Abstract
Background
Previous evidence showed a possible link of dyslipidemia with bone health. Nevertheless, the correlation of remnant cholesterol (RC) with bone mineral density (BMD) has yet to be well investigated. This study investigated the association of RC with total spine BMD in general Americans.
Methods
This study explored the relationship of RC with total spine BMD in subjects aged ≥ 20 years from the National Health and Nutrition Examination Survey (NHANES) 2013–2018. After adjusting for covariates, multivariate linear regression and stratified analyses were conducted to determine the correlation of serum RC with total spine BMD in adult Americans. Restricted cubic spline (RCS) was applied to examine the nonlinear association of serum RC with total spine BMD.
Results
This study included 3815 individuals ≥ 20 years old, 1905 (49.93%) of whom were men and 1910 (50.07%) of whom were women. After adjusting for all covariates, the results showed a negative relationship of serum RC with total spine BMD (β= -0.024, 95% CI: -0.039, -0.010). The interaction tests of age, sex, race, and BMI showed no statistically significant effects on the association. The RCS also indicated a negative linear correlation of serum RC with total spine BMD (nonlinear P = 0.068, overall P < 0.001). Moreover, RC had a stronger effect on total spine BMD than total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C).
Conclusions
This study found that serum RC was negatively related to total spine BMD in U.S. adults. These findings emphasized the important role of RC in bone health in American adults.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-024-02145-6.
Keywords: Bone mineral density, Remnant cholesterol, Americans, NHANES
Introduction
Osteoporosis, a common skeletal disorder in elderly individuals, is featured by low bone mineral density (BMD) and high fragility fracture risk [1]. A recent study indicated that 19.7% of the world’s population older than 50 years is suffering from osteoporosis [2]. As the population ages globally, this number still continues [3]. The increasing prevalence of osteoporosis is leading to high morbidity and mortality in elderly people around the world, placing significant health and economic burdens on society [3]. The development of osteoporosis can be attributed to two factors. The first aspect is the peak bone mass (PBM) accumulation during puberty, and the second is the bone mass loss in old age [4, 5]. Bone mass loss can be determined by various factors, including genetics, environment, diet, and others [5, 6]. Therefore, to reduce the high morbidity and mortality caused by osteoporosis in elderly individuals, it is essential to recognize and manage modifiable factors that contribute to osteoporosis.
Dyslipidemia is commonly observed in patients with osteoporosis and is thought to affect BMD by impairing circulation [7–9]. In a study of 4323 Koreans, Kim et al. [7] reported that serum triglyceride levels were negatively related to BMD in men aged > 50 years and postmenopausal women. Cao et al. [8] indicated that total cholesterol (TC) was negatively related to total BMD in U.S. young adults. Although several studies have demonstrated that triglyceride, low-density lipoprotein cholesterol (LDL-C), and TC are negatively correlated with BMD, the findings are not always consistent [10–12]. These inconsistent results limit the clinical utility of lipid biomarkers. There is an urgent need to explore new lipid parameters to predict osteoporosis and intervene.
Residual cholesterol (RC), the cholesterol in triglyceride-rich lipoproteins, is associated with various diseases, including metabolic, cardiovascular, and other disorders [13–15]. RC was shown to be an equal or even more reliable cardiovascular disease predictor than LDL-C or TC [16]. Although the role of RC in cardiovascular disease has been widely investigated, few studies have investigated the role of RC in bone health. An early study suggested that a reduction in the uptake of triglyceride-rich lipoproteins by osteoblasts leads to increased bone formation in mice [17]. In a northern Chinese cohort of 7,053 participants, Hou et al. [18] found that serum RC was negatively associated with BMD in men younger than 60 years after adjustment for a range of confounding factors. Therefore, RC may serve as a new marker of lipid metabolism to influence bone metabolism and BMD.
However, the relationship of RC with BMD has not been assessed in women or older people. In addition, no study has explored their relationship in Americans. Thus, this study aimed to assess the correlation of serum RC with total spine BMD in Americans aged ≥ 20 years from the National Health and Nutrition Examination Survey (NHANES) 2013–2018. We hypothesized that the serum RC is negatively related to total spine BMD.
Methods
Study design
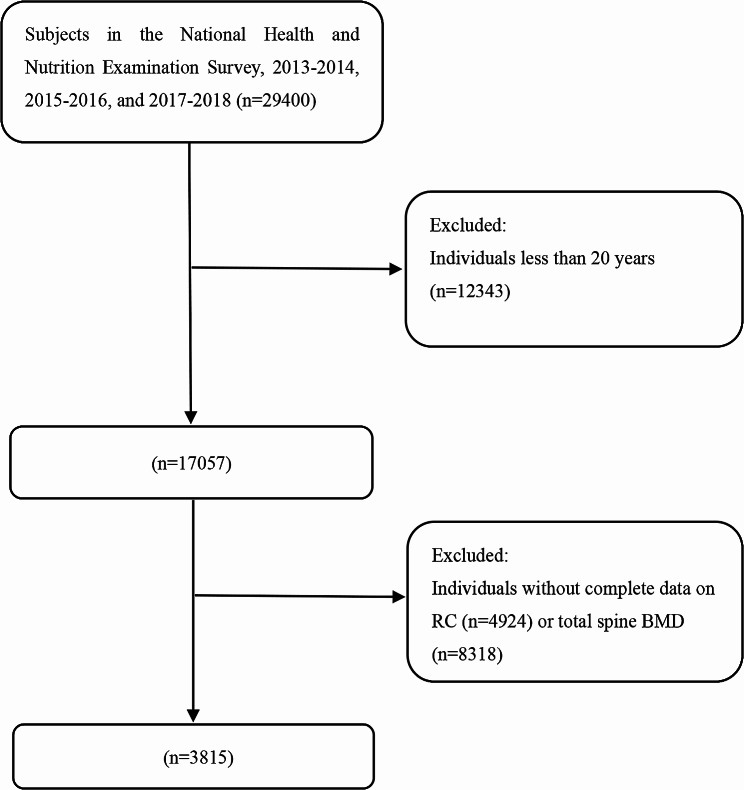
The NHANES is a national nutrition and health program that collects and publicly releases data biennially in the United States. In detail, the National Center for Health Statistics Ethics Review Committee provided ethical consent for the NHANES program. Each participant or their guardians signed informed consent forms for the NHANES programs. The latest three NHANES cycles were combined: 2013–2014, 2015–2016, and 2017–2018. Individuals aged 20 years or older were enrolled in this study. Initially, 29,400 individuals were enrolled in the NHANES 2013–2018. Then, 12,343 subjects were excluded because they were younger than 20 years, 8318 participants were excluded because of missing information on lumbar spine BMD, and 4924 participants were excluded because of missing RC information. Finally, 3815 individuals were enrolled in this study. The participant selection flowchart is displayed in Fig. 1.
