Abstract
Fungal diseases impose an escalating burden on public health in Africa, exacerbated by issues such as delayed diagnosis, inadequate therapy, and limited access to healthcare resources, resulting in significant morbidity and mortality. Effectively tackling these challenges demands a comprehensive approach encompassing research, training, and advocacy initiatives. Recent clinical mycology surveys conducted by Global Action for Fungal Infection (GAFFI) and the European Confederation of Medical Mycology/International Society for Human and Animal Mycology (ECMM/ISHAM) have underscored gaps in fungal diagnostics and the availability and accessibility of antifungal therapy in Africa. The World Health Organization (WHO) Fungal Priority Pathogens List (FPPL) identifies fungi of critical or high importance to human health, providing a roadmap for action and highlighting the urgent need for prioritizing fungal diseases and developing targeted interventions within the African context. To enhance diagnosis and treatment, it is imperative to invest in comprehensive training programs for healthcare workers across all levels and disciplines. Equipping them with the necessary knowledge and skills will facilitate early detection, accurate diagnosis, and appropriate management of fungal infections. Moreover, implementation science research in medical mycology assumes a pivotal role in bridging the gap between knowledge and practice. By identifying the barriers and facilitators that influence the adoption of diagnostic techniques and public health interventions, tailored strategies can be formulated to improve their implementation within healthcare settings. Advocacy plays a critical role in raising awareness regarding the profound impact of fungal diseases on public health in Africa. Engaging policy-makers, healthcare providers, researchers, industry experts and communities underscore the importance of addressing these diseases and galvanize efforts for change. Substantial investment in surveillance, research and development specifically focused on fungal diseases is indispensable for advancing our understanding of local epidemiology, developing effective interventions, and ultimately improving patient outcomes. In conclusion, closing the gaps in diagnosing and treating fungal diseases in Africa demands concerted research and advocacy initiatives to ensure better healthcare delivery, reduced mortality rates, and improved public health outcomes.
Keywords: Fungal infections, Antifungals, Diagnostics, Africa
Introduction
Fungal diseases are a significant threat to human health globally accounting for an estimated 1.7 to 2 million deaths annually [1]. Although commonly encountered in immunocompromised individuals [2,3], serious fungal diseases also occur in immunocompetent people, usually following occupational or environmental exposure, traumatic inoculation, or migration to an endemic region [4,5]. Invasive fungal diseases are associated with high mortality rates, especially when the diagnosis is delayed or not made at all [3,6]. This is of huge concern, particularly in Africa where the awareness of fungal diseases amongst healthcare workers is still evolving and diagnosis is often made at the terminal stage of the disease and sometimes post-mortem [3,6]. While HIV is a major cause of death linked to invasive fungal infections, these diseases are still misdiagnosed as other clinical entities, particularly presumptive tuberculosis and malignancies [7,8].
The gaps in diagnosis and effective treatment for fungal diseases often result in increased morbidity and mortality [3]. Although there have been many efforts to improve case finding and diagnostics, recent observational studies highlight the need for more surveillance and the need to prioritize research in mycology [9]. This is further affirmed by a recent survey on the diagnostic capacity of fungal infections in African countries which revealed the enormous challenges faced in the diagnosis of HIV-associated fungal infections in the continent [10]. Our review provides recommendations to further mycology research and improved the diagnosis of fungal diseases in Africa.
Common fungal infections in Africa
Cryptococcosis, histoplasmosis, aspergillosis, candidiasis, mucormycosis, Pneumocystis pneumonia, eumycetoma, sporotrichosis, and chromoblastomycosis are the fungal diseases reported in the literature as being common in Africa [9].
One large-scale review (1952 − 2017) documented 470 cases of histoplasmosis; HIV-infected patients accounted for 38 % (178) of the cases [11]. West Africa had the highest number of cases (179); the majority (162 cases) were caused by Histoplasma capsulatum var. duboisii (Hcd) while the Southern African region reported 150 cases, the majority (119) caused by Histoplasma capsulatum var. capsulatum (Hcc). No case of histoplasmosis was reported from 20 African countries, likely missed [11]. Another review (1950−2021) focused on the global epidemiology of histoplasmosis caused by Hcd, and identified 359 cases from Africa, with the highest number of cases (117) reported from Nigeria [12]. Three recent studies from Nigeria (2022), Ghana (2022) and Cameroon (2021), identified 76, 5 and 26 cases of disseminated histoplasmosis, respectively in people living with HIV/AIDS [13,14,15] and another focused on presumptive tuberculosis patients in Nigeria identified 27 cases [5].
Aspergillosis is widely reported in Africa. A review (1976 to 2021) of chronic pulmonary aspergillosis (CPA) identified 41 studies, with a total of 1247 CPA cases from 14 African countries. Most cases came from Morocco (n = 764, 62.3 %), followed by South Africa (n = 122, 9.9 %), and Senegal (n = 99, 8.1 %). The studies were retrospective cohorts (n = 17, 41.5 %), prospective cohorts (n = 5, 12.2 %), case series (n = 5, 12.2 %), cross-sectional (n = 2, 4.9 %), and case reports (12, 29.3 %) [8]. A recent study from Ghana identified 15 cases of CPA in patients with presumed tuberculosis [16]. With regards to invasive aspergillosis, six case reports, one retrospective study and four prospective cohort studies amounting to a total of 88 cases were reported from Africa [9], likely a gross underestimate.
Cryptococcosis is a major cause of morbidity and mortality, especially in people living with HIV in Africa, with mortality rate as high as 15−20 % among those with advanced HIV disease [17]. There was a major parallel increase in the incidence of cryptococcosis in Africa as HIV incidence increased, with some decline since improved ART coverage, but now many breakthroughs on ART. 40,948 cases have been reported between 1969 − 2021, out of which 97.8 % (40,053) were reported between 2000 − 2021 [18]. In addition, a recently published multicentre study conducted in 2018 identified 44 cases of asymptomatic cryptococcal antigenemia among patients with advanced HIV disease in Nigeria [19]. Recent data modeling the global burden of HIV-associated cryptococcal infection in adults estimated 152, 000 cases of cryptococcal meningitis and 112 000 cryptococcal-related deaths, of which 82,000 and 71,000 were from Africa in 2020, respectively [20].
