Abstract
Background:
In the Eastern Mediterranean region, Afghanistan ranks third for the world’s highest burden of malaria. The vast majority (95%) of malaria cases in Afghanistan are attributed to Plasmodium falciparum and 5% to Plasmodium vivax. Most cases occur in low-altitude regions, especially in the eastern province of Nangarhar, where agriculture and farming are predominant. To better understand the public sentiment toward malaria, this study aimed to understand the knowledge, attitude, and practice of patients toward malaria who visited public and private hospitals of Nangarhar province.
Methods:
A cross-sectional descriptive study was conducted on Nangarhar residents who visited the adult Outpatient departments of eight local public and private health facilities. Data collection took place from 1st August 2022 to 15th September 2022.
Results:
Of 700 participants, 37.9% (n = 265) identified as male and 62.1% (n = 435) identified as female. The majority of participants (84.6 %) were within the (18–40) age range, followed by 12.7% in the (41–60) age range, and 2.7% were aged 61 years or older. Moreover, 99.7% (n = 698) of the participants had heard of malaria. The main sources of information about malaria were family members (31.3%, n = 219), television (32.6%, n = 228), Internet (12.6%, n = 88), school (11.3%, n = 79), and health facilities (31.4%, n = 220). Most respondents correctly identified mosquito bites as the primary mode of malaria transmission (72.6%, n = 508). Others suggested that transmission could occur by close contact with a malaria patient (14.0%, n = 98) and drinking contaminated water (17.3%, n = 121). The majority of participants (70.6%) agreed that malaria is a serious and life-threatening disease. A significant number of participants (96.6%) reported owning an insecticide-treated mosquito net at home, and 87.0% reported using the net.
Conclusion:
Overall, participants reported good knowledge, attitude, and practice toward malaria. This may be linked to the awareness campaigns and preventive programs in Nangarhar province that have contributed to participant’s willingness to prevent malaria and treat themselves if they get infected. Public health campaigns are difficult in Afghanistan with weak governance and conflict, and thus, populations may find themselves at risk if health promotion activities are stopped.
Keywords: Malaria, attitude, practice, knowledge, Afghanistan
Background
Malaria, a parasitic infection caused by Plasmodium parasites, is transmitted to humans through the bites from female Anopheles mosquitoes. Humans can be affected by five different parasite species, with P. falciparum and P. vivax—posing the most significant threat. The P. vivax parasite is the predominant malaria type outside sub-Saharan Africa, notably in the Eastern Mediterranean region. In 2021, 18% of the cases in this region were attributed to P. vivax, predominantly in Afghanistan and Pakistan. 1 With Afghanistan accounting 11% of the cases in Eastern Mediterranean region, there is an urgent need for public health support and focus on malaria. 2
Symptoms of malaria include fever, headache, and chills, which typically emerge 10–15 days after the infective mosquito bite, and they might be initially mild, nonspecific, and difficult to diagnose. If P. falciparum malaria is not treated, it can proceed to severe sickness and death in less than 24 h. 3 Populations that are at higher risk of contracting malaria include infants and children under 5 years of age, pregnant women, immunocompromised individuals such as patients with HIV/AIDS, and mobile populations such as migrant workers or refugees. Early diagnosis and treatment of malaria reduces disease, prevents deaths, and contributes to reducing transmission. 3
The emergence of the COVID-19 pandemic resulted in a huge disruption in the surveillance and management of malaria. Endemic countries around the world diverted their resources to their pandemic response. The WHO Pulse survey, 4 covering data from November 2022 to January 2023, continued to report significant global disruption to health service and surveillance capacity, albeit with the positive conclusion that most countries have reported the first signs of service recovery since 2020. While this diversion of resources aided in keeping countries’ attention on the pandemic, it also resulted in significant underreporting and thus a sharp apparent decline in malaria cases. According to the World malaria report 2021, there were 241 million cases of malaria in 2020 compared to 227 million cases in 2019. The estimated number of malaria deaths stood at 627,000 in 2020—an increase of 69,000 deaths over the previous year. Of these deaths (47,000) were due to disruptions during the COVID-19 pandemic. 5
In Afghanistan, the majority of malaria cases occur in low-altitude regions where agriculture and farming are the most common industries, particularly growing rice and cattle farming. 2 These lowland areas include six provinces: Nangarhar, Paktika, Khost, Nooristan, Kunar, and Laghman, which account for 91% of confirmed P. falciparum and 89% of Plasmodium vivax. cases. Lowland areas are shown in Figure 1. 6 The province with the highest burden is Nangarhar province, with more than 45% of total malaria cases and 35% of total P. falciparum cases. 2
Figure 1.
