Abstract
This review explores the intricate relationship between knee osteotomy and frontal plane joint line orientation, emphasizing the dynamic nature of the joint line’s influence on knee forces and kinematics.
Consideration of coronal alignments, knee phenotypes, and associated angles (medial proximal tibial angle (MTPA), lateral distal femoral angle (LDFA), joint line convergence angle (JLCA)) becomes crucial in surgical planning to avoid joint line deformities.
The double-level osteotomy is to be considered a valid option, especially for severe deformities; however, the target patient cannot be selected solely based on high predicted postoperative joint line obliquity (JLO) and MPTA.
Keywords: knee osteotomy, joint line orientation, knee phenotypes, frontal plane, double level osteotomy
Introduction
Knee osteotomy, a surgical procedure designed for the correction of bone deformities, has been in use for centuries. Following the introduction and exponential development of arthroplasty surgery, this practice lost interest. However, in the last two decades it has vigorously regained popularity, which is due to the adoption of internal devices with improved biomechanical properties like locking plates (1) and the poor results of knee replacement in young patients with high functional demands (2, 3, 4).
Osteotomies around the knee redistribute the load to the compartment which is unaffected by osteoarthritis, aiming to alleviate symptoms and delay or avoid the need for later arthroplasty. Historically, osteotomies were directed at correcting a single bone: mostly proximal tibial osteotomy (PTO) for varus knees and distal femur osteotomy (DFO) for valgus knees. Today we know that tibia-based varus deformities account for approximately 30% only (5). In other cases, they are attributable to femoral, intra-articular, or combined deformities. Paley et al. (6) suggested that deformity analysis is crucial to identify its location and prevent non-physiological joint line orientation after correction. Although PTO is undoubtedly the most widely used procedure to manage medial knee osteoarthritis with good results (7, 8), single osteotomy may lead to up to 40% undesired overcorrection (9, 10), impacting middle- and long-term results. Change in joint line obliquity (JLO) pose a dilemma for orthopedic surgeons. If the decision is to accept a secondary deformity, there is a risk of compromising knee stability and altering knee biomechanics (11).
To overcome this challenge, Babis et al. (12) proposed the use of double-level osteotomy (DLO) (combination of PTO and DFO). Initially not widely adopted, this approach has gained popularity in recent years, with several authors demonstrating its effectiveness in correcting malalignment while avoiding non physiological JLO (13, 14).
This review article aims to elucidate the intricate relationship between knee osteotomy and joint line orientation, delving into the anatomical and biomechanical aspects that underscore their interdependence. By providing a comprehensive exploration of relevant literature, we intend to shed light on the current state of knowledge regarding management of joint line in the frontal plane throughout knee osteotomy, addressing both established principles and emerging perspectives.
The joint line: a dynamic concept
The joint line is not merely a geometric measure but a dynamic reference influencing the balance of forces and the kinematics of the knee.
In a properly aligned lower limb, the joint line typically exhibits a slight varus orientation of approximately 3°, leading to a medial proximal tibial angle (MPTA) of 87° and a lateral distal femoral angle (LDFA) of 87° (Fig. 1). This varus inclination is considered physiological, due to the distance between the hip joint centers and the ankle joint center. Specifically, during one-leg standing or the stance phase of gait, the leg undergoes an adduction movement that aligns the joint line parallel to the ground at a 0° orientation. This ensures that the resultant force passing through the articular surface is primarily perpendicular to the knee joint line, with a minor shear component directed medially (15). However, it is important to note that such an ideal lower limb alignment may not be present in all individuals.
Figure 1.
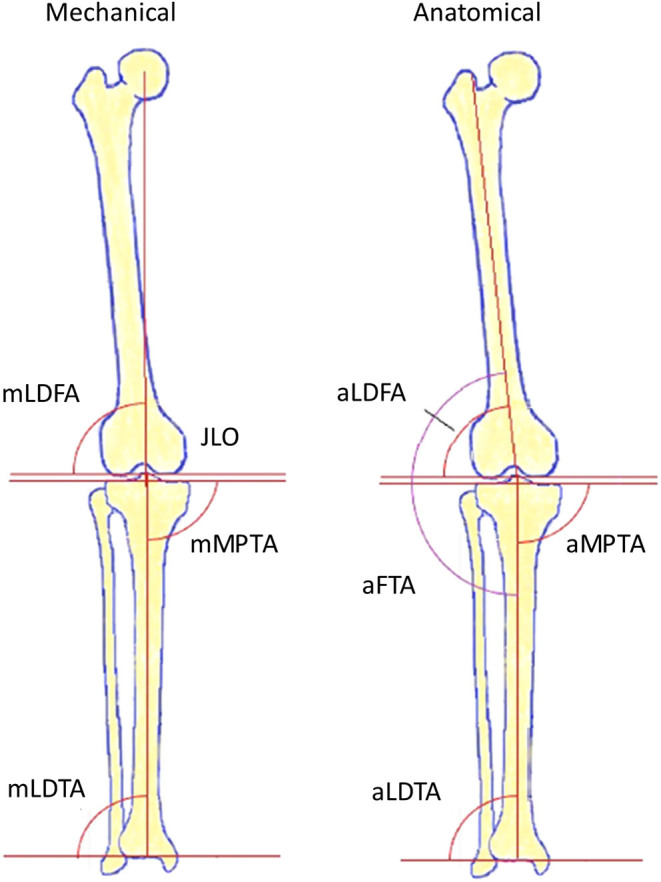
Lower limb angles. Femorotibial angle (FTA); lateral distal femoral angle (LDFA); medial proximal tibial angle (MPTA); lateral distal tibial angle (LDTA); joint line obliquity (JLO).
Evaluating the lower limb alignment in loading conditions and in its entirety is crucial, and it is essential not to solely rely on this assessment without taking into account the positions of the femoral and tibial joint lines. A lower limb that appears neutrally aligned in static conditions may not necessarily exhibit a neutral alignment in the joint line, which is independent of mechanical axis.
Assessment of frontal plane alignment
Correcting the deformity can take place in a single plane (frontal, sagittal, transverse) or multiple planes. A comprehensive radiological assessment is crucial for a thorough understanding of the deformity. Even today, more than half of the cases show a non-anatomical correction after osteotomy because the correction is not carried out at the site of the deformity (16). Regarding the frontal plane, it is mandatory to analyze and be aware of the normal values of the following parameters: MPTA, LDFA, and JLCA. Once the values are obtained, it is possible to determine the origin of the deformity requiring correction. Usually, the assessment of coronal plane alignment is performed using long-leg radiography (LLR). Several methods have been proposed to measure the mechanical axis in standard anteroposterior weight-bearing knee radiographs to avoid excessive radiation, time, and costs, but they are significantly less accurate (17). It has been demonstrated that varus malalignment increases from double-leg to single-leg stance, with a significant increase in joint line convergence angle (JLCA) due to lateral laxity. Therefore, the single-leg stance can be useful during planning to avoid postoperative overcorrection (18).
Lower limb alignment can be influenced by foot rotation. External rotation (ER) causes an increase in varus, while internal rotation (IR) leads to the opposite (19). Similarly, a deficit in knee extension underestimates varus angulation (20). The correlation between joint line orientation and the distance between the feet is evident, with a notable shift of 3.7° observed when transitioning from a position where the feet are kept together to a separation of 10 centimeters (21). Correct alignment can be achieved using the patellar orientation method described by Paley (22), with necessary adjustments for patients with patellar malalignment. Likewise, the appearance of the trochanter minor on the long-leg standing radiograph provides information on hip rotation which is also susceptible to alter alignment.
