Abstract
Practical relevance:
The femur is the most commonly fractured bone in cats. Femoral fractures usually result from high-velocity trauma such as a road traffic accident or fall from a height and, as such, are associated with a wide variety of concurrent injuries. The initial focus of treatment should always be on assessment and stabilisation of the major body systems. Once any concurrent injuries have been addressed, all femoral fractures need surgical stabilisation, with the notable exception of greenstick fractures in very young cats, which can heal with cage rest alone. A number of different surgical options are available depending on the fracture type, location, equipment, surgeon experience and owner finances.
Clinical challenges:
Femoral fractures can vary hugely in complexity and the small size of feline bones can limit the choice of implants. Furthermore, cats can present unique challenges in the postoperative period due to their active nature and the limited means to control their exercise level.
Audience:
This review is aimed at general and feline-specific practitioners who have some experience of feline orthopaedics, as well as those simply wishing to expand their knowledge.
Aims:
The aim of this review is to help clinicians assess, plan and manage feline femoral fractures. It provides an overview of diagnostic imaging and a discussion of a range of suitable surgical options, including the principles of different types of fixation. It also highlights cat-specific issues, approaches and implants pertinent to the management of these cases.
Evidence base:
A number of original articles and textbook chapters covering many aspects of femoral fractures in cats and dogs have been published. Where possible, this review draws on information from key feline research and, where necessary, extrapolates from relevant canine literature. The authors also offer practical guidance based on their own clinical experience.
Keywords: Femur, fracture, trauma, capital femoral physis, distal femoral physis, femoral
Introduction
The femur is the most commonly fractured bone in cats, representing 33-38% of all feline fractures.1,2 Femoral fractures can be considered in the following three regional categories, with diaphyseal and distal being the most common fracture locations: 3
✜Proximal, which includes proximal epiphyseal, proximal physeal, subcapital, femoral neck, trochanteric and subtrochanteric fractures;
✜Diaphyseal;
✜Distal, which includes supracondylar, distal physeal, unicondylar, bicondylar and trochlear fractures.
The regions are important as they dictate the surgical approach and options. All femoral fractures should be surgically stabilised, with the single exception of greenstick fractures in very young cats, which can heal with cage rest alone. 3 It is not possible to provide adequate stabilisation for femoral fracture healing with a cast or splinted bandage.
Presentation and initial management
Femoral fractures are usually secondary to high-velocity trauma such as road traffic accidents or falling from a height. As a result, a wide range of concurrent injuries affecting multiple body systems are common, including potentially life-threatening injuries to the head, thorax and abdomen, alongside other orthopaedic injuries such as pelvic and spinal fractures.4,5 Depending on the severity of these injuries, patients can present anywhere from cardiovascularly stable but with severe and often non-weightbearing lameness, through to collapsed and critically ill. As with all trauma patients, initial assessment should focus on the major body systems, namely the cardiovascular, respiratory and neurological systems, through a combination of clinical examination and emergency diagnostic imaging; for further details see Adamantos and Corr (2007) and Aldrich (2007).6,7 Ideally, a very brief neurological examination (including assessment of mentation, gait, withdrawal and deep pain reflexes in all limbs) should be performed prior to administration of opioid pain relief, as having opioid analgesia on board can make interpretation challenging. However, appropriate analgesia should be provided as a matter of urgency.
Once stabilised, a more thorough clinical and orthopaedic examination can be performed, followed by further diagnostic imaging under sedation or general anaesthesia. It is advisable to counsel owners that the clinical signs associated with some injuries, and in particular those of the urinary tract, may not be evident at the time of initial presentation.
Diagnostics
For any confirmed or suspected trauma, it is recommended that thoracic view radiographs are obtained as part of the initial radiographic work-up due to the high incidence of concurrent thoracic trauma. 6 Radiography should be performed under sedation or general anaesthesia to facilitate proper patient positioning, as poorly positioned radiographs can be very misleading. orthogonal views of the femur should be taken.
To ensure good radiographic positioning, the femoral condyles should be superimposed on the mediolateral view. on the craniocaudal view it has always been recommended that the fabellae should be equally bisected by the femoral condyles, although one study in dogs has shown that this is not always a reliable indicator of a straight craniocaudal femur. 8 Assuming that the same may be true in cats, other radiographic criteria should also be used, including checking that the patella is centred mediolaterally within the trochlear sulcus (but beware of underlying patellar luxation). Additionally, approximately 50% of the lesser trochanter should be visible at the medial aspect of the proximal femur, the vertical walls of the intercondylar notch should be seen as distinct parallel lines, and the proximal femoral nutrient foramen should be centred mediolaterally within the femoral diaphysis (Figure 1).9-11 It is also important to include a marker for referencing accurate size measurements.
Figure 1.
(a) Craniocaudal and (b) mediolateral radiographic views of a feline femur with the major landmarks indicated. Note the mineralisation of the medial fabella, which many cats will not have. The lateral fabella, which is always mineralised in cats, is indicated by the dotted pink circle in (a). (c) Magnified view of a section of the femoral diaphysis demonstrating how to measure the femoral diameter and medullary canal diameter. Note that it is important always to include a marker for referencing accurate size measurements; a ruler can be seen in the bottom left corner of image (b), but the remainder of the markers have been lost from these radiographs during image cropping
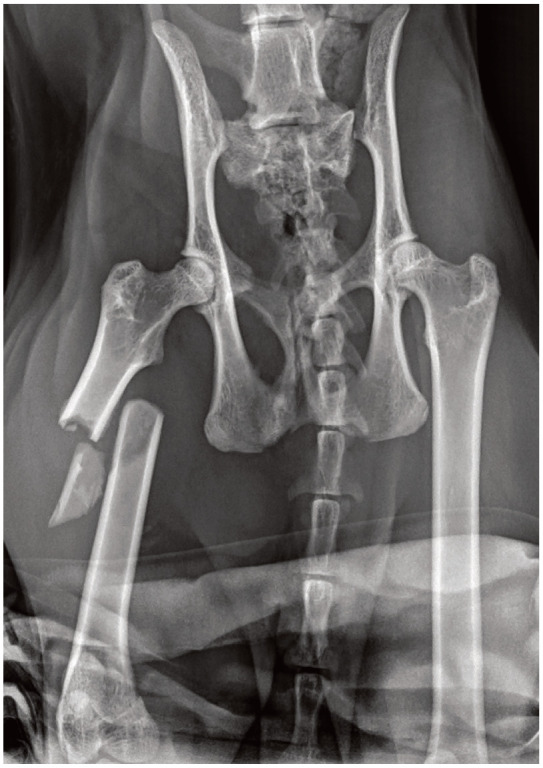
When evaluating for a potential proximal femoral fracture, it is advisable to include pelvic view radiographs; a lateral and an extended-leg ventrodorsal plus a frog-leg ventrodorsal radiographic projection (both ventrodorsal views are necessary to avoid missing subtle femoral neck or head fractures [Figure 2]12,13).
Figure 2.
(a) Ventrodorsal frog-leg radiographic view of a feline pelvis showing avulsion of the ischial tuberosity (short arrow) but no other clear injuries. (b) Ventrodorsal extended-leg radiographic view of the same feline pelvis showing again the avulsion of the ischial tuberosity (short arrow) but most importantly also a proximal femoral physeal fracture (long arrow), which was not evident on the ventrodorsal frog-leg radiograph
The vast majority of femoral fractures are detectable from radiographs alone, and the additional benefit of CT for femoral fractures is minimal except for some complex proximal or distal articular/juxta-articular fractures, where multiplanar and reconstructed views are helpful for preoperative planning.
Key surgical principles
Preoperative planning
Once the imaging has been obtained, careful attention should be given to the method of fracture fixation (Box 1). As part of this process it is important to consider the following questions:
✜ Does the fracture need to be accurately reconstructed? For example, articular fractures (Box 2).
✜ Can it be accurately reconstructed or may it benefit from reconstruction? For example, simple transverse fractures.
✜ Is it not amenable to reconstruction or is it not desirable to perform reconstruction? For example, comminuted diaphyseal fractures.
Urgency of, and options for, surgical repair
While not an emergency procedure, once a fracture is diagnosed and the patient is sufficiently stabilised, surgical repair should not be delayed unnecessarily, particularly if the fracture is in a skeletally immature patient or involves an articular surface or physis. In general, significant delays to femoral fracture repair increase the risk of quadriceps contrac-ture, especially in cases of diaphyseal fracture or where extensive muscle contusions or lacerations have occurred.14-16
Many different options are available for fixation of the variety of fractures that can be seen in the feline femur and a good understanding of the relevant forces acting on the fracture is vital for good implant selection. The availability of suitable implants for the feline femur has improved significantly in recent years with the production of 2.4 mm plating sets17-20 and feline-specific interlocking nails.12,21-23
Postoperative follow-up
Regardless of the implants used, appropriate radiographic follow-up is vital to assess the success of surgical fracture fixation. Timing of radiographic follow-up depends on the individual patient signalment and fracture configuration; for example, simple fractures in young healthy patients are likely to heal faster than comminuted fractures in older patients with comorbidities. The authors use the following timings as a guide:
✜ 4 weeks postoperatively in patients up to 3 months of age;
✜ 6 weeks postoperatively in patients up to 12 months of age;
✜ 8 weeks postoperatively in patients over 12 months of age;
✜ Up to 10 weeks postoperatively in patients with highly comminuted fractures.
These timing are based on the assumption that the patient’s clinical progress is going well. In the case of significant clinical concerns, radiographic evaluation should be expedited.
Proximal femoral fractures
Fractures of the proximal femur may variously involve the femoral head, neck, greater trochanter and/or subtrochanteric region.