Fig. 1.
Flowchart of participants selection. BMD: bone mineral density. RC: remnant cholesterol
Assessment of RC and BMD
RC was used as the exposure variable in this study. Peripheral blood was drawn from the subjects for analysis after they fasted for at least eight hours in the morning. Serum triglyceride and TC levels were analyzed using the enzymatic method. Serum High-density lipoprotein cholesterol (HDL-C) was assessed by heparin-manganese precipitation or a direct immunoassay technique method. Serum LDL-C was measured by the Friedwald calculation. Serum RC was determined using the formula [RC = TC- LDL-C - HDL-C], which was in accordance with previous research [19, 20].
The total spine BMD was assessed by dual-energy X-ray absorptiometry (DXA) using Hologic densitometers. Professionals collected and standardized BMD data. Total spine BMD was used as an outcome variable in this analysis. Detailed information on BMD can be found in the DXXLSBMD datasets on the NHANES website [21].
Covariates
Covariates were chosen based on the published study [22]. Variables such as race, age, sex, body mass index (BMI), blood urea nitrogen, total protein, serum calcium, serum vitamin D, serum phosphorus, serum uric acid, poverty income ratio (PIR), education level, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use were considered in the study. The PIR is a widely used indicator of family income. BMI was determined by dividing weight (in kilograms) by the square of height (in metres). Races were divided into five groups (Other Hispanic, Non-Hispanic Black, Mexican American, Other Race, and Non-Hispanic White). Education level was categorized into three categories (College degree or above, High school graduate, and Under high school). Total protein, blood urea nitrogen, serum total calcium, serum phosphorus, serum uric acid, and serum vitamin D were collected via laboratory measurements. Smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use were determined by questionnaires: Smoke at least 100 cigarettes in life? Have you ever had 5 or more drinks every day? Doctor told you had high blood diabetes? Ever told you had high blood pressure? How many days did you do moderate recreational activities in a typical week? Have you taken statins in the past 30 days? Detailed data on covariates can be seen at the NHANES website.
Statistical analysis
The present study used the mean ± standard deviation and percentages to represent continuous and categorical variables, respectively. The characteristics of participants were described based on serum RC quartile (Q1: ≤ 0.308 mmol/L, Q2: 0.309–0.464 mmol/L, Q3:0.465–0.699 mmol/L, Q4: ≥ 0.700 mmol/L). To compare differences between the characteristics of participants, the study used weighted linear regression models and weighted χ2 tests for continuous variables and categorical variables, respectively. Furthermore, multivariate linear regression analyses were performed to explore the relationship of RC with total spine BMD. Model 1 was built as an unadjusted model. Then, Model 2 was created by adjusting age, race, and sex. Finally, Model 3 was created by adjusting all variables of race, age, sex, BMI, blood urea nitrogen, total protein, serum calcium, serum vitamin D, serum phosphorus, serum uric acid, PIR, education level, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use. Then, the continuous variable serum RC was changed to a categorical variable (quartiles) to detect the correlation of RC with BMD. Stratified analyses and interaction tests were performed by sex (men and women), age (< 50 and ≥ 50), race (Other Hispanic, Non-Hispanic Black, Mexican American, Other Race, and Non-Hispanic White), and BMI (< 25, 25–30, > 30). To explore the effect of menopause on this relationship, further stratified analyses of menopausal women (premenopausal women and postmenopausal women) were conducted. Menopause was defined as the absence of menstruation in the past year because of hysterectomy or natural menopause/life change reasons [23]. The nonlinear association between RC and total spine BMD was detected by restricted cubic spline (RCS). All analyses were conducted by EmpowerStats (4.0) and R software (4.3.1) using MEC weight. A P value < 0.05 was deemed to indicate statistical significance.
Results
Baseline characteristics
A sample of 3815 subjects ≥ 20 years old were recruited for the present analyses; 1905 (49.93%) were men, and 1910 (50.07%) were women, with an average age of 39.78 ± 11.51 years. In the final analyses, 34.36% were Non-Hispanic White, 20.73% were Non-Hispanic Black, 18.77% were Other Race, 15.20% were Mexican American, and 10.93% were Other Hispanic. The mean serum RC of participants was 0.56 mmol/L. Individuals with higher RC were more likely to be women, older, Non-Hispanic White, Mexican American, less educated, poor, frequent smokers, diabetic, and hypertensive. They used more statins and had higher BMIs; serum uric acid, serum calcium, blood urea nitrogen, and serum vitamin D levels; and lower total spine BMD (Table 1).
Table 1.