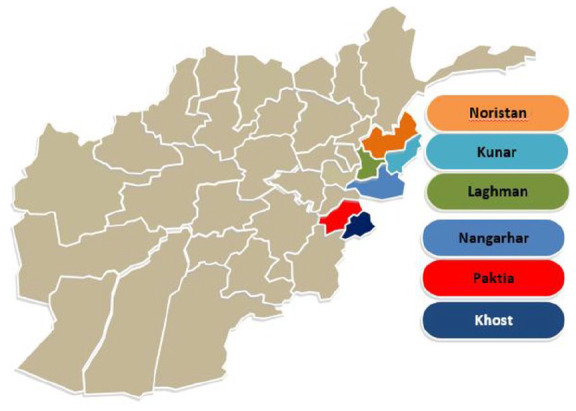
Provinces within the lowland areas of Afghanistan.
The Afghanistan Ministry of Public Health has categorized the malaria sites as high, medium, and low. High-risk areas are defined as provinces and districts with annual parasite incidence (API) rate per 1000 persons at risk of 1 or above and test positivity rate (TPR) at 9% and above. They report that 27% of the Afghan population lives in areas at high risk for malaria, 50% lives in areas at medium risk (API < 1, TPR < 9%), and the remaining 23% live in areas with low and very low risk of malaria transmission or its absence in malaria free areas. 7
The endemicity of malaria in Afghanistan is compounded by civil conflict, fragile healthcare services, and the COVID-19 pandemic. Poor testing capacity and misdiagnosis (e.g., with COVID-19) are big challenges that may have resulted in further burden of malaria. In addition, the political instability has resulted in massive suspension of funding and external support from international organizations. 8
This study aimed to understand the knowledge, attitude, and practice (KAP) of patients toward malaria who visited public and private hospitals of Nangarhar province. The results of the study aim to provide a deep insight on how the public perceives malaria burden, fills the knowledge gap, underscores key challenges that require focus, and informs key recommendations on how to improve the situation.
Methods
Study site
Afghanistan is divided into 34 provinces, with Nangarhar province located near the Pakistan border. Nangarhar is a major travel conduit between Afghanistan and Pakistan, contributing to its public health challenges, particularly in the context of a high burden of malarial disease. Therefore, our study focuses on understanding the KAP toward malaria among the general population visiting both private and public health facilities in Nangarhar province.
Study design
A cross-sectional descriptive study was conducted with Nangarhar residents who visited the adult outpatient departments of local public and private health facilities for a range of health issues. Thus, the study was not restricted to malaria patients. The health facilities included were five government hospitals: Nangarhar Medical Faculty Teaching Hospital, Nangarhar Regional Hospital, Fatima Zuhra Hospital, Surkhrod District Hospital, and Behsood District Hospital and three Private hospitals: Daudzai Medical Complex, Rokhan Hospital, and Sherzad Diagnostic Clinic. Data collection took place from 1st August 2022 to 15th September 2022.
Selection criteria
Participation in this study was voluntary. Participants had the option to withdraw from the study at any stage. Inclusion criteria were all patients 18 years of age or above, with capacity to provide informed consent, and who were Outpatient department’s referral. Exclusion criteria were patients under 18 years, if they did not have the capacity to provide informed consent, and those who were not an Outpatient department’s referral.
Data collection
The study team reviewed the literature prior to the study and opted to utilize a survey questionnaire from a similar study conducted in Tanzania. 9 Based upon the expert insight from the study team and anecdotal feedback from external stakeholders, the questionnaire was deemed appropriate and modified slightly according to the context of Afghanistan. Then, it was translated into Pashto, the national language of residents (Supplemental File 1). Questions were read out by study staff to the participants.
Sample size and sampling type
Nangarhar population has an estimated population of 1,702,000. 10 The sample size was calculated using Survey Monkey with a 95% confidence level and 5% margin of error. 11 The measured required minimum sample size was 385 participants. For this study, we employed a nonprobability convenience sampling method due to the logistical and resource limitations in Nangarhar. While convenience sampling is not as rigorous as probability sampling methods, it was a pragmatic, feasible, and safe choice for this research.
