Abstract
Attention-deficit/hyperactivity disorder (ADHD) and chronic pain are prevalent and associated. We examined the prevalence and distribution of chronic pain in adolescents and young adults with ADHD using 9-years longitudinal data (from T1:2009–2011 to T3:2018–2019) with three time points from a clinical health survey compared to two age-matched reference population-based samples. Mixed-effect logistic regression and binary linear regression were used to estimate the probability for chronic and multisite pain at each time point and to compare the prevalence of chronic pain with the reference populations. The prevalence of chronic and multisite pain was high in those with ADHD, especially in female young adults, with highly prevalent chronic pain at 9 years of follow-up (75.9%) compared to 45.7% in females in the reference population. The probability of having pain was only statistically significant for chronic pain in males at 3 years of follow-up (41.9%, p = 0.021). Those with ADHD were at higher risk of reporting single-site and multisite pain compared to the general population at all measurement points. Longitudinal studies should be tailored to further understand the complex sex differences of comorbid chronic pain and ADHD in adolescents, exploring predictive factors of pain assessing long-term associations with bodyweight, psychiatric comorbidities, and possible mechanisms of stimulant use effects on pain.
Keywords: ADHD, Adolescents, Chronic pain, Multisite pain, Single-site pain, HUNT
Introduction
Attention-deficit/hyperactivity disorder (ADHD) typically emerges in childhood with an average global prevalence of 5%, often with difficulties continuing into adulthood [1], frequently showing high concurrent comorbidity with other neurodevelopmental and psychiatric disorders [2]. ADHD diagnosis differs in level of core symptoms (inattentive or hyperactive presentation, or both), impairments, and comorbidities [3]. Comorbidities are significantly associated with somatic complaints such as pain [2, 4, 5], and persistent impairment in adult life [6]. Chronic pain, which typically is defined as pain lasting more than 3 months [7], is commonly reported by adolescents, with a wide variability in the reported prevalence estimates, varying according to age, sex (more prevalent in females), and country of origin [8, 9]. Its recurrent nature indicates that having chronic pain in adolescence is highly predictive of chronic pain in adulthood [10]. A recent systematic review examining prognostic factors of adolescent chronic pain found that chronic pain persisted in more than 50% of the adolescents at 9-year follow-up, with persistence associated with pain in seven out of nine single pain sites, most frequently occurring in the lower back, neck, and knee [11]. Female sex was commonly associated with pain at follow-up, with pain across different pain sites such as headache, pain in the upper extremities, lower extremities, chest, and back [11]. In adults, the number of pain sites is associated with poorer prognosis compared to single-site pain [12]; however, over time, studies of adult populations have shown relatively stable trajectories of pain [13].
In community prevalence studies of adolescents, ADHD was found to be twice or three times more common among males than females [1], suggesting an under-recognition of ADHD in females [14]. The clinical presentation, pharmacological treatments, and course of ADHD have been extensively characterized; however, without addressing the broader, long-term clinical needs [15]. For example, chronic pain shares common mechanisms and concerns with ADHD; pain has well-established effects on attention and vice versa [5, 16]. However, there is little detailed knowledge regarding somatic diseases in those with ADHD from a longitudinal perspective, and the extent to which ADHD alone is related to somatic complaints such as chronic pain.
Somatic comorbidity addressing the prospective course of chronic pain from adolescents to young adulthood in ADHD has received less attention in the research literature. This study aimed to (1) report the prevalence of chronic pain in adolescents and young adults with ADHD using longitudinal data from a clinical health survey and (2) compare the prevalence of chronic pain in those with ADHD using two age-matched reference population samples.
Methods
Sample and procedures
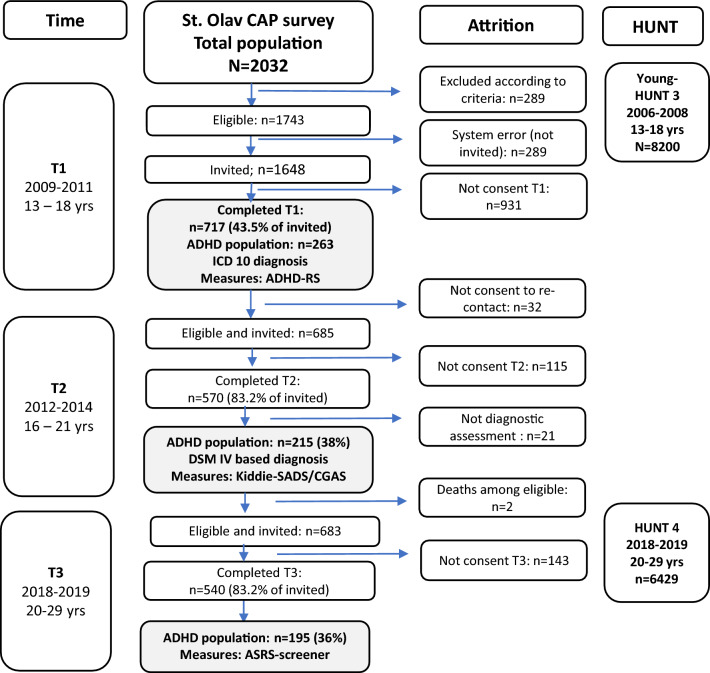
Data were obtained from a health survey in the Department of Children and Youth Division of Mental Health Care at St. Olav’s University Hospital, Trondheim University Hospital, Norway (the CAP study), along with a large Norwegian cohort of adolescents and young adults in the Norwegian county of Trøndelag (The Young-HUNT and HUNT surveys). Figure 1 presents the participant flow in these studies.
Fig. 1.
