SUMMARY
A literature review was conducted to assess the role of minimally-invasive endoscopic treatments for lacrimal pathway neoplasms. The study involved the analysis of 316 patients with benign or malignant tumours affecting the lacrimal drainage system. Histologically, the analysis revealed a prevalence of squamous cell carcinoma, followed by lymphatic neoplasms and melanomas. In terms of treatment, minimally-invasive endoscopic approaches, such as endoscopic dacryocystorhinostomy, play a predominant role in managing early-stage tumours, rather than merely obtaining samples for histological analysis. For more extensive tumours, which constitute the majority of cases, more aggressive external approaches are required, along with the use of adjuvant radiotherapy and chemotherapy. The lack of universally shared staging systems poses a limitation in standardisation and comparison of results. Treatment of these tumours remains complex due to their rarity and histological heterogeneity. A multidisciplinary approach is mandatory to optimise outcomes.
KEY WORDS: lacrimal drainage system, lacrimal pathway, tumours, endoscopic treatment, dacryocystorhinostomy, review
Introduction
Tumours of the lacrimal sac can be classified as primary, secondary, or metastatic. The latter involve the lacrimal pathways through direct extension by contiguity, predominantly originating from the orbital and nasal cavities, rather than through distant haematogenous spread. These are rare conditions that are mostly treated like primary tumours. Similarly, primary tumours of the lacrimal sac are rare: malignancies account for approximately 72% of cases, demonstrating local invasiveness and high recurrence rate. Benign tumours tend to manifest in younger adults, while malignant tumours typically present in the fifth decade 1. Tumours of the lacrimal sac are classified into four main categories: epithelial (71-75%), mesenchymal (12-15%), and haematolymphoid (10-12%). Epithelial tumours constitute the most prevalent group, with squamous papilloma, transitional papilloma, fibrous histiocytoma, oncocytoma, and solitary fibrous tumour/haemangiopericytoma being among the most frequent histotypes. The most common malignant tumours include squamous cell carcinoma (SCC), non-keratinising SCC, non-Hodgkin lymphoma, melanoma, and adenocarcinoma. SCC, the most common malignant epithelial tumour, accounts for 19-23% of all lacrimal sac tumours 1-5.
Regarding clinical presentation, lacrimal pathway tumours typically manifest with epiphora (53-100%), bleeding (11%), nasal obstruction, and purulent or bloody discharge 1,6. Notably, these non-specific clinical manifestations can lead to a misdiagnosis of lacrimal sac tumours as dacryocystitis, and patients are diagnosed with malignancy only after protracted treatment (e.g. by nasolacrimal duct cleaning) for presumed inflammatory conditions. In case of large or invasive tumours, a mass at the medial canthus or lacrimal sac is present (28-100%) 1,6-7, often associated with proptosis, ocular motility impairment, and dystopia 2,8.
Orbital or paranasal sinus CT scans are employed to diagnose lacrimal sac tumours and assess associated osteolytic changes. In cases of suspected lacrimal neoplasms, dacryo-CT and MRI of the orbit and maxillo-facial structures are essential 6-12.
Treatment should be tailored to the histological type and extent of pathological progression 13. Evidence suggests that for early-stage lesions confined to the lacrimal fossa, optimal oncological outcomes are associated with total excision of the lacrimal sac (dacryocystectomy [DCT] without osteotomy). In these cases, modified dacryocystorhinostomy (DCR) or planned reconstruction may subsequently occur, following histological confirmation and completion of treatment. Aggressive malignant lesions may necessitate more extensive resections, involving the entire lacrimal drainage system, typically performed through a lateral rhinotomic approach 8. Extension into adjacent compartments (orbit and paranasal sinuses) may require more demolitive approaches, such as exenteration orbitae and extensive resection into the sinonasal compartment 7,14. Adjuvant treatment is often required in these scenarios, usually in the form of external beam radiotherapy (RT), local RT (brachytherapy), chemotherapy (especially the combination regimen represented by cyclophosphamide, doxorubicin, vincristine, and prednisone [CHOP]) or immunotherapy 1.
It appears that a more extensive resection through lateral rhinotomy is associated with better local control (12.5% vs 43.7% local recurrence) 1. However, given the rarity of the disease, the literature provides broad ranges of recurrence rates and mortality, reaching 50% and 37-100%, respectively, for epithelial neoplasms. Concerning primary lymphomas, systemic involvement is reported in 33% of cases, with a 5-year overall survival rate of 65%. Similar to what observed for paranasal sinuses, malignant melanoma is linked to the worst prognosis, characterised by early metastatic dissemination and disease-related mortality 1,15-23.
Materials and methods
A thorough examination of the existing literature pertaining to the therapy of lacrimal pathway benign and malignant tumours was undertaken using PubMed and Google Scholar as primary resources for information retrieval. The search queries employed were “lacrimal sac tumor*,” and “nasolacrimal duct tumor*”. This study exclusively incorporated publications over the past decade, specifically from 2013 to 2023. The exclusion criteria addressed papers describing metastatic tumours and cancers infiltrating the lacrimal pathways from nearby anatomical sites (i.e. secondary malignancies). Furthermore, non-English language articles were excluded. The principal aim of this investigation was to scrutinise therapeutic modalities, encompassing both medical and surgical interventions, with a particular emphasis on the application of minimally-invasive techniques in the management of malignancies affecting the lacrimal sac and nasolacrimal duct. The following key elements were specifically delineated for the comprehensive review: tumour histology, surgical treatment (including the employed approach and associated lateral cervical lymph nodes dissection), adjuvant treatments (RT and/or chemotherapy), and overall outcomes.
Results
A total of 80 articles meeting inclusion criteria were identified, describing 315 clinical cases. One original case report from our group was also included, for a total of 316 cases (Tab. I).
Table I.
Case series of lacrimal pathway tumours.
| Authors | No. of cases | Histological diagnosis | Surgical strategy | RT/CTx | Neck dissection | Recurrence |
|---|---|---|---|---|---|---|
| Wakasaki (2023) 27 | 25 | Benign
1 inverted papilloma 2 exophytic papilloma Malignant 6 SCC 2 adenoid cystic carcinoma 2 sebaceous carcinoma 1 mucoepidermoid carcinoma 11 lymphoma |
The initial treatment of benign (n = 3) and epithelial malignancies (n = 22) was surgery. Extended total maxillary resection with eyeball resection was performed in 2 SCC and one sebaceous carcinoma.
11 of the 14 patients underwent free-flap mandibular reconstructions following resection |
