Abstract
Objectives
The objective of this study was to report the surgical outcome and complication rate of deep traction avulsion (TA) of feline aural inflammatory polyps after a lateral approach (LA) to the ear canal.
Methods
This was a retrospective analysis of data retrieved from an electronic database of 62 cats treated with TA after an LA (TALA) for removal of ear canal polyps. Long-term outcome was assessed via a telephone questionnaire survey with the owners.
Results
Domestic shorthair cats (48%) and Maine Coons (37%) were over-represented. The most common presenting clinical signs were otorrhoea, ear scratching and head shaking. Video-otoscopic examination confirmed a polypous mass in the ear canal in all patients. All 62 cats underwent TALA, with a mean surgical time of 33 mins for experienced surgeons (n = 4) and 48 mins (n = 12) for less experienced surgeons. The recurrence rate of polyp regrowth for experienced surgeons was 14.3% vs 35% for the less experienced surgeons. Postoperative complications included Horner’s syndrome (11.5%) and facial nerve paralysis (3%). Otitis interna was not observed.
Conclusions and relevance
A lateral approach to the ear canal in combination with deep TA of an aural inflammatory polyp is an effective first-line technique that results in a low recurrence and complication rate.
Introduction
Middle ear polyps in cats are relatively common benign masses that arise from the mucosal lining of the middle ear, Eustachian tube or the nasopharynx.1–5 Whereas many cats will not demonstrate any specific clinical signs associated with middle ear polyps, extension of the polyps beyond the boundaries of the middle ear leads to signs of otitis externa, otitis interna or nasopharyngitis. Diagnosis of polyps is relatively straightforward when polyps have protruded into the ear canal or into the nasopharynx where they can easily be demonstrated using otoscopy and nasopharyngoscopy. Advanced imaging in the form of CT or MRI is advised for cats that have disease confined to the middle ear cavity, and have concomitant nasal disease or otitis interna.6–15
The treatment of middle ear polyps that have protruded beyond the middle ear cavity is surgical in all cases. Described techniques for polyp removal from the ear canal include traction avulsion (TA), ventral bulla osteotomy, lateral ear resection and total ear canal ablation with lateral bulla osteotomy, although the latter two techniques are not commonly advised.1–3,16–20 TA is the least invasive technique, yet has the highest documented recurrence rate (up to 50%).1,17 Recently, however, better results have been reported using a per-endoscopic transtympanic traction technique, which resulted in polyp recurrence in only 13.5% of the 37 cats treated. Complications are minimal with these techniques. 21 A ventral bulla osteotomy (VBO) is the most invasive technique with the highest associated complication risks but with the lowest recurrence rates (0–8%).1,16,17,20,22 In one relatively large study with 19 cats treated with VBO, reported postoperative complications included Horner’s syndrome (n = 11), otitis interna (n = 2) and facial nerve paralysis (n = 5), and the recurrence rate was 3–5%. 20 Venker-van Haagen introduced TA after a lateral approach (LA) to the ear canal (TALA) as a simple, quick and effective method bypassing complications seen with VBO and generally leading to a low recurrence rate. 5 Whereas this technique has been used for decades, postoperative complications, long-term outcome and recurrence rates using this technique have so far not been reported in the veterinary literature. Therefore, the aim of the present study was to report epidemiological data, clinical signs, postoperative complications and long-term surgical outcomes of TALA for removal of middle ear polyps.
Materials and methods
Animals and data collection
Data from all cats treated surgically by a lateral approach at our department between December 2004 and June 2014 were collected retrospectively from an electronic database. Information collected included age, breed, sex, clinical signs, findings during initial physical examination, otoscopic findings, diagnostic imaging results, surgeons performing the procedure, results of histopathology and follow-up examinations. Patients were excluded from this study if digital files were incomplete or patients were lost to follow-up.
Surgery
Preoperative protocol for all cats consisted of a thorough otoscopic examination to determine the presence of a visible polyp on the affected site.