Flowchart of inclusion and attrition
Of the total of 717 participants in the CAP study at baseline (T1), n = 263 had ADHD diagnosis, and were included in this study. The mean (SD) age was 15.7 (1.65) years, ranging from 13.0 to 20.5, and 45% were females (n = 106). Adolescents enrolled at the CAP clinic received verbal and written invitations during their first visit after the project started. For participants younger than 16 years of age, parental consent was obtained; participants aged ≥ 16 years provided written informed consent to participate. From the CAP study, only those with ADHD were included.
Data from the reference population-based Young-HUNT3 study (the adolescent part of the HUNT [the Trøndelag Health Study] were collected from the third wave of the Young-HUNT study and the fourth wave of the HUNT study (HUNT4), which were conducted from 2006 to 2008 and 2018–2019, respectively, and corresponded to times T1 and T3 in the CAP study. Of the 10,464 adolescents aged 13–19 years in Trøndelag County of Norway who were invited to participate, 8200 (78.4%) participated [17]. The Young-HUNT studies aimed to capture rapidly changing health statuses, behaviors, and functions that differed from those of adults; data collection included self-reported questionnaires, and clinical measurements [18]. To ensure maximum comparability, health data in the HUNT studies were collected comparably using interviews, identical self-administrated questionnaires, including screening for ADHD problems (adolescent’s school functioning in Young-HUNT3 [19] and Adult ADHD self-report scale in HUNT4 [20]), and clinical examinations, which corresponded to the three waves of the CAP study. During the school day, students completed the questionnaires printed with a unique barcode without names or other identifiers; questionnaires were sealed in a blank envelope by the student after completion. We included subjects from the HUNT4-study from the same age group (20–29 years old) as participants in CAP-T3.
Measures
Clinical medical and psychiatric diagnostic assessments followed standardized diagnostic processes and routine assessments according to the ICD-10 [21] and the Norwegian national guidelines for ADHD [22, 23]. The procedures included information from patients and their parents and teachers regarding developmental history, somatic health status, and school functioning [24, 25]. Assessments of emotional and behavioral problems were obtained from the Achenbach System of Empirically Based Assessment (ASEBA) checklists [26] and ADHD symptoms from the ADHD Rating Scale-IV parent report (ADHD-RS-IV) [27].
Chronic pain was defined as having pain in at least one of the musculoskeletal locations occurring at least once a week in the last 3 months, and multisite pain was defined as having chronic pain in three or more locations [7, 28]. The self-reported pain questionnaires in the CAP-T1 and T3 surveys included questions regarding somatic pain symptoms that had been experienced during the last 3 months and were not related to any known disease or injury [29]. Questions from Mikkelsson et al. were used to determine the duration and location of pain, which was reported to have good test–retest reliability in detecting those who had pains at least once a week (Cohen’s kappa was 0.90). Observed agreement between pain questionnaire and interview technique was 86% and kappa was 0.67 [29]. The adolescents were asked to specify pain in different locations such as headache, abdomen, chest, upper or lower back/buttocks/limbs with five response alternatives including the frequency of experiencing pain, specified as “never/seldom”, “once a month”, “once a week”, “more than once a week” or “almost every day” [29, 30]. Assessment of pain locations was assisted by a pain mannequin and was considered appropriate to be completed unassisted by children older than 8 years of age [31]. The main outcome variable (chronic pain) was analyzed as categorical, with categories of 0 (no pain) and 1 (pain).
Statistical analyses
For those with ADHD in the CAP study, we used mixed-effect logistic regression with dichotomized chronic and multisite pain, one at a time, as dependent variables, time point (T1, T2, and T3) as a categorical covariate, and participant as a random effect. Participants without data at all time points were also included in the mixed-effect logistic regression model, as such results are approximately unbiased when data are missing at random [32]. We have presented the estimated prevalence rates (probabilities) calculated from the estimated odds from these analyses as p = odds/(odds + 1).
To compare the prevalence of chronic pain in adolescents with ADHD in CAP T1 and young adults in T3 with those in Young-HUNT3 and HUNT4, we performed binary linear regression analyses with pain as dependent variable and CAP versus HUNT, age, and sex as covariates. This analysis was performed separately for each of the site-specific pain variables, chronic pain, and multisite pain, and with separate analyses for males and females. We have reported risk difference (RD) with 95% confidence intervals (CI). The level of significance was set to p < 0.05. All data were analyzed using Stata 17 for Windows (Stata Corporation, USA).
Ethics
Written informed consent from adolescents and their parents was obtained prior to inclusion in both the CAP study and the Young-HUNT study. Study approval was granted by the Regional Committee for Medical and Health Research Ethics (reference 4.2008.1393 number for the CAP study, 4.2006.250 for the Young-HUNT3 study, 2011//2061/REK-Midt and for the present study).
Results
Sample characteristics and chronic pain prevalence
Table 1 shows the characteristics of both populations. From the Young-HUNT3 study (N = 8312), the mean age was 15.9 (1.75) years, ranging from 12.7 to 20.9, and 50.3% (n = 4181) were females. The mean number of pain sites was higher in CAP participants as compared to the general population. In the CAP study, the prevalence of multisite pain in females had decreased at 9-year follow-up but had increased in males. In the general population, the prevalence of multisite pain in both sexes had increased from Young-HUNT3 to HUNT4 but was still lower than that observed for in CAP. Additional descriptive statistics are published elsewhere [2].
Table 1.
