Abstract
This study aimed to explore the perception of an underutilised collaborative information system through qualitative research, utilizing semi-structured, in-depth interviews with independent midwives and physician. PROSPERO, is a collaborative information system designed to bridge the communication gap between community-based healthcare workers and hospital-based care teams for parturients in Lyon, France. Through 27 semi-structured in-depth interviews with midwives, obstetricians, and general practitioners, we identified key themes related to the system’s adoption: implementation challenges, utilisation barriers, interprofessional dynamics, and hidden variables affecting system use. Participants recognised the potential of PROSPERO to improve information sharing and care coordination but expressed concerns about the system’s integration into existing workflows, time constraints, and the need for adequate training and technical support. Interprofessional dynamics revealed differing perspectives between hospital and independent practitioners, emphasising the importance of trust-building and professional recognition. Hidden variables, such as hierarchical influences and confidentiality concerns, further complicated the system’s adoption. Despite the consensus on the benefits of a collaborative information system, its implementation was hindered by mistrust between healthcare workers (i.e. between independent practitioners and hospital staff). Our findings suggest that fostering trust and addressing the identified barriers are crucial steps towards successful system implementation. The study contributes to understanding the complex interplay of factors influencing the adoption of collaborative healthcare technologies and highlights the need for strategies that support effective interprofessional collaboration and communication.
ClinicalTrials ID NCT02593292.
Subject terms: Health services, Epidemiology
Introduction
Antenatal care models worldwide are shaped by diverse cultural, systemic, and professional paradigms, leading to varied dynamics between midwives and physicians. Building on Buchet and Strauss’s1 concept of evolving professional segments through internal movements and conflicts, current perinatal care often embodies both collaboration and contention. This dynamic is exemplified in the Swiss context by Cavalli and Gouilhers (2014) and in Turkey by Topçu (2019), who reveal the paradoxical trend of ‘vaginarean’ births2,3. These are vaginal deliveries conducted with the extensive use of medical technology, similar to caesarean sections, yet paradoxically viewed as risky2. Cavalli and Gouilhers3 also highlight tensions between midwives and doctors in Switzerland, pointing to conflicts over competency recognition. Despite scientific advocacy for midwife-led models by Sandall et al.4, these complex interprofessional interactions require a nuanced understanding to enhance prenatal care. France’s unique healthcare system provides a pertinent backdrop to explore these global insights.
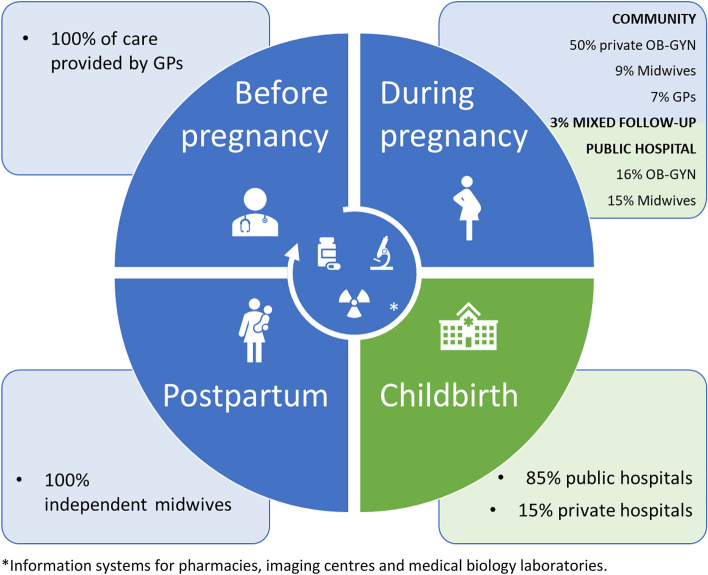
In 2021, France reported a fertility rate of 1.84 live births per woman, marking the highest among European Union member states and highlighting its unique standing in the field of childbirth and perinatal care within the European Union. This statistic positions France at the forefront of European nations in terms of birth rates, indicative of its strong healthcare infrastructure and the socio-cultural factors that influence family planning decisions. Despite witnessing approximately 723,000 births in 2022, France is observing a gradual decline in birth numbers compared to previous years5. The French healthcare system is characterised by a professional segmentation not only among healthcare workers but also between private and public sectors, as well as between community practices and hospital or clinic-based care. As Fig. 1 illustrates, while 50% of antenatal care is administered by private obstetrician-gynaecologists, a majority of childbirths take place within the public sector, predominantly in public hospitals6,7. This duality within the system, reflecting both Beveridge and Bismarckian models, underscores the urgency for a unified collaborative information system to bridge the divide, improving coordination and integration across different care settings8.
Figure 1.
Perinatal health care with diverse healthcare workers and their distinct medical information systems in France (2016, before intervention).
