Abstract
Splenic infarction is a rare and likely underdiagnosed complication of Epstein-Barr virus (EBV)-associated infectious mononucleosis (IM). Here, we describe an 18-year-old Guyanese male with persistent severe left-sided abdominal pain found to be EBV positive and have a large splenic infarct, along with a transient decrease in protein C, protein S, and antithrombin III activity levels. He was treated with supportive care and anticoagulated with heparin and apixaban. We review prior reports and perspectives on underlying pathophysiology, diagnosis, and the management of these cases, which likely do not require anticoagulation but may be considered on a per-case basis.
Keywords: ebv, case report, epstein-barr virus, splenic infarction, infectious mononucleosis
Introduction
Infectious mononucleosis (IM), caused by Epstein-Barr virus (EBV), is characterized by fever, sore throat, lymphadenopathy, and fatigue. While most cases of IM are self-limiting and resolve without complication, rare complications such as splenic rupture or infarction have been described in 0.1-0.5% of cases [1,2]. EBV-associated splenic infarction has been reported in 29 cases per our literature review, yet the mechanism by which it occurs remains unclear. Although management typically involves supportive care, infarction should be considered in patients presenting with IM and abdominal pain to prevent potential complications such as rupture, abscess, and sepsis [3,4]. Here, we present an EBV-positive young adult male with abdominal pain, found to have a splenic infarct along with a transient decrease in protein C, S, and antithrombin III (ATIII) activity levels.
This article was previously posted to the Authorea preprint server on March 25, 2023.
Case presentation
An 18-year-old male with no past medical history presented in the emergency department (ED) with persistent left-sided abdominal pain for eight days with associated subjective fevers, nausea, and non-bilious, non-bloody emesis. His pain was described as burning and stabbing diffusely and localized more to the left upper quadrant (LUQ). He denied any recent illness, diarrhea, cough, recent travel, or other symptoms. His pain was well controlled with oral acetaminophen. The patient was in college, learning remotely, and denied recent sick contacts. He took no medications, had no family history of autoimmune disorders, and denied alcohol, tobacco, or drug use.
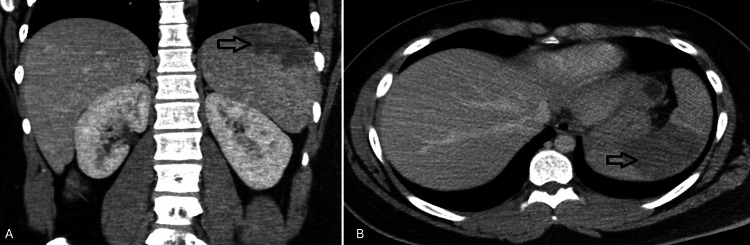
On presentation, he was afebrile (37.8°C) and tachycardic to 118 beats per minute. The exam was notable for LUQ and right lower quadrant abdominal tenderness. No lymphadenopathy, tonsillar edema/exudates, petechial hemorrhages, splenomegaly, or hepatomegaly were noted. Computed tomography (CT) revealed a mildly enlarged spleen measuring 13.8 cm with a large wedge-shaped region within the superior aspect of the spleen, compatible with infarct (Figures 1A, 1B).
Figure 1. CT scan of the abdomen demonstrating splenic infarction. (A) Coronal view and (B) transverse view.
Serology confirmed IM due to acute EBV infection with an elevated EBV immunoglobulin M (IgM) at >160.0 U/mL. Human immunodeficiency virus (HIV), coronavirus disease 2019 (COVID-19), and cytomegalovirus (CMV) tests were negative. Mild elevations in total white cell count (11.09 K/uL), prothrombin time (16.3 seconds), activated partial thromboplastin time (27.2 seconds), and international normalized ratio (1.38) were noted with unremarkable electrolyte panel. Liver function tests showed mild transaminitis with aspartate aminotransferase (AST) (51 U/L) and alanine transaminase (ALT) (74 U/L), slight elevation in lactate dehydrogenase (LDH) to 480 U/L, but normal haptoglobin and total and indirect bilirubin levels. Anti-nuclear factor titers were elevated (1:680) with speckling but with negative lupus anticoagulant (1.09, normal values < 1.2, with dilute Russell’s viper venom method). Decreased protein C antigen and activity levels (65% and 73%, respectively), protein S free activity level (49%), and a low but normal antithrombin III (ATIII) antigen level (19 mg/dL, normal values 19-31) with decreased activity (65%) were also found.