The burden of invasive candidiasis in Africa as documented in a multi-year review (1976−2021) was 18,293 cases with the highest number 15,002 (82 %) reported from South Africa. 91 % (16 636) were cases of candidaemia. HIV infection is linked to a higher mortality in patients with invasive candidiasis - in Africa, HIV co-infection was seen in 1052 (5.8 %) cases. Candida albicans was the most frequently isolated species in 6328 (32.6 %), followed by C. parapsilosis 5910 (30.4 %), and C. auris 1505 (7.8 %) [21]. Two recent reports from South Africa documented 45 cases of C. auris candidaemia [22], while another documented 610 cases of candidaemia caused by 618 isolates including C. albicans (196/618, 31.72 %), C. parapsilosis (193/618, 31.23 %), C. auris (82/618, 13.27 %), Nakaseomyces (Candida) glabrata (72/618, 11.65 %), Pichia kudriavzevii (C. krusei) (21/618, 3.40 %) and unidentified Candida species (54/618, 8.74 %) [23].
Mucormycosis is predominantly reported in North Africa and rarely reported in the rest of the African region [24]. A review (1960−2022) identified a total of 408 individual cases from 12 African countries; 330 (80.9 %) from North Africa, 63 (15.4 %) from Southern Africa, seven (1.7 %) from East Africa, seven (1.7 %) from West Africa and a single case (0.2 %) from Central Africa. Rhino-orbital-cerebral (n = 307, 75.2 %) and gastrointestinal (n = 51, 12.5 %) mucormycosis were the most frequently described clinical forms. The commonest underlying risk factors were diabetes mellitus (n = 203, 49.8 %), COVID-19 (n = 101, 24.8 %), malignancies (n = 65, 15.9 %) and neutropenia, usually with leukaemia (n = 53, 13.0 %). Fungal etiology was identified in 38 (9.3 %), of which the commonest was Rhizopus arrhizus (27/38, 71.1 %) [24].
The burden of Pneumocystis pneumonia (PCP) among people living with HIV in Africa has been described in two systematic reviews. According to a meta-analysis of hospital-based studies across 18 countries in sub-Saharan Africa, the overall prevalence of PCP was 15.4 %. However, it was notably higher among specific groups, such as individuals with respiratory symptoms (18.8 %), hospitalized patients (22.4 %), and hospitalized patients with respiratory symptoms (24 %) [25]. In a more recent meta-analysis that included studies from 15 African countries, the overall prevalence of laboratory-confirmed Pneumocystis jirovecii infection stood at 19 % among adult PLWH experiencing respiratory symptoms. This prevalence ranged from 15 % in studies using microscopy to 22 % in studies employing PCR for detection. Interestingly, the prevalence of laboratory-confirmed P. jirovecii infection has remained relatively consistent both in the pre-antiretroviral therapy (ART) era (1995−2005) at 21 % and in the ART era (2006−2020) at 18 % [26]. Furthermore, the case fatality rate associated with PCP among PLWH has been estimated to be 18.8 % [27].
The World Health Organization (WHO) lists three deep cutaneous fungal infections- mycetoma, chromoblastomycosis and sporotrichosis- as Neglected Tropical Diseases. Mycetoma was the first so listed, attributable to the high burden in Sudan and along the mycetoma belt. Mycetoma cases have been reported from over 50 % of African countries, with highest numbers in Sudan, Senegal, and several other countries across the Sahel [28–31].
Chromoblastomycosis data in Africa mainly comprises case reports and series with most of the cases reported in Madagascar [32]. An evaluation of the global burden of chromoblastomycosis from 1947 to 2018, identified 1875 cases from 22 countries [9,32]; Madagascar (1323 cases), South Africa (156 cases), Republic of the Congo and Democratic Republic of the Congo (121 cases), Gabon (64 cases), Zimbabwe (35 cases), Uganda (34 cases), Kenya (33 cases), Cameroon (23 cases), Morocco (18 cases), Tanzania (17 cases), Ethiopia (14 cases), Angola (7 cases), Nigeria (5 cases), Tunisia (5 cases), Reunion Island (5 cases), Libya (4 cases), Comoro Island (4 cases), Sierra Leone (3 cases), Senegal (2 cases), Botswana (1 case) and Djibouti (1 case) [9,32]. Chromoblastomycosis is mainly caused by Fonsecaea pedrosoi, F. monophora, Cladophialophora carrionii, Rhinocladiella aquaspersa, Phialophora species, and Exophiala species [33].
Sporotrichosis is less commonly documented in Africa with sporadic cases, except for Madagascar and South Africa which appear to have many authochonous cases [34,35]. This could reflect genuine rarity (which is likely for many countries such as Uganda [36]) or a lack of diagnostic capacity, notably lack of fungal culture and histopathologists often not using fungal stains for examination of skin biopsies.
Fungal diseases “Missing in action”
There appears to be a lack of data and uncertainty regarding the existence of some fungal diseases in Africa. Several of them including pulmonary cryptococcosis [7,37], chronic invasive Aspergillus rhinosinusitis [38], subacute invasive aspergillosis [39], and Candida peritonitis (intraabdominal candidiasis) [40], fungal keratitis [41] have few a few reported cases in the whole world and others such as allergic fungal rhinosinusitis, allergic bronchopulmonary aspergillosis (ABPA), fungal tracheobronchitis and disseminated trichosporonosis have no reported cases at all in the region [9]. In addition, there are fungal diseases with limited data available, such as conidiobolomycosis, basidiobolomycosis [42,43], blastomycosis [9,44], emergomycosis [9], white piedra (last report from Gabon in 1994) [45], hepatosplenic candidiasis in leukemia (only a small series from Cairo, Egypt) [46], and neonatal candidiasis (reported in South Africa and Nigeria) [9,47]. Furthermore, data on vulvovaginal candidiasis (VVC), and recurrent VVC in particular with regards to emerging antifungal resistance is not well described in Africa.