3 RT
5 CTx |
2 SCC underwent neck dissection.
One patient pN+ (submental and submandibular lymph nodes, no extranodal extension) |
3 of 22 patients with malignant tumour had locoregional recurrence, but only one patient with sebaceous carcinoma died of locoregional and brain/bone metastases. Two patients survived with distant metastases (one basaloid SCC and one adenoid cystic carcinoma) |
| Bai (2023) 42 | 15 | 15 lymphoma | 15 tumour resections
2 combined with DCR |
12 post-CTx | - | - |
| Sun (2022) 43 | 8 | 8 mucoepidermoid carcinoma | 6 tumours were managed with radical resection and 2 patients underwent orbital exenteration | 5 RT
1 RT+CTx |
- | 1 recurrence
2 metastases |
| Næser (2022) 44 | 1 | 1 angioleiomyoma | External DCT combined with endonasal, endoscopic anterior turbinectomy, and nasal mucosal resection | - | - | - |
| Meng (2022) 45 |
8 | 8 lymphoma | 3 Incisional biopsy
4 DCT 1 Medial maxillectomy |
5 RT
3 CTx |
- | - |
| Kim (2022) 46 | 1 | 1 large B-cell lymphoma | Lacrimal sac excision | - | - | Recurrence after 2 months, CTx |
| Kadir (2022) 1 | 10 | 1 papilloma
1 RLH 1 SFT 4 NHL 1 SCC 1 adenocarcinoma 1 mucoepidermoid carcinoma |
5 DCT
2 Incisional biopsy |
5 RT
2 CTx |
- | - |
| Amjad (2022) 47 | 1 | 1 small cell neuroendocrine carcinoma | - | CTx-RT | - | - |
| Almutairi (2022) 48 | 1 | 1 oncocytoma | DCT | - | - | Recurrence at 3 years |
| Turri-Zanoni (2022) 36 | 1 | 1 ectopic olfactory neuroblastoma | DCR, total ethmoidectomy, and medial maxillectomy | RT | - | No after 12 months |
| Howden (2021) 49 | 1 | 1 oncocytoma | Extended right Lynch incision | - | - | - |
| Azhdam (2021) 34 | 1 | 1 angioleiomyoma | 1 endoscopic excision of the lesion along with medial maxillectomy and DCR | - | - | - |
| Song (2020) 50 | 17 | 17 SCC | - | 17 RT
11 CTx |
- | 1 recurrence |
| Sharma (2020) 51 | 1 | 1 epithelial-myoepithelial carcinoma | Combined endoscopic endonasal and open approach | - | - | No after 20 months |
| Morawala (2020) 52 | 3 | 3 SFT | External and endoscopic approaches were used to assess the orbital clearance and manage the sinonasal extension and the nasolacrimal duct excision up to the inferior meatus | RT | - | - |
| Miller (2020) 53 | 1 | 1 transitional cell carcinoma | Lacrimal sac excision and medial maxillectomy | RT | - | No after 5 years |
| Cheang (2020) 54 | 1 | 1 inverted papilloma | Combined endonasal and external approach | - | - | - |
| Chang (2020) 33 | 1 | 1 SCC | Image-guided surgery, navigation-assisted transnasal endoscopic-assisted excision | RT+CTx | - | Recurrence after 3 months |
| Alam (2020) 55 | 1 | 1 apocrine adenocarcinoma | Orbital exenteration | RT | - | No after 1 year |
| Zhang (2019) 56 | 18 | 9 SCC
7 poorly differentiated carcinoma 1 transitional cell carcinoma 1 adenoid cystic carcinoma |
En bloc resection of the lacrimal sac malignancy was performed in all patients with concurrent partial ethmoidectomy in 8 patients and medial maxillectomy in 5 patients | 18 CTx+RT | - | - |
| Wu (2019) 57 | 1 | 1 sebaceous carcinoma | Combined external and endoscopic approach | - | - | No after 3 months |
| Ucgul (2019) 58 | 2 | 2 MALT lymphoma | Lacrimal sac excision within the tumour, canalicular DCR with bicanalicular silicone intubation | 1 CTx+RT
1 RT |
- | 1 recurrence |
| Purser (2019) 59 | 1 | 1 inverted papilloma | Endoscopic DCR | - | - | - |
| Morawala (2019) 60 | 1 | 1 adenocarcinoma | Combined endonasal and external approach | RT | - | No after 10 months |
| Matsuo (2019) 25 | 15 | 15 melanoma | 14 DCT
1 exenteratio orbitae |
7 CTx
2 RT 1 Immunotherapy |
3 (1 submandibular and pre-auricular nodes; 1 laterocervical nodes; 1 submandibular nodes) | 4 recurrences |
| Gervasio (2019) 61 | 1 | 1 inverted papilloma | Combined endonasal and external approach | - | - | - |
| Bowen (2019) 62 | 1 | 1 adenoid cystic carcinoma | DCT, anterior ethmoidectomy, and medial maxillectomy | RT | - | No after 5 years |
| Song (2018) 21 | 90 | 69 SCC
7 lymphoma 3 adenocarcinoma 3 adenoid cystic carcinoma 2 melanoma 2 transitional cell carcinoma 1 mucoepidermoid carcinoma 1 malignant neurilemmoma 1 haemangioendothelioma 1 Merkel cell carcinoma |
40 local tumour resections
26 extended tumour resections 3 orbital exenterations |
21 RT definitive
26 post-RT 43 pre-RT 50 RT+CTx |
Positive lymph nodes status at diagnosis significantly associated with a worse overall survival and progression-free survival (the number of patients undergoing neck dissection is not reported) | 22 recurrences |
| Nomura (2018) 63 | 1 | 1 adenocarcinoma and transitional cell carcinoma | Lateral rhinotomy | - | - | Recurrence, RT |
| Khanna (2018) 64 | 1 | 1 melanoma | Lateral rhinotomy approach, including the nasolacrimal duct, part of the lateral wall of the nose, the lacrimal sac, distal upper and lower canaliculi, and inferomedial orbital fat | RT | - | - |
| Haft (2018) 35 | 1 | 1 pleomorphic adenoma | Combined endonasal and external approach | - | - | - |
| Curragh (2018) 65 | 1 | 1 SCC | Combined external and endoscopic prelacrimal approach | - | - | - |
| Subramaniam (2017) 26 | 1 | 1 melanoma | Maxillectomy, exenteratio orbitae with radial forearm free flap reconstruction | RT | Supra-omohyoid neck dissection (pN+) | - |
| Mikhail (2017) 66 | 1 | 1 extranodal NK/T-cell lymphoma | External DCR | RT+CTx | - | - |
| Krishna (2017) 8 | 3 | 3 SLL | Incisional biopsy by DCR | CTx+RT | - | - |
| Jakobiec (2017) 67 | 1 | 1 lymphoepithelial carcinoma | DCR | - | - | Recurrence at 2 years: combined transnasal and transconjunctival diagnostic debulking of the tumour + RT-CTx for regional cervical lymph nodes metastases |
| Huggins (2017) 68 | 1 | 1 basaloid adenocarcinoma | DCT | RT | - | - |
| Grumbine (2017) 69 | 1 | 1 smooth muscle tumour of uncertain malignant potential | DCT | - | - | - |
| Dave (2017) 70 | 1 | 1 transitional cell papilloma | DCT | - | - | - |
| Zarrabi (2016) 71 | 1 | 1 large B cell lymphoma | External excisional biopsy | RT+CTx | - | - |
| Watanabe (2016) 72 | 2 | 2 haemangiopericytoma | DCT | - | - | One case recurred 3 times during an 18-year period. The other did not recur during 51 months of follow-up |
| Roos (2016) 29 | 1 | 1 mucoepidermoid carcinoma | Excision of the lacrimal sac, nasolacrimal duct, paranasal sinuses | - | Radical neck dissection + parotidectomy | Metastasis in the right cavernous sinus at 6 months,
gamma knife RT |
| Ramos (2016) 38 | 1 | 1 adenoid cystic carcinoma | Lateral rhinotomy, osteotomy from the canthal ligament to the orbital floor. The orbital floor was reconstructed | RT | - | - |
| Park (2016) 73 | 1 | 1 adenocarcinoma | Right medial maxillectomy including removal of the inferior and middle turbinates and partial orbital exenteration | RT | - | No after 25 months |
| Moriyama (2016) 74 | 1 | 1 SFT | Combined approach with endoscopic-modified medial maxillectomy and external incision | - | - | - |
| Marunaka (2016) 75 | 1 | 1 large B-cell lymphoma | Endoscopic biopsy | RT+CTx | - | No after 3 months |
| Janakiram (2016) 37 | 1 | 1 mucoepidermoid carcinoma | External maxillectomy and forehead flap reconstruction | RT+CTx | - | - |
| Bousaadani (2016) 76 | 1 | 1 epidermoid carcinoma | Combined approach with endoscopic-modified medial maxillectomy and external incision | RT | - | No after 2 years |
| Belliveau (2016) 77 | 1 | 1 ectopic olfactory neuroblastoma | Resection of the lateral nasal wall and medial maxilla en bloc, endonasal DCR and DCT | RT | - | No after 17 months |
| Walijee (2015) 78 | 1 | 1 inverted papilloma | Combined external and endoscopic approach | - | - | - |
| Wada (2015) 31 | 1 | 1 adenoid cystic carcinoma | - | Proton beam therapy | - | - |
| Vagia (2015) 79 | 1 | 1 adenocarcinoma | Maxillectomy and exenteratio orbitae | RT+CTx | Neck dissection + parotidectomy | Recurrence at 2 years: second line CTx, then third line CTx and then anti-androgens drugs (abiraterone) with good clinical response |
| Tsao (2015) 80 | 1 | 1 large B cell lymphoma | Endoscopic biopsy | RT+CTx | - | - |
| Satchi (2015) 81 | 5 | 5 melanomas | Case 1: orbital exenteration and lateral rhinotomy with en bloc excision of the orbital contents and entire lacrimal pathway
Case 2: orbital exenteration and DCT with a combined external and endonasal procedure. Case 3: orbital exenteration with en bloc excision of the entire lacrimal system within the medial wall of the orbit and maxilla. Case 4: orbital exenteration. Case 5: orbital exenteration |
- | - | Case 1: died within 8 months for metastases.
