Abstract
Introduction
Low confidence in genomics knowledge among clinicians is a major barrier to the integration of genomics into mainstream medicine. Here, we assessed the genomics confidence of UK medical students approaching graduation.
Methods
We conducted a web-based nationwide survey of UK medical students in the final 2 years of study where participants rated their confidence in genomics concepts.
Results
In total, 145 medical students across 19 medical schools participated. The amount of genomics teaching students reported receiving was positively associated with genomics confidence, with the amount of basic science teaching having the strongest influence. While confidence was high in core genomics principles, such as the difference between DNA, genes and chromosomes (95%), confidence dropped in clinical applications of genomics – only 50% reported a good understanding of the genetic contribution to disease and 28% reported good knowledge of clinically used genomic tests. Overall, 59% reported a poor understanding of variant interpretation; however, over half who reported receiving ‘lots’ of genomic medicine teaching reported a good understanding of this topic.
Conclusion
Gaps in genomics knowledge and drivers in confidence have been identified herein, highlighting the need for improvements in undergraduate genomics education to prepare future doctors to confidently practise in the genomics era.
Keywords: Basic science, Confidence, Genomic medicine, Mainstreaming, Medical education, Medical students
Introduction
Shortly after the turn of the last century, the completion of the Human Genome Project marked the beginning of a new era in medicine.1 The falling cost of DNA sequencing, with the introduction of next-generation technologies, has transformed the clinical care of patients with genetic disorders.2 Until recently, such advances in genomic medicine were only relevant to a small subset of clinicians, but the landscape of genomic medicine has changed.
The UK has been at the forefront of integrating genomics into clinical services. In 2018, building on the infrastructure developed through the landmark 100,000 Genomes Project, the NHS Genomic Medicine Service was commissioned. This service aims to provide equitable access throughout the UK to genetic testing, including whole genome sequencing (WGS), as a first-line investigation for selected clinical presentations.3 Further, in 2020, the UK government set out ambitious plans to ‘create the most advanced genomic healthcare system in the world’, prioritising the use of genomics as a routine part of healthcare.4 To implement this, mainstream clinicians are expected to request, understand, and effectively communicate the results of genomic tests.3
Doctors across mainstream medical specialties, however, consistently report poor knowledge concerning genetics and genomic medicine, highlighting a need for further education in this field.5, 6, 7, 8 In a recent study of UK oncologists – a specialty with comparatively high genomics exposure – over 90% identified a personal need for further education in the field.9 Similarly, mainstream clinicians are repeatedly found to have low confidence in their understanding of genomic medicine and its applications.8,10, 11, 12, 13 In two recent UK studies, only 28% of primary care doctors felt confident carrying out basic tasks, such as recognising when a genetic test may be indicated,11 and only 9% of gastroenterology trainees felt adequately prepared for the future practice of genomic medicine.6 Poor knowledge and low confidence pertaining to genomic medicine are major barriers to the integration of genomics into clinical practice.7,10,14,15
Furthermore, a poor understanding of genomics may begin at medical school, with studies from the US revealing that only 6% of medical students felt prepared to apply genomics to clinical care,16 and that recent graduates perceive their understanding of genetics to be significantly lower than other medical topics.17 The confidence of UK medical students in their genomics knowledge is currently unknown.
This study aims to explore the level of confidence in various genomics concepts among current UK medical students approaching the end of their courses, and thereby elucidate whether future doctors from UK medical schools feel equipped to practise medicine in the genomics era.