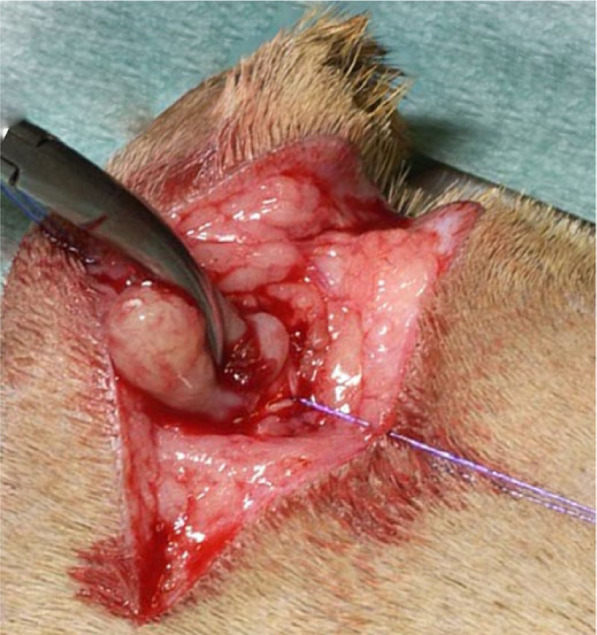
After aseptic preparation of the surgical site, an incision was made in the skin in a dorsoventral direction over the palpable vertical ear canal, starting just cranioventral to the tragus over approximately 2.5 cm.5,23 The subcutaneous tissues were dissected with small scissors to free the cartilage of the vertical ear canal to the level of the junction between the auricular and annular cartilages, reflecting the parotid gland. A vertical stab incision was made ventrally to dorsally in the auricular cartilage just above this junction with a Bard Parker scalpel handle with a no. 11 blade over 7–10 mm.5,23 Stay sutures were placed on both sides of the incision in the ear canal cartilage with fine monofilament suture material to increase visualisation and avoid damaging the cartilage. Small closed curved haemostatic forceps were then introduced into the ear canal, meticulously following the direction of the horizontal ear canal until the polyp was encountered. The forceps were then opened and advanced deeper over the polyp until it could be grasped as close as possible to the osseous meatus (Figure 1). When a firm grip had been achieved, the forceps were gently rotated to make sure no other tissue than the polyp itself had been grasped and traction was applied until the polyp avulsed from its origin (Figure 2). With complete removal of a classical middle ear inflammatory polyp, a small stalk at the base of the polyp could usually be identified. The middle ear cavity was flushed with warm saline and with a small curette the osseous meatus and most lateral aspect of the tympanic cavity was ‘palpated’ to check for additional inflammatory tissue, which was removed with this curette when encountered. 23 The stay sutures were removed and the cartilage of the ear canal was closed with 4-0 monofilament suture material in an interrupted pattern; three or four sutures were usually sufficient. The subcutis was closed in a continuous pattern with 4-0 absorbable monofilament material and the skin was closed in a subdermal suture pattern using the same material.
Figure 1.

The forceps is gently rotated while grasping the aural polyp to make sure no other tissue has been grasped
Figure 2.
Traction is applied until the polyp avulses
Postoperative management consisted of amoxicillin-clavulanic acid (Synulox; Pfizer Animal Health) or enrofloxacin (Baytril; Bayer Animal Health) for 7 days for cats without clinical signs of otitis interna and for 14–21 days for those presenting with signs of otitis interna, and meloxicam (Metacam cat; Boehringer Ingelheim) for 5 days. No corticosteroids were administrated.
Questionnaire
Each owner was contacted by telephone at least 6 months after intervention (follow-up 6 months to 10 years) and asked the following questions: (1) recovery time after surgery (estimated number of weeks for clinical signs to disappear completely: 1–2, 2–3, 3–4, 5–10, >10 weeks); (2) presence of postsurgical residual signs (head tilt, ataxia, anorexia, otorrhoea, ear scratching, head shaking, facial nerve paralysis and Horner’s syndrome); (3) clinical signs fitting with recurrence of polyp growth after initial full recovery; (4) overall owner satisfaction as evaluated on a 1–4 analogue scale (1 = displeased, 4 = very satisfied). Medical terminology was explained during the conversation with the owner.
Statistical analysis
Collected data were statistically analysed using SPSS software (V.20.0; IBM). A Kaplan–Meier was performed to evaluate the disease free interval. Cox regression analysis was preformed to evaluate significant differences (P <0.05) between variables.