Case 2: developed metastasis in the parotid gland 4 years after exenteration and underwent a superficial parotidectomy and radical neck dissection. Case 3: local recurrence in the maxilla and lateral nasal wall 4 years after exenteration: resection of the lesion and RT. Case 4: en bloc excision of the medial orbit and medial maxilla for recurrence after 2 years. Case 5: recurrence after 3 years: en bloc resection of medial orbital wall, lateral nasal wall and medial maxilla, radial forearm free flap reconstruction and postoperative RT. |
| Papastefanou (2015) 82 | 1 | 1 small lymphocytic lymphoma | Endoscopic biopsy | CTx | - | - |
| Litschel (2015) 83 | 4 | 4 small cell lymphocytic lymphomas | Biopsy by endoscopic DCR | RT+CTx | - | - |
| Lee (2015) 84 | 2 | 2 SCC | Wide resection of lacrimal sac and nasolacrimal duct via anterior orbitotomy and medial maxillectomy via lateral rhinotomy | RT | - | - |
| Lee (2015) 85 | 1 | 1 benign mixed tumour | DCT | - | - | - |
| Iordanous (2015) 86 | 1 | 1 mucoepidermoid carcinoma associated to squamous/transitional cell papilloma | Maxillectomy | - | - | - |
| Higashi (2015) 24 | 1 | 1 melanotic neuroectodermal tumour | External maxillectomy | RT+CTx | - | - |
| Hardy (2015) 87 | 1 | 1 inverted papilloma | Maxillectomy | - | - | - |
| Abdelkhalek (2015) 88 | 2 | 2 MALT lymphomas | - | RT | - | - |
| Neffendorf (2014) 89 | 1 | 1 rhabdomyosarcoma | - | RT+CTx | - | - |
| Linxweiler (2014) 90 | 1 | 1 exophytic Schneiderian carcinoma | DCT+DCR | - | - | - |
| Kurdi (2014) 91 | 1 | 1 SFT | DCT+DCR | - | - | - |
| Guo (2014) 92 | 5 | 5 lymphomas | - | RT+CTx | - | - |
| Erickson (2014) 18 | 1 | 1 transitional cell-type papillary carcinoma | Medial maxillectomy, inferior turbinectomy, ethmoidectomy, and partial rhinectomy, reconstruction by a paramedian forehead flap and myocutaneous cheek advancement flap | RT | - | No after 1 year |
| Yuksel (2013) 93 | 1 | 1 mucoepidermoid carcinoma | The tumour, lacrimal sac, and nasolacrimal duct were removed en bloc with the frontal process of the maxilla, lateral nasal wall, lacrimal fossa, ethmoids, and anterior part of the medial orbital wall | RT | - | - |
| Mulay (2013) 94 | 1 | 1 oncocytoma | DCT | - | - | - |
| Maegawa (2013) 95 | 1 | 1 melanoma | Lateral rhinotomy, en bloc excision, including the lacrimal apparatus, medial wall of the orbit, and medial upper and lower lids, and medial maxillectomy. A T-shaped, median forehead flap repaired the defect | RT+CTx | - | - |
| Kim (2013) 32 | 1 | 1 osteoma | Endoscopic DCR | - | - | - |
| Jung (2013) 96 | 1 | 1 oncocytic carcinoma | Combined approach: DCT+ endoscopic inferior medial maxillectomy, including medial wall of maxillary sinus, inferior turbinate, and lateral wall of nasal cavity | RT | - | - |
| Islam (2013) 30 | 1 | 1 bilateral metachronous SCC arising within inverted papilloma | Orbital exenteration, medial
maxillectomy and radial forearm free flap reconstruction |
- | Selective left (I-III) neck dissection (pN0) | After 2 years, excision of the contralateral lacrimal sac, lamina papyracea and anterior and posterior ethmoids for a SCC arising within an IP extended to the orbit. Died for systemic metastasis after 1 year |
| Ishida (2013) 28 | 1 | 1 adenocarcinoma | DCT and exenteratio orbitae | - | Submandibular, and upper-, mid-, and lower-internal deep cervical lymph nodes (pN+) | - |
| Hodgson (2013) 97 | 1 | 1 bilateral SCC | Medial maxillectomy and DCT through a lateral rhinotomy approach | - | - | No after 6 months |
| Gustafson (2013) 98 | 1 | 1 synchronous verrucous carcinoma and inverted papilloma | Endoscopic debulking and DCT | - | - | - |
| Eweiss (2013) 99 | 20 | 10 transitional cell papillomas
10 transitional cell carcinomas |
Lateral rhinotomy | 7 RT | - | 4 recurrences |
| Donnadieu (2013) 100 | 1 | 1 oncocytoma | DCT | - | - | - |
| Chai (2013) 101 | 1 | 1 lymphoma | - | RT+CTx | - | No after 1 year |
| Azari (2013) 102 | 1 | 1 transitional cell carcinoma | DCT | - | - | - |
| Original case report | 1 | 1 SCC arising within inverted papilloma | DCR, medial maxillectomy and anterior ethmoidectomy | - | - | No after 6 months |
| RLH: reactive lymphoid hyperplasia; SFT: solitary fibrous tumour; NHL: non-Hodgkin’s lymphoma; SCC: squamous cell carcinoma; DCT: dacryocystectomy; CTx: chemotherapy; RT: radiotherapy; SLL: small lymphocytic lymphoma; DCR: dacryocystorhinostomy; IP: inverted papilloma. | ||||||
Tumour histology
From the histological standpoint, malignant tumours were found in 276 cases (87%), benign tumours in 31 cases (9.8%), and borderline tumours with malignant potential (haemangiopericytoma, solitary fibrous tumour, smooth muscle tumour) were identified in 9 cases (2.8%). Among the malignancies, SCC was indisputably the most prevalent, identified in 36.7% of cases, followed by neoplasms of lymphatic origin (including non-Hodgkin lymphoma, MALTomas, and unspecified lymphomas) reported in 21.5% of cases, and melanomas, accounting for 7.9%, including one case of childhood neuroectodermal melanocytic tumour 24. Less represented histologies were papilloma (7.6%), mucoepidermoid carcinoma (4.7%), transitional cell carcinoma (5%), adenocarcinoma (3.5%), and adenoid cystic carcinoma (2.8%). Other tumour types were infrequently reported, with a maximum of 5 clinical cases described: solitary fibrous tumour, reactive lymphoid hyperplasia, oncocytoma, musculoskeletal tumour of uncertain malignancy, lymphoepithelial carcinoma, alveolar rhabdomyosarcoma, benign tumour with mixed histology, olfactory neuroblastoma, haemangiopericytoma, Schneiderian carcinoma, osteoma, oncocytic carcinoma, angioleiomyoma, myoepithelial carcinoma, neurilemmoma, angioendothelioma, Meckel cell carcinoma, sebaceous carcinoma, pleomorphic adenoma, and neuroendocrine carcinoma. This literature review reaffirms the remarkable histological variability of benign and malignant tumours involving this specific anatomical region, underscoring the complexity of treatment, which should be tailored to the histotype.
Surgical treatment
The surgical interventions employed for treatment of these lesions consisted of the following: demolitive surgery via an open approach (i.e., extended maxillectomy, lateral rhinotomy, orbital exenteration, and potential reconstruction with a free flap), external DCT, and endoscopic DCR. These treatments were utilised exclusively or in conjunction with each other in combined approaches (open surgery + DCR, DCR + DCT).
Out of the 316 clinical cases analysed, an open surgical approach was used in 58.9%. The combined approach of DCR + DCT was employed in 7.9% of patients, while the combined approach of open surgery + DCR was used in 5.7%. An exclusive endoscopic approach (DCR) was feasible in only 6 cases (1.9% of the present review). Finally, in the remaining 29.1% of cases, the surgical approach served solely for diagnostic purposes, and curative treatment was administered through chemo-RT; in these instances, biopsy was conducted through an endoscopic approach in 73.9% of patients.
Neck treatment
A total of 3.6% of patients with malignant tumours underwent lateral neck dissection, 4 for melanoma, 2 for SCC, 2 for adenocarcinoma, 1 for mucoepidermoid carcinoma, and 1 for SCC arising within an inverted papilloma 25-30. The lymph nodes removed were mainly preauricular and at levels IA, IB, II, III, and IV. All 4 cases of melanoma, one case of adenocarcinoma, and one case of SCC had positive lymph nodes on histopathological examination. The SCC arising within the inverted papilloma had negative lymph nodes. In the locally advanced adenocarcinoma described by Vagia 79 and in the mucoepidermoid carcinoma described by Roos 29, the histopathological outcome of neck dissection was not clearly indicated, however the resection was extended to the parotid gland. As reported by Song in 2018, positive lymph node status at diagnosis was significantly associated with worse overall and progression-free survival 21.
Due to the rarity of these tumours and the extremely small number of studies in the literature, there is currently no consensus on recommendations and/or guidelines about treatment of T and N.
Non-surgical treatments
Of the 316 patients treated, 62.6% underwent RT, either exclusively or with adjuvant intent. On the other hand, 32.6% received chemotherapy.
Only one patient, who was diagnosed with adenoid cystic carcinoma, declined the proposed surgical treatment and opted for proton beam therapy. Notably, two years after treatment, the patient exhibited clinical improvement with no clinical or instrumental signs of persistent disease 31. However, no long-term follow-up data are available, which could be of particular interest considering the specific histology of this case, characterised by a high probability of long-term recurrence.
Gamma knife RT was employed in a 44-year-old patient who had undergone maxillectomy, parotidectomy, and lateral cervical lymphadenectomy for a mucoepidermoid carcinoma of the lacrimal sac. Six months after surgery, the patient presented with diplopia due to tumour relapse in the right cavernous sinus, and was deemed unsuitable for neurosurgical intervention. Notably, the MRI conducted 4 months after gamma knife RT initiation revealed partial regression of the mass, and another MRI after 4 years demonstrated complete macroscopic tumour regression 29.
Outcomes
Recurrence and mortality rates of lacrimal pathways tumours are very variable.
Benign tumours have good prognosis if completely excised, although inverted papillomas tend to recur. The sample considered in this review includes benign and malignant tumours arising from the lacrimal sac and nasolacrimal duct; this heterogeneity, together with the lack of information about outcomes and recurrence in some articles, did not make it possible to provide statistically significant data. An interesting paper by Kadir et al. about lacrimal sac tumours reported that the recurrence rate of invasive epithelial malignancies (SCC, mucus-secreting adenocarcinoma, and non-keratinising SCC) appears to be approximately 50% 1. Metastasis to the bone and skin has been reported in the literature, especially for melanoma, mucoepidermoid carcinoma, adenoid cystic carcinoma, SCC, and sebaceous adenocarcinoma. In our study, neck dissection was performed in 10 cases, with evidence of lymph node metastasis in 6 patients. As reported by Kadir, evidence of lymph node metastasis at diagnosis is significantly associated with a worse overall and progression-free survival. Malignant melanoma is associated with the worst prognosis despite aggressive treatment 1.