Methods
The survey was developed by the primary research team, reviewed by the Clinical Director of Health Education England's (HEE) Genomics Education Programme (GEP) and the Clinical Lead for Genetic Counselling at Genomics England. It was piloted using cognitive ‘Think Aloud’ interviews with medical students, social scientists, clinical geneticists and genetic counsellors and iteratively modified based on feedback.18
The final survey comprised 18 questions (Supplementary File 1). Basic demographic information collected included participants’ medical school and expected year of graduation, with only the options ‘2023′ or ‘2024′ to limit participation to medical students who have experienced most of the curriculum. Participants were asked to rate the amount of teaching they had received on the basic science of genomics and on genomic medicine (clinical application of genomics) using visual analogue scales that ranged from ‘None’ to ‘Some’ to ‘Lots’. Using a Likert scale of discrete confidence ratings (‘Not at all confident’, ‘Somewhat confident’, ‘Neutral’, ‘Confident’ and ‘Very confident’), participants were asked how confident they felt in their understanding of ten genomics concepts. These concepts were derived from the Fundamental Principles of Genomics and the Application of Genomic Knowledge to Clinical Practice domains in the Generic Genomics Syllabus developed by the Academy of Medical Royal Colleges.19
The survey was hosted on the web-based platform, REDCap.20,21 Invitations to complete the survey using an anonymous link were sent via email to all UK medical schools on 14 November 2022. Following approval from the Education Leads Advisory Group, the Medical Schools Council also disseminated the survey on 6 January 2023. In addition, the survey was shared via the Postgraduate Medical Education Department's at Great Ormond Street Hospital social media platform and the mailing lists of several university paediatrics societies. The survey was closed on 24 February 2023.
The discrete confidence ratings were assigned a numerical value from one (‘Not at all confident’) to five (‘Very confident’) and a total confidence score was calculated. The ratings ‘Not at all confident’ and ‘Somewhat confident’ were aggregated and labelled ‘Poor’, and ‘Confident’ and ‘Very confident’ were aggregated and labelled ‘Good’. Data in the continuous variable (total confidence in genomics knowledge) satisfied three out of four tests for normality and so parametric tests were employed. The effects of independent categorical variables on the continuous variable were analysed using Welch's T-test (two levels) or ANOVA (three or more levels). A series of additive ANOVA models were run to ascertain the effect size of each categorical variable on the continuous variable. Associations between categorical variables were analysed using Fisher's exact test. Standard significance level of p ≤ 0.05 was used for all tests. Responses from participants who reported the main style of teaching at their medical school as ‘Integrated’ or ‘Problem-based’ learning were analysed together and labelled ‘Integrated’ given the considerable overlap of these teaching styles. All data analysis was performed using RStudio.22
Approval was obtained from UCL Research Ethics Committee (Project ID: 23129.001) and the Clinical Research Adoptions Committee, UCL Great Ormond Street Institute of Child Health.
Patients and the public were not involved in our work.
Results
A total of 145 complete responses were received from medical students across 19 of the 33 UK medical schools.23 Demographic details are given in Table 1. Of respondents with experience in genomics beyond the core medical school curriculum, most had intercalated or completed an undergraduate degree in genomics (64%; n = 37) and several had completed a research project outside their degree (24%; n = 14) or a student-selected component of their degree in genomics (21%; n = 12).
Table 1.
Participant characteristics.
| Characteristic | N = 145a | |
|---|---|---|
| Gender | Female | 94 (65 %) |
| Male | 43 (30 %) | |
| Non-binary | 6 (4 %) | |
| Prefer not to say | 2 (1 %) | |
| Age | 21 | 13 (9 %) |
| 22 | 35 (24 %) | |
| 23 | 41 (28 %) | |
| 24 | 23 (16 %) | |
| 25 | 8 (6 %) | |
| Over 25 | 25 (17 %) | |
| Expected year of graduation | 2023 | 49 (34 %) |
| 2024 | 96 (66 %) | |
| Teaching style | Integrated | 82 (57 %) |
| Traditional | 63 (43 %) | |
| Additional genomics experience | No | 87 (60 %) |
| Yes | 58 (40 %) | |
n (%)
Overall confidence in genomics knowledge
The mean score for total confidence in genomics knowledge was 34.4 (range: 11–50; SD = 8.73). Higher confidence was reported among students who were on traditional courses, male, had additional genomics experience, and had reported receiving more teaching on the basic science of genomics and on genomic medicine (Table 2). The factor that influenced medical students’ genomics confidence most was the amount of teaching they reported receiving on the basic science of genomics (ηp2=0.19). Teaching style also had a large effect size (ηp2=0.15). Medium, and equal, effect sizes were observed from additional genomics experience and gender (ηp2=0.09). The reported amount of teaching on genomic medicine had the smallest effect size (ηp2=0.05). The higher confidence reported among males, respondents with additional genomics experience and those who reported receiving more teaching on the basic science of genomics and on genomic medicine was independent of medical school teaching style (Supplementary Table 1).