To reduce the communication gap between community care and hospital services in the French healthcare system, we initiated and implemented the Program of Research for the Optimisation of a Supervised Parturient Pathway for Expectant Women according to their Risk in Obstetrics (PROSPERO). The endeavour to foster a collaborative information-sharing framework among independent healthcare workers presents a multifaceted challenge, necessitating robust interprofessional cooperation and dialogue between healthcare workers and information technology specialists9,10. To address these challenges, the PROSPERO programme, collaboratively designed and developed with community healthcare workers, hospital staff, and service users, sought not only to optimise the care pathway for expectant women but also to enhance medical information sharing among healthcare workers. PROSPERO is a web-based platform to streamline the medical data sharing among community providers, hospital personnel, and women. The platform proposed a tailored clinical route, predicated on early pregnancy medico-psycho-social risk assessment in hospitals, aligning with hospital caregivers’ view of pregnancy as inherently risky11.
We crafted PROSPERO with four primary structured form categories: Staturo-Ponderal Evolution, Vitals, Functional Signs, and Obstetric and Pelvic Exam, complemented by a free text field for detailed notes and consultation actions. Pre-tests revealed that completing the form takes 3 to 10 min. The platform’s dual SMS authentication, while extending login time marginally, significantly enhances data security. Community healthcare workers initially faced challenges adjusting to the new workflow, particularly when integrating with existing software. However, the secure data hosting on the Hospital Civils of Lyon’s servers ensures strict adherence to French and European data protection regulations.
The programme’s pilot phase, focusing on reliability testing without comprehensive evaluations from healthcare workers or women, places it in the early stages of the Clinical Adoption Meta-Model (CAMM), specifically in the “Preparation” and “Exploration” phases12. During these stages, the emphasis is on understanding the technology’s potential, ensuring its reliability, and identifying the initial reactions from potential users. The core components and objectives of PROSPERO are presented in Table 1 according to HITO (Health Information Technology Ontology) recommendations13. Despite collaboration with healthcare workers across sectors, the uptake by community providers was minimal, prompting us to involve a sociologist for an in-depth qualitative analysis to uncover the reasons for the limited use of the PROSPERO programme.
Table 1.
Description of PROSPERO aligned with HITO classes.
| Aspect | Description of PROSPERO |
|---|---|
| Software product | Programme of research for the optimisation of a supervised parturient pathway for expectant women according to their risk in obstetrics (PROSPERO) |
| Feature |
1. Risk assessment tools for healthcare workers and pregnant women 2. Secure information-sharing capabilities including consultation reports, ultrasound images, and lab results 3. Tools for shared clinical pathway management |
| Application system type | Web-based health information system |
| Organisational unit | Maternity care departments within community and hospital settings |
| User group | Midwives, general practitioners, specialists, and pregnant women—both community and hospital-based |
The primary aim of this study is therefore to understand this failure by exploring the perception of this collaborative information system through a qualitative study that collected data using semi-structured in-depth interviews of independent midwives and physicians.
Methods
All interviews were conducted by a male sociologist (FM) with a PhD, specialised in the sociology of work and health, collaborating with our research team. He had experience in the health field (direct observations in psychiatric wards, conducting focus groups with cystic fibrosis patients and healthcare workers) and has conducted many interviews with various healthcare workers, but had no experience in the field of midwifery or obstetrics. The sociological study was supplemented by a double reading of some of the interviews by a woman midwife trained as a health anthropologist (CP). As an independent midwife, she has expertise in the field of midwifery and obstetrics that complements the interviewer’s expertise in the sociology of work and health. The coordinating investigator (LG), a male hospital midwife, with a PhD in public health and training in qualitative research in health care, participated with them in discussions on the interpretation of interviews, based on anonymised interview extracts.
The interviewer (FM) and the second analyst (CP) had no relationship with the participants before this study. Interviewees were informed that their interviewer was a sociological researcher employed to report their experience using the collaborative information system. Grounded theory was used to generate theory through data from independent and hospital healthcare workers14.
The interviews were conducted 9 to 12 months after the initial deployment of the PROSPERO software and approximately three months prior to the recognition of its underperformance issues. We recruited healthcare workers from the information exchange platform (MonSisra) for information sharing between healthcare workers. Participants who were independent practitioners involved in antenatal care outside hospitals (general practitioners, medical gynaecologists, gynaecologist-obstetricians, and midwives) and provided care for pregnant women included in the PROSPERO trial met the study inclusion criteria. Our non-probabilistic, purposive sampling approach called for the selection of extreme or deviant cases and maximum variation sampling15. At the same time, the selection process aimed to achieve representativeness regarding the age and diversity of status of the professionals surveyed as well as to include those with much lower or higher participation than average in this exchange platform. Appointments were made in advance. The coordinating midwife (LG) and the investigating physician (RCR) facilitated the interviews by introducing the sociologist (FM) to the healthcare workers by mail, e-mail, or in person.
We aimed to conduct up to 30 interviews, with the process guided by grounded theory principles16. Interviews, mainly conducted during healthcare workers’ working hours, were designed to be exploratory and semi-structured, based on the six dimensions outlined in Table 2. The process was adaptable, with the potential to conclude early if data saturation was achieved, as determined by the sociologist17. The data collection was stopped when the theoretical framework no longer evolved under the influence of new data, reflecting grounded theory’s non-sequential approach to data analysis where hypothesis formation, data collection, and analysis occur concurrently, rather than in a step-by-step manner. Each interview was unique to the participant, recorded with consent, and the content was carefully transcribed and analysed for accuracy and insight.