Measurement methods for osteotomy planning
Effective angular correction starts with thorough preoperative surgical planning. The surgeons’ goal should be to restore proper alignment while simultaneously avoiding the development of new deformities, such as JLO, which can alter the patient’s constitutional phenotype. Various techniques have been presented in preoperative planning studies to ensure precise alignment in MOWPTO, among these, the Miniaci technique stands out as the most commonly used technique (23) (Fig. 2). Studies have demonstrated its effectiveness compared to others (24). However, uncertainties persist regarding potential measurement or correction errors that could lead to less-than-ideal outcomes.
Figure 2.
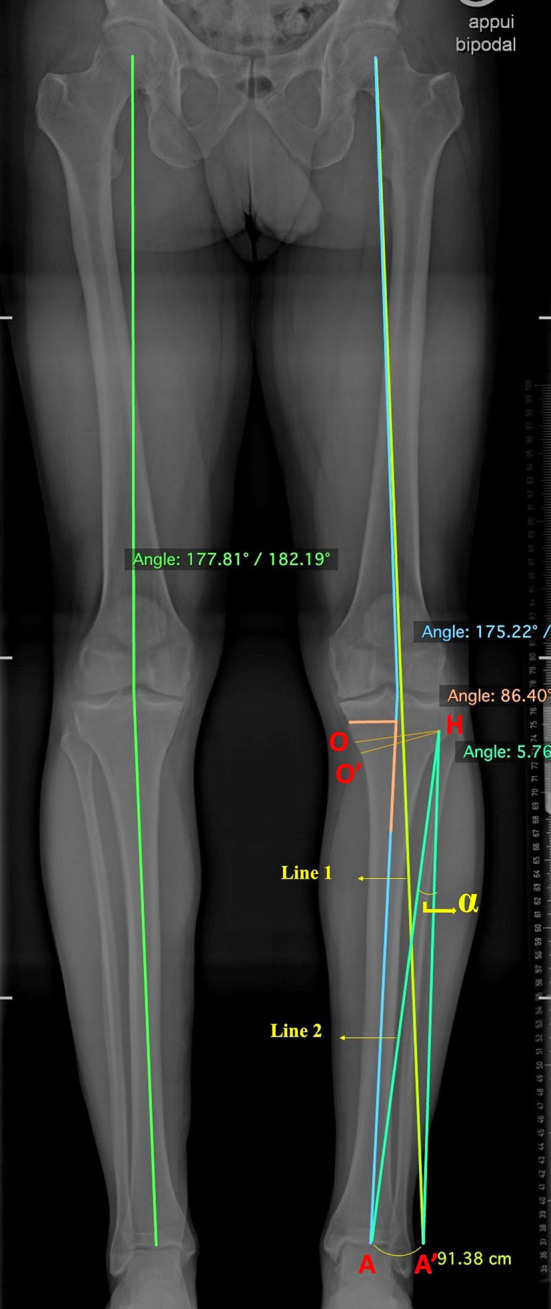
Planning OWPTO according to Miniaci’s technique using AP long-leg standing radiograph. The line 1 was drawn from the hip center through the pre-established correction point at the knee tibial plateau (this point can be positioned between 50% and 62.5% of the tibial plateau from the medial edge; the more lateral it is, the more overcorrection of the valgus axis is achieved). The hinge point H was identified, approximately 15–20 mm from the joint line and 5–10 mm from the lateral cortex. Line 2 was drawn connecting point H with the center of the ankle A. Subsequently, a circular arc was drawn with the center at point H and a radius of HA from point A to the intersection with line 1, resulting in point A′. The angle α between lines HA and HA′ represents the correction angle. Finally, a predicted osteotomy line O was drawn from point H to the predicted medial osteotomy site, approximately 40 mm inferior to the medial tibial plateau. A predicted opening line O′ was drawn from line O at the determined correction angle, and the correction gap was measured.
To minimize these unexpected errors, it is mandatory to carefully consider all the factors that play a role in defining the extent of the deformity. Of these, the most relevant is the JLCA (reference value 0° ± 2°). Various equations have been proposed to balance its effect and avoid overcorrection (25, 26, 27). In our clinical practice, we commonly use the one proposed by Micicoi et al. (28), an equation that is easy to read and apply: (JLCA – 2)/2. The obtained value represents the amount of intra-articular deformity resulting in overcorrection, and by subtracting this value from the established correction angle, the desired result can be achieved. Recently, the validity of this method has been demonstrated; for JLCA values ≥4°, there is a significant reduction in MPTA compared to not using the correction equation (29).
Recently, the reverse Miniaci method for lateral closing wedge distal femoral osteotomy (LCWDFO) has been validated (30), and, similar to its tibial counterpart, it plans the correction of deformity on a single segment, in this case, the femur. When dealing with severe deformities or those with a mixed component (tibial, femoral, and intra-articular), and a single osteotomy cannot predict acceptable JLO values, the DLO becomes necessary. In this case, planning is exclusively carried out using advanced software through virtual segmentation, such as mediCAD (Hectec GmbH, Germany), PreOPlan (Siemens; Synthes, Solothurn, Switzerland), AutoCAD (Autodesk Inc., San Rafael, CA), and TraumaCad (Brainlab AG, Munich, Germany).
In these software applications, X-ray images can be uploaded, and the user subsequently marks a series of skeletal landmarks. The various geometric calculations are preestablished but still depend on the positions of the landmarks. The software also has the ability to manipulate and rotate segments of the X-ray around hinge points, simulating osteotomy. This enables the extraction of correction angles and the thickness of the tibial and femoral wedges.
To our knowledge, a recently proposed manual method for DLO planning is the new Mikulicz-joint line (NM-JL) stands out as the only tool available. This method uses a vertical line passing through the selected correction point on the tangent to the tibial plateau, creating the NM-JL angle medially. The latter can be adjusted according to the desired JLO. Finally, the tibial and femoral correction angles are calculated using the Miniaci method. The authors compared it with results obtained using software and found remarkable agreement (31). Further validation studies are needed, but it could be a useful tool, especially for those who do not have access to specific software.
Angles for joint line measurement: challenges and considerations
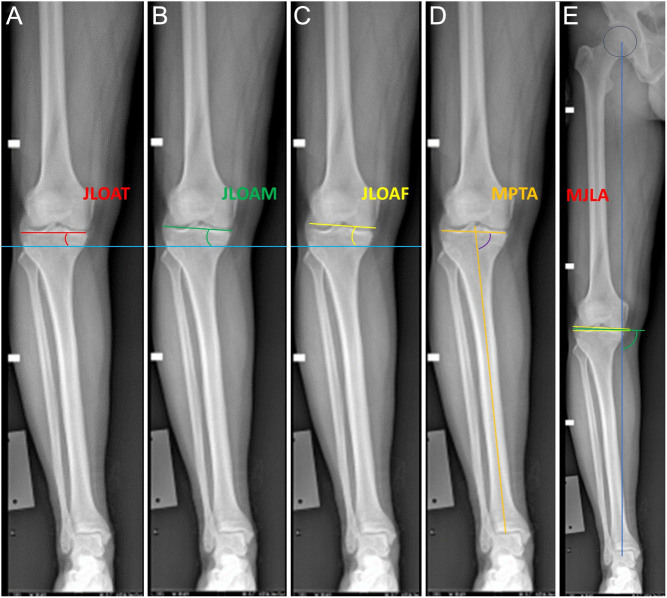
Various angles have been suggested in the literature for the measurement of joint line inclination in the coronal plane. They are of use both for preoperative planning and for postoperative assessment of the achieved correction and include the joint line orientation angle by the femoral condyles (JLOAF), the joint line orientation angle by the middle knee joint space (JLOAM), the joint line orientation angle by the tibial plateau (JLOAT), the MPTA, and the Mikulicz joint line angle (MJLA) (Table 1) (Fig. 3) (32).