Clinical cases treated by an exclusively endoscopic DCR
CASE 1 BY KIM ET AL. 32
A 47-year-old man presented with unilateral epiphora, swelling of the medial canthus, and periorbital pain that developed over the past few months. Ophthalmological and neurological evaluations revealed no diplopia, visual disturbances, or headache. CT scan unveiled a calcified mass measuring 0.5 x 0.4 cm in the left nasolacrimal duct and a mucocele in the left maxillary sinus. Dacryocystography indicated contrast medium blockage. The patient underwent DCR with marsupialisation of the mucocele and removal of the neoformation. Silicone stents were placed and subsequently removed after 6 months to ensure the patency of the lacrimal passage. The tumour displayed an irregular surface, whitish coloration, and hard consistency. Histopathological analysis confirmed the diagnosis of a mature, compact osteoma. Given the benign nature of the neoplasm, no further therapeutic steps were required. Symptoms completely regressed postoperatively, and no signs of complications or recurrence were noted at 24 months after treatment.
CASE 2 BY CHANG ET AL. 33
A 55-year-old woman with a history of thyroid carcinoma presented with epiphora persisting for several months. CT scan revealed a neoformation originating from the right lacrimal sac, extending to the ipsilateral orbit and nasal fossa. A biopsy under local anaesthesia identified the mass as a SCC. The patient declined surgical interventions that could even minimally alter her facial aesthetics, leading to the exclusive adoption of an endoscopic approach. The mass was successfully removed using image-guided surgery, completely preserving both vision and ocular motility. The postoperative course was uneventful. Subsequently, the patient underwent adjuvant chemo-RT. However, a follow-up CT scan performed at 3 months postoperatively revealed disease recurrence.
CASE 3 BY AZHDAM ET AL. 34
A 65-year-old woman with a clinical history of chronic oedema of the right lower eyelid and epiphora presented with a solid lesion in the subnasolacrimal area, lacking radiological features indicative of malignancy on CT. Preoperative diagnostic endoscopy revealed a right deviation of the nasal septum and swelling corresponding to the right lacrimal sac. The patient underwent endoscopic excision of the lesion, medial maxillectomy, septoplasty, and DCR. Intraoperative biopsy indicated the benign nature of the lesion, with smooth walls and no evidence of bone invasion or other malignant characteristics. The final histological examination identified the lesion as an angioleiomyoma, obviating the need for further medical and/or surgical treatments.
CASE 4 BY HAFT ET AL. 35
A 60-year-old man incidentally discovered a neoplasm located beneath the inferior turbinate with dilation of the ipsilateral nasolacrimal duct during a contrast-enhanced CT scan. Subsequently, an endoscopically guided biopsy was performed, revealing a tumour of glandular origin. The patient underwent endoscopic DCR, complemented by endoscopic medial maxillectomy. The conclusive histological examination confirmed the presence of a pleomorphic adenoma and, therefore, no further therapy was administered. At 8 weeks postoperatively, the patient exhibited no signs of surgical complications or disease recurrence.
CASE 5 BY TURRI-ZANONI ET AL. 36
A 41-year-old man complained of right nasal obstruction and epistaxis. Endoscopic examination and contrast-enhanced MRI showed a confined right lacrimal sac neoformation without orbital invasion. Therefore, an endoscopic biopsy was performed, and the mass was identified as an olfactory neuroblastoma Hyams II. The tumour was staged as Kadish B. Subsequently, he underwent an endoscopic endonasal resection, with total ethmoidectomy, medial maxillectomy and removal of the medial wall of the right lacrimal sac. During surgery, frozen sections revealed no invasion of the olfactory mucosa. Consequently, dural resection and olfactory bulb removal were not performed. Histologic examination confirmed the diagnosis of olfactory neuroblastoma. The patient underwent adjuvant RT. No evidence of disease was seen after 12 months of follow-up.
CASE 6, ORIGINAL CASE TREATED AT “SANT’ANNA” HOSPITAL (COMO)
A 74-year-old Caucasian woman presented with a prolonged history of left epiphora and recent recurring ipsilateral epistaxis. Nasal endoscopy revealed a bleeding neoformation emerging from the left inferior meatus. CT scan and gadolinium-enhanced MRI identified the lesion’s epicentre within the nasolacrimal duct, with widening of its caudal part and abutment of the tumour from the Hasner’s valve (Fig. 1). Histological analysis confirmed it to be an inverted papilloma with high-grade dysplasia. To achieve complete surgical excision, an endoscopic medial maxillectomy extending to the inferior turbinate and the apical portion of the nasolacrimal duct was performed. Intraoperative histopathological examination of frozen sections ensured a radical resection without lacrimal sac infiltration. Surgery was successful, with no complications and complete resolution of epiphora. Pathological examination later confirmed the diagnosis of sinonasal papilloma with mixed growth pattern and in situ SCC within high-grade dysplasia (Fig. 2). Six-month follow-up showed no recurrence (Fig. 1).
Figure 1.
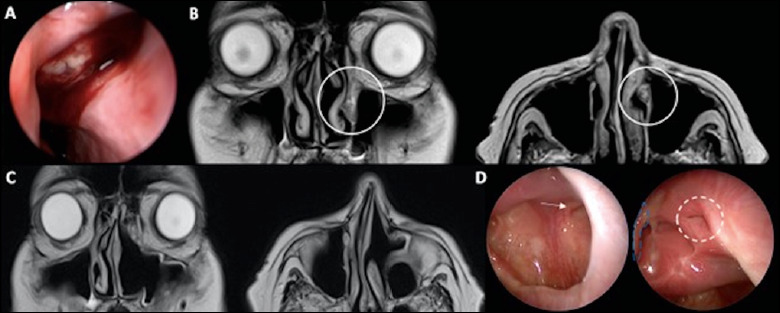
A) endoscopic appearance of the lesion during first examination; B) MRI showing a polypoid mass (10 x 7 mm in axial dimension) arising from the distal nasolacrimal duct, mildly hypo-intense on T1 and T2-weighted images, and avidly enhancing on post-contrast images with hypo-intense borders; C) follow-up MRI at 6 months after surgery showing no evidence of recurrence; D) endoscopic follow-up at 6 months after surgery showing no recurrence with residual nasolacrimal duct patency (white arrow: infraorbital nerve; white ring: opening of residual nasolacrimal duct, blue line: middle turbinate residue).
Figure 2.
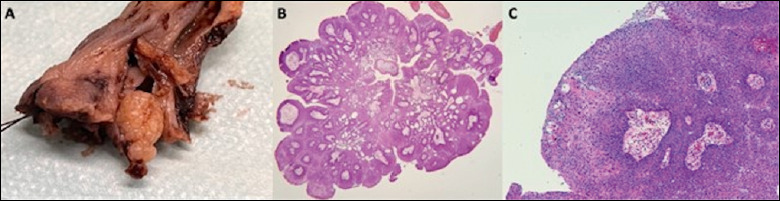
A) surgical specimen including left inferior turbinate and a white, shiny, multilobulated, and exophytic mass of 9 x 6 x 5 mm protruding from the naso-lacrimal duct opening; B) exophytic and endophytic growth pattern (haematoxylin and eosin, 4x magnification); C) transitional epithelium with scattered goblet cells and squamous metaplasia (haematoxylin and eosin, 100x magnification).
Discussion
This study gathered data from patients diagnosed with lacrimal pathways tumours across various institutions. It analysed histology, surgical approaches, and adjuvant treatments applied. The primary objective was to evaluate the feasibility of utilising minimally invasive approaches to lacrimal pathway neoplasms, particularly endoscopic DCR. The study sought to explore the oncological outcomes and prognosis of patients undergoing this specific treatment modality.
From the present analysis, the most frequently encountered tumour was SCC, found in 36.7% of cases, followed by neoplasms of lymphatic origin and melanomas. Benign tumours were identified in 9.8% of cases, with the most common histology being papilloma (inverted, transitional and exophytic types).
Our literature review confirms that the imaging techniques employed for the loco-regional study of this type of tumours include CT and contrast-enhanced MRI, although there was no homogeneous use of these methods across all investigated studies. In some papers, only contrast-enhanced MRI was used, while in others, only contrast-enhanced CT was employed. The recommendation should be to use both techniques in cases of suspected mass in the lacrimal pathways, since the information obtained from the combination of both methods is helpful in guiding treatment decisions.
Currently, due to the rarity of these neoplasms, there is no defined staging system for lacrimal pathway tumours. Canzone et al. proposed a staging system based on the outcomes of 69 patients with SCC 12: I. tumours confined to the lacrimal sac fossa; II. tumour invasion of lacrimal canaliculi/globe/nasolacrimal duct; III. tumour invasion of paranasal sinuses; IV. invasion of orbital apex, lymph nodes, and/or distant metastasis 12. However, the literature review conducted herein confirms that this type of staging system is not widely applied, making it challenging to compare results across different institutions. In this regard, an effort to adopt a shared staging system could assist in gathering multicentric data, enabling the comparison of more homogeneous oncological outcomes based on disease stage.