Diagnostic techniques for fungal diseases in Africa
Methods of diagnosis of common fungal diseases in Africa
Fungal diseases cause substantial morbidity and mortality exacerbated by the weak health systems in Africa [2,3]. The World Health Organization (WHO) recently published the fungal priority pathogens list to guide research, development, and public health action [48]. The list is divided into three sub-groups as shown in the Table 1 below: with most of the common fungal pathogens in Africa rated as critical and high priority.
Table 1.
WHO Priority Fungal pathogen list.
| Group | Fungal pathogens of particular concern in Africa |
|---|---|
| Critical priority | Cryptococcus neoformans*, Candida auris*, Aspergillus fumigatus*, Candida albicans* |
| High priority | Nakaseomyces glabrata (Candida glabrata), Histoplasma species*, Fusarium species, Candida parapsilosis, Eumycetoma causative agents*, Mucorales*, Candida tropicalis |
| Medium priority | Scedosporium species, Pichia kudriavzeveii (Candida krusei), Cryptococcus gattii, Pneumocystis jirovecii, |
Important cause of fungal diseases in Africa.
Laboratory diagnosis of fungal infections mostly relies on a combination of different tests including microscopy, culture, blood culture, serology, antigen tests, molecular tests, and histopathology [49]. Imaging, including x-rays, ultrasound, magnetic resonance imaging (MRI), and computerized tomography (CT) scan, is also important and is most useful to diagnose invasive and chronic fungal diseases. It is not reliable in the diagnosis of allergic fungal disease except for some forms of ABPA. Imaging may show the level of tissue invasion and dissemination.
Access and availability of diagnostics across Africa
Laboratory diagnosis of fungal infections is challenging and tedious, especially in resource-limited settings like Africa where both opportunistic and endemic mycoses overlap with several other bacterial, viral, and parasitic infections. Fewer than 10 African countries have national surveillance programs for fungal infections, and fewer than 5 have reference diagnostic mycology laboratories 50]. Many of the diagnostic tests were developed for high-income countries according to their regulatory guidance and market opportunity and are not readily available in Africa. Radiological diagnosis is similarly challenging. MRI and CT scans are very expensive. X-rays are relatively affordable but not available in many lower (primary) health centres. Most of the costs of diagnosis are incurred by the patients.
A recent survey done in 50 African countries showed that in the public sector, chest X-ray and CT scans were performed in 98 % and in 74 % of countries respectively, but less often in the private sector. Bronchoscopy and spirometry were done often in 56 % and occasionally in 36 % in the tertiary health facilities of public sector. The most conducted laboratory diagnostic assay was fungal culture (often or occasionally) in 58 % of African countries. This study found a huge disparity in diagnostic capability across the African continent [51].
The European Confederation of Medical Mycology (ECMM) and International Society for Human and Animal Mycology (ISHAM) also published a survey on the current state of clinical mycology in Africa. The survey revealed that only 12 % of institutions in Africa met the minimum laboratory requirements for ECMM Excellence centre blue status (the minimal requirements for the blue status are the identification of relevant yeasts and moulds, susceptibility testing on yeasts and moulds according to standard procedures, and the performance of antigen ELISA for Aspergillus (galactomannan) and cryptococcal antigen. Only 30 % of the institutions have access to susceptibility testing for both yeasts and moulds and Aspergillus antigen testing is mostly outsourced to private or national reference laboratories in 48 % of the institutions [50]. Recently, the UNITAID-Clinton Health Access Initiative (CHAI) advanced HIV diseases initiative has advanced access to liposomal amphotericin B and flucytosine to eight African countries (Botswana, Lesotho, Malawi, Nigeria, South Africa, Tanzania, Uganda, and Zimbabwe) to improve access to life-saving therapy for cryptococcal meningitis [51].
To address the lack of access to tests and testing services in multiple countries, WHO since 2018 published an essential diagnostics list (EDL), with a list of recommended in vitro diagnostics that should be available at point-of-care and in laboratories in all countries to increase timely and life-saving diagnoses. The fungal diagnostics included were microscopy, blood culture, other cultures and cryptococcal antigen test, urinary Histoplasma antigen, Aspergillus antibody, antigen, and Pneumocystis PCR [52]. These provided a good impetus for the inclusion of mycology services in African institutions where they were lacking. On May 2015, the Global Action for Fungal Infections (GAFFI) launched a 10-year ambitious target to enable 95 % of the world’s population to have access to fungal diagnostics and 95 % to have access to antifungal therapy by 2025 [53]. Table 2 below highlights the summary of the key diagnostics for lung fungal diseases that the target focuses on.
Table 2.
Ambitious ’95–95 by 2025′ targeted diagnostics for pulmonary mycoses.
| Disease type | Disorders | Key diagnostics |
|---|---|---|
| Chronic fungal disease | Chronic pulmonary aspergillosis | Fungal antibody, CXR, CT scan, microscopy, culture |
| Allergic fungal disease | Allergic bronchopulmonary aspergillosis, severe asthma with fungal sensitization | Total IgE, fungal IgE, skin allergy testing |
| Invasive fungal disease | Invasive aspergillosis, Pneumocystis pneumonia | Fungal antigen, PCR detection, CT scan, microscopy, culture, biopsy |
| Endemic fungal disease | Endemic mycoses | Fungal antibody, culture, biopsy |
Abbreviations: CXR= Chest x-ray; CT= Computed tomography; PCR= Polymerase chain reaction.