Sample characteristics
| T1 (CAP) n = 263 (2009–2011) |
T2 (CAP) n = 215 (2012–2014) |
T3 (CAP) n = 195 (2018–2019) |
Young-HUNT3 n = 8200 (2006–2008) |
HUNT4 n = 6428 (2018–2019) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Females | Males | Females | Males | Females | Males | Females | Males | Females | Males | |
| Sex % (n) | 40.3 (106/263) | 59.7 (157/263) | 41.4 (89/215) | 58.6 (126/215) | 45.6 (89/195) | 54.4 (106/195) | 50.3 (4128/8200) | 59.7 (4072/8200) | 56.5 (3633/6428) | 43.5 (2795/6428) |
| Age (SD) | 15.8 (1.89) | 15.2 (1.50) | 18.9 (1.87) | 18.1 (1.48) | 24.6 (1.82) | 24.2 (1.45) | 15.9 (1.76) | 15.9 (1.72) | 24.8 (3.01) | 24.7 (3.01) |
| Chronic pain % (n) | 81.0 (81/100) | 56.6 (82/145) | 78.8 (67/85) | 44.0 (51/116) | 75.9 (66/87) | 51.9 (54/104) | 51.1 (2000/3195) | 31.4 (1191/3778) | 45.7 (1510/3303) | 25.0 (642/2565) |
| Multisite pain % (n) | 49.0 (49/100) | 19.3 (28/145) | 51.3 (159) | 16.5 (389) | 42.5 (37/87) | 23.1 (23/104) | 20.1 (781/3883) | 9.1 (343/3757) | 26.3 (632/2408) | 16.1 (224/1389) |
| Sum pain sites mean (SD) | 2.8 (2.3) | 1.3 (1.7) | 3.4 (3.2) | 1.2 (2.0) | 3.2 (2.6) | 1.6 (2.6) | 1.3 (1.7) | 0.7 (1.3) | 1.9 (1.8) | 1.2 (1.8) |
Those with ADHD included HUNT4: those younger than 30 years included
CAP child and adolescent psychiatry (the CAP study)
The course of chronic and multisite pain in those with ADHD
Table 2 shows the estimated probability of having chronic pain and multisite pain at each time point in those with ADHD in the CAP study. The probability of having chronic pain at baseline for the total sample was 74.3% with chronic pain decreasing at T2 (62.3%, p = 0.027), and increasing at T3 (66.4%, p = 0.14). For multisite pain at baseline, the probability was 22.9%, with decreasing probability at T3 (21.5%, p = 0.76).
Table 2.
Estimated chronic pain prevalence in those with ADHD
| Total | Females | Males | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Probability (%) | 95% CI (%) | p value | Probability (%) | 95% CI (%) | p value | Probability (%) | 95% CI (%) | p value | |
| Chronic pain | |||||||||
| Baseline T1 2009–2011 | 74.3% | 65.4–81.6 | 90.4% | 78.9–96.0 | 59.2% | 48.0–69.2 | |||
| Follow-up T2 2012–2014 | 62.3% | 51.9–71.7 | 0.027 | 87.9% | 74.7–94.7 | 0.57 | 41.9% | 30.7–53.9 | 0.021 |
| Follow-up T3 2018–2019 | 66.4% | 56.0–75.4 | 0.14 | 85.4% | 71.4–93.2 | 0.29 | 50.5% | 38.1–62.9 | 0.26 |
| Multisite pain | |||||||||
| Baseline T1 2009–2011 | 22.9% | 15.9–31.8 | 48.9% | 36.2–61.7 | 8.9% | 4.0–18.6 | |||
| Follow-up T2 2012–2014 | 25.4% | 17.4–35.6 | 0.60 | 55.3% | 41.3–68.5 | 0.46 | 8.8% | 3.7–19.4 | 0.96 |
| Follow-up T3 2018–2019 | 21.5% | 14.2–31.3 | 0.76 | 39.4% | 26.8–53.4 | 0.27 | 11.6% | 5.2–23.7 | 0.48 |
The level of significance was set to p < 0.05 (in bold)
Based on mixed-effect logistic regression with pain as dependent variable and time as categorical covariate. p values for change from baseline
For females, probability for chronic pain at baseline was 90.4% but decreased at T3 (85.4%, p = 0.27). For multisite pain, the baseline probability was 48.9% with a decrease at T3 (39.4%, p = 0.76).
For males, the probability of chronic pain at baseline was 59.2%, but decreased significantly at T2 (41.9%, p = 0.021), and increased at T3 (50.5%, p = 0.26). For multisite pain, the probability was 8.9% (T1) and 11.6%, p = 0.48 (T3), respectively.
Pain sites prevalence in those with ADHD compared to the general population
Table 3 presents the estimated prevalence of chronic pain separately for each sex at each time point in CAP and the general population. The frequency of chronic pain was higher in adolescents and young adults with ADHD than in those in the reference populations, at all measurement points, but decreased with time. Table 3 presents risk differences for pain between adolescents with ADHD in CAP-T1 compared to those in Young-HUNT3, estimated from the binary linear regression and adjusted for age and sex. The risk differences were significantly higher in those with ADHD considering headache (RD = 12.2%, CI 0.07–0.18), and pain in various locations, with highest difference in neck (RD = 16.9%, CI 0.11–0.23), lower back (RD = 13.7%, CI 0.08–0.19), upper back (RD = 12.1%, CI 7.0–17.1), stomach (RD = 13.5%, CI 0.09–0.18), and other sites (RD = 26.0%, CI 0.20–0.32), as well as chronic pain (RD = 25.1%, CI 0.20–0.31) and multisite pain (RD = 17.1%, CI 0.12–0.23), compared to the general population.
Table 3.
