Abstract
Previous research has found differences in characteristics of beneficiaries enrolled in Medicare fee-for-service (FFS) versus Medicare Advantage (MA) but there has been limited research using more recent MA enrollment data. We used 1997–2005 National Health Interview Survey (NHIS) data linked to 2000–2009 Medicare enrollment data to compare characteristics of Medicare beneficiaries before their initial enrollment into Medicare FFS or MA and whether the characteristics of beneficiaries changed from 2006–2009 compared to 2000–2005. During this period of MA growth, the greatest increase in enrollment appears to have come from those with no chronic conditions and men.
Keywords: Medicare Advantage, favorable selection, managed care, Medicare
Background
Medicare Advantage (MA) was intended to provide Medicare beneficiaries with more choice in health care plans and for Medicare to benefit from possible increased efficiency of managed care plans, which could help cut overall Medicare costs (MedPAC, 2001; McGuire et al., 2011). Since managed care plans became available in the 1970’s, enrollment has increased or decreased in response to various changes in policy. The Medicare Modernization Act of 2003 (MMA) included the largest changes to the Medicare program since the program began (McGuire et al., 2011). For example, the MMA created regional preferred provider organizations (PPO’s) that were intended to increase access to managed care plans in rural areas, changed the payment structure to MA plans, and established Medicare Part D, which, as an optional benefit, created stand-alone drug plans. Many of the law’s provisions went into effect on January 1, 2006 and had a substantial impact on MA enrollment. Enrollment in MA increased from 5.3 million beneficiaries in 2005 to 14.4 million in 2013, and now covers approximately 28% of all Medicare beneficiaries (Kaiser Family Foundation, 2013).
Previous research on enrollees prior to the implementation of the MMA found differences in demographic and health characteristics of beneficiaries enrolled in traditional Medicare fee-for-service (FFS) versus MA. In these earlier studies, MA enrollees were found to be younger, female, Hispanic, lower educated and to have fewer health conditions (Riley et al., 1996; Mello et al., 2003; Taylor et al., 1995; Murgolo, 2002; Virnig et al., 1998; Morgan et al., 1997; Greenwald et al., 2000). The health characteristics of beneficiaries who enroll in MA not only have important implications concerning the cost of MA plans to Medicare but to research using Medicare data, as well. The Centers for Medicare and Medicaid Services (CMS) does not receive most claims data from MA plans and therefore, research using Medicare claims are almost exclusively limited to beneficiaries in FFS. If the characteristics of beneficiaries in FFS differ from those in MA, then the generalizability of studies on the FFS population to the entire Medicare population may be questionable. And because of various policy changes, the difference in characteristics of fee-for-serve and MA enrollees may have changed over time.
In addition to the changes from the MMA, a new risk-adjustment model from the Balanced Budget Act of 1997 was phased into the payment structure of MA from 2004 to 2007. The new risk adjustment model was intended to reduce possible overpayments to MA and limit the incentive for plans to select the mostly healthy and profitable potential enrollees. The model incorporated the demographic characteristics of beneficiaries as well as clinical diagnoses from selected inpatient and outpatient claims (McGuire et al., 2011). Only a few studies have examined the health characteristics of MA and FFS enrollees since the implementation of the MMA and the new risk adjustment model was phased in. Results from these more recent studies have been mixed (Morrisey et al., 2010; McWilliams et al., 2012; Newhouse et al., 2012; Riley, 2012). While studies have shown that favorable selection persists in beneficiaries switching into or out of MA, there is some evidence of a reduction in the degree of favorable selection (McWilliams et al., 2012; Newhouse et al., 2012).
Because claims data are not typically available for beneficiaries enrolled in MA, these studies have mostly examined the health characteristics of Medicare beneficiaries who have switched between MA and FFS to those who were only enrolled in FFS. The National Health Interview Survey (NHIS) linked to Medicare enrollment data provides a unique opportunity to examine the health characteristics of Medicare beneficiaries before their initial enrollment into Medicare at age 65 and allows for comparisons between those who choose MA versus FFS. Since health characteristics are reported from the survey, these characteristics can be examined for all linked beneficiaries and not just those who switched between MA and FFS. The NHIS includes detailed demographic information and questions regarding health status, health conditions, health behaviors, and healthcare utilization. We used 2006–2009 Medicare enrollment data linked to prior NHIS survey data to examine the demographic and health characteristics of those enrolling in MA versus FFS at the age of 65, occurring after the implementation of the MMA and new risk adjustment models. We then examined the relationship between demographic and health characteristics of those enrolling in MA versus FFS in 2000–2005, and summarized whether the characteristics of those enrolling in MA changed between the two time periods.
