Abstract
Objectives
Mobile health app-based interventions are increasingly being developed to support chronic disease management, particularly for epilepsy patients. These interventions focus on managing stress, monitoring drug side effects, providing education, and promoting adherence to medication regimens. Therefore, this scoping review aims to assess how mobile health applications improve epilepsy patients’ knowledge and seizure control, and to identify the features of these apps that are frequently used and have proven to be beneficial.
Methods
This scoping review was conducted using scientific databases such as ScienceDirect, PubMed, and Google Scholar, adhering to the Joanna Briggs Institute guidelines. The review framework consisted of five steps: identifying research questions, finding relevant articles, selecting articles, presenting data, and compiling the results. The literature search included all original articles published in English from 2013 to 2023.
Results
Among six articles that discussed mobile applications for epilepsy patients, all featured similar functionalities, including education on epilepsy management and seizure monitoring. Four of the articles highlighted behavioral interventions, such as reminder systems, designed to improve medication adherence. The remaining two articles focused on a side-effect reporting system that enabled doctors or health workers to evaluate and regularly monitor adverse effects.
Conclusions
This scoping review reveals that mobile health applications employing a combination of educational and behavioral interventions for epilepsy patients significantly improve knowledge about patient self-management and medication adherence. These interventions can prevent seizures, increase awareness, enable better activity planning, improve safety, and reduce the frequency of seizures and side effects of antiepileptic drugs.
Keywords: Epilepsy, Seizures, Mobile Applications, Knowledge, Self-management
I. Introduction
Epilepsy is a neurological condition characterized by unprovoked seizures, which include excessive abnormal discharge or neuronal activity in the brain due to factors such as head trauma, stroke, or metabolic conditions, with recurrent events [1,2]. The World Health Organization estimates that there are 50 million people with epilepsy worldwide, with higher prevalence rates in low- and middle-income countries. Epilepsy can cause daily discomfort and may lead to psychiatric problems [3]. Typically, epilepsy is managed through the administration of antiepileptic drugs, which are designed to prevent seizures. The selection of antiepileptic drugs should be tailored to the specific type of seizure [4]. Despite this, treatment failure remains significant. According to the Standard and New Antiepileptic Drug study, 29% of patients with generalized tonic-clonic seizures experienced antiepileptic drug failure [5]. This failure can result from non-adherence to prescribed medication, increasing the risk of seizure recurrence, which is directly correlated with higher rates of hospital admissions and increased healthcare costs [6,7]. Therefore, in addition to medications, it is crucial to develop behavioral interventions that effectively deliver positive clinical outcomes, such as seizure-free periods, reduced side effects, and enhanced societal contribution [1]. It is increasingly recognized that behavioral interventions for patients and their caregivers can be implemented through education, interviews, and counseling via online and digital platforms.
The use of mobile health systems in managing other chronic diseases, such as stroke, has proven beneficial in supporting patients and their families with emotional care, nutrition, exercise, and prevention of recurrent strokes [8]. Moreover, mobile applications for patients with hypertension have been shown to increase treatment adherence by up to 37.5% [9]. In today’s digital age, mobile health applications are excelling in improving health services, particularly for patients with epilepsy. These applications are expected to aid health workers in monitoring drug therapy, adherence, and adverse effects, as well as in providing drug information, motivation, and self-management tools. Additionally, clinical outcomes can be directly measured through enhanced features of mobile health applications and accessed directly by healthcare professionals such as neurologists and pharmacists.
However, little is known about the efficacy of mobile health applications in controlling seizures and the features they include to improve disease and drug-related knowledge. Therefore, this review explores how mobile health applications can improve knowledge and seizure control among epilepsy patients, aiming to identify the features that are frequently used and have proven to be beneficial. In the near future, it will be crucial to optimize application development in terms of features and outcomes to facilitate the adoption of mobile health systems in other areas.
II. Methods
This scoping review was carried out by a team consisting of pharmacists and neurologists following the Joanna Briggs Institute guidelines by Peters et al. [10] and the PRISMA Extension for Scoping Reviews by Tricco et al. [11]. The scoping review framework includes five steps: identifying research questions, finding relevant articles, selecting articles, presenting data, and compiling the results.
1. Identification of Research Questions
How can mobile health applications improve self-management knowledge and seizure control in epilepsy patients? This review seeks to explore the potential use of mobile health applications in managing epilepsy, with a particular focus on improving patient knowledge and seizure control. It also aims to examine the commonly used features of these apps that provide benefits.
2. Search for Relevant Articles
We conducted a systematic literature search across the ScienceDirect, PubMed, and Google Scholar databases using the Boolean combination: (“epilepsy” or “epileptic”) AND (“mobile” or “phone” or “applications” or “smartphone”) AND (“seizure”) AND (“self-management” or “knowledge”). This search encompassed all original articles published in English from 2013 until November 6, 2023, with full texts available. Four authors (I.E., Z.I., N.M.Y., and I.S.) employed a two-step procedure to select relevant articles. Initially, after eliminating duplicates, we independently reviewed the titles and abstracts of articles concerning interventions in mobile health applications for epilepsy patients.
