Abstract
Objective
Stress urinary incontinence (SUI) is common among females during functional fitness training, such as CrossFit. The aim of this study was to assess the effect of pelvic floor muscle training (PFMT) on SUI in female functional fitness exercisers.
Methods
This was an assessor-blinded randomised controlled trial with a PFMT group (n=22) and a control group (n=25). The PFMT group followed a 16-week home-training programme with 3 sets of 8–12 maximum pelvic floor muscle (PFM) contractions daily and weekly follow-up/reminders by phone. The primary outcome was change in a total score of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI-SF). The secondary outcomes were perceived change of symptoms of SUI, change of PFM strength measured by vaginal manometry and symptoms of anal incontinence (AI) and pelvic organ prolapse (POP).
Results
47 women, mean age of 33.5 years (SD: 8.1), participated. At 16 weeks, there was a mean difference between groups of −1.4 (95% CI: −2.6 to −0.2) in the change of the ICIQ-UI-SF score in favour of the PFMT group. The PFMT group completed a mean of 70% (SD: 23) of the prescribed protocol. 64% in the PFMT group versus 8% in the control group reported improved symptoms of SUI (p<0.001, relative risk: 7.96, 95% CI, 2.03 to 31.19). There were no group differences in the change of PFM strength or AI/POP symptoms.
Conclusion
A 16-week home-training programme of the PFM led to improvements in SUI in female functional fitness exercisers. However, PFM strength and AI and POP symptoms did not improve significantly in the PFMT group compared with the control group.
Keywords: Female, Pelvic floor, Women in sport, Exercise Therapy
WHAT IS ALREADY KNOWN ON THIS TOPIC
Current evidence supports pelvic floor muscle training (PFMT) to improve or cure urinary incontinence in the general female population. Stress urinary incontinence (SUI) (involuntary leakage of urine on physical effort) is highly prevalent among female functional fitness exercisers. There is limited knowledge of the effect of PFMT in these women who are exposed to potential strain on the pelvic floor muscles due to large increases in intra-abdominal pressure during exercise (eg, running, jumping and heavy lifting).
WHAT THIS STUDY ADDS
This study demonstrates that targeted PFMT may improve the frequency, amount and symptoms of SUI in functional fitness exercisers. A pragmatic home-based training approach was chosen, although the sample showed large variability of the effects on symptoms of SUI and pelvic floor muscle strength.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
PFMT should be offered as a first-line treatment for SUI in female functional fitness exercisers. Increased knowledge of treatment options for SUI may encourage women to stay active and continue their functional fitness training.
Introduction
The pelvic floor consists of muscles, fascia and ligaments and forms a hammock-like support for the pelvic organs at the base of the abdominopelvic cavity.1 During exercise, the pelvic floor muscles (PFMs) must counteract the increase in intra-abdominal pressure (IAP), especially during weightlifting and high-impact activities (eg, running and jumping).1 2 Indirect loading of the pelvic floor may potentially lead to stronger PFM and better pelvic floor support. However, if not able to withstand the increases in IAP, the PFM may be overloaded and weakened. This can further increase the risk of pelvic floor disorders (PFD), such as urinary incontinence (UI).2 3 CrossFit/functional fitness training includes various high-intensity weightlifting and high-impact activities (eg, rope jumping and box jumps),4 of which are shown to generate large increases in IAP.5 Given the potential impact on the pelvic floor, it is presumed that female functional fitness exercisers need well-functioning PFM to prevent PFD. A recent meta-analysis revealed a pooled prevalence of UI of 45% among CrossFit practitioners with 50% increased odds of UI compared with control groups.6 The most common type was stress UI (SUI), which is the complaint of involuntary leakage of urine on physical effort.7
There are level 1 evidence and grade A recommendation for PFM training (PFMT) as the first-line treatment for SUI in the general female population.8 Regular PFMT has been shown to change pelvic floor morphology by increased muscle volume and stiffness, reduced opening of the levator hiatus (the surrounding area where the urethra, vagina and rectum pass through) and elevated resting position of the bladder and rectum.9 Despite a high prevalence of SUI in female strenuous exercisers, the knowledge of treatment options is sparse.10 11 Therefore, the aim of this study was to assess the effects of PFMT on SUI in female functional fitness exercisers.
Methods
Design
We have followed the Consolidated Standards of Reporting Trials checklist.12 The study protocol was registered in the ClinicalTrials.gov-registry by the US National Library of Health (22 April 2022, NCT05341024, https://clinicaltrials.gov/study/NCT05341024).
Participants
Participants were recruited through social media (Facebook and Instagram) and CrossFit or functional fitness affiliates between April and December 2022. Women aged ≥18 years who habitually participated in CrossFit or functional fitness training (≥6 months of consistent participation, ≥3 times per week) with self-reported SUI were invited to participate in the study. Eligibility was verified by the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI-SF), prior to baseline evaluations. A sum score of ≥3 of the questions regarding frequency and amount of leakage was required. Further, the option ‘I leak when I am physically active/exercising’ on the question ‘When does urine leak?’ had to be chosen. The exclusion criteria were pregnancy/planning to get pregnant during the intervention period, history of hysterectomy/pelvic surgery to correct UI, anal incontinence (AI) or pelvic organ prolapse (POP), musculoskeletal injuries for the past 6 months with a negative effect on exercise, childbirth within the previous 12 months and inability to perform a correct PFM contraction.