Methods
Data Source
We used self-reported demographic and health data from the 1997–2005 NHIS linked with Medicare enrollment data from 2000–2009. The NHIS is an in-person household survey designed to produce nationally representative estimates of the civilian, non-institutionalized population of the United States. Information is collected on each member of the household, and within each family one adult is sampled to complete a more in-depth survey, which includes questions regarding various health characteristics and behaviors. A detailed description of the NHIS is available elsewhere (CDC, 2013).
Surveys from the National Center for Health Statistics (NCHS) were linked with Medicare data. Survey participants were eligible for the linkage if they provided sufficient personally identifiable information (PII) and did not refuse to have their data linked. Linkage eligibility ranged from 46% in 2005 to 59% in 1997. Of the linkage eligible respondents aged 65 years and older at the time of survey between 1997 and 2005, approximately 98% successfully linked with Medicare (CDC, 2014).
The study population was restricted to survey participants aged 60–64 years at the time of the survey with six months of Medicare enrollment data available when they aged into the program at age 65. Since we used NHIS survey data beginning in 1997 and our latest available information on Medicare enrollment was for 2009, we included NHIS survey participants from 2001–2005 for Medicare enrollment in 2006–2009 and NHIS survey participants from 1997–2004 for Medicare enrollment in 2000–2005. Our sample size for initial Medicare enrollees at age 65 was therefore larger for 2000–2005 compared to 2006–2009 since we were able to use pre-Medicare characteristics for more NHIS survey years for this Medicare enrollment sample. Using monthly Medicare enrollment indicators, we determined the first month of enrollment upon turning 65. Enrollment into MA was defined as any MA enrollment during the first 6 months of entitlement. Survey participants were excluded if they were eligible for Medicare before turning 65 as a result of a disability or End Stage Renal Disease (ESRD), or were dually eligible for Medicaid after they became eligible for Medicare. We further limited the study population to beneficiaries with both Part A and Part B Medicare during the first 6 months after turning 65 since those not enrolling in Part B may continue to have primary sources of insurance other than Medicare.
Variables
We examined demographic and health characteristics associated with MA enrollment. Demographic variables in the analysis included sex, race/ethnicity [non-Hispanic white, non-Hispanic black, Hispanic, all other races and ethnicities], highest level of education [less than high school degree, high school degree/GED/Some college, post-high school degree], household income as a percentage of the Federal Poverty Level [(FPL) <200%, 200–399%, ≥400%], and pre-Medicare health insurance coverage [private health maintenance organization (HMO), private insurance/military coverage, no coverage/Medicaid]. Geographic variables included urban/rural residence and U.S. Census Region (Northeast, Midwest, South, West).
The health characteristics of the participants were based on the presence of a chronic disease or health condition, self-rated health, healthcare utilization, and health behaviors. Health conditions were based on self-reported responses to questions beginning “Have you ever been told by a doctor or other health professional that you had….” The presence of a chronic condition included any report of diabetes, cancer (excluding non-melanoma skin cancer), hypertension (if diagnosed on more than one occasion), myocardial infarction, stroke, angina, coronary heart disease, emphysema, chronic kidney problems, liver disease, and asthma. Self-rated health status was dichotomized into Excellent/Very Good/Good and Fair/Poor. For health behaviors, we examined current smoking status (yes, no) and alcohol use (any, none) at the time of survey. We also examined self-reported healthcare utilization in the 12 months prior to the interview. This included a dichotomous variable for the number of medical visits to a physician or other health care professional (0–3, ≥4) and any hospitalization.
Statistical Analysis
We summarized average MA enrollment during 2006–2009 by demographic and health characteristics, using a chi-square test to determine bivariate differences in MA enrollment by demographic and health characteristics. We then used a logit model to calculate the multivariate association between each demographic and health characteristic and MA enrollment in 2006–2009, controlling for the other characteristics. We reported marginal effects from the logit model. That is, we report the average change in the predicted probability of MA enrollment of a one-unit change in the independent variable for each observation in the sample, holding all other covariates at their observed values.
In order to explore whether predictors of MA enrollment were different in 2006–2009 compared to earlier years, we used the same logit model to predict MA enrollment in 2000–2005 as a function of the same set of demographic and health variables. We calculated the difference in the effect of each characteristic on MA enrollment during the two periods by subtracting the marginal effect in 2006–2009 from the effect in 2000–2005. We refer to these estimates as difference-in-difference estimates. For example, we calculate the difference in MA enrollment in 2006–2009 for individuals with and without a particular characteristic and subtract the difference in MA enrollment in 2000–2005 for individuals with and without this characteristic, therefore estimating the difference in the association between this characteristic and MA enrollment in the later compared to the earlier period. The standard error on this difference came from a model pooling data from both time periods and included interactions between each independent variable and a dichotomous variable indicating data coming from the latter period.