Results
Epidemiological data
Ninety-two cats met the inclusion criteria, but only 62 owners were willing to participate in this retrospective study. Domestic shorthair cats and Maine Coons were over-represented in our population, 48% (30/62) and 37% (23/62), respectively. Other breeds that were presented more than once included the Norwegian Forest Cat (2/62; 3%) and the Oriental Shorthair (2/62; 3%). The mean age of affected cats was 3.9 years (range 0.5–14 years) with a median of 2 years. There were 27 (44%) female cats, 81% of which were neutered, and 35 (56%) male cats of which 80% were neutered.
Clinical signs and imaging results
Presenting clinical signs related to the presence of an ear polyp are listed in Table 1. The most common clinical signs were otorrhoea, ear scratching and head shaking. Signs such as ataxia, anorexia, Horner’s syndrome and deafness were rarely seen. Diagnostic imaging in the form of a CT scan was performed in 16/62 cats included in this study. Eight cats underwent CT as part of the initial work-up prior to surgery and 10 when presented with signs of recurrence (including two that had CT previously, at initial work-up). Only the first CT scan (16 cats) results were reviewed for this study. A soft tissue opacity within the tympanic bulla was seen in all cases, with additional osseous changes/thickening of the bulla wall in 9/16. Extension of soft tissue opacity from the middle ear through the external bony meatus into the ear canal was seen in 12/16 cases. In one cat the soft tissue opacity extended to the level of the external bony meatus and in three cats this specific information could not be retrieved. In six cats, in addition to the middle ear and ear canal abnormalities reported above, a protrusion of polypous tissue towards the nasopharynx was diagnosed, based on the presence of a soft tissue opacity at the level of the Eustachian tube opening in the nasopharynx (9.7%).
Table 1.
Preoperative clinical signs in 62 cats with a middle ear polyp
| Clinical signs | |
|---|---|
| Head tilt | 20 (32) |
| Ataxia | 16 (26) |
| Anorexia | 3 (5) |
| Otorrhoea | 55 (89) |
| Ear scratching | 40 (65) |
| Head shaking | 42 (68) |
| Deafness | 10 (16) |
| Horner’s syndrome | 1 (2) |
Data are n (%)
Outcome
No complications were encountered during surgery in all cases. Postoperative complications included Horner’s syndrome in seven cases and facial nerve paralysis in two. Vestibular signs were not observed. All patients were discharged from the hospital.
Forty-seven (75.8%) cat owners indicated that their cats had completely recovered following surgery and were not exhibiting any residual signs. Clinical signs had disappeared within 1–3 weeks in 91% of these animals, with a mean of 2.6 weeks. In six of the 47 (12.7%) cats that made an initial full recovery after the surgery, clinical signs compatible with possible recurrence of polyp growth developed 12, 21, 23, 34, 41 and 101 months postoperatively, respectively. For these late recurrences the median disease-free interval was 27.5 months. All cats were re-examined at our institution and a new polyp in the external ear canal was confirmed in four cats and otitis media in two of these cats using CT and/or video-otoscopy.
Owners of 15 cats (24.2%) reported that their cats had not fully recovered. In these cats clinical signs such as otorrhoea, head shaking and ear scratching persisted postoperatively beyond 4 weeks. Recurrence of (or residual) polyp growth was confirmed at re-examination in our clinic using CT scan and/or video-otoscopy in 8/15 (53%) cases. Of the other seven cats with persisting clinical signs after surgery two owners declined further work-up and five cats were lost to follow-up.
Auxiliary surgery in the cats with confirmed regrowth of polyps consisted of polyp removal via TA under video-otoscopic guidance (3/12), VBO (7/12) or a second lateral approach as described above (2/12).
An experienced ear, nose and throat surgeon had performed the polyp removal in 40 cats included in this study. In the remainder of the cases (n = 22), the procedure had been carried out by a less experienced surgeon (resident). Mean surgical time was 33 mins for experienced surgeon and 48 mins for the less experienced surgeon.