Table 2.
Analytical framework to understand healthcare workers’ perspectives in the PROSPERO study.
| Dimension | Description | Key Questions |
|---|---|---|
| Participant’s career path | Exploring the healthcare workers’ journey into their current role, emphasising the transition to independent practice | Could you tell me about your career history? |
| Relationships: parturient/community/hospital | Assessing the dynamics between the healthcare worker, their patients, and the hospital, focusing on pregnancy care | In the context of pregnancy care, what are your current links with the hospital? |
| Attitude towards ICTs | Understanding the role and significance of ICT in their professional activities | How important is the use of ICT in your work? |
| Relationship with the hospital | Gauging the nature of the healthcare workers’ relationship and interactions with hospital staff | How would you describe your relationship with the hospital? |
| Collaborative information system | Investigating the methods and practices for information exchange about parturient women among healthcare workers | How do you exchange information about a woman with your colleagues? |
| Outstanding issues | Providing an open-ended opportunity for participants to discuss additional topics or concerns not covered in the interview | Is there anything I haven’t mentioned that you’d like to discuss? |
ICT Information and Communication Technology.
Data analysis took place as the data was collected. Further comparative analyses were conducted after each round of interviews. All transcripts were reviewed manually (no software was used). The decision to forgo verbatim analysis software stemmed from the lead sociologist’s methodological approach, prioritising in-depth, interpretive analysis of interview content. This choice reflects a focus on qualitative richness and contextual in-depth understanding of participants’ perspectives, aligning with the study’s exploratory aims. More than the quantification of a theme, which has no statistical value, it is the meaning given by the actors to their experience and actions that has been considered, independently of the number of occurrences. This approach was essential in order to gain an analytical and not just a descriptive perspective. The transcript was first reviewed by the interviewer who used open-coding to identify emerging concepts related to perceptions of the collaborative information system. This text-based coding assigned a theme to each speech segment. After the initial open-coding of all interviews, i.e., the assignment of new themes to each text segment, the codes and related transcript excerpts were examined and grouped into similar themes, according to a coding tree. Thus similar minor themes were grouped into major themes, as conceptualised in the scientific literature18. The themes were not identified in advance, but were derived from the data.
A second member of the research team (CP) then used her own open-coding to independently analyse six of the transcripts, selected by the first coder for their relevance to and richness regarding the subject matter of the research. The concepts and associated definitions of these separate codes were then merged into a jointly developed coding scheme19, and areas of disagreement resolved through in-depth discussions.
Obstetricians or midwives had provided women with information about the trial during the first prenatal visits at hospital. Individual consent was obtained from all healthcare workers participating of this study. In accordance with current French legislation, this study was reported to the French commission for information technology and civil liberties (CNIL; registered number: HCL 18-165). Further, it was approved by the French ethics research committee Ouest VI under the authority of the French Directorate General for Health (approval number: CPP 1084 RNI). This study was also registered at the ClinicalTrials website under ID NCT02593292. This study was reported in accordance with the Consolidated criteria for reporting qualitative research (COREQ) guidelines.
Ethical approval
Obstetricians or midwives provided women with information about the trial during the first prenatal visits at hospital. Women confirmed participation and provided written informed consent. Individual consent was obtained from all participants of this study. In accordance with current French legislation, this study was reported to the French commission for information technology and civil liberties (CNIL; registered number: HCL 18-165). Further, it was approved by the French ethics research committee Ouest VI under the authority of the French Directorate General for Health (approval number: CPP 1084 RNI). This study was also registered at the ClinicalTrials website under ID NCT02593292.
Results
Sample characteristics
Our initial sample included 30 participants but 3 obstetricians were ineligible because they did not use the collaborative information system. We therefore analysed the interviews of 27 participants: 22 midwives (including 2 males), 3 obstetricians (2 females and 1 male), and 2 general practitioners (1 male and 1 female). Saturation was reached at this point according to FM. The duration of the interviews ranged from 35 to 75 min, with a majority lasting around 50 min. The mean age of the study population was 41.5 years.
We identified three major themes and eight subthemes related to the use/adoption of the collaborative information system through thematic analysis of the interviews (Table 3).
Table 3.