All estimates were weighted to account for non-response and sampling probabilities. To account for possible differences between survey participants who were eligible for the linkage and those who were not, survey weights were further adjusted by sex, race/ethnicity, and self-rated health status using PROC WTADJUST in SUDAAN (Judson et al., 2013). Standard errors were calculated using SUDAAN to account for the complex survey design. Estimates were considered statistically significant at p ≤ 0.10, although we indicate whether estimates are statistically significant at the 10, 5, or 1 percent level.
Study Population
There were 5,970 NHIS participants from 2001–2005 aged 60–64 years at the time of survey who could potentially turn 65 between 2006 and 2009. Of this group, 2,821 (47%) were eligible for the linkage with Medicare. When limiting the population to those with a full 6 months of initial enrollment data (n=1,671) and excluding participants who were eligible for Medicare due to disabilities or ESRD (n=43), were dually eligible for Medicaid (n=121), missing explanatory variables (n=60), or enrolled in Part A only (n=300), there were 1,147 participants included in the analysis for 2006–2009. In the earlier Medicare time-period (2000–2005), with a larger number of survey participants eligible for the study population from 1997–2004, there were 3,707 participants included in the analysis after similar exclusions.
Results
The study population had a larger percentage of women (55%) compared to men (45%; Table 1). Approximately 82% of the weighted population was non-Hispanic white and just over two-thirds of the study population lived in an urban residence. Approximately 85% of the population had a least a high school degree and over 50% had a household income ≥400% of the FPL. Prior to Medicare enrollment, 14% of participants had Medicaid or no health care coverage and almost one quarter were enrolled in an HMO.
Table 1.
Characteristics of the Sample and Mean Enrollment in Medicare Advantage in 2006–2009 by Self-reported Demographic and Health Characteristics.a
| n | Distribution of Sample % |
Mean Medicare Advantage Enrollment % (SE) |
|
|---|---|---|---|
| All | 1147 | 100 | 23.9 (1.3) |
| Sex | |||
| Men (Reference) | 498 | 45 | 25.0 (2.1) |
| Women | 649 | 55 | 23.0 (1.8) |
| Race/Ethnicity | |||
| Hispanic | 106 | 7.1 | 34.7 (5.9)c |
| Non-Hispanic White (Reference) | 909 | 82.4 | 23.1 (1.4) |
| Non-Hispanic Black | 101 | 6.9 | 22.5 (4.9) |
| All Other Races and Ethnicities | 31 | 3.6 | -- |
| Education | |||
| <High School (HS) Degree (Reference) | 185 | 15.1 | 27.3 (3.5) |
| HS Degree/GED/Some College | 561 | 47.2 | 25.0 (1.9) |
| Post-HS Degree | 401 | 37.6 | 21.2 (2.4) |
| Family Income as Percentage of Federal Poverty Level (FPL) | |||
| <200% FPL | 251 | 17.1 | 20.1 (2.9) |
| 200–399% FPL | 350 | 29.4 | 26.7 (2.5) |
| ≥400% FPL (Reference) | 546 | 53.5 | 23.6 (1.9) |
| Residence | |||
| Urban (Reference) | 801 | 68.7 | 25.4 (1.6) |
| Rural | 346 | 31.3 | 20.6 (2.3) |
| Region | |||
| Northeast | 184 | 17.3 | 29.3 (3.0)e |
| Midwest | 322 | 29.2 | 18.9 (2.1) |
| South (Reference) | 425 | 35.8 | 19.6 (2.2) |
| West | 216 | 17.7 | 35.4 (3.6)e |
| Pre-Medicare Insurance | |||
| Private – Health Maintenance Organization | 256 | 23 | 41.8 (3.6)e |
| Private Insurance / Military Coverage (Reference) | 698 | 63 | 17.1 (1.5) |
| No Coverage / Medicaid | 193 | 14 | 25.0 (3.5)e |
| Self-Reported Disease/Conditions b | |||
| None (Reference) | 464 | 41 | 27.6 (2.3) |
| ≥1 | 683 | 59 | 21.3 (1.7)d |
| Self-Reported Health Status | |||
| Good/Very Good/Excellent (Reference) | 997 | 88.1 | 24.0 (1.4) |
| Fair/Poor | 150 | 11.9 | 22.7 (4.2) |
| Current Smoker | |||
| No (Reference) | 924 | 82.7 | 24.5 (1.5) |
| Yes | 223 | 17.3 | 21.1 (2.9) |
| Current Alcohol Use | |||
| No (Reference) | 449 | 37.2 | 24.6 (2.4) |
| Yes | 698 | 62.8 | 23.4 (1.6) |
| Medical Visits in Past 12 Months | |||
| 0–3 (Reference) | 621 | 55.6 | 25.0 (1.8) |
| ≥4 | 526 | 44.4 | 22.5 (2.0) |
| Hospitalization in Past 12 Months | |||
| No (Reference) | 1036 | 91.3 | 24.0 (1.4) |
| Yes | 111 | 8.7 | 22.9 (4.5) |
Study population limited to National Health Interview Survey participants (2001–2005) aged 60–64 years with 6 months of Medicare enrollment data (2006–2009) upon turning 65. The table consists of weighted percents with standard errors in parentheses. SE stands for standard error. GED stands for General Educational Development tests. FPL stands for Federal poverty level.