Pain prevalence in CAP-T1 and Young-HUNT3
| Pain locations | T1 (n = 263) | YH3 (n = 8312) | Difference % 95% CI | p value |
|---|---|---|---|---|
| Head | 33.3% (85/255) | 22.4% (1896/8033) | 12.2% [6.7–17.8%] | < 0.001 |
| Neck | 33.9% (86/254) | 17.8% (1418/7969) | 16.9% [11.3–22.5%] | < 0.001 |
| Upper back | 21.5% (54/251) | 10.0% (802/7994) | 12.1% [7.0–17.1%] | < 0.001 |
| Lower back | 27.8% (72/255) | 14.6% (1172/8016) | 13.7% [8.4–19.0%] | < 0.001 |
| Chest | 10.6% (27/254) | 4.4% (352/7994) | 6.2% [2.5–9.9%] | 0.001 |
| Gastrointestinal | 25.1% (64/255) | 11.6% (923/985) | 13.5% [8.5–18.5%] | < 0.001 |
| Left arm | 7.4% (19/256) | 2.7% (212/7992) | 4.7% [1.5–7.9%] | 0.004 |
| Right arm | 6.3% (16/255) | 3.1% (248/7988) | 2.9% [0.0–5.9%] | 0.049 |
| Left leg | 14.3% (37/258) | 8.0% (643/8002) | 5.7% [1.5–9.9%] | 0.008 |
| Right leg | 15.6% (40/257) | 8.9% (715/8016) | − 1.4% [− 1.7% to − 1.0] | < 0.001 |
| Other pain | 33.2% (83/250) | 7.3% (543/7453) | 26.0% [20.2–31.9%] | < 0.001 |
| Chronic pain | 66.5% (163/245) | 44.5% (3401/7640) | 25.1% [19.5–30.8%] | < 0.001 |
| Multisite pain | 31.4% (77/245) | 14.7% (1124/7640) | 17.1% [11.6–22.7%] | < 0.001 |
| Females | 40.3% (106/263) | 50.3% (4181/8312) | ||
| Head | 49.5% (52/105) | 30.4% (1237/4066) | 19.3% [9.8–28.9%] | < 0.001 |
| Neck | 50.5% (53/105) | 23.0% (927/4039) | 28.0% [18.6–37.3%] | < 0.001 |
| Upper back | 25.7% (26/101) | 12.8% (519/4047) | 12.9% [4.4–21.4%] | 0.003 |
| Lower back | 38.1% (40/105) | 17.7% (719/4061) | 20.2% [11.2–29.3%] | < 0.001 |
| Chest | 16.0% (17/106) | 5.2% (211/4050) | 10.8% [3.8–17.8%] | 0.002 |
| Gastrointestinal | 40.6% (43/106) | 17.5% (709/4053) | 23.1% [13.9–32.4%] | < 0.001 |
| Left arm | 7.6% (8/106) | 2.8% (115/4059) | 4.7% [− 0.3% to 9.8%] | 0.067 |
| Right arm | 6.6% (7/106) | 3.3% (133/4055) | 3.1% [− 1.5% to 7.7%] | 0.19 |
| Left leg | 18.9% (20/106) | 9.2% (374/4055) | 9.3% [2.0–16.7%] | 0.013 |
| Right leg | 22.9% (24/105) | 10.0% (405/4060) | 12.9% [4.8–21.0%] | 0.002 |
| Other pain | 40.2% (42/102) | 8.7% (325/3743) | 31.5% [22.0–41.1%] | < 0.001 |
| Chronic pain | 81.0% (81/100) | 54.6% (2120/3883) | 27.0% [19.4–34.5%] | < 0.001 |
| Multisite pain | 49.0% (49/100) | 20.1% (781/3883) | 29.2% [19.5–38.8%] | < 0.001 |
| Males | 59.7% (157/263) | 49.7% (4131/8312) | ||
| Head | 22.0% (33/150) | 14.1% (559/3967) | 8.0% [1.3–14.8%] | 0.019 |
| Neck | 22.2% (33/149) | 12.5% (491/3930) | 10.1% [3.4–16.9%] | 0.003 |
| Upper back | 18.7% (28/150) | 7.2% (283/3947) | 11.5% [5.2–17.8%] | < 0.001 |
| Lower back | 20.7% (31/150) | 11.5% (453/3955) | 9.7% [3.4–16.1%] | 0.003 |
| Chest | 6.8% (10/148) | 13.6% (41/3994) | 3.4% [− 0.7% to 7.6%] | 0.103 |
| Gastrointestinal | 14.1% (21/149) | 5.4% (214/3932) | 8.3% [2.7–13.9%] | 0.004 |
| Left arm | 7.3% (11/150) | 2.5% (97/3933) | 4.6% [0.4–8.7%] | 0.031 |
| Right arm | 6.0% (9/149) | 2.9% (115/3933) | 2.8% [− 1.0% to 6.7%] | 0.15 |
| *Left leg | 11.2% (17/152) | 6.8% (269/3949) | 4.4% [− 0.7% to 9.4%] | 0.091 |
| Right leg | 10.5% (16/152) | 7.8% (310/3956) | 1.7% [− 3.1% to 6.6%] | 0.48 |
| Other pain | 28.4% (31/148) | 5.9% (218/3710) | 22.4% [15.1–29.7%] | < 0.001 |
| Chronic pain | 56.6% (82/145) | 34.1% (1282/3757) | 22.3% [14.1–30.6%] | < 0.001 |
| Multisite pain | 19.3% (28/145) | 9.1% (343/3757) | 10.1% [3.6–16.7%] | 0.002 |
The level of significance was set to p < 0.05 (in bold)
Confidence intervals (CI) and p values from binary linear regression, adjusted for age and sex in total sample
ADHD attention-deficit hyperactivity disorder, CAP child and adolescent psychiatry, T1 baseline (2009–2011), YH3 the Nord-Trøndelag Health Study—Young-HUNT3 (2006–2008)
*Unadjusted for age. Computation did not converge when adjusting for age
Table 4 presents results for those with ADHD aged 20–29 years in CAP-T3 compared to those in HUNT4 in the same age range. The risk differences were significantly higher in those with ADHD, considering pain in the shoulders (RD = 18.1%, CI 12.0–24.3), neck (RD = 13.4%, CI 0.08–0.19), lower back (RD = 13.9%, CI 0.08–0.20), knee (RD = 13.4%, CI 0.08–0.19), and ankle (RD = 12.1%, CI 0.07–0.17) as well as bilateral pain (RD = 53.6%, CI 0.43–0.64) and multisite pain (RD = 11.3%, CI 0.05–0.18), but not chronic pain, compared to the general population.
