Abstract
OBJECTIVE:
To examine trends in severe maternal morbidity from 2008 to 2012 in delivery and postpartum hospitalizations among pregnancies conceived with or without assisted reproductive technology (ART).
METHODS:
In this retrospective cohort study, deliveries were identified in the 2008–2012 Truven Health MarketScan Commercial Claims and Encounters Databases. Severe maternal morbidity was identified using International Classification of Diseases, 9th Revision, Clinical Modification diagnosis codes and Current Procedural Terminology codes. Rate of severe maternal morbidity was calculated for ART and non-ART pregnancies. We performed multivariable logistic regression, controlling for maternal characteristics, and calculated adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for severe morbidity. Additionally, a propensity score analysis was performed between ART and non-ART deliveries.
RESULTS:
Of 1,016,618 deliveries, 14,761 (1.5%) were identified as pregnancies conceived with ART. Blood transfusion was the most common severe morbidity indicator for ART and non-ART pregnancies. For every 10,000 singleton deliveries, there were 273 ART deliveries or postpartum hospitalizations with severe maternal morbidity compared with 126 for non-ART (P<.001). For ART singleton deliveries, the rate of severe morbidity decreased from 369 per 10,000 deliveries in 2008 to 219 per 10,000 deliveries in 2012 (P=.025). Odds of severe morbidity were increased for ART compared with non-ART singletons (adjusted OR 1.84, 95% CI 1.63–2.08). Among multiple gestations, there was no significant difference between ART and non-ART pregnancies (rate of severe morbidity for ART 604/10,000 and non-ART 539/ 10,000 deliveries, P=.089; adjusted OR 1.04, 95% CI 0.91–1.20). Propensity score matching agreed with these results.
CONCLUSION:
Singleton pregnancies conceived with ART are at increased risk for severe maternal morbidity; however, the rate has been decreasing since 2008. Multiple gestations have increased risk regardless of ART status.
Severe maternal morbidity is associated with significant health care cost, family burden, and may herald maternal mortality,1 the most tragic event in obstetrics. Previously defined as physical and psychological conditions resulting from or aggravated by pregnancy that have an adverse effect on the woman’s health,1 severe maternal morbidity was found to affect more than 60,000 women in the United States every year and has been steadily increasing since 1998: the rate of deliveries with severe maternal morbidity increased from approximately 70 deliveries per 10,000 in 1998–1999 to 160 deliveries per 10,000 in 2010–2011.2
Several obstetric conditions have been associated with severe maternal morbidity.3,4 In a recent study, odds of severe maternal morbidity were found to be twofold higher in pregnancies complicated by gestational diabetes, more than threefold higher in pregnancies complicated by hypertensive disorders, and more than 58 times higher in the setting of placenta accreta.3 Many studies have linked assisted reproductive technology (ART) to adverse obstetric outcomes including increased risk of gestational diabetes, hypertensive disorders of pregnancy, placenta previa, antepartum hemorrhage, placental abruption, and cesarean delivery.5–7 It is unknown if these associations translate into increased severe maternal morbidity after ART.
The use of ART has doubled over the past decade. In 2013, 1.5% of all neonates born in the United States were conceived with ART.8 Given the growing number of pregnancies conceived after ART, it is pertinent to know if there is an increased risk of severe maternal morbidity in this potentially high-risk population. We compared rates of severe maternal morbidity in ART pregnancies with rates among pregnancies conceived without ART during delivery hospitalizations and postpartum readmissions for singleton and multiple gestation pregnancies.
MATERIALS AND METHODS
We used Truven Health MarketScan Commercial Claims and Encounters Databases, which include longitudinal, deidentified health insurance claims data from large employers and health plans across the United States, to conduct a retrospective cohort study. All women 15 years of age or older who had a delivery hospitalization and were continuously enrolled for at least 1 year before delivery through 42 days after delivery (unless death occurred) between January 1, 2008, and November 19, 2012, were identified by International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes and Current Procedural Terminology (CPT) codes. Deliveries were defined as any inpatient hospital admission record including a pregnancy-related diagnosis or procedure code for vaginal or cesarean delivery identified by the ICD-9-CM codes 650, 669.7, V27.x, or procedure codes 72.0–72.9, 73.22, 73.59, 73.6, 74.0–74.2, 74.4, 74.99; Diagnosis-Related Group codes for vaginal or cesarean delivery, 370–375 for version 24 or earlier, or 765–768, 774, 775 for version 25 and later; and CPT codes 59409, 59612 for vaginal delivery and 59514, 59620 for cesarean delivery. Deliveries were identified as a multiple gestation if one or more of following codes were present: 651.x, V27.2–V27.7, V91.x. A postpartum readmission was defined as any admission to the hospital within 6 weeks (42 days) from the delivery admission date.