There were no significant differences in recurrence rates between the experienced surgeon, (average recurrence rate was 14.3% vs 35% for the less experienced surgeon). The cats with confirmed recurrences (n = 13) included seven domestic shorthairs, five Maine Coons and one Birman. Recurrence was seen in six females (6/27; 22%) vs seven male cats (7/35; 20%). There were no significant differences in recurrence rates between males and females, and neutered and intact cats.
A Kaplan–Meier analysis was performed to evaluate the time between surgery and recurrence of polyp growth (disease-free interval) (Figure 3). For this purpose, a time frame between surgery (t = 0) and the time of recurrence of polyp growth, or the time at which the case was censored was used. Cases were censored when recurrence of polyp growth did not occur (48 cats). At 1 year 97% and at 2 years 88% of the cats had survived without recurrence of a polyp. Histopathological examination was performed in 39 cases (including 10 of the 12 recurrences) and confirmed the presence of an inflammatory polyp in all.
Figure 3.
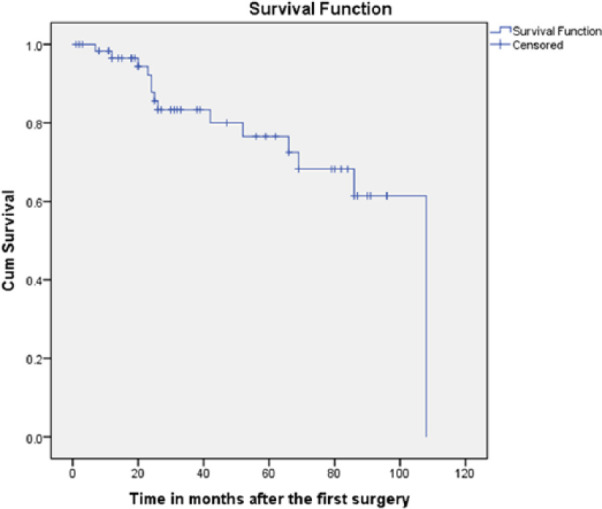
Kaplan–Meier curve of disease-free interval in months
Discussion
The aim of this study was to evaluate the efficacy, long-term outcome of and complications associated with TALA of aural inflammatory polyps in cats.
The current study demonstrates that TALA of an aural polyp is a time-efficient surgical technique, associated with an uneventful postoperative recovery, minor postoperative complications and a low recurrence rate of 14% for experienced surgeons. Although the surgery is relatively easy to perform, a learning curve is associated with the technique as both surgical time and recurrence rates depend on the experience of the surgeon.
No apparent breed or sex predilection has been reported for aural polyps, but it has been noted by many authors that polyp formation is more commonly seen in specific cat breeds like the Norwegian Forest, Sphynx, Maine Coon, Persian, Ragdoll and Abyssinian.1–3,18,24,25 Similar to what has been reported before, domestic shorthair cats were over-represented in our study.1,21,25–28 In contrast to previous publications, however, the Maine Coon was also over-represented (37%). Although this confirms previous anecdotal evidence, further research is needed to see if this reflects a bias in our study population or truly reflects a breed predisposition.
The mean age at presentation, male–female distribution and the most common clinical findings (ie, otorrhoea, head shaking and ear scratching) were similar to those that have been previously reported.1,2,5,20,21,24,26 Clinical signs associated with otitis interna (ie, vestibular ataxia, anorexia and deafness) were less commonly seen in our study compared with previous reports. 4 Only 16 cats presented with ataxia in our study, which resolved in all cats after surgical removal of the polyp and consecutive antibiotic treatment. Prognosis of animals presenting with vestibular signs did not appear to be worse than that of those presenting without. Recurrence rates were similar for both groups.