Table 1.
Various angles described to measure joint line obliquity.
| Reference | Angle | Definition |
|---|---|---|
| Oh et al. (61) | JLOAT | Angle between a line tangent to tibial plateau and the horizontal line |
| Lee et al. (74) | JLOAM | Angle between the middle knee joint space line and the horizontal line |
| Akamatsu et al. (71) | JLOAF | Angle between a line tangent to distal femoral condyles and the horizontal line |
| Rosso et al. (36) | MPTA | Angle between a line tangent to proximal tibia and tibial mechanical axis |
| Rosso et al. (36) | MJLA | Angle between the Mikulicz line (weight-bearing line) and the bisector of the joint line congruency angle |
JLOAT,joint line orientation angle by the tibial plateau; JLOAM, joint line orientation angle by the middle knee joint space; JLOAF, joint line orientation angle by the femoral condyles; MPTA, medial proximal tibial angle; MJLA, Mikulicz joint line angle.
Figure 3.
JLO measurement methods on AP long-leg standing radiograph. The description is provided in Table 2. (A)Joint line orientation angle by the tibial plateau (JLOAT). (B)Joint line orientation angle by the middle knee joint space (JLOAM). (C)Joint line orientation angle by the femoral condyles (JLOAF). (D) Medial proximal tibial angle (MPTA). (E) Mikulicz joint line angle (MJLA).
Reference values for these measures have not undergone extensive study and validation. In some instances, certain authors have identified thresholds beyond which the JLO was considered excessively high, potentially compromising long-term clinical outcomes. However, a threshold from which a negative clinical impact can be expected after osteotomy has yet to be defined. Babis et al. (12) proposed a JLOAT cutoff of 4°. Nakayama et al. (33) established a cutoff value of 95° for MPTA. Lobenhoffer et al. (35) characterized a pathological JLO as a MJLA ≥94° (Table 2). Between these angles the most used are JLOAT and JLOAM. They represent two very similar concepts. The first is based exclusively on the bony configuration of the tibia, thus representing a clear and easy to define reference point. The second method has a higher inter- and intra-observer variability in identifying the mid-point landmarks of the medial and lateral compartment (35). Both may show a slight difference in the measured value and it is currently unknown which is the most accurate.
Table 2.
Different JLO cutoff values proposed in the literature.
| Reference | Value |
|---|---|
| Babis et al. (77) | JLOAT post-op ≥4° |
| Kim C W et al. (78) | JLOAM post-op >5° |
| Akamatsu et al. (71), Kim et al. (79), Schuster et al. (73), Goshima et al. (9), Sohn et al. (59) | MPTA post-op >95° |
| Rosso et al. (36) | MJLA post-op ≥94° |
| Song et al. (72) | JLOAT post-op ≥4° (predictor inferior KSS) |
| JLOAT post-op ≥6° (predictor inferior KSS and joint space narrowing) |
KSS, Knee Society score.
Some authors prefer the use of the MJLA that does not depend on the floor as a reference point, eliminating the limitation associated with alterations in lower limb adduction/abduction positioning during long-leg radiographs (36). However, it utilizes the JLCA, which, conversely, may be influenced by potential intra-articular changes, and by the impact of weight-bearing status on soft tissues. Furthermore, it turns out to be more complicated to perform and time-consuming. Also, MPTA has the advantage of not being influenced by the position of the lower limbs during the execution of the radiograph. This is because it depends solely on the geometry of the tibia, which remains unchanged in every situation (32). However, as previously stated, from our perspective, the joint line is not a simple geometric entity but rather dynamic. Its influence on knee kinematics is closely related to the position of the tibia relative to the ground, and in this regard, other factors come into play, such as the position of the hip and ankle. Studies of comparison and agreement between the various methods proposed are certainly necessary.
Kim et al. (37) recently proposed a deep learning algorithm to measure various parameters related to knee alignment, including JLOAT, based on long-leg radiographs. They considered over 11 000 radiographs taken with different machines, and 19 landmarks along the entire lower limb were manually defined by two orthopedic surgeons. The measurements obtained showed excellent accuracy and reliability, comparable to those performed by orthopedic specialists, with significant time savings and the ability to measure large volumes. At present, this method still has some limitations, such as operator-dependent landmark identification and the inability to differentiate radiographs with rotational defects. However, with careful development, it can prove to be a game changer in both clinical practice and research, providing extensive data for analysis.
Biomechanical implications of JLO
Osteotomies may lead to the development of secondary deformities, such as excessive JLO. In these cases, the knee can undergo degenerative changes. The risk is related to the amount of shear forces generated and compressive forces discharged in areas not able to absorb them.
In a knee with a normal joint line, the load distribution is determined by the adduction moment, which is the moment acting in the frontal plane during walking (38). Typically, it acts by medially rotating the tibia on the femur and shifting most of the load to the medial compartment, inducing opening of the lateral compartment (39). An increase in the adduction moment has been observed in patients with varus alignment and osteoarthritis, because of the increased flexion-extension moment and muscular forces to compensate for malalignment (40). Furthermore, the generated forces are almost exclusively perpendicular to the joint line, allowing for better dissipation of these forces due to the so-called cushion principle. Excessively oblique joint line results in an increased adduction moment and increased shear forces. This leads to excessive stress on the cartilage and may induce the release of pro-inflammatory cytokines and chondrocyte apoptosis (41). Studies on cadavers have demonstrated that an increase in the joint line causes the femur to slide along the tibial plateau with a mediolateral subluxation, resulting in a shift in areas of higher pressure but not an increase in peak pressures. Femoral translation is greater in the case of a medially tilted joint line. The areas where the load shifts include the intercondylar eminence and the menisci, which act as opposing structures against the sliding of the femoral condyle. The menisci resist a force pushing them out, generating significant stress at the roots and meniscofemoral ligaments. The shift of the load to areas and structures not suitable for absorbing it has been correlated with degenerative changes (11). In a 3D finite element analysis, Nakayama et al. (33) illustrated that an increase in JLO exceeding 5 degrees could potentially result in harmful shear stresses on the articular cartilage, while axial stress does not show significant changes up to 7.5 degrees.
These biomechanical changes are significant, but it has not yet been definitively established how negatively they affect clinical and radiological outcomes.
Knee phenotypes
The understanding of the variability and distribution within the population of coronal alignment has made significant strides in recent years. Efforts have been made to define the constitutional alignment of the healthy population, examining how it differs from the osteoarthritic population, with the aim of customizing surgical treatment and improve clinical and radiological results.
From a population of young healthy individuals, 43 different, clinically relevant, functional knee phenotypes have been described, resulting from the combination of various values of HKA, mLDFA, and mMTPA. The eight most common phenotypes represent two-thirds of the entire population. About half of it has 180 ± 3° HKA, 90 ± 5° mLDFA, and 90 ± 5° mMPTA (42).
The Coronal Plane Alignment of the Knee (CPAK) classification system presents a groundbreaking insight to unveil the intricate relationship between alignment and joint line. To assess constitutional alignment, the system uses LDFA and MPTA measurements. HKA and JLO are determined by calculating their difference and summing values, resulting in nine phenotypes covering different HKA conditions and JLO orientations. The JLO direction is defined as apex distal, neutral, or proximal, representing a medially tilted, neutral, or laterally tilted joint line, respectively. Notably, the neutral value of JLO is fixed at 180° ± 3°, while HKA is fixed at 0° ± 2° (Fig. 4) (43).
Figure 4.
