Highlights:
-
•
Incidence of cecal volvulus after laparoscopic surgery, especially in gynecologic oncology, has not been well studied.
-
•
Cecal volvulus can result in serious complications such as intestinal strangulation or necrosis.
-
•
Minimally invasive surgery is increasingly utilized in gynecologic oncology.
-
•
Potential benefit in identifying gynecologic oncology patients at increased risk and considering intraoperative factors.
Keywords: Robotic, Endometrial cancer, Volvulus, Minimally invasive
Abstract
Cecal volvulus is a rare and life-threatening cause of intestinal obstruction with multiple risk factors including prior abdominal surgery and cecal hypermobility. Although its incidence has been reported after common procedures such as cholecystectomy and appendectomy, it has not been well studied after laparoscopy, especially in gynecological surgeries. If untreated, a cecal volvulus can result in serious complications such as intestinal strangulation, necrosis, or perforation. Therefore, early identification of risk factors and intervention is important in prevention of these sequelae. Here, we report a case of cecal volvulus in a patient with endometrial carcinoma after a staging robotic-assisted laparoscopic hysterectomy and the risk factors that may have led to her complication.
1. Introduction
Cecal volvulus is a rare cause of intestinal obstruction and is characterized by torsion of the cecum around its mesentery (Hasbahceci et al., 2012). Although its etiology is multifactorial, previous abdominal surgery has been shown to be an important risk factor due to adhesion formation creating a fulcrum for cecal rotation around its mesenteric axis (Rehfuss et al., 2018). In a case series of patients presenting with cecal volvulus, 23–53 % of patients had previous abdominal surgery, although timing of diagnosis after surgery appeared to be variable (Ferguson et al., 2008 Jun). The incidence of cecal volvulus after laparoscopic abdominal surgery specifically has not been well studied, but the three most common procedures reported include cholecystectomy, ventral hernia repair, and appendectomy (Duron et al., 2000). Upon review of the literature, the incidence of volvulus after gynecological surgery is even more rare with only one case reported of a patient with endometrial clear cell carcinoma who had an open hysterectomy (Mathew and Chin, 2003).
Here, we present a case of cecal volvulus diagnosed in a patient with endometrial carcinoma shortly after a staging robotic-assisted laparoscopic hysterectomy.
2. Case
The patient is a 64-year-old with a medical history significant for chronic hypertension and a remote history of appendectomy performed via a supraumbilical incision for ruptured appendicitis while in the third trimester of pregnancy. The patient’s preoperative endometrial biopsy was high grade carcinoma, but her final diagnosis was Stage IA Grade 2 endometrial adenocarcinoma. The preoperative CT abdomen and pelvis demonstrated no evidence of metastatic disease and significant colonic redundancy with the cecum positioned in the left upper quadrant (Fig. 1). She underwent a robotic assisted total laparoscopic hysterectomy, bilateral salpingo-oophorectomy, bilateral sentinel lymph node dissection. During the surgery, the patient was placed in Trendelenburg position of 21 degrees. Dense adhesions were noted along the right pelvic sidewall. To access the retroperitoneal space safely due to the retroperitoneal fibrosis of the right pelvic sidewall, we extended our dissection superiorly along the white line of Toldt. We then were able to access the correct plane and identify retroperitoneal structures to safely proceed with dissection in an inferior fashion along with ureterolysis to the level of the uterine artery. Otherwise, the planned surgery was completed without complication. Her immediate postoperative course was uncomplicated, and the patient was discharged on postoperative day 1.
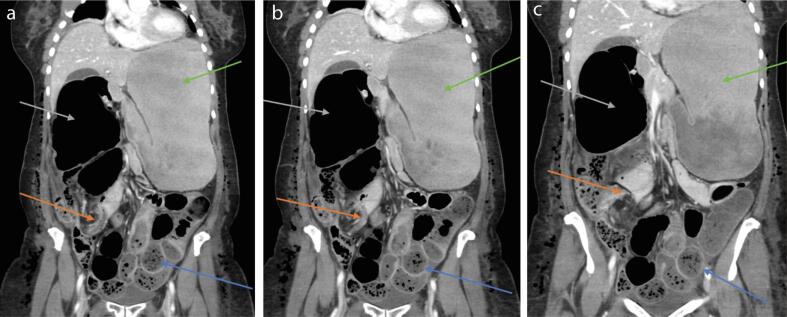
Fig. 1.