Characteristics of the study population based on RC quartiles
| Remnant cholesterol (mmol/L) | ||||||
|---|---|---|---|---|---|---|
| total | Q1 (≤ 0.308) | Q2 (0.309–0.464) | Q3 (0.465–0.699) | Q4 (≥ 0.700) | P value | |
| Number of subjects (n) | 3815 | 933 | 965 | 959 | 958 | |
| Age (years) | 39.78 ± 11.51 | 36.34 ± 11.21 | 38.94 ± 11.73 | 41.37 ± 11.43 | 42.36 ± 10.70 | < 0.001 |
| Sex, n (%) | < 0.001 | |||||
| Men | 1905 (49.93%) | 442 (45.80%) | 491 (51.20%) | 583 (60.86%) | 389 (41.69%) | |
| Women | 1910 (50.07%) | 523 (54.20%) | 468 (48.80%) | 375 (39.14%) | 544 (58.31%) | |
| Race/ethnicity, n (%) | < 0.001 | |||||
| Mexican American | 580 (15.20%) | 91 (9.75%) | 140 (14.51%) | 163 (17.00%) | 186 (19.42%) | |
| Other Hispanic | 417 (10.93%) | 77 (8.25%) | 94 (9.74%) | 127 (13.24%) | 119 (12.42%) | |
| Non-Hispanic White | 1311 (34.36%) | 312 (33.44%) | 304 (31.50%) | 335 (34.93%) | 360 (37.58%) | |
| Non-Hispanic Black | 791 (20.73%) | 289 (30.98%) | 241 (24.97%) | 165 (17.21%) | 96 (10.02%) | |
| Other Race | 716 (18.77%) | 186 (19.27%) | 169 (17.62%) | 197 (20.56%) | 164 (17.58%) | |
| BMI | 29.15 ± 7.12 | 26.70 ± 6.72 | 28.80 ± 7.12 | 29.99 ± 7.23 | 31.06 ± 6.68 | < 0.001 |
| PIR | 2.50 ± 1.57 | 2.54 ± 1.54 | 2.49 ± 1.60 | 2.50 ± 1.58 | 2.46 ± 1.56 | 0.630 |
| Education, n (%) | < 0.001 | |||||
| < High school diploma | 717 (18.79%) | 136 (14.58%) | 153 (15.85%) | 199 (20.75%) | 229 (23.90%) | |
| High school diploma | 838 (21.97%) | 193 (20.69%) | 223 (23.11%) | 216 (22.52%) | 206 (21.50%) | |
| ≥Some college | 2260 (59.24%) | 604 (64.74%) | 589 (61.04%) | 544 (56.73%) | 523 (54.59%) | |
| Blood urea nitrogen (mmol/L) | 4.58 ± 1.63 | 4.45 ± 1.36 | 4.52 ± 1.69 | 4.63 ± 1.74 | 4.72 ± 1.68 | 0.002 |
| Serum calcium (mmol/L) | 2.33 ± 0.08 | 2.32 ± 0.08 | 2.33 ± 0.08 | 2.32 ± 0.08 | 2.33 ± 0.08 | 0.038 |
| Serum phosphorus (mmol/L) | 1.18 ± 0.18 | 1.18 ± 0.17 | 1.18 ± 0.18 | 1.17 ± 0.18 | 1.17 ± 0.18 | 0.443 |
| Total protein (g/L) | 71.71 ± 4.27 | 71.47 ± 4.26 | 71.65 ± 4.13 | 71.74 ± 4.35 | 71.97 ± 4.32 | 0.087 |
| Serum uric acid (umol/L) | 319.95 ± 83.24 | 287.26 ± 71.86 | 309.38 ± 75.82 | 330.06 ± 81.30 | 352.31 ± 88.72 | < 0.001 |
| Serum vitamin D (nmol/L) | 61.02 ± 25.18 | 59.67 ± 25.60 | 59.67 ± 24.31 | 61.99 ± 25.65 | 62.73 ± 25.05 | 0.010 |
| 4/5 or more drinks every day, n (%) | 0.072 | |||||
| Yes | 477 (12.50%) | 95 (10.18%) | 127 (13.16%) | 128 (13.35%) | 127 (13.26%) | |
| No | 2647 (69.38%)) | 668 (71.60%) | 644 (66.74%) | 658 (68.61%) | 677 (70.67%) | |
| No reported | 691 (18.11%) | 170 (18.22%) | 194 (20.10%) | 173 (18.04%) | 154 (16.08%) | |
| Smoked at least 100 cigarettes in life, n (%) | < 0.001 | |||||
| Yes | 1524 (39.95%) | 298 (31.94%) | 361 (37.41%) | 397 (41.40%) | 468 (48.85%) | |
| No | 2291 (60.05%) | 635 (68.06%) | 604 (62.59%) | 562 (58.60%) | 490 (51.15%) | |
| Every told you had high blood pressure, n (%) | < 0.001 | |||||
| Yes | 945 (24.77%) | 147 (15.76%) | 235 (24.35%) | 250 (26.07%) | 313 (32.67%) | |
| No | 2870 (75.23%) | 786 (84.24%) | 730 (75.65%) | 709 (73.93%) | 645 (67.33%) | |
| Doctor told you had high blood diabetes, n (%) | < 0.001 | |||||
| Yes | 281 (7.37%) | 25 (2.68%) | 55 (5.70%) | 74 (7.72%) | 127 (13.26%) | |
| No | 3449 (90.41%) | 892 (95.61%) | 891 (92.33%) | 854 (89.05%) | 812 (84.76%) | |
| Borderline | 85 (2.23%) | 16 (1.71%) | 19 (1.97%) | 31 (3.23%) | 19 (1.98%) | |
| Days moderate recreational activities in a typical week, n (%) | < 0.001 | |||||
| ≤ 3 | 1054 (27.63%) | 285 (30.55%) | 271 (28.08%) | 257 (26.80%) | 241 (25.16%) | |
| ≥ 4 | 627 (16.44%) | 192 (20.58%) | 173 (17.93%) | 146 (15.22%) | 116 (12.11%) | |
| No reported | 2134 (55.94%) | 456 (48.87%) | 521 (53.99%) | 556 (57.98%) | 601 (62.73%) | |
| Statin use, n (%) | < 0.001 | |||||
| Yes | 545 (14.29%) | 47 (5.04%) | 109 (11.30%) | 163 (17.00%) | 226 (23.59%) | |
| No | 3270 (85.71%) | 886 (94.96%) | 856 (88.70%) | 796 (83.00%) | 732 (76.41%) | |
| Total spine BMD (g/cm2) | 1.03 ± 0.15 | 1.05 ± 0.15 | 1.04 ± 0.15 | 1.03 ± 0.16 | 1.00 ± 0.14 | < 0.001 |
| Remnant cholesterol (mmol/L) | 0.56 ± 0.43 | 0.23 ± 0.05 | 0.38 ± 0.05 | 0.57 ± 0.07 | 1.06 ± 0.57 | < 0.001 |
Mean ± SD for continuous variables: the P value was calculated by the weighted linear regression model. (%) for categorical variables. The P value was calculated by the weighted chi-square test. Abbreviation: BMI: body mass index. PIR: poverty income ratio. BMD: bone mineral density. RC: remnant cholesterol.