Major themes and subthemes identified through thematic analysis.
| Major themes | Subthemes | Description |
|---|---|---|
| 1. Implementation challenges | Necessity of a collaborative information system | Exploring the perceived need for the collaborative information system among healthcare workers |
| Work habit changes | The difficulties healthcare workers face in altering established work routines to accommodate the new system | |
| 2. System utilisation barriers | Time constraints | Concerns about the time required to effectively use the system within the confines of existing consultation structures |
| Training and technical issues | The lack of adequate training for healthcare workers and technical limitations of the system hindering its use | |
| 3. Interprofessional dynamics | Hospital vs. Independent practice | The differing perspectives and practices between hospital-employed and independent healthcare workers |
| Cure vs. Care | The dichotomy between the clinical, intervention-focused approach (cure) and the holistic, patient-centred approach (care) within the collaborative information system context | |
| Professional recognition | The quest for acknowledgment and respect among different healthcare professions and settings | |
| 4. Hidden influences | Hierarchical influences | The influence of hierarchical structures on system adoption, revealing how power dynamics shape professional autonomy and interprofessional relationships |
| Funding and resources | The role of financial support and resource allocation in the system’s implementation and use | |
| Confidentiality concerns | The importance of maintaining patient privacy and confidentiality in collaborative information systems |
Theme 1: implementation challenges
Necessity of collaborative information system
The introduction of a collaborative information system is perceived as a significant advancement by healthcare workers. A general practitioner reflects on the potential benefits: “If I had software that would be straightforward and where, at the end, it’s as if my patient had been seen by another midwife or another physician at the hospital, that would be amazing” (General practitioner, in his 40 s, independent).
Work habit changes
Adapting to the new system requires healthcare workers to modify their established work routines, a process which is not without challenges. One midwife candidly shares: “But when there are particular problems, it’s true you don’t have to note it; if the baby’s in intensive or special care, and why, that’s written on the health booklet, but then, you’d have to read it, you’d have to ask questions, and that’s work” (Midwife, in his 40 s, independent). This highlights the effort required to fully engage with the new system and utilise its potential effectively. Despite the challenges, healthcare workers recognize the potential of the collaborative information system to enhance communication and coordination in patient care. Another midwife notes: “Most of the time, it’s more efficient to use the phone. Afterwards, there is everyone’s email addresses. The way it’s structured, it’s quite easy when you know their names and their first names, to find their email addresses.” (Midwife, in her 50 s, independent), suggesting that while the system delivers upon its promise, existing methods of communication still play a crucial role.
Theme 2: system utilisation barriers
Time constraints
Healthcare workers expressed concerns about the time-consuming nature of integrating the new system into their workflow. One midwife highlighted the duplicative nature of tasks, stating, “The hospital midwife who sees my patient is already taking her history, and all that history, if she sent it to me, I wouldn’t have to do it again. It would save me an incredible amount of time” (Midwife, in her 50 s, independent). Another midwife elaborated on the process, “We midwives do half-hour consultations. … If everything goes well and it’s quick, in 20 min, it can be done. And afterwards, I will take the time … I have to transform [my consultation report] into PDF, and send it to My Documents, then go to … my [professional software] account, then the patient’s account, [back to] My Documents, to transmit the PDF. It takes me an incredible amount of time” (Midwife, in her 50 s, independent).
Training and technical issues
The lack of training and technical support was another significant barrier to the system’s effective use. One midwife suggested, “Maybe there should be training for professionals as well… and show us that it works, that it functions, that it’s easy, that it doesn’t take time” (Midwife, in her 50 s, mixed hospital-independent practice). Technical limitations also posed challenges, as another midwife pointed out, “We’re limited in the size of the attachments. So, depending on how we scanned them or not, not all attachments fit” (Midwife, in her 50 s, independent).
Theme 3: interprofessional dynamics
Hospital vs. Independent practice
Healthcare workers from independent practices often perceive a divide in professional respect and acknowledgment compared to their hospital-employed counterparts. One independent midwife expressed, “There are a lot of [hospital healthcare workers] who think that the real midwives are in the hospital, and that as an independent, it’s… it’s sub… [we’re] sub-midwives.” (Midwife, in her 50 s, independent). This sentiment was echoed by an obstetrician who felt marginalized by hospital processes, stating, “The hospital doesn’t need us, that’s the way we feel. But we need to know what’s going on in the hospital.” (Obstetrician, in her 60 s, mixed hospital-independent practice). The lack of communication and collaboration between these two sectors was a recurring concern, with one midwife regretting the absence of information sharing by the hospital, “Given modern means of communication [and that] she was first seen at the hospital, they could send me a letter saying, ‘you’re going to have this patient to follow up, here’s the history, here’s what we did.’ No, they don’t do that.” (Midwife, in her 50 s, independent).
Cure vs. care
A tension between the technical, medical aspects of healthcare (cure) and the supportive, preventative side (care) was also highlighted. An obstetrician commented on the collaborative information system’s limitation in transmitting medical instructions, reflecting a broader issue in the interprofessional dynamics, “Finally, it is important to note that the software was built to allow the exchange of information about women’s care and situation, but not to transmit medical instructions. Their profession [speaking about midwifery] is one of support, it’s not a profession of medical decision-making.” (Obstetrician, female, in her 60 s, mixed practice).