The number of chronic condition includes any self-report of diabetes, cancer (excluding non-melanoma skin cancer), hypertension (if diagnosed on more than one occasion), myocardial infarction, stroke, angina, or coronary heart disease, emphysema, chronic kidney problems, liver disease, and asthma.
indicate that Medicare Advantage enrollment is statistically significantly different relative to the reference group at the 10, 5, or 1 percent levels, respectively.
For the health characteristics, close to 60% had a chronic condition (Table 1) but almost 90% reported that their health was Good/Very Good/Excellent. Seventeen percent of the adults were current smokers and 63% drank alcohol in the past year. In the 12 months prior to interview, approximately 44% of participants had more than 3 medical visits, although less than 10% had been hospitalized.
Initial MA enrollment upon turning 65 was 23.9% in 2006–2009 (Table 1). The percent enrolled in MA differed significantly by race/ethnicity, region and pre-Medicare health insurance. Hispanic participants were more likely to enroll in MA compared to non-Hispanic white participants (p≤0.10). Individuals in the Northeast or West regions were more likely than those in the South to enroll in MA (p≤0.01 for both). Individuals who were uninsured or on Medicaid or were on private HMO insurance were more likely than those with private, non-HMO coverage to enroll in MA (nearly 25 and 42 percent, respectively compared to about 17 percent; p≤0.01 and p≤0.10, respectively). MA enrollment was significantly lower among those with a chronic condition compared to those with no reported health conditions (p≤0.05). However, there were no significant differences in MA enrollment for any of the other health characteristics examined.
The leftmost column of Table 2 reports results from our multivariate logit model predicting MA enrollment in 2006–2009. When adjusting for other covariates, we found that MA enrollment was no longer significantly different between Hispanic and white non-Hispanic participants but there was a borderline significant difference between participants with less than a high school degree enrolling in MA compared to those with a post-high school degree (p≤0.10). The associations with region (p≤0.01) and pre-Medicare insurance (p≤0.01) remained significant. For health characteristics, individuals with no conditions were still significantly more likely to enroll in MA, by about 7.5 percentage points, compared to those with any chronic condition (p≤0.01), similar to the bivariate results reported in Table 1. There remained no difference in MA enrollment by other health characteristics, including self-reported health status, smoking and alcohol use, or healthcare utilization.
Table 2.
Association of Demographic and Health Characteristics with Medicare Advantage Enrollment in 2006–2009, 2000–2005 and 2006–2009 Compared to 2000–2005.a
| 2006–2009 | 2000–2005 | 2006–2009 Compared to 2000–2005 | |
|---|---|---|---|
| Difference (SE) | Difference (SE) | Difference-in-Difference (SE) | |
| Sex (Relative to Men) | |||
| Women | −3.6 (2.9) | 4.3 (1.0)e | −7.9 (3.2)d |
| Race/Ethnicity (Relative to Non-Hispanic White) | |||
| Hispanic | 1.8 (5.6) | 5.8 (2.3)e | −4.0 (6.3) |
| Non-Hispanic Black | 1.8 (4.6) | −1.8 (1.9) | 0.0 (5.2) |
| Education (Relative to Post High School Degree) | |||
| <High School (HS) Degree | 7.4 (4.5)c | 4.1 (1.9)d | 3.3 (4.9) |
| HS Degree/GED/Some College | 4.6 (3.1) | 4.0 (1.2)e | 0.6 (3.3) |
| Family Income as Percentage of Federal Poverty Level (FPL) (Relative to ≥400% FPL) | |||
| <200% FPL | −2.5 (4.2) | 0.0 (1.7) | −2.5 (4.7) |
| 200–399% FPL | 3.7 (3.1) | 1.4 (1.3) | 2.3 (3.6) |
| Residence (Relative to Urban) | |||
| Rural | −2.4 (3.1) | −5.2 (1.2)e | 2.8 (3.3) |
| Region (Relative to South) | |||
| Northeast | 7.2 (3.4)d | 5.5 (1.5)e | 1.7 (3.8) |
| Midwest | −0.4 (3.2) | 1.2 (1.3) | −1.6 (3.5) |
| West | 14.4 (4.0)e | 11.5 (1.9)e | 2.9 (4.1) |
| Pre-Medicare Insurance (Relative to Private Insurance or Military Coverage) | |||
| Private – Health Maintenance Organization | 22.8 (3.7)e | 17.4 (1.6)e | 5.4 (3.8) |
| No Coverage / Medicaid | 8.1 (4.5)c | 1.5 (1.4) | 6.6 (4.6) |
| Self-Reported Disease/Conditions (Relative to None) b | |||
| ≥1 | −7.5 (3.0)e | −0.6 (1.2) | −6.9 (3.3)d |
| Self-Reported Health Status (Relative to Good/Very Good/Excellent) | |||
| Fair/Poor | −2.6 (4.4) | −1.6 (1.5) | −1.0 (4.8) |
| Current Smoker (Relative to No) | |||