Associations of serum RC with total spine BMD
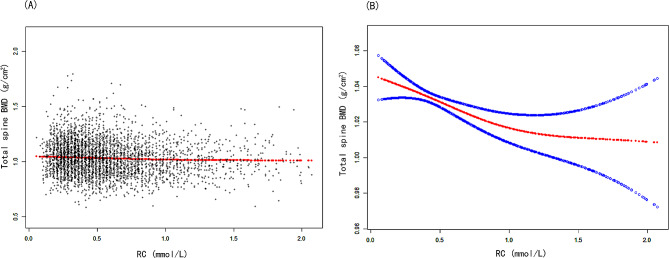
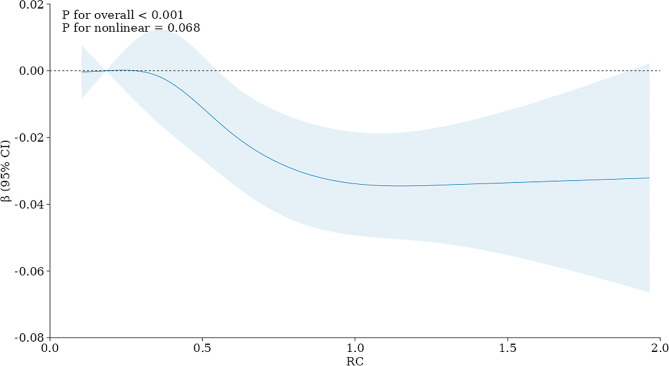
Models 1 and 2 revealed a negative association of RC with total spine BMD (Table 2). In Model 3, a negative correlation was also observed between serum RC and total spine BMD (β= -0.024, 95% CI: -0.039, -0.010). Figure 2 showed the smooth curve fittings of the correlation of serum RC with total spine BMD. Then, the continuous variable of RC was changed to a categorical variable (quartiles). According to Model 3, subjects in the highest quarter of serum RC have a significantly reduced BMD compared to subjects in the first quarter. (β= -0.024, 95% CI: -0.038, -0.010). Figure 3 showed the results of RCS. Consistent with the findings of the multivariate linear regression analyses, the dose–response association also indicated a negative linear association of serum RC with total spine BMD (nonlinear P = 0.068, overall P < 0.001) (Fig. 3).
Table 2.
The association between serum RC and total spine bone mineral density (g/cm2)
| Model 1 β (95% CI) P value | Model 2 β (95% CI) P value | Model 3 β (95% CI) P value | |
|---|---|---|---|
| RC | -0.044 (-0.058, -0.030) < 0.001 | -0.019 (-0.033, -0.005) 0.007 | -0.024 (-0.039, -0.010) < 0.001 |
| RC categories | |||
| Q1 | Reference | Reference | Reference |
| Q2 | -0.008 (-0.022, 0.005) 0.232 | 0.002 (-0.011, 0.015) 0.767 | -0.001 (-0.014, 0.013) 0.997 |
| Q3 | -0.025 (-0.038, -0.011) < 0.001 | -0.005 (-0.018, 0.009) 0.496 | -0.008 (-0.022, 0.006) 0.249 |
| Q4 | -0.045 (-0.059, -0.031) < 0.001 | -0.018 (-0.031, -0.004) 0.011 | -0.024 (-0.038, -0.010) 0.001 |
| P for trend | < 0.001 | 0.007 | < 0.001 |
| Subgroup analysis stratified by sex | |||
| Men | -0.045 (-0.063, -0.026) < 0.001 | -0.028 (-0.046, -0.010) 0.002 | -0.030 (-0.050, -0.011) < 0.001 |
| Women | -0.049 (-0.070, -0.027) < 0.001 | -0.019 (-0.042, 0.003) 0.097 | -0.011 (-0.034, 0.012) 0.351 |
| P for interaction | 0.741 | 0.135 | 0.173 |
| Stratified analysis by race/ethnicity | |||
| Mexican American | -0.029 (-0.060, 0.002) 0.066 | -0.022 (-0.054, 0.009) 0.168 | -0.018 (-0.050, 0.013) 0.256 |
| Other Hispanic | -0.030 (-0.071, 0.012) 0.159 | -0.024 (-0.066, 0.019) 0.274 | -0.019 (-0.064, 0.026) 0.402 |
| Non-Hispanic White | -0.030 (-0.051, -0.009) 0.005 | -0.024 (-0.045, -0.002) 0.033 | -0.030 (-0.053, -0.007) 0.010 |
| Non-Hispanic Black | -0.005 (-0.024, 0.015) 0.650 | -0.002 (-0.022, 0.017) 0.810 | -0.012 (-0.059, 0.036) 0.624 |
| Other races (Including multi-racial) | -0.025 (-0.053, 0.002) 0.074 | -0.023 (-0.052, 0.006) 0.117 | -0.030 (-0.061, 0.001) 0.056 |
| P for interaction | 0.324 | 0.533 | 0.767 |
| Stratified analysis by age | |||
| < 50 | -0.029 (-0.041, -0.016) < 0.001 | -0.026 (-0.042, -0.010) 0.001 | -0.033 (-0.049, -0.016) < 0.001 |
| ≥ 50 | -0.010 (-0.037, 0.016) 0.438 | 0.004 (-0.023, 0.031) 0.787 | -0.010 (-0.039, 0.019) 0.484 |
| P for interaction | 0.212 | 0.025 | 0.148 |
| Stratified analysis by BMI | |||
| < 25 | -0.086 (-0.173, 0.000) 0.053 | -0.045 (-0.078, -0.012) 0.007 | -0.030 (-0.042, -0.018) < 0.001 |
| 25–30 | -0.045 (-0.078, -0.012) 0.007 | -0.009 (-0.042, 0.024) 0.580 | -0.033 (-0.057, -0.010) 0.008 |
| > 30 | -0.031 (-0.044, -0.019) < 0.001 | -0.032 (-0.067, 0.002) 0.068 | -0.021 (-0.044, -0.003) 0.040 |
| P for interaction | 0.439 | 0.692 | 0.377 |
Model 1 adjusted no covariates. Model 2 adjusted age, sex, and race. Model 3 adjusted age, sex, race, PIR, education level, BMI, total protein, blood urea nitrogen, serum total calcium, serum phosphorus, serum uric acid, serum vitamin D, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use. Abbreviation: BMI: body mass index. PIR: poverty income ratio. BMD: bone mineral density. RC: remnant cholesterol.