Intervention
The intervention consisted of a home-based PFMT programme with weekly follow-up by phone with a physiotherapist (alternating follow-up phone call or SMS) who had received thorough teaching of the PFMT programme from the founder of the original evidence-based programme (KB). The PFMT programme was based on the protocols from previous studies of strength training of the PFM with proven effectiveness in improving symptoms of SUI and POP.13–16 Prior to the intervention, the participants were taught how to perform a correct PFM contraction by vaginal palpation and received instruction on how to perform the training programme. The programme consisted of 3 sets of 8–12 maximum PFM contractions of approximately 6–8 s holding time per day in lying, kneeling, sitting or standing positions with the legs apart to facilitate maximum or close to maximum contractions with simultaneous relaxation of other muscles.14 The participants were encouraged to contract as close to maximum as possible (this is relative as strength increases). They were encouraged to begin their PFMT in a position where they felt they could manage to perform strong PFM contractions, for example, lying or sitting. When they felt able to perform ≥12 strong contractions, they were encouraged to change position, for example, standing, and to add 3–4 fast contractions on top of each holding period.14 During the fortnightly calls, training progression was discussed individually for each participant. They also received an information booklet (with information on the pelvic floor and a description of the PFMT, including options for training position and progression alternatives) and a video showing the exercise programme with the performance of 3 sets of 8–12 contractions in different positions. The participants could choose to follow the video instructions if needed for motivation and coaching during their sessions. To assess adherence to the prescribed exercises, the participants were asked to register their sessions in an electronic app (AthleteMonitoring). A reminder was sent by SMS if registration for the daily session was lacking by 8PM. The training period lasted 16 weeks, and the programme took about 10 min per day.
The participants in the control group were informed to continue their functional fitness training as usual and asked not to perform any specific training of the PFMs during the intervention period. The control group did not receive any education on PFMT, lifestyle modifications or other pelvic floor treatment options during the intervention period. All participants in the control group received instructions for PFMT by email (including the booklet and the instruction video) after the completion of post-tests with the opportunity to contact one of the physiotherapists involved in the study if they had any questions related to the PFMT. Information regarding the protocol for the control group was included in the informed consent form.
Outcomes
Primary outcome
The primary outcome was the change in total score of the ICIQ-UI-SF. The ICIQ-UI-SF is a reliable and valid questionnaire assessing the frequency, amount, bother of urinary leakage and type of UI.17 The ICIQ-UI-SF score (0–21) is the sum of the first three questions (frequency, amount and bother). A change of the ICIQ-UI-SF score of 2.5 has been identified to be the minimal important difference (MID) and 1.58 as between-treatment MID.18
Secondary outcomes
Patient global impression of improvement scale
At post-test, the participants were asked to rate their perceived change of SUI. A validated 7-point scale with response choices ranging from ‘very much better’ to ‘very much worse’ was used.19
Manometry measurements of the PFM
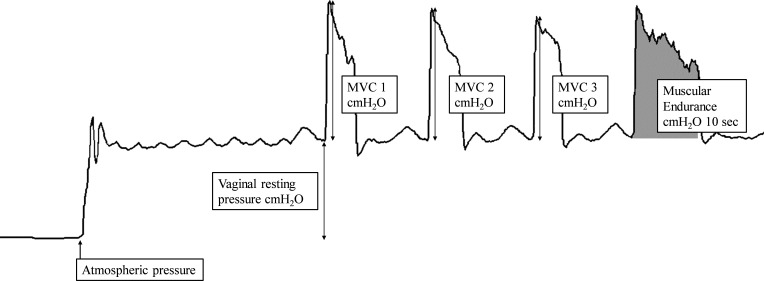
Vaginal resting pressure, PFM strength (maximum voluntary contraction) and PFM endurance were measured with a high-precision pressure transducer connected to a vaginal balloon catheter (Camtech AS, Sandvika, Norway). The method has demonstrated good intraobserver reliability.20–24 PFM resting pressure was measured as the difference between the atmospheric pressure and the vaginal high-pressure zone at rest in cmH2O (figure 1). PFM strength was calculated as the mean peak from the resting pressure line of three maximum voluntary contraction curves (cmH2O), while PFM endurance was quantified as the area under the curve for 10 s (cmH2O/sec) (figure 1). Only measurements with simultaneous observable inward movement of the catheter/perineum were considered as valid measurements of correct PFM contractions.21
Figure 1.
Example of pressure curves of vaginal resting pressure, pelvic floor muscle strength (MVC 1–3) and muscular endurance. MVC, maximum voluntary contraction.
Other PFD
Questions from patient-reported outcome measures with grade A recommendation from the International Consensus on Incontinence 2017 were used to assess the prevalence and bother of AI (ICIQ-B) and symptomatic POP (ICIQ-VS).25 AI was classified into three subgroups as follows: involuntary loss of gas, solid stool and liquid stool.
Self-Efficacy Scale for Practising Pelvic Floor Exercises
At baseline, the participants were asked to rate their self-efficacy of pelvic floor exercises by using a reliable and valid self-efficacy scale,26 including 17 items. This was repeated after 1 month of PFMT.
Data collection and procedures
The data were collected between May 2022 and April 2023. Eligible participants were invited to participate in two test sessions (at baseline and postintervention (16 weeks)) at the Norwegian School of Sport Sciences. The testing was performed in a private test laboratory. Ten participants were tested at 2 different physiotherapy clinics outside of Oslo (Trondheim Fysikalske Institutt, Trondheim, Norway, and Klinikk for Alle, Drammen, Norway). Informed consent, background variables (age; parity; mode of delivery; training habits; chronic diseases such as diabetes type 1 or 2, Crohn’s disease or irritable bowel syndrome; and prior PFMT), the ICIQ-UI-SF, report of AI, POP and Self-Efficacy Scale for Practicing Pelvic Floor Exercises (SESPPFE) were collected in an electronic questionnaire (Survey Xact) 1–2 days prior to the baseline evaluation. Baseline testing included measurements of height, weight and PFM manometry. All participants were reassessed with a questionnaire (ICIQ-UI-SF, Patient Global Impression of Improvement (PGI-I) scale and reports of AI and POP) and PFM manometry after the intervention period.