Professional recognition
The quest for professional recognition was a significant concern among independent healthcare workers. The feeling of being undervalued or not fully recognized by hospital counterparts was a common theme. This segment also highlights the dissatisfaction of independent healthcare workers with tasks they deem menial, such as floor cleaning or filling out collaborative information system, further contributing to their sense of underappreciation. A midwife shared how her frustration of her work at the hospital was what led her to become independent, “I didn’t study midwifery to type on a computer or mop floors. I didn’t like it any more. So, I decided to go into independent practice, where I’m devoted solely to my patients.” (Midwife, in her 50 s, independent). The desire for a more collaborative and respectful relationship between hospital and independent healthcare workers was evident, with one midwife emphasising the importance of direct communication with women, “We midwives usually have half-hour consultations. I am there for the woman, to talk with her, to respond to her.” (Midwife, in her 50 s, independent).
Theme 4: hidden influences
Hierarchical influences
The hierarchical structure within healthcare settings can greatly affect the flow of information and collaboration. For example, “I have always found it difficult, the relationship with midwife-managers, with the whole pyramidal and hierarchical system of the hospital. I wasn’t comfortable with that. And I found that as an independent practitioner, you’re really in control, you work as you want, you do what you want…” (Midwife, in her 30 s, independent). This quote highlights how hierarchical pressures can drive healthcare workers towards independent practice, seeking autonomy over their work. A tool, even collaborative, imposed by the hospital could give them the feeling of returning to hierarchical dependency.
Funding and resources
The availability of funding and resources is a critical yet often overlooked aspect that can determine the success or failure of implementing new systems. The need for adequate support is encapsulated in the frustration of a midwife: “If I had a secretary, I could ask her to do it, but I don’t have a secretary, I’m on my own. So once, twice, three times and after a while I stopped because it was too complicated.” (Midwife, in her 30 s, independent). This statement underlines the challenges healthcare workers face when expected to manage additional administrative tasks without the necessary support infrastructure or financial resources.
Confidentiality concerns
Confidentiality remains a paramount concern in the healthcare sector, especially when transitioning to a collaborative information system. The delicate balance between sharing necessary information and protecting patient privacy is articulated by a midwife: “I don’t enjoy writing on her file that the patient was raped when she was 15 years old: ‘difficulties, visits her shrink+++’. I can’t do it. I’m not gonna write that on her chart. If she sees it, she’s going to think the midwife said that something was wrong.” (Midwife, in her 20 s, independent). This quote illustrates the ethical dilemmas healthcare workers face when documenting sensitive information in a collaborative information system.
Discussion
Drawing from interviews with 27 healthcare workers, our findings emphasise the importance of system reliability and comprehensive training, aligning with DeLone and McLean’s dimensions of system and information quality. The imperative to tailor technology to the varied needs of healthcare roles, as depicted in our “Hospital vs. Independent practice” and “Cure vs. Care” themes, mirrors the “Individual-Technology Fit” concept of the FITT framework. Furthermore, information sharing was perceived as a subordinate (i.e. menial) task, highlighting the entrenched professional divisions between independent and public hospital care in France, ultimately impacting patient care.
Interpretation
Our investigation aligns with the “System Quality” and “Information Quality” dimensions of DeLone and McLean’s model, highlighting the necessity for effective and reliable collaborative information systems in obstetrics20. Challenges were revealed in our study, such as “technical limitations” and “insufficient training”; that accentuate the need for proficient systems and precise, relevant data to facilitate successful adoption of healthcare Information Technology (IT). In accordance with the “Individual-Technology Fit” of the FITT framework, our findings, particularly “Hospital vs. Independent practice” and “Cure vs. Care”, illustrate the critical importance of tailoring technology to the diverse requirements and practices of healthcare workers21. Echoing prior studies, research from the United States (US) revealed that vital clinical care details, such as social health determinants, frequently escape documentation in electronic medical records (EMRs) due to their designs not tailored to accommodate such information22. Also in the US, healthcare workers identified the complexity and time-consuming aspect of consulting EMRs as major obstacles in a 2015 study23. Community clinics in New York faced challenges related to time, staffing, and funding, which subsequently restricted administrative support for EMR usage and access to training24.
Our study also introduces innovative themes such as “Interprofessional dynamics” and “Hidden influences” like “Professional recognition” and “Hierarchical influences” extend beyond traditional IT adoption frameworks, suggesting the complexity of sociotechnical interactions in healthcare settings, which may not be fully captured by existing models like those of DeLone and McLean or the FITT framework20,21.
The sociological insights of Florent Champy resonate profoundly in our study, particularly his concept of “prudential practice” within health professions. Champy articulates that these practices necessitate practical judgment (phronesis) in the face of complex and uncertain situations, tailored to individual users25. This perspective is mirrored in our findings, especially within themes such as “Cure vs. Care” and “Confidentiality concerns”. Our data suggest that our collaborative information system, though intended to enhance care, may inadvertently hinder the exercise of phronesis. Factors such as bureaucratisation, division of labour, an emphasis on performance and objectivity, and the erosion of professional autonomy appear to complicate the practical judgment essential in healthcare.