3. Research Article Selection
The next step in the screening process involved a detailed review of full-text articles that satisfied the inclusion criteria, specifically those describing mobile health system interventions administered to epilepsy patients. The therapeutic parameters evaluated included knowledge pertaining to self-management and seizure control among these patients.
4. Data Presentation
Four authors (I.E., Z.I., N.M.Y., and I.S) were responsible for data extraction and presentation from the included studies. The information recorded in Tables 1 and 2 comprises authors, intervention description, participants involved, study design, components of the mobile health application for epilepsy, outcome parameters, instrument outcome parameters, and study results. The data are presented in a qualitative analysis based on the existing data in each article [12–17].
Table 1.
Summary of the included studies
| Author | Intervention description | Participants involved | Study design |
|---|---|---|---|
| Le Marne et al. [12] | “EpApp,” aiming to educate adolescents with epilepsy and facilitate their management. | Adolescents with epilepsy, ages 13–19, who were patients of the Sydney Children’s Hospital Network (Randwick and Westmead), of whom 51 adolescents completed baseline questionnaires. | Prospective cohort |
| Rajbhandari et al. [13] | Four local residents (trained as EFWs) used a smartphone application to estimate a potential score for an epileptic episode and contact an epilepsy expert. | 97 patients with epilepsy, ranging in age from 6 years to 77 years (from 112 patients with epilepsy-suggestive scores in the app). | Clinical intervention trial where EFWs used a smartphone application. |
| Simblett et al. [14] | Intervention with mobile health (mHealth) technology for real-time measurement and management of epilepsy, aiming to improve the care provided to people currently experiencing epileptic seizures. | Twenty people who were currently experiencing epileptic seizures. Adult patients with epilepsy who were over the age of 18 years and were experiencing at least one seizure per month. | A qualitative study with focus group discussions |
| Si et al. [15] | Intervention based upon a smartphone application in patients with epilepsy; the outcomes included self-management of epilepsy and self-reported seizure frequency | 380 patients with epilepsy were enrolled; 327 completed the 6-month follow-up (176 in the app group, 151 in the control group). The sample included adult patients (ages more than 18 but less than 60 years) with epilepsy of more than 1 year’s duration who had more than three seizures during the 6 months. | Randomized controlled trial |
| Mirpuri et al. [16] | Epilepsy smartphone application | Adult patients with epilepsy (age 18 years and above) and at least 1 year into treatment for epilepsy. 96 participants from a neurology outpatient department were randomly assigned to one of two groups: standard treatment and a mobile application group that employed a smartphone application. | Two-armed randomized controlled trial |
| Choi et al. [17] | A mobile epilepsy treatment app linked to a hospital’s electronic health record | Patients with epilepsy (aged ≥15) or caregivers of children with epilepsy (aged 1–15 years) at Seoul National University Bundang Hospital. The recruitment period lasted from April 2019 through August 2019. | A prospective study was conducted to compare healthcare data from clinics and the mobile application to assess whether the mobile application would improve self-management. |
EpApp: Epilepsy Mobile Application, EFW: epilepsy field workers.
Table 2.
Summary of the components of mobile health (mHealth) applications for epilepsy in the included studies
| Author | Components of the mobile health application for epilepsy | Outcome parameter measurements | Instrument outcome parameters | Study results |
|---|---|---|---|---|
| Le Marne et al. [12] |
|
|
|
|
| Rajbhandari et al. [13] |
|
|
|
|
| Simblett et al. [14] |
|
|
|
|
| Si et al. [15] |
|
|
|
|
| Mirpuri et al. [16] |
|
|
|
|
| Choi et al. [17] |
|
|
|
|
EpApp: epilepsy mobile application, AKEQ: adolescent knowledge of epilepsy, SSES-C: Seizure Self-Efficacy Scale for Children, EFW: epilepsy field workers, MGLs: Morisky Green Levine scale, ESMS: Epilepsy Self-Management Scale.
5. Results Compilation
A series of discussions between all authors were held to refine the best approach for reviewing, summarizing, and presenting the literature findings consistently. The results are organized and summarized according to their relevance to the overall research question.
III. Results
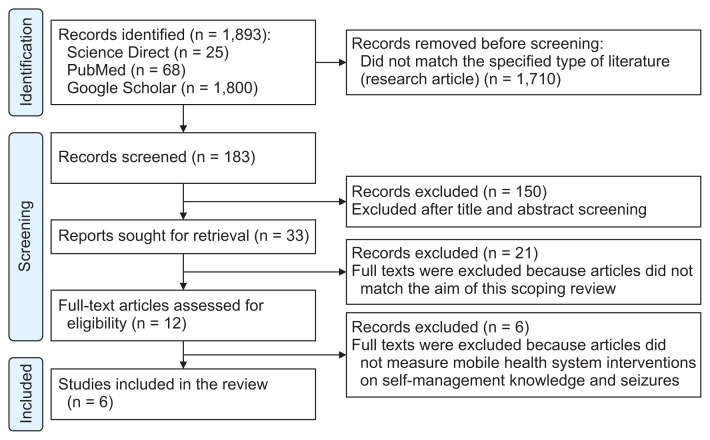
A comprehensive search of the ScienceDirect, PubMed, and Google Scholar databases yielded a total of 1,893 entries identified as potentially relevant for the study. After screening to remove duplicates and examining the abstracts of articles used in this scoping review, 183 articles were obtained. Upon reviewing the full text, we excluded 177 articles due to objectives that did not match and because they did not measure self-management knowledge and seizures as outcome parameters. Consequently, six articles were included in this scoping review (Figure 1). Of these, five were quantitative experimental studies, and one was a qualitative study featuring focus group discussions (Table 1). Table 2 describes the components found in the epileptic mobile applications, the outcome parameters measured, and the study results. Table 3 provides an explanation of the function of each feature and its effects or implications on epilepsy patients [12–22].