Randomisation and blinding
A randomisation list was computer generated by an independent biostatistician. Block randomisation was used with different block sizes in random order. Allocation was concealed in sequentially numbered sealed and opaque envelopes. The assessor and statistician were blinded to group allocation. Randomisation was revealed to the participants and physiotherapist in charge of the intervention after baseline testing. The assessor (KLS) enrolled the participants in the study, and the physiotherapists in charge of the intervention randomised the participants.
Statistics
An a priori power calculation was conducted based on the mean ICIQ-UI-SF score (4.3, SD: 2.8) from a previous study in female strength athletes27 and the MID in total score of 2.5.18 With a decrease in ICIQ-UI-SF score from 4.3 to 1.8 (SD: 2.8) in the PFMT group and no change (SD: 2.8) in the control group, 80% of power, 5% of significance level and an estimated dropout rate of 20%, at least 24 participants were required in each group (total n=48). To account for uncertainties in the power calculations, we aimed to include 50 participants.
Data were analysed in SPSS 28. Background variables were reported as means with SD or numbers with percentages. For analyses of dichotomous variables, the Pearson χ2 test was used. The expected cell counts were calculated and found to be above five in all cases. Between-group differences of ordinal data were analysed by Mann-Whitney U test and continuous variables by analyse of covariance as a linear regression with week 16 value as the dependent variable and group allocation and the baseline variable as independent variables. Normality, homogeneity of variance of residuals and linearity for quantitative predictors were assessed by histograms, normal probability plots and scatter plots of the standardised residuals.
The difference in change between groups from baseline to week 16 was reported with 95% CIs. We applied a two-sided alpha level of 5% to determine statistical significance. The analyses were based on a full analysis set where all available participants at follow-up were analysed in the groups to which they were originally randomised. Additional sensitivity analyses were conducted with imputations of missing data due to the loss to follow-up. Post-ICIQ-UI-SF scores for the four participants who dropped out in the PFMT group were imputed (improvement, no change and worsening), based on the lower-limit CI for score reduction in the PFMT group (−2.6) and the upper-limit CI of score increase in the control group (0.9) from the main analysis.
Equity, diversity and inclusion statement
The study included only female participants and authors. Several publications have pointed out that women are strikingly under-represented both as authors and participants in sports medicine and exercise research.28–30 Also, PFD has been shown to affect female athletes/exercisers on a much larger scale than males.27 31 Women with different ethnic and socioeconomic backgrounds were welcome to participate.
Results
Flow of participants
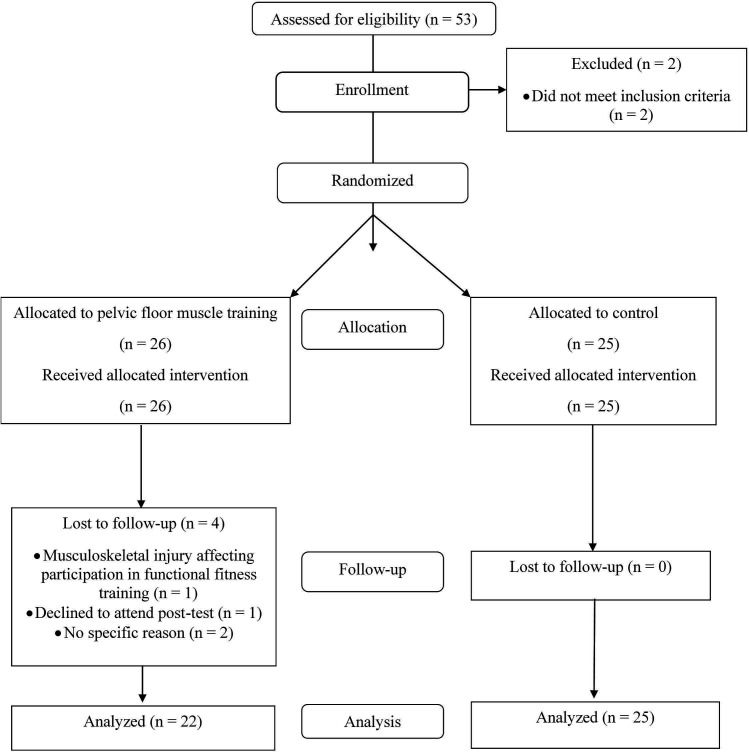
Fifty-three women were recruited to baseline assessments. Two were excluded due to the inability to perform a correct PFM contraction. Of the remaining 51 participants, 26 participants were randomised to the PFMT group and 25 to the control group. Four participants dropped out of the PFMT group and none in the control group. Reasons for dropout are described in figure 2. PFM measurement data at week 16 were missing for one participant in the control group due to equipment impairments. There were no observed differences in background variables between groups at baseline (table 1). At baseline, none reported regular PFMT within the previous 3 months. All parous women had given birth vaginally, while two in the control group had also delivered by caesarian section.
Figure 2.
Flowchart of participants through each stage of the randomised controlled trial.
Table 1.