Table 4.
Pain prevalence in CAP-T3 and HUNT4
| T3 (n = 195) | HUNT4 (n = 6428) | Difference % 95% CI | p value | |
|---|---|---|---|---|
| Head | 51.8% (99/191) | 50.8% (1927/3797) | 5.7% [− 1.3% to 12.7%] | 0.11 |
| Jaw | 8.2% (16/195) | 2.1% (133/6428) | 6.0% [2.4–9.7%] | 0.001 |
| Neck | 23.6% (46/195) | 10.8% (695/6428) | 13.4% [7.7–19.1%] | < 0.001 |
| Upper back | 15.4% (30/195) | 6.6% (422/6428) | 9.2% [4.2–14.1%] | < 0.001 |
| Lower back | 24.1% (47/195) | 10.3% (663/6428) | 13.9% [8.1–19.7%] | < 0.001 |
| Chest | 7.7% (15/195) | 1.7% (111/6428) | 5.9% [2.3–9.6%] | 0.001 |
| Shoulders | 27.2% (53/195) | 9.4% (603/6428) | 18.1% [12.0–24.3%] | < 0.001 |
| Elbow | 2.6% (5/195) | 1.8% (117/6428) | 0.8% [− 1.4% to 3.1%] | 0.48 |
| Hand | 11.8% (23/195) | 4.9% (314/6428) | 6.9% [2.6–11.3%] | 0.002 |
| *Hip | 11.3% (22/195) | 4.9% (312/6428) | 6.6% [2.2–11.1%] | 0.004 |
| Thigh | 5.6% (11/195) | 1.2% (80/6428) | 4.4% [1.2–7.5%] | 0.007 |
| Knee | 19.5% (38/195) | 6.4% (410/6428) | 13.4% [7.9–18.9%] | < 0.001 |
| Leg | 5.1% (10/195) | 2.3% (149/6428) | 2.9% [− 0.1% to 5.9%] | 0.060 |
| Ankle | 15.9% (31/195) | 4.1% (263/6428) | 12.1% [7.0–17.2%] | < 0.001 |
| Bilateral pain | 67.6% (50/74) | 15.2% (978/6428) | 53.6% [43.4–63.7%] | < 0.001 |
| Chronic pain | 62.8% (120/191) | 62.8% (2383/3797) | 4.1% [− 2.7–10.9%] | 0.24 |
| Multisite pain | 31.9% (61/191) | 22.6% (857/3797) | 11.3% [4.7–17.8%] | 0.001 |
| Females | 40.3% (106/263) | 56.5% (3633/6428) | ||
| Head | 66%.7 (58/87) | 59.3% (1429/2408) | 7.3% [− 2.7% to 17.5%] | 0.15 |
| Jaw | 49.5% (52/105) | 3.1% (111/3633) | 9.3% [2.5–16.2%] | 0.008 |
| Neck | 33.7% (30/89) | 14.9% (541/3633) | 18.9% [9.0–28.8%] | < 0.001 |
| Upper back | 20.2% (18/89) | 8.4% (305/3633) | 11.9% [3.5–20.3%] | 0.006 |
| Lower back | 34.8% (31/89) | 12.8% (464/3633) | 22.1% [12.1–32.0%] | < 0.001 |
| Chest | 11.2% (10/89) | 2.3% (83/3633) | 9.0% [2.4–15.5%] | 0.008 |
| Shoulders | 37.1% (33/89) | 12.2% (443/3633) | 24.9% [14.8–35.0%] | < 0.001 |
| Elbow | 2.3% (2/89) | 1.8% (65/3633) | 0.4% [− 2.6% to 3.5%] | 0.79 |
| Hand | 18.0% (16/89) | 6.3% (228/3633) | 11.7% [3.7–19.7%] | 0.004 |
| Hip | 19.1% (17/89) | 7.2% (260/43633) | 12.2% [3.9–20.5%] | 0.004 |
| Thigh | 7.9% (7/89) | 1.7% (60/3633) | 6.2% [0.6–11.8%] | 0.030 |
| Knee | 23.6% (21/89) | 7.9% (287/3633) | 15.7% [6.8–24.5%] | 0.001 |
| Leg | 6.7% (6/89) | 3.0% (108/3633) | 3.8% [− 1.5% to 9.0%] | 0.16 |
| Ankle | 19.1% (17/89) | 5.4% (195/3633) | 13.7% [5.5–21.9%] | 0.001 |
| Bilateral pain | 82.9% (34/41) | 19.8% (719/3633) | 62.9% [51.2–74.6%] | < 0.001 |
| Chronic pain | 75.9% (33/87) | 69.6% (1677/2408) | 6.2% [− 2.9% to 15.4%] | 0.18 |
| Multisite pain | 42.5% (37/87) | 26.3% (633/2408) | 16.4% [5.8–26.8%] | 0.002 |
| Males | 54.4% (106/195) | 43.5% (2795/6428) | ||
| Head | 39.4% (41/104) | 35.6% (498/1389) | 4.4% [− 5.4% to 14.1%] | 0.38 |
| Jaw | 4.7% (5/106) | 2.1% (22/27957) | 3.9% [− 0.1% to 8.0%] | 0.056 |
| Neck | 15.1% (16/106) | 5.5% (154/2795) | 10.0% [3.1–16.9%] | 0.005 |
| Upper back | 11.3% (12/106) | 4.2% (117/2795) | 7.4% [1.3–13.5%] | 0.018 |
| Lower back | 15.1% (16/106) | 7.1% (199/2795) | 8.2% [1.3–15.0%] | 0.020 |
| Chest | 4.7% (5/106) | 1.0% (28/2795) | 3.8% [− 0.3% to 7.9%] | 0.066 |
| Shoulders | 18.9% (20/106) | 5.7% (160/2795) | 13.3% [5.0–20.1%] | 0.001 |
| Elbow | 2.8% (3/106) | 1.9% (52/2795) | 1.2% [− 2.1% to 4.5%] | 0.47 |
| Hand | 6.6% (7/106) | 23.1% (86/2795) | 3.9% [− 1.0% to 8.8%] | 0.12 |
| *Hip | 7.2% (5/106) | 1.9% (52/2795) | 3.0% [− 1.0% to 7.0%] | 0.15 |
| Thigh | 3.8% (4/106) | 0.7% (20/2795) | 3.1% [ −0.5% to 6.7%] | 0.096 |
| Knee | 16.0% (17/106) | 4.4% (123/2795) | 11.8% [4.8% to 18.8%] | 0.001 |
| Leg | 3.8% (4/106) | 1.5% (41/2795) | 2.3% [− 1.3% to 6.0%] | 0.21 |
| Ankle | 13.2% (14/106) | 2.4% (68/2795) | 10.9% [4.4% to 17.3%] | 0.001 |
| Bilateral pain | 48.5% (16/33) | 9.3% (259/2795) | 39.6% [22.5% to 56.7%] | < 0.001 |
| Chronic pain | 51.9% (54/104) | 50.8% (706/1389) | 2.0% [− 8.0% to 12.0%] | 0.69 |
| Multisite pain | 23.1% (24/104) | 16.1% (224/1389) | 7.9% [− 0.4% to 16.2%] | 0.063 |
The level of significance was set to p < 0.05 (in bold)
Confidence intervals (CI) and p values from binary linear regression, adjusted for age and sex in total sample. Only those younger than 30 years included
ADHD attention-deficit hyperactivity disorder, CAP child and adolescent psychiatry, T3 nine -year follow-up (2018–2019), HUNT4 the Nord-Trøndelag Health Study 4 (2018–2019)
*Unadjusted for age. Computation did not converge when adjusting for age
In summary, the results indicated significant higher risk for single-site pain in specified locations and multisite pain in those with ADHD, with the highest risk differences in females, as compared to those in the Young-HUNT3 and HUNT4 populations.
Discussion