Table 2.
Mean confidence in genomics knowledge for respondents grouped by categorical variable.
| Characteristic | Mean total confidence | p-value | |
|---|---|---|---|
| Teaching style | Traditional | 37.6 | <0.001a |
| Integrated | 31.9 | ||
| Gender | Male | 37.5 | <0.005a |
| Female | 32.7 | ||
| Additional genomics experience | Yes | 37.2 | <0.005a |
| No | 32.5 | ||
| Amount of basic science teaching | Lots | 40.8 | <0.001b |
| Some | 32.7 | ||
| None | 24.4 | ||
| Amount of genomic medicine teaching | Lots | 42.9 | <0.001b |
| Some | 35.3 | ||
| None | 29.4 | ||
Comparative analysis performed using T-test
Comparative analysis performed using ANOVA, followed by Tukey test for pairwise comparisons.
Amount of genomics teaching and teaching style
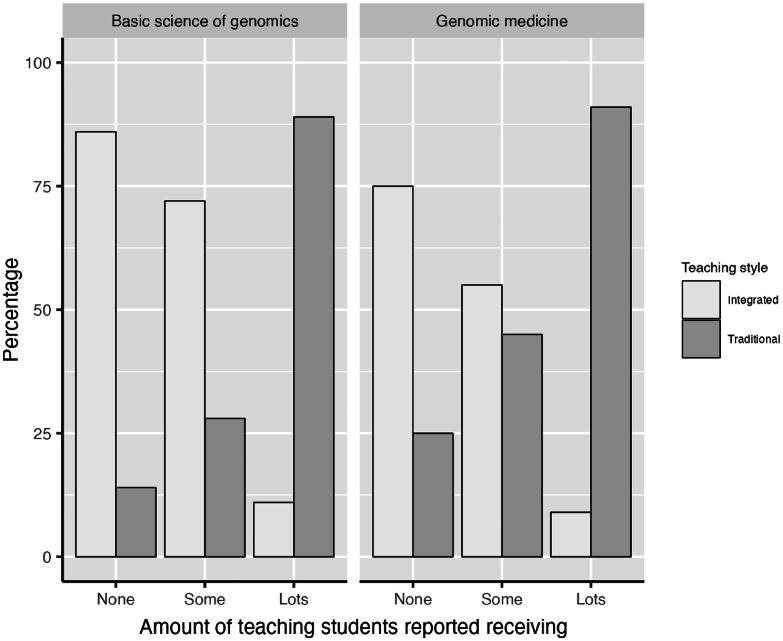
Overall, respondents reported to have received more teaching on the basic science of genomics than on genomic medicine, with significantly more respondents reporting to have not received any teaching on genomic medicine (25 %; n = 36) compared to the basic science (5 %; n = 7; p < 0.001). The majority of respondents reported having received ‘some’ teaching on the basic science of genomics (69 %; n = 100) and genomic medicine (68 %; n = 98). There was a significant association between teaching style and the reported amount of teaching received on both the basic science of genomics (p < 0.001) and on genomic medicine (p < 0.001), indicating that students on traditional courses receive more genomics teaching than those on integrated courses (Fig. 1).