Participant characteristics of the training group and control group at baseline. Mean with SD or number with percentages
| Total sample (n=47) | PFMT group (n=22) | Control group (n=25) | |
| Age (y), mean (SD) | 33.5 (8.1) | 34.7 (8.3) | 32.5 (7.8) |
| Height (cm), mean (SD) | 167.9 (5.4) | 167.7 (5.9) | 168.1 (5.0) |
| Weight (kg), mean (SD) | 71.6 (10.1) | 71.1 (8.6) | 72.0 (11.4) |
| Body mass index (kg/m2), mean (SD) | 25.4 (3.2) | 25.3 (2.8) | 25.4 (3.6) |
| Years of CF/FFT participation, mean (SD) | 3.8 (2.2) | 4.0 (2.5) | 3.6 (2.0) |
| Hours of CF/FFT per week, mean (SD) | 5.6 (3.3) | 5.4 (2.9) | 5.8 (3.6) |
| College/university degree, n yes (%) | 40 (85) | 18 (82) | 22 (88) |
| Numbers of parous women, n yes (%) | 23 (49) | 13 (59) | 10 (40) |
| Parity, mean (SD) | 1.9 (0.7) | 1.9 (0.7) | 2.0 (0.7) |
| Years since last childbirth, mean (SD) | 7.4 (5.1) | 7.7 (4.4) | 7.0 (6.0) |
| Chronic disease, n yes (%) | 13 (28) | 6 (27) | 7 (28) |
| ICIQ-UI-SF score | 7.5 (3.2) | 7.5 (3.3) | 7.5 (3.1) |
| Severity categories, n (%) | |||
| Mild (score 1–5) | 23 (49) | 11 (50) | 12 (48) |
| Moderate (score 6–12) | 21 (45) | 9 (41) | 12 (48) |
| Severe (score 13–18) | 3 (6) | 2 (9) | 1 (4) |
| Very severe (19–21) | 0 (0) | 0 (0) | 0 (0) |
| Other pelvic floor disorders, n yes (%) | |||
| Involuntary leakage of gas | 31 (66) | 14 (64) | 17 (68) |
| Involuntary leakage of solid stool | 2 (4) | 1 (5) | 1 (4) |
| Involuntary leakage of liquid stool | 16 (34) | 8 (36) | 8 (32) |
| Symptoms of pelvic organ prolapse | 9 (19) | 5 (23) | 4 (16) |
| Score of SESPPFE (scale 0–100), mean (SD) | 78.9 (15.2) | 81.2 (15.0) | 76.9 (15.4) |
CF, CrossFit; FFT, functional fitness training; ICIQ-UI-SF, International Consultation of Incontinence Questionnaire-Urinary Incontinence Short Form; PFMT, pelvic floor muscle training; SESPPFE, Self-Efficacy Scale for Practicing Pelvic Floor Exercises.
The participants in the PFMT group completed in mean 70% (SD: 23) of the prescribed exercise sessions. Thirteen (59%) adhered to >70%. No adverse effects were reported.
ICIQ-UI-SF
At 16 weeks, we found a mean change in the ICIQ-UI-SF score of −1.3 (95% CI: −2.6 to −0.03) in the PFMT group and 0.1 (95% CI: −0.6 to 0.9) in the control group. There was a mean difference between groups of −1.4 (95% CI: −2.6 to −0.2) in the change of the ICIQ-UI-SF score in favour of the PFMT group.
Sensitivity analysis
Results from the sensitivity analysis of between-group comparisons of change in the ICIQ-UI-SF score are described in table 2.
Table 2.
Sensitivity analysis of the between-group mean differences (95% CI) of change in ICIQ-UI-SF score with imputations of post-ICIQ-UI-SF (reduction, no change or increase) for the missing data for the four participants who were lost to follow-up at week 16. PFMT group (n=26) versus control group (n=25)
| Between-group differences | |||
| Mean difference (week 16 minus week 0, PFMT minus control) | 95% CI | P value | |
| ICIQ-UI-SF score (−2) | −1.6 | −2.7 to −0.5 | 0.005 |
| ICIQ-UI-SF score (−3) | −1.8 | −2.3 to −0.6 | 0.003 |
| ICIQ-UI-SF score (no change) | −1.3 | −2.4 to −0.2 | 0.020 |
| ICIQ-UI-SF score (+1) | −1.2 | −2.3 to −0.1 | 0.042 |
ICIQ-UI-SF, International Consultation of Incontinence Questionnaire-Urinary Incontinence Short Fort; PFMT, pelvic floor muscle training.
PFM resting pressure, strength and endurance
Changes in PFM variables are described in table 3. We found no between-group differences in change of PFM resting pressure, strength or endurance between groups.
Table 3.
Mean of groups (SD), mean (SD) within-group difference and mean (95% CI) between-group difference for manometry measures of the pelvic floor muscles
| Outcome | Groups | Within-group differences | Between-group difference | ||||
| Week 0 | Week 16 | Week 16 minus week 0 | Week 16 minus week 0 | ||||
| PFMT (n=22) |
Control (n=25) |
PFMT (n=22) |
Control (n=24)* |
PFMT (n=22) |
Control (n=24)* |
PFMT minus control | |
| PFM resting pressure, cmH2O | 30.5 (7.1) | 32.3 (7.9) | 28.5 (5.7) | 28.0 (5.3) | −2.1 (6.6) | −4.4 (5.6) | 1.3 (−1.4 to 4.0) |
| PFM strength, cmH2O | 17.4 (10.9) | 22.2 (14.4) | 21.3 (10.5) | 20.9 (14.0) | 3.9 (7.9) | −1.0 (8.3) | 3.8 (−0.8 to 8.4) |
| PFM endurance, cmH2O/sec | 122.1 (86.9) | 143.2 (110.8) | 147.5 (84.1) | 119.9 (94.2) | 28.0 (82.4) | −19.8 (77.2) | 39.28 (−1.5 to 80.1) |
*Missing data of one participant due to measurement error.
PFMT, pelvic floor muscle training.
Patient Global Impression of Improvement (PGI-I) scale
64% in the PFMT group versus 8% in the control group reported improved symptoms of the SUI group (p<0.001, RR: 7.96, 95% CI 2.03 to 31.19) on the PGI-I scale. None in the PFMT group and one participant in the control group reported worsening of symptoms (table 4).