Figure 1.
Flow chart summarizing the literature search strategy and results.
Table 3.
Features of mobile health applications for epilepsy
| Features of mobile health applications for epilepsy | Function | Effects of features |
|---|---|---|
| Information about epilepsy | The provision of information related to epilepsy and management of medication [18]. | Education regarding the disease and treatment of epilepsy patients is very useful for increasing patient knowledge and improving awareness of the patient’s condition [12]. |
| Seizure diary | The provision of information regarding seizures, recording seizure events, time, and duration [16,17]. | This feature can also help patients write down seizure triggers. Patients can write down the form of seizures or aura events experienced by epilepsy patients [19]. |
| Reminder drug system | Reminders to take medication according to the schedule or rules prescribed by the doctor; reminders for taking medication can be in the form of an alarm for taking medication as well as a checklist or tracking that can determine medication usage. The drug reminder system can also be added to remind the user to consult or check with a doctor or refill a medication [18]. | The medication reminder feature in a mobile health system can increase compliance with medication use [20]. Research by Mirpuri et al. [16] has shown that the use of a mobile health system that uses the drug reminder feature can increase compliance with drug use. |
| Self-management of epilepsy | This feature contains information on the self-management of epilepsy patients, including lifestyle and other knowledge related to one’s ability to manage/manage epilepsy treatment [15]. | Self-management in epilepsy patients refers to the patient’s ability to adapt and adhere to behavioral adjustments necessary to reduce seizure frequency and improve overall health [21,22]. Self-management in epilepsy patients includes a set of skills, including good medication adherence, being able to explain, accurately documenting seizures, practicing seizure prevention measures, adequate rest, and self-management regarding stress levels [22]. Based on previous research, the use of a mobile health system can increase knowledge related to patient self-management [14,15]. |
| Adverse reaction reporting | This feature contains the presentation of complaints from epilepsy patients related to the use of antiepileptic drugs, including undesirable events and other side effects [17]. | Submitting complaints due to side effects of using antiepileptic drugs in the mobile health system feature can raise awareness, thereby increasing patient safety and providing information for doctors to consider in administering drugs and their dosage [13]. The side effect reporting feature can also make it more likely for patients to directly report their side effects [17]. |
IV. Discussion
1. Mobile Health Applications for Epilepsy Patients
Mobile application developers are increasingly focusing on helping chronic disease patients manage their daily health needs, including stress management, side effects of medications, sleep quality, medication adherence, and seizure control for those with epilepsy [21]. Our literature review identified several mobile health applications with unique features. For instance, the “EpApp” (epilepsy mobile application) is designed to educate and aid in the management of adolescents with epilepsy [12]. Additionally, there are systems that predict seizure episodes and facilitate contact with healthcare professionals [13,14]. Si et al. [15] and Mirpuri et al. [16] have also developed an epilepsy smartphone application that includes features for medication adherence, disease information, and patient seizure data. Furthermore, some epilepsy smartphone applications are integrated with a hospital’s electronic health record system [17] (Tables 1, 2).
Le Marne et al. [12] developed the “EpApp” mobile application to educate and facilitate epilepsy management for adolescents aged 13–19. This app includes two main features: educational content and seizure-related content. During clinical trials at the Sydney Children’s Hospital Network (Randwick and Westmead), the authors assessed patients’ knowledge, psychosocial factors, and clinical parameters, including medication adherence and seizure burden. In a separate study by Rajbhandari et al. [13], the intervention involved epilepsy field workers who utilized smartphone applications and telephone telemedicine to evaluate the safety and effectiveness of services for epilepsy patients. This application was designed to estimate the number of seizure episodes in epilepsy patients and to gauge the patient’s responsiveness in contacting health workers. Additional research on mobile health applications was conducted by Simblett et al. [14]. Through data collection via focus group discussions and interviews with patients who had experienced seizures, it was found that this application could improve self-management knowledge, helping patients understand and identify factors that provoke or trigger seizures, and potentially prevent them. Three other articles discussed the development of mobile health applications with features related to medication, self-management, and seizure frequency recording. These apps were accessible to patients directly on their mobile phones [15–17]. Among the six mobile applications reviewed for epilepsy patients, all shared common features, such as providing education on epilepsy management and monitoring seizures. Four of the articles described interventions aimed at increasing medication adherence through medication reminder systems. Two articles included features related to a side-effect reporting system, which allows doctors or health workers to evaluate and regularly monitor adverse effects.
