Dear Editor,
Ticks, the carriers of over 90 % of vector-borne diseases, pose a growing public health challenge. A novel threat, the Yezo virus (YEZV), originating from Hokkaido Island in Japan, has emerged. This orthonairovirus which also includes the Crimean-Congo hemorrhagic fever (CCHF) virus—can cause acute febrile illnesses in both humans and animals [1]. YEZV shares close genetic similarities with the Romanian Sulina virus and the Uzbek Tamdy virus [2]. Transmission of YEZV primarily occurs through the infected bites of tick species—Ixodes persulcatus, I. ovatus, and Haemaphysalis megaspinosa—which spread the virus to reservoir hosts like deer, raccoons, and horses [3]. As global climate patterns shift and humans encroach on previously untouched natural areas, the likelihood of tick-borne diseases becoming more prevalent is expected to rise [4,5].
The virus has been found in Japan and China, with at least seven documented infections in Japan since 2014 and one in China, though no fatalities have been reported so far [2]. The discovery of YEZV occurred when a 41-year-old man was admitted to a hospital in 2019 suffering from fever and leg pain following a tick bite during a walk in a Hokkaido Forest. To trace the virus's origin, researchers examined wild animal samples collected from 2010 to 2020, detecting antibodies in Hokkaido shika deer and raccoons [3]. YEZV infection typically presents as mild fever, thrombocytopenia, and leukopenia, with elevated liver enzymes and ferritin levels indicating possible liver involvement. These clinical manifestations can vary based on the patient's age, medical history, and other factors [1].
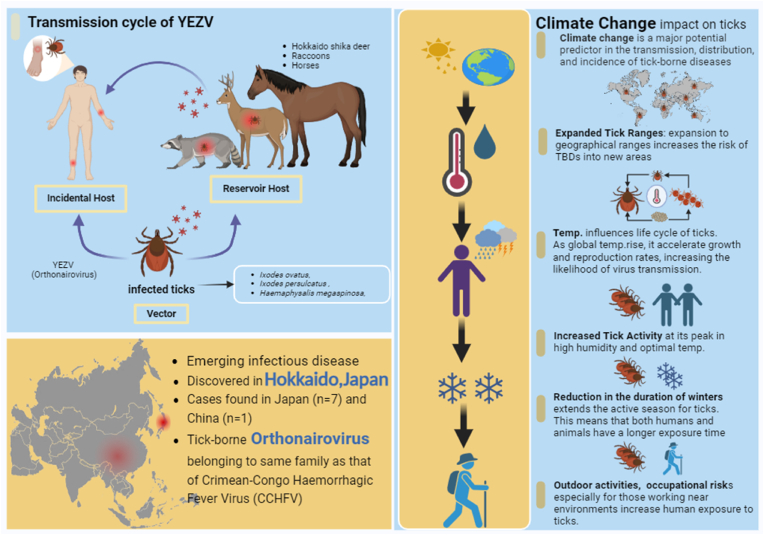
Given the influence of climate change on the transmission of tick-borne diseases, it is crucial to understand how environmental factors affect the spread of YEZV. Climate change impacts the spread of the YEZV, echoing its effects on other tick-borne diseases. Rising global temperatures enable ticks to inhabit previously inhospitable areas, enhancing their distribution and accelerating their lifecycle. This leads to longer periods of activity for ticks, heightening the chances of YEZV transmission as humans and animals experience extended exposure to potential tick bites. Furthermore, environmental changes such as habitat fragmentation and biodiversity loss modify tick dynamics, affecting their interactions with host species and increasing the risk of transmission. These factors necessitate proactive public health monitoring and adaptive strategies to address the challenges posed by climate-driven shifts in disease dynamics [Insert Fig. 1].
Fig. 1.
illustrates a visual representation of YEZV and its transmission pathways, and the influence of climate on disease dynamics.
The clinical diagnosis of YEZV involves assessing symptoms and epidemiological factors, with patients often exhibiting acute febrile illness, high fever, appetite loss, and malaise. Laboratory findings typically show thrombocytopenia, leukopenia, elevated liver enzymes, and high ferritin levels, indicating possible liver involvement. Diagnostic confirmation is achieved through qRT-PCR to detect YEZV RNA and ELISA tests for antibodies, suggesting active or past infection. Radiological findings are required to exclude other conditions. Differential diagnosis is essential to distinguish YEZV from other tick-borne illnesses [1].
