Abstract
Background
Mental health problems, and major depression in particular, are important public health issues. Following trends in the prevalence of major depression is difficult because of the costs and complications of diagnostic interviews and general population self-report health surveys. Scandinavian countries, however, have several central, population-based health registries. We aimed to investigate how well these registries capture the epidemiology of major depression in the population.
Methods
In two Norwegian regional surveys of general population health, each repeated after 10 years, responders were asked to report depressive symptoms using the Hopkins Symptom Checklist (HSCL) or the Hospital Anxiety and Depression Scale (HADS). Data were linked to three central health registries capturing contact with primary care, specialist care and prescriptions for antidepressants, to investigate how well these registries reflected self-reported depressive symptoms.
Results
Most responders scored low on Hopkins Symptom Checklist (HSCL) and the Hospital Anxiety and Depression Scale (HADS), but 10% and 13%, respectively, scored above cut-off, with only minor changes between the two survey times. Females scored higher than males. Older people scored lower than younger, and a social gradient was visible. Around 12% of those who scored above the cut-off on either scale were recorded in the central health registries during the following year. This correlation was highest in primary care data, followed by prescription data and lowest in specialist care. Females were more often recorded in registries (p < 0.001), as were younger people (p < 0.001).
Conclusions
There was a strong association between scores on screening for major depression in the general population surveys and being recorded in central health registries. There was a low sensitivity of these registries. and there was some variation in how sensitive the central health registries were in picking up depression, especially for males and older people. However, the stability of the measures over time suggests we may get an impression of the prevalence of major depression in the general population by using data from the central health registries. A combination of primary care data, prescription data and specialist care data have a higher sensitivity.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-18754-w.
Introduction
Severe mental health disorders, major depression, and anxiety disorders account for a sizable and potentially increasing part of non-communicable diseases and form a disproportionately high burden of disease in all regions of the world. According to Global Health Estimates for the WHO European Region these disorders accounted for 29% of non-fatal disease burden (years lived with disability) and 15% of total disease burden (disability-adjusted life years; DALYs) [1]. However, these figures do not capture the full consequences of these disorders. They contributed heavily to as many as 141 000 deaths attributed to self-harm in the European Region in 2016 [2]. Furthermore, people with severe mental disorders and drug use disorders have a much higher average mortality compared to the general population, which translates to a reduction in life expectancy of 10–15 years [3]; these premature deaths are most commonly due to unrecognized and untreated physical health conditions [4, 5].
It is vital in the work on prevention and treatment of non-communicable diseases that we have reliable estimates of the occurrence of mental health disorders. Major depression is one of the most common disorders with a life-time prevalence of 5–17% [6]. The prevalence varies between groups: traditionally, more depressive symptoms are reported by females than by males [7–9], and more females than males are diagnosed with [10] and treated for [11] major depression, although this can vary [12]. Several studies have shown social gradients in depressive symptoms with lower socio-economic status (SES) being associated with more depressive symptoms [13, 14]. Still a study from Denmark found that higher socio-economic status predicts more use of antidepressants [15], while the reverse has been shown in Norway [16, 17]. It has also been debated whether the threshold for reporting mental health issues has changed over time [18]. There have been reports of increasing trends for reporting depressive symptoms, especially in females and at least in adolescents [19–21]. Furthermore, some studies have reported an increase in diagnosis [22] and treatment of major depression [23, 24], but this is not true for all studies [12, 25].
Unfortunately, data on mental health disorders are difficult to collect [26]. One approach is to perform population-based diagnostic interviews trying to capture the prevalence. However, such surveys are arduous, costly, and potentially have high attrition rates resulting in different forms of selection bias. Only a few such studies have been performed in Norway [8, 9, 23, 27].
An alternative approach is to conduct general population health surveys, using self-report questionnaires, rather than diagnostic tools. These are easier and cheaper to administer [28]. Although self-reporting of mental discomfort and depressive symptoms is not the same as having a mental health or depressive disorder [29], there are several validated self-report instruments for depressive symptoms with set cut-offs for major depression with established sensitivity and specificity. Two examples are the Hopkins Symptom Checklist (HSCL – referred to below as Hopkins) and the Hospital Anxiety and Depression Scale (HADS). Several studies have shown that they also tap into clinically valid information. Using Hopkins with a cut-off of 1.85 gives a sensitivity of 0.89 and a specificity of 0.98 for major depressive disorder [30]. Using HADS with a cut-off of 6 gives a sensitivity of 0.88 and a specificity of 0.70, the more optimal cut-off being 8 or 11 [31]. Although they cost less, such surveys are not performed in the whole population on a regular basis, so they are not ideal for ongoing estimates of prevalence.
An alternative, in Scandinavian countries, could be using national health registries and databases with nationwide coverage to provide estimates, as this information is already collected. Norway has several registries that could provide information about non-communicable diseases in general and major depression specifically. The Norwegian Control and Payment of Health Reimbursements Database, is an administrative register that covers treatment contacts in primary health care [32]. We refer to this below as the “primary care database”. the Norwegian Prescription Database (NorPD) covers prescriptions dispensed outside of institutions [33]. This is referred to below as “the prescription database”. The Norwegian Patient Registry (NPR) covers all treatment contacts in specialised health care [32], so this is referred to below as “the specialist care registry”. These registries offer readily available large data sets with full coverage and possibly less bias than surveys, but they are “shallow” in that they do not include much clinical detail or desired control variables [34]. Furthermore, the large discrepancy between symptoms reported and depression care received known from international [35] and national [36] research may imply that these registries do not represent the true morbidity in the population. Investigations have shown that only 36% of patients with major depressive disorder have been recorded for this in primary care and only 15% in specialised health care [36]. So, we need to find out how these registries may reflect the real illness levels in their target populations. Some groups may be better represented, and other groups less well.
In this study, we wanted to explore how well three of the central administrative/health registries in Norway – the primary care database, the prescription database, and the specialist care treatment registry – reflect the morbidity caused by major depression in the population. This was done by linking self-report of depressive symptoms in population-based health surveys to data from the health registries. We ask the following questions:
What is the level of self-reported depressive symptoms in population-based surveys, and does this level differ between age groups, sexes, or socioeconomic groups or over time?
What are the recodings of cases of depression found in population-based surveys in the central health registries, and does this differ between age groups, sexes or socioeconomic groups or over time?
Materials and methods
Health survey data
Data were retrieved from four different Norwegian population based health presented here by name (and year for data collection): two waves of the Tromsø Study, Tromsø6 (2007-08) and Tromsø7 (2015-16), and two waves of the Trøndelag Health Study, HUNT3 (2006-08) and HUNT4 (2017-19). All these surveys are comprehensive general population health surveys based in urban and rural areas of northern and central Norway targeting the resident adult population. Both Tromsø surveys included adults 40–70 years of age and both HUNT surveys included adults 20–79 years of age.
From all responders in the Tromsø6 and Tromsø7 surveys, the score on the Hopkins Symptom Checklist 10-item version was noted. HSCL-10 is a measure of psychological distress [37], and is a shorter version of the Hopkins checklist, which performs almost as well as the longer versions [30]. The HSCL-10 asks the respondent about symptoms related to anxiety and depression over the past week on a scale of 1 (not at all) to 4 (extremely). The mean score is calculated, producing a range of scores from 1 to 4 where higher score corresponds to more psychological distress. An average score ≥ 1.85 has commonly been considered a cut-off to identify cases [30]. HSCL-10 consists of two factors – depression and [38, 39] anxiety. For this study the five items covering depression were included. Only those responding to all five questions were included, no imputation was performed.