Advanced diagnostic imaging was not performed in most animals included in this study and diagnosis was confirmed by (video-)otoscopy in all cases with subsequent histopathological evaluation in 60% of these. In most of the cases where recurrence was suspected, advanced diagnostic imaging was performed. Even though polyps can be visualised on radiographs in many cases,18,24,25,29 for proper (surgical) treatment planning, CT of the entire skull is advised. CT also offers a higher true-positive diagnostic rate for the detection of otitis media, otitis interna and provides information on concomitant changes in the nasal cavity, nasopharynx and frontal sinuses.30,31 Findings on diagnostic imaging in our population were similar to changes associated with ear canal and middle ear polyps reported before. Eight patients received a CT before the initial surgery and involvement of the middle ear was demonstrated in all. Only three of these eight cats developed a recurrence of the polyp, despite obvious changes in the middle ear. Whereas definite conclusions cannot be drawn based on our data, it does suggest that despite middle ear involvement on CT imaging TALA is usually curative. Further studies specifically designed to evaluate the use of CT as a predictor of outcome after TALA are required in a larger population. Diagnostic imaging such as CT, based on our results, is advised for cats that require more elaborate surgical procedures such as ventral bulla osteotomy or present with recurrence after polyp removal.
In this study histopathological confirmation of the diagnosis was, unfortunately, only performed in 63% of the cases. Although this would have ideally been performed in all cases, especially in the older animals,3,24–26 the absence of recurrence of signs after removal of the mass in the ear canal indicates the presumptive diagnosis was correct. However, this clearly presents a limitation inherent to the retrospective study design. As a general rule, histopathology should be performed for accurate diagnosis in all cases. Histopathology was performed in 83% of the animals that presented with recurrence, which confirmed the diagnosis of inflammatory polyp in all.
TA and VBO have been the most commonly used techniques for treatment of aural inflammatory polyps. VBO is associated with a low recurrence rate (0–8%) but is more invasive and is associated with a higher incidence of iatrogenic complications (Horner’s syndrome, facial nerve paralysis, otitis interna). 20 In this study TALA was used as a first-choice treatment for all cases with ear canal polyps visible upon otoscopy, regardless of imaging results, indicating middle ear involvement or clinical signs indicative of otitis interna. This technique resulted in a much lower recurrence rate of 14.3% compared with other described TA techniques (around 50% recurrence) and a similar recurrence rate as per-endoscopic transtympanic TA (PTT). Whereas recurrence rates are higher than reported for VBO, TALA is easy to perform, efficient and not associated with major complications (ie, bleeding, facial nerve paralysis). Another major advantage of this lateral approach is the short anaesthetic and surgical time compared with previously described surgical techniques. The average surgical time amounted to only 33 mins for experienced ear, nose and throat surgeons, and 48 mins for less experienced surgeons. The study on PTT reported a minimal surgery duration of 45 mins and a maximum of 2.5 h. 21 Although the latter is a minimally invasive technique associated with minor complications, the present study proved to have similar results in outcome and complication rates with a significantly shorter surgical time and without the need for endoscopic equipment.
TALA is associated with minor complications of transient nature. Peri- and postoperative bleeding, and vestibular signs upon recovery were not noted in any of the cats. Horner’s syndrome was seen in seven cats (11.5%). Two cats developed postoperative facial nerve paralysis, one of which had resolved at the time of follow-up. The other cat was lost to follow-up. An inexperienced resident performed the surgeries in the latter two cats and facial nerve damage could have resulted from inadvertent ventral dissection beyond the level of the transition between vertical and horizontal ear canal. Owing to the retrospective nature of this study, it is possible that some minor complications (ie, Horner’s syndrome) were under-reported. Major complications including otitis interna and/or facial nerve paralysis most likely would have been reported. The number of complications appears comparable with previous reports on TA techniques, including the PTT study where three cats (8%) developed Horner’s syndrome, 25 but is much higher after VBO. Horner’s syndrome is observed in 25–80% of the cases,26,32 and vestibular signs after VBO range from 4–42%.16,17 Facial nerve paralysis was seen in 16% of 18 procedures, 24 but when accompanied by total ear canal ablation the incidence can increase up to 31%. 33 In contrast to vestibular symptoms and/or facial nerve paralysis, Horner’s syndrome is considered only a mild complication. The condition does not affect quality of life and often resolves in 2–4 weeks. 26
Recurrence of polyp growth was seen in 13 cats of the 62 included in this study. The choice between a lateral approach and a VBO for revisional surgery was made based on the size of the polyp and the owners preferences. Very small polyps that barely extend beyond the external bony meatus are difficult to grasp using the lateral approach. For polyps properly protruding beyond the external bony meatus, a lateral approach can be repeated. For very small polyps, a VBO is advised, especially when dealing with possibly multiple small polyps confined to the middle ear cavity.