In order to maintain integrity and reliability, we provided training to the data collection team about good research practice, data management, and protocols. At the end of each day of data collection, debriefing sessions were held to address any issues promptly. No significant issues were raised during the study.
Written informed consent was taken from the participants prior to their participation. For participants who were unable to read the consent form or participant information, these were verbally read out loud to them, in a language they understood, and this was done in the presence of an impartial witness. After ensuring comprehension, verbal consent was obtained from each participant, and the witness co-signed the form to attest to the participant’s informed consent. This process was approved by the ethics committee.
Data entry was subjected to validation checks to prevent errors. Double data entry was performed for a randomly selected subset of questionnaires (10% of all data) to ensure accuracy. Discrepancies were resolved through consensus, referring back to the original questionnaires.
Pilot study
The questionnaire was pretested on 50 participants to confirm the acceptability and clarity of questions. Expert researchers reviewed the questionnaire for content validity and considered their comments. No changes were made to the final questionnaires. For reliability, Cronbach’s alpha was 0.753 for every questionnaire section, with a score of >0.7 typically used as a threshold to indicate an acceptable level of consistency. 12 Observations from this pilot study were not included in the final analysis.
Ethical Approval: Ethical approval was obtained from the Microbiology Department of Kabul University of Medical Sciences Research Committee (KUMS-MD-22101). Informed consent was taken from the participants before they participated in the study.
Statistical analysis
The statistical analysis for this study was carried out utilizing the Statistical Package for the Social Sciences (SPSS) version 16. 13
During the descriptive analysis, the frequencies of distinct categories within each variable were calculated. The frequencies were then expressed as percentages to provide a clearer representation of the distribution of responses within each variable.
Results
Characteristics of study participants
A total of 700 participants were surveyed, with 37.9% (n = 265) male and 62.1% (n = 435) female participants. By age, the majority of participants (84.6 %) were within the 18–40 years age range, followed by 12.7% aged 41–60 years, and 2.7% aged 61 years or older. By measure of literacy, 54.9% (n = 384) reported being able to read and write, whereas 45.1% (n = 316) indicated they could not read and write. Among female respondents, 26.1% (n = 118) reported being pregnant. In terms of occupational status, 22.9% (n = 160) reported being employed (Table 1).
Table 1.
Demographic distribution and characteristics of survey participants.
| Demographics | N, % |
|---|---|
| Gender | |
| Male | 265 (37.9) |
| Female | 435 (62.1) |
| Age (years) | |
| 18–40 | 592 (84.6) |
| 41–60 | 89 (12.7) |
| >61 | 19 (2.7) |
| What is your level of education? | |
| I can read and write | 384 (54.9) |
| I cannot read and write | 316 (45.1) |
| Are you pregnant? (only females should answer this question) | |
| Yes | 118 (26.1) |
| No | 512 (73.15) |
| What is your occupation status? | |
| I have job | 160 (22.9) |
| Jobless | 540 (77.1) |
Respondent’s knowledge of malaria transmission and symptoms
The findings showed that 99.7% (n = 698) of the participants had heard of malaria. The main sources of information reported were via family members (31.3%, n = 219), television (32.6%, n = 228), Internet (12.6%, n = 88), school (11.3%, n = 79), and health facilities (31.4%, n = 220). Most respondents correctly identified mosquito bites as the primary mode of malaria transmission (72.6%, n = 508). Others indicated that transmission could occur following close contact with a malaria patient (14.0%, n = 98), and drinking contaminated water (17.3%, n = 121). Commonly reported symptoms included elevated temperatures (50.7%, n = 355), general body weakness (26.0%, n = 182), vomiting (22.0%, n = 154), sweating (12.7%, n = 89), headache (17.4%, n = 122), dizziness (7.0%, n = 49), and chills (24.6%, n = 172). The preventive measures mentioned by participants included wearing long-sleeved clothing (10.4%, n = 73), sleeping under bed nets (73.3%, n = 513), spraying insecticides (17.3%, n = 121), and cleaning dark corners in the house (6.3%, n = 44) (Table 2).
Table 2.