Surgical approach
A craniolateral approach to the hip joint is most commonly used for repair of proximal physeal and femoral neck fractures, with slight variations described to facilitate implant placement.24,25 Visualisation can be improved by performing a tenotomy in the tendinous portion of the deep gluteal muscle close to the insertion on the greater trochanter, being careful to leave enough tendon on the bone to allow reconstruction. 25 There are a number of anatomical differences to be aware of when using this approach in cats compared with dogs; namely, the gluteal muscles may be relatively larger and the caudofemoralis muscle, not present in the dog, is interposed between the superficial gluteal and biceps femoris muscles (Figure 3). 25 A longitudinal incision through the joint capsule may then be required to access capital physeal fractures and fractures of the femoral neck within the joint capsule.
Figure 3.
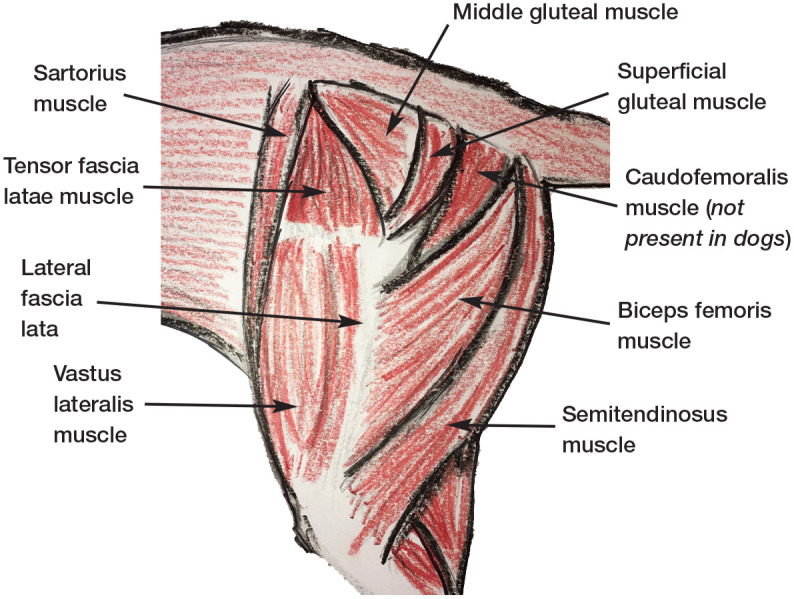
Musculature of the proximal hindlimb of the cat. Note that the gluteal muscles may be relatively larger in cats than dogs and the caudofemoralis muscle, not present in the dog, is interposed between the superficial gluteal and biceps femoris muscles
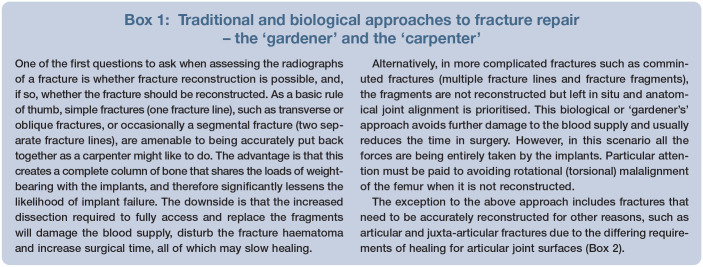
Figure 4.
(a) Model showing the ideal overlap position of two Kirschner wires for femoral neck or proximal femoral physeal fractures. Ideally the pins should be parallel to the femoral neck and start distal to the third trochanter. (b) Lateral and (c) ventrodorsal extended and (d) frog-leg views showing the repair of a Salter-Harris type I femoral head fracture with two parallel Kirschner wires
Combining the initial steps of a craniolateral approach to the hip with a lateral approach to the femur is generally the easiest way to access the greater trochanter and subtrochanteric region; 25 this is discussed in more detail for diaphyseal fractures. An alternative and far less commonly used approach is via a ventral incision with the cat placed in dorsal recumbency and the limbs abducted, with or without pectineal myotomy. 25 However, this approach risks damaging the medial circumflex femoral artery and vein, 26 and is not recommended.
Proximal physeal fractures and femoral neck fractures
While proximal physeal fractures and femoral neck fractures both occur frequently in the cat, traumatic femoral neck fractures are the more common, and are usually simple in configura-tion.27-29 Affected patients are typically under 12 months of age. While the majority of cats with femoral fractures present with non-weightbear-ing lameness, cats with fractures of the femoral head and neck can present with more subtle clinical signs, which may or may not progress to more severe lameness. 30 Thorough orthopaedic examination usually reveals pain, crepitus and a reduced range of motion of the hip joint, with final diagnosis achieved on radiography.
It is important to be aware that physeal fractures can on occasion occur in cats markedly older than 12 months of age.24,28 This is thought to be due to the effect of gonadectomy in delaying physeal closure, which is usually expected to occur at between 30 and 40 weeks of age.31-33 Due to the close proximity of the hip joint, alterations in hip position can greatly affect the clinician’s ability to identify physeal fractures. It is suggested that tightening of the joint capsule in hip extension results in reduction and thus concealment of the fracture, making detection very challenging on the ventrodorsal extended-leg view compared with the frog-leg view. 34 However, it is the authors’ experience that the opposite is frequently demonstrated in cats, where the fracture is most obvious in extension but not in a frog-leg position (Figure 2), due to displacement of the distal portion of the femur away from the femoral head, which is tethered to the acetabulum. Therefore, where there is a suspicion of a proximal femoral fracture, radiographs should include ventrodorsal frog-leg and extended views before proximal physeal fractures can be ruled out.
While physeal fractures can be truly traumatic, non-traumatic femoral capital physeal fractures have also been well documented. These typically occur secondarily to physeal dysplasia and metaphyseal disorders, with a higher incidence in overweight, male, neutered cats and in certain breeds of pedigree cat.30,35-42 They can usually be identified by the lack of a history of trauma, often progressive clinical signs, a potential for bilateral lesions and signalment. Two pathological entities are described. First is the so-called ‘spontaneous capital physeal fracture’, which is where underlying physeal dysplasia leads to physical separation. This can be difficult to differentiate from a traumatic fracture as it appears radio-graphically as an acute physeal separation and typically occurs in cats under 2 years of age.38,43 This disease is not well understood, but it has been suggested that physeal dysplasia may be part of a widespread multicentric disorder of the chondrocytes. 44 The second described pathology is metaphyseal osteopathy of the femoral neck. This may be more easily identified, due to the appearance of a chronic fracture/femoral neck metaphyseal remodelling at diagnosis and older age of the patient. 30 Accurately identifying cats with pathological fractures due to underlying disease is important as repair is less likely to be successful and salvage surgery should be considered. 38
Non-surgical treatment of traumatic proximal physeal and femoral neck fractures has been described but is associated with malunion or non-union and subsequent hypertrophic pseudoarthrosis, resulting in persistent lame-ness.27,28 By comparison, surgical treatment has been associated with a short recovery period, good prognosis for return to function and minimal complications, even without optimal fracture fixation.24,45 Where complications are seen, these are more common with steeper fracture lines due to the greater shear forces acting on the repair. 29
Fracture repair is usually achieved through reduction and stabilisation with small ‘Kirschner (K)-wires’ (Box 3). 29 Every effort must be made to minimise any vascular damage caused by surgery, as this can result in subsequent aseptic necrosis of the femoral head and/ or neck and the development of osteoarthritis of the hip joint. 46 It is therefore recommended to limit the number of passes made with a K-wire, to include only two pins and to consider relatively small diameter pins. It is postulated that a ventral approach rather than a craniolateral approach may better preserve the blood supply from the joint cap-sule; 47 however, the authors would recommend a careful craniolateral approach, as this is the most familiar surgical approach to the hip. Large adult patients may be able to take a fully threaded cortical screw placed in a lag fashion with the aid of a pointed drill guide, alongside an anti-rotational K-wire. 29 Placement of such implants should be avoided in immature patients with the potential for significant additional growth as compression of the physis is likely to cause premature closure and arrest growth. 46
Depending upon available experience and equipment, and with the possible advantage of minimising vascular compromise, it is possible to perform closed reduction with fluoroscopic-assisted percutaneous pinning (FAPP), 48 a form of minimally invasive osteosynthesis (MIO; Box 4).
Following open or closed repair, activity must be restricted until clinical union is achieved, usually after approximately 4 weeks, with, or more typically without, a non-weight-bearing bandage for the first 1-2 weeks. 29 Resolution of lameness can be expected after 4-8 weeks. 24 The implants are often left in situ but can be removed following fracture healing in young animals where there is concern for interference with ongoing growth or where implant-related complications are suspected. 24
As for comminuted, non-reconstructable fractures, primary fixation is often not possible or not indicated for chronic fractures with rounded and fibrotic fracture ends, and non-traumatic femoral capital physeal fractures. Historically, in these instances the only option has been femoral head and neck excision (covered in more detail by Lafuente [2011] 38 and Harper [2017] 57 ). While good outcomes are possible, 58 this procedure involves sacrifice of the hip joint and clinical outcomes are not absolutely predictable. However, the development of smaller total hip replacement prostheses has now allowed total hip replacements to be performed in cats as a first-line treatment or as revision surgery following femoral head and neck excision, with some good preliminary results.59-64
Avulsion fractures of the greater trochanter
Avulsion fractures through the physis of the greater trochanter are rare, and typically occur in cats less than 1 year of age prior to closure of the greater trochanteric physis, which normally takes place between 38 and 42 weeks of age. 33 These fractures are frequently seen alongside hip luxations (Figure 5a), or femoral neck or femoral capital physeal fractures.13,27 As these fractures are not always easy to detect on radiographs (Figure 5a) and commonly occur alongside more obvious radiographic abnormalities, careful radiographic assessment is vital. 13 Due to the attachment of the gluteal muscles, proximal displacement of the fracture fragment can occur, and stabilisation is important to restore gluteal muscle function and hip joint stability. 13
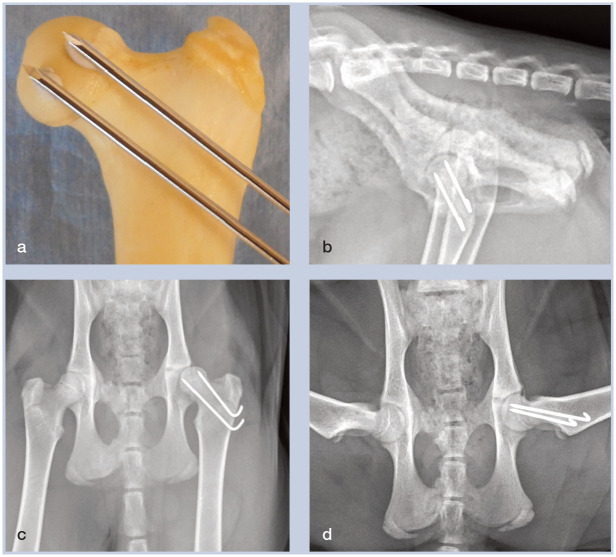
Figure 5.
