in orthopedic and infectious diseases; however, most of these attempts targeted a single bacterium [27, 34–36]. Multiplex LAMP assays that can simultaneously detect multiple bacteria have rarely been developed. We designed LAMP assays to enable clinicians to detect as many types of bacteria simultaneously as possible. However, like PCR and LAMP, molecular diagnostic methods using primers or probes are limited because they can only detect a predetermined number of targets. Similarly, our multiplex LAMP assay is limited to detecting only the five target bacteria we selected. We selected five bacteria based on the frequency with which they cause PJIs [22]. Although the number is limited to five, the assay is still clinically useful.
The analytical sensitivity of the LAMP assay has been reported in previous studies to be between 102 and 105 CFU/mL for bacteria [37–39]. In our multiplex LAMP assay, four types of bacteria except E. coli were detected at 103–105 CFU/mL, with analytical sensitivity values similar to those reported in previous studies. However, the analytical sensitivity of the multiplex LAMP assay for E. coli was 106 CFU/mL. This may be because primer and probe efficiencies were not sufficiently high. Further research could achieve a lower analytical sensitivity. Additionally, the LODs in previous studies were all for single-plex LAMP assays, whereas ours is a multiplex LAMP assay. Therefore, we inferred that, overall, the analytical sensitivity of our assay was higher than that reported in previous studies [40]. The sensitivity to each target does not deteriorate when LAMP is developed as a multiplex assay, as with real-time PCR [40, 41]. In our study, the analytical sensitivity was approximately 10–102 times lower when each type of bacterium was individually tested in a single-plex assay than in a multiplex assay. However, we postulated that for diagnosing PJI, it would be helpful to detect as many types of bacteria as possible in a single reaction by increasing the analytical sensitivity using a multiplex, and we developed a multiplex assay.
We compared our multiplex LAMP assay, including analytical sensitivity, with a qPCR assay reported in the literature; among the PCR-based molecular assays, there is no widely used commercial real-time PCR kit for PJI diagnosis. To compare the analytical sensitivity, we designed a single-plex qPCR assay targeting each of the five bacteria and compared it with the multiplex LAMP assay developed in this study. Using our LAMP assay, gram-positive bacteria, such as S. agalactiae and S. aureus, had an analytical sensitivity approximately ten times higher than that of qPCR, whereas S. epidermidis had the same analytical sensitivity. Additionally, P. aeruginosa had an analytical sensitivity ten times higher than qPCR among gram-negative bacteria, whereas E. coli had an analytical sensitivity approximately 100 times higher. According to a previous study, the analytical sensitivity of LAMP was approximately 100 times lower than that of conventional PCR and 10–100 times higher than that of real-time PCR [39]. Therefore, the multiplex LAMP assay developed in this study showed a consistent analytical sensitivity difference compared to qPCR. Additionally, it should be noted that our analytical sensitivity analysis compared multiplex LAMP with single-plex qPCR; the analytical sensitivity difference may be even greater.
We tested our multiplex LAMP assay for cross-reactivity by adding four additional ATCC strains, E. aerogenes, E. faecalis, S. pneumoniae, and K. pneumoniae to determine whether it would produce a positive reaction to bacteria other than the five targeted bacteria. The test results showed that the assay did not produce a positive reaction to any bacteria other than the original target bacteria, indicating excellent specificity. In a clinical performance evaluation using synovial fluid from actual patients, the assay showed 100% sensitivity and specificity compared to the culture results. Although the clinical sample size was small, these results indicate that the performance of the gram-positive/negative bacterial multiplex LAMP assay is similar to that of the qPCR assay for detecting bacteria in joint synovial fluid clinical samples. Therefore, our gram-positive/negative bacterial multiplex LAMP assay is a reliable alternative for detecting these pathogens in clinical samples.
In our study, we developed a LAMP test that showed significantly faster results compared to the qPCR test. The LAMP test took only 30 minutes to complete, while the qPCR test took approximately 120 minutes. The LAMP test’s rapid turnaround time is attributed to its isothermal amplification process, which eliminates the need for temperature cycling steps required in PCR. This makes the LAMP test more efficient and faster. Furthermore, the LAMP test only requires a heat block to maintain a constant temperature, whereas the qPCR requires a costly thermocycler. This makes the LAMP test more accessible and cost-effective for diagnostic applications.