Fig. 2.
The association between poverty RC and total spine BMD. (A) Each black point represents a sample. (B) Red line represents the smooth curve fit between variables. Blue lines represent the 95% of confidence interval from the fit. Age, sex, race, PIR, education level, BMI, total protein, blood urea nitrogen, serum total calcium, serum phosphorus, serum uric acid, serum vitamin D, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use were adjusted. Abbreviation: PIR: poverty income ratio. BMI: body mass index. BMD: bone mineral density. RC: remnant cholesterol
Fig. 3.
Restricted cubic spline (RCS) analysis with multivariate-adjusted associations between RC and total spine BMD. Age, sex, race, PIR, education level, BMI, total protein, blood urea nitrogen, serum total calcium, serum phosphorus, serum uric acid, serum vitamin D, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use were adjusted. Abbreviation: PIR: poverty income ratio. BMI: body mass index. BMD: bone mineral density. RC: remnant cholesterol
Stratified analysis and interaction testing
Stratified analysis and interaction tests were conducted for age, sex, race, and BMI (Table 2). The interaction tests showed that those subgroups had no significant effect on the relationship (P for interaction > 0.05). In Model 3, the results revealed a negative correlation of RC with total spine BMD in men (β= − 0.030, 95% CI: − 0.050, − 0.011) but not in women (β= − 0.011, 95% CI: − 0.034, 0.012). However, no interaction effect was found (P for interaction = 0.173). For race, the results found the negative association was stronger in Non-Hispanic White (β= − 0.030, 95% CI: − 0.053, − 0.007) than others. Nevertheless, the results found no interaction effect (P for interaction = 0.767). For age groups, the results showed a negative association of RC with total spine BMD in individuals aged < 50 years (β= − 0.033, 95% CI: − 0.049, − 0.016) but not in individuals aged ≥ 50 years (β= − 0.010, 95% CI: − 0.039, 0.019). (P for interaction = 0.148). For all three BMI groups, the results indicated a negative correlation of serum RC with total spine BMD: BMI < 25: (β= -0.030, 95% CI: -0.042, -0.018); 25 ≤ BMI ≤ 30: (β= -0.033, 95% CI: -0.057, -0.010); BMI > 30: (β= -0.021, 95% CI: -0.044, -0.003). Further stratified analyses were conducted by menopause status in women (Appendix 1). The results showed that menopause status has no interaction effect on the correlation of serum RC with total spine BMD in women (P for interaction = 0.582).
The effect of TC, LDL-C, HDL-C, and RC on total spine BMD
The effects of RC and classical lipid composition on total spine BMD were compared (Table 3). RC had a greater impact on BMD than did TC, LDL-C, or HDL-C. According to the fully adjusted model, every unit increase in TC, LDL-C, and RC was related to decreases in total spine BMD of 0.010, 0.013, and 0.024 g/cm2, respectively. Every unit increase in HDL-C was related to a 0.022 g/cm2 increase in total spine BMD.
Table 3.
The effect of TC, LDL-C, HDL-C, and RC on total spine BMD (g/cm2)
| Exposure | Model 1 β (95% CI) P value | Model 2 β (95% CI) P value | Model 3 β (95% CI) P value |
|---|---|---|---|
| TC | -0.017 (-0.021, -0.012) < 0.001 | -0.011 (-0.016, -0.007) < 0.001 | -0.010 (-0.015, -0.005) < 0.001 |
| LDL-C | -0.018 (-0.024, -0.013) < 0.001 | -0.014 (-0.019, -0.009) < 0.001 | -0.013 (-0.018, -0.007) < 0.001 |
| HDL-C | 0.020 (0.008, 0.032) 0.001 | 0.014 (0.002, 0.027) 0.023 | 0.022 (0.009, 0.035) 0.002 |
| RC | -0.044 (-0.058, -0.030) < 0.001 | -0.019 (-0.033, -0.005) 0.007 | -0.024 (-0.039, -0.010) < 0.001 |
Model 1 adjusted no covariates. Model 2 adjusted age, sex, and race. Model 3 adjusted age, sex, race, PIR, education level, BMI, total protein, blood urea nitrogen, serum total calcium, serum phosphorus, serum uric acid, serum vitamin D, smoking and drinking behaviors, high pressure, diabetes, physical activities, and statin use. Abbreviation: BMD: bone mineral density. TC: total cholesterol. LDL-C: low-density lipoprotein cholesterol. HDL-C: high-density lipoprotein cholesterol. RC: remnant cholesterol. BMI: body mass index. PIR: poverty income ratio.