Fig. 1.
The amount of genomics teaching students on traditional and integrated medicine courses reported having received.
Confidence in genomics topics
Almost all respondents reported a good understanding of the difference between DNA, genes and chromosomes (95%; n = 138) and how to identify inheritance patterns (90%; n = 131). Most also reported a good understanding of the difference between somatic and germline variants (65%; n = 94) and the concept of mosaicism (59%; n = 86). Approximately half (50%; n = 73) reported a good understanding of the genetic contribution to disease but only 28% (n = 41) reported a good knowledge of clinically used genomic tests. Despite many reporting a good understanding of the difference between certain types of variants – loss-of-function and gain-of-function (79%; n = 115), synonymous and missense (45%; n = 65) – more than half (59%; n = 85) reported a poor understanding of variant interpretation.
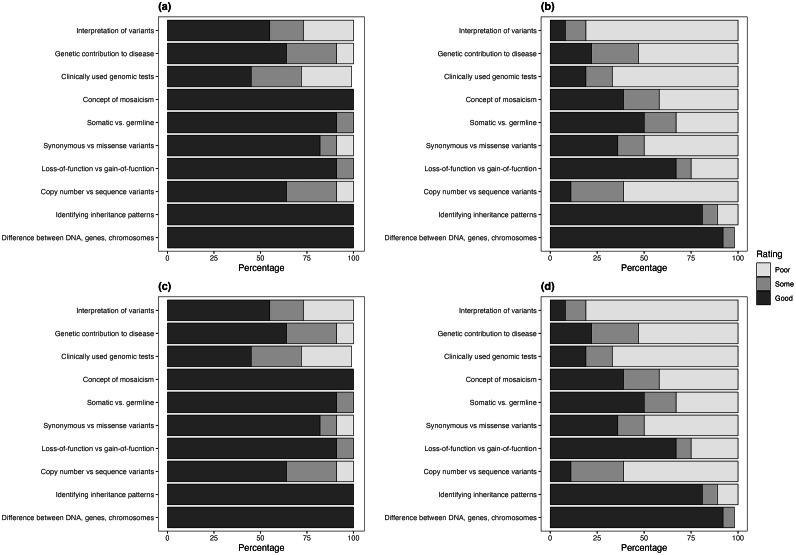
All respondents who reported receiving ‘lots’ of teaching on the basic science of genomics (100%; n = 38) and on genomic medicine (100%; n = 11), and almost all who reported having received no genomics teaching (86%; n = 7; 92%; n = 33, respectively) still reported a good understanding of the difference between DNA, genes and chromosomes (Fig. 2).
Fig. 2.
Respondents’ confidence in their understanding of genomics concepts according to whether they reported having received lots (a) or no (b) teaching on the basic science of genomics and lots (c) or no (d) teaching on genomic medicine.
Most respondents who reported receiving ‘lots’ of teaching on the basic science of genomics and on genomic medicine reported a good understanding of the difference between types of variants: copy number and sequence (55%; n = 21; 64%; n = 7, respectively), somatic and germline (84%; n = 32; 91%; n = 10, respectively), synonymous and missense (68%; n = 26; 82%; n = 9, respectively), and of the concept of mosaicism (94%; n = 34; 100%; n = 11, respectively). However, varying low levels of confidence on these topics was found among those who reported receiving no teaching on the basic science of genomics and on genomic medicine (Fig. 2).
A poor understanding of the genetic contribution to disease was identified among most of those who reported to have not received teaching on the basic science of genomics (86%; n = 6) and on genomic medicine (53%; n = 19), compared to the majority of respondents who had reported receiving ‘lots’ of genomics teaching who had a good understanding of this concept (74%; n = 28; 64%; n = 7, respectively).