Limitations of current diagnostic techniques
Microscopy has a short turnaround time but has low sensitivity and needs high level of expertise to read. Fungal culture is considered the gold standard but has a long turnaround time and is less sensitive especially in allergic fungal disease. Most fungal pathogens grow slowly and may fail to grow in culture and expertise is needed for identification. Blood culture is limited to isolation of yeasts and some moulds such as Fusarium and Scedosporium species, Aspergillus species do not grow in blood culture. Furthermore, fungal culture is difficult in low-income countries due to a lack of maintenance and upkeep of the laboratories and their equipment so environmental contamination is common. Also access to commercial selective media is limited. Serology may not distinguish between active and past infection and may not be so useful in allergic and invasive disease. Antigen tests are quick but have issues with specificity. Molecular tests especially polymerase chain reaction (PCR) have a good sensitivity but are usually very expensive and not standardized or commercialized. In addition, PCR cannot distinguish between dead and dying cells, needs infrastructures, including electricity supply and well-trained personnel. Histopathology provides a presumptive diagnosis of invasive disease by demonstrating fungal elements in tissue but does not confirm the causative agent. However, histopathology is mainly available in reference centers and needs expertise. X-rays are less sensitive and not specific. Ultrasound has a limited utility in fungal infection diagnosis with less sensitivity. MRI and CT scans are rarely specific and usually expensive. Majority of these tests cannot be done in field conditions and have a long turnaround time. Besides the inherent limitations of the diagnostic methods, there is the challenge of acquiring appropriate clinical specimens. Blood cultures are rarely ordered, lumbar punctures are often not performed, bronchoscopy is generally unavailable and tissue biopsies are rarely performed in all settings where needed, leading to a reliance on non-invasive or poor-quality specimens. This calls for advocacy for point of care tests that fulfill REASSURED (real-time connectivity, ease of sample collection, affordable, sensitive, specific, user-friendly, robust, equipment-free and deliverable to end-users) criteria [54].
Opportunities for improved diagnostics
In the last decade, we have seen significant innovations in the diagnostics for cryptococcal antigen, Aspergillus antibody, Histoplasma urine antigen, and Pneumocystis PCR testing. Point-of-care (POC) tests are warranted to address the issue of delayed diagnosis. The diagnostic performance issues of some tests need to be addressed. With the high burden of risk factors such as HIV and pulmonary tuberculosis (PTB) in Africa, diagnostics for fungal infections can be incorporated into existing national programmes for TB and advanced HIV disease to screen routinely for potential opportunistic infections. There is also a need for sensitization to build local capacity in African institutions to increase the index of clinical suspicion for fungal diseases among doctors who make the laboratory requisitions. We can leverage and build on the existing laboratory capacity for HIV and TB research in African institutions to advance laboratory capacity for fungal infections. Therefore, education of clinicians, laboratory personnel as well as the public is key to raise awareness and early diagnosis and management of fungal diseases, Fig. 1.
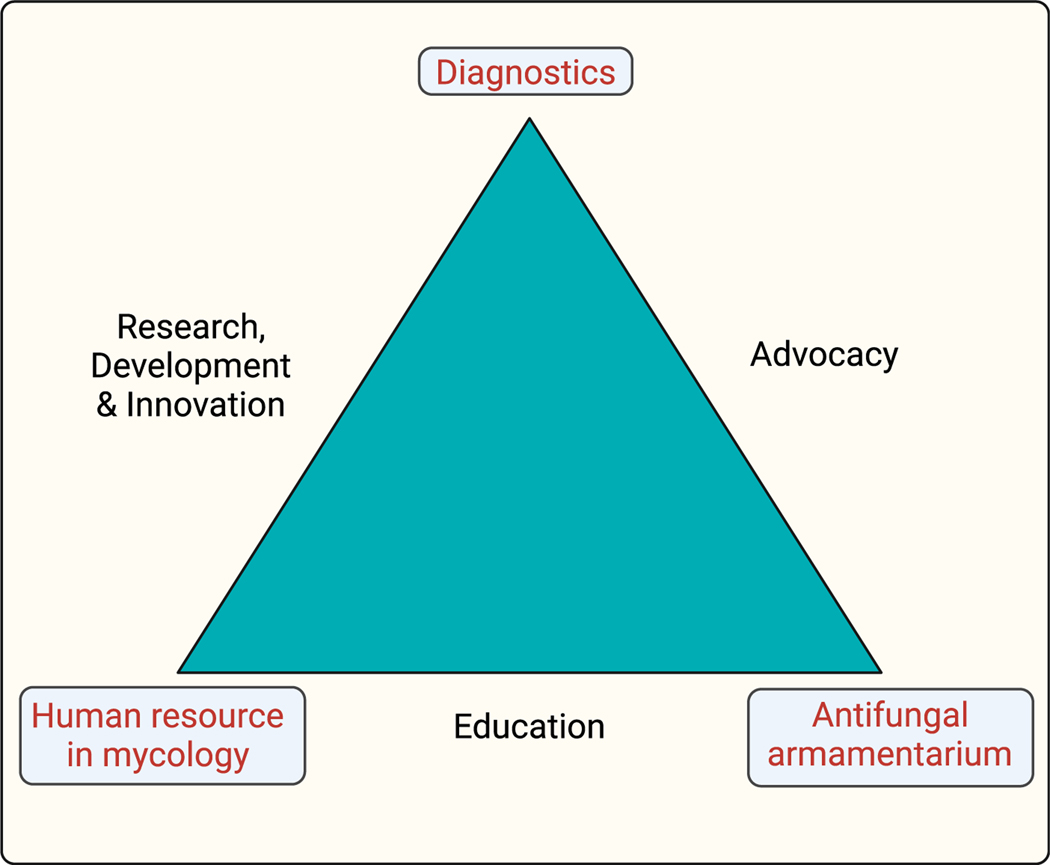
Fig. 1.
Towards a patient-centered care for fungal diseases in Africa: Much emphasis has been placed on the need for diagnostics, human resources (both clinical and laboratory) and affordable and accessible antifungals to improve patient outcomes when it comes to tackling fungal diseases. However, research, development and innovation, advocacy and education of the public can further compliment addressing the more obvious challenges. Furthermore, education of both the clinical and laboratory scientists as well as the public is key to allow early diagnosis, optimize antifungal therapy and improve clinical outcomes.