Conclusions
Inflammatory polyps in the ear canal and middle ear are frequently encountered in cats. Whereas diagnosis relies heavily on visualisation of a polypous growth in the ear canal during otoscopy, advanced imaging such as CT can be a useful aid. First-line treatment for removal of polyps can consist of a lateral approach to the ear canal in combination with TA of the polyp. This study demonstrates this is an effective, fast and inexpensive technique that results in a low recurrence and complication rate. The technique can be performed by first-line practitioners but is associated with a higher recurrence rate if not performed by a surgeon familiar with the technique.
Acknowledgments
We would like to acknowledge Sharon Rook for her assistance with study data retrieval. Further, we would like to acknowledge Dr Jan van den Broek for his assistance in the statistical analysis.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Accepted: 16 June 2016
Sara Janssens received the 2016 JFMS Resident Best Paper Award for this study.
References
- 1. Anderson DM, Robinson RK, White RA. Management of inflammatory polyps in 37 cats. Vet Rec 2000; 147: 684–687. [PubMed] [Google Scholar]
- 2. Fan TM, de Lorimier LP. Inflammatory polyps and aural neoplasia. Vet Clin North Am Small Anim Pract 2004; 34: 489–509. [DOI] [PubMed] [Google Scholar]
- 3. Pope ER. Feline inflammatory polyps. Semin Vet Med Surg (Small Anim) 1995; 10: 87–93. [PubMed] [Google Scholar]
- 4. Haar Ter G. Inner ear dysfunction related to ear disease in dogs and cats. Eur J Companion Anim Pract 2006; 16: 127–136. [Google Scholar]
- 5. Venker-van Haagen A. The ear. In: Venker-van Haagen A. (eds). Ear, nose, throat, and tracheobronchial diseases in dogs and cats. Hannover: Schlütersche, 2005, pp 1–50. [Google Scholar]
- 6. Allgoewer I, Lucas S, Schmitz SA. Magnetic resonance imaging of the normal and diseased feline middle ear. Vet Radiol Ultrasound 2000; 41: 413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barthez PY, Koblik PD, Hornof WJ, et al. Apparent wall thickening in fluid filled versus air filled tympanic bulla in computed tomography. Vet Radiol Ultrasound 1996; 37: 95–98. [Google Scholar]
- 8. Dayrell-Hart BL. MR imaging of the vestibular apparatus of the dog. In: Proceedings 15th ACVIM Forum, 1997, May 22–25, Orlando, FL: American College of Veterinary Internal Medicine, 1997, pp 606–607. [Google Scholar]
- 9. Dvir E, Kirberger RM, Terblanche AG. Magnetic resonance imaging of otitis media in a dog. Vet Radiol Ultrasound 2000; 41: 46–49. [DOI] [PubMed] [Google Scholar]
- 10. Garosi LS, Lamb CR, Targett MP. MRI findings in a dog with otitis media and suspected otitis interna. Vet Rec 2000; 146: 501–502. [DOI] [PubMed] [Google Scholar]
- 11. Garosi LS, Dennis R, Penderis J, et al. Results of magnetic resonance imaging in dogs with vestibular disorders: 85 cases (1996–1999). J Am Vet Med Assoc 2001; 218: 385–391. [DOI] [PubMed] [Google Scholar]
- 12. Garosi LS, Dennis R, Schwarz T. Review of diagnostic imaging of ear diseases in the dog and cat. Vet Radiol Ultrasound 2003; 44: 137–146. [DOI] [PubMed] [Google Scholar]
- 13. Hoskinson JJ. Imaging techniques in the diagnosis of middle ear disease. Semin Vet Med Surg (Small Anim) 1993; 8: 10–16. [PubMed] [Google Scholar]
- 14. Russo M, Covelli EM, Meomartino L, et al. Computed tomographic anatomy of the canine inner and middle ear. Vet Radiol Ultrasound 2002; 43: 22–26. [DOI] [PubMed] [Google Scholar]