(a) Ventrodorsal radiographic view of a kitten with polytrauma including a left hip luxation, left sacroiliac luxation, right ischial fractures and left ischial tuberosity avulsion. The greater trochanter of the left femur does not have a normal appearance (arrow); however, this could be due to rotation. At surgery a trochanteric avulsion was also found. (b) Ventrodorsal radiographic view of the pelvis of the same kitten following repair of the greater trochanteric fracture with two Kirschner wires and a polydioxanone tension band. Note that the left sacroiliac luxation has also been stabilised via placement of a sacroiliac screw
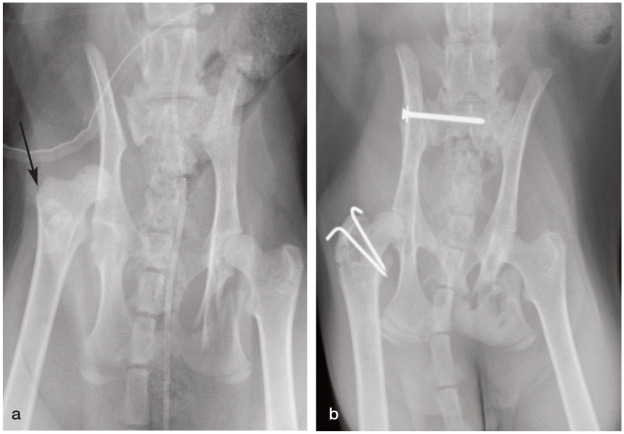
Figure 6.

Ventrodorsal radiographic view of a feline femur showing an intramedullary pin that was placed as a sole means of fixation for a simple mid-diaphyseal fracture. The fracture subsequently displaced and then fissures developed in line with the axis of the pin
Stabilisation techniques that can withstand the distractive forces of the gluteal muscles during weightbearing include pin and tension band (Figure 5b), lag screw and bone plate. 46 Pin and tension band fixation is the most commonly used repair technique. First, two K-wires or pins are placed across the greater trochanter in a laterome-dial direction, exiting through the medial cortex of the proximal femur. A figure-of-eight stainless steel wire is then placed on the lateral surface of the femur. In very young kittens, polydiox-anone suture can be used as an alternative to stainless steel wire. Where hip luxation or fractures of the femoral head and neck are present, these should be addressed first, prior to repair of the trochanter. Limited, low-impact activity is recommended for 2-4 weeks following fixation but external support is not usually required. 29
Subtrochanteric fractures
Subtrochanteric fractures are rarely seen in the cat, and are usually an extension of a comminuted proximal diaphyseal fracture. 3 As such, they are stabilised by surgical repair of the diaphyseal fracture, paying particular attention to contouring of the plate up and over the proximal greater trochanter (discussed later). Intramedullary pins (Box 5) can aid stability as part of a plate-rod construct, or as part of a tied-in external skeletal fixator, with two or more transosseous pins per fragment. 73 No external support is required, and activity restriction only until bony union is achieved. Implant removal may be necessary if soft tissue irritation occurs. 29
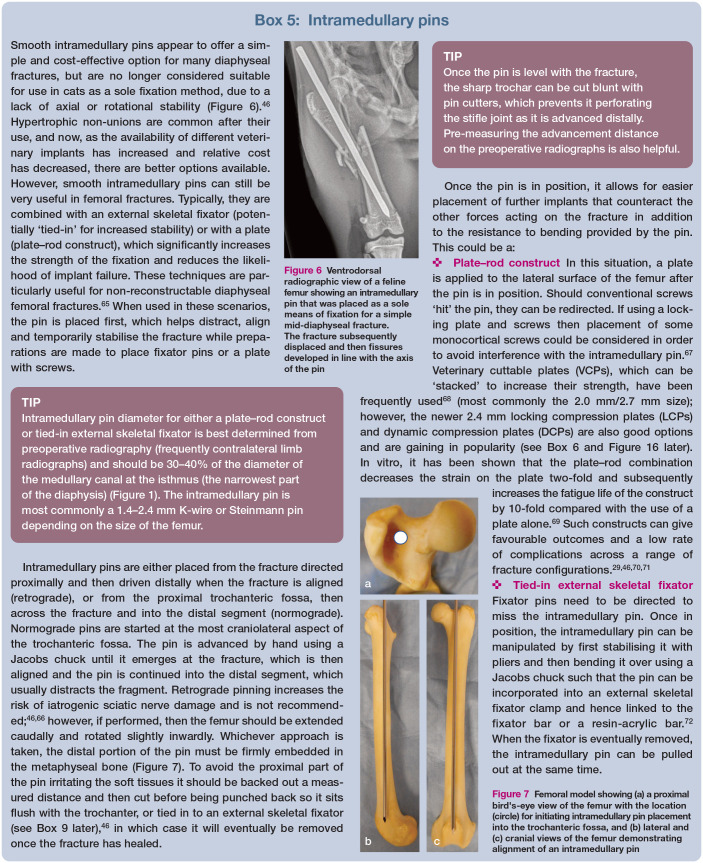
Figure 7.

Femoral model showing (a) a proximal bird’s-eye view of the femur with the location (circle) for initiating intramedullary pin placement into the trochanteric fossa, and (b) lateral and (c) cranial views of the femur demonstrating alignment of an intramedullary pin
Prognosis
Most proximal femoral fractures are quite rare and little is known about their outcome. The prognosis for proximal femoral fractures is generally thought to be good, although identification of underlying pathology in the femoral physis or neck could negatively influence outcome.
Diaphyseal femoral fractures
Surgical approach
Traditionally, an open reduction via a lateral approach to the femoral shaft has been favoured for fractures of the diaphysis and is the surgical approach that will be familiar to the majority of practitioners. 54 However, the feline femur is a relatively straight bone, and minimally invasive surgical techniques are now described (discussed in more detail in Box 4). 52 For an open approach, after incising the fascia lata along the cranial border of the biceps femoris, the muscle is carefully retracted caudally, avoiding sharp instruments placed deep to the muscle due to the risk of damaging the sciatic nerve. This exposes the vastus lateralis over the craniolateral femur, and adductor magnus caudally, with the division between them providing safe access to the femur.
Simple transverse and oblique fractures
The relatively straight conformation of the feline femoral diaphysis (Figure 8) makes plating these fractures fairly straightforward. Once the bone for plating has been approached, the fracture ends should have any fracture haematoma removed before reapposing them in order to achieve anatomical reconstruction suitable for compression via a plate or via a lag screw initially. Frequently there is overriding (overlapping) of bone fragments within diaphyseal fractures, which can require significant distraction (see box below) to alleviate the muscle contraction preventing alignment of the fracture ends.
Figure 8.
Three-dimensional CT reconstruction of a feline femur shown from (a) craniocaudal, (b) lateromedial, (c) caudocranial and (d) mediolateral directions. Slight anteversion (pointing forwards) of the femoral head can be seen, which is typical in cats. The linea aspera, identified by the arrow on images (b) and (c), can be a helpful visual aid when assessing for accurate fracture reduction and/or anatomical alignment. The long and relatively straight femoral canal with minimal metaphyseal flare is typical in cats. Also note this cat has both medial and lateral fabellae
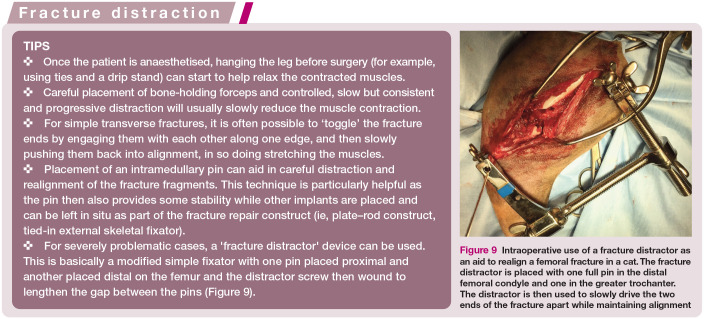
For severely problematic cases, a ‘fracture distractor’ device can be used. This is basically a modified simple fixator with one pin placed proximal and another placed distal on the femur and the distractor screw then wound to lengthen the gap between the pins (Figure 9).
Figure 9.

Intraoperative use of a fracture distractor as an aid to realign a femoral fracture in a cat. The fracture distractor is placed with one full pin in the distal femoral condyle and one in the greater trochanter. The distractor is then used to slowly drive the two ends of the fracture apart while maintaining alignment
Once the fracture is reduced, for most cats a 2.4 mm DCP or LCP works best, although a 2.7 mm plate can be considered in larger cats (Box 6), and can be applied in either compression or neutralisation mode (Box 7). The VCP is a further option, and the 2.0 mm/ 2.7 mm is most commonly applied in cats. The VCP does not allow for compression of a transverse fracture, which is a disadvantage; however, VCPs are stackable and cuttable, which greatly adds to their versatility for a relatively low-cost plating option.