We excluded deliveries with ICD-9-CM codes indicating a molar pregnancy (630), spontaneous abortion or termination (631, 632, 634.x–638.x, 69.01, 69.51, 74.91, 75.0; Diagnosis-Related Group 380, 381 for version 24 or earlier, 770, 779 for version 25 and later; or CPT codes 59840, 59841, 59850–59852, 59855–59857), ectopic pregnancy (633.x, Diagnosis-Related Group 378 for version 24 and earlier and 777 for version 25 and later), or complication after an abortion, ectopic, or molar pregnancy (639.x). Deliveries were also excluded if the maternal discharge status was listed as death without any severe morbidity present during the admission. Because death without any severe morbidity is unlikely, we felt these deliveries either had an incorrect discharge status or actually did have severe morbidity that was not captured in the database.
Deliveries were classified as ART if a CPT code was present indicating an ART procedure (CPT 58970, 58974, 58976) within 45 weeks before delivery. All remaining deliveries were considered non-ART. See Appendix 1, available online at http://links.lww.com/AOG/A729, for a list and description of codes used for inclusion and exclusion criteria and ART identification. Because MarketScan is a publicly available database and does not contain direct personal identifiers, review by the Centers for Disease Control and Prevention institutional review board was not needed.
Characteristics of the ART and non-ART groups were compared using Pearson χ2 and Fisher exact tests and included maternal age at delivery, parity, comorbid conditions, history of prior cesarean delivery, plurality, and region of delivery. Comorbidities were identified using ICD-9-CM codes reported within 1 year before delivery, or at the time of delivery, in inpatient or outpatient claims and included tobacco use (305.1, 649.0, V15.82, CPT 99406, 99407), pregestational diabetes (250–250.93 and 648.00–648.04), chronic hypertension (401.0, 401.1, 401.9, 402.00–405.99, 642.0, 642.1, 642.2), pre-existing renal disease (250.4, 403, 404, 405.01, 405.11, 405.91, 585.1–585.6, 585.9), cardiovascular disease (412, 414.0, 414.8, 414.9, 429.2), and obesity (649.1, 278.00, 278.01, 278.03). Women were identified as having a comorbid condition based on the presence of at least one inpatient claim or two or more outpatient claims at least 30 days apart, except for tobacco use and obesity, which were present at much lower rates than expected and were therefore included if only one or more outpatient claim was present. Prior cesarean delivery was identified using the ICD-9-CM code 654.2. See Appendix 1 (http://links.lww.com/AOG/A729) for a list of codes used to identify comorbidities.
Comorbid conditions may have a part in causing severe morbidity. To assess the magnitude of effect comorbid conditions have on severe morbidity and to evaluate potential bias caused by including comorbid conditions as a covariate in adjusted models, we examined the association of severe morbidity and ART separately for those with and without comorbid conditions. We performed a sensitivity analysis restricted to singleton deliveries among women without any comorbid conditions and with at least one comorbid condition.
Severe maternal morbidity was identified by having at least 1 of the 25 previously established list of ICD-9-CM diagnosis and procedure codes (severe maternal morbidity indicators) published by Callaghan et al9 and available on the Centers for Disease Control and Prevention, Department of Reproductive Health web site10 present at the delivery or postpartum readmission. In addition to the published ICD-9-CM codes, we used CPT codes to identify a severe maternal morbidity indicator (see Appendix 2, available online at http://links.lww.com/AOG/A730, for ICD-9-CM and CPT codes). The delivery hospitalization or postpartum readmission also had to meet at least one of the following three criteria to be considered severe maternal morbidity: 1) length of stay equal to or greater than 3 days; 2) discharge status listed as transferred; or 3) discharge status listed as death. This was to exclude less severe complications that likely did not signify severe morbidity.
We calculated rates of having at least one severe maternal morbidity indicator per 10,000 deliveries for ART and non-ART delivery hospitalizations or postpartum readmissions for each year, 2008–2012, and all years combined. Rates were calculated for delivery hospitalizations and postpartum readmissions combined and separately for both singleton and multiple gestation deliveries. For our sensitivity analysis, rates of severe morbidity were calculated for all years combined, 2008–2012, for ART and non-ART singleton deliveries restricted to women without any comorbid conditions and women with at least one comorbid condition. Rates were compared using a Fisher exact test for each year. A Wilcoxon rank-sum test was used to compare the rates between ART and non-ART groups across all years. We then performed linear regression to determine if the rate of severe maternal morbidity significantly increased or decreased for ART and non-ART singleton and multiple gestations from 2008 to 2012. As a result of the large number of comparisons between groups in each statistical comparison, a Holm-Bonferroni correction was applied, resulting in different P values denoting statistical significance for each level of analysis.