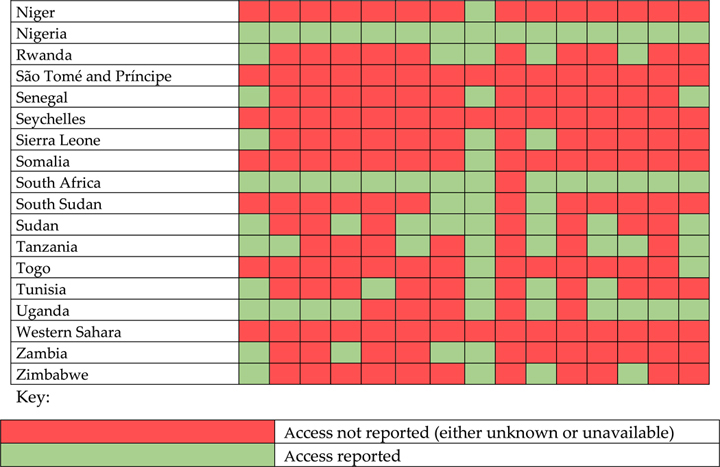
Availability and access to antifungals in Africa
Access to antifungals in Africa has been mapped by various organizations including GAFFI [55], in parallel with other world regions (Table 3). Amphotericin B is the drug of choice for a variety of mycoses, including the more common cryptococcosis [56,57], and mucormycosis [58]. On the other hand, fluconazole is still recommended for the treatment of susceptible candidemia/invasive candidiasis, and consolidation and maintenance phases of cryptococcal meningitis treatment [57]. Echinocandins (micafungin, caspofungin and anidulafungin) were listed as Essential by the WHO in 2019, and have utility for life-threatening Candida infections, especially due to C. auris.
Table 3.

|
|
Overall, fluconazole is considered the most widely used antifungal drug on the continent and is already available in 84 % of countries. Additionally, 55 % of countries reported the availability of at least one formulation of amphotericin B, the most common being deoxycholate rather than the recommended liposomal. Itraconazole is the most common mold-active triazole, reported in 46 % of countries for the treatment of endemic mycoses currently found in Africa (i.e., blastomycosis, emergomycosis, histoplasmosis, and sporotrichosis) [56]. Additionally, amphotericin B is the drug of choice for a variety of mycoses, including the more common cryptococcosis [57], and mucormycosis [58]. On the other hand, fluconazole is still recommended for the treatment of susceptible candidemia/invasive candidiasis, and consolidation and maintenance phases of cryptococcal meningitis treatment [59,60].
Access to other newer systemic antifungal agents such as echinocandins (available in 30 % of countries) and other triazoles (available in 30 % for voriconazole, 5 % for isavuconazole and 5 % for posaconazole) is more limited. This situation severely compromises the ability to treat emerging fungal infections such as mucormycosis [58], trichosporonosis [61], or fluconazole-resistant candidemia/candidiasis [59]. In addition, is the limited availability of the agents of choice for invasive aspergillosis, isavuconazole or voriconazole, which jeopardizes adequate treatment [54]. Moreover, adequate treatment of other mycoses, such as scedosporiosis/lomentosporiosis [61], or cryptococcosis [60] for which terbinafine and flucytosine, with access in 30 % and the 29 % of the countries, respectively, are recommended antifungals is also not guaranteed.
The limitations mentioned above exist despite the inclusion of some of these antifungals, namely amphotericin B, fluconazole, flucytosine, itraconazole, micafungin, and voriconazole in the WHO list of essential medicines [62]. In parallel, Africa does not have immediate and wide access to the antifungals required to combat any of the pathogens mentioned in the WHO list of critical priority (A. fumigatus, C. neoformans, C. auris, and C. albicans). A similar situation applies to pathogens in the high and medium priority lists, such as other Candida spp. [59], eumycetoma-causing agents, Fusarium spp., Histoplasma spp [56], Mucorales or Scedosporium/Lomentospora spp. [63].
The highlighted challenges endanger the fulfillment of the 2015 GAFFI 95−95 initiative for 2025 [54], which aims to provide access to antifungal therapy to 95 % of the world’s population by 2025. Further-more, it is necessary to remember that local access to a particular antifungal drug does not necessarily ensure the eventual administration of such drug to the patient. This is because many patients are unable to afford full treatment courses of systemic antifungals. Opportunities for improvement lie in building laboratory capacity for susceptibility testing and therapeutic drug monitoring, promoting access to affordable generic drugs, raising awareness about local antifungal availability, emphasizing treatment adherence, promoting antifungal stewardship, and managing drug interactions and adverse effects (Table 4).
Table 4.
Challenges to Treatment and opportunities for optimizing antifungal treatment.
| Challenges | Opportunities for improvement |
|---|---|
| Lack of diagnostic capacity and late diagnosis [50] | Diagnostic capacity building for early diagnosis [50] |
| Affordable prices[50,66] | Access to generic drugs[67,68] |
| Local antifungal availability under normal circumstances and if stock-outs [50,65] | - Raising awareness [50] |
| Treatment adherence to comorbidity treatments (i.e., HIV/AIDS) [69,70] Antifungal resistances: acquired and intrinsic [50] |
- Enhanced Access to therapeutic drug monitoring to address drug-drug interactions |
| Antifungal susceptibility testing | - Antifungal stewardship to address emerging antifungal resistance |
| Drug-drug interactions and drug-related adverse effects (use ART and anti-TBs [50,71] |
Abbreviations: ART-anti-retroviral therapy, TB, tuberculosis.
Conclusions
In conclusion, fungal diseases exert a significant burden on public health systems in Africa, necessitating a comprehensive approach involving research, training, and advocacy. The effect on metrics such as quality adjusted- and disability adjusted life years needs to be quantified to determine the full economic impact in Africa as part of advocacy for increased investment on prevention and treatment of fungal diseases. The WHO FPPL serves as a guide for urgent action, emphasizing the need to prioritize fungal diseases and develop targeted interventions. Likewise, the WHO essential medicines list and essential diagnostics list arm us with tools for advocacy. Implementation science research in medical mycology can play a significant role in bridging the gap between knowledge and practice. By identifying barriers and facilitators to the adoption of diagnostics and public health interventions, tailored strategies can be developed for improved implementation. This review emphasizes the importance of context-specific approaches, considering local epidemiology, antifungal resistance patterns, and the development of affordable and accessible diagnostic tools and treatment options.