Knowledge of malaria transmission and symptoms among survey participants (N = 700).
| Malaria transmission measures | Responses | N, % |
|---|---|---|
| Have you ever heard of malaria? | Yes | 698 (99.7%) |
| No | 2 (0.3%) | |
| Source of information? | Family members | 219 (31.3) |
| Television | 228 (32.6) | |
| Internet | 88 (12.6) | |
| School | 79 (11.3) | |
| Health facility | 220 (31.4) | |
| How malaria can be transmitted? | Bite by mosquito infected with malaria | 508 (72.6) |
| Coming into close contact with malaria patient | 98 (14.0) | |
| Drinking contaminated water | 121 (17.3) | |
| The following are signs/symptoms of malaria | Elevated temperature | 355 (50.7) |
| General body weakness | 182 (26.0) | |
| Vomiting | 154 (22.0) | |
| Sweating | 89 (12.7) | |
| Headache | 122 (17.4) | |
| Dizziness | 49 (7.0) | |
| Chills | 172 (24.6) | |
| The following can be used to prevent/control malaria | Wearing long sleeved clothing | 73 (10.4) |
| Sleeping under bed net | 513 (73.3) | |
| Spraying insecticides | 121 (17.3) | |
| Cleaning dark corners in the house | 44 (6.3) |
Participant’s attitudes toward malaria
A majority of participants (70.6%) reported that malaria is a serious and life-threatening disease. However, 29.4% of participants did either strongly disagree, or disagree with this statement. Furthermore, opinions varied concerning the transmission of malaria, with 67.7% suggesting that it can be transmitted from person-to-person. Just over one-fifth (22.8%) disagreed that avoiding mosquito bites is the best preventive measure, and a considerable proportion (76.8%) believed that only specific groups, such as children and pregnant women, are at risk. With respect to self-treatment, 23.8% indicated confidence in their ability to treat themselves if they contracted malaria, while 79.4% believed prompt blood testing at a health center or clinic was necessary. However, more than a quarter of the participants (35.2%) considered purchasing antimalarial drugs from a pharmacy as sufficient (Table 3)
Table 3.
Attitudes toward malaria among survey participants (N = 700).
| Malaria attitude measures | Strongly disagree (N, %) | Disagree (N, %) | Agree (N, %) | Strongly agree (N, %) |
|---|---|---|---|---|
| Malaria is a serious and life-threatening disease | 96 (13.7) | 110 (15.7) | 356 (50.9) | 138 (19.7) |
| Malaria can be transmitted from one person to another like common cold | 128 (18.3) | 346 (49.4) | 195 (27.9) | 31 (4.4) |
| The best way to prevent myself getting malaria is to avoid getting mosquito bites | 62 (8.9) | 97 (13.9) | 340 (48.6) | 201 (28.7) |
| I am sure that anyone can get malaria | 64 (9.1) | 189 (27.0) | 308 (44.0) | 139 (19.9) |
| Sleeping under a mosquito net can prevent myself getting malaria | 74 (10.6) | 107 (15.3) | 299 (42.7) | 220 (31.4) |
| I can treat myself if I get malaria | 196 (28.0) | 337 (48.1) | 94 (13.4) | 72 (10.4) |
| Only children and pregnant women are at risk of malaria | 208 (29.7) | 330 (47.1) | 106 (15.1) | 56 (8.0) |
| One can recover spontaneously from malaria | 198 (28.3) | 368 (52.6) | 71 (10.1) | 63 (9.0) |
| If someone has malaria, people should avoid having close contact with him/her | 122 (17.4) | 318 (45.4) | 181 (25.9) | 79 (11.3) |
| It is dangerous when malaria medicine is not taken completely | 109 (15.9) | 156 (22.3) | 304 (43.3) | 131 (18.7) |
| I can buy antimalaria drugs from the drug shop/pharmacy to treat myself when I get malaria | 164 (23.4) | 289 (41.3) | 141 (20.1) | 106 (15.1) |
| I think that I should go to the health center/clinic to have my blood tested as soon as I suspect that I am suffering from malaria | 59 (8.4) | 85 (12.1) | 253 (36.1) | 303 (43.3) |
Malaria preventive measures reported by participants
A significant majority (96.6%) reported owning an insecticide-treated mosquito net (ITN) at home, whereas only a small proportion (3.4%) did not. The use of mosquito nets was also prevalent, with 87.0% indicating usage and 13.0% reporting no usage. When it came to mosquito repellents (designed to deter mosquitoes from landing on skin or clothes), 50.0% reported using them and 50.0% said they did not use them. The use of mosquito coils was relatively low, with 31.3% using them. Similarly, the use of mosquito sprays was reported by 57.6% of participants in the room, while 42.4% did not use them. Regarding structural measures, a significant proportion (66.4%) reported closing windows to prevent mosquito entry, whereas 33.6% did not follow this practice. Additionally, 61.3% reported having window screens as an additional protective measure (Table 4).