Mobile health systems for epilepsy can remind patients to take their medication, record seizures, and facilitate online consultations with healthcare professionals [15]. Additionally, several apps provide information on lifestyle and offer education on health and self-management [12,16,17]. Some developers have also included features for monitoring drug side effects, comorbidities, and seizure-triggering factors, which both neurologists and patients can analyze to better understand their conditions and potentially prevent seizures [13,17]. There is an urgent need to report side effects associated with long-term medication use in conditions like epilepsy, to better understand the issues patients face due to drug use. The use of antiepileptic drugs in combination therapy (polytherapy) poses a higher risk of side effects compared to monotherapy [23]. The features were designed to improve medication adherence through various methods. An educational approach includes knowledge features about medication adherence and behavior change techniques, such as customizable drug reminders tailored to each patient’s regimen [17]. Medication adherence is crucial in epilepsy management apps because it is a key factor that affects seizure control. It has been demonstrated that the use of mobile applications with features for drug management reminders and self-management can significantly improve adherence to medication regimens, with an increase of about 60% in adherence observed in the intervention group [16].
Before discussing the impact of mobile health applications, it is necessary to consider the factors that contribute to successful epilepsy therapy. The first factor involves the patients’ characteristics, such as the onset of epilepsy, its etiology, the type and duration of seizures, and the duration of antiepileptic drug usage [24,25]. Additionally, socioeconomic factors including profession, education, culture, income, stigma, and family or community support can significantly affect quality of life and, consequently, influence adherence to medication and therapeutic outcomes [26–28]. The primary therapeutic goal for epilepsy patients is to achieve either seizure freedom or controlled seizures [29]. The administration of antiepileptic drugs typically starts with a monotherapy tailored to the type of seizure and epilepsy syndrome, beginning at the lowest possible dose. The dosage may be increased based on the effectiveness and side effects observed [30,31]. Despite good adherence to medication, seizures may still be triggered by various factors and conditions such as fever, trauma or injuries, lack of sleep, hypoxia, tumors, bleeding, poisoning, hyperventilation, photo-stimulation, stress, hormonal changes, puberty, and pregnancy [32,33]. Adherence to antiepileptic drug therapy can prevent up to 70% of recurrent seizures [34]. Moreover, other factors influencing patients’ adherence include ease of access to health facilities [35,36], treatment complexity [37], comorbidities, beliefs about the treatment [29], and adverse effects [37,38].
2. Impacts of Mobile Health Applications on Patients with Epilepsy
The use of mobile health applications by epilepsy patients has been shown to reduce non-adherence to antiepileptic medications and improve understanding of self-management [16]. Improving self-management skills and understanding patient self-efficacy in treatment can lead to increased success in therapy and improved quality of life [39–41]. Both educational and behavioral interventions can be implemented through mobile application usage. According to a study by Tang et al. [42], a mixed intervention combining educational strategies (such as verbal counseling or written education) and behavioral change interventions (like using a medication reminder) can decrease the number of patients who experience seizures and forget to take their medication [15,16]. The existence of motivation or self-perception related to health behavior that influences a person’s behavior is affected by at least three factors: general health values, which encompass interest and concern about health, specific health beliefs about vulnerability to particular health threats, and beliefs about the consequences of health problems [43]. Skill-based psychological interventions for adult and adolescent epilepsy patients have been shown to improve their quality of life [44].
Furthermore, seizure recording is a key feature of the mobile health application designed for epilepsy patients. Seizures are temporary events characterized by signs and/or symptoms that arise from excessive or abnormally synchronous neural activity in the brain [45]. It is important to maintain a seizure diary that includes the time, duration, and potential triggers of each seizure, as this information enables neurologists to assess the effectiveness of medications and the success of therapeutic interventions [46]. The mobile health application’s ability to evaluate seizure triggers helps patients identify and understand each event, potentially reducing the frequency of seizures [17]. Triggers such as lack of sleep, poor sleep quality, stress or psychological disorders, and non-adherence to medication can be monitored using the application [17]. The benefit of digital-based applications lies in their ability to provide patients with easy access to health information and consultations without the need for an inperson doctor visit [13].
The use of antiepileptic drugs frequently causes distress due to adverse drug reactions. Monitoring side effects is also a crucial parameter in managing both epilepsy and drug efficacy [30]. Side effects pose a significant challenge in the use of antiepileptic drugs and can greatly diminish quality of life [47]. These side effects often result from idiosyncratic neurocognitive reactions related to dosage or complications from long-term use [48,49]. Patients experiencing side effects may reduce their medication adherence or discontinue treatment altogether, thereby compromising the success of the therapy [50,51]. Successful therapy for managing epilepsy involves controlling seizures and improving quality of life without inducing side effects [49,52]. There is an urgent need to report side effects in long-term medications, such as those used for epilepsy, to better understand the issues that arise from the patient’s perspective regarding medication use.