For all the responders in the two population surveys HUNT3 and HUNT4 responses for the Hospital Anxiety and Depression Scale (HADS) were recorded. HADS is a 14-item scale measuring self-reported anxiety and depression, where the scale goes from 0 to 3. There is a reliable two factor structure of the instrument [40], with items 2, 4, 6, 8, 10, 12 and 14 tapping depression (HADS-D). From these seven questions a sum score was calculated. Usually, three cut-offs are set for HADS-D: ≥5 for mild depression, ≥8 for moderate depression and ≥ 11 for severe depression [41]. To enable a comparable rate for depression with HSCL we used a HADS cut-off score of 7 or more as indicative of depression. Only those responding to all seven questions were included. No imputation was performed.
Data from central health registries
The data from the four population-based surveys – Tromsø6, Tromsø7, HUNT3 and HUNT4 - were linked with data from three national databases and registries; the Norwegian Control and Payment of Health Reimbursements Database (the primary care database) 2006–2020, the Norwegian Prescription Database 2004–2020, and the Norwegian Patient Registry (specialist care registry) 2008–2020 using the Norwegian 11-digit unique person-identifier, encrypted. Codes for identification of outcome and their interpretation (wording) are given in Table 1. We looked for records in the registries 0-365 days after the date of the health survey symptom scores.
Table 1.
Overview of the central health registries and diagnostic codes used
| Register | Codes | Interpretation/wording |
|---|---|---|
| Norwegian Control and Payment of Health Reimbursements Database (CPHR – the primary care database) | ||
| ICPC-2 | P73, P76 | Affective disorder, Depressive disorder |
| ICD-10 | F32-F34 | Depressive episode, recurrent depressive disorder, persistent mood (affective) disorder |
| Norwegian Prescription Database (NorPD) | ||
| Drug ATC-codes | N06A* | Antidepressants |
| Reimbursement codes ICD-10 | F32-F34, -F3 | Affective disorders needing treatment, Affective disorders |
| Reimbursement codes ICPC-2 | P73, P76, -73 | |
| Diagnosis recorded in Norwegian Patient Registry (NPR – the specialist care registry) | ||
| ICD-10 | F32-F34 | Depressive episode, recurrent depressive disorder, persistent mood (affective) disorder |
* any digit after this, indicating all antidepressants
The primary care database is an administrative database that registers all claims from primary health care providers (doctors, psychologists, physiotherapists, etc.) in Norway from 2006 onwards. The database has full national coverage and all primary health care physicians send their claims to the Norwegian authorities. From the primary care database, we included all patients who were given an ICPC-2 diagnosis of a depressive disorder P73 or P76 or an ICD-10 diagnosis of F32-34 at least once. For the Tromsø6 and the HUNT3 surveys – because these were earlier - we only had 1 year of data available from the primary care database.
In the prescription database (available from 2004 onwards) we only registered those prescriptions for antidepressants (ATC-code N06A*) that included a reimbursement code for depression (any combination of ICD-10 codes -F3 and F32-F34 or ICPC-2 codes − 73, P73, and P76; Table 2), to avoid including prescriptions of antidepressants for other reasons. To ensure that these were, in fact, used for depression, we only included as outcome those who received at least two prescriptions between 90 and 365 days apart. For the 1-year window, at least one of the two prescriptions had to be within the window.
Table 2.
Overview of the Norwegian population surveys included
| Survey | Years performed | Age range | Screening instrument used | Number of invitees | Number (%) with complete data |
|---|---|---|---|---|---|
| Tromsø6 | 2007-08 | 40–79 years of age | 5 items from HSCL-10 | 11,899 | 10,991 (92.4%) |
| Tromsø7 | 2015-16 | 40–79 years of age | 5 items from HSCL-10 | 21,082 | 19,423 (92.1%) |
| HUNT3 | 2006-08 | 20–79 years of age | 7 items from HADS | 41,184 | 37,560 (91.2%) |
| HUNT4 | 2017-19 | 20–79 years of age | 7 items from HADS | 42,053 | 38,560 (91.7%) |
Abbreviations: HSCL: Hopkin’s Symptom Checklist; HADS: Hospital Anxiety and Depression Scale; HUNT: Health Survey of Nord-Trøndelag County
The specialist care registry (NPR) covers all treatment of patients in specialised health care in Norway, with full national coverage since 2008. From the specialist care registry, we included all patients who were given an ICD-10 diagnosis of F32-F34 at least once.
Background variables
Data on included ages, screening instruments for depressive symptoms, number of invitees and responders (and rates) are given in Table 2. Background variables included in the study were age, sex, and socio-economic status. Socio-economic status was measured by level of education and income by linking to data provided by Statistics Norway. Education was stratified into primary (12 years), secondary (15 years) and tertiary (≥ 16 years), and income into quartiles of household income per consumption unit, where the number of consumption units was computed according to the OECD modified scale which assigns a value of 1 to the household head, of 0.5 to each additional adult and of 0.3 to each child [42]. The quartiles were computed for the total Norwegian population per calendar year, sex, and 10-year age group (20–29, 30–39,…,70+).
Statistical analysis
For the later surveys (Tromsø7 and HUNT4), we computed relative risks (RRs) for being recorded in one of the three health registries 0-365 days after the survey date, using uni- and multivariate Poisson regressions with robust variance estimates. The variables included in the regression models were the psychological distress HSCL/HADS score (above limit yes/no), age (continuous, per 10-year increment), sex (male/female), education (low/medium/high), income quartile (q1, q2, q3, q4), the last category being the reference for each categorical variable. Analyses were performed using R version 4.0.3.
Results
Response to general health survey questions on depressive symptoms
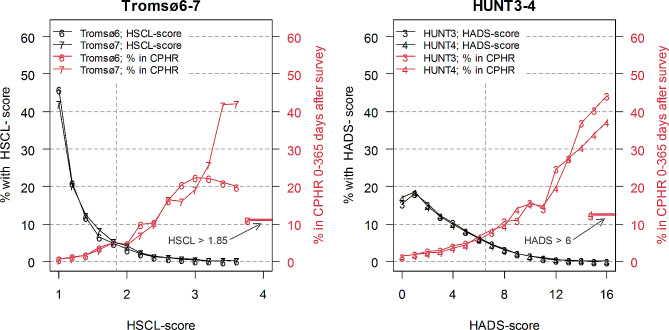
Figure 1 shows that most people scored low on both the Tromsø (panel A) and the HUNT (panel B) population surveys, with minor changes between the two time points at which each of these surveys was repeated. The distribution of both Hopkins HCSL-10 (Tromsø6 and 7) and HADS (HUNT3 and 4) scores were skewed heavily towards the left, or to lower scores. This was most obvious in the Tromsø surveys which used the Hopkins HCSL-10 scoring instrument. In Table 3 we see an increase in the number who scored above cut-off from the Tromsø6 (2007-08) to the Tromsø7 (2015-16) survey (9.6–11.4%; change of 1.8 [95% CI 1.0, 2.5]), while the number of responders scoring above cut-off showed a slight decrease from HUNT3 (2006-08) to HUNT4 (2017-19) (from 13.9 to 13.5%; change of -0.4; [-0.9, 0.1]). For the Tromsø studies, there was an overweight of females scoring above cut-off, while for the HUNT surveys there was an overweight of males. Table 3 (and supplementary figure S1) shows the age distribution of respondents who reported depressive symptoms above cut-off. In the HUNT Study, the score versus age was reversed with the elderly having the highest share above cut-off in the 2006-08 study, but the youngest in the 2017-19 survey. In the Tromsø surveys, there was a similar trend over time but less pronounced. There was a strong social gradient for reporting depressive symptoms above cut-off with those who had lower socio-economic status (both education and income) more often scoring above cut-off. This gradient was more pronounced in the HUNT surveys and when using income – rather than education - as determinant of socio-economic status.