Acknowledgment
Dr Felix Bongomin is a PhD student at the University of Manchester, United Kingdom. His work is supported by the Carigest SA Conny Naeva Charitable Foundation as part of the “Chronic Pulmonary Aspergillosis: Optimization of Therapy, Immunogenetic Screening, and Diagnosis in Uganda [CPA_OPTIONS_Uganda]” project. CARIGEST SA did not play any role in the design, implementation, and analysis of the study.
This work was presented in part at the 1st Pan-African Mycology Working Group Conference, Nairobi, Kenya by Dr. Felix Bongomin.
Funding
Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under Award Number D43 TW010543. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures
The authors declare that they have no conflict of interest.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- [1].Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med 2012;4(165) 165rv13-. [DOI] [PubMed] [Google Scholar]
- [2].Okoye CA, Nweze E, Ibe C. Invasive candidiasis in Africa, what is the current picture? Pathog Dis 2022;80(1) ftac012. [DOI] [PubMed] [Google Scholar]
- [3].Mandengue CE, Ekeng BE, Oladele RO. Disseminated Histoplasmosis; A threat in advanced HIV Disease population in sub-Saharan Africa? J Adv Med Med Res 2021;33(3):115–44. [Google Scholar]
- [4].Akaihe CL, Nweze EI. Epidemiology of Cryptococcus and cryptococcosis in Western Africa. Mycoses 2021;64(1):4–17 Jan. [DOI] [PubMed] [Google Scholar]
- [5].Ekeng BE, Oladele RO, Emanghe UE, Ochang EA, Tatfeng YM. Prevalence of Histoplasmosis and Molecular characterisation of Histoplasma species in patients with presumptive pulmonary tuberculosis in Calabar. Nigeria. OFID. 2022:ofac368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yerbanga IW, Nakanabo Diallo S, Rouamba T, Denis O, Rodriguez-Villalobos H, Montesinos I, et al. A systematic review of epidemiology, risk factors, diagnosis, antifungal resistance, and management of invasive aspergillosis in Africa. J Mycol Med 2023;33(1):101328. [DOI] [PubMed] [Google Scholar]
- [7].Echieh C, Nwagboso C, Ogbudu S, Eze J, Ochang E, Jibrin P, Etiuma A, Bassey O. Invasive pulmonary cryptococcal infection masquerading as lung cancer with brain metastases: a case report. J West Afr Coll Surg 2020;10(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Olum R, Osaigbovo II, Baluku JB, Stemler J, Kwizera R, Bongomin F. Mapping of chronic pulmonary aspergillosis in Africa. J Fungi 2021;7:790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bongomin F, Ekeng BE, Kibone W, Nsenga L, Olum R, Itam-Eyo A, Kuate MPN, Pebolo FP, Davies AA, Manga M, Ocansey B, Kwizera R, Baluku JB. Invasive fungal diseases in Africa: a critical literature review. J Fungi 2022;8:1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lakoh S, Kamudumuli PS, Penney ROS, Haumba SM, Jarvis JN, Hassan AJ, et al. Diagnostic capacity for invasive fungal infections in advanced HIV disease in Africa: a continent-wide survey. Lancet Infect Dis 2022. S1473–3099(22)00656–9. [DOI] [PubMed] [Google Scholar]
- [11].Oladele RO, Ayanlowo OO, Richardson MD, Denning DW. Histoplasmosis in Africa: an emerging or a neglected disease? PLoS Negl Trop Dis 2018;12: e0006046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ekeng BE, Davies AA, Ocansey BK, Stone NRH, Oladele RO. Histoplasma capsulatum var duboisii infection: a global review, 1950–2021. MID 2022. [Google Scholar]
- [13].Oladele RO, Osaigbovo II, Alani Akanmu, Adekanmbi OA, Ekeng BE, Yahayah M. Prevalence of histoplasmosis among persons with advanced HIV disease. Nigeria: EID; 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ocansey BK, Otoo B, Asamoah I, Ganu V, Berko KP, Oladele O, Amankwa EA, Opoku-Asare B, Agyei M, George L, et al. Cryptococcal and histoplasma antigen screening among people with human immunodeficiency virus in ghana and comparative analysis of OIDx histoplasma lateral flow assay and IMMY histoplasma enzyme immunoassay. Open Forum Infect Dis 2022;9:ofac277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kuate MPN, Nyasa R, Mandengue C, Tendongfor N, Bongomin F, Denning DW. Screening for acute disseminated histoplasmosis in HIV disease using urinary antigen detection enzyme immunoassay: a pilot study in Cameroon. J Microbiol Methods 2021;185:106226. [DOI] [PubMed] [Google Scholar]
- [16].Ocansey BK, Otoo B, Adjei A, Gbadamosi H, Kotey FCN, Kosmidis C, Afriyie-Mensah JS, Denning DW, Opintan JA. Chronic pulmonary aspergillosis is common among patients with presumed tuberculosis relapse in Ghana. Med Mycol 2022;60(9) myac063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ibe C, Okoye CA. Integrated healthcare approach can curb the increasing cases of cryptococcosis in Africa. PLoS Negl Trop Dis 2022;16(8):e0010625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ibe C, Okoye CA, Nweze E, Out A. Cryptococcosis in Africa: what the data tell us. Med Mycol 2023;61(6) myad049. [DOI] [PubMed] [Google Scholar]
- [19].Oladele RO, Jordan AM, Okaa JU, Osaigbovo II, Shettima SA, Shehu NY, et al. A multicenter survey of asymptomatic cryptococcal antigenemia among patients with advanced HIV disease in Nigeria. PLOS Glob Public Health 2023;3(1):e0001313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis 2017;17(8):873–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Okoye CA, Nweze E, Ibe C. Invasive candidiasis in Africa, what is the current picture? Patho and Dis 2022;80 ftac012. [DOI] [PubMed] [Google Scholar]
- [22].Parak A, Stacey SL, Chibabhai V. Clinical and laboratory features of patients with Candida auris cultures, compared to other Candida, at a South African Hospital. J Infect Dev Ctries 2022;16:213–21. [DOI] [PubMed] [Google Scholar]