Moreover, the lukewarm reception of our collaborative information systems among healthcare workers may be partially attributed to the traditional notion of “professionalism”. This concept posits that professional groups strive to develop and maintain exclusivity within their domain to safeguard their interests, such as salary, status, power, and the monopolistic protection of their professional jurisdiction26. The rise of independent midwifery in France, where the involvement of midwives in pregnancy follow-ups increased from 8.5% in 2016 to 22.9% in 2021, primarily at the expense of private practice gynaecologists whose share decreased from 49.7% to 39.4%, highlights increasing interprofessional tensions7. This shift raises significant questions related to our sub-themes of “Professional recognition”, and “Funding and resources”. These barriers to collaborative practice are not unique to obstetrics; a study involving 229 healthcare workers across various specialties in Lahore identified role ambiguity, divergent individual team member goals, and differences in authority levels, expertise, and income as the main obstacles to effective interprofessional collaboration27.
Finally, these tensions between independent and hospital-based healthcare workers over information transmission reflect different values attributed to healthcare work. They also reveal a vision of this work of information provision as menial28,29. As Hughes argued, work is composed of a more or less noble set of tasks to be accomplished. The core of this bundle of tasks is the prestigiousness or honourability of the work, while the subordinate or peripheral—the menial—tasks can be delegated to others30. In our study, some midwives considered listening to women as the noble part of their work, while doctors put more emphasis on decision-making. But both professions and both segments of each (independent ambulatory and hospital sectors) appeared to treat the use of information transmission collaborative information system as a menial task. This most likely explains why its implementation failed.
Strength and limitations
The main strength of this study is the ethnographic approach’s ability to uncover deep insights into the users’ perceptions and experiences with PROSPERO, providing a rich understanding of the complex interplay of social, organisational, and technological factors affecting the platform’s adoption. A sociologist previously uninvolved in this topic and without prior knowledge—and therefore preconceptions—about care providers specialised in the perinatal period conducted and analysed the interviews. He considered that data saturation was reached, and the final sample size was aligned with sample sizes recommended for qualitative methods16,32. Then, an additional analysis was entrusted to an independent midwife not part of the system under study. The diversity of the researchers (including a male sociologist, a female independent midwife, and both male and female obstetricians and hospital midwives, with various levels of education) enabled triangulation and reduced the risk of potential for bias.
While the study’s insights are valuable, it’s important to acknowledge limitations. The reliance on the lead sociologist’s judgment for data saturation and the absence of verbatim analysis software could introduce subjectivity, potentially impacting the analysis’ comprehensiveness. Additionally, the skewed distribution of participants, with a predominance of midwives over doctors, may limit the generalisability of findings across the broader healthcare worker spectrum. It provides only an overview during an ephemeral phase of a failed implementation. Moreover, although independent obstetricians provide antenatal and postnatal care for many pregnancies, they accounted for only a small part of our sample because only half of those who agreed to meet us were using the collaborative information system.
Implications
The findings from our study underscore a critical need for a re-evaluation of the design and implementation strategies of collaborative information systems in obstetric care. To address the technical and training challenges identified, there is an imperative for developers and healthcare administrators to foster systems that are not only technically reliable but also intuitive and accommodating to the diverse needs of healthcare workers. This may include enhancing system features such as single sign-on capabilities, streamlined data entry through voice-to-text functionalities, and advanced data analytics to provide actionable insights for healthcare providers. This entails a shift towards more user-centric designs that prioritise ease of use and relevance of information, potentially through iterative co-design processes with healthcare workers. The sociotechnical complexity uncovered in our themes, such as “Interprofessional dynamics” and “Hidden influences”, requires embedding sociological insights into IT adoption strategies. For instance, including tools for automatic data synchronization between community and hospital care software to reduce redundancy and ease the workflow for healthcare providers. This could imply the development of policies and practices that recognise and mitigate the effects of professional hierarchies and segmentation, fostering a culture of mutual respect and understanding across different healthcare roles.
Moreover, the concept of “professionalism” and the protective stance of professional groups towards their domain should be carefully navigated. Engaging healthcare workers in meaningful dialogues about the benefits of collaborative systems, beyond mere information-sharing, could help in aligning the system functionalities with their professional values and practices. Emphasizing the role of the system in supporting clinical decision-making and patient management might also diminish resistance to technology adoption. This approach could mitigate the perception of information transmission as a “menial task” and reframe it as an integral part of quality patient care.
Furthermore, the incorporation of “prudential practice” into the system design, by allowing for the documentation and recognition of nuanced patient care practices, could enhance the system’s utility and acceptance. Enhanced customizability and the integration of decision support tools could further validate the clinician's expertise in the caregiving process. Finally, addressing the barriers to collaborative practice identified, such as role ambiguity and divergent goals, through targeted interprofessional education and collaborative workshops, could improve the adoption and effective use of collaborative information systems in obstetric care. The establishment of a dedicated support and liaison team might also provide ongoing assistance and promote a seamless integration of the system into daily clinical routines.
Importantly, integrating artificial intelligence (AI) and natural language processing (NLP) for voice analysis could play a transformative role, particularly in the detection of depression—a leading cause of maternal mortality in high-income countries. By analysing voice intonation patterns, AI can assist in identifying early signs of depression, thereby facilitating timely intervention and support33.