Alongside histological type, tumour size, local infiltration, potential aesthetic-functional impact of resection, and the patient’s general conditions are all factors to be considered in planning treatment. Considering the crucial position of the lacrimal pathways in relation to the orbit, nasal pyramid, paranasal sinuses, and cranial base, especially in cases of advanced and extensively infiltrating neoplasms, achieving radical resection becomes challenging without employing extensive and demolitive approaches. Consequently, a multidisciplinary approach that combines surgery, RT, and systemic treatment is often utilised and should be evaluated within a multidisciplinary setting.
Considering the standard approach, management of these tumours typically involves surgical resection, followed in most cases by adjuvant RT. However, this approach poses challenges due to the close proximity of the lacrimal pathways to the orbit, the primary organ at risk. Orbital exenteration is often included in the therapeutic plan, and extensive resection involving portions of the maxilla, orbital frame, and facial soft tissues is undertaken 37. Nevertheless, it remains unclear whether the addition of orbital exenteration, as well as the use of such extensive resections, is truly effective in improving prognosis 38, similar to the case of orbital apex involvement by paranasal sinus tumours. Additionally, the procedure adds morbidity that is related not only to the loss of ocular function, but also to the psychological impact associated with facial disfigurement 39.
This literature review suggests that an exclusively endoscopic approach is insufficient to manage these types of tumours and has been employed in only 1% of the cases analysed. This approach might be suitable for early-stage tumours that are limited to the lacrimal sac (stage I) or, at most, extending to the nasolacrimal duct without involvement of the canaliculi or orbital cavity (selected stage II). In most cases, however, surgical intervention requires an external approach, sometimes with the need for simultaneous reconstruction. The primary utility of an exclusive endoscopic approach lies in obtaining adequate material for pre-treatment diagnosis, which is crucial in therapeutic planning based on histotype. In a significant percentage of cases (29.7%) biopsy led to a diagnosis followed by non-surgical treatment. In 72.3% of these cases, the biopsy was obtained exclusively through an endoscopic approach, avoiding external incisions to obtain an adequate sample. The combined use of the endoscope for definitive surgical treatment was relatively rare, accounting for 11% of cases overall (DCR + DCT was used in 7.9% of cases, while a combined open surgery + DCR approach was applied in 5.7%). In these cases, the endoscope assists the surgeon, especially in managing the deep extension of the pathology towards the paranasal sinuses or the posterior region of the orbit, which are areas with poor visibility even with external approaches. Use of the endoscope can provide better visibility and disease control at this level, similarly to paranasal sinus tumours 39-41. Although this statement cannot be evidence-based for lacrimal sac tumours due to the rarity of such a disease, it is reasonable to assume that the advantage afforded by the endoscope may play a similar role in this type of condition.
Conclusions
Managing lacrimal sac tumours poses a complex and multidisciplinary challenge. Lack of international consensus on the staging of lacrimal tumours makes it difficult to establish standardised treatment strategies. However, it is evident that the most appropriate approach depends on histological type, tumour size, and the patient’s overall condition. Use of endoscopic DCR has shown promise for stage I lacrimal sac tumours that do not involve the canaliculi, offering success rates similar to external DCR but with fewer postoperative complications, superior aesthetic results, and shorter recovery times. However, for more extensive tumours or those with an infiltrative behaviour, a minimally-invasive endoscopic approach does not seem to be sufficient in obtaining local disease control. The surgical goal should remain radical resection, which cannot be sacrificed for the sake of the surgical technique employed. Finally, it is crucial to emphasise the importance of a multidisciplinary approach that combines surgery, RT, and pharmacological therapy to achieve the best clinical outcomes, similar to what has become the standard of care for paranasal sinus tumours.
Acknowledgements
The authors deeply thank all the partecipants in the study.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
MSR, AM, SC, FB, GG, PL, ADA, LV: contributed to data collection and analysis; MSR, AM, SC, FB: performed statistical analysis; MSR, AM, SC, FB, GG, PL, ADA, LV: performed manuscript preparation; GC, AMDG, MB: performed final edits and approved the submitted version.
Ethical consideration
Not applicable.
Figures and tables
References
- 1.Kadir SMU, Rashid R, Sultana S, et al. Lacrimal sac tumors: a case series. Ocul Oncol Pathol 2022;8:42-51. https://doi.org/10.1159/000520086 10.1159/000520086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montalban A, Liétin B, Louvrier C, et al. Malignant lacrimal sac tumors. Eur Ann Otorhinolaryngol Head Neck Dis 2010;127:165-172. https://doi.org/10.1016/j.anorl.2010.09.001 10.1016/j.anorl.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 3.Pe’er J, Hidayat AA, Ilsar M, et al. Glandular tumors of the lacrimal sac. Their histopathologic patterns and possible origins. Ophthalmology 1996;103:1601-1605. https://doi.org/10.1016/s0161-6420(96)30457-0 10.1016/s0161-6420(96)30457-0 [DOI] [PubMed] [Google Scholar]
- 4.Katircioglu YA, Altiparmak UE, Akmansu H, et al. Squamous cell carcinoma of the lacrimal sac. Orbit 2003;22:151-153. https://doi.org/10.1076/orbi.22.3.151.15616 10.1076/orbi.22.3.151.15616 [DOI] [PubMed] [Google Scholar]
- 5.Ansari SA, Pak J, Shields M. Pathology and imaging of the lacrimal drainage system. Neuroimaging Clin N Am 2005;15:221-237. https://doi.org/10.1016/j.nic.2005.02.001 10.1016/j.nic.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 6.Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye 2003;17:599-606. https://doi.org/10.1038/sj.eye.6700516 10.1038/sj.eye.6700516 [DOI] [PubMed] [Google Scholar]
- 7.Heindl LM, Jünemann AG, Kruse FE, et al. Tumors of the lacrimal drainage system. Orbit 2010;29:298-306. https://doi.org/10.3109/01676830.2010.492887 10.3109/01676830.2010.492887 [DOI] [PubMed] [Google Scholar]
- 8.Krishna Y, Coupland SE. Lacrimal sac tumors: a review. Asia Pac J Ophthalmol 2017;6:173-178. https://doi.org/10.22608/APO.201713 10.22608/APO.201713 [DOI] [PubMed] [Google Scholar]
- 9.Kim HJ, Shields CL, Langer PD. Lacrimal sac tumors: diagnosis and treatment. In: Black EH, Nesi FA, Cavana CJ, Gladstone GJ, Levine MR, eds. Smith and Nesi’s ophthalmic plastic and reconstructive surgery. New York: Springer; 2012. pp. 609-614. [Google Scholar]
- 10.Koturović Z, Knežević M, Rašić DM. Clinical significance of routine lacrimal sac biopsy during dacryocystorhinostomy: a comprehensive review of the literature. Bosn J Basic Med Sci 2017;17:1-8. https://doi.org/10.17305/bjbms.2016.1424 10.17305/bjbms.2016.1424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shao JW, Yin JH, Xiang ST, et al. CT and MRI findings in relapsing primary malignant melanoma of the lacrimal sac: a case report and brief literature review. BMC Ophthalmol 2020;20:191-195. https://doi.org/10.1186/s12886-020-01356-6 10.1186/s12886-020-01356-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song X, Wang S, Wang J, et al. Clinical management and outcomes of lacrimal sac squamous cell carcinoma. Head Neck 2019;41:974-981. https://doi.org/10.1002/hed.25529 10.1002/hed.25529 [DOI] [PubMed] [Google Scholar]