Figure 10.

Plate options for a feline femur laid out to demonstrate the different screw hole densities. From left to right the plates are: a 2.0 mm dynamic compression plate, a 2.4 mm locking compression plate (LCP), a 2.7 mm LCP and a 2.0 mm/2.7 mm veterinary cuttable plate
Figure 11.
Plate options for a feline femur as demonstrated on a model femur: (a) 2.0 mm/2.7 mm veterinary cuttable plate, (b) 2.4 mm locking compression plate (LCP), (c) 2.7 mm LCP and (d) a plate-rod configuration
Figure 12.

Models showing the three options for plate application and the subsequent effect on the implant’s function and the forces acting through the bone and implant. (a) Compression (fracture fragments are compressed and the fracture has load sharing). (b) Neutralisation (lag screw placed across the fracture; the fracture ends are compressed by the lag screw but not by the plate and, as such, the fracture still has some load sharing). (c) Bridging (the fracture ends are not compressed and there is no load sharing; the plate takes all of the load)
Interlocking nails are also well suited to dia-physeal fractures (Box 8), but feline interlocking nail systems are not especially widespread in practice. Although not necessarily a first choice, the use of an external skeletal fixator with a tied-in intramedullary pin (Boxes 5 and 9; Figure 14a,b) is a viable alternative to plating if this option is not available. Use of a free-form tied-in external skeletal fixator with a resin-acrylic bar can provide an inexpensive and versatile alternative to the traditional linear bar systems (Figure 14c,d). 72
Figure 14.
(a) Lateral femoral radiograph showing a long spiral fracture of the mid-femoral diaphysis in a cat. (b) Craniocaudal femoral radiograph of the cat in (a) following stabilisation with an intramedullary pin tied into a type Ia external skeletal fixator using two end-threaded positive profile pins proximally and distally. (c) Lateral femoral radiograph of a different cat showing a grade II open distal diaphyseal femoral fracture (note the gas in the soft tissues). (d) Lateral femoral radiograph of the cat in (c) following stabilisation with an epoxy putty free-form fixator, combining a tied-in intramedullary pin
Figure 13.
Fixator pin options include those that are (a) end-threaded positive profile, (b) end-threaded negative profile and (c) mid-threaded positive profile. Single clamp options include (d) Kirschner-Ehmer (KE)-style clamps and (e) IMEX-SK-style clamps. Double clamp options include (f) IMEX-SK-style clamps and (g) KE-style clamps. (h) Lateral radiographic view of a feline femur showing measurement of the isthmus (narrowest part) for estimation of appropriate fixator pin sizes (femoral diameter) and intramedullary pin sizes (medullary canal diameter)
For long oblique diaphyseal femoral fractures and simple multifragmentary fractures (Figure 15) that are amenable to anatomical reduction, stabilisation under compression is usually recommended. Historically, some would advocate an intramedullary pin and cerclage wires; however, better alternatives are now available that are more reliable and give improved results. After approaching the fracture, it is helpful to reduce and hold the fracture fragments in position with pointed reduction forceps while one or two 1.5-2.0 mm screws are placed in a lag fashion perpendicular to the fracture line, either independently or through a plate hole. The lag screws compress the gap and then a plate is applied to the lateral surface of the femur in a neutralisation fashion (Box 7). Alternatively, if there are concerns about placing a lag screw then it is possible to use a K-wire instead (Figure 16); however, it must be noted that this will not provide compression.
Figure 15.
Ventrodorsal radiographic view of a feline pelvis showing a mid- to proximal third diaphyseal femoral segmental fracture
Figure 16.
(a) Ventrodorsal radiographic view of a feline pelvis showing a short oblique slightly comminuted mid-diaphyseal femoral fracture. A historical femoral neck fracture, stabilised with three pins, and repaired with two pins and a figure-of-eight tension band wire) is also evident. (b) Craniocaudal radiographic view of the femur in (a) following surgical stabilisation. A pin was placed across the fracture, and a 2.4 mm locking compression plate was applied to the lateral aspect with a mixture of cortical and locking screws
While an interlocking nail or a tied-in intramedullary pin with an external skeletal fixator (Figure 14) do not enable compression of the fracture, they do provide a load-sharing construct and can still achieve good healing. This is particularly applicable to immature cats where their bone is relatively small and soft, reducing implant stability, yet their periosteum is approximately twice the thickness of that of an adult cat, helping with fracture stability and healing. As a result, even where diaphyseal femoral fractures are anatomically reducible, in immature cats they may be best treated with a type I external skeletal fixator. 3 In very young cats it is advisable to place a fixator without a tied-in pin due to the potential for impact on the physes and subsequent growth of the femoral head and neck, something that has been shown in growing dogs. 95
Comminuted fractures
Comminuted fractures are usually, or ought to be, considered non-reconstructable (Figure 17), and frequently result from significant trauma. The focus therefore shifts to a biolog-ical/’gardener’s’ approach (Box 1) whereby soft tissues and fracture fragments are not disturbed but the fracture is stabilised proximally and distally, thus preserving blood supply and promoting indirect bone healing. Fixation options include interlocking nails, external skeletal fixators and plate osteosynthesis (Boxes 6-9). All can be applied via a minimally invasive approach or the last with an OBDNT approach (Box 4).52,96
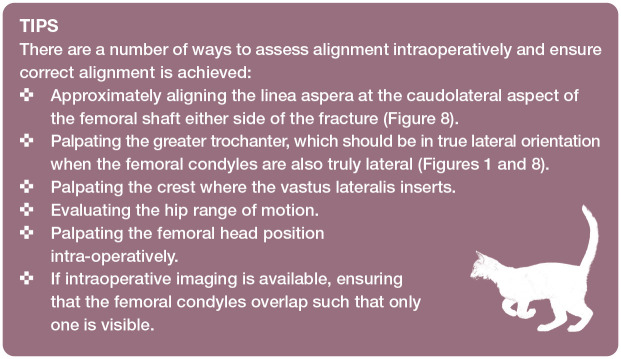
Figure 17.
(a) Lateral and (b) craniocaudal radiographic views of a highly comminuted and fissured diaphyseal femoral fracture. Postoperative (c) lateral and (d) craniocaudal radiographic views of the cat in (a,b) showing a plate-rod repair, whereby a 1.6 mm Kirschner wire has been placed as an intramedullary pin and a lateral 2.4 mm locking compression plate has been contoured and applied. Note that no attempt has been made to reconstruct the fracture
Although plating can be perfectly appropriate, it should be remembered that there will be no load sharing between the plate and the bone, and so implant failure is more likely than when the fracture is reconstructed and considered ‘load sharing’. For that reason, plate size should be carefully considered - some cats can take a 2.7 mm DCP/LCP and this remains an option to increase the strength of fixation, but more commonly surgeons opt for a plate-rod solution (Box 5) or an interlocking nail (Box 8). Intramedullary implants (ie, intramedullary pin or interlocking nail) provide good resistance to bending forces and can be placed open or via MIO. Where a plate-rod fixation is used, the intramedullary pin helps align and stabilise the fracture prior to plate application. Placement of an appropriately sized intramedullary pin can impede screw placement, resulting in the concentration of screws in the metaphyseal areas where more bone stock is available. Careful plate selection can help to reduce pin-screw interference. Most commonly, a 2.4 mm LCP or a 2.0 mm/2.7 mm VCP are used, due to the ability to place mono-cortical screws in the former and the increased screw hole density and ability to carefully direct the screws in the latter, thus enabling the surgeon to avoid screw-pin interference.
When anatomical reduction is not possible, careful attention must be paid to spatial and rotational alignment of the limb as there is a tendency to stabilise diaphyseal fractures with retroversion of the femoral head and neck, which can lead to a functional gait abnormality and lateral patellar luxation (see the box on page 16 for tips for intraoperatively assessing alignment). 3 Bone grafts are generally not required unless sufficient cortical fracture gaps exist to allow soft tissue invasion, in which case cancellous autograft, cancellous allograft and synthetic alternatives have proved effective. 97
Ensuring careful assessment of limb alignment is particularly important when performing MIO as not all landmarks are visible intraoperatively. As such, fluoroscopy is often used to aid in the assessment of joint alignment in these surgeries.
Prognosis
Most diaphyseal femoral fractures in cats will heal without complications if treated appropriately and a return to full function can be expected. 73 Bone plates and external skeletal fixators, both with (ie, plate-rod constructs and tied-in external skeletal fixators) and without the aid of an intramedullary pin, and interlocking nails can all be successful means of achieving bone healing when used judiciously, but all have advantages and disadvantages. It is well recognised that external skeletal fixators can require greater postoperative management and are associated with a high level of minor (mostly pin-related) com-plications.70,94 While in one study bone plates showed a lower complication rate than external skeletal fixators, and plate-rod constructs a lower complication rate again, the rate of major complications was highest in the plate-rod constructs, followed by the bone plates, both exceeding the external skeletal fixator group. 70 By comparison, the angle-stable interlocking nail appears to be associated with a very low complication rate and rapid achievement of clinical union based on early clinical studies. 81 Other factors can also influence healing, including increasing age, increasing weight and increasing fracture complexity. 70
Complex fractures typically occur secondarily to high-energy trauma and are associated with greater vascular compromise and soft tissue disruption, which impedes healing. 98 As such, these patients often need a longer period of restricted activity and owners should be warned of the potential requirement for additional radiographic examinations until fracture union can be confirmed.
Distal femoral fractures
Most distal femoral fractures are located within the stifle joint capsule, which can make them difficult to differentiate from joint instability on clinical examination alone, 99 depending on the experience of the clinician. Careful palpation of the patella and patellar ligament while paying particular attention to any crepitus can help with identification of these fractures.