This study examined the prevalence, course, and distribution of chronic pain in adolescents with ADHD within a clinical population, along with two age-matched reference population samples. Chronic pain in specified locations and multisite pain were highly prevalent among all adolescents, particularly in females and those with ADHD.
The prospective course of chronic and multisite pain in those with ADHD
We found that those with ADHD seemed significantly more prone to experiencing single-site and multisite pain at each time of assessment, with females to a greater extent, corresponding well to other studies [28, 33]. ADHD and chronic pain share similar overlapping cognitive and behavioral processes [5, 33, 34]. Neuroinflammation is considered at the origin of ADHD and pain comorbidity [5], but it is unclear how neuroinflammation is related to sex differences in pain prevalence in children. Accordingly, the prevalence of pain in those with ADHD is complex and multifactorial and includes risk factors such as genetics and intergenerational recurrence of ADHD or chronic pain [19, 35]. The prospective decrease in pain prevalence in ADHD patients may be attributable to symptoms in chronic pain states that are episodic and fluctuates in narrow time scale [13, 36]. However, it is evident that previous chronic pain in childhood or adolescents may have strong predictive power for pain later in life [10, 11].
Difference in pain prevalence
Pain prevalence, including single pain sites, in those with ADHD was significantly higher at all time points as compared to the adolescents and young adults in the general population, and was most prevalent in females.
We found significant risk differences in adolescents with ADHD compared to the general population in reporting single-site pain, particularly in the head, neck, back, abdomen as well as chronic pain and multisite pain. This effect also applied to young adults with ADHD, especially those reporting pain in the neck, back, and lower limbs as well as multisite pain, but not those reporting chronic pain. According to previous studies, experiencing single-site pain does not have substantial impact on everyday functioning; however, the impact increases significantly with increasing numbers of pain sites [11, 12, 28]. In HUNT4, more than half of those with chronic pain reported single-site pain, while 12% of those with chronic pain in CAP-T3 reported single-site pain. Thus, there is a clear need to further understand the clinical relevance of comorbid chronic pain and ADHD in adolescents. Relevant avenues for further research must address the complex sex differences as risk/protective factors concerning the high prevalence of ADHD in males and chronic pain in females [37, 37], also assessing long-term associations with bodyweight, psychiatric comorbidities, and possible mechanisms of stimulant use effects on pain, which were limitations in this study.
The prospective design of this study, acceptable participation rates, and the use of standardized and comparable questions to collect pain data ensured the comparability of results across different studies. We focused on somatic comorbidity in ADHD, which has received less attention in the research literature. In clinical practice, such inattention can lead to misdiagnosis or incorrect treatment, with potentially serious consequences if medical conditions causing the chronic pain are overlooked [39]. However, some limitations need to be considered. The ADHD diagnosis at baseline was based on clinical ICD-10 diagnoses and DSM-IV at T2. Because the criteria for ADHD according to ICD-10 are stricter than the criteria for ADHD in DSM-IV, this may have affected prevalence rates [2]. Even though comorbid psychiatric diagnoses are prevalent in adolescent ADHD, we excluded this perspective. Moreover, the comparison of a clinical population to general reference populations may have produced bias in that the reference populations may have experienced less severe problems, for example more limited impact of pain on functioning as compared to the clinical samples [40]. All samples included in this study are ethnically homogeneous, which limit the generalizability to people of non-European ancestry [18], we relied on self-reporting of pain symptoms rather than clinical findings, suggesting that the complex nature of chronic pain might represent a limitation of this study.
Conclusion
This longitudinal study of chronic pain in a clinical sample of adolescents and young adults with ADHD compared to the general population found that chronic pain in specified locations as well as multisite pain, was highly prevalent among all adolescents, particularly in females and those with ADHD. To explore the nature of these findings further, we suggest examining the complex sex differences of comorbid chronic pain and ADHD in adolescents in a long-term perspective.