Table 4.
Self-perceived improvements in stress urinary incontinence reported by PGI-I and change in frequency of bowel symptoms and pelvic organ prolapse, numbers with percentages
| PFMT group (n=22) | Control group (n=25) | Group differences p value | |
| PGI-I: how is your urinary leakage now compared with before you entered the study? n (%) | |||
| Very much better | 0 (0) | 1 (4) | <0.001* |
| Much better | 3 (14) | 0 | |
| Better | 11 (50) | 1 (4) | |
| No change | 8 (36) | 22 (88) | |
| Worse | 0 (0) | 1 (4) | |
| Much worse | 0 (0) | 0 | |
| Very much worse | 0 (0) | 0 | |
| Improvement PGI-I score ≥1 | 15 (64) | 2 (8) | <0.001† |
| Bowel symptoms, n (%) | |||
| Involuntary leakage of gas: | |||
| Reduced frequency | 5 (23) | 6 (24) | 0.890* |
| No change | 11 (50) | 13 (52) | |
| Increased frequency | 6 (27) | 6 (24) | |
| Involuntary leakage of solid stool: | |||
| Reduced frequency | 1 (5) | 1 (4) | 0.642* |
| No change | 18 (82) | 22 (88) | |
| Increased frequency | 3 (14) | 2 (8) | |
| Involuntary leakage of liquid stool: | |||
| Reduced frequency | 3 (14) | 3 (12) | 0.568* |
| No change | 17 (77) | 22 (88) | |
| Increased frequency | 2 (9) | 0 (0) | |
| Pelvic organ prolapse symptoms, n (%) | |||
| Bulging/lump inside of the vagina: | |||
| Reduced frequency | 1 (5) | 3 (12) | |
| No change | 19 (86) | 21 (84) | |
| Increased frequency | 2 (9) | 1 (4) | 0.263* |
| Bulging/lump outside of the vagina: | |||
| Reduced frequency | 2 (9) | 1 (4) | |
| No change | 19 (86) | 22 (88) | |
| Increased frequency | 1 (5) | 2 (8) | 0.440* |
*Analysed by Mann-Whitney U test.
†Analysed by χ2 test.
PFMT, pelvic floor muscle training; PGI-I, Patient Global Impression of Improvement.
Other pelvic floor disorders
Table 4 shows that changes in symptoms of AI and POP were similar in both groups.
Self-Efficacy Scale for Practising Pelvic Floor Exercises
Twenty (90%) participants in the PFMT group responded to the SESPPFE after 1 month of PFMT. The mean change in total score was −0.7 (95% CI: −9.2 to 7.8, p=0.875) on a scale of 0–100, suggesting that the participants did not improve their self-efficacy for PFMT or beliefs in expected results.
Discussion
We found that a 16-week PFM home-training programme may improve the frequency, amount and bother of SUI in female functional fitness exercisers. The within-group reduction of the ICIQ-UI-SF score of 1.3 for the PFMT group and the between-group difference of 1.4 to the control group were below the previously reported MIDs of 2.5 and 1.6, respectively.18 However, the upper ends of the CIs reached worthwhile effects, indicating a possibility of beneficial effects on symptoms of SUI in favour of the PFMT group. Our sample had a lower severity of preintervention total scores compared with the sample used to calculate MIDs (mean: 10.2).18 A large prospective study of an app-based approach to PFMT found that more severe baseline scores of the ICIQ-UI-SF were related to larger improvements,32 and a change of 1.33 has been calculated as MID for women with moderate severity.33 ICIQ-UI-SF baseline severity should therefore be considered when using MID to interpret results. Additionally, nulliparous women often report mild UI symptoms.34 35 Given the large proportion of nulliparous women in our sample (50%), the mean reduction in ICIQ-UI-SF score may have been influenced by less severe UI at baseline among these women. Unfortunately, we lacked statistical power to perform subgroup analysis based on severity categories in our sample. In our sample, >60% of the women in the PFMT group and only 8% in the control group reported improvements on the PGI-I scale, suggesting clinically relevant changes of the ICIQ-UI-SF score in favour of the PFMT group.
A Cochrane review of >1800 women showed that women who performed PFMT were six times more likely to be cured of SUI compared with control groups with no treatment.8 None of the participants in our study reported a complete cure for SUI. This may be explained by a higher exposure to high-intensity training and possible constant triggers of leakage in this group of sportswomen compared with the general female population.
To our knowledge, this is the first RCT of PFMT in functional fitness exercisers. In a recent systematic review of PFMT in athletic women with SUI,10 the results from the included studies showed promising results for improving SUI and PFM strength. However, none of the studies included functional fitness exercisers, and most studies were small scaled. PFMT in female volleyball players was shown to significantly reduce the amount of leakage compared with a control group with no intervention in a previous RCT.36 Comparisons of the results with our study are challenging due to differences in intervention, participant characteristics and measurement methods.
The ICIQ-UI-SF was chosen as a primary outcome since it has been proven valid, reliable and responsive to change17 and has recommendation A by the International Continence Society to assess symptoms of UI.37 However, self-reported data may be limited by recall bias and inaccuracy of categorical data.38 In studies of PFMT in volleyball athletes, short-term pad tests were used as the primary outcome measure.36 39 The pad test offers the advantage of providing a direct measure of the amount of urine loss during exercise. Studies of short-term pad tests have revealed poor reproducibility and various sensitivity (34%–83%) and specificity (65%–89%) in accurately predicting UI.40 If the pad test is to be used in future studies, a standardised and sport-specific protocol should be established and further validated and reliability tested.