Surgical approach
Depending on the required surgical exposure, access to the distal femur and stifle can be via a lateral, medial or bilateral parapatellar approach or minimally invasive approach (discussed briefly in Box 4).52,54 A single skin incision with bilateral parapatellar arthrotomy is often necessary for intracondylar fractures. For physeal fractures a lateral parapatellar approach, with an arthrotomy, is most commonly performed, with an additional small medial parapatellar approach used for medial implant placement. 3 It is therefore recommended to position the patient in dorsal recumbency to allow an intraoperative change/extension to the planned approach.
For an open lateral approach, first the fascia lata is incised along the cranial border of the biceps. The incision is then extended distally through the lateral fascia of the stifle joint parallel to the patellar ligament, ensuring that sufficient fascia is left adjacent to the patella for closure. Caudal retraction of the biceps and lateral fascia away from the vastus later-alis allows identification of the intermuscular septum, formed from the fascia lata and attached to the femur. This is incised, thus providing access to the distal femur. Access to the joint can be achieved via incision in the joint capsule if required. 54
For an open medial approach, the medial fascia is incised parallel to the patellar ligament, again ensuring that sufficient fascia is left for closure. An initial stab incision is then made into the joint capsule before being extended proximally through the joint capsule, medial parapatellar fibrocartilate, medial fascia, vastus medialis muscle and the cranial part of the sartorius muscle, taking care to cut parallel to the muscle fibres. 54 An open bilateral approach is a combination of the above, through a single or separate skin incisions as desired. 54
Supracondylar fractures
Supracondylar fractures can be surgically challenging as even simple fractures may not have inherent rotational or shearing stability and the distal fragment is inevitably short. 100 While stabilisation with dynamic intramedullary cross-pinning has been described, 101 rigid stabilisation with a bone plate, external skeletal fixator or angle-stable interlocking nail 81 is recommended, with care being taken not to penetrate the stifle joint 99 or impinge patellar tracking.
Due to the caudal bowing of the femoral condyle, 2.0 mm or possibly 2.4 mm anatomical condylar/J-shaped/’hockey-stick’ plates are frequently used to facilitate placement of at least three screws in the distal fragment (Figure 18). Alternatives include a 2.7 mm veterinary reconstruction plate or a 2.7 mm string of pearls locking plate, or other similar systems. Both plates can be cut to size and contoured in three dimensions, thus accommodating the distal curvature of the femur.100,102 However, for both, the disadvantage of their malleability is that they are not sufficiently strong or stiff to act as a bridging plate without a high risk of implant failure.29,100,102 Therefore, reconstruction plates and string of pearls plates should only be placed as a sole method of fixation when accurate anatomical reduction can be achieved and the plate can function as a neutralisation implant. If accurate anatomical reduction cannot be achieved, adjunct fixation such as an intramedullary pin (plate-rod construct) (Box 5) or double plating should be used. 102
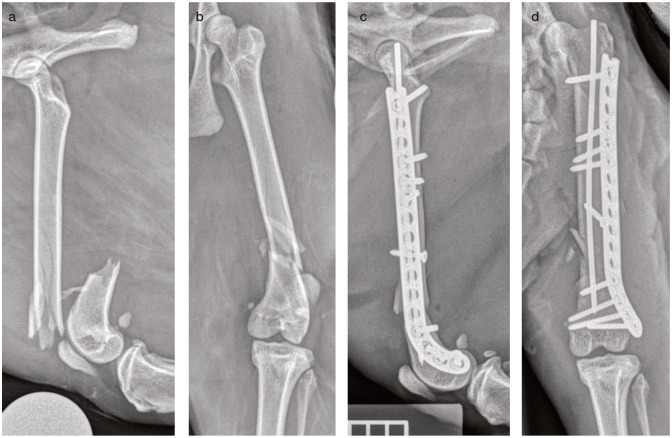
Figure 18.
(a) Lateral and (b) craniocaudal radiographic views of a comminuted and fissured supracondylar femoral fracture. (c) Lateral and (d) craniocaudal radiographic views of the cat in (a,b) following stabilisation with an intramedullary pin and a J-shaped hockey-stick plate (plate-rod construct), which allows for more screws to be placed in the short and backward-curving distal fragment. The plate has been cut to length proximally using large pin cutters
When straight plates are used, it is unlikely that the distal fragment will accommodate more than two screws. Two screws in the distal fragment can provide adequate fixation, particularly if there is the option to place one as a locking screw and if anatomical reduction is achieved. However, a caveat is that the most distal screw often needs to be carefully angled away from the joint surface and therefore usually needs to be a nonlocking screw or placed as a monocortical locking screw. The authors’ preference is to use a J-shaped plate.
Supracondylar fractures are also amenable to external skeletal fixation. A modified type II hybrid linear fixator can be used, whereby a full pin is placed across the femoral condyle in addition to one or two anti-rotational half pins, followed by three half pins in the diaphysis proximal to the fracture. An alternative approach is to use a distal miniature circular fixator construct (IMEX).103,104 The major disadvantage of using external skeletal fixators for these fractures is the pin tract morbidity, which is seen due to the mobile skin and soft tissue around the stifle and the muscular envelope surrounding the femur. 94 If a fixator is chosen, a modified type II configuration is commonly used, with or without a tied-in intramedullary pin. Use of a tied-in intramedullary pin is recommended if only one additional half pin can be placed in the distal fragment. 99
Unlike most other femoral fractures, stabilisation of distal femoral fractures with an interlocking nail has traditionally been performed in a retrograde fashion. 21 Retrograde insertion reduces the need for the length of the interlocking nail to match that of the femur exactly, facilitates accurate placement of the distal screws due to the small distance between the first hole and the jig, and does not appear to result in radiographically evident stifle arthritis or pain on stifle manipulation. 21 However, not all interlocking nails are compatible with retrograde placement and more recently normograde placement has been described for these fractures, with positive initial out-comes. 81 If available, fluoroscopic guidance should enable a true MIO approach with closed reduction and stabilisation. Alternatively, an OBDNT approach can be used successfully where fluoroscopy is not available. 21
The prognosis for cats following appropriate surgical management for supracondylar fractures is good to excellent when anatomical reconstruction of the stifle is achieved, and a satisfactory or good clinical outcome is seen in the majority of cases with significant comminution.3,105
Distal physeal fractures
Fractures of the distal femoral physis are common in cats, with the vast majority being Salter-Harris type I or II (Figure 19). The distal femoral physis should close between 54 and 76 weeks of age in cats; 31 however, the effects of early neutering can delay this beyond 24 months of age, 32 thus extending the window for physeal fractures. Salter-Harris type IV fractures (Figure 20) are rarely encountered and can be treated as simple intracondylar fractures (described later). Reduction and stabilisation is vital in order to restore stifle configuration, maximise possible future physeal growth and reduce the risk of excessive callus formation, which can predispose to quadriceps contracture. 106
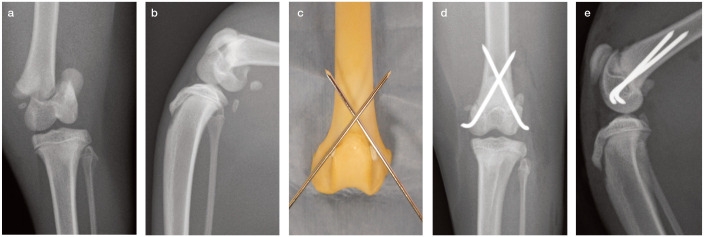
Figure 19.
Preoperative (a) caudocranial and (b) mediolateral radiographic views of a feline stifle, showing a Salter-Harris type I distal femoral physeal fracture. (c) Model showing correct cross-pin placement and alignment. Postoperative (d) caudocranial and (e) mediolateral radiographic views of the stifle in (a,b) showing fracture reduction and crossed Kirschner wire pin placement (1.2 mm pins), with the ends bent over. Note the pins must cross above the fracture and the trochar tip must exit through the femoral cortex
Figure 20.

Craniocaudal radiographic projection of a cat with a Salter-Harris type IV femoral condylar fracture
The caudal pulling forces of the hamstrings tend to promote under-reduction of the distal femoral condyle, and therefore it is important to apply traction and compression to correctly reduce it. 99 Reduction is best achieved with the stifle in extension. Some surgeons advocate placement of pointed reduction forceps between the intercondylar notch and the cranial cortex just proximal to the trochlea; 3 however, this should be performed with caution in very young animals with soft bone.
The distal femoral physis has four depressions in the epiphysis, which correspond to bony protuberances in the metaphysis. Once reduced, these provide inherent resistance to rotation and shearing forces. 106 As a result of this inherent stability, a relatively weak fixation can be used, including a figure-of-eight stainless steel wire, 107 a single intramedullary pin, paired rush pins, 108 or the authors’ preference of cross pins (Figure 19), 101 which have been experimentally shown to be the most resistant to torsional loads. 109
With cross pins, typically 1.0-1.4 mm K-wires are inserted just cranial to the medial and lateral collateral ligaments and are directed prox-imally to engage the contralateral cortex of the proximal fragment; this can be performed via an open approach or, more recently, has been described using the minimally invasive technique FAPP (Box 4). 48 It is important that the pins are introduced distal enough in the epi-physeal fragment and that they cross above the fracture line to give sufficient rotational stability. Rush pinning or dynamic intramedullary pinning is performed with a similar technique but the angle of the K-wires is steeper such that they glance off the endosteum instead of penetrating the transcortex. If this occurs inadvertently during a cross- pinning attempt, there is no need to redirect the pin; instead it should be advanced more proximally to the level of the greater trochanter. 108
Key Points.
✜ Initial focus must always be on assessment and stabilisation of the major body systems as life-threatening concurrent injuries are common.