The development of health applications for epilepsy patients includes a range of features, including information about epilepsy, seizure tracking, trigger identification, medication reminders, and tools for self-management [12,15,40]. Knowledge about the disease helps patients recognize their condition better, enabling them to respond more effectively during a seizure [40]. This disease-related information also covers aspects of self-management, such as the patient’s ability to adapt and adhere to behavioral changes necessary to decrease seizure frequency and improve overall health [21,22]. Self-management for epilepsy patients involves a set of skills that include proper medication adherence, the ability to communicate effectively, accurate seizure documentation, practicing seizure prevention strategies, ensuring adequate rest, and managing stress levels [22]. Understanding self-management is important for patients with epilepsy because it involves a personalized approach to recognizing conditions and actions that can prevent seizures, including lifestyle adjustments and trigger management. Personal factors influencing self-management include knowledge of procedures and guidelines, perceived benefits, the importance of self-management to the individual, and the skills required to implement these behaviors. Environmental factors and healthcare providers also play significant roles; appropriate information from healthcare providers can positively impact patients, and support from family or the environment can aid in the success of treatment. The use of mobile health system applications in epilepsy self-management has been shown to increase the proportion of patients who remain seizure-free. Within a 6-month observation period, 28% of patients in the intervention group remained seizure-free, compared to only 12% in the control group [15].
Chronically ill individuals, including those with epilepsy, face challenges in managing complex behaviors and often experience poor psychosocial adjustment and a diminished quality of life. Therefore, a self-care or self-management system is essential to complement pharmacological treatment [53]. Epilepsy self-care involves an individual’s ability to adapt to and comply with the necessary behavioral changes to decrease seizure frequency and improve quality of life [21,22]. Self-management for epilepsy patients encompasses skills such as medication adherence, accurate seizure documentation, implementation of seizure prevention strategies, obtaining adequate rest, and regulating stress effectively [22]. For pediatric epilepsy patients, self-management also involves educating the family and managing anxiety related to the patient’s condition [54,55]. When it comes to the use of medications and therapies in epilepsy patients, it is crucial to provide comprehensive information about the treatment— including drug usage, potential complaints, and the benefits of medication—to ensure optimal therapeutic outcomes [56]. Therefore, interventions aimed at self-management education and skill development help individuals with epilepsy increase their self-efficacy and improve their coping mechanisms, thereby improving their quality of life. In this context, mobile health applications play a significant role by enabling frequent communication between patients and healthcare providers, facilitating the transfer of health information and knowledge, and providing remote support to patients [19].
3. Limitations and Conclusion
The primary weakness of the epilepsy mobile health system, similar to other health applications, lies in the security of patient data and the stability of the network [57]. Challenges in developing mobile health system applications for epilepsy patients include the need to improve knowledge about creating secure mobile health systems [58]. Additionally, the availability of developers/stakeholders and the financial resources required for development are significant considerations [59,60]. In the realm of health applications, particularly mobile health systems for epilepsy patients, both development and evaluation are crucial. The application must be user-friendly, simple, and engaging to ensure that patients can effectively utilize it [19,61]. The use of a mobile health system for epilepsy significantly aids in the self-management of the condition. Employing an electronic seizure diary helps mitigate errors in recalling the number of seizures due to amnesia [19,62]. Another advantage of utilizing a mobile health system for epilepsy patients is that it assists them in remembering when to take their medication, thereby improving compliance and patients’ knowledge about their treatment [15,16]. The mobile health application for epilepsy integrates educational and behavioral elements, which can increase patients’ knowledge about self-management, adherence to medication, and the evaluation of seizures and side effects.
Acknowledgments