Unfractionated heparin was started in the ED, pain was well controlled with acetaminophen as needed, and the patient was discharged home on day 4 with apixaban 10 mg twice daily for seven days (loading dose) followed by 5 mg daily. He was evaluated in the clinic two months later during which magnetic resonance imaging (MRI) showed no change in spleen size or infarct, labs showed a still positive but reduced EBV IgM titer (56.0 U/mL). As the patient was asymptomatic following discharge, it was concluded that further follow-up was unnecessary. Consequently, apixaban was discontinued due to the lack of evidence supporting long-term anticoagulation for resolving previous infarcts.
Discussion
Previous cases of IM-associated splenic infarcts show several similarities; patients often present with a fever and abdominal pain (most commonly LUQ), and have splenomegaly on exam, although up to 30% of patients may be asymptomatic (Table 1) [5]. In our case, unfractionated heparin was initiated in the ED, and apixaban was started prophylactically due to a dearth of prior evidence and our patient’s decrease in protein C, S, and ATIII activity levels, with the anticipation of likely discontinuation on outpatient follow-up. Given that almost all prior reported cases improved with supportive management only, therapeutic anticoagulation is likely unnecessary in management but should still be considered on a case-by-case basis.
Table 1. Literature review of splenic infarction in EBV infectious mononucleosis.
M, male; F, female; LUQ, left upper quadrant; RUQ, right upper quadrant; N/A, not applicable; ASA, aspirin; EBV, Epstein-Barr virus
| Year | Age/Sex | Abdominal Pain | Splenomegaly | Splenic Rupture | Splenectomy | Anticoagulation | Survival | |
| Chevat et al. [6] | 1961 | N/A | LUQ | Yes | Yes | Yes | N/A | Yes |
| Guibaud et al. [7] | 1983 | 34/M | LUQ | N/A | N/A | Yes | N/A | Yes |
| Boivin and Bernard [8] | 1990 | 19/F | LUQ | Yes | No | Yes | N/A | Yes |
| Garten et al. [9] | 1992 | 57/F | No | Yes | No | Yes | N/A | Yes |
| Trevenzoli et al. [10] | 2001 | 17/M | LUQ | Yes | No | No | No | Yes |
| Symeonidis et al. [11] | 2001 | 17/M | LUQ | Yes | No | No | No | Yes |
| Kim and Kopelman [12] | 2005 | 40/M | LUQ | No | No | No | No | Yes |
| van Hal et al. [13] | 2005 | 35/F | LUQ | No | No | No | No | Yes |
| Benz et al. [14] | 2007 | 19/F | LUQ | Yes | No | No | No | Yes |
| Hunt et al. [4] | 2010 | 29/F | LUQ | Yes | No | No | No | Yes |
| Breuer et al. [15] | 2010 | 13/M | LUQ | Yes | No | No | No | Yes |
| Cull and Stein [16] | 2012 | 18/F | LUQ | Yes | Yes | No | No | Yes |
| Gang et al. [17] | 2013 | 7/F | RUQ | Yes | No | No | No | Yes |
| Gavriilaki et al. [18] | 2013 | 17/M | LUQ | Yes | No | No | No | Yes |
| Kobe et al. [19] | 2013 | 22/M | RUQ | Yes | No | No | No | Yes |
| Mackenzie and Liebmann [20] | 2013 | 18/M | LUQ | Yes | No | No | No | Yes |
| Li et al. [21] | 2014 | 19/F | Upper | Yes | No | No | No | Yes |
| Bhattarai et al. [22] | 2014 | 16/M | Epigastric | Yes | No | No | No | Yes |
| Machado et al. [23] | 2015 | 24/M | LUQ | Yes | No | No | No | Yes |
| Heo et al. [24] | 2016 | 20/F | LUQ | No | No | No | No | Yes |
| Naviglio et al. [25] | 2016 | 14/M | LUQ | Yes | No | No | No | Yes |
| Noor et al. [26] | 2017 | 25/F | LUQ | Yes | No | No | No | Yes |
| Li et al. [27] | 2018 | 24/F | LUQ | No | No | No | No | Yes |
| 20/M | LUQ | No | No | No | No | Yes | ||
| 25/F | LUQ | Yes | No | No | No | Yes | ||
| Pervez et al. [28] | 2020 | 20/M | LUQ | No | No | No | No | Yes |
| Turrian [29] | 2021 | 24/M | LUQ | N/A | No | No | 7 Days | Yes |
| Nishioka et al. [30] | 2022 | 19/M | LUQ | No | No | No | No | Yes |