Fig. 1.
The distribution of scores (in percentage of the whole sample) on HSCL (average of 5 depression items, with a cut-off at an average score of > 1.85) in Tromsø6 and 7 (left panel) and HADS-D (sum of 7 depression items, with a cut-off score sum score of 7 or more) in HUNT3 and 4 (right panel). Both panels also show the share of responders that are found in the CPHR (primary care database) with an ICPC-2 diagnosis P73 or P76 or an ICD-10 diagnosis F32, F33 or F34 within 1 year after the survey. Black lines represent the earliest surveys, red lines the latest surveys. The included age span in Tromsø is 40–79 years, and in HUNT 20–79 years
Table 3.
Number and proportion of those scoring above cut-off in the population surveys on HSCL or HADS and the share of these that are found in different central health registries 0-365 days after symptom scores
| Early surveys (Tromsø6 and HUNT3) | Late surveys (Tromsø7 and HUNT4) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study area | Group | Represented in (%) | |||||||||
| N a | Scoring above cut-off (%) | Recorded in CPHR (%) | N* | Scoring above cut-off (%) | CPHR | NorPD | NPR | Any | |||
| Tromsø | All | All | 10,991 | 9.6 | 11.0 | 19,423 | 11.4 | 11.2 | 8.7 | 3.9 | 16.1 |
| Sex | Female | 5662 | 11.8 | 12.4 | 10,140 | 13.3 | 12.4 | 9.2 | 3.9 | 17.4 | |
| Male | 5329 | 7.3 | 8.7 | 9283 | 9.3 | 9.3 | 7.8 | 3.9 | 14.2 | ||
| Age (years) | 40–49 | 3262 | 10.4 | 12.7 | 5829 | 13.2 | 13.4 | 8.6 | 5.2 | 18.2 | |
| 50–59 | 2322 | 10.9 | 13.0 | 5926 | 13.9 | 12.5 | 8.1 | 3.8 | 16.6 | ||
| 60–69 | 3775 | 8.5 | 9.4 | 5067 | 9.1 | 8.0 | 9.1 | 3.0 | 13.4 | ||
| 70–79 | 1632 | 9.0 | 7.5 | 2601 | 6.1 | - | 10.7 | - | 11.3 | ||
| Education | Low | 2433 | 12.4 | 10.6 | 2968 | 13.6 | 8.9 | 12.9 | 2.5 | 17.4 | |
| Medium | 4554 | 9.8 | 9.2 | 7048 | 11.5 | 9.7 | 6.7 | 3.0 | 13.5 | ||
| High | 3992 | 7.8 | 14.2 | 9356 | 10.6 | 13.3 | 8.7 | 5.2 | 17.8 | ||
| Income | q1 | 1892 | 16.1 | 12.8 | 2639 | 20.6 | 13.8 | 12.1 | 5.3 | 21.1 | |
| q2 | 2881 | 10.0 | 12.5 | 5038 | 12.9 | 12.7 | 9.4 | 4.3 | 17.9 | ||
| q3 | 3219 | 7.9 | 9.1 | 6044 | 9.4 | 10.7 | 6.8 | 3.5 | 13.8 | ||
| q4 | 2981 | 7.0 | 9.1 | 5679 | 7.9 | 6.3 | 5.8 | 2.2 | 10.3 | ||
| HUNT | All | All | 37,560 | 13.9 | 12.4 | 38,560 | 13.5 | 12.7 | 12.8 | 3.7 | 20.5 |
| Sex | Female | 20,969 | 12.5 | 16.3 | 22,034 | 12.6 | 16.4 | 16.0 | 4.7 | 25.7 | |
| Male | 16,591 | 15.6 | 8.5 | 16,526 | 14.6 | 8.6 | 9.2 | 2.5 | 14.6 | ||
| Age (years) | 20–29 | 2655 | 7.2 | 19.4 | 3532 | 15.0 | 17.0 | 11.0 | 6.4 | 21.6 | |
| 30–39 | 4682 | 9.5 | 18.9 | 4413 | 14.8 | 18.8 | 10.2 | 6.7 | 22.3 | ||
| 40–49 | 7612 | 12.3 | 15.6 | 6185 | 13.7 | 15.8 | 11.7 | 5.1 | 22.0 | ||
| 50–59 | 9149 | 14.6 | 14.5 | 8214 | 12.9 | 12.8 | 12.4 | 4.0 | 20.8 | ||
| 60–69 | 8501 | 15.6 | 9.0 | 9074 | 12.1 | 10.8 | 14.2 | 1.9 | 19.8 | ||
| 70–79 | 4961 | 19.6 | 6.7 | 7142 | 14.0 | 5.9 | 15.5 | 0.7 | 18.1 | ||
| Education | Low | 7368 | 19.8 | 11.7 | 5181 | 19.3 | 12.1 | 14.5 | 3.3 | 22.5 | |
| Medium | 18,898 | 14.2 | 12.0 | 18,219 | 14.0 | 10.8 | 12.6 | 2.5 | 18.8 | ||
| High | 11,244 | 9.5 | 14.6 | 15,051 | 10.6 | 16.4 | 12.4 | 5.7 | 22.3 | ||
| Income | q1 | 8873 | 17.9 | 14.9 | 6612 | 20.5 | 15.0 | 14.8 | 4.3 | 24.4 | |
| q2 | 11,852 | 13.9 | 11.8 | 11,489 | 14.3 | 12.7 | 13.7 | 3.4 | 21.4 | ||
| q3 | 10,067 | 12.2 | 10.7 | 11,614 | 11.5 | 11.6 | 10.7 | 3.8 | 17.9 | ||
| q4 | 6700 | 10.7 | 11.5 | 8802 | 9.6 | 11.0 | 11.4 | 3.1 | 17.0 | ||
Abbreviations: HSCL: Hopkin’s Symptom Checklist; HADS: Hospital Anxiety and Depression Scale; HUNT: Health Survey of Nord-Trøndelag County; CPHR: Norwegian Control and Payment of Health Reimbursements Database; NorPD: Norwegian Prescription Database; NPR: Norwegian Patient Registry
a) N with missing education in Tromsø6/7, HUNT3/4: 15, 55, 52, 115; N with missing income in Tromsø6/7, HUNT3/4: 21, 32, 97, 88
Recordings in central health registries
Around 12% of those who scored above cut-off in either the Tromsø or the HUNT population surveys were found in the primary care database. This was the case for both the early and later surveys (Table 3). The rate of being recorded in the primary care database was closely and positively related to scores on the Hopkins and HADS scales (Fig. 1). There was no difference in the proportion recorded in the primary care database between the first survey and the second in either study, in the unadjusted or adjusted analysis (Table 4). More females than males were found in the primary care database, with only marginal developments over time. The sex difference was larger in the HUNT studies. There was an inverted age gradient of similar magnitude in the Tromsø and HUNT surveys. The higher the age, the lower the proportion recorded in the primary care database (Table 5). This was maintained over the two waves (supplementary figure S1).