The types of bacteria that can be detected by the multiplex LAMP assay developed in this study are mostly consistent with those commonly found to cause septic arthritis or osteomyelitis [42–45]. Therefore, our assay can diagnose bacterial septic arthritis and osteomyelitis and is a high-throughput assay that can diagnose PJI and other orthopedic infections.
This study had several limitations. First, this study focused on developing a multiplex LAMP assay for diagnosing PJI and evaluating its analytical performance using ATCC standard strains. The clinical performance evaluation used a few clinical specimens. Most were negative specimens, and only a few positive specimens were used. Therefore, further studies using sufficient clinical specimens are required to confirm the clinical utility of the LAMP assay developed in this study. Second, our LAMP assay can only detect target bacteria that bind to primers and probes, and the number of multiplexing reactions that can be performed is limited. Therefore, the multiplex LAMP assay developed in this study cannot detect bacteria other than the five selected targets or other types of microorganisms that rarely cause PJI, such as fungi and mycobacteria. Third, we did not include an internal control in this study. Adding an internal control in future research is crucial to ensure more accurate and reliable results. Fourth, this study highlights LAMP’s efficiency and simplicity over PCR, but we used the same equipment typically required for PCR. Thus, this study may not fully show LAMP’s potential for less complex and more affordable operation. However, recent advances have led to the development and commercial availability of cost-effective, portable isothermal amplification devices capable of four-channel multiplexing (https://www.gencurix.com/eng/sub_2_8.php). Consequently, future studies evaluating LAMP kits with these portable devices could fully leverage LAMP’s advantages, demonstrating its cost-effectiveness, simplicity, and rapid operation.
In conclusion, the multiplex LAMP assay developed in this study can rapidly detect five bacterial species with high prevalence among the causative bacteria of bacterial PJI with excellent sensitivity and specificity in less than 1 h. Thus, the multiplex LAMP assay may be helpful in the early diagnosis of PJI.
Supporting information
(XLSX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
MCCHO was supported by the Korea University Guro Hospital (KOREA RESEARCH-DRIVEN HOSPITAL), a grant funded by the Korea University Medicine (No. K2313921). CSLIM was a grant from the Korea Health Technology R&D project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number HR20C0021). The funders did not play any role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bemer P, Plouzeau C, Tande D, Leger J, Giraudeau B, Valentin AS, et al. Evaluation of 16S rRNA gene PCR sensitivity and specificity for diagnosis of prosthetic joint infection: a prospective multicenter cross-sectional study. J Clin Microbiol. 2014;52(10):3583–9. doi: 10.1128/JCM.01459-14 ; PubMed Central PMCID: PMC4187742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corvec S, Portillo ME, Pasticci BM, Borens O, Trampuz A. Epidemiology and new developments in the diagnosis of prosthetic joint infection. Int J Artif Organs. 2012;35(10):923–34. doi: 10.5301/ijao.5000168 . [DOI] [PubMed] [Google Scholar]
- 3.Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645–54. doi: 10.1056/NEJMra040181 . [DOI] [PubMed] [Google Scholar]
- 4.Gatti G, Taddei F, Brandolini M, Mancini A, Denicolo A, Congestri F, et al. Molecular Approach for the Laboratory Diagnosis of Periprosthetic Joint Infections. Microorganisms. 2022;10(8). doi: 10.3390/microorganisms10081573 ; PubMed Central PMCID: PMC9414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parvizi J, Gehrke T, International Consensus Group on Periprosthetic Joint I. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29(7):1331. doi: 10.1016/j.arth.2014.03.009 . [DOI] [PubMed] [Google Scholar]