Acknowledgements
Open Access funding is provided by NTNU Norwegian University of Science and Technology. The Health Survey in Department of Children and Youth, Division of Mental Health Care, St. Olavs hospital, Trondheim University Hospital, Norway (St. Olav CAP Survey), is a product of professional and financial collaboration between St. Olavs hospital—Trondheim University Hospital, and the Regional Centre for Child and Youth Mental Health and Child Welfare, Department of Mental Health, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU). The Trøndelag Health Study (HUNT) is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU), Trøndelag County Council, Central Norway Regional Health Authority, and the Norwegian Institute of Public Health.
Author contributions
IM, JS, and SL designed the study, and IM drafted the first manuscript. SL and IM performed the statistical analyses. JS, SL, PHT, TN, and LRK provided quality assessment and guidance. Each version of the draft was circulated to all authors for comments and endorsement of the consensus, and all authors contributed to drafting, interpretation, and critically revising the paper. All authors have read and approved the manuscript to be published and agreed to be accountable for all aspects of the work.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This work is supported by the Regional Centre for Child and Youth Mental Health and Child Welfare (RKBU), Department of Mental Health, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU). IM is supported by a postdoctoral grant from The Regional academic community for autism, ADHD and Tourette’s syndrome (RFM). RFM had no role in the design of the study and collection, analysis, interpretation of data or writing the manuscript.
Data availability
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was carried out in accordance with the code of ethics of the Declaration of Helsinki, and all procedures and consent forms were reviewed and approved by the Regional Committee for Medicine and Health Research Ethics in Mid-Norway (ref.: 2011//2061).
Informed consent
Participation in the CAP study and the Young-HUNT and HUNT studies was voluntary. All participants gave an informed written consent to participate. For adolescents under 16 years old, parents had to consent. According to study procedures, written informed consent was obtained from adolescents and parents participating at T1 and T2, and from the young adults at T3. All parents received oral and written information. Consent was implicitly given by anonymously responding to the questionnaires and returning the envelope at the end of the course. Personal information, names or any other identifying information were not collected, and confidentiality and anonymity were carefully ensured.
Consent for publication
Not applicable.
References
- 1.Sayal K, Prasad V, Daley D, Ford T, Coghill D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatr. 2018;5(2):175–186. doi: 10.1016/S2215-0366(17)30167-0. [DOI] [PubMed] [Google Scholar]
- 2.Gårdvik KS, Rygg M, Torgersen T, Lydersen S, Indredavik MS. Psychiatric morbidity, somatic comorbidity and substance use in an adolescent psychiatric population at 3-year follow-up. Eur Child Adolesc Psychiatr. 2021;30(7):1095–1112. doi: 10.1007/s00787-020-01602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387(10024):1240–1250. doi: 10.1016/S0140-6736(15)00238-X. [DOI] [PubMed] [Google Scholar]
- 4.Holmberg K, Hjern A. Health complaints in children with attention-deficit/hyperactivity disorder. Acta paediatrica (Oslo, Norway: 1992) 2006;95(6):664–670. doi: 10.1080/08035250600717121. [DOI] [PubMed] [Google Scholar]
- 5.Kerekes N, Sanchéz-Pérez AM, Landry M. Neuroinflammation as a possible link between attention-deficit/hyperactivity disorder (ADHD) and pain. Med Hypotheses. 2021;157:110717. doi: 10.1016/j.mehy.2021.110717. [DOI] [PubMed] [Google Scholar]
- 6.Sonuga-Barke EJS, Becker SP, Bölte S, Castellanos FX, Franke B, Newcorn JH, Nigg JT, Rohde LA, Simonoff E. Annual research review: perspectives on progress in ADHD science—from characterization to cause. J Child Psychol Psychiatr Allied Discip. 2022 doi: 10.1111/jcpp.13696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. doi: 10.1097/j.pain.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swain MS, Henschke N, Kamper SJ, Gobina I, Ottová-Jordan V, Maher CG. An international survey of pain in adolescents. BMC Public Health. 2014;14(1):447. doi: 10.1186/1471-2458-14-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Blanchflower DG, Bryson A. Chronic pain: evidence from the national child development study. PLoS One. 2022;17(11):e0275095. doi: 10.1371/journal.pone.0275095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pourbordbari N, Riis A, Jensen MB, Olesen JL, Rathleff MS. Poor prognosis of child and adolescent musculoskeletal pain: a systematic literature review. BMJ Open. 2019;9(7):e024921. doi: 10.1136/bmjopen-2018-024921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamaleri Y, Natvig B, Ihlebaek CM, Bruusgaard D. Localized or widespread musculoskeletal pain: does it matter? Pain. 2008;138(1):41–46. doi: 10.1016/j.pain.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Leino-Arjas P, Rajaleid K, Mekuria G, Nummi T, Virtanen P, Hammarström A. Trajectories of musculoskeletal pain from adolescence to middle age: the role of early depressive symptoms, a 27-year follow-up of the Northern Swedish Cohort. Pain. 2018;159(1):67–74. doi: 10.1097/j.pain.0000000000001065. [DOI] [PubMed] [Google Scholar]
- 14.Erskine HE, Ferrari AJ, Nelson P, Polanczyk GV, Flaxman AD, Vos T, Whiteford HA, Scott JG. Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the global burden of disease study 2010. J Child Psychol Psychiatr. 2013;54(12):1263–1274. doi: 10.1111/jcpp.12144. [DOI] [PubMed] [Google Scholar]