Conclusion
Our study provides valuable insights into the challenges and dynamics of implementing a collaborative information system in obstetric care, highlighting the need for systems that not only cater to the technical aspects of healthcare delivery but also respect and integrate the diverse professional practices and values within the field. The findings underscore the importance of designing user-centric systems that facilitate seamless communication and collaboration among healthcare workers, thereby enhancing the quality of antenatal care.
Acknowledgements
We thank the French Ministry of Solidarity and Health for funding data acquisition and analysis through its research program on the performance of the healthcare system (PREPS). We thank Pr René-Charles RUDIGOZ, Pr Pascal GAUCHERAND, Pr Gil DUBERNARD, Pr Muriel DORET-DION for approving the study in their maternity ward. We thank Pr Cyrille COLIN, and Dr Sandrine TOUZET, Dr Muriel RABILLOUD, who served with Corinne DUPONT and Laurent GAUCHER on the study steering committee. We thank Pr Anne-Marie SCHOTT-PETHELAZ, Pr Olivier CLARIS, Pr François GOFFINET, Pr Marie FLORI, Dr Laurent LETRILLARD, Pr Jean-Pierre DUBOIS, Pr Jacques GAUCHER, Dr Marie-Pierre FERNANDEZ for serving as the scientific committee of the study. We thank Daniel BETITO, Cécile BOURGEAT, Philippe CASTETS, Marthe CHAVERONDIER, Aurélie CHIKH, Marie COMBE, Patricia CURTET, Dr Jean DERRIEN†, Catherine DE WECK, Cécile DOLLA, Nicole DUPIN, Anne EVRARD, Marlène FRASCHINI, Mathieu GROBERT, Maëlle GUITTON, Pr Cyril HUISSOUD, Marie-Pierre LASSARA, Nathalie LAURENCEAU, Marc LOPVET, Dr Serge MARVALIN, Karine MICHEL, Isabelle MORTIER, Marie-Françoise OYSELET, Noëlle PRAL, Christine PREVOT, Marie-Pierre ROYER, and Laurence TOURATIER for their participation in the working group that led to the creation of the software and collaborative information system. We thank the doctoral students of the ORGASM research group (Organe de Réflexion sur les questions de Grossesse, Accouchement, santé sexuelle, Sexualité, et Maternité), a think tank offering crossed perspectives of sociologists, anthropologists, political scientists and historians on pregnancy, childbirth, sexual health and motherhood, for their help in analysing the results. We thank Jo Ann CAHN for her careful editing of our English. We thank Prof. Patricia PERRENOUD for her review and valuable socio-cultural insights on the article.
Author contributions
L.G. participated in the study design and drafted the article. C.P. participated in the data analysis, and drafted parts of the article. S.B. helped revise the article. S.T., S.H., R.C.R., M.C., C.H., P.G., and C.D. participated in the study design and helped to revise the article. F.M. participated in the study design, acquired and analysed the data, and revised the article.
Funding
The French Ministry of Solidarity and Health through its research program on the performance of the health care system (PREPS) supported this work.
Data availability
The data that support the findings of this study are available from Frédéric Mougeot (frederic.mougeot@gmail.com) upon reasonable request.
Competing interests
All authors have completed the ICMJE uniform disclosure form. The authors certify that they have NO affiliations with or involvement in any organisation or entity with any financial or non-financial interests in the subject matter of this article.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bucher R, Strauss A. Professions in process. Am. J. Sociol. 1961;66:325–334. doi: 10.1086/222898. [DOI] [Google Scholar]
- 2.Topçu S. Caesarean or vaginarean epidemics ? Techno-birth, risk and obstetric practice in Turkey. Health Risk Soc. 2019;21:141–163. doi: 10.1080/13698575.2019.1641588. [DOI] [Google Scholar]
- 3.Cavalli, S. & Gouilhers-Hertig, S. Gynécologues-obstétriciens et sages-femmes dans le suivi de la grossesse : une complémentarité sous contrôle médical ?: in Accompagner la naissance 85–106 (BSN Press, 2014). 10.3917/bsn.burt.2014.01.0085
- 4.Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016;4:CD004667. doi: 10.1002/14651858.cd004667.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fertility Statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Fertility_statistics
- 6.Bellamy, V. Les 784 000 Naissances de 2016 Ont Eu Lieu Dans 2 800 Communes. https://www.insee.fr/fr/statistiques/3047024#titre-bloc-10 (2017).
- 7.Blondel, B., Gonzalez, L. & Raynaud, P. Enquête Nationale Périnatale 2016. Les Naissances et Les Établissements, Situation et Évolution Depuis 2010 - Rapports - Ministère Des Solidarités et de La Santé. https://drees.solidarites-sante.gouv.fr/sites/default/files/2021-01/rapport_Perinat_2016.pdf (2016).