- 6.Premkumar A, Morse K, Levack AE, Bostrom MP, Carli AV. Periprosthetic Joint Infection in Patients with Inflammatory Joint Disease: Prevention and Diagnosis. Curr Rheumatol Rep. 2018;20(11):68. doi: 10.1007/s11926-018-0777-6 ; PubMed Central PMCID: PMC6543529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benito N, Franco M, Ribera A, Soriano A, Rodriguez-Pardo D, Sorli L, et al. Time trends in the aetiology of prosthetic joint infections: a multicentre cohort study. Clin Microbiol Infect. 2016;22(8):732 e1–8. doi: 10.1016/j.cmi.2016.05.004 . [DOI] [PubMed] [Google Scholar]
- 8.Arvieux C, Common H. New diagnostic tools for prosthetic joint infection. Orthop Traumatol Surg Res. 2019;105(1S):S23–S30. doi: 10.1016/j.otsr.2018.04.029 . [DOI] [PubMed] [Google Scholar]
- 9.Stylianakis A, Schinas G, Thomaidis PC, Papaparaskevas J, Ziogas DC, Gamaletsou MN, et al. Combination of conventional culture, vial culture, and broad-range PCR of sonication fluid for the diagnosis of prosthetic joint infection. Diagn Microbiol Infect Dis. 2018;92(1):13–8. doi: 10.1016/j.diagmicrobio.2018.04.008 . [DOI] [PubMed] [Google Scholar]
- 10.Marin M, Garcia-Lechuz JM, Alonso P, Villanueva M, Alcala L, Gimeno M, et al. Role of universal 16S rRNA gene PCR and sequencing in diagnosis of prosthetic joint infection. J Clin Microbiol. 2012;50(3):583–9. doi: 10.1128/JCM.00170-11 ; PubMed Central PMCID: PMC3295163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Huang Z, Li W, Fang X, Zhang W. Can metagenomic next-generation sequencing identify the pathogens responsible for culture-negative prosthetic joint infection? BMC Infect Dis. 2020;20(1):253. doi: 10.1186/s12879-020-04955-2 ; PubMed Central PMCID: PMC7106575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000;28(12):E63. doi: 10.1093/nar/28.12.e63 ; PubMed Central PMCID: PMC102748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagamine K, Hase T, Notomi T. Accelerated reaction by loop-mediated isothermal amplification using loop primers. Mol Cell Probes. 2002;16(3):223–9. doi: 10.1006/mcpr.2002.0415 . [DOI] [PubMed] [Google Scholar]
- 14.Dhama K, Karthik K, Chakraborty S, Tiwari R, Kapoor S, Kumar A, et al. Loop-mediated isothermal amplification of DNA (LAMP): a new diagnostic tool lights the world of diagnosis of animal and human pathogens: a review. Pak J Biol Sci. 2014;17(2):151–66. doi: 10.3923/pjbs.2014.151.166 . [DOI] [PubMed] [Google Scholar]
- 15.Lisa Becherer NB, Mohammed Bakheit, Sieghard Frischmann, Roland Zengerle, Felix von Stetten Loop-mediated isothermal amplification (LAMP)–review and classification of methods for sequence-specific detection. Analytical Methods. 2020;12:30. [Google Scholar]
- 16.Zerilli F, Bonanno C, Shehi E, Amicarelli G, Adlerstein D, Makrigiorgos GM. Methylation-specific loop-mediated isothermal amplification for detecting hypermethylated DNA in simplex and multiplex formats. Clin Chem. 2010;56(8):1287–96. doi: 10.1373/clinchem.2010.143545 . [DOI] [PubMed] [Google Scholar]
- 17.Kubota R M. Alvarez A, Su WW, Jenkins D M. FRET-Based Assimilating Probe for Sequence-Specific Real-Time Monitoring of Loop-Mediated Isothermal Amplification (LAMP). Biological Engineering Transactions. 2011;4(2):81–100. doi: 10.13031/2013.38509 [DOI] [Google Scholar]
- 18.Gadkar VJ, Goldfarb DM, Gantt S, Tilley PAG. Real-time Detection and Monitoring of Loop Mediated Amplification (LAMP) Reaction Using Self-quenching and De-quenching Fluorogenic Probes. Sci Rep. 2018;8(1):5548. doi: 10.1038/s41598-018-23930-1 ; PubMed Central PMCID: PMC5883045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tanner NA, Zhang Y, Evans TC, Jr. Simultaneous multiple target detection in real-time loop-mediated isothermal amplification. Biotechniques. 2012;53(2):81–9. doi: 10.2144/0000113902 . [DOI] [PubMed] [Google Scholar]