| Sowka and Mali [31] | 2022 | 60/M | Left Side | N/A | No | No | Lovenox to ASA | Yes |
The mechanism behind splenic infarction with EBV infection remains unclear. Splenic histopathology results are limited but have noted splenic lymphoid hyperplasia, partial fibrosis, and sinus congestion without thrombus formation. This hypercellularity has been thought to disrupt splenic sinus infrastructure, causing shifts in blood flow that are unable to meet the increased oxygen demand of an enlarged spleen and thereby increase the risk of ischemia [6,9,32,33]. Earlier case reports and studies have also suggested that transient coagulopathic states may be involved, with instances of decreased activity of proteins C and S, positive lupus anticoagulant and anticardiolipin antibodies, positive antiphospholipid antibodies, and increased factor VIII [4,15-17,23,27]. However, thrombophilia studies in most reports were unremarkable. An underlying predisposition in conjunction with the above may predispose certain patients to be more coagulopathic including hereditary spherocytosis, sickle cell trait, pyruvate kinase deficiency, or co-infection with other viruses [8,21,32,33]. However, most reports showed unremarkable thrombophilia studies and no signs of thrombus formation in other organ systems. Furthermore, almost all cases exhibited splenomegaly. Thus, we suspect architectural changes with lymphoproliferation within splenic sinuses likely contribute to infarction more than a transient thrombogenic state.
Point-of-care ultrasound is becoming more utilized as a first-line imaging modality in the acute setting for abdominal pain [7], but given that a 2009 retrospective study showed ultrasound sensitivity to be only 18% [2], contrast-enhanced CT should be the test of choice. MRI may be considered for pediatric populations in particular if ionizing radiation is a concern. Few prior studies reported follow-up imaging like ours, but results vary from improvement to no significant changes. Repeat CT or MRI is likely an unnecessary and costly test with little benefit in guiding further management. Patients should avoid contact sports to reduce the risk of splenic rupture for a minimum of three weeks after onset of clinical symptoms [34], although splenomegaly has been reported in cases to persist for longer (>8 weeks in our case). Clinicians may use ultrasound to help gauge improvement in splenomegaly if a patient plans to return to contact sports.
Conclusions
Although rare, splenic infarctions associated with IM should be considered in patients presenting with abdominal pain. There are currently no guidelines for diagnosis and management of these patients. Despite some cases having a self-limiting transient thrombogenic phase which doesn’t require anticoagulation, clinicians should be aware of potential complications including abscess and rupture.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Himanshu Patel, Awais Paracha, Adit Singhal, Vedika Agrawal, Jessica Cohen
Critical review of the manuscript for important intellectual content: Himanshu Patel, Awais Paracha, Adit Singhal, Kelly I. Suchman, Aaron Rhee, Vedika Agrawal, Jessica Cohen
Acquisition, analysis, or interpretation of data: Adit Singhal, Kelly I. Suchman, Aaron Rhee
Drafting of the manuscript: Adit Singhal, Aaron Rhee
Supervision: Jessica Cohen
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Infectious mononucleosis. Luzuriaga K, Sullivan JL. N Engl J Med. 2010;362:1993–2000. doi: 10.1056/NEJMcp1001116. [DOI] [PubMed] [Google Scholar]
- 2.Splenic infarction: 10 years of experience. Antopolsky M, Hiller N, Salameh S, Goldshtein B, Stalnikowicz R. Am J Emerg Med. 2009;27:262–265. doi: 10.1016/j.ajem.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 3.The natural history of splenic infarction. Jaroch MT, Broughan TA, Hermann RE. https://pubmed.ncbi.nlm.nih.gov/3764696/ Surgery. 1986;100:743–750. [PubMed] [Google Scholar]