Table 4.
Relative risk of being recorded in CPHR (the primary care database) 0-365 days after symptom scores in later study compared to earlier study for those scoring above cut-off
| Found in CPHR (unadjusted) | Found in CPHR (adjusted a) | ||||||
|---|---|---|---|---|---|---|---|
| Ref | RR | 95%CI | p-value | RR | 95%CI | p-value | |
| Tromsø | |||||||
| Later study | Earlier study = 1 (ref) | 0.99 | (0.80–1.22) | 0.927 | 1.12 | (0.91–1.37) | 0.289 |
| HUNT | |||||||
| Later study | Earlier study = 1 (ref) | 0.98 | (0.88–1.08) | 0.635 | 1.11 | (1.00-1.22) | 0.050 |
Abbreviations: CPHR: Norwegian Control and Payment of Health Reimbursements Database; RR: Relative risk; HUNT: Health Survey of Nord-Trøndelag County
a) adjusted for HSCL/HADS score (continuous), age (continuous; 40–79 years of age in Tromsø and 20–79 years of age in HUNT), sex, education (3 levels), and income quartile
Table 5.
Binary poisson regression analysis for the risk of being recorded in central health registries (CPHR, NorPD, NPR or any). Data are given as relative risk (RR) and with a p-value. 95% confidence intervals for the RR can be found in supplementary table S1
| Found in central health registries (unadjusted) | Found in central health registries (adjusted a) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CPHR | NorPD | NPR | Any | CPHR | NorPD | NPR | Any | ||||||||||
| Ref. | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Tromsø7 | |||||||||||||||||
| HSCL (Above limit) | No | 8.46 | (7,10–10,07) | 6.14 | (5,11 − 7,38) | 11.86 | (8,52 − 16,52) | 7.23 | (6,30 − 8,29) | 6.79 | (5,64 − 8,16) | 5.48 | (4,53 − 6,64) | 10.10 | (7,17 − 14,23) | 6.10 | (5,29 − 7,04) |
| Age (10 years) | Cont. | 0.68 | (0,62 − 0,74) | 0.98 | (0,90 − 1,07) | 0.74 | (0,62 − 0,88) | 0.81 | (0,76 − 0,87) | 0.77 | (0,69 − 0,84) | 1.10 | (1,00–1,20) | 0.89 | (0,74 − 1,08) | 0.91 | (0,85 − 0,98) |
| Sex | Male | 1.83 | (1,52 − 2,21) | 1.69 | (1,39 − 2,05) | 1.72 | (1,22 − 2,42) | 1.69 | (1,46 − 1,96) | 1.56 | (1,30 − 1,89) | 1.48 | (1,21 − 1,79) | 1.42 | (1,00–2,01) | 1.47 | (1,27 − 1,70) |
| Education (medium) | High | 0.83 | (0,68 − 1,02) | 1.02 | (0,82 − 1,26) | 0.66 | (0,45 − 0,95) | 0.90 | (0,77 − 1,06) | 0.82 | (0,67 − 1,00) | 0.89 | (0,71 − 1,10) | 0.60 | (0,41 − 0,88) | 0.84 | (0,71 − 0,99) |
| Education (low) | High | 0.91 | (0,70 − 1,18) | 1.54 | (1,21 − 1,97) | 0.72 | (0,44 − 1,19) | 1.23 | (1,01–1,49) | 0.78 | (0,60 − 1,02) | 1.15 | (0,90 − 1,47) | 0.57 | (0,34 − 0,95) | 0.99 | (0,82 − 1,21) |
| Income, q3 | q4 | 1.42 | (1,06 − 1,90) | 1.34 | (1,00–1,79) | 1.51 | (0,90 − 2,54) | 1.39 | (1,11 − 1,75) | 1.28 | (0,96 − 1,71) | 1.31 | (0,98 − 1,76) | 1.41 | (0,84 − 2,36) | 1.31 | (1,05 − 1,64) |
| Income, q2 | q4 | 2.35 | (1,78 − 3,09) | 2.08 | (1,57 − 2,74) | 2.21 | (1,34 − 3,64) | 2.21 | (1,78 − 2,74) | 1.91 | (1,45 − 2,51) | 1.83 | (1,37 − 2,42) | 1.80 | (1,09 − 2,97) | 1.86 | (1,50 − 2,31) |
| Income, q1 | q4 | 3.84 | (2,90 − 5,08) | 3.14 | (2,36 − 4,19) | 3.65 | (2,18 − 6,10) | 3.47 | (2,79 − 4,33) | 2.52 | (1,88 − 3,37) | 2.20 | (1,63 − 2,98) | 2.42 | (1,43 − 4,10) | 2.35 | (1,87 − 2,95) |
| HUNT4 | |||||||||||||||||
| HADS (above limit) | No | 4.66 | (4,24 − 5,13) | 3.56 | (3,25 − 3,89) | 6.90 | (5,64 − 8,45) | 3.82 | (3,56 − 4,10) | 4.54 | (4,12 − 5,01) | 3.43 | (3,13 − 3,76) | 6.82 | (5,54 − 8,39) | 3.68 | (3,42 − 3,95) |
| Age (10 years) | Cont. | 0.82 | (0,80 − 0,85) | 1.14 | (1,10 − 1,17) | 0.71 | (0,67 − 0,76) | 0.99 | (0,97 − 1,01) | 0.85 | (0,83 − 0,88) | 1.15 | (1,12 − 1,18) | 0.75 | (0,70 − 0,80) | 1.01 | (0,99 − 1,03) |
| Sex | Male | 1.89 | (1,69 − 2,10) | 1.86 | (1,68 − 2,05) | 1.77 | (1,41 − 2,21) | 1.85 | (1,71 − 2,00) | 1.86 | (1,67 − 2,07) | 2.03 | (1,84 − 2,23) | 1.63 | (1,30 − 2,05) | 1.94 | (1,79 − 2,09) |
| Education (medium) | High | 0.84 | (0,76 − 0,94) | 1.32 | (1,20 − 1,47) | 0.59 | (0,47 − 0,74) | 1.09 | (1,01–1,18) | 0.86 | (0,77 − 0,95) | 1.15 | (1,03 − 1,28) | 0.63 | (0,50 − 0,79) | 1.02 | (0,94 − 1,11) |
| Education (low) | High | 1.09 | (0,94 − 1,26) | 1.99 | (1,76 − 2,26) | 0.95 | (0,71 − 1,28) | 1.57 | (1,42 − 1,74) | 0.89 | (0,77 − 1,04) | 1.42 | (1,24 − 1,62) | 0.79 | (0,58 − 1,08) | 1.21 | (1,09 − 1,34) |
| Income, q3 | q4 | 1.16 | (0,99 − 1,35) | 1.12 | (0,97 − 1,28) | 1.21 | (0,88 − 1,65) | 1.15 | (1,02 − 1,28) | 1.13 | (0,97 − 1,31) | 1.08 | (0,94 − 1,24) | 1.17 | (0,86 − 1,59) | 1.11 | (1,00–1,25) |
| Income, q2 | q4 | 1.58 | (1,37 − 1,83) | 1.47 | (1,29 − 1,68) | 1.33 | (0,98 − 1,81) | 1.54 | (1,39 − 1,72) | 1.45 | (1,25 − 1,68) | 1.32 | (1,16 − 1,51) | 1.19 | (0,88 − 1,62) | 1.40 | (1,26 − 1,56) |
| Income, q1 | q4 | 2.07 | (1,77 − 2,41) | 2.05 | (1,79 − 2,36) | 1.91 | (1,39 − 2,63) | 2.09 | (1,87 − 2,33) | 1.68 | (1,44 − 1,96) | 1.63 | (1,41 − 1,88) | 1.48 | (1,08 − 2,05) | 1.68 | (1,50 − 1,88) |
Abbreviations: CPHR: Norwegian Control and Payment of Health Reimbursements Database (primary care database); NorPD: Norwegian Prescription Database; NPR: Norwegian Patient Registry (specialist care database); RR: Relative risk; HSCL: Hopkin’s Symptom Checklist; HADS: Hospital Anxiety and Depression Scale; q: quartile
a) adjusted for HSCL/HADS score, age (40–79 years of age in Tromsø and 20–79 years of age in HUNT), sex, educational level and income
Overall, above cut-off responders were recorded more often in the primary care database than in the prescription database, and least often in the specialist care registry (Table 3). More responders from the later HUNT4 survey who scored above the cut-off were found in at least one of the registries after one year than responders with scores above cut-off in the later Tromsø7 survey (20.5% vs. 16.1%; difference of 4.4 [2.5, 6.3]). This difference was mostly explained by more recordings in the prescription database, where 50% more of those above cut-off were treated with antidepressants in the HUNT4 survey than the Tromsø7 survey.