We found no change in symptoms of POP or AI. A few participants from both groups reported worsening of symptoms of AI and POP, but there were no differences in change of frequency when comparing the two groups. These results may be explained by random recall bias of the categorical responses, increased training intensities or increased awareness of these symptoms in both groups. To date, there is good evidence/recommendations that PFMT is effective in improving symptoms of POP,41 but for AI, the results are inconsistent.42
Our PFMT protocol followed recommendations for effective training dosage,43 but the PFMT group did not improve their PFM strength or endurance significantly compared with the control group. The CIs were wide, suggesting various responses related to improvements in PFM strength and endurance. The upper limits of the CIs for within-group and between-group differences were above the previously reported minimal detectable change of 7.6 cmH2O for PFM strength and 59.5 cmH2O/s for endurance,23 suggesting possible worthwhile effects in favour of the PFMT group. Previous studies with similar intervention and measurement methods used to assess PFM variables have shown larger improvements in PFM strength of 15.5 cmH2O14 and 13.1 cmH2O.16 In these studies, the participants had weekly supervised training with a physiotherapist and more follow-up assessments of the PFMs, and the intervention period was longer compared with ours (6 months vs 4 months). The two former RCTs also reported better adherence with close to 100% and 80%, respectively. These results suggest that supervised training, follow-up assessments and training durations of at least 6 months should be recommended to improve PFM strength and endurance. However, our pragmatic approach may be more in line with a real-life setting for athletes where not all may have the opportunity to attend weekly/monthly visits with a physiotherapist. Although no change in PFM variables was found, the reported improvements in UI symptoms may have been explained by other morphological changes, such as elevated bladder neck and bowel position and narrowing of the levator hiatus.9 These changes may result in an improved firmness of the pelvic floor with less opening of the levator hiatus and downward movement during an increase in IAP and possibly also automatic PFM response to increases in IAP.9 15 If available, 3D/4D ultrasonography measures of the pelvic floor may provide valuable measures of physiological adaptions of PFMT9 44 45 in future studies.
Strengths of the present study are the randomised design, concealed allocation, blinding of the assessor, a priori power calculation and the use of valid and reliable measurement tools to assess UI and PFM variables. Further, the same assessor performed all measurements of the PFMs with a standardised and consistent protocol. Finally, the intervention was based on strength training principles and followed a previously proven effective protocol to improve SUI and PFM strength. The women received advice on alternative progressions and reminders to adhere to the prescribed training sessions. Our inclusion criteria were not restricted to performance level, age or severity of SUI, and our results may therefore be generalisable to a variety of female adults who engage in functional fitness training with symptoms of SUI.
A limitation of the study is the lack of supervised training and follow-up assessments which may have negatively influenced adherence and intensity of the training. The use of a self-reported questionnaire as the main outcome may have been affected by recall bias, and the treatment effect may have been underestimated by categorical responses. The questionnaire did not include questions regarding urinary leakage during functional fitness-specific exercises (such as rope jumping), and possible improvements in UI during these exercises may not have been covered by the ICIQ-UI-SF. We did not monitor functional fitness training loads or exercise types during the intervention period, which may influence the amount/frequency of UI. Also, questions regarding the use of tampons or other anti-incontinence devices (pessaries and vaginal inserts) were not included. These devices have previously been shown to decrease the amount of leakage during CrossFit exercises.46 However, due to the RCT design, this would be equally distributed between the two groups and not systematically affect one group more than the other. Finally, our results may have been influenced by response bias due to missing outcome data from four participants at post test.
Practical implications
PFMT should be recommended as first-line treatment in female functional fitness exercisers as it may improve symptoms of SUI. However, supervised training and follow-up assessments with a pelvic floor specialist may be beneficial to improve self-efficacy, adherence and PFM strength. A longer training period (>6 months) may lead to further improvements in SUI and PFM strength. Increased knowledge of treatment options may encourage women to stay active and continue their functional fitness training.
Conclusion
We found that a 16-week home-training programme of the PFM led to improvements in SUI in female functional fitness exercisers. However, the PFMT group did not improve their PFM strength and endurance significantly compared with the control group.
Acknowledgments
The authors would like to thank all the women who participated in the study for their contribution and all who helped us share information about the study on social media. In addition, we would like to thank PhD Candidate Marte Charlotte Dobbertin Gram, Norwegian School of Sport Sciences, for the randomisation of the participants and follow-up of the intervention group; Ingeborg Hoff Brækken, Merete Kolberg Tennfjord and Ingrid Næss for teaching of the pelvic floor muscle assessments; Tove Villumstad for the help with the Camtech Software; Associate Professor Morten Wang Fagerland and Professor Ingar Holme, Norwegian School of Sport Sciences, for the advice on the statistical analysis; Clara Karoliussen and Kristian Gabrielsen for providing physiotherapy rooms for testing at Trondheim and Drammen; Francois Gazzona for the technical support for AthleteMonitoring; and CrossFit Level 2 trainer Mathias Hauger and CrossFit Level 1 trainer Marie Vogt for their advises in the development of the study protocol.
Footnotes
Contributors: KLS: concept/design, data collection, data analysis, manuscript draft, critical revision and guarantor. MEE: concept/design and critical revision. KB: concept/design, advice during data collection and data analysis, and critical revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Regional Ethics Committee (2018/2211/REK Sør-øst B, 20.12.2018) of the Norwegian Centre for Research Data (NSD: 199381, 24.01.2019). Participants gave informed consent to participate in the study before taking part.