| Yes | −3.5 (3.4) | 0.2 (1.5) | −3.7 (3.8) |
| Current Alcohol Use | |||
| Yes | 0.5 (2.8) | 1.8 (1.2) | −2.3 (3.1) |
| Medical Visits in Past 12 Months (Relative to 0–3) | |||
| ≥4 | 0.8 (2.9) | 1.9 (1.2)d | −2.7 (3.3) |
| Hospitalization in Past 12 Months (Relative to No) | |||
| Yes | 1.5 (4.8) | −1.0 (1.7) | 2.5 (5.1) |
Study population limited to National Health Interview Survey participants (2001–2005) aged 60–64 years with 6 months of Medicare enrollment data (2006–2009) upon turning 65. All figures are weighted. SE stands for standard error. GED stands for General Educational Development tests. FPL stands for Federal poverty level. The table reports marginal effects from logit models predicting Medicare Advantage enrollment in 2006–2009 (first column) and 2000–2005 (second column). Differences and standards errors in the final column are marginal effects from a logit model pooling data from 2000–2005 and 2006–2009 and including interactions between each independent variable and a dichotomous variable indicating data coming from the latter period. The standard errors are those associated with the appropriate interactions. Because there were so few participants (n=38) with a race/ethnicity in the “all other races and ethnicities” category, they were recoded into the white non-Hispanic category in our multivariate models.
The presence of a chronic condition includes any self-report of diabetes, cancer (excluding non-melanoma skin cancer), hypertension (if diagnosed on more than one occasion), myocardial infarction, stroke, angina, or coronary heart disease, emphysema, chronic kidney problems, liver disease, or asthma.
indicate that Medicare Advantage enrollment is statistically significantly different relative to the reference group at the 10, 5, or 1 percent levels, respectively.
The middle column of Table 2 reports results from our multivariate logit model predicting MA enrollment in 2000–2005. Although not reported in the table, mean MA enrollment in 2000–2005 was 11.8%, with enrollment increasing to 23.9% in 2006–2009. Several predictors of MA enrollment were similar in 2000–2005 and 2006–2009. For example, those with less than a high school degree (compared to a post high school degree), in the Northeast or West region relative to the South, and with private HMO or no insurance/Medicaid prior to age 65 were more likely to enroll in MA at age 65 in both time periods. However, the final column of Table 2, which compares the predictors of MA enrollment in the later compared to the earlier time period, does show that the association between two characteristics and MA enrollment changed over time. The first is gender. Women were more likely than men to enroll in MA in the earlier period but no longer more likely to enroll in MA in the later period. So the increase in MA enrollment between 2000–2005 and 2006–2009 occurred differentially among men (The p-value for difference-in-difference in the final column of Table 2 is 0.01). We also found that the presence of a chronic condition was associated with a 7.5 percentage point lower MA enrollment rate in 2006–2009 and only a slightly (and not statistically significant) lower enrollment rate in 2000–2005, indicating that the increase in MA enrollment between 2000–2005 and 2006–2009 came disproportionately from those with no chronic conditions (p≤0.05).
To further investigate the results we found for the presence of a health condition, we replaced the dichotomous condition variable in each multivariate logit model with variables for specific chronic conditions that had sufficient numbers for the 2006–2009 Medicare enrollment years, including hypertension (n=478), a combined cardiovascular disease variable (including myocardial infarction, stroke, angina, or coronary heart disease) (n=199), and cancer (n=91). We found that MA enrollment for those with cardiovascular disease was 5.5 percentage points lower than those without in 2006–2009 while there was not a significant difference in MA enrollment by disease status in the earlier period (Figure 1). As a result, the increase in MA enrollment between the two time-periods came differentially from those without cardiovascular disease (p≤0.05 for difference-in-difference). Although they followed the same pattern, there were no significant differences in MA enrollment by presence of hypertension or cancer in either time-period, and the changes from 2000–2005 to 2006–2009 were not significantly different for those with or without the conditions.