Table 4.
Malaria preventive measures reported by participants (N = 700).
| Malaria preventive measures | Yes (N, %) | No (N, %) |
|---|---|---|
| Own an ITN at home | 676 (96.6) | 24 (3.4) |
| Use of mosquito nets | 609 (87.0) | 91 (13.0) |
| Use of mosquito repellents | 350 (50.0) | 350 (50.0) |
| Use of mosquito coil | 218 (31.3) | 482 (68.9) |
| Use of mosquito spray | 403 (57.6) | 297 (42.4) |
| Close window | 465 (66.4) | 235 (33.6) |
| Have window screen | 429 (61.3) | 271 (38.7) |
Regarding sleeping habits, 41.0% of participants reported always using a mosquito net as a habit, 51.0% reported sometimes, and 8.0% reported never using one. When describing their other household members, 36.4% of participants reported they would always use mosquito nets, 54.3% reported sometimes, and 9.3% reported never. In terms of checking for holes in mosquito nets, 38.0% of participants reported always doing so, 47.6% reported sometimes, and 14.4% reported never. The use of sprays in the house varied, with 23.7% reporting always using them, 47.1% sometimes, and 29.1% never using them. Additionally, 34.1% reported always cleaning around the house from extra plants, while 52.7% reported sometimes, and 13.1% reported never doing so. When it came to removing standing water around the house, 34.1% reported always, 52.7% sometimes, and 13.1% never doing so. Finally, 59.4% of the respondents reported going to a healthcare center when falling sick, 37.7% sometimes, and 2.9% never going (Table 5).
Table 5.
Household practices related to malaria prevention among participants.
| Questions | Always (N, %) | Sometimes (N, %) | Never (N, %) |
|---|---|---|---|
| How often do you sleep in a mosquito net? | 287 (41.0) | 357 (51.0) | 57 (8.0) |
| How often do other members of household sleep in a mosquito net? | 255 (36.4) | 380 (54.3) | 65 (9.3) |
| Do you check mosquito nets for finding and fixing wholes? | 266 (38.0) | 333 (47.6) | 101 (14.4) |
| Do you use spray in your house? | 166 (23.7) | 330 (47.1) | 204 (29.1) |
| Do you clean around your house with extra plants? | 239 (34.1) | 369 (52.7) | 92 (13.1) |
| Do you remove around your house from stock waters? | 259 (34.1) | 369 (52.7) | 92 (13.1) |
| Do you go to healthcare center when you feel sick | 416 (59.4) | 214 (37.7) | 20 (2.9) |
Discussion
This study assessed KAPs toward malaria among patients attending public and private hospitals in the eastern region of Afghanistan. Nangarhar province, which is located near the border of Pakistan and serves as a migratory route to Pakistan, is particularly vulnerable to malaria due to its climate variations and presence of mosquitoes. To the best of our knowledge, this is the first study investigating the level of awareness of malaria in Nangarhar.
Regarding the knowledge about malaria transmission and symptoms, the study revealed that almost all participants had heard of the disease. The identification of mosquito bites as the primary mode of malaria transmission by the majority of respondents (72.6%) demonstrated a satisfactory understanding of this crucial aspect. Arguably, this is very high given that Afghanistan’s population in general has a high illiteracy level, and shows how other modes of communication, including word of mouth, are important in populations such as these for good dissemination of public health messaging. 14 There has previously been many years of extended health promotion, with availability of nets and insecticides combined with awareness programs in Afghanistan, including within Nangarhar province. The importance of health promotion activities is also reflected in a study conducted in Bangladesh. The authors have revealed significant associations between sociodemographic factors and malaria vaccine acceptance, similar to patterns observed in our study. This parallel highlights the universal influence of factors like education and occupation on malaria-related knowledge and attitudes, reinforcing the need for any health promotion to be locally tailored, to help maximize the influence and impact of the messaging contexts. 15 However, this is not the case in all high-burden malaria zones. A study conducted in Yemen reported the knowledge of and attitude toward malaria prevention were poor. For example, only 7% and 2% of study participants mentioned the importance of sleeping under ITNs or using indoor residual spraying as methods of malaria prevention, respectively. 16 This is despite the local public health guidance in Yemen recommending these preventive practices.