Discussion
This study first explored the correlation of serum RC with BMD in U.S. adults. The results showed a negative correlation of serum RC with total spine BMD in Americans aged ≥ 20 years old. The interaction tests showed that the age, sex, race, and BMI subgroups had no significant effect on the relationship. Dose-response analysis by RCS also confirmed a negative linear relationship between serum RC and BMD. These findings emphasize the critical role of RC in bone health.
RC includes cholesterol in very low-density lipoproteins (VLDLs), cholesterol in celiac residue in the postprandial state, and intermediate-density lipoproteins (IDLs) in the fasting state. Many recent NHANES studies have identified RC as a biomarker of various diseases [24–27]. In a survey of 7777 subjects from the NHANES 1999–2008, Yan et al. [24] reported a positive association between serum RC and rheumatoid arthritis (RA). Thus, RC may serve as an essential predictor of RA occurrence. Zhang et al. [25] found that RC was positively associated with cardiovascular mortality in a cohort of 19,650 individuals from the NHANES 1999–2014. This positive association was independent of traditional risk factors like HDL-C and LDL-C. He et al. [26] established a link between RC and albuminuria or renal function. They found a negative correlation between serum RC and eGFR (β= -2.12, 95% CI: -3.04, -1.21). Xie et al. [19] observed that serum RC was negatively associated with memory function and verbal learning in individuals aged ≥ 60 years. Therefore, lower levels of RC may be beneficial for preventing cognitive impairment in older adults. In another study by Chen et al. [27], a nonlinear association between RC and nonalcoholic fatty liver disease (NAFLD) was found. Risk ratios for NAFLD on the left and right sides of the inflection point are 3.88 (95% CI: 2.43–6.2) and 0.59 (95% CI: 0.21–1.71). Nevertheless, the possible link between RC and BMD has not been well explained. Hou et al. [18] investigated the correlation of RC with BMD in 7053 Chinese men, and they indicated that serum RC was negatively related to hip BMD. Every one mmol/l increase in RC was related to a 0.0079 g/cm2 decrease in hip BMD. Furthermore, compared with people of the lowest serum RC quartile, people of the highest serum RC quartile have a 1.43-fold risk of low bone mass. However, the subjects in this study were only middle-aged men. It is well known that advanced age and women are high-risk factors for osteoporosis. Therefore, the correlation of RC with BMD in older people and women is still unknown. This study first indicated a negative correlation of RC with BMD in Americans ≥ 20 years. Furthermore, the interaction tests showed that age and sex have no interaction effects on the final results (P for interaction > 0.05). Thus, RC may serve as a novel lipid metabolism marker to predict bone health in the population.
Although no studies have investigated the mechanisms of RC in bone metabolism, many basic investigations have assessed the impacts of classical lipid metabolism on bone health. Overall, the effect of abnormal lipid metabolism on bone health is complex and involves several factors. Both osteoblasts and adipocytes are derived from the differentiation of mesenchymal stem cells (MSCs) [28]. The Wnt/β-catenin signalling pathway regulates this differentiation process [29]. When this pathway is blocked, MSCs will favour adipocyte differentiation. In a study by Pelton et al. [30], after four months of feeding, mice fed a high-cholesterol diet showed significantly reduced femoral and cranial BMD compared to those fed a low- or no-cholesterol diet. They also suggested that high cholesterol intake could inhibit osteoblast differentiation and enhance osteoclast function in mice [30]. Furthermore, high TC and LDL-C can increase bone marrow microcirculatory stress and decrease bone vascularization, leading to bone loss [31].
Epidemiological studies have also widely discussed the relationship of lipid profiles with BMD. Most studies showed a negative or no correlation of LDL-C and TC with BMD [7, 32, 33]. The adverse effects of LDL-C and TC on bone health can often be attributed to vascular calcification and atherosclerosis [34, 35]. However, studies showed a positive, negative, or no correlation between HDL-C and BMD [36–39]. In a study by Sun et al. [38], their survey indicated that HDL-C was negatively related to lumbar BMD after adjusting a large range of confounders. However, Zolfaroli et al. [39] found a positive correlation of HDL-C with total spine and femur neck BMD in postmenopausal females. These differences may be explained in part by differences in study population, study methodology, or error control. In total, the relationship between traditional lipid profiles and BMD has been controversial in previous studies. This study identified a negative association of serum RC, TC, and LDL-C with total spine BMD in U.S. adults, with the effect of RC being stronger. In contrast, HDL-C was found to have a positive association. Thus, RC could be a new predictor of low BMD in clinical practice.
Strengths and limitations
The study has a variety of strengths. First, this study first assessed the correlation of RC with BMD in U.S. adults. The study used data from the recent cycles in the NHANES 2013–2018, which represent the general American population. Second, this study suggested that RC may serve as a new bone health marker, revealing the importance of lipid metabolism disorders in the mechanisms of bone loss. Third, linear regression analyses were conducted after adjusting for a large number of confounders. In addition, the nonlinear RCS test made the results more reliable.
The present study also has several limitations. First, some confounders in this study were collected through questionnaires and recall, which may suffer from recall bias and lead to inaccuracies. Second, although the study adjusted for many confounders, there remains the possibility of residual confounding. Third, the results cannot be used to make causal inferences because of the nature of cross-sectional studies. Further prospective studies are required to validate their causal inferences.
Conclusions
This study indicated a negative correlation of serum RC with total spine BMD in U.S. adults. Moreover, RC showed a stronger effect on total spine BMD than TC, LDL-C, and HDL-C. The finding emphasized the important role of RC in bone health in Americans. RC may be a new indicator for the early detection and prevention of osteoporosis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1. Appendix 1: stratified analysis by menopause status in women
Acknowledgements
We acknowledge the data from the National Health and Nutrition Examination Survey (NHANES).