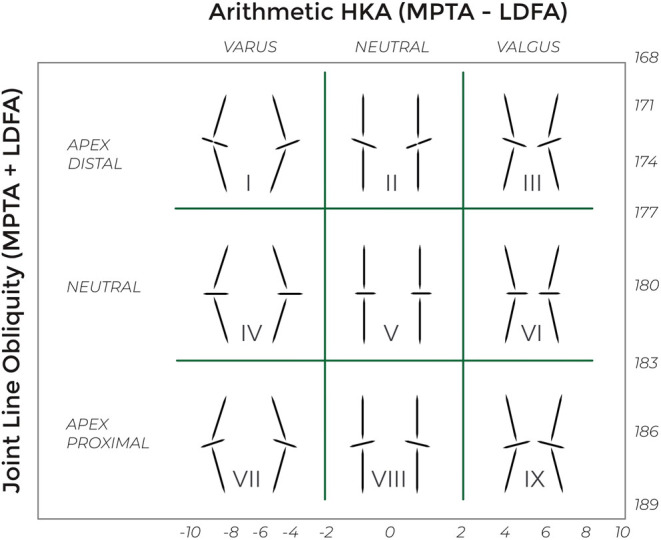
Coronal plane alignment of the knee classification (43). Nine different phenotypes of knee. HKA, hip–knee–ankle angle; JLO, joint line obliquity angle; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Both in healthy individuals and those with arthritis, the most common phenotypes are CPAK type I and CPAK type II. The prevalence varies among different patient groups analyzed in various geographic areas, Indian and Japanese populations have shown a prevalence of CPAK type I above 50%, compared to Caucasian populations with values ranging from 20% to 30% (44). A significant finding is that individuals, both healthy and arthritic, across various populations, typically demonstrate approximately 40% constitutional varus, 40% neutral alignment, and the remaining portion exhibits valgus alignment. While at least two-thirds exhibit an apex distal JLO (43, 44). Varus alignment was more common in men, while neutral and valgus alignment was more common in women (45).
Constitutional varus (HKA <177°) results from increased medial compartment forces during walking or physical activity. This may be linked to delayed medial physis development during growth (15, 46, 47). These individuals show higher tibia vara (MPTA 83.3° ± 2.1°) and lower femoral valgus (LDFA 87.4° ± 1.9°) compared to neutral alignment (MPTA 85.8° ± 2.1° and LDFA 85.7° ± 1.8°) (48). However, this does not equally affect the joint line inclination relative to the ground; the tibia is pushed laterally, maintaining JLO within neutral or slightly medial-tilted ranges (49, 50).
Frontal plane joint line values are impacted by the equation used for measurement. A modified version of the CPAK classification has proposed the use of the following equation: JLO = 90° – (LDFA + MPTA)/2 and enlarged boundaries of HKA between 0° ± 3° for neutral alignment (Fig. 5). According to the authors, this approach takes better account of the deviation of the joint line from the ground. Using this equation, about 30% of the study population shifts from an apex distal to a neutral joint line, with high clinical significance (51).
Figure 5.
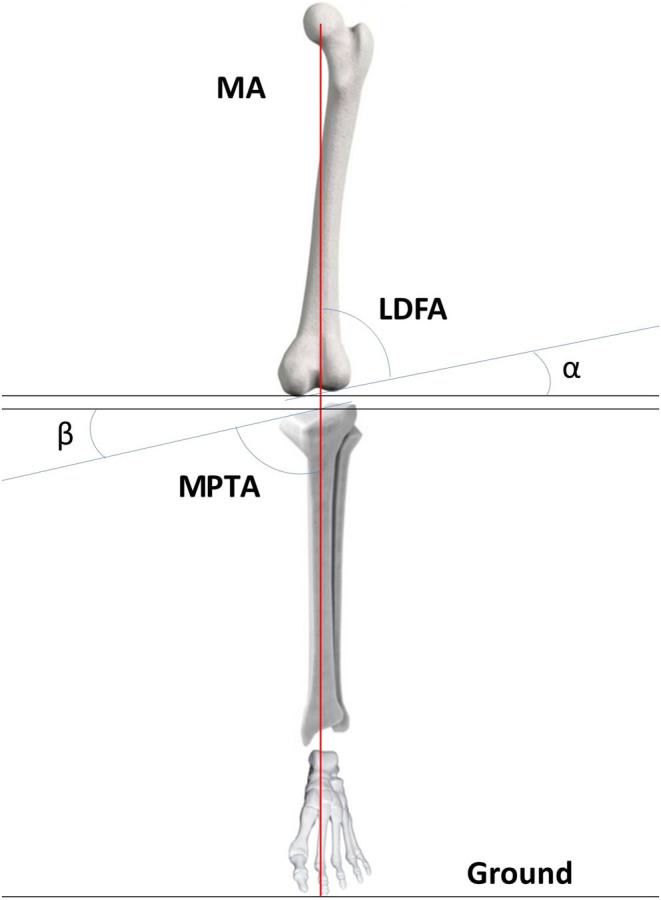
The calculation of the joint line obliquity (JLO) according to Hsu et al. (51). For a neutral knee with an apex distal JLO, having its mechanical axis (MA) vertical to the ground, involves two angles. The α angle is determined as 90° − lateral distal femoral angle (LDFA), and the β angle is calculated as 90° − medial proximal tibial angle (MPTA). Both α and β angles contribute equally to half of the apex distal JLO. Therefore, the JLO to the ground is calculated as JLO = (α + β)/2, which is equivalent to 90° − (LDFA + MPTA)/2.
It should be emphasized that these results are from an Asian population, which might influence them.
The used radiological method does also influence the distribution of knee phenotypes; comparing LLR to a CT-based 3D model shows an increased prevalence of constitutional varus and apex distal JLO with the latter. This is because, on average, lower values are obtained for both MPTA and LDFA with 3D reconstruction, as it allows the identification of the correct points through which weight-bearing occurs, whereas in radiography, one usually relies on the anterior or posterior cortical bone (52). Despite the potential for this modality to correct positioning errors and analyze all planes, it is performed under non-weight-bearing conditions. Consequently, it may not be directly comparable to images obtained through LLR.
Analyzing knee phenotypes guides clinical efforts to restore constitutional alignment for optimal kinematics and soft tissue balance. Considering constitutional varus, which represents the most commonly managed patients, the challenge arises because changes in coronal plane alignment occur during osteoarthritis (53).
Determining the pre-arthritic knee phenotype is still a subject of debate. The use of the contralateral limb has been set aside because alignment correspondence between the right and left sides is not always present (54). Recently, an equation has been proposed that considers all factors influencing phenotype change: Kellgren–Lawrence grade, current CPAK phenotype, LDFA, MPTA, JLO, and JLCA. It has been validated for CPAK phenotypes I and II, which constitute most of the population (55). However, further large-scale studies are needed to validate it comprehensively.
Factors associated with postoperative JLO in medial open wedge proximal tibial osteotomy
The JLO is influenced by a combination of factors rather than a single factor. The correction angle targeted remains the only parameter under the surgeon's control, while the other parameters are predetermined before the surgery.
Preoperative MPTA, LDFA, JLCA, and JLO are all factors associated with an undesirable increase in postoperative JLO. Specifically, JLCA (0° ± 2°) plays a significant role; it represents the angle formed by the tangent to the femoral condyles and the tibial plateau. JLCA progressively increases with the development of unicompartmental osteoarthritis. Therefore, it reflects the wear of the articular surfaces and quantifies the level of deformity resulting from it. It can be used as a classification parameter for the progression of osteoarthritis, like the Ahlbäck and Kellgren–Lawrence classification systems (56). Additionally, JLCA reflects the laxity of surrounding soft tissues, both on the medial and lateral sides (26, 57). Neglecting this parameter causes the degrees of intra-articular deformity which are wrongly attributed to the extra-articular bony component. Therefore, if an overestimated extra-articular deformity is obtained during planning, it will result in a high postoperative MPTA and JLO.