- 4.Case records of the Massachusetts General Hospital. Case 29-2010. A 29-year-old woman with fever and abdominal pain. Hunt DP, Thabet A, Rosenberg ES. N Engl J Med. 2010;363:1266–1274. doi: 10.1056/NEJMcpc1007084. [DOI] [PubMed] [Google Scholar]
- 5.The clinical spectrum of splenic infarction. Nores M, Phillips EH, Morgenstern L, Hiatt JR. https://pubmed.ncbi.nlm.nih.gov/9486895/ Am Surg. 1998;64:182–188. [PubMed] [Google Scholar]
- 6.Splenic infarct and infectious mononucleosis [Article in French] Chevat H, Aulong C, Demaille A, Adenis L, Bertrand M. https://pubmed.ncbi.nlm.nih.gov/13692963/ Lille Med. 1961;6:314–317. [PubMed] [Google Scholar]
- 7.Transient neutrophil aggregation in a patient with infectious mononucleosis. Guibaud S, Plumet-Leger A, Frobert Y. Am J Clin Pathol. 1983;80:883–884. doi: 10.1093/ajcp/80.6.883. [DOI] [PubMed] [Google Scholar]
- 8.Pyruvate kinase deficiency, infectious mononucleosis, hemolytic anemia with cold autoantibodies and massive splenic infarction [Article in Turkish] Boivin P, Bernard JF. Presse Med. 1990;28:818–819. [PubMed] [Google Scholar]
- 9.CT manifestations of infectious mononucleosis. Garten AJ, Mendelson DS, Halton KP. Clin Imaging. 1992;16:114–116. doi: 10.1016/0899-7071(92)90123-q. [DOI] [PubMed] [Google Scholar]
- 10.Splenic infarct during infectious mononucleosis. Trevenzoli M, Sattin A, Sgarabotto D, Francavilla E, Cattelan AM. Scand J Infect Dis. 2001;33:550–551. doi: 10.1080/00365540110026629. [DOI] [PubMed] [Google Scholar]
- 11.Non hypoxia-related splenic infarct in a patient with sickle cell trait and infectious mononucleosis. Symeonidis A, Papakonstantinou C, Seimeni U, et al. Acta Haematol. 2001;105:53–56. doi: 10.1159/000046534. [DOI] [PubMed] [Google Scholar]
- 12.Medical mystery: abdominal pain--the answer. Kim KM, Kopelman RI. N Engl J Med. 2005;353:1421–1422. doi: 10.1056/NEJMc055352. [DOI] [PubMed] [Google Scholar]
- 13.Splenic infarction due to transient antiphospholipid antibodies induced by acute Epstein-Barr virus infection. van Hal S, Senanayake S, Hardiman R. J Clin Virol. 2005;32:245–247. doi: 10.1016/j.jcv.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 14.A surprising cause of chest pain. Benz R, Seiler K, Vogt M. https://pubmed.ncbi.nlm.nih.gov/18173027/ J Assoc Physicians India. 2007;55:725–726. [PubMed] [Google Scholar]
- 15.Splenic infarction in a patient hereditary spherocytosis, protein C deficiency and acute infectious mononucleosis. Breuer C, Janssen G, Laws HJ, Schaper J, Mayatepek E, Schroten H, Tenenbaum T. Eur J Pediatr. 2008;167:1449–1452. doi: 10.1007/s00431-008-0781-3. [DOI] [PubMed] [Google Scholar]
- 16.Splenic infarction, warm autoimmune hemolytic anemia and antiphospholipid antibodies in a patient with infectious mononucleosis. Cull E, Stein BL. Int J Hematol. 2012;95:573–576. doi: 10.1007/s12185-012-1047-4. [DOI] [PubMed] [Google Scholar]
- 17.Splenic infarction in a child with primary Epstein-Barr virus infection. Gang MH, Kim JY. Pediatr Int. 2013;55:0–8. doi: 10.1111/ped.12143. [DOI] [PubMed] [Google Scholar]
- 18.Splenic infarction as a rare complication of infectious mononucleosis due to Epstein-Barr virus infection in a patient with no significant comorbidity: case report and review of the literature. Gavriilaki E, Sabanis N, Paschou E, Grigoriadis S, Mainou M, Gaitanaki A, Skargani-Koraka M. Scand J Infect Dis. 2013;45:888–890. doi: 10.3109/00365548.2013.821627. [DOI] [PubMed] [Google Scholar]