Abbreviations
- RC
Remnant cholesterol
- BMD
Bone mineral density
- RCS
Restricted cubic spline
- NHANES
National Health and Nutrition Examination Survey
- LDL-C
Low-density lipoprotein cholesterol
- TC
Total cholesterol
- HDL-C
High-density lipoprotein cholesterol
- PBM
Peak bone mass
- PIR
Poverty income ratio
- BMI
Body mass index
- VLDLs
Very low-density lipoproteins
- IDLs
Intermediate-density lipoproteins
- RA
Rheumatoid arthritis
- NAFLD
Nonalcoholic fatty liver disease
- MSCs
Mesenchymal stem cells
Author contributions
Conceptualization, Peilun Xiao, Ye Tian; Data curation, Peilun Xiao, Zhihang Wang, Zeyao Lu; Formal analysis, Peilun Xiao, Zhihang Wang, Zeyao Lu; Investigation, Peilun Xiao, Ying Xu, Ye Tian; Methodology, Peilun Xiao, Zhihang Wang, Zeyao Lu; Project administration, Peilun Xiao, Ye Tian; Software, Peilun Xiao, Shijia Liu, Chongjun Huang, Ye Tian; Visualization, Peilun Xiao, Ye Tian; Writing – original draft, Peilun Xiao, Zhihang Wang, Zeyao Lu; Writing – review & editing, Peilun Xiao, Ye Tian.
Funding
This work was supported in part by the following grants: the National Natural Science Foundation of China (Grant No. 82271294) to YX, the Natural Science Foundation of Liaoning Province (Grant No. 2021-MS-201) to YX, the Applied Basic Research Program of Liaoning Province (Grant No. 2022JH2/101500050) to YT, the Basic Scientific Research Projects of Liaoning Provincial Department of Education (Grant No. LJKMZ20221164) to YT. The funder has a no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript, this should be declared.
Data availability
The datasets generated and/or analysed during the current study are available in the [NHANES] repository, [https://www.cdc.gov/nchs/nhanes/].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ying Xu, Email: xuy5@sj-hospital.org.
Ye Tian, Email: tiany3@sj-hospital.org.
References
- 1.Ensrud KE, Crandall CJ, Osteoporosis Ann Intern Med. 2024;177:Itc1–16. doi: 10.7326/AITC202401160. [DOI] [PubMed] [Google Scholar]
- 2.Xiao PL, Cui AY, Hsu CJ, et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos Int. 2022;33:2137–53. doi: 10.1007/s00198-022-06454-3. [DOI] [PubMed] [Google Scholar]
- 3.Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA. Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos Int. 2017;28:1979–88. doi: 10.1007/s00198-017-3996-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akhiiarova K, Khusainova R, Minniakhmetov I, Mokrysheva N, Tyurin A. Peak Bone Mass Formation: Mod View Problem Biomedicines 2023;11. [DOI] [PMC free article] [PubMed]
- 5.Lo JC, Yang W, Park-Sigal JJ, Ott SM. Osteoporosis and fracture risk among older US Asian adults. Curr Osteoporos Rep. 2023;21:592–608. doi: 10.1007/s11914-023-00805-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rizzoli R, Biver E, Brennan-Speranza TC. Nutritional intake and bone health. Lancet Diabetes Endocrinol. 2021;9:606–21. doi: 10.1016/S2213-8587(21)00119-4. [DOI] [PubMed] [Google Scholar]
- 7.Kim J, Ha J, Jeong C, et al. Bone mineral density and lipid profiles in older adults: a nationwide cross-sectional study. Osteoporos Int. 2023;34:119–28. doi: 10.1007/s00198-022-06571-z. [DOI] [PubMed] [Google Scholar]
- 8.Cao L, Wu W, Deng X, Guo H, Pu F, Shao Z. Association between total cholesterol and total bone mineral density in US adults: National Health and Nutrition Examination Survey (NHANES), 2011–2018. J Orthop Surg Res. 2023;18:40. doi: 10.1186/s13018-022-03485-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ohta H, Uemura Y, Sone T, et al. Effect of bone resorption inhibitors on serum cholesterol level and fracture risk in osteoporosis: Randomized comparative study between Minodronic Acid and Raloxifene. Calcif Tissue Int. 2023;112:430–9. doi: 10.1007/s00223-023-01060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li S, Guo H, Liu Y, et al. Relationships of serum lipid profiles and bone mineral density in postmenopausal Chinese women. Clin Endocrinol (Oxf) 2015;82:53–8. doi: 10.1111/cen.12616. [DOI] [PubMed] [Google Scholar]
- 11.Tang Y, Wang S, Yi Q, Xia Y, Geng B. High-density lipoprotein cholesterol is negatively correlated with bone Mineral density and has potential predictive value for bone loss. Lipids Health Dis. 2021;20:75. doi: 10.1186/s12944-021-01497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Q, Zhou J, Wang Q, et al. Association between Bone Mineral Density and lipid Profile in Chinese women. Clin Interv Aging. 2020;15:1649–64. doi: 10.2147/CIA.S266722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li ZH, Hao QY, Zeng YH, et al. Remnant cholesterol and the risk of aortic valve calcium progression: insights from the MESA study. Cardiovasc Diabetol. 2024;23:20. doi: 10.1186/s12933-023-02081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu X, Qiu W, He H, Zhao G, Liu J. Associations of the triglyceride-glucose index and remnant cholesterol with coronary artery disease: a retrospective study. Lipids Health Dis. 2024;23:45. doi: 10.1186/s12944-024-02036-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian Y, Wu Y, Qi M, et al. Associations of remnant cholesterol with cardiovascular and cancer mortality in a nationwide cohort. Sci Bull (Beijing) 2024;69:526–34. doi: 10.1016/j.scib.2023.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Guo DC, Gao JW, Wang X et al. Remnant cholesterol and risk of incident hypertension: a population-based prospective cohort study. Hypertens Res 2024. [DOI] [PubMed]
- 17.Schilling AF, Schinke T, Münch C, et al. Increased bone formation in mice lacking apolipoprotein E. J Bone Min Res. 2005;20:274–82. doi: 10.1359/JBMR.041101. [DOI] [PubMed] [Google Scholar]
- 18.Hou X, Tian F, Guo L et al. Remnant cholesterol is associated with hip BMD and low bone mass in young and middle-aged men: a cross-sectional study. J Endocrinol Invest 2024. [DOI] [PubMed]
- 19.Xie YY, Zhao L, Gao LJ, et al. Association between remnant cholesterol and verbal learning and memory function in the elderly in the US. Lipids Health Dis. 2022;21:120. doi: 10.1186/s12944-022-01729-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y, Shen R. Association of remnant cholesterol with depression among US adults. BMC Psychiatry. 2023;23:259. doi: 10.1186/s12888-023-04770-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.https://www.cdc.gov/nchs/nhanes/.