In a multiple logistic regression analysis, it has been demonstrated that an increase in JLCA associated with elevated values of LDFA poses a higher risk of having JLO ≥5°. Specifically, if LDFA ≤87°, JLO remains in normal values for any associated JLCA value. As the LDFA increases, JLO values exceed the threshold at lower JLCA values (58). In another study, it was found that the combination of JLCA ≥5° associated with a preoperative JLO ≥3° results in an almost 80% incidence of having a postoperative MPTA ≥95° (59).
On the other hand, the factors that may influence JLO after MOWPTO are MPTA and changes in hip abduction/adduction and ankle JLO. JLO changes are usually smaller compared to those of MPTA. This is mainly due to a compensatory effect provided by the change in orientation in the ankle joint relative to the ground, facilitated by subtalar joint mobility (60, 61). Following the valgus osteotomy of the proximal tibia, the ankle JLO also transitions from varus to a neutral alignment (62).
Tseng et al. (63) demonstrated through a multiple linear regression analysis that the angle between the tangent to the tibial plateau and the articular surface of the distal tibia (knee ankle joint line angle) is a significant risk factor for elevated JLO. They also established a reference threshold of 9.6°, beyond which the ankle's compensatory ability is nullified, consequently increasing JLO.
After MOWPTO, there is an increase in femoral adduction to ensure proper contact of the foot with the ground. An increase in femoral adduction is positively correlated with changes in JLO. However, it has a less strong effect compared to changes in ankle loading. This is likely due to the distance from the knee and the correction of JLCA, which mitigates femoral adduction (62).
Factors associated with postoperative JLO in DFO
Recently, the lateral closing wedge DFO (LCWDFO) has been proposed for patients with isolated varus deformity (LDFA >90°) to preserve the JLO. In patients primarily affected by femoral deformity, the preoperative JLO is already laterally tilted by about 2° (64); this is a contraindication for performing a MOWPTO. In the literature, there are no defined thresholds for the various radiological parameters analyzed so far. However, Ollivier et al. (65), in a case series of 75 LCWDFO, achieved excellent clinical results without a change in JLO for postoperative LDFA values >85°.
More commonly, DFO is used for valgus malalignment. Medial closing wedge (MCWDFO) and lateral open wedge (LOWDFO) are described, with no evidence of the superiority of either (66). It is important to know that only 24% of valgus deformities are femur-based (67), this increases the risk of obtaining a high JLO if the deformity involves the tibia or is mixed. Wu et al. (68), in a finite element analysis, found that the ideal correction angle for valgus knees is neutral or slightly varus (0° ± 2°). Overcorrection is discouraged as it could lead to increased stress on the medial compartment and accelerate the osteoarthritis process. Schröter et al. (69) have proposed an LDFA threshold between 85° and 90° as a reference, which allows for excellent clinical outcomes compared to LDFA >90°. If it is not feasible to keep LDFA below this threshold in preoperative planning, DLO should be considered.
Role of double-level osteotomy
The goal of implementing a double-level osteotomy for varus and valgus deformity around the knee is to either restore normal anatomy or relieve stress on an affected joint compartment. Simultaneously, the objective is to normalize knee joint angles and orientation. DLO addressing malalignment in both the femur and the tibia is recommended when deformity analysis reveals a substantial misalignment in both bones (Fig. 6).
Figure 6.
Example of double level osteotomy for left varus knee. Lateral closing wedge distal femur osteotomy and medial open wedge proximal tibia osteotomy.
In recent years, it has become popular, especially as an alternative to MOWPTO. The guidelines in use state that DLO should be contemplated when, during the planning of a single-level correction, the resulting JLO >5˚ or the MPTA >95°, and/or predicted wedge size >15 mm (Table 2) (70).
However, these thresholds have been mainly defined based on the worst clinical outcomes observed in some patient cohorts after MOWPTO, without using logistic regression and without excluding potential confounding factors (71, 72, 73). The clinical outcome after osteotomy is multifactorial, influenced by covariates such as age, gender, preoperative knee arthritis, body mass index, preoperative patient-reported outcome, overcorrection of valgus alignment, and JLCA. Additionally, other study groups have not found an association between these thresholds and worse clinical outcomes (9, 74). Biomechanical studies on cadavers, which have contributed to establishing these thresholds, are also subject to criticism (11, 33, 75). In vivo, we do not know the changes that occur and the impact on the degeneration of joint structures. All studies have been conducted in a static environment, while the role of the joint line manifests in vivo during walking.
Analyzing the distribution of JLO values within the healthy population, it is observed to roughly follow the shape of a Gaussian curve centered around JLO values just above zero, with a range approximately from −6° to 6° (50). This can provide information about our target since most individuals have neutral JLO values. Therefore, using these cutoffs can be helpful in restoring alignment as anatomically as possible.
These values individually cannot be considered as an indication for DLO but rather can be regarded as warning signs to thoroughly analyze the complex interplay of all the different parameters. For example, Sohn et al. (59) proposed a treatment algorithm in which he defines DLO as mandatory for preoperative JLO values ≥3° associated with JLCA ≥ 5°. Recently, DLO has been proposed for bifocal valgus knees (MPTA >90° and LDFA <84°). The surgical technique involved patient-specific cutting guide and medial closing wedge osteotomy on both the femur and the tibia. It has proven to be effective and safe without affecting lower limb length or compromising JLO (14). Taylor and Getgood (76) recommended a DLO for knee with valgus over 10° or when the deformity at both distal femur and proximal tibia are present.
Further studies are needed to delve into this topic and potentially develop treatment algorithms which may be stratified based on the specific patient phenotype. Despite these limitations, DLO maintains a leading role in knee realignment procedures and has demonstrated excellent outcomes with a relatively low rate of complications. It has the advantage of easily preserving proper JLO, avoiding extensive corrections on a single bone segment, and facilitating a potential conversion to total knee arthroplasty. The downside includes increased invasiveness, costs, and surgery duration.
Conclusion
The joint line, traditionally viewed as a static geometric measure, is recognized in this review as a dynamic entity influencing knee forces and kinematics. Incorporating modern classification systems for phenotyping coronal alignments in candidates for osteotomies is a progressive step. This allows for a more precise definition of our patients, aids in specifying the intended correction strategy, and enhances the ability to accurately compare results. The challenges in measuring joint line inclination and the associated angles necessitate a comprehensive understanding of the factors influencing these measurements. MPTA, LDFA, JLCA, and hip and ankle joints significantly influence postoperative JLO values.