There were some misconceptions reported such as a notable proportion of respondents associated malaria transmission from close contact with a malaria patient or drinking contaminated water. Incorrect health knowledge can delay accessing healthcare, and thus, it is important to maintain to provide correct information to support issues such as trust and acceptability in the health services. 17 However, given the current instability in Afghanistan and the recent Taliban takeover, it is not clear if educational campaigns on malaria continue. Previous progress in the healthcare system has come to a halt, and the lack of a strong surveillance system, coupled with a favorable breeding environment for malaria parasites, indicates a high probability of a significant malaria burden in rural areas. 2
Regarding the attitude toward malaria, the majority of the participants agreed that malaria is a serious and life-threatening disease (70.6%). However, in a study conducted in Makenene Cameroon, only 48.4% of the participants reported a good attitude toward malaria. 18 Additionally, in this study, it was observed that participants with good knowledge had a good overall attitude toward malaria.
The study revealed mixed attitudes toward self-treatment for malaria, with 28.0% of participants expressing confidence in their ability to treat themselves, and the majority (79.4%) believing that prompt blood testing at a healthcare center or clinic is necessary. It is encouraging that a significant proportion recognizes the importance of seeking professional healthcare for accurate diagnosis and appropriate treatment. However, the finding that 35.2% of participants consider purchasing antimalaria drugs from a pharmacy sufficient highlights the need for stricter regulation and enforcement to prevent self-medication practices that may contribute to drug resistance and inadequate treatment outcomes. There is some evidence around the presence of counterfeit antimalarial medicines within Afghanistan, 19 though the extent is not fully known. Self-medication practices have been observed in different parts of the country and are linked with unfavorable health consequences.20,21 Hence, it is important for the government to place regulations on self-medication practices.
Examination of malaria preventive measures and practices indicated positive trends. The high ownership of ITNs (96.6%) and their usage (87.0%) reflects the successful implementation of mosquito net distribution programs and community awareness campaigns. This may reflect the relatively high knowledge scores, combined with availability of ITNs and known burden of disease, with these components resulting in high practice scores. Levels of good practice are variable in other studies. Similar findings were observed in Bangladesh where the majority of the respondents reported good practice toward malaria. There, bed nets (93.7%) were the most common preventive method used against mosquito bites, followed by coils (85.7%), electric bats (42.0%), and insecticide spray (33.1%). 22 The majority of participants declared that they cleaned their surroundings (76.0%). However, in Ratuwamai Municipality in Nepal, 52.6% reported poor practice toward malaria. 23
When considering yellow fever, another mosquito-transmitted disease, a KAP study describing nomadic populations in a high-burden area of rural Ghana reported poor knowledge, but higher scores for both attitude and practice. 24 Due to their mobility and low access to healthcare, this Nomadic group had a low vaccine uptake. Following a locally delivered extended health promotion campaign, delivered by the trusted local health directorates, vaccine uptake significantly increased in this Nomadic population. 25 This illustrates the importance of high-quality public health information for groups at risk from vector-borne disease, in order to improve KAP and ultimately healthcare-seeking behavior. The evolving threat of climate change is anticipated to result in changes in habitats for mosquitoes and thus new threats to human health. 26 This means that health systems must adapt, and the populations at risk need tailored information to support their decision-making. The situation is complicated with areas of conflict or unstable governance, such as Afghanistan. The Taliban regime continuing to ban women from working in humanitarian job roles will have further health and socioeconomic consequences for the country. 27 A UN report, from April 2023, described how the current governance in Afghanistan will lead to further withdrawal of international donors and support, and send the country to the bottom of global poverty scale rankings. 28
In the present study, we did not find a direct analysis of gender’s impact on knowledge or attitude; nonetheless, it is essential to consider the potential gender-specific vulnerabilities, such as the pregnant women’s increased susceptibility to malaria. This emphasizes how counterproductive it is to ban women working in responsibility in the health, education, and humanitarian sectors, where their knowledge, skills, and potential to engage with vulnerable groups (such as other women) would be vital.
Strengthens and limitations
The study has several strengths and limitations. It focused on malaria, a disease in Afghanistan with high mortality. The study site and Nangarhar province is a high transmission zones and shares a border with Pakistan, serving as a route for daily travel and potential disease transmission.