- 22.Xiao PL, Fuerwa C, Hsu CJ, et al. Socioeconomic status influences on bone mineral density in American men: findings from NHANES 2011–2020. Osteoporos Int. 2022;33:2347–55. doi: 10.1007/s00198-022-06498-5. [DOI] [PubMed] [Google Scholar]
- 23.Liu J, Tian C, Tang Y, Geng B. Associations of the serum vitamin D with mortality in postmenopausal women. Clin Nutr. 2024;43:211–7. doi: 10.1016/j.clnu.2023.11.041. [DOI] [PubMed] [Google Scholar]
- 24.Yan Y, La R, Jiang M, et al. The association between remnant cholesterol and rheumatoid arthritis: insights from a large population study. Lipids Health Dis. 2024;23:38. doi: 10.1186/s12944-024-02033-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang K, Qi X, Zhu F, et al. Remnant cholesterol is associated with cardiovascular mortality. Front Cardiovasc Med. 2022;9:984711. doi: 10.3389/fcvm.2022.984711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He X, Zou R, Du X, Li K, Sha D. Association of remnant cholesterol with decreased kidney function or albuminuria: a population-based study in the U.S. Lipids Health Dis. 2024;23:2. doi: 10.1186/s12944-023-01995-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen J, Su Y, Su X, Luo F. Remnant cholesterol has a non-linear association with non-alcoholic fatty liver disease. Diabetes Res Clin Pract. 2023;201:110733. doi: 10.1016/j.diabres.2023.110733. [DOI] [PubMed] [Google Scholar]
- 28.Katzmarzyk PT, Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Gimble JM. Relationship between abdominal fat and bone mineral density in white and African American adults. Bone. 2012;50:576–9. doi: 10.1016/j.bone.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ge J, Yu YJ, Li JY, et al. Activating Wnt/β-catenin signaling by autophagic degradation of APC contributes to the osteoblast differentiation effect of soy isoflavone on osteoporotic mesenchymal stem cells. Acta Pharmacol Sin. 2023;44:1841–55. doi: 10.1038/s41401-023-01066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pelton K, Krieder J, Joiner D, Freeman MR, Goldstein SA, Solomon KR. Hypercholesterolemia promotes an osteoporotic phenotype. Am J Pathol. 2012;181:928–36. doi: 10.1016/j.ajpath.2012.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zeng X, Zhan K, Zhang L, et al. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J Orthop Surg Res. 2017;12:30. doi: 10.1186/s13018-017-0532-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Makovey J, Chen JS, Hayward C, Williams FM, Sambrook PN. Association between serum cholesterol and bone mineral density. Bone. 2009;44:208–13. doi: 10.1016/j.bone.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 33.Cui LH, Shin MH, Chung EK, et al. Association between bone mineral densities and serum lipid profiles of pre- and post-menopausal rural women in South Korea. Osteoporos Int. 2005;16:1975–81. doi: 10.1007/s00198-005-1977-2. [DOI] [PubMed] [Google Scholar]
- 34.Cui R, Sun SQ, Zhong N, et al. The relationship between atherosclerosis and bone mineral density in patients with type 2 diabetes depends on vascular calcifications and sex. Osteoporos Int. 2020;31:1135–43. doi: 10.1007/s00198-020-05374-4. [DOI] [PubMed] [Google Scholar]
- 35.Xu X, Zhang M, Fei Z, Sheng H, Qu S, Cui R. Calcification of lower extremity arteries is related to the presence of osteoporosis in postmenopausal women with type 2 diabetes mellitus: a cross-sectional observational study. Osteoporos Int. 2021;32:1185–93. doi: 10.1007/s00198-020-05775-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solomon DH, Avorn J, Canning CF, Wang PS. Lipid levels and bone mineral density. Am J Med. 2005;118:1414. doi: 10.1016/j.amjmed.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 37.Jeong IK, Cho SW, Kim SW, et al. Lipid profiles and bone mineral density in pre- and postmenopausal women in Korea. Calcif Tissue Int. 2010;87:507–12. doi: 10.1007/s00223-010-9427-3. [DOI] [PubMed] [Google Scholar]
- 38.Sun Y, Qi X, Wang X, et al. Association between high-density lipoprotein cholesterol and lumbar bone mineral density in Chinese: a large cross-sectional study. Lipids Health Dis. 2024;23:27. doi: 10.1186/s12944-024-02023-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zolfaroli I, Ortiz E, García-Pérez M, Hidalgo-Mora JJ, Tarín JJ, Cano A. Positive association of high-density lipoprotein cholesterol with lumbar and femoral neck bone mineral density in postmenopausal women. Maturitas. 2021;147:41–6. doi: 10.1016/j.maturitas.2021.03.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1. Appendix 1: stratified analysis by menopause status in women
Data Availability Statement
The datasets generated and/or analysed during the current study are available in the [NHANES] repository, [https://www.cdc.gov/nchs/nhanes/].