The DLO emerges as a valuable option, particularly in cases of substantial deformities. However, it should not be based solely on the thresholds established so far for JLO and MPTA.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this instructional lecture.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
References
- 1.Brinkman JM Lobenhoffer P Agneskirchner JD Staubli AE Wymenga AB & van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. Journal of Bone and Joint Surgery 2008901548–1557. ( 10.1302/0301-620X.90B12.21198) [DOI] [PubMed] [Google Scholar]
- 2.Castagnini F Sudanese A Bordini B Tassinari E Stea S & Toni A. Total knee replacement in young patients: survival and causes of revision in a registry population. Journal of Arthroplasty. 2017323368–33. ( 10.1016/j.arth.2017.05.052) [DOI] [PubMed] [Google Scholar]
- 3.Walker-Santiago R Tegethoff JD Ralston WM & Keeney JA. Revision total knee arthroplasty in young patients: higher early reoperation and Rerevision. Journal of Arthroplasty 202136653–656. ( 10.1016/j.arth.2020.08.052) [DOI] [PubMed] [Google Scholar]
- 4.Keeney JA Eunice S Pashos G Wright RW & Clohisy JC. What is the evidence for total knee arthroplasty in young patients? A systematic review of the literature. Clinical Orthopaedics and Related Research 2011469574–583. ( 10.1007/s11999-010-1536-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feucht MJ Winkler PW Mehl J Bode G Forkel P Imhoff AB & Lutz PM. Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surgery, Sports Traumatology, Arthroscopy 2021293299–3309. ( 10.1007/s00167-020-06166-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paley D Herzenberg JE Tetsworth K McKie J & Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthopedic Clinics of North America 199425425–465. ( 10.1016/S0030-5898(2031927-1) [DOI] [PubMed] [Google Scholar]
- 7.Ferreira A Jacquet C Guy S Khakha R Kley K Argenson JN & Ollivier M. Distal femoral osteotomy planning: reversed Miniaci’s method is more accurate than Dugdale and Paley methods. Orthopaedics and Traumatology, Surgery and Research 2024110103697. [DOI] [PubMed] [Google Scholar]
- 8.Ollivier B Berger P Depuydt C & Vandenneucker H. Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surgery, Sports Traumatology, Arthroscopy 2021293569–3584. ( 10.1007/s00167-020-06262-4) [DOI] [PubMed] [Google Scholar]
- 9.Goshima K Sawaguchi T Shigemoto K Iwai S Fujita K & Yamamuro Y. Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy 2019352898–2908.e1. ( 10.1016/j.arthro.2019.04.030) [DOI] [PubMed] [Google Scholar]
- 10.Tsuji M Akamatsu Y Kobayashi H Mitsugi N Inaba Y & Saito T. Joint line convergence angle predicts outliers of coronal alignment in navigated open-wedge high tibial osteotomy. Archives of Orthopaedic and Trauma Surgery 2020140707–715. ( 10.1007/s00402-019-03245-0) [DOI] [PubMed] [Google Scholar]
- 11.Wang D Willinger L Athwal KK Williams A & Amis AA. Knee joint line obliquity causes tibiofemoral subluxation that alters contact areas and meniscal loading. American Journal of Sports Medicine 2021492351–2360. ( 10.1177/03635465211020478) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Babis GC An KN Chao EYS Rand JA & Sim FH. Double level osteotomy of the knee: a method to retain joint-line obliquity. Clinical results. Journal of Bone and Joint Surgery 2002841380–1388. ( 10.2106/00004623-200208000-00013) [DOI] [PubMed] [Google Scholar]
- 13.Schuster P Rathgeb F Mayer P Michalski S Hielscher L Buchholz J Krüger L & Richter J. Double level osteotomy for medial osteoarthritis and bifocal varus malalignment has excellent short-term results while maintaining physiologic radiographic joint parameters. Knee Surgery, Sports Traumatology, Arthroscopy 2023313124–3132. ( 10.1007/s00167-022-07247-1) [DOI] [PubMed] [Google Scholar]
- 14.Pioger C Mabrouk A Siboni R Jacquet C Seil R & Ollivier M. Double-level knee osteotomy accurately corrects lower limb deformity and provides satisfactory functional outcomes in bifocal (femur and tibia) valgus malaligned knees. Knee Surgery, Sports Traumatology, Arthroscopy 2023313007–3014. ( 10.1007/s00167-023-07325-y) [DOI] [PubMed] [Google Scholar]
- 15.Hsu RWW Himeno S Coventry MB & Chao EYS. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clinical Orthopaedics and Related Research 1990255215–227. ( 10.1097/00003086-199006000-00029) [DOI] [PubMed] [Google Scholar]
- 16.Micicoi G Grasso F Kley K Favreau H Khakha R Ehlinger M Jacquet C & Ollivier M. Osteotomy around the knee is planned toward an anatomical bone correction in less than half of patients. Orthopaedics and Traumatology, Surgery and Research 2021107102897. ( 10.1016/j.otsr.2021.102897) [DOI] [PubMed] [Google Scholar]
- 17.Graden NR Dean RS Kahat DH DePhillipo NN & LaPrade RF. True mechanical alignment is found only on full-limb and not on standard anteroposterior radiographs. Arthroscopy, Sports Medicine, and Rehabilitation 20202e753–e759. ( 10.1016/j.asmr.2020.06.010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bardot LP Micicoi G Favreau H Zeman P Khakha R Ehlinger M & Ollivier M. Global varus malalignment increase from double-leg to single-leg stance due to intra-articular changes. Knee Surgery, Sports Traumatology, Arthroscopy 202230715–720. ( 10.1007/s00167-021-06446-6) [DOI] [PubMed] [Google Scholar]
- 19.Ahrend MD Baumgartner H Ihle C Histing T Schröter S & Finger F. Influence of axial limb rotation on radiographic lower limb alignment: a systematic review. Archives of Orthopaedic and Trauma Surgery 20221423349–3366. ( 10.1007/s00402-021-04163-w) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brunner J Jörgens M Weigert M Kümpel H Degen N & Fuermetz J. Significant changes in lower limb alignment due to flexion and rotation-a systematic 3D simulation of radiographic measurements. Knee Surgery, Sports Traumatology, Arthroscopy 2023311483–1490. ( 10.1007/s00167-022-07302-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee NK Kim TW Lee S Choi YS Kang SB & Chang CB. Effect of distance between the feet on knee joint line orientation after total knee arthroplasty in standing full-limb radiographs. Knee Surgery, Sports Traumatology, Arthroscopy 2022303032–3040. ( 10.1007/s00167-021-06662-0) [DOI] [PubMed] [Google Scholar]
- 22.Paley D & Pfeil J. Principles of deformity correction around the knee. Orthopade 20002918–38. ( 10.1007/s001320050004) [DOI] [PubMed] [Google Scholar]
- 23.Miniaci A Ballmer FT Ballmer PM & Jakob RP. Proximal tibial osteotomy. A new fixation device. Clinical Orthopaedics and Related Research 1989. (246) 250–259. ( 10.1097/00003086-198909000-00035). [DOI] [PubMed] [Google Scholar]
- 24.Aygün Ü Bölükbaşı M Yamak K & Çiçek AC. Comparison of the Miniaci and Dugdale techniques on functional outcomes in medial open wedge high tibial osteotomy. Journal of Experimental Orthopaedics 20231086. ( 10.1186/s40634-023-00653-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akasaki Y Mizu-Uchi H Hamai S Tsushima H Kawahara S Horikawa T & Nakashima Y. Patient-specific prediction of joint line convergence angle after high tibial osteotomy using a whole-leg radiograph standing on lateral-wedge insole. Knee Surgery, Sports Traumatology, Arthroscopy 2020283200–3206. ( 10.1007/s00167-019-05821-8) [DOI] [PubMed] [Google Scholar]