Scoring above cut-off on the Hopkins scale (the Tromsø surveys) was associated with more than 6 times the risk of being recorded in one of the central health registries, ranging from about 6 times risk for being given a diagnosis in primary health care or receiving a prescription for an antidepressant to a more than 10 times risk of being treated for depression in specialist care (Table 5). Scoring above cut off on the HADS-scale (HUNT surveys) showed similar patterns of increase but of a lower magnitude.
Females who scored above the cut-off in the population surveys were more often recorded in the central health registries than males (p < 0.001) (Tables 3 and 5 and S1). This difference was more pronounced in HUNT4 than in Tromsø7 for registration in any of the central health registries within one year, and also in each of the single registries. An exception was a similar rate of recordings for both sexes in the prescriptions database in Tromsø7 (3.9%).
In Tromsø7 and HUNT4, the likelihood of receiving help for depression in primary care (CPHR) and/or specialist care (NPR) decreased with increasing age, while the likelihood of drug treatment increased with increasing age (Table 5 and S1).
In Tromsø7 and HUNT4, the likelihood of receiving primary and/or specialist care for depression increased with increasing educational level, while the likelihood of drug treatment decreased with increasing education. With regard to income, higher income was associated with depression care and drug treatment (Tables 3 and 5).
The specificity of the central health registries for major depression seemed to be high (supplementary table S2), with values above 0.92 for all groups and studies. The sensitivity of the health registries was, however, low with values ranging from very low (0.01–0.07) in the specialist care registry to low (0.08–0.19) in the primary care database. The highest sensitivity was found when combining all three registries, which captured 11–26% of the major depression, the lowest values among older males in the Tromsø7 and the highest sensitivity among younger females in the HUNT4.
Discussion
This study aimed to investigate how well central health registries – covering primary and secondary health care and a prescription database – reflected self-reported depressive symptoms in the general population. Ten to 13% of the responders scored above cut-off for depression on the screening instruments in the general population, with an overweight of females and young respondents. About 12% of those who scored above cut-off were recorded in the central health registries, more often in the primary care database than in the prescription database and least often in the specialist care registry. In the registries, females and younger people were more often represented. However, the stable proportion of self-reported cases which are also found in the central health registries indicates that these registries are well suited to following the epidemiology of major depression in the population over time.
Depression prevalence in the population studies
We investigated depressive symptoms in two different general population studies in Norway, which were each carried out at two different time points. We found that the average depression symptom score remained constant, with approximately 12% of the population scoring above the set cut-off. Females scored higher than males when using the Hopkins scale (HSCL-10), but not with HADS. There was a strong age gradient, with fewer older people having high scores in either survey and at both times. The exception was the inverse relationship in the earlier HUNT3 survey, which may indicate a changed association between age and depression over time [21]. There was also a strong social gradient in the scoring of depressive symptoms, where those with lower socio-economic status scored higher than those with higher socio-economic status.
Eleven per cent of the population scored above cut-off for HCSL-10 and 14% above cut-off for HADS. With the known specificities of HSCL and HADS of 0.98 and 0.70 [30, 31, 43], respectively, and with a sensitivity of 0.88–0.89, this would indicate a point prevalence of 10–11% of the population had major depression. This is very close to the population-based surveys conducted previously in Norway [36, 44] and in other countries [39, 45, 46].
A higher female score on the Hopkins scale (HSCL-10) [47] and higher depression prevalence [7] has been found in many studies. The lack of sex difference in the HADS scale may be because the items included in HADS are more weighted towards the psychological aspects and less for the physical aspects of depression [48], moderating the sex difference [49].
An earlier HUNT publication showed that the prevalence of depressive symptoms increased with age in the 1990s [50]. In data from HUNT3, this distribution is still present, while in both surveys from Tromsø and the later HUNT4 survey this age gradient had changed significantly in the direction of a greater prevalence of depressive symptoms in young adults, reducing into adult age and lowest in the elderly [21]. Again, the psychometric properties of HSCL vs. HADS may have influenced the results in the Tromsø surveys vs. HUNT4, but not the difference found between HUNT3 and HUNT4. It seems to be a new trend that younger people report more symptoms of mental distress, and this finding is replicated in many newer surveys [51], but we do not know for certain how well these reports reflect a true increase in depressive symptoms.
Lastly, irrespective of how socio-economic status was measured, there was a significant social gradient with lower socio-economic groups reporting more depressive symptoms. This is a common finding across different studies [52, 53]. Traditionally Norway is a country with low economic differences, but a slight increase in these differences may be an important finding [54].
Recordings in central health registries
There was a clear correlation between the increasing depression scores in the general population surveys and increased recordings in central health registries. This dose-response relationship shows the validity of using central health registries to monitor changes in trends of major depression in the population. As would be expected, more people were recorded in the primary care registry than in the prescription database, and fewest in the specialist care registry. Being recorded in any of the three health registries captured substantially more than any of the health registries alone. The specificity of the central health registries was overall very high, but the sensitivity of the registries was low, indicating that they do not reveal the true prevalence of major depression in the population.
The figures for recordings in central health registries the following year were 11–12% in the primary care database and around 4% in the prescriptions database. A twin study based on diagnostic interviews and national registry data concluded that 6.9% and 2.8% of the patients with major depression were also found in primary care and secondary care registries, respectively, over a period of approximately 3 years [36]. In our study, we included a slightly wider range of diagnoses from the primary care and prescription databases, which may have contributed to the higher numbers. Also, we used screening instruments which are not designed for diagnostic purposes. The known sensitivities and specificities of HSCL and HADS for major depression give a positive predictive value of scoring above cut-off as low as 30% [30, 31, 43]. Only if we were to set cut-off as high as 3 on HSCL or 14 on HADS (resulting in a dramatically reduced sensitivity) [30] would we get a treatment frequency comparable to that found in the diagnostic based population surveys [36]. The falling proportion of records from the primary care registry to the prescription registry and lastly to the specialist care registry appears natural, as many people with depression are followed up and treated in primary health care [12] and not everyone with depressive symptoms is treated with drugs. Even fewer are referred to specialist care. The exception here is the HUNT4 Survey where more people were treated with antidepressants than were given a diagnosis of depression in primary care. Even if we have information about the indication for prescribing, we may not be able to exclude all those receiving antidepressant prescriptions for other indications, such as anxiety, insomnia, or anorexia [55].