Using multivariable logistic regression, we calculated crude and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) to examine which patient factors were associated with severe morbidity. Model fitting for the logistic regression used both backward elimination and forward selection. Multivariable logistic regression was also performed for subgroups of women with and without comorbid conditions, comparing odds of severe morbidity between ART and non-ART singleton deliveries. Variables with P values <.05 were retained in the final model. Finally, to supplement these results, we performed a propensity score match analysis for singleton and multiple deliveries separately. The matching between ART and non-ART deliveries used 11 covariates, year of delivery, and all covariates (excluding ART) in Table 1. To validate the data obtained from the MarketScan databases, two programmers worked independently until results matched. SAS 9.3 and SUDAAN 11 were used for all analyses.
Table 1.
Maternal Characteristics by Assisted Reproductive Technology Status Among Liveborn Deliveries 2008–2012
| Characteristic | Non-ART | ART | P * |
|---|---|---|---|
| Total | 1,001,857 (98.5) | 14,761 (1.5) | |
| Age (y) | <.001 | ||
| Younger than 25 | 147,200 (14.7) | 90 (0.6) | |
| 25–29 | 290,808 (29.0) | 1,599 (10.8) | |
| 30–34 | 344,459 (34.4) | 5,282 (35.8) | |
| 35–39 | 175,954 (17.6) | 5,166 (35.0) | |
| 40–44 | 39,543 (3.9) | 2,174 (14.7) | |
| 45 or older | 3,893 (0.4) | 450 (3.1) | |
| Parity | <.001 | ||
| Nulliparous | 342,860 (34.2) | 7,439 (50.4) | |
| Nonnulliparous | 658,997 (65.8) | 7,322 (49.6) | |
| Comorbid condition | |||
| Tobacco use | 33,966 (3.4) | 159 (1.1) | <.001 |
| Pregestational diabetes | 22,925 (2.3) | 397 (2.7) | .001 |
| Chronic hypertension | 41,136 (4.1) | 741 (5.0) | <.001 |
| Pre-existing renal disease | 819 (0.1) | † | .246 |
| Cardiovascular disease | 289 (0.0) | † | .331 |
| Obesity | 60,851 (6.1) | 772 (5.2) | <.001 |
| Prior cesarean delivery | 165,038 (16.5) | 1,961 (13.3) | <.001 |
| Plurality | <.001 | ||
| Singleton | 980,031 (97.8) | 10,355 (70.2) | |
| Multiple | 21,826 (2.2) | 4,406 (29.8) | |
| Region of delivery | <.001 | ||
| Northeast | 131,407 (13.1) | 3,600 (24.4) | |
| North–central | 251,878 (25.2) | 4,829 (32.7) | |
| South | 419,955 (41.9) | 4,569 (30.9) | |
| West | 183,538 (18.3) | 1,695 (11.5) | |
| Unknown | 15,079 (1.5) | 68 (0.5) |
ART, assisted reproductive technology.
Data are n (%) unless otherwise specified.
Holm-Bonferroni corrected P≤.001 denotes statistical significance of Pearson χ2 and Fisher exact tests.
Not reported owing to small sample size to protect patient confidentiality.
RESULTS
There were 1,016,618 deliveries identified between 2008 and 2012. Of those, 14,761 (1.5%) were classified as ART pregnancies. Women who delivered after ART were more likely to be 35 years old or older and nulliparous than women who did not use ART. They were less likely to use tobacco, be obese, and have a prior cesarean delivery and more likely to have chronic hypertension and reside in the North. Of all ART deliveries, 29.8% were multiple gestations compared with 2.2% of non-ART deliveries (Table 1).
Delivery admissions contributed to the majority (greater than 85%) of severe morbidity indicators for singleton and multiple gestations (Appendix 3, available online at http://links.lww.com/AOG/A731). The number of severe morbidity indicators and rate of severe morbidity were low among postpartum readmissions for singleton and multiple gestation pregnancies regardless of ART (17/10,000 deliveries among non-ART singletons, 29/10,000 deliveries among ART singletons, 44/10,000 deliveries among non-ART multiples, and 54/10,000 deliveries among ART multiples; Appendix 3, http://links.lww.com/AOG/A731). Results from delivery hospitalizations alone were similar to results calculated for delivery hospitalizations or postpartum readmissions combined. No significant difference between ART and non-ART groups was found for either singletons or multiples in any year for postpartum readmissions alone (Appendix 3, http://links.lww.com/AOG/A731). Results are therefore only presented for delivery or postpartum readmissions combined.