- 26.Lee DK Wang JH Won Y Min YK Jaiswal S Lee BH & Kim JY. Preoperative latent medial laxity and correction angle are crucial factors for overcorrection in medial open-wedge high tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2020281411–1418. ( 10.1007/s00167-019-05502-6) [DOI] [PubMed] [Google Scholar]
- 27.Takagawa S Kobayashi N Yukizawa Y Oishi T Tsuji M & Inaba Y. Preoperative soft tissue laxity around knee was associated with less accurate alignment correction after hybrid closed-wedge high tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2020283022–3030. ( 10.1007/s00167-019-05762-2) [DOI] [PubMed] [Google Scholar]
- 28.Micicoi G Khakha R Kley K Wilson A Cerciello S & Ollivier M. Managing intra-articular deformity in high Tibial osteotomy: a narrative review. Journal of Experimental Orthopaedics 2020765. ( 10.1186/s40634-020-00283-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Behrendt P Akoto R Bartels I Thürig G Fahlbusch H Korthaus A Dalos D Hoffmann M Frosch KH & Krause M. Preoperative joint line convergence angle correction is a key factor in optimising accuracy in varus knee correction osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2023311583–1592. ( 10.1007/s00167-022-07092-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferreira A Jacquet C Guy S Khakha R Kley K Argenson JN & Ollivier M. Distal femoral osteotomy planning: reversed Miniaci’s method is more accurate than Dugdale and Paley methods. Orthopaedics and Traumatology, Surgery and Research 2024110103697. ( 10.1016/j.otsr.2023.103697) [DOI] [PubMed] [Google Scholar]
- 31.Capella M Sabatini L Bosco F Barberis L Giustra F Risitano S Camazzola D & Massè A. A novel geometrical planning method to restore knee joint obliquity in double-level osteotomies. Archives of Orthopaedic and Trauma Surgery 20231436685–6693. ( 10.1007/s00402-023-04997-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie T van der Veen HC van den Akker-Scheek I & Brouwer RW. Assessment of joint line obliquity and its related frontal deformity using long-standing radiographs. Journal of Orthopaedics 20234057–64. ( 10.1016/j.jor.2023.04.014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakayama H Schröter S Yamamoto C Iseki T Kanto R Kurosaka K Kambara S Yoshiya S & Higa M. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surgery, Sports Traumatology, Arthroscopy 2018261873–1878. ( 10.1007/s00167-017-4680-x) [DOI] [PubMed] [Google Scholar]
- 34.Lobenhoffer P van Heerwaarden RJ Staubli AE & Jakob RP.. Osteotomies around the Knee Indications-Planning- Surgical Techniques Using Plate Fixators. Switzerland: AO Publishing; 2008. [Google Scholar]
- 35.Mehta N Duryea J Badger GJ Akelman MR Jones MH Spindler KP & Fleming BC. Comparison of 2 radiographic techniques for measurement of tibiofemoral joint space width. Orthopaedic Journal of Sports Medicine 201752325967117728675. ( 10.1177/2325967117728675) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosso F Rossi R Cantivalli A Pilone C & Bonasia DE. Joint line obliquity does not affect the outcomes of opening wedge high tibial osteotomy at an average 10-year follow-up. American Journal of Sports Medicine 202250461–470. ( 10.1177/03635465211059811) [DOI] [PubMed] [Google Scholar]
- 37.Kim SE Nam JW Kim JI Kim JK & Ro DH. Enhanced deep learning model enables accurate alignment measurement across diverse institutional imaging protocols. Knee Surgery and Related Research 2024364. ( 10.1186/s43019-023-00209-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hunt MA Birmingham TB Giffin JR & Jenkyn TR. Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis. Journal of Biomechanics 2006392213–2220. ( 10.1016/j.jbiomech.2005.07.002) [DOI] [PubMed] [Google Scholar]
- 39.Shelburne KB Torry MR & Pandy MG. Contributions of muscles, ligaments, and the ground-reaction force to tibiofemoral joint loading during normal gait. Journal of Orthopaedic Research 2006241983–1990. ( 10.1002/jor.20255) [DOI] [PubMed] [Google Scholar]
- 40.Sharma L Hurwitz DE Thonar EJ Sum JA Lenz ME Dunlop DD Schnitzer TJ Kirwan-Mellis G & Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis and Rheumatism 1998411233–1240. () [DOI] [PubMed] [Google Scholar]
- 41.Smith RL Carter DR & Schurman DJ. Pressure and shear differentially alter human articular chondrocyte metabolism : a review. Clinical Orthopaedics and Related Research 2004427(Supplement) S89–S95. [PubMed] [Google Scholar]
- 42.Hirschmann MT Moser LB Amsler F Behrend H Leclerq V & Hess S. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surgery, Sports Traumatology, Arthroscopy 2019271394–1402. ( 10.1007/s00167-019-05509-z) [DOI] [PubMed] [Google Scholar]
- 43.MacDessi SJ Griffiths-Jones W Harris IA Bellemans J & Chen DB. Coronal Plane Alignment of the Knee (CPAK) classification. Bone and Joint Journal 2021103–B329–337. ( 10.1302/0301-620X.103B2.BJJ-2020-1050.R1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pagan CA Karasavvidis T Lebrun DG Jang SJ MacDessi SJ & Vigdorchik JM. Geographic variation in knee phenotypes based on the coronal plane alignment of the knee classification: a systematic review. Journal of Arthroplasty 2023381892–1899.e1. ( 10.1016/j.arth.2023.03.047) [DOI] [PubMed] [Google Scholar]
- 45.Huber S Mitterer JA Vallant SM Simon S Hanak-Hammerl F Schwarz GM Klasan A & Hofstaetter JG. Gender-specific distribution of knee morphology according to CPAK and functional phenotype classification: analysis of 8739 osteoarthritic knees prior to total knee arthroplasty using artificial intelligence. Knee Surgery, Sports Traumatology, Arthroscopy 2023314220–4230. ( 10.1007/s00167-023-07459-z) [DOI] [PubMed] [Google Scholar]
- 46.Eastwood DM & Sanghrajka AP. Guided growth: recent advances in a deep-rooted concept. Journal of Bone and Joint Surgery 20119312–18. ( 10.1302/0301-620X.93B1.25181) [DOI] [PubMed] [Google Scholar]
- 47.Witvrouw E Danneels L Thijs Y Cambier D & Bellemans J. Does soccer participation lead to genu varum? Knee Surgery, Sports Traumatology, Arthroscopy 200917422–427. ( 10.1007/s00167-008-0710-z) [DOI] [PubMed] [Google Scholar]
- 48.Micicoi G Jacquet C Sharma A LiArno S Faizan A Kley K Parratte S & Ollivier M. Neutral alignment resulting from tibial vara and opposite femoral valgus is the main morphologic pattern in healthy middle-aged patients: an exploration of a 3D-CT database. Knee Surgery, Sports Traumatology, Arthroscopy 202129849–858. ( 10.1007/s00167-020-06030-4) [DOI] [PubMed] [Google Scholar]
- 49.Bellemans J Colyn W Vandenneucker H & Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? the concept of constitutional Varus. Clinical Orthopaedics and Related Research 201247045–53. ( 10.1007/s11999-011-1936-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Victor JMK Bassens D Bellemans J Gürsu S Dhollander AAM & Verdonk PCM. Constitutional varus does not affect joint line orientation in the coronal plane. Clinical Orthopaedics and Related Research 201447298–104. ( 10.1007/s11999-013-2898-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hsu CE Chen CP Wang SP Huang JT Tong KM & Huang KC. Validation and modification of the coronal plane alignment of the knee classification in the Asian population. Bone and Joint Open 20223211–217. ( 10.1302/2633-1462.33.BJO-2022-0001.R1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tarassoli P Corban LE Wood JA Sergis A Chen DB & MacDessi SJ. Long leg radiographs underestimate the degree of constitutional varus limb alignment and joint line obliquity in comparison with computed tomography: a radiographic study. Knee Surgery, Sports Traumatology, Arthroscopy 2023314755–4765. ( 10.1007/s00167-023-07505-w) [DOI] [PubMed] [Google Scholar]