Females were more often recorded than males in all central health registries. This is similar to studies which have found that females more often seek help for mental health problems [56], and are more often prescribed antidepressants in general [11], even if results are more mixed for antidepressants prescribed for major depression [17]. This may still be of concern because of the negative health consequences, such as suicide, which more often follow self-reported mental distress in males [57].
For age, we saw two competing trends: fewer recordings in patient registries (primary or specialist care) but more prescriptions for major depression with increasing age. Other studies have similarly found an increased use of antidepressants later in life [15]. When socio-economic status was measured by educational level we saw the same competing trends, with a lower proportion recorded in patient registries (primary or specialist care) for those with lower educational level, while this group was more often prescribed antidepressant drugs. For socio-economic status measured by income, this phenomenon was not present. Lower income was associated with a higher number of recordings in all central health registries. The clearer association between income and recordings in central health registries could be due to mental health problems affecting ability to hold a steady job. There was also a clear higher rate of being recorded in the prescription database in the HUNT area, suggesting that the use of drugs shows local variations [10].
Using health registries to monitor depression in the population
In some ways, this study assumes that scores above cut-off in general population surveys represent the true prevalence of major depression. This assumption is certainly not fully valid. Firstly, not everybody will participate in such surveys. Depressed patients and people with low socioeconomic status are less likely to respond [21, 58]. Secondly, a high score on the HSCL and HADS scales may not represent a true major depression, even if we have chosen to use only those items most related to major depression. Short-term crises or events in life, that should not be seen or treated as major depression, could lead to high scores on these instruments.
Strengths and limitations
In this study, we wanted to investigate the usefulness of central health registries in picking up major depression in the general population. This involves some challenges. Firstly, there has over time been a declining response rate in general population surveys. Previously, response rates could be above 80%, but in the current studies there was only a 65% attendance rate in the Tromsø studies [59] and around 54% in the HUNT studies [21]. Secondly, and related to this, there may be a selection bias, with those who have poorer health less likely to respond [60]. In this study, we found differences between sexes, age groups and across socio-economic status that could reflect such biases [11, 15, 47]. Thirdly, there may be reporting bias that differs between groups [61]. Fourthly, and related to the central health registries, we have demonstrated that far from all self-reported depressed patients were recorded in these the year following the survey. This could, in part, be due to under-treatment [36]. We opted to use certain diagnoses as outcomes (F32-34 from ICD-10 and ICPC P73 and P76 from ICPC), but arguments could be made for leaving out F34 and P73, as they are more related to bipolar disorder. However, there are limited instances of these diagnoses and it did not change the results if they were taken out. Also, we do not know how self-reported mental health problems are related to “the true” level of mental health problems, as the self-report instruments used are not diagnostic and may pick up on phenomena other than major depression. We saw, for example, that males and those with higher socio-economic status were less often recorded in the central health registries. Even if neither the population health surveys, nor the central health registries represent “a gold standard” for the prevalence of major depression in the population, this study still suggests some sort of stability over time in these registries. This makes it possible to use the central health registries to make estimates of the proportion of the population that will need treatment for mental health problems, and it makes it possible to track changes over time if other important assumptions do not change [62].
Conclusion
In conclusion, this study - using data both from population self-report health surveys and central health registries - does not indicate any significant change in the average prevalence of major depression in the Norwegian population, but does suggest a change in the age distribution. The validity of self-report depression scoring instruments and data from central health registries align with previous research on the occurrence of depressive disorders.
The study illustrates a close relationship between score on either the HSCL or HADS scale in general population surveys and records in central health registries, be it in primary care, by filling prescriptions for antidepressants or in specialist care. Even if there is a low sensitivity of the registries and there is some group variation in how sensitive the central health registries are for picking up major depression, the stability of the measures over time indicates that following a combination of primary care data, prescription data and specialist care data from the central health registries may give a valid impression of the prevalence in the general population.
Combining data from population studies and central health registries could also have clinical implications. Our study highlighted the finding that people with depressive symptoms who have low educational level or who are older are more rarely recorded in central health registries, showing that they have fewer treatment consultations, even though they are more often treated with antidepressant drugs.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
NCDNOR is a research project aiming at establishing new knowledge in the prevention of non-communicable diseases by combining non-communicable disease endpoints across somatic disciplines, examining effects of socio-economic circumstances, health behaviours, biological markers, and mental health throughout the life-course [63].
The Trøndelag Health Study (HUNT) is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU), Trøndelag County Council, Central Norway Regional Health Authority, and the Norwegian Institute of Public Health.
The Tromsø Study as a cohort has, since 1974, been supported by several institutions and funding agencies, mostly the University of Tromsø, now UiT The Arctic University of Norway, but also The Northern Norway Regional Health Authority Medical Programme, and supported by grants from, inter alia, the Norwegian Research Council.
Abbreviations
- CPHR
Norwegian Control and Payment of Health Reimbursements Database – “the primary care database”
- DALY
Disability-adjusted life year
- HADS
Hospital Anxiety and Depression Scale
- HSCL
Hopkins Symptom Checklist
- HUNT
Trøndelag Health Study
- ICD-10
International classification of disease version 10 (WHO)
- ICPC-2
International classification of primary care (WHO)
- NCD
Noncommunicable diseases
- NorPD
Norwegian Prescription Database – “the prescription database”
- NPR
Norwegian Patient Registry – “the specialist care registry”
- SES
Socio-economic status
- WHO
World Health Organization
Author contributions
All the auhtors have contributed equally to the idea, drafting, writing and final approvement of the manuscript.
Funding
Open access funding provided by Norwegian Institute of Public Health (FHI). The project is partly funded by The Research Council of Norway project NO: 319705/10.
Open access funding provided by Norwegian Institute of Public Health (FHI)
Data availability
The datasets used and/or analysed during this study are available from the corresponding author only after application has been made to and permission given by the ethics committee.
Declarations
Ethics approval and consent to participate
This a sub-study in the project A life-course approach to prevent noncommunicable diseases in an aging population - NCDNOR, approved by the Regional Committee for Medical and Health Research Ethics of South-Eastern Norway 2019/1203. Informed consent was obtained from all those participating in the general population surveys. The research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Health statistics and information systems. WHO Global Health estimates, 2000–2016. editor. Geneva: World Health Organization; 2018. WHO.