Clinical manifestations of YEZV infection generally involve various hematological and hepatic symptoms. Patients may experience leukopenia (a reduction in WBCs), lymphocytopenia (a decrease in lymphocytes), thrombocytopenia (low platelet count), and coagulation disorders. Elevated liver enzymes - aspartate aminotransferase (AST) and alanine aminotransferase (ALT), along with high ferritin levels, indicate liver inflammation. The clinical presentation of YEZV can vary based on factors like the patient's age, medical history, and concurrent medications [3].
Management of YEZV infection focuses on supportive care, as specific antiviral treatments are unavailable. Monitoring through liver function tests and hepatoprotective agents is recommended. Most cases have recovered without severe complications, and preventive antibacterial treatment for tick bites is advised, although some cases resolve without it. Differential diagnosis is crucial for febrile patients with tick bite histories to exclude other viruses. Further research into antiviral treatment and active surveillance of tick-exposed populations are essential due to the limited data on virus impact [2,3].
A coordinated public health approach is essential due to the lack of specific antivirals. This strategy focuses on enhanced surveillance and reporting to track YEZV cases efficiently. Attention is given to advancing research for effective antiviral treatments and public education to increase awareness about tick bite risks and virus symptoms. Moreover, healthcare provider training will improve diagnosis and management of YEZV. Community involvement is greatly encouraged, particularly in high-risk areas, to support prevention and manage landscapes effectively. Supporting policies and regulations will also play a key role in controlling tick populations, finally aiming to mitigate YEZV's impact and protect public health [1,5].
The emergence of this novel threat underscores the evolving nature of vector-borne diseases and the influence of environmental and human factors. The virus’ presence in two Asian countries necessitates strong public health measures, targeted research, and the future development of treatments. Effective health measures like enhanced disease surveillance, education on tick-borne diseases, and intensified therapeutic research, are crucial. Public health efforts must also include community engagement and policy adaptation to effectively control and mitigate the spread of the disease. These proactive measures are essential to enhance our capacity to tackle the transmission of tick-borne diseases effectively.
CRediT authorship contribution statement
Pawan Kumar: Writing – original draft, Visualization, Conceptualization. Priyanshu Priyanshu: Writing – original draft, Visualization. Rakesh Kumar Sharma: Writing – review & editing, Supervision. Divya Sharma: Writing – review & editing, Supervision. Mithhil Arora: Writing – review & editing, Supervision. Abhay M. Gaidhane: Writing – review & editing, Visualization. Quazi Syed Zahiruddin: Supervision. Sarvesh Rustagi: Supervision. Edward Mawejje: Writing – review & editing, Supervision, Resources, Conceptualization. Prakasini Satapathy: Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: Patricia Schlagenhauf
Contributor Information
Pawan Kumar, Email: pawankumar705c@gmail.com.
Priyanshu Priyanshu, Email: priyanshu6504@gmail.com.
Rakesh Kumar Sharma, Email: prochancellor@geu.ac.in.
Divya Sharma, Email: divya.sharma.orp@chitkara.edu.in.
Mithhil Arora, Email: mithhil.arora.orp@chitkara.edu.in.
Abhay M. Gaidhane, Email: abhaygaidhane@gmail.com.
Quazi Syed Zahiruddin, Email: zahirquazi@gmail.com.
Sarvesh Rustagi, Email: sarveshrustagi@uumail.in.
Edward Mawejje, Email: emawejje@urc-chs.com.
Prakasini Satapathy, Email: prakasini.satapathy@gmail.com.
References
- 1.Ogata, Y., et al., A case of tick-borne Yezo virus infection: concurrent detection in the patient and tick. Int J Infect Dis.. [DOI] [PubMed]
- 2.Lv X., et al. Yezo virus infection in tick-bitten patient and ticks, northeastern China. Emerg Infect Dis. 2023;29(4):797–800. doi: 10.3201/eid2904.220885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kodama F., et al. A novel nairovirus associated with acute febrile illness in Hokkaido, Japan. Nat Commun. 2021;12(1):5539. doi: 10.1038/s41467-021-25857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dantas-Torres F. Climate change, biodiversity, ticks and tick-borne diseases: the butterfly effect. Int J Parasitol: Parasites and Wildlife. 2015;4(3):452–461. doi: 10.1016/j.ijppaw.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Satapathy P., et al. The rising tide of tick-borne encephalitis across European nations. QJM: Int J Med. 2023;116(12):973–975. doi: 10.1093/qjmed/hcad226. [DOI] [PubMed] [Google Scholar]