A poor understanding of clinically used genomic tests was reported by most respondents who had reported not receiving any teaching on the basic science of genomics and on genomic medicine (86%; n = 6 and 67%; n = 24, respectively). Confidence remained low among those who had received more teaching, with fewer than half of those who reported receiving ‘lots’ of teaching on the basic science of genomics (45%; n = 17) and on genomic medicine (45%; n = 5) reporting a good understanding of this topic.
Slightly more than half of respondents who reported having received ‘lots’ of genomic medicine teaching reported a good understanding of variant interpretation (55%; n = 6). Only 39% (n = 15) of those who reported receiving ‘lots’ of teaching on the basic science of genomics reported a good understanding of this topic. All who reported receiving no teaching on the basic science of genomics (100%; n = 7) and most of those who reported receiving no genomic medicine teaching (81%; n = 29) reported a poor understanding of variant interpretation.
Discussion
This is the first survey to explore UK medical students’ confidence in their knowledge of genomics topics. Since higher confidence encourages genomic medicine practice,7, 8, 9,11,14 drivers of confidence and gaps in knowledge could inform strategies to better prepare the future workforce for employing genomic medicine throughout the healthcare service. Here, we found that most participants reported being taught at least some aspects of genomics in their undergraduate medicine course and many reported a good understanding of several genomics concepts. This indicates that UK medical schools have been adapting curricula to reflect advances in the field, as indicated in a recent systematic review that identified better genetics knowledge among more recent nursing and physician graduates internationally compared to their more experienced colleagues.14
The amount of genomics teaching students reported having received was positively associated with their perceived confidence in genomics, consistent with existing literature – primary care physicians with the lowest levels of confidence were those with the least exposure to medical genetics in training,11 and several studies have called for further education to remedy mainstream clinicians’ lack of confidence.7, 8, 9, 10 Notably, in our study, the amount of teaching on the basic sciences of genomics had the strongest influence on confidence, emphasising the importance of a strong foundation in scientific knowledge in producing doctors equipped to practise genomic medicine.
Teaching style also influenced genomics confidence. In our study, the mean total confidence of students on traditional courses was higher than those on integrated courses. We found that although traditional courses were associated with more teaching on the basic science of genomics, the strong effects of these factors were independent of each other. Despite previous criticisms of the problem-based learning (PBL) pedagogy,24 a recent scoping systematic review found either no difference or superiority in learning retention of students on PBL courses compared to those on traditional lecture-based learning, in most studies.25 Studies included in this review did not examine knowledge of basic science concepts or genomic medicine specifically; further research is required to delineate how different teaching styles may influence students’ knowledge and confidence in genomics and hence promote genomic medicine practice.
Additionally, those who identified as male reported higher genomics confidence than females – a trend which has also been observed among primary care physicians concerning confidence in ability to perform clinical genomics tasks.11 This gender disparity in self-perceived confidence is consistently reported within the profession, throughout the levels of training: female medical students have been found to underestimate their performance more than males26; and in a nationwide study of resident physicians in Japan, women reported lower clinical confidence, even after adjusting for amount of clinical experience.27 Broad consideration for how to address this social phenomenon throughout the field of medicine is needed, and attention to tackling this issue within genomics is warranted given the clinical implications of low genomics confidence.14
Like previous studies involving mainstream clinicians,8, 9, 10 we found that confidence in knowledge of discrete genomics concepts among medical students varied. Although almost all were confident in their understanding of core genomics principles, such as the difference between DNA, genes and chromosomes and how to identify inheritance patterns, confidence was lower in more advanced topics, such as the difference between types of variants. This culminated in nearly two-thirds of students not being confident in their understanding of variant interpretation – a topic that underpins effective counselling and communication with patients and families around genomic testing, as stipulated in HEE GEP's competency framework.28 This finding was more pronounced among those who reported receiving less genomics teaching and was also observed among those who reported receiving lots of basic science teaching, with fewer than half of this group reporting good confidence in their understanding of variant interpretation. In contrast, over half of those who reported receiving ‘lots’ of genomic medicine teaching reported a good understanding of this topic. Therefore, even in those students who reported having a strong foundation in basic science, specific education in genomic medicine appears to have a valuable role in enabling students to apply their basic science knowledge clinically.