The pre-operative contrast enhanced coronal CT image through the abdomen and pelvis shows a redundant proximal colonic mesentery with a mobile right colon (yellow arrows) and the cecal tip in the left upper quadrant (green arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
The patient presented to the emergency department on postoperative day 3 with abdominal pain, increasing abdominal distension and shortness of breath. She had tolerated small amounts of PO intake but had not passed flatus since surgery. Vital signs were notable for tachycardia and tachypnea. Lab work was significant for elevated lactate 4.0 mmol/L. CT abdomen and pelvis showed the presence of a cecal volvulus causing obstruction with dilation of the stomach, small bowel and cecum and decompression of the distal colon (Figs. 2a-c, 3). The patient was made NPO and a nasogastric tube was placed. She was taken emergently to the operating room and underwent exploratory laparotomy, ileocecectomy, and primary ileocolic anastomosis. The cecum, which coursed along the ileocolic trunk mesentery, appeared massively dilated and ischemic.
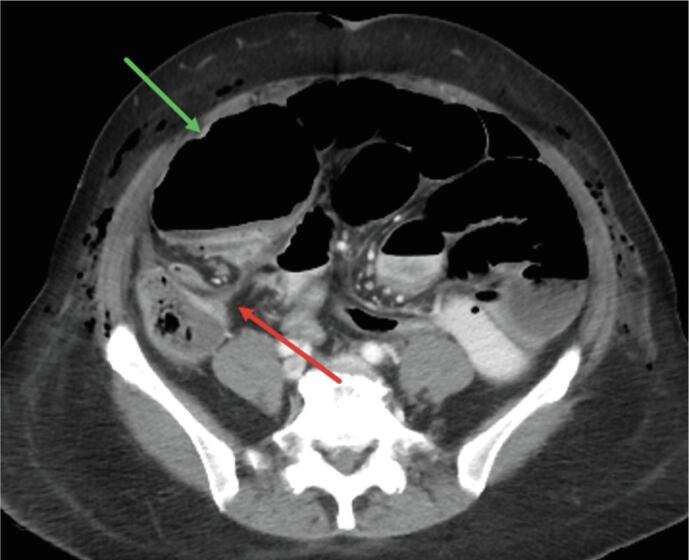
Fig. 2.
a-c. Postoperative day #3 contrast enhanced coronal CT images through the abdomen and pelvis show a distended cecum (gray arrows) with a cecal volvulus in the right lower quadrant (orange arrows). This results in a high-grade obstruction as demonstrated by multiple distended air and fluid-filled small bowel loops in the left lower quadrant (blue arrows) and a massively distended stomach (green arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
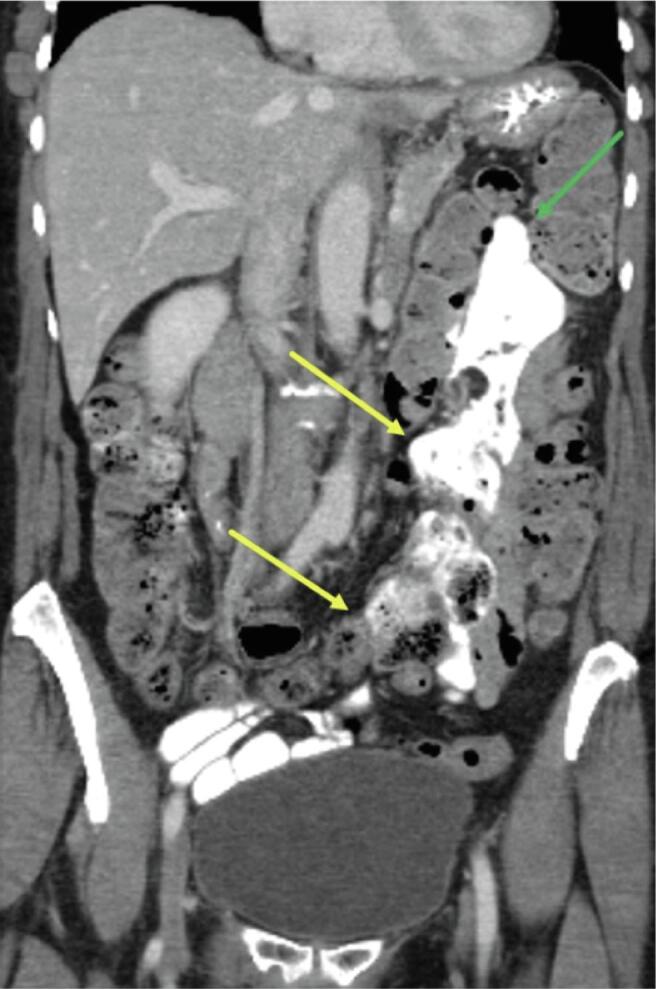
Fig. 3.