Figure 1.
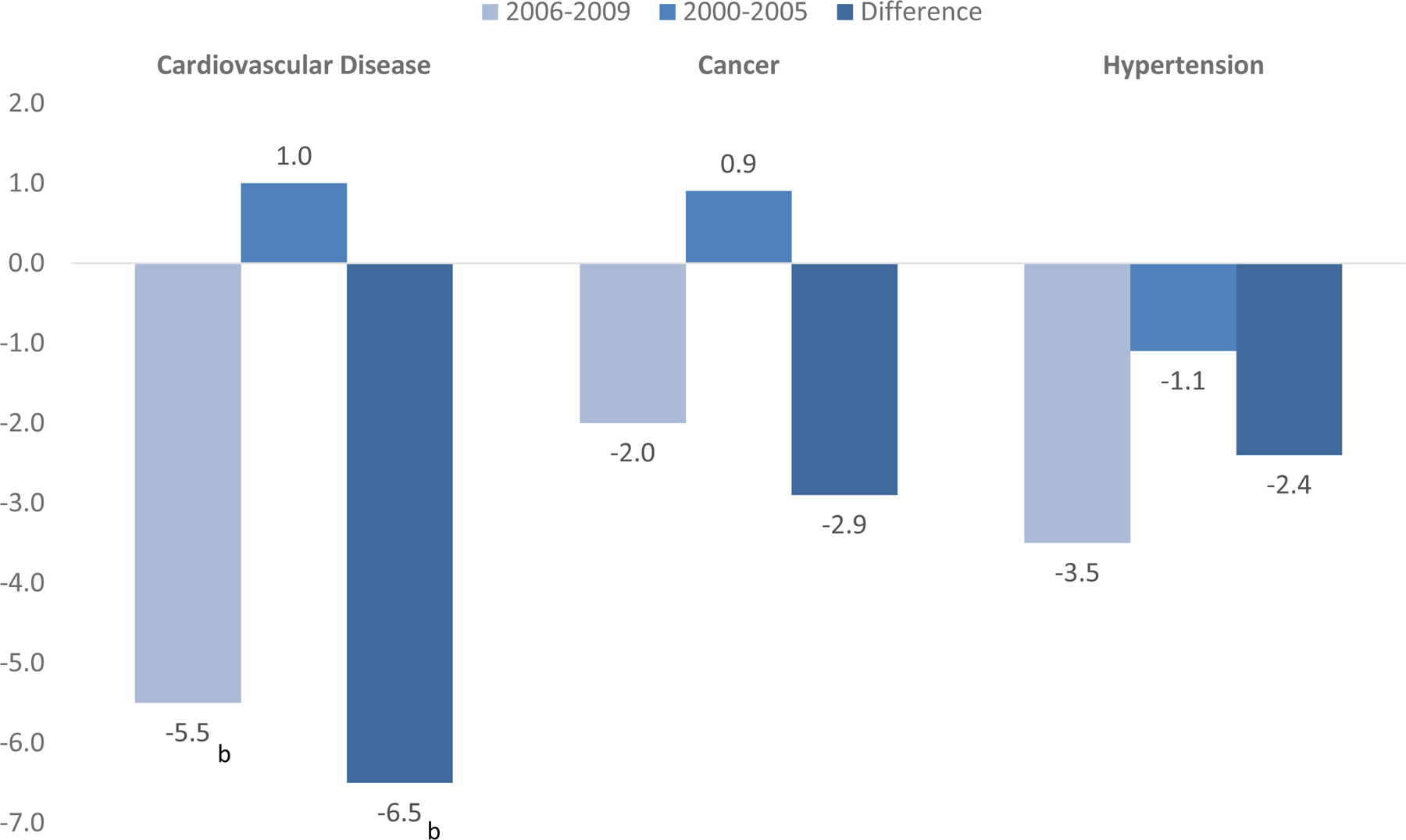
Association Between the Presence of Selected Chronic Conditions and Medicare Advantage Enrollment in 2006–2009, 2000–2005 and in 2006–2009 compared to 2000–2005
Note: The figure reports marginal effects from logit models predicting Medicare Advantage enrollment those with compared to without selected chronic conditions in 2006–2009 (first bar) and 2000–2005 (second bar). Differences and standards errors in the final bar are marginal effects from a logit model pooling data from 2000–2005 and 2006–2009 and including interactions indicating the presence of the chronic condition and a dichotomous variable indicating data coming from the latter period. The standard errors are those associated with the appropriate interaction. All control variables listed in Table 2 are included. The symbols a, b, and c indicate statistical significance at the 10, 5, and 1 percent levels, respectively.