Rates for the most commonly reported and statistically significant severe morbidity indicators for ART and non-ART pregnancies are shown in Table 2. The three most common severe morbidities among singleton pregnancies were blood transfusion (36 and 77/10,000 non-ART and ART deliveries, respectively) followed by disseminated intravascular coagulation (20 and 46/10,000 non-ART and ART deliveries, respectively) and mechanical ventilation (18 and 33/10,000 non-ART and ART deliveries, respectively). Among multiple gestations, blood transfusion was most common (215 and 200/10,000 non-ART and ART deliveries, respectively) followed by mechanical ventilation (105 and 143/10,000 non-ART and ART deliveries, respectively) and disseminated intravascular coagulation (68 and 98/10,000 non-ART and ART deliveries, respectively). Singleton ART pregnancies had significantly higher rates of blood transfusion, disseminated intravascular coagulation, acute renal failure, and hysterectomy compared with singleton non-ART pregnancies (P≤.001). Higher rates of internal injuries of the thorax, abdomen, and pelvis and shock were also detected among ART singletons compared with non-ART singletons (P≤.001). Rates between multiple gestation ART and non-ART pregnancies for each indicator were not significantly different.
Table 2.
Rates of Most Commonly Reported and Statistically Significant Severe Maternal Morbidity Indicators and Overall Rate of Any Indicator During Delivery Hospitalizations or Postpartum Readmissions Per 10,000 Deliveries by Assisted Reproductive Technology Status, 2008–2012
| Indicator | Singleton Pregnancies |
Multiple Pregnancies |
||||
|---|---|---|---|---|---|---|
| Non-ART | ART | p * | Non-ART | ART | p * | |
| Blood transfusion | 36 | 77 | <.001 | 215 | 200 | .567 |
| Disseminated intravascular coagulation | 20 | 46 | <.001 | 68 | 98 | .042 |
| Mechanical ventilation | 18 | 33 | .001 | 105 | 143 | .034 |
| Adult respiratory distress syndrome | 12 | 21 | .009 | 49 | 48 | 1 |
| Eclampsia | 11 | 13 | .656 | 34 | 41 | .488 |
| Heart failure during procedure or surgery | 11 | 23 | .001 | 26 | 25 | 1 |
| Hysterectomy | 9 | 27 | <.001 | 38 | 34 | .892 |
| Sepsis | 7 | 15 | .004 | 22 | 32 | .227 |
| Acute renal failure | 6 | 18 | <.001 | 30 | 32 | .881 |
| Puerperal cerebrovascular disorders | 6 | 9 | .324 | 19 | 18 | 1 |
| Operations on heart and pericardium | 6 | 12 | .041 | 21 | 23 | .720 |
| Internal injuries of thorax, abdomen, and pelvis | 3 | 14 | <.001 | 10 | 25 | .018 |
| Shock | 4 | 14 | <.001 | 22 | 16 | .585 |
| Overall | 126 | 273 | <.001 | 539 | 604 | .089 |
ART, assisted reproductive technology.
Data are n unless otherwise specified.
Holm-Bonferroni corrected P≤.001 denotes statistical significance of Pearson χ2 and Fisher exact tests.
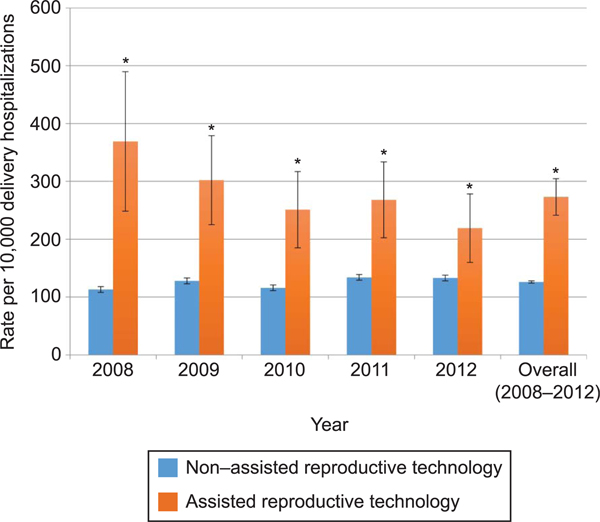
For every 10,000 deliveries for all years combined (2008–2012), there were 273 delivery or postpartum readmissions with at least one severe maternal morbidity indicator for singleton pregnancies conceived after ART compared with 126 for singleton non-ART pregnancies (P<.001). The rate of having at least one severe maternal morbidity indicator per 10,000 deliveries was significantly higher for singleton ART pregnancies compared with singleton non-ART pregnancies for each year, 2008–2012 (P<.001). Considering the entire period, a significant difference between the two groups was detected (Wilcoxon rank-sum test, P=.008) (Fig. 1). Using linear regression, we found the rate of severe maternal morbidity in ART singletons significantly decreased from 369 per 10,000 deliveries in 2008 to 219 per 10,000 deliveries in 2012 (r2=85.2%, P=.025). There was no trend among non-ART singleton deliveries over time with the rate ranging from 113 to 134 per 10,000 deliveries (r2=55.9%, P=.147).