Additionally, over half of students were not confident in their knowledge of clinically used genomic tests. This observation does not appear to be strongly influenced by the amount of genomics teaching students received – fewer than half of even those who reported receiving ‘lots’ of genomic medicine teaching reported good knowledge of this topic. Similar findings were presented in a recent study of mainstream clinicians in Australia, where despite three-quarters of respondents reporting they had already learnt basic concepts of genomics, over 80% requested further education on genomic medicine topics such as the clinical utility of genomic tests.8
A review of undergraduate medicine curricula could be considered, given that a quarter of respondents in our study reported to have not received any genomic medicine teaching and confidence in key genomic medicine concepts was low. Since clinicians with more genomics knowledge and confidence are more likely to use genomics in clinical practice,14 our findings support the ‘Genome UK’ implementation plan that suggests undergraduate curricula need to be ‘update[d]... to integrate genomic medicine’29 to ensure that the mainstream workforce has a strong genomic medicine knowledge base to facilitate the effective delivery of genomics within the healthcare service. Careful consideration could be given to the design of schemes such as the Medical Doctor Apprenticeship,30 that plan to train doctors largely through practical clinical experience, to not compromise knowledge of basic science concepts that are crucial for practising in ‘the most advanced genomic healthcare system in the world’.29 Strategies for educational reform of current curricula could involve collaboration with HEE GEP, which provides a wealth of online educational resources and delivers genomics education to UK healthcare professionals,31,32 as well as the creation of opportunities for experiential learning in clinical environments, which have been shown to promote confidence.33
Limitations
There are several limitations to this study. Given that students are emailed many questionnaires, disseminating our survey in this way may have limited our response rate (although, we have no reason to believe this is not a representative sample given the spread of responses from 19 medical schools). The results may be subject to selection bias as those interested in genomics may be more likely to participate. A possible weakness in the survey is the subjective nature of some data generated – asking students about the amount of genomics teaching they received is vulnerable to variation in inter-respondent interpretation and may not reflect the true levels of teaching delivered on curricula. Another possible weakness is that only three out of the ten genomics concepts on which participants were asked to rate their confidence were drawn from the Application of Genomic Knowledge to Clinical Practice domain of the Generic Genomic Syllabus,19 perhaps limiting our ability to measure confidence in genomic medicine and, given the additive model employed for assessing overall confidence, this may have underestimated the influence of the amount of genomic medicine teaching on overall confidence.
Conclusions
Although current UK medical students in their final 2 years of study may be confident in many basic science genomics topics, confidence in how to apply this clinically is low, with most not being confident in their understanding of variant interpretation or clinically used genomic tests. The success of genomic medicine relies on the translation of genomics knowledge into mainstream clinical settings. Therefore, educational reform could help ensure that the next generation of medical professionals are prepared to practise in the genomics era and harness the clinical benefits of genomic advances, ultimately improving patient care and facilitating equitable access to genomic medicine in the NHS.
Summary box.
What is known?
Low confidence in genomics knowledge among clinicians is a major barrier to practising genomic medicine in mainstream clinical specialties.
What is the question?
How confident are UK medical students nearing the end of their course in their genomics knowledge?
What was found?
Confidence was high in some basic concepts, like the difference between DNA, genes and chromosomes, but confidence was much lower in more complex topics and in their clinical applications, such as clinically used tests and understanding variant interpretation.
What is the implication for practice now?
Consideration to reviewing and updating undergraduate medical curricula should be given with a view to improving education on genomic medicine, to improve future clinician's confidence and hence the practice genomic medicine.