- 53.Colyn W Bruckers L Scheys L Truijen J Smeets K & Bellemans J. Changes in coronal knee-alignment parameters during the osteoarthritis process in the varus knee. Journal of ISAKOS 2023868–73. ( 10.1016/j.jisako.2022.12.002) [DOI] [PubMed] [Google Scholar]
- 54.Beckers L Colyn W Bellemans J Victor J & Vandekerckhove PJ. The contralateral limb is no reliable reference to restore coronal alignment in TKA. Knee Surgery, Sports Traumatology, Arthroscopy 202230477–487. ( 10.1007/s00167-020-06152-9) [DOI] [PubMed] [Google Scholar]
- 55.Colyn W Cleymans A Bruckers L Truijen J Smeets K & Bellemans J. The pre-diseased coronal alignment can be predicted from conventional radiographs taken of the varus arthritic knee. Archives of Orthopaedic and Trauma Surgery 20231434425–4436. ( 10.1007/s00402-022-04709-6) [DOI] [PubMed] [Google Scholar]
- 56.Mabrouk A An JS Glauco L Jacque C Kley K Sharma A & Ollivier M. The joint line convergence angle (JLCA) correlates with intra-articular arthritis. Knee Surgery, Sports Traumatology, Arthroscopy 2023315673–5680. ( 10.1007/s00167-023-07616-4) [DOI] [PubMed] [Google Scholar]
- 57.Park JG Kim JM Lee BS Lee SM Kwon OJ & Bin SI. Increased preoperative medial and lateral laxity is a predictor of overcorrection in open wedge high tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2020283164–3172. ( 10.1007/s00167-019-05805-8) [DOI] [PubMed] [Google Scholar]
- 58.Hiramatsu K Yamada Y Nakamura N & Mitsuoka T. Factors associated with postoperative knee joint line obliquity after medial open wedge high tibial osteotomy. American Journal of Sports Medicine 2022501651–1658. ( 10.1177/03635465221079343) [DOI] [PubMed] [Google Scholar]
- 59.Sohn S Koh IJ Kim MS & In Y. Risk factors and preventive strategy for excessive coronal inclination of tibial plateau following medial opening-wedge high tibial osteotomy. Archives of Orthopaedic and Trauma Surgery 2022142561–569. ( 10.1007/s00402-020-03660-8) [DOI] [PubMed] [Google Scholar]
- 60.Lee JH & Jeong BO. Radiologic changes of ankle joint after total knee arthroplasty. Foot and Ankle International 2012331087–1092. ( 10.3113/FAI.2012.1087) [DOI] [PubMed] [Google Scholar]
- 61.Oh KJ Ko YB Bae JH Yoon ST & Kim JG. Analysis of knee joint line obliquity after high tibial osteotomy. Journal of Knee Surgery 201629649–657. ( 10.1055/s-0036-1571430) [DOI] [PubMed] [Google Scholar]
- 62.Kim SG Jun JB Bae IW & Lee DH. Changes in ankle and hip joints following medial opening-wedge high tibial osteotomy affect knee joint line obliquity. Knee Surgery, Sports Traumatology, Arthroscopy 2023315420–5427. ( 10.1007/s00167-023-07581-y) [DOI] [PubMed] [Google Scholar]
- 63.Tseng TH Wang HY Tzeng SC Hsu KH & Wang JH. Knee-ankle joint line angle: a significant contributor to high-degree knee joint line obliquity in medial opening wedge high tibial osteotomy. Journal of Orthopaedic Surgery and Research 20221779. ( 10.1186/s13018-022-02976-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Park JG Han SB & Jang KM. Association of preoperative tibial Varus deformity with joint line orientation and clinical outcome after open-wedge high tibial osteotomy for medial compartment osteoarthritis: a propensity score-matched analysis. American Journal of Sports Medicine 2021493551–3560. ( 10.1177/03635465211044146) [DOI] [PubMed] [Google Scholar]
- 65.Ollivier M Fabre-Aubrespy M Micicoi G Ehlinger M Hanak L & Kley K. Lateral femoral closing wedge osteotomy in genu varum. Orthopaedics and Traumatology, Surgery and Research 2021107102989. ( 10.1016/j.otsr.2021.102989) [DOI] [PubMed] [Google Scholar]
- 66.Wylie JD Jones DL Hartley MK Kapron AL Krych AJ Aoki SK & Maak TG. Distal femoral osteotomy for the valgus knee: medial closing wedge versus lateral opening wedge: a systematic review. Arthroscopy 2016322141–2147. ( 10.1016/j.arthro.2016.04.010) [DOI] [PubMed] [Google Scholar]
- 67.Eberbach H Mehl J Feucht MJ Bode G Südkamp NP & Niemeyer P. Geometry of the valgus knee: contradicting the dogma of a femoral-based deformity. American Journal of Sports Medicine 201745909–914. ( 10.1177/0363546516676266) [DOI] [PubMed] [Google Scholar]
- 68.Wu Y Jin X Zhao X Wang Y Bai H Lu B Tong X Ma J & Ma X. Computer-aided design of distal femoral osteotomy for the valgus knee and effect of correction angle on joint loading by finite element analysis. Orthopaedic Surgery 2022142904–2913. ( 10.1111/os.13440) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schröter S Konrads C Maiotti M Mederake M Fischer C Ahrend M & Schüll D. In closed wedge distal femur osteotomies for correction of valgus malalignment overcorrection of mLDFA should be avoided. Knee Surgery, Sports Traumatology, Arthroscopy 2023313992–3999. ( 10.1007/s00167-023-07449-1) [DOI] [PubMed] [Google Scholar]
- 70.Alves P van Rooij F Kuratle T Saffarini M & Miozzari H. Consistent indications, targets and techniques for double-level osteotomy of the knee: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy 2022304078–4087. ( 10.1007/s00167-022-06915-6) [DOI] [PubMed] [Google Scholar]
- 71.Akamatsu Y Kumagai K Kobayashi H Tsuji M & Saito T. Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy 2018342158–2169.e2. ( 10.1016/j.arthro.2018.01.055) [DOI] [PubMed] [Google Scholar]
- 72.Song JH Bin SI Kim JM & Lee BS. What is an acceptable limit of joint-line obliquity after medial open wedge high tibial osteotomy? Analysis based on midterm results. American Journal of Sports Medicine 2020483028–3035. ( 10.1177/0363546520949552) [DOI] [PubMed] [Google Scholar]
- 73.Schuster P Geßlein M Schlumberger M Mayer P Mayr R Oremek D Frank S Schulz-Jahrsdörfer M & Richter J. Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and Varus malalignment. American Journal of Sports Medicine 2018461362–1370. ( 10.1177/0363546518758016) [DOI] [PubMed] [Google Scholar]
- 74.Lee KM Chang CB Park MS Kang SB Kim TK & Chung CY. Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis and Cartilage 201523232–238. ( 10.1016/j.joca.2014.11.001) [DOI] [PubMed] [Google Scholar]
- 75.Hooper JM Walker P Hsu TT Kurtz A Reynolds R Hennessy D & Chu A. Biomechanical implications of an oblique knee joint line. Journal of Knee Surgery 201831761–766. ( 10.1055/s-0037-1608821) [DOI] [PubMed] [Google Scholar]
- 76.Taylor S & Getgood A. Genu valgum correction and biplanar osteotomies. Clinics in Sports Medicine 20224147–63. ( 10.1016/j.csm.2021.08.001) [DOI] [PubMed] [Google Scholar]
- 77.Babis GC An KN Chao EYS Larson DR Rand JA & Sim FH. Upper tibia osteotomy: long term results - realignment analysis using OASIS computer software. Journal of Orthopaedic Science 200813328–334. ( 10.1007/s00776-008-1234-6) [DOI] [PubMed] [Google Scholar]
- 78.Kim CW Seo SS Lee CR Gwak HC Kim JH & Jung SG. Factors affecting articular cartilage repair after open-wedge high tibial osteotomy. Knee 2017241099–1107. ( 10.1016/j.knee.2017.06.001) [DOI] [PubMed] [Google Scholar]
- 79.Kim GW Kang JK Song EK & Seon JK. Increased joint obliquity after open-wedge high tibial osteotomy induces pain in the lateral compartment: a comparative analysis of the minimum 4-year follow-up outcomes using propensity score matching. Knee Surgery, Sports Traumatology, Arthroscopy 2021293495–3502. ( 10.1007/s00167-020-06342-5) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a