We acknowledge the support received from the Indonesian Endowment Funds for Education (LPDP) and the Center for Higher Education Funding (BPPT) number 202209091837 for financial support for education and research dissertations.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Cascino GC, Sirven JI, Tatum WO. Epilepsy. 2nd ed. Hoboken (NJ): John Wiley & Sons; 2021. [Google Scholar]
- 2.Aminoff M, Douglas V. Nervous system disorders. In: Papadakis MA, McPhee SJ, Rabow MW, editors. Current medical diagnosis & treatment. 56th ed. New York (NY): Mc-Graw Hill Education; 2023. pp. 970–1045. [Google Scholar]
- 3.World Health Organization . Epilepsy [Internet] Geneva, Switzerland: World Health Organization; 2024. [cited 2024 Apr 20]. Available from: https://www.who.int/news-room/fact-sheets/detail/epilepsy. [Google Scholar]
- 4.Nwani PO, Asomugha LA, Arinze EO, Ewereji KO, Nwosu MC, Ogunniyi A. Patterns of antiepileptic drug use and seizure control among people with epilepsy in a suburban community in Southeast Nigeria. Afr J Neurol Sci. 2012;31(2):36–42. [Google Scholar]
- 5.Bonnett LJ, Tudur Smith C, Smith D, Williamson PR, Chadwick D, Marson AG. Time to 12-month remission and treatment failure for generalised and unclassified epilepsy. J Neurol Neurosurg Psychiatry. 2014;85(6):603–10. doi: 10.1136/jnnp-2013-306040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faught RE, Weiner JR, Guerin A, Cunnington MC, Duh MS. Impact of nonadherence to antiepileptic drugs on health care utilization and costs: findings from the RANSOM study. Epilepsia. 2009;50(3):501–9. doi: 10.1111/j.1528-1167.2008.01794.x. [DOI] [PubMed] [Google Scholar]
- 7.Lie IA, Hoggen I, Samsonsen C, Brodtkorb E. Treatment non-adherence as a trigger for status epilepticus: an observational, retrospective study based on therapeutic drug monitoring. Epilepsy Res. 2015;113:28–33. doi: 10.1016/j.eplepsyres.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Firmawati E, Setyopanoto I, Pangastuti HS. Mobile health application to support family caregivers in recurrent stroke prevention: scoping review. Open Access Maced J Med Sci. 2021;9(T5):142–51. doi: 10.3889/oamjms.2021.7859. [DOI] [Google Scholar]
- 9.Volpi SS, Biduski D, Bellei EA, Tefili D, McCleary L, Alves AL, et al. Using a mobile health app to improve patients’ adherence to hypertension treatment: a non-randomized clinical trial. PeerJ. 2021;9:e11491. doi: 10.7717/peerj.11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6. doi: 10.1097/xeb.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 11.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/m18-0850. [DOI] [PubMed] [Google Scholar]
- 12.Le Marne FA, Butler S, Beavis E, Gill D, Bye AM. EpApp: development and evaluation of a smartphone/tablet app for adolescents with epilepsy. J Clin Neurosci. 2018;50:214–20. doi: 10.1016/j.jocn.2018.01.065. [DOI] [PubMed] [Google Scholar]
- 13.Rajbhandari H, Joshi S, Malakar S, Paudel P, Jain P, Uppadaya K, et al. Epilepsy field workers, a smartphone application and telephone telemedicine: safe and effective epilepsy care in rural Nepal. Seizure. 2019;64:54–8. doi: 10.1016/j.seizure.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Simblett SK, Bruno E, Siddi S, Matcham F, Giuliano L, Lopez JH, et al. Patient perspectives on the acceptability of mHealth technology for remote measurement and management of epilepsy: a qualitative analysis. Epilepsy Behav. 2019;97:123–9. doi: 10.1016/j.yebeh.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 15.Si Y, Xiao X, Xia C, Guo J, Hao Q, Mo Q, et al. Optimising epilepsy management with a smartphone application: a randomised controlled trial. Med J Aust. 2020;212(6):258–62. doi: 10.5694/mja2.50520. [DOI] [PubMed] [Google Scholar]
- 16.Mirpuri P, Chandra PP, Samala R, Agarwal M, Doddamani R, Kaur K, et al. The development and efficacy of a mobile phone application to improve medication adherence for persons with epilepsy in limited resource settings: a preliminary study. Epilepsy Behav. 2021;116:107794. doi: 10.1016/j.yebeh.2021.107794. [DOI] [PubMed] [Google Scholar]
- 17.Choi SA, Lim K, Baek H, Yoo S, Cho A, Kim H, et al. Impact of mobile health application on data collection and self-management of epilepsy. Epilepsy Behav. 2021;119:107982. doi: 10.1016/j.yebeh.2021.107982. [DOI] [PubMed] [Google Scholar]
- 18.Yoo S, Lim K, Baek H, Jang SK, Hwang GY, Kim H, et al. Developing a mobile epilepsy management application integrated with an electronic health record for effective seizure management. Int J Med Inform. 2020;134:104051. doi: 10.1016/j.ijmedinf.2019.104051. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadzadeh N, Khenarinezhad S, Ghazanfarisavadkoohi E, Safari MS, Pahlevanynejad S. Evaluation of m-health applications use in epilepsy: a systematic review. Iran J Public Health. 2021;50(3):459–69. doi: 10.18502/ijph.v50i3.5586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldenholz DM, Moss R, Jost DA, Crone NE, Krauss G, Picard R, et al. Common data elements for epilepsy mobile health systems. Epilepsia. 2018;59(5):1020–6. doi: 10.1111/epi.14066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DiIorio C, Bamps Y, Walker ER, Escoffery C. Results of a research study evaluating WebEase, an online epilepsy self-management program. Epilepsy Behav. 