Fig. 1.
Rate of severe maternal morbidity for singleton pregnancies during delivery hospitalization or postpartum readmissions per 10,000 deliveries. *Holm-Bonferroni corrected P≤.001 denotes statistical significance of Fisher exact test for individual years. Wilcoxon rank-sum test P5.008 (Holm-Bonferroni corrected P≤.008 denotes statistical significance) over all years combined.
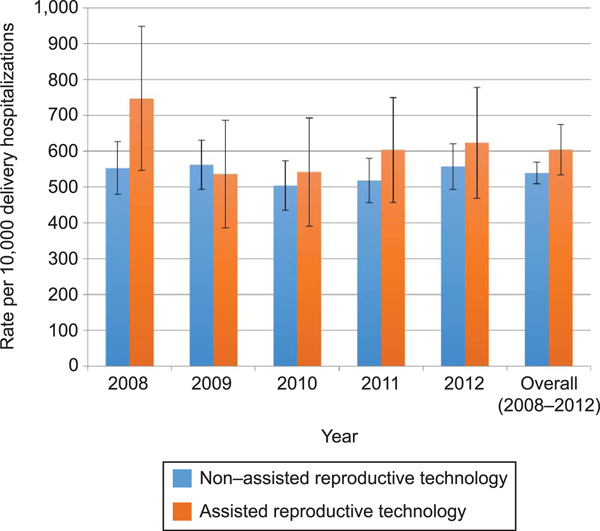
Among multiple gestation pregnancies, the overall rate of having at least one severe maternal morbidity indicator was 604 per 10,000 ART deliveries and 539 per 10,000 non-ART deliveries. Figure 2 shows the rates for multiple gestation pregnancies for each year by ART status. When comparing ART with non-ART deliveries, the rates were not significantly higher in any year or all years combined (Wilcoxon rank-sum test P=.222). Linear regression did not show a significant trend of severe maternal morbidity over time for ART or non-ART multiple gestation pregnancies (ART r2=11.3%, P=.581; non-ART r2=0.1%, P=.724).
Fig. 2.
Rate of severe maternal morbidity for multiple gestation pregnancies during delivery hospitalization or postpartum readmissions per 10,000 deliveries. No statistically significant difference between non–assisted reproductive technology and assisted reproductive technology for any year using Fisher exact test with Holm-Bonferroni corrected P≤.001. Wilcoxon rank-sum test for all years combined P=.222 (Holm-Bonferroni corrected P≤.008 denotes statistical significance).
Patient factors significantly associated with severe morbidity among singleton deliveries are presented in Table 3. ART singletons had significantly higher odds of severe maternal morbidity compared with non-ART singletons after controlling for age, parity, comorbid conditions, prior cesarean delivery, and year of delivery (adjusted OR 1.84, 95% CI 1.63–2.08). Pre-existing renal disease and cardiovascular disease were the factors most strongly associated with severe morbidity (renal disease adjusted OR 5.21, 95% CI 4.20–6.44; cardiovascular disease adjusted OR 5.15, 95% CI 3.54–7.49). Age 35 years or older, nulliparity, pregestational diabetes, chronic hypertension, obesity, and having a prior cesarean delivery were also significantly associated with severe morbidity among singleton deliveries as was age 30–34 years, tobacco use, and selected years of delivery, although the association with these latter factors was weaker.
Table 3.