✜ Orthogonal views of both femora are essential for all cases. Lateral, extended ventrodorsal and frog-leg ventrodorsal radiographic projections of the pelvis facilitate an accurate diagnosis when fractures affecting the proximal femur are suspected.
✜ Nearly all femoral fractures in cats should be managed surgically. The feline femur is not amenable to casting or bandaging.
✜ It is not recommended to attempt temporary external coaptation or support of femoral fractures with bandages or splints, and strict cage rest is preferred until treatment can be instigated.
✜ A range of repair options are available for femoral fractures in cats, including internal and external fixation. The 2.4 mm plating system is a highly appropriate implant for cat femoral fractures, and 4.0 mm interlocking nails have also been shown to be appropriate in most cats.
✜ Intramedullary pinning is not recommended either as a sole treatment or combined with cerclage wire; however, combining an intramedullary pin with a plate (plate-rod construct) or an external skeletal fixator (tied-in external skeletal fixator) is recommended, particularly if there is comminution associated with the fracture.
Implants causing compression across the physis are not recommended due to the potential impact on future growth in these immature patients. 46 In cats with remaining growth potential (<6 months old), follow-up radiographs should be taken at 2-4 weeks with consideration of possible implant removal. More commonly than not, however, the physis has closed due to the inciting or surgical trauma and then implant removal is not necessary unless it is causing irritation. 110
Fractures through the femoral condyle
Simple, unicondylar fractures more commonly affect the medial aspect of the distal femoral condyle and are usually minimally displaced as a result of the soft tissue support provided by the caudal cruciate and medial collateral ligaments. 29 More complex bicondylar fractures separate the medial and lateral aspects of the condyle from the diaphysis, often with a Y- or T-configuration, although comminution can be seen more proximally. Occasionally these fractures involve the trochlear groove, ranging from a single to multiple fracture lines crossing the trochlea. 105 The principles of articular fracture management (Box 2) must be followed in order to return joint function and minimise the development of osteoarthritis, although anatomical reduction and rigid fixation can be very challenging.
Critically, the intra-articular fracture fragments are aligned first. Anatomical reduction of the joint surface, and compression by placement of a transcondylar lag screw (2.0-2.7 mm), is required. Where a lag screw is used alone, an anti-rotational K-wire (0.8-1.2 mm) can also be placed. It is advisable to check the intra-articular structures (cruciate ligaments and menisci) during the arthrotomy procedure and manage any associated damage. 29 Once the condyle is reconstructed, the approach to the fracture is similar to either distal physeal or supracondylar fracture repair. As discussed earlier, options for fixation of the supracondy-lar portion include reconstruction plates, supracondylar plates or locking plates, the last of which can provide good stability when placed bilaterally. 99 If comminuted, the repair is often very challenging. Large fragments can be secured with pins; small fragments may require removal but, wherever possible, the largest components of the condyle should be compressed together with a lag screw. 99
Prognosis
The prognosis for return to full function is good for distal femoral fractures, although osteoarthritis and/ or meniscal calcification are likely sequelae of fractures affecting the weightbearing articular surface. 3
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and / or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/ or publication of this article.
Ethical approval: This work did not involve the use of animals and therefore ethical approval was not specifically required for publication in JFMS.
Informed consent: This work did not involve the use of animals and therefore informed consent was not required. No animals or humans are identifiable within this publication, and therefore additional informed consent for publication was not required.
Contributor Information
Victoria J Roberts, Pride Veterinary Centre, Derby, UK.
Richard L Meeson, Department of Clinical Science and Services, Queen Mother Hospital for Animals, Royal Veterinary College, University of London, London, UK.
References
- 1. Hill FW. A survey of bone fractures in the cat. J Small Anim Pract 1977; 18: 457-463. [DOI] [PubMed] [Google Scholar]
- 2. Bookbinder PF, Flanders JA. Characteristics of pelvic fracture in the cat. Vet Comp Orthop Traumatol 1992; 37: 122-127. [Google Scholar]
- 3. Voss K, Langley-Hobbs SJ, Montavon PM. Femur. In: Montavon PM, Voss K, Langley-Hobbs SJ. (eds). Feline orthopaedic surgery and musculoskeletal disease. Edinburgh: Saunders Elsevier, 2009, pp 455-474. [Google Scholar]
- 4. Meeson R, Corr S. Management of pelvic trauma: neurological damage, urinary tract disruption and pelvic fractures. J Feline Med Surg 2011; 13: 347-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meeson RL, Geddes AT. Management and long-term outcome of pelvic fractures: a retrospective study of 43 cats. J Feline Med Surg 2017; 19: 36-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Adamantos S, Corr S. Emergency care of the cat with multi-trauma. In Pract 2007; 29: 388-396. [Google Scholar]
- 7. Aldrich J. Assessment and diagnosis of shock. In: King LG, Boag A. (eds). BSAVA manual of canine and feline emergency and critical care. 2nd ed. Gloucester: BSAVA, 2007, pp 17-29. [Google Scholar]
- 8. Aiken M, Barnes D. Are the fabellae bisected by the femoral cortices in a true craniocaudal pelvic limb radiograph? J Small Anim Pract 2014; 55: 465-470. [DOI] [PubMed] [Google Scholar]
- 9. Dudley RM, Kowaleski MP, Drost WT, et al. Radiographic and computed tomographic determination of femoral varus and torsion in the dog. Vet Radiol Ultrasound 2006; 47: 546-552. [DOI] [PubMed] [Google Scholar]
- 10. Tomlinson J, Fox D, Cook JL, et al. Measurement of femoral angles in four dog breeds. Vet Surg 2007; 36: 593-598. [DOI] [PubMed] [Google Scholar]
- 11. Swiderski JK, Radecki SV, Park RD, et al. Comparison of radio-graphic and anatomic femoral varus angle measurements in normal dogs. Vet Surg 2008; 37: 43^8. [DOI] [PubMed] [Google Scholar]
- 12. Bruckner M, Unger M, Spies M. Early clinical experience with a newly designed interlocking nail system-Targon(®) vet. Vet Surg 2016; 45: 754-763. [DOI] [PubMed] [Google Scholar]
- 13. Pinna S, Cella V. Avulsion of the greater trochanter and craniodorsal luxation of the hip joint in a cat: importance of precise radiographic evaluation. Iran J Vet Res 2014; 15: 413-415. [PMC free article] [PubMed] [Google Scholar]
- 14. Fries CL, Binnington AG, Cockshutt JR. Quadriceps contrac-ture in four cats: a complication of internal fixation of femoral fractures. Vet Comp Orthop Traumatol 1988; 1: 91-96. [Google Scholar]
- 15. Taylor J, Tangner CH. Acquired muscle contractures in the dog and cat. A review of the literature and case report. Vet Comp Orthop Traumatol 2007; 20: 79-85. [DOI] [PubMed] [Google Scholar]
- 16. Carberry CA, Flanders JA. Quadriceps contracture in a cat. J Am Vet Med Assoc 1986; 189: 1329. [PubMed] [Google Scholar]
- 17. Vallefuoco R, Le Pommellet H, Savin A, et al. Complications of appendicular fracture repair in cats and small dogs using locking compression plates. Vet Comp Orthop Traumatol 2016; 29: 46-52. [DOI] [PubMed] [Google Scholar]
- 18. Voss K, Kull M, Hassig M, et al. Repair of long-bone fractures in cats and small dogs with the Unilock mandible locking plate system. Vet Comp Orthop Traumatol 2009; 22: 398^05. [DOI] [PubMed] [Google Scholar]
- 19. Hammel SP, Elizabeth Pluhar G, Novo RE, et al. Fatigue analysis of plates used for fracture stabilization in small dogs and cats. Vet Surg 2006; 35: 573-578. [DOI] [PubMed] [Google Scholar]
- 20. Barnhart MD, Rides CF, Kennedy SC, et al. Fracture repair using a polyaxial locking plate system (PAX). Vet Surg 2013; 42: 60-66. [DOI] [PubMed] [Google Scholar]
- 21. Scotti S, Klein A, Pink J, et al. Retrograde placement of a novel 3.5 mm titanium interlocking nail for supracondylar and diaphyseal femoral fractures in cats. Vet Comp Orthop Traumatol 2007; 20: 211-218. [DOI] [PubMed] [Google Scholar]
- 22. Nabholz K, Pozzi A, Schmierer PA, et al. Safety and accuracy of minimally invasive long bone fracture repair using a 2.5-mm interlocking nail: a cadaveric feline study. Vet Comp Orthop Traumatol 2019; 32: 351-361. [DOI] [PubMed] [Google Scholar]
- 23. Bruckner M, Unger M, Spies M. In vitro biomechanical comparison of a newly designed interlocking nail system to a standard DCP. Testing of cat femora in an osteotomy gap model. Tierarztl Prax Ausg K Kleintiere Heimtiere 2014; 42: 79-87. [PubMed] [Google Scholar]