- 19.A case of infectious mononucleosis with splenic infarction [Article in Japanese] Kobe D, Nakatani T, Fujinaga Y, et al. https://www.jstage.jst.go.jp/article/nisshoshi/110/8/110_1461/_article/-char/ja/ Nihon Shokakibyo Gakkai Zasshi. 2013;110:1461–1467. [PubMed] [Google Scholar]
- 20.Identification of splenic infarction by emergency department ultrasound. Mackenzie DC, Liebmann O. J Emerg Med. 2013;44:450–452. doi: 10.1016/j.jemermed.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Splenic infarction caused by a rare coinfection of Epstein-Barr virus, cytomegalovirus, and Mycoplasma pneumoniae. Li Y, Pattan V, Syed B, Islam M, Yousif A. Pediatr Emerg Care. 2014;30:636–637. doi: 10.1097/PEC.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 22.Splenic infarct: a rare presentation in a pediatric patient. Bhattarai P, Pierr L, Adeyinka A, Sadanandan S. https://pubmed.ncbi.nlm.nih.gov/26982903/ JNMA J Nepal Med Assoc. 2014;52:1017–1019. [PubMed] [Google Scholar]
- 23.The unexpected finding of a splenic infarction in a patient with infectious mononucleosis due to Epstein-Barr virus. Machado C, Melo Salgado J, Monjardino L. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-212428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Splenic infarction associated with acute infectious mononucleosis due to Epstein-Barr virus infection. Heo DH, Baek DY, Oh SM, Hwang JH, Lee CS, Hwang JH. J Med Virol. 2017;89:332–336. doi: 10.1002/jmv.24618. [DOI] [PubMed] [Google Scholar]
- 25.Splenic infarction in acute infectious mononucleosis. Naviglio S, Abate MV, Chinello M, Ventura A. J Emerg Med. 2016;50:0–3. doi: 10.1016/j.jemermed.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 26.Splenic infarct in a patient with infectious mononucleosis: a rare presentation. Noor M, Sadough M, Chan S, Singh G. J Community Hosp Intern Med Perspect. 2017;7:248–250. doi: 10.1080/20009666.2017.1361291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Splenic infarction: an under-recognized complication of infectious mononucleosis? Li Y, George A, Arnaout S, Wang JP, Abraham GM. Open Forum Infect Dis. 2018;5:0. doi: 10.1093/ofid/ofy041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.A mysterious case of an infarcted spleen due to kissing disease: a rare entity. Pervez H, Tameez Ud Din A, Khan A. Cureus. 2020;12:0. doi: 10.7759/cureus.6700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Splenic infarction after Epstein-Barr virus infection: case report. Turrian U. Ann Clin Case Rep. 2021;6:2045. [Google Scholar]
- 30.Case report: splenic infarction in infectious mononucleosis due to Epstein-Barr virus infection. Nishioka H, Hayashi K, Shimizu H. Am J Trop Med Hyg. 2021;106:623–625. doi: 10.4269/ajtmh.21-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.S3213 Transient splenic infarct in a patient with Epstein Barr virus (EBV) infection: a rare presentation. Sowka B, Mali P. https://journals.lww.com/ajg/fulltext/2022/10002/s3213_transient_splenic_infarct_in_a_patient_with.3213.aspx Am J Gastroenterol. 2022;117:0. [Google Scholar]
- 32.Splenic infarction after Epstein-Barr virus infection in a patient with hereditary spherocytosis. Suzuki Y, Shichishima T, Mukae M, et al. Int J Hematol. 2007;85:380–383. doi: 10.1532/IJH97.07208. [DOI] [PubMed] [Google Scholar]
- 33.Splenic infarction after Epstein-Barr virus infection in a patient with hereditary spherocytosis: a case report and literature review. Ma Z, Wang Z, Zhang X, Yu H. BMC Surg. 2022;22:136. doi: 10.1186/s12893-022-01580-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Infectious mononucleosis in the athlete. Diagnosis, complications, and management. Maki DG, Reich RM. Am J Sports Med. 1982;10:162–173. doi: 10.1177/036354658201000308. [DOI] [PubMed] [Google Scholar]