- 20.Ball CS, Light YK, Koh CY, Wheeler SS, Coffey LL, Meagher RJ. Quenching of Unincorporated Amplification Signal Reporters in Reverse-Transcription Loop-Mediated Isothermal Amplification Enabling Bright, Single-Step, Closed-Tube, and Multiplexed Detection of RNA Viruses. Anal Chem. 2016;88(7):3562–8. doi: 10.1021/acs.analchem.5b04054 . [DOI] [PubMed] [Google Scholar]
- 21.Liu W, Huang S, Liu N, Dong D, Yang Z, Tang Y, et al. Establishment of an accurate and fast detection method using molecular beacons in loop-mediated isothermal amplification assay. Sci Rep. 2017;7:40125. doi: 10.1038/srep40125 ; PubMed Central PMCID: PMC5216335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manning L, Metcalf S, Clark B, Robinson JO, Huggan P, Luey C, et al. Clinical Characteristics, Etiology, and Initial Management Strategy of Newly Diagnosed Periprosthetic Joint Infection: A Multicenter, Prospective Observational Cohort Study of 783 Patients. Open Forum Infect Dis. 2020;7(5):ofaa068. doi: 10.1093/ofid/ofaa068 ; PubMed Central PMCID: PMC7224250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheet OH, Grabowski NT, Klein G, Abdulmawjood A. Development and validation of a loop mediated isothermal amplification (LAMP) assay for the detection of Staphylococcus aureus in bovine mastitis milk samples. Mol Cell Probes. 2016;30(5):320–5. doi: 10.1016/j.mcp.2016.08.001 . [DOI] [PubMed] [Google Scholar]
- 24.Suebsing R, Kampeera J, Tookdee B, Withyachumnarnkul B, Turner W, Kiatpathomchai W. Evaluation of colorimetric loop-mediated isothermal amplification assay for visual detection of Streptococcus agalactiae and Streptococcus iniae in tilapia. Lett Appl Microbiol. 2013;57(4):317–24. doi: 10.1111/lam.12114 . [DOI] [PubMed] [Google Scholar]
- 25.Jang WS, Lim DH, Nam J, Mihn DC, Sung HW, Lim CS, et al. Development of a multiplex isothermal amplification molecular diagnosis method for on-site diagnosis of influenza. PLoS One. 2020;15(9):e0238615. doi: 10.1371/journal.pone.0238615 ; PubMed Central PMCID: PMC7485819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jang WS, Lim DH, Yoon J, Kim A, Lim M, Nam J, et al. Development of a multiplex Loop-Mediated Isothermal Amplification (LAMP) assay for on-site diagnosis of SARS CoV-2. PLoS One. 2021;16(3):e0248042. doi: 10.1371/journal.pone.0248042 ; PubMed Central PMCID: PMC7928493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo XG, Zhuang YR, Wen JZ, Xie TA, Liu YL, Zhu GD, et al. Evaluation of the real-time fluorescence loop-mediated isothermal amplification assay for the detection of Streptococcus agalactiae. Biosci Rep. 2019;39(5). doi: 10.1042/BSR20190383 ; PubMed Central PMCID: PMC6522725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kilic A, Basustaoglu AC. Double triplex real-time PCR assay for simultaneous detection of Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus hominis, and Staphylococcus haemolyticus and determination of their methicillin resistance directly from positive blood culture bottles. Res Microbiol. 2011;162(10):1060–6. doi: 10.1016/j.resmic.2011.07.009 . [DOI] [PubMed] [Google Scholar]
- 29.Escobar DF, Diaz-Dinamarca DA, Hernandez CF, Soto DA, Manzo RA, Alarcon PI, et al. Development and analytical validation of real-time PCR for the detection of Streptococcus agalactiae in pregnant women. BMC Pregnancy Childbirth. 2020;20(1):352. doi: 10.1186/s12884-020-03038-z ; PubMed Central PMCID: PMC7285471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li H, Xin H, Li SF. Multiplex PMA-qPCR Assay with Internal Amplification Control for Simultaneous Detection of Viable Legionella pneumophila, Salmonella typhimurium, and Staphylococcus aureus in Environmental Waters. Environ Sci Technol. 2015;49(24):14249–56. doi: 10.1021/acs.est.5b03583 . [DOI] [PubMed] [Google Scholar]