Odds Ratios and 95% Confidence Intervals for Severe Maternal Morbidity in Delivery and Postpartum Hospitalizations Among Singleton Pregnancies for Selected Characteristics, 2008–2012
| Characteristic | OR (95% CI) | aOR* (95% CI) |
|---|---|---|
| ART | 2.21 (1.96–2.49) | 1.84 (1.63–2.08) |
| Age (y) | ||
| Younger than 25 | Referent | Referent |
| 25–29 | 0.98 (0.92–1.04) | 0.96 (0.90–1.02) |
| 30–34 | 1.14 (1.07–1.2) | 1.08 (1.02–1.14) |
| 35–39 | 1.46 (1.37–1.55) | 1.24 (1.17–1.33) |
| 40–44 | 2.03 (1.87–2.21) | 1.61 (1.48–1.75) |
| 45 or older | 3.54 (2.97–4.21) | 2.64 (2.21–3.15) |
| Nulliparity | 1.21 (1.17–1.26) | 1.29 (1.25–1.34) |
| Tobacco use | 1.18 (1.08–1.29) | 1.14 (1.04–1.25) |
| Pregestational diabetes | 2.11 (1.94–2.30) | 1.32 (1.20–1.44) |
| Chronic hypertension | 3.32 (3.14–3.51) | 2.56 (2.42–2.72) |
| Pre-existing renal disease | 12.38 (10.11–15.16) | 5.21 (4.20–6.44) |
| Cardiovascular disease | 11.63 (8.19–16.51) | 5.15 (3.54–7.49) |
| Obesity | 1.91 (1.81–2.03) | 1.46 (1.38–1.55) |
| Prior cesarean delivery | 1.60 (1.54–1.67) | 1.56 (1.49–1.63) |
| Year | ||
| 2008 | Referent | Referent |
| 2009 | 1.13 (1.07–1.20) | 1.10 (1.04–1.17) |
| 2010 | 1.03 (0.96–1.09) | 0.99 (0.93–1.06) |
| 2011 | 1.18 (1.12–1.25) | 1.13 (1.07–1.20) |
| 2012 | 1.17 (1.10–1.23) | 1.12 (1.05–1.89) |
OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; ART, assisted reproductive technology.
Bold indicates statistically significant aOR.
Each odds ratio is adjusted for all other variables in the table.
Patient factors significantly associated with severe morbidity among multiple gestation deliveries are presented in Table 4. ART was not associated with severe morbidity (adjusted OR 1.04, 95% CI 0.91–1.20). Pre-existing renal and cardiovascular disease was both strongly associated with severe morbidity (renal disease adjusted OR 5.66, 95% CI 2.72–11.79; cardiovascular disease adjusted OR 5.04, 95% CI 1.71–14.87). Age 30 years or older and chronic hypertension were the only other patient factors with increased odds of severe morbidity among multiple gestations (age 30–34 years, adjusted OR 1.36, 95% CI 1.05–1.76; age 35–39 years, adjusted OR 1.50, 95% CI 1.15–1.95; age 40–44 years, adjusted OR 1.93, 95% CI 1.44–2.60; age 45 years or older, adjusted OR 3.19, 95% CI 2.23–4.57; chronic hypertension adjusted OR 1.33, 95% CI 1.09–1.62), whereas having a prior cesarean delivery slightly decreased the odds of severe morbidity (adjusted OR 0.82, 95% CI 0.70–0.96).
Table 4.
Odds Ratios and 95% Confidence Intervals for Severe Maternal Morbidity in Delivery and Postpartum Hospitalizations Among Multiple Gestation Pregnancies for Selected Characteristics, 2008–2012
| Characteristic | OR (95% CI) | aOR* (95% CI) |
|---|---|---|
| ART | 1.13 (0.98–1.29) | 1.04 (0.91–1.20) |
| Age (y) | ||
| Younger than 25 | Referent | Referent |
| 25–29 | 1.18 (0.9–1.54) | 1.19 (0.91–1.55) |
| 30–34 | 1.35 (1.05–1.75) | 1.36 (1.05–1.76) |
| 35–39 | 1.49 (1.15–1.94) | 1.50 (1.15–1.95) |
| 40–44 | 1.93 (1.44–2.59) | 1.93 (1.44–2.60) |
| 45 or older | 3.28 (2.3–4.67) | 3.19 (2.23–4.57) |
| Nulliparity | 1.06 (0.95–1.18) | |
| Tobacco use | 1.2 (0.88–1.64) | |
| Pregestational diabetes | 1.34 (1.00–1.80) | |
| Chronic hypertension | 1.50 (1.24–1.81) | 1.33 (1.09–1.62) |
| Pre-existing renal disease | 7.32 (3.61–14.85) | 5.66 (2.72–11.79) |
| Cardiovascular disease | 6.64 (2.36–18.64) | 5.04 (1.71–14.87) |
| Obesity | 1.20 (0.99–1.46) | |
| Prior cesarean delivery | 0.85 (0.73–1.00) | 0.82 (0.70–0.96) |
| Year | ||
| 2008 | Referent | |
| 2009 | 0.95 (0.80–1.14) | |
| 2010 | 0.87 (0.73–1.04) | |
| 2011 | 0.91 (0.77–1.08) | |
| 2012 | 0.97 (0.82–1.15) |
OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; ART, assisted reproductive technology.