- [23].Chibabhai V. Incidence of candidemia and prevalence of azole-resistant candidemia at a tertiary South African hospital—a retrospective laboratory analysis 2016–2020. South Afr. J Infect Dis 2022;37:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Osaigbovo II, Ekeng BE, Davies AA, Oladele RO. Mucormycosis in Africa: epidemiology, diagnosis and treatment outcomes. Mycoses 2023;00:1–8. [DOI] [PubMed] [Google Scholar]
- [25].Wasserman S, Engel ME, Griesel R, Mendelson M. Burden of pneumocystis pneumonia in HIV-infected adults in sub-Saharan Africa: a systematic review and meta-analysis. BMC Infect Dis 2016;16:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wills NK, Lawrence DS, Botsile E, Tenforde MW, Jarvis JN. The prevalence of laboratory-confirmed Pneumocystis jirovecii in HIV-infected adults in Africa: a systematic review and meta-analysis. Med Mycol 2021;59:802–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wasserman S, Engel ME, Griesel R, Mendelson M. Burden of pneumocystis pneumonia in HIV-infected adults in sub-Saharan Africa: a systematic review and meta-analysis. BMC Infect Dis 2016;16:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Emery D, Denning DW. The global distribution of actinomycetoma and eumycetoma. PLoS Negl Trop Dis 2020. Sep 24;14(9):e0008397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Oladele RO, Ly F, Sow D, Akinkugbe AO, Ocansey BK, Fahal AH, van de Sande WW. Mycetoma in West Africa. Trans R Soc Trop Med Hyg 2021;115(4):328–36 Apr. [DOI] [PubMed] [Google Scholar]
- [30].Badiane AS, Ndiaye M, Diongue K, Diallo MA, Seck MC, Ndiaye D. Geographical distribution of mycetoma cases in senegal over a period of 18 years. Mycoses 2020;63(3):250–6 Mar. [DOI] [PubMed] [Google Scholar]
- [31].Hassan R, Cano J, Fronterre C, Bakhiet S, Fahal A, Deribe K, Newport M. Estimating the burden of mycetoma in Sudan for the period 1991−2018 using a model-based geostatistical approach. PLoS Negl Trop Dis 2022;16(10):e0010795 Oct 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Santos DWCL, de Azevedo CdMPeS Vicente VA, Queiroz-Telles F, Rodrigues AM, de Hoog GS, et al. The global burden of chromoblastomycosis. PLoS Negl Trop Dis 2021;15(8):e0009611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Queiroz-Telles F, de Hoog S, Santos DW, Salgado CG, Vicente VA, Bonifaz A, et al. Chromoblastomycosis. Clin Microbiol Rev 2017;30(1):233–76 Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rasamoelina T, Maubon D, Raharolahy O, Razanakoto H, Rakotozandrindrainy N, Rakotomalala FA, Bailly S, Sendrasoa F, Ranaivo I, Andrianarison M, Rakotonirina B. Sporotrichosis in the highlands of Madagascar, 2013−2017. Emerging Infect Dis 2019;25(10):1893. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mapengo RE, Maphanga TG, Grayson W, Govender NP. Endemic mycoses in South Africa, 2010−2020: a decade-long description of laboratory-diagnosed cases and prospects for the future. PLoS Negl Trop Dis 2022;16(9):e0010737 Sep 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kwizera R, Bongomin F, Lukande R. Deep fungal infections diagnosed by histology in Uganda: a 70-year retrospective study. Med Mycol 2020;58(8):1044–52 Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Nakatudde I, Kasirye P, Kiguli S, Musoke P. It is not always Tuberculosis! A case of pulmonary cryptococcosis in an immunocompetent child in Uganda. Afr Health Sci 2021;21:990–4. doi: 10.4314/ahs.v21i3.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Awolola NA, Oladele RO, Akinde OR, Bamigboye BA, Oguntunde OA. Chronic invasive fungal granulomatous rhino-sinusitis: a case report with review of literature. Nigerian Medical Practitioner 2017;72(1−2):16–7 Jan 8. [Google Scholar]
- [39].Ekeng BE, Akpu BB, Ahaneku CA, Udoh UA, Ita OI, Elem DE, et al. Subacute invasive pulmonary aspergillosis misdiagnosed as tuberculosis in a Nigerian man: a case report: subacute invasive pulmonary aspergillosis in a Nigerian man. Indian J Case Rep 2022;8(11):369–72. [Google Scholar]
- [40].Ali AM, Mohamed AN, Mohamed YG, Keleşoğlu SIİ. Clinical presentation and surgical management of perforated peptic ulcer in a tertiary hospital in Mogadishu, Somalia: a 5-year retrospective study. World J Emerg Surg 2022;17(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Brown L, Leck AK, Gichangi M, Burton MJ, Denning DW. The global incidence and diagnosis of fungal keratitis. Lancet Infect Dis 2021;21(3):e49–57 Mar 1. [DOI] [PubMed] [Google Scholar]
- [42].Darré T, Saka B, Mouhari-Toure A, Djiwa T, Pitché P, Napo-Koura G. Basidiobolo-mycosis in Togo: clinicopathological study of a series of 12 presumed cases. BMC Res Notes 2018;11(1):667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Atadokpédé F, Gnossikè J, Adégbidi H, Dégboé B, Sissinto-Savi de Tovè Y, Adéyé A, et al. Cutaneous basidiobolomycosis: seven cases in southern Benin. Ann Dermatol Venereol 2017;144(4):250–4. [DOI] [PubMed] [Google Scholar]
- [44].Maphanga TG, Birkhead M, Muñoz JF, Allam M, Zulu TG, Cuomo CA, Schwartz IS, Ismail A, Naicker SD, Mpembe RS, Corcoran C. Human blastomycosis in South Africa caused by Blastomyces percursus and Blastomyces emzantsi sp. nov., 1967 to 2014. J Clin Microbiol 2020;58(3) Feb 24e01661–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Therizol-Ferly M, Kombila M, de Diaz MG, Duong TH, Richard-Lenoble D. White piedra and Trichosporon species in equatorial Africa. I. History and clinical aspects: an analysis of 449 superficial inguinal specimens: weiβe Piedra und Tri-chosporon-Arten in Äquatorialafrika. I. Klinische Aspekte: eine Analyse von 449 oberflächlichen Untersuchungsproben der Inguinalregion. Mycoses 1994;37(7−8):249–53. [DOI] [PubMed] [Google Scholar]