- 13.Singh S, Ali MJ. Primary malignant epithelial tumors of the lacrimal drainage system: a major review. Orbit 2021;40:179-192. https://doi.org/10.1080/01676830.2020.1769684 10.1080/01676830.2020.1769684 [DOI] [PubMed] [Google Scholar]
- 14.Valenzuela AA, Selva D, McNab AA, et al. En bloc excision in malignant tumors of the lacrimal drainage apparatus. Ophthalmic Plast Reconstr Surg 2006;22:356-360. https://doi.org/10.1097/01.iop.0000235819.06507.b1 10.1097/01.iop.0000235819.06507.b1 [DOI] [PubMed] [Google Scholar]
- 15.Sjö LD, Ralfkiaer E, Juhl BR, et al. Primary lymphoma of the lacrimal sac: an EORTC Ophthalmic Oncology Task Force study. Br J Ophthalmol 2006;90:1004-1009. https://doi.org/10.1136/bjo.2006.090589 10.1136/bjo.2006.090589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Palma P, Ravalli L, Modestino R, et al. Primary lacrimal sac B-cell immunoblastic lymphoma simulating an acute dacryocystitis. Orbit 2003;22:171-175. https://doi.org/10.1076/orbi.22.3.171.15620 10.1076/orbi.22.3.171.15620 [DOI] [PubMed] [Google Scholar]
- 17.Palamar M, Midilli R, Ozsan N, et al. Primary diffuse large B-cell lymphoma of the lacrimal sac simulating chronic dacryocystitis. Auris Nasus Larynx 2011;38:643-645. https://doi.org/10.1016/j.anl.2011.01.012 10.1016/j.anl.2011.01.012 [DOI] [PubMed] [Google Scholar]
- 18.Erickson BP, Modi YS, Ko MJ, et al. Transitional cell-type papillary carcinoma of the lacrimal sac manifesting as a medial canthal skin lesion. Orbit 2014;33:378-381. https://doi.org/10.3109/01676830.2014.894541 10.3109/01676830.2014.894541 [DOI] [PubMed] [Google Scholar]
- 19.Kuo CY, Tsai CC, Kao SC, et al. Comparison of clinical features and treatment outcome in benign and malignant lacrimal sac tumors. Biomed Res Int 2020;3545839. https://doi.org/10.1155/2020/3545839 10.1155/2020/3545839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabundayo MS, Takahashi Y, Kakizaki H. Lacrimal sac lymphoma: a series of Japanese patients. Eur J Ophthalmol 2019;29:678-684. https://doi.org/10.1177/1120672118803510 10.1177/1120672118803510 [DOI] [PubMed] [Google Scholar]
- 21.Song X, Wang J, Wang S, et al. Clinical analysis of 90 cases of malignant lacrimal sac tumor. Graefes Arch Clin Exp Ophthalmol 2018;256:1333-1338. https://doi.org/10.1007/s00417-018-3962-4 10.1007/s00417-018-3962-4 [DOI] [PubMed] [Google Scholar]
- 22.McGrath LA, O’Hagan SB. Malignant melanoma of the lacrimal sac: case report and major review with treatment update. J Ophthalmol Vis Neurosci 2016;1:1-4. https://scientonline.org/open-access/malignant-melanoma-of-the-lacrimal-sac-case-report-and-major-review-with-treatment-update.pdf [Google Scholar]
- 23.Grossniklaus HE, Eberhart CG, Kivelä TT. Lyon: International Agency for Research on Cancer (IARC); 2018. WHO classification of tumours of the eye; pp. 173-184. [Google Scholar]
- 24.Higashi K, Ogawa T, Onuma M, et al. Clinicopathological features of melanotic neuroectodermal tumor of infancy: report of two cases. Auris Nasus Larynx 2016;43:451-454. https://doi.org/10.1016/j.anl.2015.10.010 10.1016/j.anl.2015.10.010 [DOI] [PubMed] [Google Scholar]
- 25.Matsuo T, Tanaka T, Yamasaki O. Lacrimal sac malignant melanoma in 15 Japanese patients: case report and literature review. J Investig Med High Impact Case Rep 2019;7:2324709619888052. https://doi.org/10.1177/2324709619888052 10.1177/2324709619888052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Subramaniam SS, Anand R, Mellor TK, et al. Primary lacrimal sac melanoma with metastatic cervical disease: a review of the literature and case report. J Oral Maxillofac Surg 2017;75:1438-1441. https://doi.org/10.1016/j.joms.2017.01.015 10.1016/j.joms.2017.01.015 [DOI] [PubMed] [Google Scholar]
- 27.Wakasaki T, Yasumatsu R, Tanabe M, et al. Lacrimal sac tumors: a single-institution experience, including new insights. In Vivo 2023;37:1219-1225. https://doi.org/10.21873/invivo.13198 10.21873/invivo.13198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ishida M, Iwai M, Yoshida K, et al. Primary ductal adenocarcinoma of the lacrimal sac: the first reported case. Int J Clin Exp Pathol 2013;6:1929-1934. [PMC free article] [PubMed] [Google Scholar]
- 29.Roos JC, Beigi B. Lacrimal sac mucoepidermoid carcinoma with metastases to the cavernous sinus following dacryocystorhinostomy treated with stereotactic radiotherapy. Case Rep Ophthalmol 2016;7:274-278. https://doi.org/10.1159/000446152 10.1159/000446152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Islam S, Eisenberg RL, Hoffman GR. Malignant transformation of metachronous bilateral Schneiderian inverted papilloma of the lacrimal sac: management considerations and the contentious issue of orbital exenteration. Eur Arch Otorhinolaryngol 2014;271:1857-1860. https://doi.org/10.1007/s00405-013-2632-8 10.1007/s00405-013-2632-8 [DOI] [PubMed] [Google Scholar]
- 31.Wada K, Arai C, Suda T, et al. Primary adenoid cystic carcinoma of the nasolacrimal duct treated with proton beam therapy. Auris Nasus Larynx 2015;42:496-500. https://doi.org/10.1016/j.anl.2015.04.008 10.1016/j.anl.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 32.Kim JY, Kwon JH. An isolated nasolacrimal duct osteoma. J Craniofac Surg 2013;24:E319-E320. https://doi.org/10.1097/SCS.0b013e3182869f57 10.1097/SCS.0b013e3182869f57 [DOI] [PubMed] [Google Scholar]
- 33.Chang CH, Ku WN, Kung WH, et al. Navigation-assisted endoscopic surgery of lacrimal sac tumor. Taiwan J Ophthalmol 2020;10:141-143. https://doi.org/10.4103/tjo.tjo_65_19 10.4103/tjo.tjo_65_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azhdam AM, Wang Y, Douglas RS, et al. Angioleiomyoma of the nasolacrimal duct: case report and literature review. Orbit 2022;41:783-785. https://doi.org/10.1080/01676830.2021.1933080 10.1080/01676830.2021.1933080 [DOI] [PubMed] [Google Scholar]
- 35.Haft SJ, Jafari A, Lowenthal BM, et al. Pleomorphic adenoma of the nasolacrimal duct. JAMA Otolaryngol Head Neck Surg 2018;144:849-851. https://doi.org/10.1001/jamaoto.2018.1448 10.1001/jamaoto.2018.1448 [DOI] [PubMed] [Google Scholar]
- 36.Turri-Zanoni M, Gravante G, Dalfino G, et al. Ectopic primary olfactory neuroblastoma: case series and literature review. World Neurosurg 2022;158:E645-E653. https://doi.org/10.1016/j.wneu.2021.11.035 10.1016/j.wneu.2021.11.035 [DOI] [PubMed] [Google Scholar]
- 37.Alabiad CR, Weed DT, Walker TJ, et al. En bloc resection of lacrimal sac tumors and simultaneous orbital reconstruction: surgical and functional outcomes. Ophthal Plast Reconstr Surg 2014;30:459-467. https://doi.org/10.1097/IOP.0000000000000134 10.1097/IOP.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 38.Janakiram TN, Sagar S, Sharma SB, et al. Primary mucoepidermoid carcinoma of the lacrimal sac – A case report literature review. Klin Onkol 2016;29:291-294. [PubMed] [Google Scholar]
- 39.Ramos A, Pozo CD, Chinchurreta A, et al. Adenoid cystic carcinoma of the lacrimal sac: case report. Arq Bras Oftalmol 2016;79:333-335. https://doi.org/10.5935/0004-2749.20160095 10.5935/0004-2749.20160095 [DOI] [PubMed] [Google Scholar]
- 40.Turri-Zanoni M, Arosio AD, Agosti E, et al. Endoscopic-assisted orbital exenteration: technical feasibility and surgical results from a single-center consecutive series. J Craniomaxillofac Surg 2022;50:156-162. https://doi.org/10.1016/j.jcms.2021.11.005 10.1016/j.jcms.2021.11.005 [DOI] [PubMed] [Google Scholar]
- 41.Deganello A, Ferrari M, Paderno A, et al. Endoscopic-assisted maxillectomy: operative technique and control of surgical margins. Oral Oncol 2019;93:29-38. https://doi.org/10.1016/j.oraloncology.2019.04.002 10.1016/j.oraloncology.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 42.Bai F, Tao H, Zhou XB, et al. Primary lacrimal sac lymphoma: a case-based retrospective study in a Chinese population. Int J Ophthalmol 2023;16:532-538. https://doi.org/10.18240/ijo.2023.04.06 10.18240/ijo.2023.04.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun H, Cai R, Zhai C, et al. Primary mucoepidermoid carcinoma of the lacrimal apparatus. Am J Ophthalmol 2022;239:170-179. https://doi.org/10.1016/j.ajo.2022.03.008 10.1016/j.ajo.2022.03.008 [DOI] [PubMed] [Google Scholar]