- 31.Lee CS, Wetzel K, Buckley T, Wozniak D, Lee J. Rapid and sensitive detection of Pseudomonas aeruginosa in chlorinated water and aerosols targeting gyrB gene using real-time PCR. J Appl Microbiol. 2011;111(4):893–903. doi: 10.1111/j.1365-2672.2011.05107.x ; PubMed Central PMCID: PMC3173516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics. 2006;118(2):511–21. doi: 10.1542/peds.2005-2824 . [DOI] [PubMed] [Google Scholar]
- 33.Vandercam B, Jeumont S, Cornu O, Yombi JC, Lecouvet F, Lefevre P, et al. Amplification-based DNA analysis in the diagnosis of prosthetic joint infection. J Mol Diagn. 2008;10(6):537–43. doi: 10.2353/jmoldx.2008.070137 ; PubMed Central PMCID: PMC2570637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim SG, Choi GW, Choi WS, Lim CS, Jang WS, Bae JH. Feasibility of Loop-Mediated Isothermal Amplification for Rapid Detection of Methicillin-Susceptible and Methicillin-Resistant Staphylococcus aureus in Tissue Samples. Clin Orthop Surg. 2022;14(3):466–73. doi: 10.4055/cios21277 ; PubMed Central PMCID: PMC9393274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li C, Shi Y, Yang G, Xia XS, Mao X, Fang Y, et al. Establishment of loop-mediated isothermal amplification for rapid detection of Pseudomonas aeruginosa. Exp Ther Med. 2019;17(1):131–6. doi: 10.3892/etm.2018.6910 ; PubMed Central PMCID: PMC6307377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramezani R, Kardoost Parizi Z, Ghorbanmehr N, Mirshafiee H. Rapid and Simple Detection of Escherichia coli by Loop-Mediated Isothermal Amplification Assay in Urine Specimens. Avicenna J Med Biotechnol. 2018;10(4):269–72. ; PubMed Central PMCID: PMC6252025. [PMC free article] [PubMed] [Google Scholar]
- 37.Lin Q, Xu P, Li J, Chen Y, Feng J. Direct bacterial loop-mediated isothermal amplification detection on the pathogenic features of the nosocomial pathogen—Methicillin resistant Staphylococcus aureus strains with respiratory origins. Microb Pathog. 2017;109:183–8. doi: 10.1016/j.micpath.2017.05.044 . [DOI] [PubMed] [Google Scholar]
- 38.Xu Z, Li L, Chu J, Peters BM, Harris ML, Li B, et al. Development and application of loop-mediated isothermal amplification assays on rapid detection of various types of staphylococci strains. Food Res Int. 2012;47(2):166–73. doi: 10.1016/j.foodres.2011.04.042 ; PubMed Central PMCID: PMC3390935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou W, Zhang Y, Wang S, Li Y, Zhang J, Zhang C, et al. LAMP, PCR, and real-time PCR detection of Acetobacter aceti in yogurt. Food Sci Biotechnol. 2017;26(1):153–8. doi: 10.1007/s10068-017-0020-7 ; PubMed Central PMCID: PMC6049496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parker J, Fowler N, Walmsley ML, Schmidt T, Scharrer J, Kowaleski J, et al. Analytical Sensitivity Comparison between Singleplex Real-Time PCR and a Multiplex PCR Platform for Detecting Respiratory Viruses. PLoS One. 2015;10(11):e0143164. doi: 10.1371/journal.pone.0143164 ; PubMed Central PMCID: PMC4646456 research could be based on the same materials used for FDA-approval. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang X, Zhao Y, Zeng Y, Zhang C. Evolution of the Probe-Based Loop-Mediated Isothermal Amplification (LAMP) Assays in Pathogen Detection. Diagnostics (Basel). 2023;13(9). doi: 10.3390/diagnostics13091530 ; PubMed Central PMCID: PMC10177487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364(9431):369–79. doi: 10.1016/S0140-6736(04)16727-5 . [DOI] [PubMed] [Google Scholar]
- 43.Bury DC, Rogers TS, Dickman MM. Osteomyelitis: Diagnosis and Treatment. Am Fam Physician. 2021;104(4):395–402. . [PubMed] [Google Scholar]
- 44.Elsissy JG, Liu JN, Wilton PJ, Nwachuku I, Gowd AK, Amin NH. Bacterial Septic Arthritis of the Adult Native Knee Joint: A Review. JBJS Rev. 2020;8(1):e0059. doi: 10.2106/JBJS.RVW.19.00059 . [DOI] [PubMed] [Google Scholar]
- 45.Mathews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. Lancet. 2010;375(9717):846–55. doi: 10.1016/S0140-6736(09)61595-6 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.