- 15. Seitz SE, Losonsky JM, Marretta SM. Computed tomographic appearance of inflammatory polyps in three cats. Vet Radiol Ultrasound 1996; 37: 99–104. [Google Scholar]
- 16. Faulkner J, Budsberg S. Results of ventral bulla osteotomy for treatment of middle ear polyps in cats. J Am Anim Hosp Assoc 1990; 26: 496–499. [Google Scholar]
- 17. Kapatkin A, Matthiesen D, Noone K, et al. Results of surgery and long-term follow-up in 31 cats with nasopharyngeal polyps. J Am Anim Hosp Assoc 1990; 26: 387–392. [Google Scholar]
- 18. Muilenburg RK, Fry TR. Feline nasopharyngeal polyps. Vet Clin North Am Small Anim Pract 2002; 32: 839–849. [DOI] [PubMed] [Google Scholar]
- 19. Schmidt J, Kapatkin A. Nasopharyngeal and ear canal polyps in the cat. Feline Pract 1990; 18: 16–19. [Google Scholar]
- 20. Trevor PB, Martin RA. Tympanic bulla osteotomy for treatment of middle-ear disease in cats: 19 cases (1984–1991). J Am Vet Med Assoc 1993; 202: 123–128. [PubMed] [Google Scholar]
- 21. Greci V, Vernia E, Mortellaro CM. Per-endoscopic trans-tympanic traction for the management of feline aural inflammatory polyps: a case review of 37 cats. J Feline Med Surg 2014; 16: 645–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bradley R, Noone K, Saunders GK, et al. Nasopharyngeal and middle ear polypoid masses in five cats. Vet Surg 1985; 14: 141–144. [Google Scholar]
- 23. Haar Ter G. Basic principles of surgery of the external ear (pinna and ear canal). In: Kirpensteijn J, Klein WR. (eds). The cutting edge: basic operating skills for the veterinary surgeon. London, UK: Roman House Publishers, 2006, pp 272–283. [Google Scholar]
- 24. Davidson J. Otopharyngeal polyps. In: Bojrab M. (eds). Current techniques in small animal surgery. 4th ed. Philadelphia: Lea & Febiger, 1998, pp 147–150. [Google Scholar]
- 25. Harvey CE, Goldschmidt MH. Inflammatory polypoid growths in the ear canal of cats. J Small Anim Pract 1978; 19: 669–677. [DOI] [PubMed] [Google Scholar]
- 26. Anders BB, Hoelzler MG, Scavelli TD, et al. Analysis of auditory and neurologic effects associated with ventral bulla osteotomy for removal of inflammatory polyps or nasopharyngeal masses in cats. J Am Vet Med Assoc 2008; 233: 580–585. [DOI] [PubMed] [Google Scholar]
- 27. Lane J, Orr C, Lucke V, et al. Nasopharyngeal polyps arising in the middle ear of the cat. J Small Anim Pract 1981; 22: 511–522. [DOI] [PubMed] [Google Scholar]
- 28. Veir JK, Lappin MR, Foley JE, et al. Feline inflammatory polyps: historical, clinical, and PCR findings for feline calici virus and feline herpes virus-1 in 28 cases. J Feline Med Surg 2002; 4: 195–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kirpensteijn J. Aural neoplasms. Semin Vet Med Small Anim 1993; 8: 17–23. [PubMed] [Google Scholar]
- 30. Bischoff MG, Kneller SK. Diagnostic imaging of the canine and feline ear. Vet Clin North Am Small Anim Pract 2004; 34: 437–458. [DOI] [PubMed] [Google Scholar]
- 31. Detweiler DA, Johnson LR, Kass PH, et al. Computed tomographic evidence of bulla effusion in cats with sinonasal disease: 2001–2004. J Vet Intern Med 2006; 20: 1080–1084. [DOI] [PubMed] [Google Scholar]
- 32. Hardie EM. Surgical diseases of the middle ear. In: Monnet E. (eds). Small animal soft tissue surgery. Iowa: John Wiley & Sons, 2012, pp 149–156. [Google Scholar]
- 33. Sharp N. Chronic otitis externa and otitis media treated by total ear canal ablation and ventral bulla osteotomy in thirteen dogs. Vet Surg 1990; 19: 162–166. [DOI] [PubMed] [Google Scholar]