- 44.Næser K, Pagh P, Friis P, et al. A rare case of lacrimal sac angioleiomyoma managed with dacryocystectomy and turbinectomy. Orbit 2024;43:147-150. https://doi.org/10.1080/01676830.2022.2085306 10.1080/01676830.2022.2085306 [DOI] [PubMed] [Google Scholar]
- 45.Meng FX, Yue H, Yuan YQ, et al. Lacrimal sac lymphoma: a case series and literature review. Int J Ophthalmol 2022;15:1586-1590. https://doi.org/10.18240/ijo.2022.10.04 10.18240/ijo.2022.10.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim J, Kim J, Baek S. Diffuse large B-cell lymphoma arising in the lacrimal sac. J Craniofac Surg 2022;33:E19-E21. https://doi.org/10.1097/SCS0000000000007861 10.1097/SCS0000000000007861 [DOI] [PubMed] [Google Scholar]
- 47.Amjad MM, Jacobs SM, Callahan MA, et al. Small cell neuroendocrine carcinoma presenting as recurrent dacryocystitis: case report of a rare entity. Ophthalmic Plast Reconstr Surg 2022;38:E2-E6. https://doi.org/10.1097/IOP.0000000000002052 10.1097/IOP.0000000000002052 [DOI] [PubMed] [Google Scholar]
- 48.Almutairi F, Alsamnan M, Maktabi A, et al. Recurrent oncocytoma of the lacrimal sac. Case Rep Pathol 2022;2955030. https://doi.org/10.1155/2022/2955030 10.1155/2022/2955030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Howden WB, Gunaratne DA, Gallagher RM. Excision of an unusual tumour of oncocytic origin: a case report. J Surg Case Rep 2021(5):rjab154. https://doi.org/10.1093/jscr/rjab154 10.1093/jscr/rjab154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Song X, He H, Zhu Y, et al. Treatment outcomes after definitive radio(chemo)therapy for 17 lacrimal sac squamous cell carcinoma. Br J Radiol 2020;93:20190633. https://doi.org/10.1259/bjr.20190633 10.1259/bjr.20190633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharma D, Neiweem A, Davis K, et al. Epithelial-myoepithelial carcinoma of the lacrimal sac and literature review of the lacrimal system. Allergy Rhinol (Providence) 2020;11:2152656720920600. https://doi.org/10.1177/2152656720920600 10.1177/2152656720920600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morawala A, Bothra N, Dendukuri G, et al. Solitary fibrous tumors of the lacrimal drainage system with variable orbital and sinonasal extensions: combined external and endoscopic surgical approach. Ophthalmic Plast Reconstr Surg 2020;36:403-409. https://doi.org/10.1097/IOP.0000000000001596 10.1097/IOP.0000000000001596 [DOI] [PubMed] [Google Scholar]
- 53.Miller HV, Siddens JD. Rare transitional cell carcinoma of the lacrimal sac. Am J Ophthalmol Case Rep 2020;20:100899. https://doi.org/10.1016/j.ajoc.2020.100899 10.1016/j.ajoc.2020.100899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cheang YFA, Loke D. Inverted papilloma of the lacrimal sac and nasolacrimal duct: a case report and review of the literature. Cureus 2020;12:E6989. https://doi.org/10.7759/cureus.6989 10.7759/cureus.6989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alam MS, Chandran VA, Krishnakumar S. Primary apocrine adenocarcinoma of the lacrimal sac: an extremely rare variant of lacrimal sac neoplasm. Orbit 2022;41:241-244. https://doi.org/10.1080/01676830.2020.1825752 10.1080/01676830.2020.1825752 [DOI] [PubMed] [Google Scholar]
- 56.Zhang R, Qian J, Meng F, et al. A staged procedure in the treatment of primary lacrimal sac epithelial malignancy: a retrospective cases analysis. Ophthalmic Plast Reconstr Surg 2019;35:187-192. https://doi.org/10.1097/IOP.0000000000001206 10.1097/IOP.0000000000001206 [DOI] [PubMed] [Google Scholar]
- 57.Wu A, Curragh DS, Morrow R, et al. Nasolacrimal duct obstruction secondary to lacrimal sac involvement by sebaceous carcinoma. Orbit 2020;39:433-436. https://doi.org/10.1080/01676830.2019.1700282 10.1080/01676830.2019.1700282 [DOI] [PubMed] [Google Scholar]
- 58.Ucgul AY, Tarlan B, Gocun PU, et al. Primary mucosa-associated lymphoid tissue (MALT) lymphoma of the lacrimal drainage system in two pediatric patients. Eur J Ophthalmol 2020;30:NP18-NP23. https://doi.org/10.1177/1120672119837085 10.1177/1120672119837085 [DOI] [PubMed] [Google Scholar]
- 59.Purser J, Arffa R, Clark D. Sinonasal (Schneiderian) papilloma of the lacrimal sac. Proc (Bayl Univ Med Cent) 2019;32:121-123. https://doi.org/10.1080/08998280.2018.1533357 10.1080/08998280.2018.1533357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morawala A, Bothra N, Mishra DK, et al. Poorly differentiated primary adenocarcinoma of the lacrimal sac and the nasolacrimal duct. Orbit 2020;39:289-292. https://doi.org/10.1080/01676830.2019.1687736 10.1080/01676830.2019.1687736 [DOI] [PubMed] [Google Scholar]
- 61.Gervasio KA, Mellen PL, Boparai RS, et al. Combined endoscopic and external resection of an inverted papilloma of the lacrimal sac: a case report and review of the literature. Allergy Rhinol (Providence) 2019;10:2152656719876254. https://doi.org/10.1177/2152656719876254 10.1177/2152656719876254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bowen RC, Ko HC, Avey GD, et al. Personalized treatment for lacrimal sac adenoid cystic carcinoma: case report and literature review. Pract Radiat Oncol 2019;9:136-141. https://doi.org/10.1016/j.prro.2019.01.011 10.1016/j.prro.2019.01.011 [DOI] [PubMed] [Google Scholar]
- 63.Nomura T, Maki D, Matsumoto F, et al. A rare case of coexisting lacrimal sac adenocarcinoma and transitional cell carcinoma. Ear Nose Throat J 2018;97:E32-E35. [PubMed] [Google Scholar]
- 64.Khanna RK, Fontaine A, Lemacon JM, et al. Hemolacria revealing a primary nasolacrimal duct melanoma. Can J Ophthalmol 2019;54:E70-E73. https://doi.org/10.1016/j.jcjo.2018.05.009 10.1016/j.jcjo.2018.05.009 [DOI] [PubMed] [Google Scholar]
- 65.Curragh DS, Psaltis AJ, Tan NC, et al. Prelacrimal approach for nasolacrimal duct excision in the management of lacrimal system tumours. Orbit 2019;38:308-312. https://doi.org/10.1080/01676830.2018.1518464 10.1080/01676830.2018.1518464 [DOI] [PubMed] [Google Scholar]
- 66.Mikhail M, Michel RP, Chankowsky J, et al. Epiphora as first presenting sign of primary extranodal NK/T-cell lymphoma of the lacrimal sac. Orbit 2017;36:19-21. https://doi.org/10.1080/01676830.2017.1279649 10.1080/01676830.2017.1279649 [DOI] [PubMed] [Google Scholar]
- 67.Jakobiec FA, Stagner AM, Rubin PAD. Lymphoepithelial carcinoma of the nasolacrimal duct: clinical, radiologic, and immunopathologic features. Ophthalmic Plast Reconstr Surg 2017;33:S18-S21. https://doi.org/10.1097/IOP.0000000000000478 10.1097/IOP.0000000000000478 [DOI] [PubMed] [Google Scholar]
- 68.Huggins AB, Stefanyszyn MA, Nyquist G, et al. Basaloid adenocarcinoma of the lacrimal sac: a rare entity and approach to management. Orbit 2017;36:441-444. https://doi.org/10.1080/01676830.2017.1337186 10.1080/01676830.2017.1337186 [DOI] [PubMed] [Google Scholar]
- 69.Grumbine FL, DeParis SW, Vagefi MR, et al. Lacrimal sac smooth muscle tumor of uncertain malignant potential. Ophthalmic Plast Reconstr Surg 2017;33:S29-S31. https://doi.org/10.1097/IOP.0000000000000726 10.1097/IOP.0000000000000726 [DOI] [PubMed] [Google Scholar]
- 70.Dave TV, Mishra D, Mittal R, et al. Accidentally diagnosed transitional cell papilloma of the lacrimal sac. Saudi J Ophthalmol 2017;31:177-179. https://doi.org/10.1016/j.sjopt.2017.04.010 10.1016/j.sjopt.2017.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zarrabi K, Desai V, Yim B, et al. Primary diffuse large B-cell lymphoma localized to the lacrimal sac: a case presentation and review of the literature. Case Rep Hematol 2016;499:1-3. https://doi.org/10.1155/2016/5612749 10.1155/2016/5612749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Watanabe A, Wu A, Sun MT, et al. Haemangiopericytoma of the lacrimal sac. Orbit 2016;35:233-235. https://doi.org/10.1080/01676830.2016.1176208 10.1080/01676830.2016.1176208 [DOI] [PubMed] [Google Scholar]