2011;22(3):469–74. doi: 10.1016/j.yebeh.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 22.Bautista RE. Understanding the self-management skills of persons with epilepsy. Epilepsy Behav. 2017;69:7–11. doi: 10.1016/j.yebeh.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 23.Joshi R, Tripathi M, Gupta P, Gulati S, Gupta YK. Adverse effects & drug load of antiepileptic drugs in patients with epilepsy: monotherapy versus polytherapy. Indian J Med Res. 2017;145(3):317–26. doi: 10.4103/ijmr.ijmr_710_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Obiako OR, Sheikh TL, Kehinde JA, Iwuozo EU, Ekele N, Elonu CC, et al. Factors affecting epilepsy treatment outcomes in Nigeria. Acta Neurol Scand. 2014;130(6):360–7. doi: 10.1111/ane.12275. [DOI] [PubMed] [Google Scholar]
- 25.Fisher RS, Cross JH, D’Souza C, French JA, Haut SR, Higurashi N, et al. Instruction manual for the ILAE 2017 operational classification of seizure types. Epilepsia. 2017;58(4):531–42. doi: 10.1111/epi.13671. [DOI] [PubMed] [Google Scholar]
- 26.Chaka A, Awoke T, Yohannis Z, Ayano G, Tareke M, Abate A, et al. Determinants of depression among people with epilepsy in Central Ethiopia. Ann Gen Psychiatry. 2018;17:27. doi: 10.1186/s12991-018-0197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blixen C, Ogede D, Briggs F, Aebi ME, Burant C, Wilson B, et al. Correlates of stigma in people with epilepsy. J Clin Neurol. 2020;16(3):423–32. doi: 10.3988/jcn.2020.16.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huber R, Weber P. Is there a relationship between socioeconomic factors and prevalence, adherence and outcome in childhood epilepsy? A systematic scoping review. Eur J Paediatr Neurol. 2022;38:1–6. doi: 10.1016/j.ejpn.2022.01.021. [DOI] [PubMed] [Google Scholar]
- 29.Niriayo YL, Mamo A, Kassa TD, Asgedom SW, Atey TM, Gidey K, et al. Treatment outcome and associated factors among patients with epilepsy. Sci Rep. 2018;8(1):17354. doi: 10.1038/s41598-018-35906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boon P, Ferrao Santos S, Jansen AC, Lagae L, Legros B, Weckhuysen S. Recommendations for the treatment of epilepsy in adult and pediatric patients in Belgium: 2020 update. Acta Neurol Belg. 2021;121(1):241–57. doi: 10.1007/s13760-020-01488-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thompson ME, Goodwin R, Ojeda A, Morris L, Fairman AD. User preferences for the design of a mobile health system to support transition-age youth with epilepsy. J Pediatr Health Care. 2020;34(3):e28–36. doi: 10.1016/j.pedhc.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Sibernagl S, Lang F. Color of atlas pathophysiology. 3rd ed. New York (NY): Thieme Publishers; 2016. pp. 364–5. [Google Scholar]
- 33.Ikawati Z, Anurogo D. Tata Laksana Terapi Penyakit Sistem Syaraf Pusat [Management of therapy for central nervous system diseases] Yogyakarta, Indonesia: Bursa Ilmu; 2018. pp. 89–115. [Google Scholar]
- 34.Belayneh Z, Mekuriaw B. A systematic review and meta-analysis of anti-epileptic medication non-adherence among people with epilepsy in Ethiopia. Arch Public Health. 2020;78:23. doi: 10.1186/s13690-020-00405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ernawati I, Islamiyah WR, Sumarno How to improve clinical outcome of epileptic seizure control based on medication adherence? A literature review. Open Access Maced J Med Sci. 2018;6(6):1174–9. doi: 10.3889/oamjms.2018.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zena D, Tadesse A, Bekele N, Yaregal S, Sualih N, Worku E. Seizure control and its associated factors among epileptic patients at Neurology Clinic, University of Gondar hospital, Northwest Ethiopia. SAGE Open Med. 2022;10:20503121221100612. doi: 10.1177/20503121221100612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferrari CM, de Sousa RM, Castro LH. Factors associated with treatment non-adherence in patients with epilepsy in Brazil. Seizure. 2013;22(5):384–9. doi: 10.1016/j.seizure.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 38.Elsayed MA, El-Sayed NM, Badi S, Ahmed MH. Factors affecting adherence to antiepileptic medications among Sudanese individuals with epilepsy: a cross-sectional survey. J Family Med Prim Care. 2019;8(7):2312–7. doi: 10.4103/jfmpc.jfmpc_405_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shegog R, Bamps YA, Patel A, Kakacek J, Escoffery C, Johnson EK, et al. Managing epilepsy well: emerging e-tools for epilepsy self-management. Epilepsy Behav. 2013;29(1):133–40. doi: 10.1016/j.yebeh.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Pandey DK, Levy J, Serafini A, Habibi M, Song W, Shafer PO, et al. Self-management skills and behaviors, self-efficacy, and quality of life in people with epilepsy from underserved populations. Epilepsy Behav. 2019;98(Pt A):258–65. doi: 10.1016/j.yebeh.2019.07.042. [DOI] [PubMed] [Google Scholar]