- 2.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of Disease Study 2010. Lancet. 2013;382(9904):1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 3.Plana-Ripoll O, Pedersen CB, Agerbo E, Holtz Y, Erlangsen A, Canudas-Romo V, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827–35. doi: 10.1016/S0140-6736(19)32316-5. [DOI] [PubMed] [Google Scholar]
- 4.Heiberg IH, Nesvåg R, Balteskard L, Bramness JG, Hultman CM, Naess Ø, et al. Diagnostic tests and treatment procedures performed prior to cardiovascular death in individuals with severe mental illness. Acta Psychiatr Scand. 2020;141(5):439–51. doi: 10.1111/acps.13157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heiberg IH, Jacobsen BK, Nesvåg R, Bramness JG, Reichborn-Kjennerud T, Næss Ø, et al. Total and cause-specific standardized mortality ratios in patients with schizophrenia and/or substance use disorder. PLoS ONE. 2018;13(8):e0202028. doi: 10.1371/journal.pone.0202028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, et al. A Comprehensive Nationwide Study of the incidence rate and lifetime risk for treated Mental disorders. JAMA Psychiatry. 2014;71(5):573–81. doi: 10.1001/jamapsychiatry.2014.16. [DOI] [PubMed] [Google Scholar]
- 7.Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult DSM-5 major depressive disorder and its Specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–46. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158(7):1091–8. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- 9.Kringlen E, Torgersen S, Cramer V. Mental illness in a rural area: a Norwegian psychiatric epidemiological study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):713–9. doi: 10.1007/s00127-006-0080-0. [DOI] [PubMed] [Google Scholar]
- 10.Balinskaite V. Trends and geographical variation in antidepressant prescribing in primary care in England: a descriptive analysis. Lancet. 2019;394:S21. doi: 10.1016/S0140-6736(19)32818-1. [DOI] [Google Scholar]
- 11.Thunander Sundbom L, Bingefors K, Hedborg K, Isacson D. Are men under-treated and women over-treated with antidepressants? Findings from a cross-sectional survey in Sweden. BJPsych Bull. 2017;41(3):145–50. doi: 10.1192/pb.bp.116.054270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruths S, Haukenes I, Hetlevik Ø, Smith-Sivertsen T, Hjørleifsson S, Hansen AB, et al. Trends in treatment for patients with depression in general practice in Norway, 2009–2015: nationwide registry-based cohort study (the Norwegian GP-DEP Study) BMC Health Serv Res. 2021;21(1):697. doi: 10.1186/s12913-021-06712-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lund J, Andersen AJW, Haugland SH. The social gradient in stress and depressive symptoms among adolescent girls: a systematic review and narrative synthesis. Norsk Epidemiologi. 2019;28(1–2).
- 14.Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 15.Hansen DG, Søndergaard J, Vach W, Gram LF, Rosholm JU, Mortensen PB, et al. Socio-economic inequalities in first-time use of antidepressants: a population-based study. Eur J Clin Pharmacol. 2004;60(1):51–5. doi: 10.1007/s00228-003-0723-y. [DOI] [PubMed] [Google Scholar]
- 16.von Soest T, Bramness JG, Pedersen W, Wichstrøm L. The relationship between socio-economic status and antidepressant prescription: a longitudinal survey and register study of young adults. Epidemiol Psychiatr Sci. 2012;21(1):87–95. doi: 10.1017/S2045796011000722. [DOI] [PubMed] [Google Scholar]
- 17.Hansen AB, Baste V, Hetlevik O, Haukenes I, Smith-Sivertsen T, Ruths S. GPs’ drug treatment for depression by patients’ educational level: registry-based study. BJGP Open. 2021;5(2). [DOI] [PMC free article] [PubMed]
- 18.Gagné T, Henderson C, McMunn A. Is the self-reporting of mental health problems sensitive to public stigma towards mental illness? A comparison of time trends across English regions (2009-19). Soc Psychiatry Psychiatr Epidemiol. 2022:1–10. [DOI] [PMC free article] [PubMed]
- 19.Torikka A, Kaltiala-Heino R, Rimpelä A, Marttunen M, Luukkaala T, Rimpelä M. Self-reported depression is increasing among socio-economically disadvantaged adolescents – repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. 2014;14(1):408. doi: 10.1186/1471-2458-14-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keyes KM, Gary D, O’Malley PM, Hamilton A, Schulenberg J. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol. 2019;54(8):987–96. doi: 10.1007/s00127-019-01697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krokstad S, Weiss DA, Krokstad MA, Rangul V, Kvaløy K, Ingul JM, et al. Divergent decennial trends in mental health according to age reveal poorer mental health for young people: repeated cross-sectional population-based surveys from the HUNT study, Norway. BMJ Open. 2022;12(5):e057654. doi: 10.1136/bmjopen-2021-057654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Proudman D, Greenberg P, Nellesen D. The growing Burden of Major Depressive disorders (MDD): implications for researchers and policy makers. PharmacoEconomics. 2021;39(6):619–25. doi: 10.1007/s40273-021-01040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sivertsen B, Knudsen AKS, Kirkøen B, Skogen JC, Lagerstrøm BO, Lønning K-J et al. Prevalence of mental disorders among Norwegian college and university students: a population-based cross-sectional analysis. Lancet Reg Health - Europe. 2023:100732. [DOI] [PMC free article] [PubMed]
- 24.Sclar DA, Robison LM, Schmidt JM, Bowen KA, Castillo LV, Oganov AM. Diagnosis of depression and use of antidepressant pharmacotherapy among adults in the United States: does a disparity persist by ethnicity/race? Clin Drug Investig. 2012;32(2):139–44. doi: 10.2165/11598950-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Kendrick T, Stuart B, Newell C, Geraghty AW, Moore M. Did NICE guidelines and the Quality outcomes Framework change GP antidepressant prescribing in England? Observational study with time trend analyses 2003–2013. J Affect Disord. 2015;186:171–7. doi: 10.1016/j.jad.2015.06.052. [DOI] [PubMed] [Google Scholar]
- 26.Clark HW, Power AK, Le Fauve CE, Lopez EI. Policy and practice implications of epidemiological surveys on co-occurring mental and substance use disorders. J Subst Abuse Treat. 2008;34(1):3–13. doi: 10.1016/j.jsat.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 27.Knudsen AKS, Stene-Larsen K, Gustavson K, Hotopf M, Kessler RC, Krokstad S, et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg Health Eur. 2021;4:100071. doi: 10.1016/j.lanepe.2021.100071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boerma JT, Stansfield SK. Health statistics now: are we making the right investments? Lancet. 2007;369(9563):779–86. doi: 10.1016/S0140-6736(07)60364-X. [DOI] [PubMed] [Google Scholar]
- 29.Fechner-Bates S, Coyne JC, Schwenk TL. The relationship of self-reported distress to depressive disorders and other psychopathology. J Consult Clin Psychol. 1994;62:550–9. doi: 10.1037/0022-006X.62.3.550. [DOI] [PubMed] [Google Scholar]
- 30.Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36) Nord J Psychiatry. 2003;57(2):113–8. doi: 10.1080/08039480310000932. [DOI] [PubMed] [Google Scholar]
- 31.Wu Y, Levis B, Sun Y, He C, Krishnan A, Neupane D, et al. Accuracy of the hospital anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: systematic review and individual participant data meta-analysis. BMJ. 2021;373:n972. doi: 10.1136/bmj.n972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bakken IJ, Ariansen AMS, Knudsen GP, Johansen KI, Vollset SE. The Norwegian patient Registry and the Norwegian Registry for Primary Health Care: Research potential of two nationwide health-care registries. Scand J Public Health. 2020;48(1):49–55. doi: 10.1177/1403494819859737. [DOI] [PubMed] [Google Scholar]
- 33.Furu K. Establishment of the nationwide Norwegian prescription database (NorPD) – new opportunities for research in pharmacoepidemiology in Norway. Norsk Epidemiologi. 2009;18(2).