References
- 1. Ruiz-Zapata AM, Feola AJ, Heesakkers J, et al. Biomechanical properties of the pelvic floor and its relation to pelvic floor disorders. European Urology Supplements 2018;17:80–90. 10.1016/j.eursup.2017.12.002 [DOI] [Google Scholar]
- 2. Bø K, Nygaard IE. Is physical activity good or bad for the female pelvic floor. Sports Med 2020;50:471–84. 10.1007/s40279-019-01243-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bø K. Urinary Incontinence, pelvic floor dysfunction, exercise and sport. Sports Med 2004;34:451–64. 10.2165/00007256-200434070-00004 [DOI] [PubMed] [Google Scholar]
- 4. Dominski FH, Tibana RA, Andrade A. "Functional fitness training", Crossfit, HIMT, or HIFT: what is the preferable terminology. Front Sports Act Living 2022;4:882195. 10.3389/fspor.2022.882195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gephart LF, Doersch KM, Reyes M, et al. Intraabdominal pressure in women during Crossfit exercises and the effect of age and parity. Proc (Bayl Univ Med Cent) 2018;31:289–93. 10.1080/08998280.2018.1446888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dominguez-Antuña E, Diz JC, Suárez-Iglesias D, et al. Prevalence of urinary Incontinence in female Crossfit athletes: a systematic review with meta-analysis. Int Urogynecol J 2023;34:621–34. 10.1007/s00192-022-05244-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haylen BT, de Ridder D, Freeman RM, et al. An international Urogynecological Association (IUGA)/International continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29:4–20. 10.1002/nau.20798 [DOI] [PubMed] [Google Scholar]
- 8. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary Incontinence in women. Cochrane Database Syst Rev 2018;10:CD005654. 10.1002/14651858.CD005654.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoff Brækken I, Majida M, Engh ME, et al. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: a randomized controlled trial. Obstet Gynecol 2010;115:317–24. 10.1097/AOG.0b013e3181cbd35f [DOI] [PubMed] [Google Scholar]
- 10. Fukuda FS, Arbieto ERM, Da Roza T, et al. Pelvic floor muscle training in women practicing high-impact sports: a systematic review. Int J Sports Med 2023;44:397–405. 10.1055/a-1939-4798 [DOI] [PubMed] [Google Scholar]
- 11. Romero-Franco N, Molina-Mula J, Bosch-Donate E, et al. Therapeutic exercise to improve pelvic floor muscle function in a female sporting population: a systematic review and meta-analysis. Physiotherapy 2021;113:44–52. 10.1016/j.physio.2021.04.006 [DOI] [PubMed] [Google Scholar]
- 12. Pandis N, Chung B, Scherer RW, et al. CONSORT 2010 statement: extension checklist for reporting within person randomised trials. Br J Dermatol 2019;180:534–52. 10.1111/bjd.17239 [DOI] [PubMed] [Google Scholar]
- 13. Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress Incontinence in women. BMJ 1999;318:487–93. 10.1136/bmj.318.7182.487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bø K, Hagen RH, Kvarstein B, et al. Pelvic floor muscle exercise for the treatment of female stress urinary Incontinence: III. effects of two different degrees of pelvic floor muscle exercises. Neurourol Urodyn 1990;9:489–502. 10.1002/nau.1930090505 [DOI] [Google Scholar]
- 15. Bø K. Physiotherapy management of urinary Incontinence in females. J Physiother 2020;66:147–54. 10.1016/j.jphys.2020.06.011 [DOI] [PubMed] [Google Scholar]
- 16. Braekken IH, Majida M, Engh ME, et al. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol 2010;203:170. 10.1016/j.ajog.2010.02.037 [DOI] [PubMed] [Google Scholar]
- 17. Avery K, Donovan J, Peters TJ, et al. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 2004;23:322–30. 10.1002/nau.20041 [DOI] [PubMed] [Google Scholar]
- 18. Nyström E, Sjöström M, Stenlund H, et al. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn 2015;34:747–51. 10.1002/nau.22657 [DOI] [PubMed] [Google Scholar]
- 19. Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol 2003;189:98–101. 10.1067/mob.2003.379 [DOI] [PubMed] [Google Scholar]
- 20. Bø K, Kvarstein B, Hagen R, et al. Pelvic floor muscle exercise for the treatment of female stress urinary Incontinence, I: reliability of vaginal pressure measurements of pelvic floor muscle strength. Neurourol Urodyn 1990;9:471–7. 10.1002/nau.1930090503 [DOI] [Google Scholar]
- 21. Bø K, Kvarstein B, Hagen RR, et al. Pelvic floor muscle exercise for the treatment of female stress urinary Incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods for control of correct contraction. Neurourol Urodyn 1990;9:479–87. 10.1002/nau.1930090504 [DOI] [Google Scholar]
- 22. Bø K. Pressure measurements during pelvic floor muscle contractions: the effect of different positions of the vaginal measuring device. Neurourol Urodyn 1992;11:107–13. 10.1002/nau.1930110205 [DOI] [Google Scholar]
- 23. Tennfjord MK, Engh ME, Bø K. An Intra- and interrater reliability and agreement study of vaginal resting pressure, pelvic floor muscle strength, and muscular endurance using a manometer. Int Urogynecol J 2017;28:1507–14. 10.1007/s00192-017-3290-y [DOI] [PubMed] [Google Scholar]
- 24. Brækken IH, Stuge B, Tveter AT, et al. Reliability, validity and responsiveness of pelvic floor muscle surface electromyography and manometry. Int Urogynecol J 2021;32:3267–74. 10.1007/s00192-021-04881-0 [DOI] [PubMed] [Google Scholar]