- 24. Fischer HR, Norton J, Kobluk CN, et al. Surgical reduction and stabilization for repair of femoral capital physeal fractures in cats: 13 cases (1998-2002). J Am Vet Med Assoc 2004; 224: 1478-1482. [DOI] [PubMed] [Google Scholar]
- 25. Johnson KA. Section 6: the pelvis and hip joint. In: Johnson KA. (ed). Piermattei’s atlas of surgical approaches to the bones and joints of the dog and cat. 5th ed. St Louis, MO: Elsevier Saunders, 2014, pp 311-365. [Google Scholar]
- 26. Kawamata T, Niiyama M, Taniyama H. Open reduction and stabilisation of coxofemoral joint luxation in dogs and cats, using a stainless steel rope inserted via a ventral approach to the hip joint. Aust Vet J 1996; 74: 460-464. [DOI] [PubMed] [Google Scholar]
- 27. Bennett D. Orthopaedic disease affecting the pelvic region of the cat. J Small Anim Pract 1975; 16: 723-738. [DOI] [PubMed] [Google Scholar]
- 28. Perez-Aparicio FJ, Fjeld TO. Femoral neck fractures and capital epiphyseal separations in cats. J Small Anim Pract 1993; 34: 445-449. [Google Scholar]
- 29. DeCamp CE, Johnston SA, Dejardin LM, et al. Fractures of the femur and patella. In: DeCamp CE, Johnston SA, Dejardin LM, et al. (eds). Brinker, Piermattei and Flo’s handbook of small animal orthopaedics and fracture repair. 5th ed. St Louis, MO: Elsevier, 2016, pp 518-596. [Google Scholar]
- 30. Queen J, Bennett D, Carmichael S, et al. Femoral neck metaphyseal osteopathy in the cat. Vet Rec 1998; 142: 159-162. [DOI] [PubMed] [Google Scholar]
- 31. Smith RN. Fusion of ossification centres in the cat. J Small Anim Pract 1969; 10: 523-530. [DOI] [PubMed] [Google Scholar]
- 32. Perry KL, Fordham A, Arthurs GI. Effect of neutering and breed on femoral and tibial physeal closure times in male and female domestic cats. J Feline Med Surg 2014; 16: 149-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miranda FG, Souza IP, Viegas FM, et al. Radiographic study of the development of the pelvis and hip and the femorotibial joints in domestic cats. J Feline Med Surg 2020; 22: 476^83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Smith GK, Biery DN, Gregor TP. New concepts of coxofemoral joint stability and the development of a clinical stress-radiographic method for quantitating hip joint laxity in the dog. J Am Vet Med Assoc 1990; 196: 59-70. [PubMed] [Google Scholar]
- 35. Craig LE. Physeal dysplasia with slipped capital femoral epiphysis in 13 cats. Vet Pathol 2001; 38: 92-97. [DOI] [PubMed] [Google Scholar]
- 36. Diehm M, Dening R, Dziallas P, et al. Bilateral femoral capital physeal fractures in an adult cat with suspected congenital primary hypothyroidism. Tierarztl Prax Ausg K Kleintiere Heimtiere 2019; 47: 48-54. [DOI] [PubMed] [Google Scholar]
- 37. Borak D, Wunderlin N, Bruckner M, et al. Slipped capital femoral epiphysis in 17 Maine Coon cats. J Feline Med Surg 2017; 19: 13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lafuente P. Young, male neutered, obese, lame? Non-traumatic fractures of the femoral head and neck. J Feline MedSurg 2011; 13: 498-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nappier M, Robertson B, LeRoith T. Acute hindlimb lameness in a 6-month-old cat. J Feline Med Surg 2019; 21: 449-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schwartz G. Spontaneous capital femoral physeal fracture in a cat. Can Vet J 2013; 54: 698-700. [PMC free article] [PubMed] [Google Scholar]
- 41. Burke J. Physeal dysplasia with slipped capital femoral epiphysis in a cat. Can Vet J 2003; 44: 238-239. [PMC free article] [PubMed] [Google Scholar]
- 42. McNicholas WT, Wilkens BE, Blevins WE, et al. Spontaneous femoral capital physeal fractures in adult cats: 26 cases (1996-2001). J Am Vet Med Assoc 2002; 221: 1731-1736. [DOI] [PubMed] [Google Scholar]
- 43. Isola M, Baroni E, Zotti A. Radiographic features of two cases of feline proximal femoral dysplasia. J Small Anim Pract 2005; 46: 597-599. [DOI] [PubMed] [Google Scholar]
- 44. Newton AL, Craig LE. Multicentric physeal dysplasia in two cats. Vet Pathol 2006; 43: 388-390. [DOI] [PubMed] [Google Scholar]
- 45. Culvenor JA, Black AP, Lorkin KF, et al. Repair of femoral capital physeal usuries in cats - 14 cases. Vet Comp Orthop Traumatol 1996; 9: 182-185. [Google Scholar]
- 46. Beale B. Orthopedic clinical techniques femur fracture repair. Clin Tech Small Anim Pract 2004; 19: 134-150. [DOI] [PubMed] [Google Scholar]
- 47. Guerrero TG, Koch D, Montavon PM. Fixation of a proximal femoral physeal fracture in a dog using a ventral approach and two Kirschner wires. Vet Comp Orthop Traumatol 2005; 18: 110-114. [PubMed] [Google Scholar]
- 48. Boekhout-Ta CL, Kim SE, Cross AR, et al. Closed reduction and fluoroscopic-assisted percutaneous pinning of 42 physeal fractures in 37 dogs and 4 cats. Vet Surg 2017; 46: 103-110. [DOI] [PubMed] [Google Scholar]
- 49. Hudson CC, Pozzi A, Lewis DD. Minimally invasive plate osteosynthesis: applications and techniques in dogs and cats. Vet Comp Orthop Traumatol 2009; 22: 175-182. [DOI] [PubMed] [Google Scholar]
- 50. Peirone B, Rovesti GL, Baroncelli AB, et al. Minimally invasive plate osteosynthesis fracture reduction techniques in small animals. Vet Clin North Am Small Anim Pract 2012; 42: 873-895. [DOI] [PubMed] [Google Scholar]
- 51. Palmer RH, Hulse DA, Hyman WA, et al. Principles of bone healing and biomechanics of external skeletal fixation. Vet Clin North Am Small Anim Pract 1992; 22: 45-68. [DOI] [PubMed] [Google Scholar]
- 52. Schmierer PA, Pozzi A. Guidelines for surgical approaches for minimally invasive plate osteosynthesis in cats. Vet Comp Orthop Traumatol 2017; 30: 272-278. [DOI] [PubMed] [Google Scholar]
- 53. Guiot LP, Dejardin LM, Guillou RP. Overview of minimally invasive osteosynthesis principles. In: Johnston SA, Tobias KM. (eds). Veterinary surgery: small animal. 2nd ed. St Louis, MO: Elsevier, 2018, pp 721-736. [Google Scholar]
- 54. Johnson KA. Section 7: the hindlimb. In: Johnson KA. (ed). Piermattei’s atlas of surgical approaches to the bones and joints of the dog and cat. 5th ed. St Louis, MO: Elsevier Saunders, 2014, pp 368458. [Google Scholar]
- 55. Bone LB. Indirect fracture reduction: a technique for minimizing surgical trauma. J Am Acad Orthop Surg 1994; 2:247-254. [DOI] [PubMed] [Google Scholar]
- 56. Heitemeyer U, Kemper F, Hierholzer G, et al. Severely comminuted femoral shaft fractures: treatment by bridging-plate osteosynthesis. Arch Orthop Trauma Surg 1987; 106: 327-330. [DOI] [PubMed] [Google Scholar]
- 57. Harper TAM. Femoral head and neck excision. Vet Clin North Am Small Anim Pract 2017; 47: 885-897. [DOI] [PubMed] [Google Scholar]
- 58. Yap FW, Dunn AL, Garcia-Fernandez PM, et al. Femoral head and neck excision in cats: medium- to long-term functional outcome in 18 cats. J Feline Med Surg 2015; 17: 704-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Witte PG, Scott HW, Tonzing MA. Preliminary results of five feline total hip replacements. J Small Anim Pract 2010; 51: 397-402. [DOI] [PubMed] [Google Scholar]
- 60. Liska WD, Doyle N, Marcellin-Little DJ, et al. Total hip replacement in three cats: surgical technique, short-term outcome and comparison to femoral head ostectomy. Vet Comp Orthop Traumatol 2009; 22: 505-510. [DOI] [PubMed] [Google Scholar]
- 61. Liska WD, Doyle ND, Schwartz Z. Successful revision of a femoral head ostectomy (complicated by postoperative sciatic neurapraxia) to a total hip replacement in a cat. Vet Comp Orthop Traumatol 2010; 23: 119-123. [DOI] [PubMed] [Google Scholar]
- 62. Kalis RH, Liska WD, Jankovits DA. Total hip replacement as a treatment option for capital physeal fractures in dogs and cats. Vet Surg 2012; 41: 148-155. [DOI] [PubMed] [Google Scholar]
- 63. Schiller TD. BioMedtrix total hip replacement systems: an overview. Vet Clin North Am Small Anim Pract 2017; 47: 899-916. [DOI] [PubMed] [Google Scholar]
- 64. Fitzpatrick N, Pratola L, Yeadon R, et al. Total hip replacement after failed femoral head and neck excision in two dogs and two cats. Vet Surg 2012; 41: 136-142. [DOI] [PubMed] [Google Scholar]
- 65. Radke H, Aron DN, Applewhite A, et al. Biomechanical analysis of unilateral external skeletal fixators combined with IM-Pin and without IM-Pin using finite-element method. Vet Surg 2006; 35: 15-23. [DOI] [PubMed] [Google Scholar]
- 66. Stigen O. Supracondylar femoral fractures in 159 dogs and cats treated using a normograde intramedullary pinning technique. J Small Anim Pract 1999; 40: 519-523. [DOI] [PubMed] [Google Scholar]
- 67. Niederhauser SK, Tepic S, Weber UT. Effect of screw position on single cycle to failure in bending and torsion of a locking plate-rod construct in a synthetic feline femoral gap model. Am J Vet Res 2015; 76: 402-410. [DOI] [PubMed] [Google Scholar]
- 68. Vedrine B, Gerard F. Veterinary cuttable plate in a plate-rod construct for repair of diaphyseal femoral fractures in the cat. Vet Comp Orthop Traumatol 2018; 31: 479-487. [DOI] [PubMed] [Google Scholar]