- 34.Thygesen LC, Ersbøll AK. When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol. 2014;29(8):551–8. doi: 10.1007/s10654-013-9873-0. [DOI] [PubMed] [Google Scholar]
- 35.Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. 2017;210(2):119–24. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Torvik FA, Ystrom E, Gustavson K, Rosenstrom TH, Bramness JG, Gillespie N, et al. Diagnostic and genetic overlap of three common mental disorders in structured interviews and health registries. Acta Psychiatr Scand. 2018;137(1):54–64. doi: 10.1111/acps.12829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 38.Syed HR, Zachrisson HD, Dalgard OS, Dalen I, Ahlberg N. Concordance between Hopkins Symptom Checklist (HSCL-10) and Pakistan anxiety and Depression Questionnaire (PADQ), in a rural self-motivated population in Pakistan. BMC Psychiatry. 2008;8:59. doi: 10.1186/1471-244X-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmalbach B, Zenger M, Tibubos AN, Kliem S, Petrowski K, Brähler E. Psychometric properties of two brief versions of the Hopkins Symptom Checklist: HSCL-5 and HSCL-10. Assessment. 2019;28(2):617–31. doi: 10.1177/1073191119860910. [DOI] [PubMed] [Google Scholar]
- 40.Djukanovic I, Carlsson J, Årestedt K. Is the hospital anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual Life Outcomes. 2017;15(1):193. doi: 10.1186/s12955-017-0759-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brennan C, Worrall-Davies A, McMillan D, Gilbody S, House A. The Hospital anxiety and Depression Scale: a diagnostic meta-analysis of case-finding ability. J Psychosom Res. 2010;69(4):371–8. doi: 10.1016/j.jpsychores.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 42.OECD, OECD-Note-EquivalenceScales. WHAT ARE EQUIVALENCE SCALES? OECD; 2022.
- 43.Sirpal MK, Haugen W, Sparle K, Haavet OR. Validation study of HSCL-10, HSCL-6, WHO-5 and 3-key questions in 14–16 year ethnic minority adolescents. BMC Fam Pract. 2016;17(1):7. doi: 10.1186/s12875-016-0405-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Søgaard m.fl AJ. A comparison of the CONOR Mental Health Index to the HSCL-10 and HADS: measuring mental health status in the Oslo Health Study and the Nord-Trøndelag Health Study. Norsk Epidemiologi. 2009;13(2).
- 45.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of Depression in adolescents and Young adults. Pediatrics. 2016;138(6). [DOI] [PMC free article] [PubMed]
- 46.Sjöberg L, Karlsson B, Atti AR, Skoog I, Fratiglioni L, Wang HX. Prevalence of depression: comparisons of different depression definitions in population-based samples of older adults. J Affect Disord. 2017;221:123–31. doi: 10.1016/j.jad.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Knapstad M, Sivertsen B, Knudsen AK, Smith ORF, Aarø LE, Lønning KJ, et al. Trends in self-reported psychological distress among college and university students from 2010 to 2018. Psychol Med. 2021;51(3):470–8. doi: 10.1017/S0033291719003350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Silverstein B, Edwards T, Gamma A, Ajdacic-Gross V, Rossler W, Angst J. The role played by depression associated with somatic symptomatology in accounting for the gender difference in the prevalence of depression. Soc Psychiatry Psychiatr Epidemiol. 2013;48(2):257–63. doi: 10.1007/s00127-012-0540-7. [DOI] [PubMed] [Google Scholar]
- 49.Grønli OK, Bramness JG, Wynn R, Høye A. Depressive symptoms in the general population: the 7th Tromsø Study. J Affect Disorders Rep. 2022;8:100322. doi: 10.1016/j.jadr.2022.100322. [DOI] [Google Scholar]
- 50.Stordal E, Bjartveit Krüger M, Dahl NH, Krüger Ø, Mykletun A, Dahl AA. Depression in relation to age and gender in the general population: the Nord-Trøndelag Health Study (HUNT) Acta Psychiatr Scand. 2001;104(3):210–6. doi: 10.1034/j.1600-0447.2001.00130.x. [DOI] [PubMed] [Google Scholar]
- 51.Thiagarajan T, Newson J. The Mental State of the World in 2022. Mental Health Million Project; 2023.
- 52.Reiss F, Meyrose A-K, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: results of the German BELLA cohort-study. PLoS ONE. 2019;14(3):e0213700–e. doi: 10.1371/journal.pone.0213700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kinge JM, Øverland S, Flatø M, Dieleman J, Røgeberg O, Magnus MC, et al. Parental income and mental disorders in children and adolescents: prospective register-based study. Int J Epidemiol. 2021;50(5):1615–27. doi: 10.1093/ije/dyab066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Slettebak MH. Labour migration and increasing inequality in Norway. Acta Sociol. 2020;64(3):314–30. doi: 10.1177/0001699320930261. [DOI] [Google Scholar]
- 55.Edinoff AN, Akuly HA, Hanna TA, Ochoa CO, Patti SJ, Ghaffar YA, et al. Selective serotonin reuptake inhibitors and adverse effects: a narrative review. Neurol Int. 2021;13(3):387–401. doi: 10.3390/neurolint13030038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fosu GB. Women’s orientation toward help-seeking for mental disorders. Soc Sci Med. 1995;40(8):1029–40. doi: 10.1016/0277-9536(94)00170-X. [DOI] [PubMed] [Google Scholar]
- 57.Bramness JG, Walby FA, Hjellvik V, Selmer R, Tverdal A. Self-reported mental health and its gender differences as a predictor of suicide in the middle-aged. Am J Epidemiol. 2010;172(2):160–6. doi: 10.1093/aje/kwq091. [DOI] [PubMed] [Google Scholar]
- 58.Freudenstein U, Arthur AJ, Matthews RJ, Jagger C. Community surveys of late-life depression: who are the non-responders? Age Ageing. 2001;30(6):517–21. doi: 10.1093/ageing/30.6.517. [DOI] [PubMed] [Google Scholar]
- 59.Hopstock LA, Grimsgaard S, Johansen H, Kanstad K, Wilsgaard T, Eggen AE. The seventh survey of the Tromsø Study (Tromsø7) 2015–2016: study design, data collection, attendance, and prevalence of risk factors and disease in a multipurpose population-based health survey. Scand J Public Health. 2022;50(7):919–29. doi: 10.1177/14034948221092294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Søgaard AJ, Selmer R, Bjertness E, Thelle D. The Oslo Health Study: the impact of self-selection in a large, population-based survey. Int J Equity Health. 2004;3(1):3. doi: 10.1186/1475-9276-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. 2017;73:133–6. doi: 10.1016/j.addbeh.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Peitz D, Kersjes C, Thom J, Hoelling H, Mauz E. Indicators for Public Mental Health: a scoping review. Front Public Health. 2021;9:714497. doi: 10.3389/fpubh.2021.714497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nurnberger JI, Jr, Foroud T, Flury L, Su J, Meyer ET, Hu K, et al. Evidence for a locus on chromosome 1 that influences vulnerability to alcoholism and affective disorder. Am J Psychiatry. 2001;158(5):718–24. doi: 10.1176/appi.ajp.158.5.718. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during this study are available from the corresponding author only after application has been made to and permission given by the ethics committee.