The post-operative day #3 contrast enhanced axial CT image through the abdomen and pelvis show a markedly dilated cecum now within the right abdomen (green arrow) with a “whirl sign” within the right lower quadrant (red arrow) consistent with a cecal volvulus. Foci of subcutaneous gas are expected post-operative sequela. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
After extubation in the OR, she was admitted to the intensive care unit after surgery for close monitoring of her respiratory status due to presence of postoperative atelectasis, pulmonary edema, and pleural effusions. The patient remained NPO, and nasogastric tube was placed in the OR. She received maintenance intravenous fluids and electrolytes repletion as needed. She was transferred out of the intensive care unit on postoperative day 2. Her course was complicated by an ileus that was managed conservatively and ultimately was stable for discharge home on postoperative day 12 from her bowel surgery.
3. Discussion
Laparoscopic surgery is now the most common surgical technique in most surgical specialties including gynecologic and general surgery. Cecal volvulus is a rare complication of laparoscopy; however, it has not been extensively studied after these procedures. It can have life-threatening ramifications if untreated including intestinal strangulation, ischemia, necrosis or perforation. Therefore, early recognition and intervention is essential.
Multiple etiologies of cecal volvulus have been implicated including prior abdominal surgery, abdominal masses, chronic constipation, and distal colon obstruction (Consorti and Liu, 2005). Some patients may be anatomically susceptible due to cecal hypermobility as a result of impaired fixation of the mesentery to the retroperitoneum (Kim et al., 2013). It has also been proposed that a cecal volvulus can occur after laparoscopy due to deflation of pneumoperitoneum causing increased laxity of the cecum (Geoghegan et al., 1994).
For this patient, cecal hypermobility had been noted on her preoperative imaging, placing her at higher risk for a volvulus (Fig. 1). It is possible that the dense retroperitoneal adhesions related to our patient’s previous appendectomy may have promoted development of a volvulus by providing a fixation point for rotation (Consorti and Liu, 2005). An appendectomy itself has been shown to increase cecal mobility as a result of freeing peritoneal attachments (Kim et al., 2013). Additionally, extensive right pelvic sidewall dissection was performed during this patient’s hysterectomy, leading to increased mobility of the cecum and may have also contributed. Another intraoperative factor that has not previously been mentioned is the possible effect of steep Trendelenberg positioning in a patient with pre-existing or surgically induced colonic hypermobility. This risk factor has not previously been described in the literature and cannot be definitively attributed as the cause, but it may be of benefit to visually ensure restoration of the colon's normal position for patients who have previously been identified as having cecal hypermobility or in whom mobilization of the ascending or descending colon has been required.
Cecal hypermobility intraoperatively would appear as a cecum that is loose on a stretched mesentery. The cecum is usually fixed at least partially in the right iliac fossa along with the white line of Toldt. Identifying any deviation from this characteristic location can be an effective strategy to identify possible risk of developing a volvulus. Although the preoperative CT for the patient showed significant colonic redundancy and the malpositioned cecum, intraoperatively the cecum had returned to the right abdomen. Other studies in patients with cecal hypermobility have found that cecal location can be dependent on patient positioning (Fukuda et al., 2017). This suggests that CT scan alone is situationally-dependent and may not be sensitive in assessing risk of post-operative volvulus. While it is valuable to consider other intraoperative signs, even with intraoperative recognition, cecopexy is not routinely performed at this time in otherwise asymptomatic patients. However, if there is concern for cecal hypermobility on imaging, it may be of benefit to screen for symptoms of mobile cecal syndrome as symptoms such as colicky right-sided pain or distention that resolve after flatus may be present in half of patients who develop volvulus and should be considered for concurrent cecopexy procedure (Zabeirou et al., 2019 Oct). This may serve as a prophylactic factor.