- 15.Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450–462. doi: 10.1016/S0140-6736(19)33004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore DJ, Meints SM, Lazaridou A, Johnson D, Franceschelli O, Cornelius M, Schreiber K, Edwards RR. The effect of Induced and chronic pain on attention. J Pain. 2019;20(11):1353–1361. doi: 10.1016/j.jpain.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Holmen TL, Bratberg G, Krokstad S, Langhammer A, Hveem K, Midthjell K, Heggland J, Holmen J. Cohort profile of the Young-HUNT Study, Norway: a population-based study of adolescents. Int J Epidemiol. 2014;43(2):536–544. doi: 10.1093/ije/dys232. [DOI] [PubMed] [Google Scholar]
- 18.Åsvold BO, Langhammer A, Rehn TA, Kjelvik G, Grøntvedt TV, Sørgjerd EP, Fenstad JS, Heggland J, Holmen O, Stuifbergen MC, et al. Cohort profile update: the HUNT study Norway. Int J Epidemiol. 2023;52(1):e80–e91. doi: 10.1093/ije/dyac095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaasbøll J, Lydersen S, Indredavik MS. Psychological symptoms in children of parents with chronic pain-the HUNT study. Pain. 2012;153(5):1054–1062. doi: 10.1016/j.pain.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, et al. The world health organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. doi: 10.1017/S0033291704002892. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization (WHO) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 22.Schei J, Nøvik TS, Thomsen PH, Lydersen S, Indredavik MS, Jozefiak T. What predicts a good adolescent to adult transition in ADHD? The role of self-reported resilience. J Atten Disord. 2018;22(6):547–560. doi: 10.1177/1087054715604362. [DOI] [PubMed] [Google Scholar]
- 23.ADHD/Hyperkinetisk forstyrrelse – Nasjonal faglig retningslinje for utredning, behandling og oppfølging. Helsedirektoratet. 2016 https://helsedirektoratet.no/retningslinjer/adhd. Accessed 23 Jan 2023
- 24.American Psychiatric Association D, Association AP . Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association; 2013. [Google Scholar]
- 25.Nøvik TS, Haugan AJ, Lydersen S, Thomsen PH, Young S, Sund AM. Cognitive-behavioural group therapy for adolescents with ADHD: study protocol for a randomised controlled trial. BMJ Open. 2020;10(3):e032839. doi: 10.1136/bmjopen-2019-032839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Achenbach TM (2009) Achenbach system of empirically based assessment (ASEBA): development, findings, theory, and applications. Research Center of Children, Youth & Families: University of Vermont
- 27.DuPaul GJ, Reid R, Anastopoulos AD, Lambert MC, Watkins MW, Power TJ. Parent and teacher ratings of attention-deficit/hyperactivity disorder symptoms: factor structure and normative data. Psychol Assess. 2016;28(2):214–225. doi: 10.1037/pas0000166. [DOI] [PubMed] [Google Scholar]
- 28.Hoftun GB, Romundstad PR, Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the Young-HUNT Study 2008. J Pain. 2012;13(9):874–883. doi: 10.1016/j.jpain.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 29.Mikkelsson M, Salminen JJ, Kautiainen H. Non-specific musculoskeletal pain in preadolescents. Prevalence and 1-year persistence. Pain. 1997;73(1):29–35. doi: 10.1016/S0304-3959(97)00073-0. [DOI] [PubMed] [Google Scholar]
- 30.Mikkelsson M, El-Metwally A, Kautiainen H, Auvinen A, Macfarlane GJ, Salminen JJ. Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain. 2008;138(3):681–687. doi: 10.1016/j.pain.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 31.von Baeyer CL, Lin V, Seidman LC, Tsao JC, Zeltzer LK. Pain charts (body maps or manikins) in assessment of the location of pediatric pain. Pain Manag. 2011;1(1):61–68. doi: 10.2217/pmt.10.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Kelly, M, Bohdana R (2014) Clinical trials with missing data: a guide for practitioners. Wiley
- 33.Asztély K, Kopp S, Gillberg C, Waern M, Bergman S. Chronic pain and health-related quality of life in women with autism and/or ADHD: a prospective longitudinal study. J Pain Res. 2019;12:2925–2932. doi: 10.2147/JPR.S212422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alabaf S, Gillberg C, Lundström S, Lichtenstein P, Kerekes N, Råstam M, Anckarsäter H. Physical health in children with neurodevelopmental disorders. J Autism Dev Disord. 2019;49(1):83–95. doi: 10.1007/s10803-018-3697-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Solberg BS, Hegvik TA, Halmøy A, Skjaerven R, Engeland A, Haavik J, Klungsøyr K. Sex differences in parent-offspring recurrence of attention-deficit/hyperactivity disorder. J Child Psychol Psychiatr. 2021;62(8):1010–1018. doi: 10.1111/jcpp.13368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Foss JM, Apkarian AV, Chialvo DR. Dynamics of pain: fractal dimension of temporal variability of spontaneous pain differentiates between pain States. J Neurophysiol. 2006;95(2):730–736. doi: 10.1152/jn.00768.2005. [DOI] [PubMed] [Google Scholar]
- 37.Boerner KE, Eccleston C, Chambers CT, Keogh E. Sex differences in the efficacy of psychological therapies for the management of chronic and recurrent pain in children and adolescents: a systematic review and meta-analysis. Pain. 2017;258(4):569–582. doi: 10.1097/j.pain.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 38.Loyer Carbonneau M, Demers M, Bigras M, Guay MC. Meta-analysis of sex differences in ADHD symptoms and associated cognitive deficits. J Atten Disord. 2021;25(12):1640–1656. doi: 10.1177/1087054720923736. [DOI] [PubMed] [Google Scholar]
- 39.American Psychiatric Association Diagnostic and statistical manual of mental disorders. Am Psychiatr Assoc. 2013;5:612. [Google Scholar]
- 40.Holden S, Rathleff MS, Roos EM, Jensen MB, Pourbordbari N, Graven-Nielsen T. Pain patterns during adolescence can be grouped into four pain classes with distinct profiles: a study on a population based cohort of 2953 adolescents. Eur J Pain. 2018;22(4):793–799. doi: 10.1002/ejp.1165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.