- 69. Hulse D, Hyman W, Nori M, et al. Reduction in plate strain by addition of an intramedullary pin. Vet Surg 1997; 26: 451-459. [DOI] [PubMed] [Google Scholar]
- 70. Konning T, Maarschalkerweerd RJ, Endenburg N, et al. A comparison between fixation methods of femoral diaphyseal fractures in cats - a retrospective study. J Small Anim Pract 2013; 54: 248-252. [DOI] [PubMed] [Google Scholar]
- 71. Reems MR, Beale BS, Hulse DA. Use of a plate-rod construct and principles of biological osteosynthesis for repair of diaphyseal fractures in dogs and cats: 47 cases (1994-2001). J Am Vet Med Assoc 2003; 223: 330-335. [DOI] [PubMed] [Google Scholar]
- 72. Worth AJ. Management of fractures of the long bones of eight cats using external skeletal fixation and a tied-in intra-medullary pin with a resin-acrylic bar. N Z Vet J 2007; 55: 191-197. [DOI] [PubMed] [Google Scholar]
- 73. Langley-Hobbs SJ, Carmichael S, McCartney W. Use of external skeletal fixators in the repair of femoral fractures in cats. J Small Anim Pract 1996; 37: 95-101. [DOI] [PubMed] [Google Scholar]
- 74. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury 2003; 34 Suppl 2: B63-76. [DOI] [PubMed] [Google Scholar]
- 75. Wagner M. General principles for the clinical use of the LCP. Injury 2003; 34 Suppl 2: B31-42. [DOI] [PubMed] [Google Scholar]
- 76. Frigg R. Locking compression plate (LCP). An osteo-synthesis plate based on the dynamic compression plate and the point contact fixator (PC-Fix). Injury 2001; 32 Suppl 2: 63-66. [DOI] [PubMed] [Google Scholar]
- 77. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 2002; 84: 1093-1110. [DOI] [PubMed] [Google Scholar]
- 78. Stoffel K, Dieter U, Stachowiak G, et al. Biomechanical testing of the LCP - how can stability in locked internal fixators be controlled? Injury 2003; 34 Suppl 2: B11-19. [DOI] [PubMed] [Google Scholar]
- 79. Pearson T, Glyde MR, Day RE, et al. The effect of intramedullary pin size and plate working length on plate strain in locking compression plate-rod constructs under axial load. Vet Comp Orthop Traumatol 2016; 29: 451-458. [DOI] [PubMed] [Google Scholar]
- 80. Palierne S, Froidefond B, Swider P, et al. Biomechanical comparison of two locking plate constructs under cyclic loading in four-point bending in a fracture gap model: two screws versus three screws per fragment. Vet Comp Orthop Traumatol 2019; 32: 59-66. [DOI] [PubMed] [Google Scholar]
- 81. Marturello DM, Perry KL, Dejardin LM. Clinical application of the small I-Loc interlocking nail in 30 feline fractures: a prospective study. Vet Surg 2021; 50: 588-599. [DOI] [PubMed] [Google Scholar]
- 82. Diaz-Bertrana MC, Durall I, Puchol JL, et al. Interlocking nail treatment of long-bone fractures in cats: 33 cases (1995-2004). Vet Comp Orthop Traumatol 2005; 18: 119-126. [PubMed] [Google Scholar]
- 83. Larin A, Eich CS, Parker RB, et al. Repair of diaphyseal femoral fractures in cats using interlocking intramedullary nails: 12 cases (1996-2000). J Am Vet Med Assoc 2001; 219: 1098-1104. [DOI] [PubMed] [Google Scholar]
- 84. Duhautois B. Use of veterinary interlocking nails for diaphy-seal fractures in dogs and cats: 121 cases. Vet Surg 2003; 32: 8-20. [DOI] [PubMed] [Google Scholar]
- 85. Horstman CL, Beale BS, Conzemius MG, et al. Biological osteosynthesis versus traditional anatomic reconstruction of 20 long-bone fractures using an interlocking nail: 1994-2001. Vet Surg 2004; 33: 232-237. [DOI] [PubMed] [Google Scholar]
- 86. Dejardin LM, Cabassu JB, Guillou RP, et al. In vivo biomechan-ical evaluation of a novel angle-stable interlocking nail design in a canine tibial fracture model. Vet Surg 2014; 43: 271-281. [DOI] [PubMed] [Google Scholar]
- 87. von Pfeil DJ, Dejardin LM, DeCamp CE, et al. In vitro biome-chanical comparison of a plate-rod combination-construct and an interlocking nail-construct for experimentally induced gap fractures in canine tibiae. Am J Vet Res 2005; 66: 1536-1543. [DOI] [PubMed] [Google Scholar]
- 88. Basinger RR, Suber JT. Two techniques for supplementing interlocking nail repair of fractures of the humerus, femur, and tibia: results in 12 dogs and cats. Vet Surg 2004; 33: 673-680. [DOI] [PubMed] [Google Scholar]
- 89. Marturello DM, von Pfeil DJF, Dejardin LM. Mechanical comparison of two small interlocking nails in torsion using a feline bone surrogate. Vet Surg 2020; 49: 380-389. [DOI] [PubMed] [Google Scholar]
- 90. Macedo AS, Moens NM, Runciman J, et al. Ex vivo torsional properties of a 2.5 mm veterinary interlocking nail system in canine femurs. Comparison with a 2.4 mm limited contact bone plate. Vet Comp Orthop Traumatol 2017; 30: 118-124. [DOI] [PubMed] [Google Scholar]
- 91. Marturello DM, von Pfeil DJF, Dejardin LM. Evaluation of a feline bone surrogate and in vitro mechanical comparison of small interlocking nail systems in mediolateral bending. Vet Comp Orthop Traumatol 2021; 34: 223-233. [DOI] [PubMed] [Google Scholar]
- 92. Fauron AH, Dejardin LM, Phillips R, et al. Clinical application of the I-LOC angle-stable interlocking nail in 100 traumatic fractures of the humerus, femur and tibia. Vet Comp Orthop Traumatol 2018; 31: A1-A25.30060271 [Google Scholar]
- 93. Harari J. Complications of external skeletal fixation. Vet Clin North Am Small Anim Pract 1992; 22: 99-107. [DOI] [PubMed] [Google Scholar]
- 94. Beever L, Giles K, Meeson R. Postoperative complications associated with external skeletal fixators in cats. J Feline Med Surg 2017; 19: 727-736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Black PA, Withrow SJ. Changes in the proximal femur and coxofemoral joint following intramedullary pinning of diaphyseal fractures in young dogs. Vet Surg 1979; 8: 19-24. [Google Scholar]
- 96. Cabassu J. Minimally invasive plate osteosynthesis using fracture reduction under the plate without intraoperative fluo-roscopy to stabilize diaphyseal fractures of the tibia and femur in dogs and cats. Vet Comp Orthop Traumatol 2019; 32: 475^82. [DOI] [PubMed] [Google Scholar]
- 97. Dorea HC, McLaughlin RM, Cantwell HD, et al. Evaluation of healing in feline femoral defects filled with cancellous autograft, cancellous allograft or Bioglass. Vet Comp Orthop Traumatol 2005; 18: 157-168. [PubMed] [Google Scholar]
- 98. McCartney WT, MacDonald BJ. Incidence of non-union in long bone fractures in 233 cats. Int J Appl Res Vet Med 2006; 4: 209-212. [Google Scholar]
- 99. Conte A, Addison E. Management of severe stifle trauma: 2. Periarticular fractures. J Feline Med Surg 2019; 21: 633-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Harasen G. Fractures involving the distal extremity of the femur: part 2 - the mature patient. Can Vet J 2002; 43: 131-132. [PMC free article] [PubMed] [Google Scholar]
- 101. Whitney WO, Schrader SC. Dynamic intramedullary crosspinning technique for repair of distal femoral fractures in dogs and cats: 71 cases (1981-1985). J Am Vet Med Assoc 1987; 191: 1133-1138. [PubMed] [Google Scholar]
- 102. Field MR, Butler R, Wills RW, et al. Retrospective evaluation of perioperative and short term clinical outcomes in appendic-ular long bone skeleton fractures repaired via the string of pearls (SOP) locking plate system. BMC Vet Res 2018; 14: 386. DOI: 10.1186/s12917-018-1707-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Farese JP, Lewis DD, Cross AR, et al. Use of IMEX SK-circular external fixator hybrid constructs for fracture stabilization in dogs and cats. J Am Anim Hosp Assoc 2002; 38: 279-289. [DOI] [PubMed] [Google Scholar]
- 104. Klause SE, Schwarz PD, Egger EL, et al. A modification of the unilateral type I external skeletal fixator configuration for primary or secondary support of supracondylar humeral and femoral fractures. Vet Comp Orthop Traumatol 1990; 3: 130-134. [Google Scholar]
- 105. Chico AC, Font J, Marti JM. Trochlear femoral fractures in cats: results of seven cases. Vet Comp Orthop Traumatol 2001; 14: 51-55. [Google Scholar]
- 106. Harasen G. Fractures involving the distal extremity of the femur. Part 1 - the immature patient. Can Vet J 2001; 42: 949-950. [PMC free article] [PubMed] [Google Scholar]
- 107. Spangberg C, Spangberg IB, Bergstrom A. Stainless steel wire in a figure-of-eight for repair of distal femoral physeal fractures in ten cats: a case report. J Vet Sci 2019; 20: e71. DOI: 10.4142/jvs.2019.20.e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Campbell JR. The technique of fixation of fractures of the distal femur using Rush pins. J Small Anim Pract 1976; 17: 323-329. [DOI] [PubMed] [Google Scholar]
- 109. Sukhiani HR, Holmberg DL. Ex vivo biomechanical comparison of pin fixation techniques for canine distal femoral physeal fractures. Vet Surg 1997; 26: 398^07. [DOI] [PubMed] [Google Scholar]
- 110. Rubinos C, Meeson RL. Traumatic physeal fractures in cats: a review of 36 cases (2010-2020). J Feline Med Surg 2022; 24: 98-106. [DOI] [PMC free article] [PubMed] [Google Scholar]