Bold indicates statistically significant aOR.
Each odds ratio is adjusted for all other variables in the table.
In our sensitivity analysis of singleton deliveries among women without comorbidities, the rate of severe morbidity was 109 per 10,000 non-ART deliveries compared with 246 per 10,000 ART deliveries. As expected, this rate was lower than the rate seen Table 3. Odds Ratios and 95% Confidence among singleton deliveries to women with at least one comorbid condition (233/10,000 non-ART deliveries compared with 472/10,000 ART deliveries). The adjusted odds of severe morbidity remained significant for ART deliveries compared with non-ART deliveries for both subgroups and was similar for both groups (adjusted OR without comorbidities 1.86, 95% CI 1.62–2.13; adjusted OR with at least one comorbid condition 1.71, 95% CI 1.31–2.24).
After propensity score matching, there were 858,295 non-ART and 10,323 ART singleton deliveries. ART remained significantly associated with severe maternal morbidity (OR 2.37, 95% CI 2.10–2.67; P<.001). Among multiple gestations, after propensity score matching, there were 18,677 non-ART and 4,289 ART deliveries; the association of ART with severe maternal morbidity was similar to results before matching (OR 1.15, 95% CI 1.00–1.33, P=.05).
DISCUSSION
Severe maternal morbidity can be tragic and may herald impending mortality. We found the odds of severe maternal morbidity from 2008 to 2012 were 1.8 times higher among singleton ART pregnancies compared with non-ART pregnancies during delivery or postpartum readmissions after controlling for maternal age, parity, comorbid conditions, history of prior cesarean delivery, and year of delivery, suggesting that ART is a risk factor for severe morbidity in singleton pregnancies.
An important question is whether increased risk of severe morbidity among ART singleton pregnancies is the result of maternal characteristics and underlying infertility of women seeking treatments or the ART procedures themselves. We found similar odds of severe morbidity in groups with and without comorbidities, thereby suggesting differences in comorbid conditions among ART and non-ART women do not explain the observed association between ART and severe morbidity. A study examining risk of severe morbidity using an infertile population who ultimately conceived without ART is needed to address confounding factors associated with underlying infertility.
We were encouraged by the decreasing rate of severe morbidity among ART singletons over time, from 369 per 10,000 deliveries in 2008 to 219 per 10,000 deliveries in 2012. This trend could be the result of enhanced techniques, protocols, and medications used in ART. Improved gonadotropin antagonist protocols have greatly reduced ovarian hyperstimulation syndrome,11 and there is evidence that supraphysiologic estrogen may alter early placental development predisposing women to conditions such as preeclampsia.12 Practices are changing to include more elective single embryo transfers,8,13 which may decrease growth restriction and preterm birth among singletons.13,14 The mechanism improving perinatal outcomes after elective single embryo transfer may also reduce adverse obstetric conditions such as preeclampsia and placenta previa, ultimately leading to a decrease in severe morbidity. Additionally, characteristics of women seeking ART may be changing, contributing to decreasing risk.
The rate of severe maternal morbidity was more than double among ART multiple gestations and more than four times higher among non-ART multiples compared with ART and non-ART singletons, respectively. Interestingly, rates were not significantly different between ART and non-ART multiple gestations and there was no significant increase in the adjusted odds of severe morbidity. Multiple gestations are at increased risk for many obstetric conditions associated with severe morbidity including gestational diabetes, hypertensive disorders, cesarean delivery, and abruption.15 Furthermore, it is well established that carrying multiples increases the risk of preterm delivery.15 Grobman et al3 found severe maternal morbidity to have an inverse relationship with gestational age at delivery. The increased odds of severe morbidity with preterm delivery may in part explain why both ART and non-ART multiples are at increased risk. Regardless of the etiology, these findings highlight the importance of minimizing multiple gestations when possible, which can be accomplished by elective single embryo transfer with appropriate patient selection.
The strengths of our study include a large, contemporary database with the ability to identify a unique population at risk for severe maternal morbidity. In addition, we were able to control for important maternal characteristics. This study was subject to several limitations. There are inherent limitations when using ICD-9 codes to identify comorbidities and pregnancy conditions and using ICD-9 codes to identify severe morbidity has not been validated against a gold standard such as medical record review. However, there are few true gold standards for severe morbidity, and these are based on expert opinion.16,17 MarketScan is a health insurance claims database; therefore, women who paid for ART out of pocket may have been misclassified. Similarly, a woman who conceived spontaneously after an oocyte retrieval or embryo transfer, but within 45 weeks of delivery, would have been considered an ART delivery. This would have equalized the ART and non-ART groups, however, minimizing differences found. Additionally, MarketScan is not a random sample and results may not generalize to the general population. Data were derived from a commercially insured population; thus, women without insurance, or who were publically insured, were not included. Finally, certain potential confounding variables could not be obtained, including ethnicity and socioeconomic status.