- 73.Park IA, Sa HS, Chung YS, et al. Androgen receptor-positive ductal adenocarcinoma of the nasolacrimal duct: a case report. Am J Ophthalmol Case Rep 2016;5:33-37. https://doi.org/10.1016/j.ajoc.2016.11.003 10.1016/j.ajoc.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moriyama M, Kodama S, Hirano T, et al. Endoscopic-modified medial maxillectomy and its limitation for a solitary fibrous tumor of the lacrimal sac and nasolacrimal duct. Auris Nasus Larynx 2017;44:370-374. https://doi.org/10.1016/j.anl.2016.07.010 10.1016/j.anl.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 75.Marunaka H, Orita Y, Tachibana T, et al. Diffuse large B-cell lymphoma of the lacrimal sac arising from a patient with IgG4-related disease. Mod Rheumatol 2018;28:559-563. https://doi.org/10.3109/14397595.2015.1131353 10.3109/14397595.2015.1131353 [DOI] [PubMed] [Google Scholar]
- 76.El Bousaadani A, Abada R, Belhadji M, et al. Primary epidermoid carcinoma of the lacrimal sac. Eur Ann Otorhinolaryngol Head Neck Dis 2016;133:373-374. https://doi.org/10.1016/j.anorl.2015.03.013 10.1016/j.anorl.2015.03.013 [DOI] [PubMed] [Google Scholar]
- 77.Belliveau MJ, Wang JC, Nijhawan N, et al. Staged endonasal-external resection of olfactory neuroblastoma involving the nasolacrimal duct and lacrimal sac. Can J Ophthalmol 2016;51:E173-E175. https://doi.org/10.1016/j.jcjo.2016.06.012 10.1016/j.jcjo.2016.06.012 [DOI] [PubMed] [Google Scholar]
- 78.Walijee HZ, Berry S, Quine S, et al. Inverted papilloma originating primarily from the nasolacrimal duct: a case report and review of the pertinent literature. Case Rep Otolaryngol 2015;2015:123694. https://doi.org/10.1155/2015/123694 10.1155/2015/123694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vagia E, Economopoulou P, Oikonomopoulos N, et al. Androgen-receptor positive lacrimal sac adenocarcinoma demonstrating long-lasting response to LHRH analog plus abiraterone treatment. Front Oncol 2015;5:10. https://doi.org/10.3389/fonc.2015.00010 10.3389/fonc.2015.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsao WS, Huang TL, Hsu YH, et al. Primary diffuse large B cell lymphoma of the lacrimal sac. Taiwan J Ophthalmol 2016;6:42-44. https://doi.org/10.1016/j.tjo.2014.11.002 10.1016/j.tjo.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Satchi K, McKelvie P, McNab AA. Malignant melanoma of the lacrimal drainage apparatus complicating conjunctival melanoma. Ophthalmic Plast Reconstr Surg 2015;31:207-210. https://doi.org/10.1097/IOP.0000000000000256 10.1097/IOP.0000000000000256 [DOI] [PubMed] [Google Scholar]
- 82.Papastefanou VP, René C, O’Donovan DG, et al. Atypical presentation of low-grade small lymphocytic lymphoma of the lacrimal sac. Ophthalmic Plast Reconstr Surg 2015;31:E163-E165. https://doi.org/10.1097/IOP.0000000000000188 10.1097/IOP.0000000000000188 [DOI] [PubMed] [Google Scholar]
- 83.Litschel R, Siano M, Tasman AJ, et al. Nasolacrimal duct obstruction caused by lymphoproliferative infiltration in the course of chronic lymphocytic leukemia. Allergy Rhinol (Providence) 2015;6:191-194. https://doi.org/10.2500/ar.2015.6.0130 10.2500/ar.2015.6.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee KH, Han SH, Yoon JS. Case reports of lacrimal sac tumors discovered in patients with persistent epiphora following dacryocystorhinostomy. Korean J Ophthalmol 2015;29:66-67. https://doi.org/10.3341/kjo.2015.29.1.66 10.3341/kjo.2015.29.1.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee JS, Lee H, Chang M, et al. Benign mixed tumor of the lacrimal sac. Indian J Ophthalmol 2015;63:282-284. https://doi.org/10.4103/0301-4738.156940 10.4103/0301-4738.156940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Iordanous Y, Belrose JC, Cadieux DC, et al. P63 positive mucoepidermoid tumor of the lacrimal sac with associated papilloma. Orbit 2015;34:220-222. https://doi.org/10.3109/01676830.2015.1049370 10.3109/01676830.2015.1049370 [DOI] [PubMed] [Google Scholar]
- 87.Hardy AW, Dwivedi RC, Masterson L, et al. Inverted papilloma of lacrimal sac invading into the orbit: case report and review of literature. J Cancer Res Ther 2015;11:238-240. https://doi.org/10.4103/0973-1482.155111 10.4103/0973-1482.155111 [DOI] [PubMed] [Google Scholar]
- 88.Abdelkhalek R, Ahmimech J, Mouzariae Y, et al. Traitement médical exclusif d’un lymphome bilatéral du MALT du sac lacrymal: à propos d’un cas [Case of a bilateral MALT lymphoma of the lacrimal sac treated only medically]. J Fr Ophtalmol 2015;38:E237. https://doi.org/10.1016/j.jfo.2014.11.026 10.1016/j.jfo.2014.11.026 [DOI] [PubMed] [Google Scholar]
- 89.Neffendorf JE, Bagdonaite L, Mudhar HS, et al. Adult alveolar rhabdomyosarcoma of the lacrimal sac. Orbit 2014;33:468-470. https://doi.org/10.3109/01676830.2014.950295 10.3109/01676830.2014.950295 [DOI] [PubMed] [Google Scholar]
- 90.Linxweiler M, Schick B, Hasenfus A, et al. Exophytic schneiderian carcinoma of the lacrimal sac: first case report. Pathology 2014;46:462-464. https://doi.org/10.1097/PAT.0000000000000129 10.1097/PAT.0000000000000129 [DOI] [PubMed] [Google Scholar]
- 91.Kurdi M, Allen L, Wehrli B, et al. Solitary fibrous tumour of the lacrimal sac presenting with recurrent dacryocystitis. Can J Ophthalmol 2014;49:E108-E110. https://doi.org/10.1016/j.jcjo.2014.05.011 10.1016/j.jcjo.2014.05.011 [DOI] [PubMed] [Google Scholar]
- 92.Guo P, Yan F, Tian C, et al. Imaging and histopathological findings of lacrimal sac lymphoma. Chin Med J (Engl) 2014;127:120-124. https://doi.org/10.3760/cma.j.issn.0366-6999.20132416 10.3760/cma.j.issn.0366-6999.20132416 [DOI] [PubMed] [Google Scholar]
- 93.Yuksel D, Kosker M, Saribas F, et al. Surgical treatment of mucoepidermoid carcinoma of the lacrimal sac. Semin Ophthalmol 2014;29:70-72. https://doi.org/10.3109/08820538.2013.771192 10.3109/08820538.2013.771192 [DOI] [PubMed] [Google Scholar]
- 94.Mulay K, Nair A, Honavar SG. Occult oncocytoma of the lacrimal sac. Saudi J Ophthalmol 2014;28:76-78. https://doi.org/10.1016/j.sjopt.2013.08.003 10.1016/j.sjopt.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Maegawa J, Yasumura K, Iwai T, et al. Malignant melanoma of the lacrimal sac: a case report. Int J Dermatol 2014;53:243-245. https://doi.org/10.1111/j.1365-4632.2012.05480.x 10.1111/j.1365-4632.2012.05480.x [DOI] [PubMed] [Google Scholar]
- 96.Jung JH, Shin DH, Cho KS, et al. Nasolacrimal duct obstruction caused by oncocytic carcinoma. Korean J Ophthalmol 2013;27:126-129. https://doi.org/10.3341/kjo.2013.27.2.126 10.3341/kjo.2013.27.2.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hodgson N, Whipple K, Lin JH, et al. Bilateral squamous cell carcinoma of the lacrimal sac. Ophthalmic Plast Reconstr Surg 2013;29:E149-E151. https://doi.org/10.1097/IOP.0b013e3182831c2d 10.1097/IOP.0b013e3182831c2d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gustafson C, Einhorn E, Scanlon MH, et al. Synchronous verrucous carcinoma and inverted papilloma of the lacrimal sac: case report and clinical update. Ear Nose Throat J 2013;92:E1. https://doi.org/10.1177/0145561313092010-1101 10.1177/0145561313092010-1101 [DOI] [PubMed] [Google Scholar]
- 99.Eweiss AZ, Lund VJ, Jay A, et al. Transitional cell tumours of the lacrimal drainage apparatus. Rhinology 2013;51:349-354. https://doi.org/10.4193/Rhino13.016 10.4193/Rhino13.016 [DOI] [PubMed] [Google Scholar]
- 100.Donnadieu B, Gire J, Boulze M, et al. Oncocytome du sac lacrymal: à propos d’un cas [Oncocytoma of the lacrimal sac: case report]. J Fr Ophtalmol 2013;36:E181-E182. https://doi.org/10.1016/j.jfo.2013.02.005 10.1016/j.jfo.2013.02.005 [DOI] [PubMed] [Google Scholar]
- 101.Chai CK, Tang IP, Tan TY. Primary lacrimal sac lymphoma with recurrence: a case report. Med J Malaysia 2013;68:269-270. https://www.e-mjm.org/2013/v68n3/lacrimal-sac-lymphoma.pdf [PubMed] [Google Scholar]
- 102.Azari AA, Kanavi MR, Saipe N, et al. Transitional cell carcinoma of the lacrimal sac presenting with bloody tears. JAMA Ophthalmol 2013;131:689-690. https://doi.org/10.1001/jamaophthalmol.2013.2907 10.1001/jamaophthalmol.2013.2907 [DOI] [PMC free article] [PubMed] [Google Scholar]