Discussion
Using health survey data linked with future Medicare enrollment data available since the MMA went into effect, we examined the association between demographic and health characteristics and initial enrollment into MA at age 65. We also assessed whether the relationships between these characteristics and MA enrollment were different during this recent period compared to an earlier one (2000–2005). We found that some predictors of MA enrollment were the same in the two time periods. For example, being enrolled in an HMO and leaving in the Northeast or West rather than the South significantly predicted MA enrollment in both 2000–2005 and 2006–2009. However, we found that those with a chronic condition, cardiovascular disease in particular, were less likely to enroll in MA in 2006–2009 compared to those without these conditions, a relationship that was not as apparent in the earlier period. However, we did not find differential enrollment for any other health characteristic examined. We also found that the increase in MA enrollment from 2000–2005 to 2006–2009 came disproportionately from men who were less likely than women to enroll in MA in 2000–2005 but no longer less likely to enroll in 2006–2009.
While the demographic characteristics of participants enrolling in MA during the earlier time-period were consistent with previous literature, the increase in enrollment we observed for participants with a chronic condition appears to be in contrast to recent studies (McWilliams et al., 2012; Newhouse et al., 2012). There are a number of possible reasons for the difference in results. Unlike previous studies that assessed the characteristics of beneficiaries who switched between MA and FFS, with the linked NHIS-Medicare data we were able to compare the characteristics of those who enroll in MA and FFS in the first six months after turning age 65 using characteristics of beneficiaries before they turned 65. Most beneficiaries who enroll in MA do not switch to FFS (Newhouse et al., 2012; Riley, 2012) and therefore, the limited number of beneficiaries who switch from MA to FFS may not be comparable to the larger population that initially enrolls in one program or the other. Consistent with this, McWilliams et al. (2012) found differences in the health characteristics of beneficiaries who switched into or out of MA compared to the overall MA population that did not switch (McWilliams et al., 2012).
Although improved risk adjustment should have reduced the incentive for selection of healthier individuals into MA in the later period, there is evidence that plan offerings may still foster selection. For example, Cooper and Trivedi (2012) found that some plans offer fitness club memberships and attract a healthier population than those that do not. They also found that the number of plans offering memberships had substantially increased from 2004 to 2008. In addition, Brown et al. (2012) provided evidence that MA plans may have increased selection for healthier beneficiaries by targeting factors not included in the newly implemented risk models. However, this finding was not replicated in a similar analysis with a larger sample size and additional year of data (Newhouse et al., 2012). It is also possible that the introduction of Medicare Part D reduced the incentive for some individuals with chronic conditions to enroll in MA since prior to the MMA, Medicare FFS did not offer drug coverage while some MA plans did.
One of the strengths of this analysis is having self-reported health characteristics prior to enrollment in Medicare. While self-reported data are subject to reporting bias and mis-reporting, McWilliams et al. (2012) found self-reported health care utilization to be predictive of Medicare spending. In addition, self-reported health conditions are not subject to coding practices, which can be influenced by payment incentives.
However, there are a number of limitations that need to be acknowledged in this analysis. We were not able to differentiate between the types of MA plans, which could include private FFS, preferred provider organizations, Special Needs Plans, and health maintenance organizations. It is unclear if the results in this analysis would be similar for all types of MA plans. Also, although we considered the association between the presence of self-reported health conditions and MA enrollment, we were unable to determine the severity of the conditions, which could influence enrollment decisions. However, our models did control for the self-reported number of hospitalizations and medical visits in our analysis, which might act as a proxy for illness severity. Finally, since we consider MA enrollment among individuals who enroll in Medicare Parts A and B in the first six months after turning 65, we do not examine the MA enrollment decisions for the minority of individuals who continue to work full-time for a period after age 65 and maintain private employer-provided insurance as a primary insurance source. These individuals make the MA enrollment decision at later ages and their MA enrollment patterns may differ significantly from those who enroll fully in Medicare at age 65.
Use of the linked NHIS-Medicare data allowed us to examine the health characteristics of the overall population entering into Medicare, as opposed to the subpopulation of beneficiaries switching between MA and FFS. The benefits of the linked survey data included the ability to examine and control for various health and demographic characteristics that are not available from Medicare data alone. In addition, we were able to examine characteristics in the time-period before and after implementation of many MMA policies, which spurred substantial growth in MA. Importantly, the enrollment estimates and patterns over time observed with this linked data source were consistent with statistics using Medicare enrollment files (Kaiser Family Foundation, 2013). For example, our estimates compared to Kaiser’s are 12 and 13 percent, respectively, for 2005 and 23 percent from both sources for 2009 (Kaiser Family Foundation, 2013). Using our data source, we found that there still may be differences in the health characteristics of beneficiaries enrolling into MA even after recent improved risk adjustment of payment to MA plans. Researchers conducting analyses on claims data from Medicare FFS beneficiaries should be cognizant that their results may not be generalizable to the entire Medicare population and that differences between FFS and MA beneficiaries may not be constant over time.