- [46].Madney Y, Shalaby L, Elanany M, Adel N, Nasr E, Alsheshtawi K, et al. Clinical features and outcome of hepatosplenic fungal infections in children with haematological malignancies. Mycoses 2020;63(1):30–7. [DOI] [PubMed] [Google Scholar]
- [47].Ezenwa BN, Oladele RO, Akintan PE, Fajolu IB, Oshun PO, Oduyebo OO, et al. Invasive candidiasis in a neonatal intensive care unit in Lagos, Nigeria. Niger Postgrad Med J 2017;24(3):150–4 Jul-Sep doi: 10.4103/npmj.npmj_104_17. [DOI] [PubMed] [Google Scholar]
- [48].WHO. fungal priority pathogens list to guide research, development and public health action. Geneva: World Health Organization; 2022. [Google Scholar]
- [49].Sharma G, Saxena S, Singh P, Singh SK. Laboratory diagnosis of fungal infection − a review. Oral Maxillofac Pathol J 2021;12(2):69–72. [Google Scholar]
- [50].Driemeyer C, Falci DR, Oladele RO, Bongomin F, Ocansey BK, Govender NP, et al. The current state of clinical mycology in Africa: a European confederation of medical mycology and international society for human and animal mycology survey. Lancet Microbe 2022;3(6):e464–70. [DOI] [PubMed] [Google Scholar]
- [51].The Road to Zero. Report on the implementation of the advanced HIV disease package of care in Low- and Middle-Income countries. Clinton Health Access Initiative; 2022. [Google Scholar]
- [52].Mushi MF, Zaki SM, Penney ROS, Bamba S, Ngouanom Kuate MP, Kasamba EL, et al. Diagnostic options for pulmonary fungal diseases in Africa. ERJ Open Res 2023;9(2):00397–2022 Apr 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].First WHO. Model list of essential in vitro diagnostics. Geneva: World Health Organization; 2019. WHO Technical Report Series, No. 1017. [Google Scholar]
- [54].Denning DW. The ambitious ‘95–95 by 2025’ roadmap for the diagnosis and management of fungal diseases. Thorax 2015;70:613–4. [DOI] [PubMed] [Google Scholar]
- [55].Kneale Matthew. Global access to antifungal therapy and its variable cost. J Anti-microb Chemother 2016;71(12):3599–606 VolumeIssue1 DecemberPages. [DOI] [PubMed] [Google Scholar]
- [56].Land KJ, Boeras DI, Chen XS, et al. Reassured diagnostics to inform disease control strategies, strengthen health systems and improve patient outcomes. Nat Micro-biol 2019;4:46–54 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Thompson 3rd GR Le T, Chindamporn A, Kauffman CA, Alastruey-Izquierdo A, Ampel NM, et al. Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology. Lancet Infect Dis 2021;21(12):e364–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Mucormycosis ECMM MSG Global Guideline Writing Group. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis 2019;19(12): e405–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Mellinghoff SC, Hoenigl M, Koehler P, Kumar A, Lagrou K, Lass-Flörl C, et al. EQUAL Candida Score: an ECMM score derived from current guidelines to measure QUAlity of Clinical Candidaemia Management. Mycoses 2018;61(5):326–30. [DOI] [PubMed] [Google Scholar]
- [60].Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of America. Clin Infect Dis 2010;50(3):291–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Hoenigl M, Salmanton-García J, Walsh TJ, Nucci M, Neoh CF, Jenks JD, et al. Global guideline for the diagnosis and management of rare mould infections: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect Dis 2021;21(8):e246–57. [DOI] [PubMed] [Google Scholar]
- [62].World Health Organization. Model list of essential medicines −22nd list. Geneva: World Health Organization; 2021. 2021. WHO/MHP/HPS/EML/2021.02. [Google Scholar]
- [63].Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 2018;24(1):e1–e38 Suppl. [DOI] [PubMed] [Google Scholar]
- [64].Diongue K, Diallo MA, Seck MC, Ndiaye M, Badiane AS, Ndiaye D. The evidence for unavailability of systemic antifungals in Senegal. Ther Adv Infect Dis 2021;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Kneale M, Bartholomew JS, Davies E, Denning DW. Global access to antifungal therapy and its variable cost. J Antimicrob Chemother 2016;71(12):3599–606. [DOI] [PubMed] [Google Scholar]
- [66].Nussbaumer-Pröll AK, Eberl S, Welte R, Gasperetti T, Marx J, Bellmann R, Zeitlinger M. Comparison of antimycotic activity of originator and generics of voriconazole and anidulafungin against clinical isolates of Candida albicans and Candida glabrata. J Fungi (Basel) 2022;8(2):195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Hoharitanon S, Chaichalotornkul J, Sindhupak W. A comparison of the efficacy between two itraconazole generic products and the innovative itraconazole in the treatment of tinea pedis. J Med Assoc Thai. 200;88 Suppl 4:S167–72. [PubMed] [Google Scholar]
- [68]. https://gaffi.org/antifungal-drug-maps/ [Google Scholar]
- [69].Oladele RO, Akanmu AS, Nwosu AO, Ogunsola FT, Richardson MD, Denning DW. Cryptococcal antigenemia in Nigerian patients with advanced human immunodeficiency virus: influence of antiretroviral therapy adherence. Open Forum Infect Dis 2016;3(2) ofw055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Salmanton-García J, Herrador Z, Ruiz-Seco P, Nzang-Esono J, Bendomo V, Bashmakovic E, et al. Self-reported adherence to antiretroviral therapy in HIV+ population from Bata, Equatorial Guinea. AIDS Care 2016;28(5):543–53. [DOI] [PubMed] [Google Scholar]
- [71].Chaudhary RG, Rathod SP, Jagati A, Zankat D, Brar AK, Mahadevia B. Oral antifungal therapy: emerging culprits of cutaneous adverse drug reactions. Indian Dermatol Online J 2019;10(2):125–30. [DOI] [PMC free article] [PubMed] [Google Scholar]