Several limitations of the study should be noted. It is difficult to carry out original research in Afghanistan, and our study focused on individuals attending a healthcare setting in Nangarhar. Therefore, generalizability to other populations is difficult. Access to wider populations is limited, and convenience sampling within a healthcare setting is typically the most pragmatic, and safest, research methodology available to us. We do not want to put participants or the research team at any unacceptable level of risk, and so safety took precedent over enhancing the methodology. Further cross-sectional studies ideally are needed to provide in-depth assessment of malaria in other high transmission zone areas, and longitudinal research can consider temporal trends to better understand any evolving changes in public understanding of, and healthcare-seeking behavior for, malaria. Additionally, the study was conducted predominantly urban or periurban neighborhoods. Hence, there could be differences among participants in the community, or in rural settings.
Conclusion
Overall, participants reported good KAP toward malaria. This could be attributed to the awareness campaigns and preventive programs in Nangarhar province, which have encouraged participants to take preventive measures against malaria and seek appropriate care if get infected. A recommendation for policymakers is to acknowledge the high level of malaria knowledge within this study population, utilizing it as a foundation for future health promotion activities. Therefore, it is important for future awareness-raising campaigns to be tailored to the specific needs and socioeconomic circumstances of the target communities. Furthermore, additional research could include cross-sectional studies from other populations in Afghanistan, alongside longitudinal studies to observe changes in temporal trends. Proactive approaches to countering misinformation may also be helpful, particularly ahead of any future malaria vaccine rollout in Afghanistan.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121241251758 for Knowledge, attitude, and practices toward malaria among hospital outpatients in Nangarhar, Afghanistan: A cross-sectional study by Arash Nemat, Abdul Ghafar Sherzad, Ehsanullah Ehsan, Asadullah Hassnzai, Mehrab Naderi, Naqeebullah Zaki, Mohammad Yasir Essar, Wafaa Binti Mowlabaccus, Michael G Head and Abdullah Asady in SAGE Open Medicine
Acknowledgments
None declared.
Footnotes
Authors’ contributions: AN and MYE conceptualized the topic, drafted the protocol and designed the questionnaires. AGS, EE, AH, MN, and NZ contributed to the data collection. MYE wrote the first draft of the manuscript. WBM did the statistical analysis. MGH and AA edited the second draft and made critical comments. All authors agreed to the submission of the article.
Availability of data and materials: All data are available in the article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Ethical approval was obtained from the Microbiology Department of Kabul University of Medical Sciences Research Committee (KUMS-MD-22101) on 1st July 2022. Informed consent was taken from the participants before they participated in the study.
Informed consent: Written informed consent was obtained from all subjects before the study.
Consent for publication: All authors agreed to the publication of this article.
Trial registration: Not applicable.
ORCID iDs: Arash Nemat  https://orcid.org/0000-0002-7044-5473
https://orcid.org/0000-0002-7044-5473
Mohammad Yasir Essar  https://orcid.org/0000-0002-6554-7619
https://orcid.org/0000-0002-6554-7619
Abdullah Asady  https://orcid.org/0000-0001-9775-739X
https://orcid.org/0000-0001-9775-739X
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Malaria Report 2022.World | ReliefWeb. 2022, https://reliefweb.int/report/world/world-malaria-report-2022 (2022, accessed 7 June 2023).
- 2. Siddiqui JA, Aamar H, Siddiqui A, et al. Malaria in Afghanistan: challenges, efforts and recommendations. Ann Med Surg (Lond) 2022; 81: 104424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fact sheet about malaria, https://www.who.int/news-room/fact-sheets/detail/malaria (2023, accessed 7 June 2023).
- 4. Fourth round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November 2022–January 2023, https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2023.1 (2023, accessed 7 June 2023).
- 5. World malaria report 2021, https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021 (2021, accessed 7 June 2023).
- 6. Essar MY, Siddiqui A, Head MG. Infectious diseases in Afghanistan: strategies for health system improvement. Health Sci Rep 2023; 6(12): e1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Trends in malaria indicators after scale-up of community-based malaria management in Afghanistan | Malaria Journal | Full Text, https://malariajournal.biomedcentral.com/articles/10.1186/s12936-022-04174-x (2022, accessed 7 June 2023). [DOI] [PMC free article] [PubMed]
- 8. Shah J, Essar MY, Qaderi S, et al. Respiratory health and critical care concerns in Afghanistan. Lancet Respir Med 2022; 10(3): 229–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Munisi DZ, Nyundo AA, Mpondo BC. Knowledge, attitude and practice towards malaria among symptomatic patients attending Tumbi Referral Hospital: a cross-sectional study. PLoS One 14(8): e0220501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nangarhar. European Union Agency for Asylum, https://euaa.europa.eu/country-guidance-afghanistan-2020/nangarhar (2020, accessed 7 June 2023).