Alt-text: Unlabelled box
CRediT authorship contribution statement
Lydia Seed: Conceptualization, Formal analysis, Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing, Project administration. Anna Scott: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. Michelle Peter: Formal analysis, Data curation, Methodology, Software, Supervision, Writing – review & editing. Shereen Tadros: Conceptualization, Methodology, Supervision, Writing – review & editing. Melissa Hill: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing, Resources, Funding acquisition. Cristine Sortica da Costa: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing, Resources, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We are very grateful to all of the medical students who took part in the survey. Thank you to Marissa Willock, Postgraduate Medical Education Department at Great Ormond Street Hospital for supporting medical student research and facilitating medical students to join research placements at Great Ormond Street Hospital. MP and MH are partially funded by the NIHR Biomedical Research Centre at Great Ormond Street Hospital. All research at Great Ormond Street Hospital NHS Foundation Trust and UCL Great Ormond Street Institute of Child Health is made possible by the NIHR Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the UK Department of Health.
Footnotes
This article reflects the opinions of the author(s) and should not be taken to represent the policy of the Royal College of Physicians unless specifically stated.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.fhj.2024.100133.
Appendix. Supplementary materials
References
- 1.Lander ES, Linton LM Birren B., et al Initial sequencing and analysis of the human genome. Nature. 2001-02-15 2001;409(6822):860–921. doi:10.1038/35057062 [DOI] [PubMed]
- 2.Shendure J, Findlay GM, Snyder MW. Genomic medicine–progress, pitfalls, and promise. Cell. 2019;177(1):45–57. doi: 10.1016/j.cell.2019.02.003. 2019-03-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snape K, Wedderburn S, Barwell J. The new genomic medicine service and implications for patients. Clin Med. 2019;19(4):273–277. doi: 10.7861/clinmedicine.19-4-273. 2019-07-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Genome UK: the future of healthcare (gov.uk) (2020).
- 5.Mladenić T, Mavrinac M, Dević Pavlić S, et al Non-genetic physicians' knowledge, attitudes and behavior towards medical genetics. Wien Klin Wochenschr. 2023; 10.1007/s00508-023-02152-0 [DOI] [PubMed]
- 6.Al Bakir I, Sebepos-Rogers GM, Burton H, Monahan KJ. Mainstreaming of genomic medicine in gastroenterology, present and future: a nationwide survey of UK gastroenterology trainees. BMJ Open. 2019;9(10) doi: 10.1136/bmjopen-2019-030505. 2019-10-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rasouly HM, Balderes O, Marasa M, et al. The effect of genetic education on the referral of patients to genetic evaluation: Findings from a national survey of nephrologists. Genet Med. 2023;25(5) doi: 10.1016/j.gim.2023.100814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nisselle A, King EA, McClaren B, Janinski M, Metcalfe S, Gaff C. Measuring physician practice, preparedness and preferences for genomic medicine: a national survey. BMJ Open. 2021;11(7) doi: 10.1136/bmjopen-2020-044408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tutika RK, Bennett JA, Abraham J, et al. Mainstreaming of genomics in oncology: a nationwide survey of the genomics training needs of UK oncologists. Clin Med. 2023;23(1):9–15. doi: 10.7861/clinmed.2022-0372. 2023-01-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson L-M, Valdez JM, Quinn EA, et al. Integrating next-generation sequencing into pediatric oncology practice: an assessment of physician confidence and understanding of clinical genomics. Cancer. 2017;123(12):2352–2359. doi: 10.1002/cncr.30581. 2017-06-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nippert I, Harris HJ, Julian-Reynier C, et al. Confidence of primary care physicians in their ability to carry out basic medical genetic tasks—a European survey in five countries—Part 1. J Community Genet. 