Given varying possible etiologies for this patient’s presentation, it is difficult to ascertain the exact cause, and it is likely that the constellation of risk factors led to the outcome in this case.
4. Conclusion
To our knowledge, this is the first reported case of cecal volvulus as a postoperative complication of scheduled robotic assisted hysterectomy and sentinel lymph node dissection. Given that minimally invasive surgery is increasingly utilized in gynecologic oncology, there may be some benefit in identifying patients at increased risk of a cecal volvulus and taking intraoperative factors into consideration. However, although a variety of predisposing factors for this complication have been identified, the exact cause is ultimately multifactorial and may not be preventable.
Consent:
An informed written consent was obtained from the patient for publication of this report and accompanying images. The patient has not consented for intraoperative photography.
CRediT authorship contribution statement
Divya Gowthaman: Writing – original draft. Lauren Scanlon: Writing – review & editing, Methodology. John C. McAuliffe: Writing – review & editing, Methodology. Shabnam Fidvi: Writing – review & editing, Methodology. Carly Schwartz: Writing – review & editing, Methodology. Sara S. Isani: Writing – review & editing, Visualization, Conceptualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Consorti E.T., Liu T.H. Diagnosis and treatment of caecal volvulus. Postgrad Med J. 2005;81:772–776. doi: 10.1136/pgmj.2005.035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duron J., Hay J.M., Msika S., et al. Prevalence and Mechanisms of Small Intestinal Obstruction Following Laparoscopic Abdominal Surgery: A Retrospective Multicenter Study. Arch Surg. 2000;135(2):208–212. doi: 10.1001/archsurg.135.2.208. [DOI] [PubMed] [Google Scholar]
- Ferguson L., Higgs Z., Brown S., McCarter D. McKay CJ Laparoendosc Adv Surg Tech a. 2008 Jun;18(3):405–410. doi: 10.1089/lap.2007.0027. [DOI] [PubMed] [Google Scholar]
- Fukuda Y, Higuchi Y, Shinozaki K, Tanigawa Y, Abe T, Hanaoka N, Matsubayashi S, Yamaguchi T, Kosho T, Nakamichi K. Mobile Cecum in a Young Woman with Ehlers-Danlos Syndrome Hypermobility type: A Case Report and Review of the Literature. Intern Med. 2017 Oct 15;56(20):2791-2796. doi: 10.2169/internalmedicine.8758-16. Epub 2017 Sep 15. PMID: 28924124; PMCID: PMC5675945. [DOI] [PMC free article] [PubMed]
- Geoghegan J.G., Maher M., McNally O.M., et al. Acute midgut volvulus following laparoscopic cholecystectomy. Surg Endosc. 1994;8:903. doi: 10.1007/BF00843467. [DOI] [PubMed] [Google Scholar]
- Hasbahceci M., Basak F., Alimoglu O. Cecal volvulus. Indian J Surg. 2012;74:476–479. doi: 10.1007/s12262-012-0432-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Nguyen S., Leung P., Divino C. Cecal bascule after laparoscopic ventral hernia repair. JSLS. 2013;17(3):484–486. doi: 10.4293/108680813X13693422521917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew H.M., Chin K. Caecal volvulus—an unusual cause of post-operative pain following gynaecological surgery. Journal of Obstetrics and Gynaecology. 2003;23(6):685–686. doi: 10.1080/01443610310001609588. [DOI] [PubMed] [Google Scholar]
- Rehfuss JP, Friedman JE, Tan SA, Lottenberg LL, Goldstein LE. Cecal volvulus caused by internal herniation after roux-en-y gastric bypass surgery. J Surg Case Rep. 2018;2018(9):rjy241. Published 2018 Sep 11. doi:10.1093/jscr/rjy241. [DOI] [PMC free article] [PubMed]
- Zabeirou A.A., Belghali H., Souiki T., Ibn Majdoub K., Toughrai I., Mazaz K. Acute cecal volvulus: A diagnostic and therapeutic challenge in emergency: A case report. Ann Med Surg (lond). 2019 Oct;31(48):69–72. doi: 10.1016/j.amsu.2019.10.021. PMID: 31737261; PMCID: PMC6849140. [DOI] [PMC free article] [PubMed] [Google Scholar]