Identifying groups at high risk for severe maternal morbidity is an important step in minimizing its potentially devastating occurrence. The results of this study identify singleton ART pregnancies and multiple gestations as high-risk groups. Although further investigations into the reasons for this increased morbidity are needed, regardless of the etiology, health care providers should optimize maternal health before conception, if possible, to help reduce the risk of severe morbidity. In addition, they should have a heightened awareness for signs of impending severe morbidity throughout pregnancy in these high-risk populations.
Supplementary Material
Acknowledgments
The authors thank the Division of Health Informatics and Surveillance within the Center for Surveillance, Epidemiology, and Laboratory Services for the facilitation of the MarketScan license to the Centers for Disease Control and Prevention.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Callaghan WM, Grobman WA, Kilpatrick SJ, Main EK, D’Alton M. Facility-based identification of women with severe maternal morbidity: it is time to start. Obstet Gynecol 2014; 123:978–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Creanga AA, Berg CJ, Ko JY, Farr SL, Tong VT, Bruce FC,et al. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt) 2014;23:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM,Varner MW, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol 2014;123: 804–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS.Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol 2014;124:771–81. [DOI] [PubMed] [Google Scholar]
- 5.Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update 2012;18:485–503. [DOI] [PubMed] [Google Scholar]
- 6.Smithers PR, Halliday J, Hale L, Talbot JM, Breheny S,Healy D. High frequency of cesarean section, antepartum hemorrhage, placenta previa, and preterm delivery in in-vitro fertilization twin pregnancies. Fertil Steril 2003;80:666–8. [DOI] [PubMed] [Google Scholar]
- 7.Schieve LA, Cohen B, Nannini A, Ferre C, Reynolds MA,Zhang Z, et al. A population-based study of maternal and perinatal outcomes associated with assisted reproductive technology in Massachusetts. Matern Child Health J 2007;11:517–25. [DOI] [PubMed] [Google Scholar]
- 8.Assisted reproductive technology (ART). 2014. Available at: http://www.cdc.gov/art/. Retrieved March 15, 2015.
- 9.Callaghan WM, Creanga AA, Kuklina EV. Severe maternalmorbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012;120:1029–36. [DOI] [PubMed] [Google Scholar]
- 10.Severe maternal morbidity in the United States. 2013. Available at: http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/Severematernalmorbidity.html. Retrieved January 24, 2015.
- 11.de Ziegler D, Gambone JC, Meldrum DR, Chapron C. Riskand safety management in infertility and assisted reproductive technology (ART): from the doctor’s office to the ART procedure. Fertil Steril 2013;100:1509–17. [DOI] [PubMed] [Google Scholar]
- 12.Imudia AN, Awonuga AO, Doyle JO, Kaimal AJ, Wright DL,Toth TL, et al. Peak serum estradiol level during controlled ovarian hyperstimulation is associated with increased risk of small for gestational age and preeclampsia in singleton pregnancies after in vitro fertilization. Fertil Steril 2012;97:1374–9. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg ML, Boulet S, Kissin D, Warner L, Jamieson DJ.Elective single embryo transfer trends and predictors of a good perinatal outcome—United States, 1999 to 2010. Fertil Steril 2013;99:1937–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Sutter P, Delbaere I, Gerris J, Verstraelen H, Goetgeluk S,Van der Elst J, et al. Birthweight of singletons after assisted reproduction is higher after single- than after double-embryo transfer. Hum Reprod 2006;21:2633–7. [DOI] [PubMed] [Google Scholar]
- 15.American College of Obstetricians and Gynecologists. Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Practice Bulletin No. 144. Obstet Gynecol 2014;123: 1118–32. [DOI] [PubMed] [Google Scholar]
- 16.You WB, Chandrasekaran S, Sullivan J, Grobman W. Validation of a scoring system to identify women with near-miss maternal morbidity. Am J Perinatol 2013;30:21–4. [DOI] [PubMed] [Google Scholar]
- 17.Geller SE, Rosenberg D, Cox SM, Kilpatrick S. Defining a conceptual framework for near-miss maternal morbidity. J Am Med Womens Assoc 2002;57:135–9. [PubMed] [Google Scholar]
- 18.Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol 2006;194: 992–1001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.