2011;2(1):1–11. doi: 10.1007/s12687-010-0030-0. 2011-03-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cox SL, Zlot AI, Silvey K, et al. Patterns of cancer genetic testing: a randomized survey of oregon clinicians. J Cancer Epidemiol. 2012;2012:1–11. doi: 10.1155/2012/294730. 2012-01-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jayasinghe K, Quinlan C, Mallett AJ, et al. Attitudes and practices of Australian nephrologists toward implementation of clinical genomics. Kidney Int Rep. 2021;6(2):272–283. doi: 10.1016/j.ekir.2020.10.030. 2021-02-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White S, Jacobs C, Phillips J. Mainstreaming genetics and genomics: a systematic review of the barriers and facilitators for nurses and physicians in secondary and tertiary care. Genet Med. 2020;22(7):1149–1155. doi: 10.1038/s41436-020-0785-6. [DOI] [PubMed] [Google Scholar]
- 15.Gray SW, Hicks-Courant K, Cronin A, Rollins BJ, Weeks JC. Physicians' attitudes about multiplex tumor genomic testing. J Clin Oncol. 2014;32(13):1317–1323. doi: 10.1200/jco.2013.52.4298. 2014-05-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eden C, Johnson KW, Gottesman O, Bottinger EP, Abul-Husn NS. Medical student preparedness for an era of personalized medicine: findings from one US medical school. Per Med. 2016;13(2):129–141. doi: 10.2217/pme.15.58. 2016-03-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haspel RL, Genzen JR, Wagner J, et al. Call for improvement in medical school training in genetics: results of a national survey. Genet Med. 2021;23(6):1151–1157. doi: 10.1038/s41436-021-01100-5. 2021-06-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12(3):229–238. doi: 10.1023/a:1023254226592. [DOI] [PubMed] [Google Scholar]
- 19.Colleges AoMR. Generic genomic syllabus. 2021.
- 20.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.R: a language and environment for statistical computing Version 4.2.3. R Foundation for Statistical Computing; 2023. https://www.R-project.org/.
- 23.Council GM Awarding bodies and new schools. 2023. https://www.gmc-uk.org/education/how-we-quality-assure-medical-education-and-training/evidence-data-and-intelligence/awarding-bodies-and-new-schoolshttps://www.gmc-uk.org/education/how-we-quality-assure-medical-education-and-training/evidence-data-and-intelligence/awarding-bodies-and-new-schools.
- 24.Shanley PF. Viewpoint: leaving the “Empty Glass” of problem-based learning behind: new assumptions and a revised model for case study in preclinical medical education. Acad Med. 2007;82(5):479–485. doi: 10.1097/ACM.0b013e31803eac4c. [DOI] [PubMed] [Google Scholar]
- 25.Trullàs JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1):104. doi: 10.1186/s12909-022-03154-8. 2022/02/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blanch-Hartigan D. Medical students' self-assessment of performance: results from three meta-analyses. Patient Educ Couns. Jul 2011;84(1):3–9. doi: 10.1016/j.pec.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 27.Nomura K, Yano E, Fukui T. Gender differences in clinical confidence: a nationwide survey of resident physicians in Japan. Acad Med. Apr 2010;85(4):647–653. doi: 10.1097/ACM.0b013e3181d2a796. [DOI] [PubMed] [Google Scholar]
- 28.Programme GE A cross-professional competency framework for communicating germline genomic results. [DOI] [PubMed]
- 29.Genome UK: 2022 to 2025 implementation plan for England (2022).
- 30.NHS long term workforce plan (2023).
- 31.Genomics education programme HEE. NHS England Genomics Education.
- 32.Copson E, Mcveigh T, Frost A, Tatton-Brown K. GeNotes: a new online ‘just in time’ genomics resource for healthcare professionals. Fut Healthc J. 2022;9(Suppl 2):68–69. doi: 10.7861/fhj.9-2-s68. 2022-07-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McClaren BJ, Crellin E, Janinski M, et al. Preparing medical specialists for genomic medicine: continuing education should include opportunities for experiential learning. Front Genet. 2020;11:151. doi: 10.3389/fgene.2020.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.