- 41.Escoffery C, McGee R, Bidwell J, Sims C, Thropp EK, Frazier C, et al. A review of mobile apps for epilepsy self-management. Epilepsy Behav. 2018;81:62–9. doi: 10.1016/j.yebeh.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 42.Tang F, Zhu G, Jiao Z, Ma C, Chen N, Wang B. The effects of medication education and behavioral intervention on Chinese patients with epilepsy. Epilepsy Behav. 2014;37:157–64. doi: 10.1016/j.yebeh.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 43.McKellar K, Sillence E. Teenagers, sexual health information and the digital age. In: McKellar K, Sillence E, editors. Current research on sexual health and teenagers. London, UK: Academic Press; 2020. pp. 5–23. [Google Scholar]
- 44.Michaelis R, Tang V, Nevitt SJ, Wagner JL, Modi AC, LaFrance WC, et al. Cochrane systematic review and meta-analysis of the impact of psychological treatment on health-related quality of life in people with epilepsy: an update by the ILAE Psychology Task Force, highlighting methodological changes. Epileptic Disord. 2021;23(6):803–11. doi: 10.1684/epd.2021.1357. [DOI] [PubMed] [Google Scholar]
- 45.Falco-Walter JJ, Scheffer IE, Fisher RS. The new definition and classification of seizures and epilepsy. Epilepsy Res. 2018;139:73–9. doi: 10.1016/j.eplepsyres.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 46.Paschal AM, Hawley SR, St Romain T, Ablah E. Measures of adherence to epilepsy treatment: review of present practices and recommendations for future directions. Epilepsia. 2008;49(7):1115–22. doi: 10.1111/j.1528-1167.2008.01645.x. [DOI] [PubMed] [Google Scholar]
- 47.Beyene YB, Daba FB, Goro KK, Senbeta BS. Drug therapy problems and predicting factors among ambulatory epileptic patients in Jimma Medical Center, Southwest Ethiopia. PLoS One. 2022;17(4):e0267673. doi: 10.1371/journal.pone.0267673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.French JA, Pedley TA. Clinical practice. Initial management of epilepsy. N Engl J Med. 2008;359(2):166–76. doi: 10.1056/nejmcp0801738. [DOI] [PubMed] [Google Scholar]
- 49.Ayalew MB, Muche EA. Patient reported adverse events among epileptic patients taking antiepileptic drugs. SAGE Open Med. 2018;6:2050312118772471. doi: 10.1177/2050312118772471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perucca P, Carter J, Vahle V, Gilliam FG. Adverse antiepileptic drug effects: toward a clinically and neurobiologically relevant taxonomy. Neurology. 2009;72(14):1223–9. doi: 10.1212/01.wnl.0000345667.45642.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peasah SK, Fishman J, Ems D, Vu M, Huynh TT, Beaty S. Association between adverse events and discontinuation of antiepileptic drugs among drug-naive adults with epilepsy. Drugs Real World Outcomes. 2021;8(1):5–14. doi: 10.1007/s40801-020-00216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reis TM, Campos M, Nagai MM, Pereira L. Contributions of pharmacists in the treatment of epilepsy: a systematic review. Am J Pharm Benefits. 2016;8(3):e55–e60. [Google Scholar]
- 53.Aliasgharpour M, Dehgahn Nayeri N, Yadegary MA, Haghani H. Effects of an educational program on self-management in patients with epilepsy. Seizure. 2013;22(1):48–52. doi: 10.1016/j.seizure.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 54.Wagner JL, Modi AC, Johnson EK, Shegog R, Escoffery C, Bamps Y, et al. Self-management interventions in pediatric epilepsy: what is the level of evidence? Epilepsia. 2017;58(5):743–54. doi: 10.1111/epi.13711. [DOI] [PubMed] [Google Scholar]
- 55.Ozuna J, Kelly P, Towne A, Hixson J. Self-management in epilepsy care: untapped opportunities. Fed Pract. 2018;35(Suppl 3):S10–6. [PMC free article] [PubMed] [Google Scholar]
- 56.Singh S, Mishra VN, Rai A, Singh R, Chaurasia RN. Myths and superstition about epilepsy: a study from North India. J Neurosci Rural Pract. 2018;9(3):359–62. doi: 10.4103/jnrp.jnrp_63_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aljedaani B, Babar MA. Challenges with developing secure mobile health applications: systematic review. JMIR Mhealth Uhealth. 2021;9(6):e15654. doi: 10.2196/15654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zubaydi F, Saleh A, Aloul F, Sagahyroon A. Security of mobile health (mHealth) systems. Proceedings of 2015 IEEE 15th International Conference on Bioinformatics and Bioengineering (BIBE); 2015 Nov 2–4; Belgrade, Serbia. pp. 1–5. [DOI] [Google Scholar]
- 59.Lewis TL, Wyatt JC. mHealth and mobile medical Apps: a framework to assess risk and promote safer use. J Med Internet Res. 2014;16(9):e210. doi: 10.2196/jmir.3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moalong KM, Espiritu AI, Fernandez ML, Jamora RD. Treatment gaps and challenges in epilepsy care in the Philippines. Epilepsy Behav. 2021;115:107491. doi: 10.1016/j.yebeh.2020.107491. [DOI] [PubMed] [Google Scholar]
- 61.Abreu M, Carmo AS, Franco A, Parreira S, Vidal B, Costa M, et al. Mobile applications for epilepsy: where are we? where should we go? A systematic review. Signals. 2022;3(1):40–65. doi: 10.3390/signals3010005. [DOI] [Google Scholar]
- 62.Patel J, Feng W, Chen K, French JA, Rushton M, Hubbard S, et al. Use of an electronic seizure diary in a randomized, controlled trial of natalizumab in adult participants with drug-resistant focal epilepsy. Epilepsy Behav. 2021;118:107925. doi: 10.1016/j.yebeh.2021.107925. [DOI] [PubMed] [Google Scholar]