Acknowledgments
The authors would like to acknowledge Dr. Frederic Selck for his valuable comments and feedback on this manuscript. This analysis included use of the Integrated Health Interview Series (http://www.ihis.us), provided by the Minnesota Population Center and State Health Access Data Assistance Center.
The authors have no conflicts of interest or financial support to report.
Footnotes
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the National Center for Health Statistics, Centers for Disease Control and Prevention.
References
- Brown J, Duggan M, Kuziemko I, Woolston W: How does risk selection respond to risk adjustment? Evidence from the Medicare Advantage program. NBER Working Paper No. 16977 National Bureau of Economic Research, 2011. [DOI] [PubMed] [Google Scholar]
- CDC National Center for Health Statistics (NCHS): 2005 NHIS Survey Description. Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2005/srvydesc.pdf Accessed December 13, 2013.
- CDC: Match Rate Table for NCHS-CMS Medicare Linked Data. Retrieved from http://www.cdc.gov/nchs/data/datalinkage/cms_medicare_match_rate_table_final.pdf Accessed 01/23/14, 2014.
- Cooper AL, Trivedi AN: Fitness memberships and favorable selection in Medicare Advantage plans. New England Journal of Medicine 2012; 366:150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald LM, Levy JM, Ingber MJ: Favorable selection in the Medicare+Choice program: new evidence. Health Care Financing Review 2000; 21:127–34. [PMC free article] [PubMed] [Google Scholar]
- Judson DH, Parker JD, Larsen MD. Adjusting sample weights for linkage-eligibility using SUDAAN. National Center for Health Statistics, Hyattsville Maryland. May 2013. Available at: http://www.cdc.gov/nchs/data/datalinkage/adjusting_sample_weights_for_linkage_eligibility_using_sudaan.pdf [Google Scholar]
- Kaiser Family Foundation: Medicare Advantage Fact Sheet. http://kff.org/medicare/fact-sheet/medicare-advantage-fact-sheet/ Accessed 12/13/13, 2013.
- McGuire TG, Newhouse JP, Sinaiko AD: An economic history of Medicare part C. Milbank Quarterly 2011; 89:289–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams JM, Hsu J, Newhouse JP: New Risk-Adjustment System Was Associated With Reduced Favorable Selection In Medicare Advantage. Health Affairs 2012; 31:2630–2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MedPAC: Report to Congress: Medicare in Rural America. Medicare Payment Advisory Commission, 2001. [Google Scholar]
- Mello MM, Stearns SC, Norton EC, Ricketss TC 3rd: Understanding biased selection in Medicare HMOs. Health Services Research 2003; 38:961–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan RO, Virnig BA, DeVito CA, Persily NA: The Medicare-HMO revolving door--the healthy go in and the sick go out. New England Journal of Medicine 1997; 337:169–75. [DOI] [PubMed] [Google Scholar]
- Morrisey MA, Kilgore M, Becker DJ, Smith W, Delzell E: Favorable Selection, Risk Adjustment and the Medicare Advantage Program. 2010. Health Services Research 2013; 48:1039–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murgolo MS: Comparison of Medicare risk HMO and FFS enrollees. Health Care Financing Review 2002; 24:177–85. [PMC free article] [PubMed] [Google Scholar]
- Newhouse JP, Price M, Huang J, McWilliams JM, Hsu J: Steps To Reduce Favorable Risk Selection In Medicare Advantage Largely Succeeded, Boding Well For Health Insurance Exchanges. Health Affairs 2012; 31:2618–2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley G, Tudor C, Chiang YP, Ingber M: Health status of Medicare enrollees in HMOs and fee-for-service in 1994. Health Care Financing Review 1996; 17:65–76. [PMC free article] [PubMed] [Google Scholar]
- Riley GF: Impact of Continued Biased Disenrollment from the Medicare Advantage Program to Fee-for-Service. Medicare & Medicaid Research Review. Vol. 2 Centers for Medicare and Medicaid Services, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AK, Beauregard KM, Vistnes JP: Who belongs to HMOs: a comparison of fee-for-service versus HMO enrollees. Medical Care Research and Review 1995; 52:389–408. [DOI] [PubMed] [Google Scholar]
- Virnig BA, Morgan RO, DeVito CA, Persily NA: Medicare HMOs: who joins and who leaves? American Journal of Managed Care 1998; 4:511–8. [PubMed] [Google Scholar]