- 11. SurveyMonkey. Sample size calculator and tips for determining sample size, https://www.surveymonkey.com/mp/sample-size-calculator/ (2022, accessed 18 February 2024).
- 12. Cortina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol 1993; 78: 98–104. [Google Scholar]
- 13. IBM SPSS Statistics, https://www.ibm.com/products/spss-statistics (accessed 16 March 2024).
- 14. UNESCO stands with all Afghans to ensure youth and adults in Afghanistan, especially women and girls, achieve literacy and numeracy by 2030 | UNESCO, https://www.unesco.org/en/articles/unesco-stands-all-afghans-ensure-youth-and-adults-afghanistan-especially-women-and-girls-achieve (2023, accessed 18 February 2024).
- 15. Amin MA, Afrin S, Bonna AS, et al. Knowledge and acceptance of malaria vaccine among parents of under-five children of malaria endemic areas in Bangladesh: a cross-sectional study. Health Expect 2023; 26(6): 2630–2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bamaga OA, Mahdy MA, Mahmud R, et al. Malaria in Hadhramout, a southeast province of Yemen: prevalence, risk factors, knowledge, attitude and practices (KAPs). Parasites Vectors 2014; 7(1): 351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Borges do, Nascimento IJ, Pizarro AB, Almeida JM, et al. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ 2022; 100(9): 544–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Djoufounna J, Bamou R, Mayi MPA, et al. Population knowledge, attitudes and practices towards malaria prevention in the locality of Makenene, Centre-Cameroon. Malaria J 2022; 21(1): 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lalani M, Kaur H, Mohammed N, et al. Substandard antimalarials available in Afghanistan: a case for assessing the quality of drugs in resource poor settings. Am J Trop Med Hyg 2015; 92(Suppl 6): 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nemat A, Rezayee KJ, Essar MY, et al. A report of Kabul internet users on self-medication with over-the-counter medicines. Sci Rep 2023; 13(1): 8500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roien R, Bhandari D, Hosseini SMR, et al. Prevalence and determinants of self-medication with antibiotics among general population in Afghanistan. Expert Rev Anti Infect Ther 2022; 20(2): 315–321. [DOI] [PubMed] [Google Scholar]
- 22. Mobin M, Khan M, Anjum H, et al. Knowledge, attitudes, and practices in relation to mosquito-borne diseases in Bangladesh. Int J Environ Res Public Health 2022; 19(14): 8258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Karki R, Bartoula N, Kaphle M, et al. Knowledge and practice of malaria prevention among residents of Ratuwamai Municipality, Nepal. One Health Bull 2023; 3: 6. [Google Scholar]
- 24. Inusah AW, Collins G, Dzomeku P, et al. Knowledge, attitudes and practice towards yellow fever among nomadic populations: a cross-sectional study in yellow fever outbreak communities in Ghana. PLoS Global Public Health 2023; 3(3): e0000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Inusah AW, Collins G, Head MG, et al. Yellow fever vaccination coverage among nomadic populations in Savannah region, Ghana; a cross-sectional study following an outbreak. medRxiv 2022. DOI: 10.1101/2022.08.22.22279078v1. [DOI] [Google Scholar]
- 26. Gaythorpe KA, Hamlet A, Cibrelus L, et al. The effect of climate change on yellow fever disease burden in Africa. eLife 2020; 9: e55619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Essar MY, Raufi N, Head MG, et al. Afghan women are essential to humanitarian NGO work. Lancet Global Health 2023; 11(4): e497–e498. [DOI] [PubMed] [Google Scholar]
- 28. Afghanistan Socio-Economic Outlook 2023 Executive Summary. United Nations Development Program. UNDP, https://www.undp.org/da/denmark/publications/afghanistan-socio-economic-outlook-2023-executive-summary (2023, accessed 7 June 2023). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121241251758 for Knowledge, attitude, and practices toward malaria among hospital outpatients in Nangarhar, Afghanistan: A cross-sectional study by Arash Nemat, Abdul Ghafar Sherzad, Ehsanullah Ehsan, Asadullah Hassnzai, Mehrab Naderi, Naqeebullah Zaki, Mohammad Yasir Essar, Wafaa Binti Mowlabaccus, Michael G Head and Abdullah Asady in SAGE Open Medicine