- 8.Steffen M. The French health care system: Liberal universalism. J. Health Polit. Policy Law. 2010;35:353–387. doi: 10.1215/03616878-2010-003. [DOI] [PubMed] [Google Scholar]
- 9.Petersen LS, Bertelsen P, Bjørnes C. Cooperation and communication challenges in small-scale eHealth development projects. Int. J. Med. Inf. 2013;82:e375–e385. doi: 10.1016/j.ijmedinf.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Elias B, Barginere M, Berry PA, Selleck CS. Implementation of an electronic health records system within an interprofessional model of care. J. Interprof. Care. 2015;29:551–554. doi: 10.3109/13561820.2015.1021001. [DOI] [PubMed] [Google Scholar]
- 11.Blatgé M. Béatrice Jacques, Sociologie de l’accouchement. Lectures. 2007 doi: 10.4000/lectures.403. [DOI] [Google Scholar]
- 12.Price M, Lau F. The clinical adoption meta-model: A temporal meta-model describing the clinical adoption of health information systems. BMC Med. Inform. Decis. Mak. 2014;14:43. doi: 10.1186/1472-6947-14-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jahn F, et al. A linked open data-based terminology to describe libre/free and open-source software: Incremental development study. JMIR Med. Inform. 2023;11:e38861. doi: 10.2196/38861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glaser, B. G. & Strauss, A. L. The discovery of grounded theory: Strategies for qualitative research. (Aldine, 1967). 10.4324/9780203793206
- 15.Patton, M. Q. Qualitative evaluation and research methods, 2nd Ed. 532 (Sage Publications, Inc, 1990). https://aulasvirtuales.files.wordpress.com/2014/02/qualitative-research-evaluation-methods-by-michael-patton.pdf.
- 16.Creswell, J. W. Qualitative inquiry and research design: Choosing among Five traditions. xv, 403 (Sage Publications, Inc, 1998). https://revistapsicologia.org/public/formato/cuali2.pdf.
- 17.Morse JM. The significance of saturation. Sage Publications; 1995. [Google Scholar]
- 18.Bowen GA. Supporting a grounded theory with an audit trail: An illustration. Int. J. Soc. Res. Methodol. 2009;12:305–316. doi: 10.1080/13645570802156196. [DOI] [Google Scholar]
- 19.Ulin PR, Robinson ET, Tolley EE. Qualitative methods in public health: A field guide for applied research. Med. Sci. Sports Exerc. 2005;37:1249. doi: 10.1249/01.mss.0000172593.20181.14. [DOI] [Google Scholar]
- 20.Delone WH, McLean ER. The DeLone and McLean model of information systems success: A ten-year update. J. Manag. Inf. Syst. 2003;19:9–30. doi: 10.1080/07421222.2003.11045748. [DOI] [Google Scholar]
- 21.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: A fit framework and a case study. BMC Med. Inform. Decis. Mak. 2006;6:3. doi: 10.1186/1472-6947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ingram M, et al. Community health worker impact on chronic disease outcomes within primary care examined using electronic health records. Am. J. Public Health. 2017;107:1668–1674. doi: 10.2105/ajph.2017.303934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reinschmidt KM, et al. Documenting community health worker roles in primary care: Contributions to evidence-based integration into health care teams, 2015. J. Ambulatory Care Manag. 2017;40:305–315. doi: 10.1097/jac.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 24.Divney AA, et al. Research-grade data in the real world: Challenges and opportunities in data quality from a pragmatic trial in community-based practices. J. Am. Med. Inform. Assoc. JAMIA. 2019;26:847–854. doi: 10.1093/jamia/ocz062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Champy F. The sociology of prudential activities: From collective commitment to social innovations. Sociol. Probl. E Práticas. 2018;88:79–94. [Google Scholar]
- 26.Evetts, J. The concept of professionalism: Professional work, professional practice and learning. In International handbook of research in professional and practice-based learning (eds. Billett, S., Harteis, C. & Gruber, H.) 29–56 (Springer Netherlands, 2014). 10.1007/978-94-017-8902-8_2
- 27.Jabbar S, et al. A cross-sectional study on attitude and barriers to interprofessional collaboration in hospitals among health care professionals. Inq. J. Health Care Organ. Provis. Financ. 2023;60:004695802311710. doi: 10.1177/00469580231171014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hughes EC. The humble and the proud: The comparative study of occupations*. Sociol. Q. 1970;11:147–156. doi: 10.1111/j.1533-8525.1970.tb01440.x. [DOI] [Google Scholar]
- 29.Hughes EC. Good people and dirty work. Soc. Probl. 1962;10:3–11. doi: 10.2307/799402. [DOI] [Google Scholar]
- 30.Lhuilier D. Le <<sale boulot>>. Travailler. 2005;2:73–98. doi: 10.3917/trav.014.0073. [DOI] [Google Scholar]
- 31.Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2016 doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 32.Morse JM. Determining sample size. Qual. Health Res. 2000 doi: 10.1177/104973200129118183. [DOI] [PubMed] [Google Scholar]
- 33.Cummins N, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10–49. doi: 10.1016/j.specom.2015.03.004. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from Frédéric Mougeot (frederic.mougeot@gmail.com) upon reasonable request.