- 25. Diaz DC, Robinson D, Bosch R, et al. Patient-reported outcome assessment. In: Abrams P, Cardozo L, Wagg A, et al., eds. Incontinence. 1. 6 ed. Tokyo: 6th International Consultation on Incontinence, 2017: 541–98. [Google Scholar]
- 26. Sacomori C, Cardoso FL, Porto IP, et al. The development and psychometric evaluation of a self-efficacy scale for practicing pelvic floor exercises. Braz J Phys Ther 2013;17:336–42. 10.1590/S1413-35552013005000104 [DOI] [PubMed] [Google Scholar]
- 27. Skaug KL, Engh ME, Frawley H, et al. Prevalence of pelvic floor dysfunction, bother, and risk factors and knowledge of the pelvic floor muscles in Norwegian male and female Powerlifters and Olympic Weightlifters. J Strength Cond Res 2022;36:2800–7. 10.1519/JSC.0000000000003919 [DOI] [PubMed] [Google Scholar]
- 28. D’Lauro C, Jones ER, Swope LM, et al. Under-representation of female athletes in research informing influential concussion consensus and position statements: an evidence review and synthesis. Br J Sports Med 2022;56:981–7. 10.1136/bjsports-2021-105045 [DOI] [PubMed] [Google Scholar]
- 29. Anderson N, Robinson DG, Verhagen E, et al. Under-representation of women is alive and well in sport and exercise medicine: what it looks like and what we can do about it. BMJ Open Sport Exerc Med 2023;9:e001606. 10.1136/bmjsem-2023-001606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Paul RW, Sonnier JH, Johnson EE, et al. Inequalities in the evaluation of male versus female athletes in sports medicine research: a systematic review. Am J Sports Med 2023;51:3335–42. 10.1177/03635465221131281 [DOI] [PubMed] [Google Scholar]
- 31. Dominguez-Antuña E, Diz JC, Ayán C, et al. Prevalence and severity of urinary Incontinence among male and female competitors and recreational Crossfit(R) practitioners. Eur J Obstet Gynecol Reprod Biol 2022;276:144–7. 10.1016/j.ejogrb.2022.07.014 [DOI] [PubMed] [Google Scholar]
- 32. Rygh P, Asklund I, Samuelsson E. Real-world effectiveness of app-based treatment for urinary Incontinence: a cohort study. BMJ Open 2021;11:e040819. 10.1136/bmjopen-2020-040819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Asklund I, Nyström E, Lindam A, et al. 233 minimum important difference of the ICIQ-UI SF score after self-management of urinary Incontinence via a freely available mobile App. Continence 2022;2:100322. 10.1016/j.cont.2022.100322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Al-Mukhtar Othman J, Åkervall S, Milsom I, et al. Urinary Incontinence in nulliparous women aged 25-64 years: a national survey. Am J Obstet Gynecol 2017;216:149. 10.1016/j.ajog.2016.09.104 [DOI] [PubMed] [Google Scholar]
- 35. Skaug KL, Engh ME, Frawley H, et al. Urinary and anal incontinence among female gymnasts and cheerleaders-bother and associated factors. A cross-sectional study. Int Urogynecol J 2022;33:955–64. 10.1007/s00192-021-04696-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ferreira S, Ferreira M, Carvalhais A, et al. Reeducation of pelvic floor muscles in volleyball athletes. Rev Assoc Med Bras 2014;60:428–33. 10.1590/1806-9282.60.05.010 [DOI] [Google Scholar]
- 37. Dumoulin C, Booth J, Cacciari L, et al. Adult conservative management. In: Cardozo L, Rovner E, Wagg A, eds. Incontinence. 7th ed. Bristol UK: ICI-ICS. International Continence Society, 2023: 798–1021. [Google Scholar]
- 38. Choi BCK, Pak AWP. A catalog of biases in questionnaires. Prev Chronic Dis 2005;2:A13. [PMC free article] [PubMed] [Google Scholar]
- 39. Pires TF, Pires PM, Moreira MH, et al. Pelvic floor muscle training in female athletes: a randomized controlled pilot study. Int J Sports Med 2020;41:264–70. 10.1055/a-1073-7977 [DOI] [PubMed] [Google Scholar]
- 40. Ferreira CHJ, Bø K. The pad test for urinary incontinence in women. J Physiother 2015;61:98. 10.1016/j.jphys.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 41. Bø K, Anglès-Acedo S, Batra A, et al. International urogynecology consultation chapter 3 committee 2; conservative treatment of patient with pelvic organ prolapse: pelvic floor muscle training. Int Urogynecol J 2022;33:2633–67. 10.1007/s00192-022-05324-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bliss D, Mimura T, Berghmans B, et al. Assessment and conservative management of Feacal Incontinence and quality of life. In: Incontinence, 7th ed. Bristol UK: ICI-ICS. International Continence Society, 2023: 1577–653. [Google Scholar]
- 43. Bø K. Pelvic floor muscle training is effective in treatment of female stress urinary Incontinence, but how does it work. Int Urogynecol J Pelvic Floor Dysfunct 2004;15:76–84. 10.1007/s00192-004-1125-0 [DOI] [PubMed] [Google Scholar]
- 44. Braekken IH, Majida M, Engh ME, et al. Test-retest reliability of pelvic floor muscle contraction measured by 4D ultrasound. Neurourol Urodyn 2009;28:68–73. 10.1002/nau.20618 [DOI] [PubMed] [Google Scholar]
- 45. Majida M, Braekken IH, Umek W, et al. Interobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and function. Ultrasound Obstet Gynecol 2009;33:567–73. 10.1002/uog.6351 [DOI] [PubMed] [Google Scholar]
- 46. Gephart L, High R, Lewis A, et al. Comparison of anti-Incontinence devices during Crossfit exercise. IUGA 43rd Annual Meeting June 27-30; Vienna, Austria: Int Urogynecol J, 2018:1–272 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.