Abstract
Objectives
This study sought to explore the clinicopathological features and comorbidities of cats with mild, moderate and severe hyperthyroidism in a radioiodine referral population.
Methods
Medical records were reviewed, along with results of serum biochemistry, urinalysis, systolic blood pressure and diagnostic imaging performed at the time of radioiodine referral. Cats were grouped by total thyroxine (TT4) levels as mildly (TT4 60.1–124.9 nmol/l), moderately (TT4 125–250 nmol/l) or severely (TT4 >250 nmol/l) hyperthyroid at the time of diagnosis and referral.
Results
Thirty percent (42/140) of the cats were <10 years old at diagnosis. In 24.3% (34/140), hyperthyroidism was diagnosed incidentally. The time between diagnosis and referral for radioiodine was significantly longer in cats with severe hyperthyroidism at the time of referral (P = 0.004). An increase in severity group between the time of diagnosis and referral occurred in 38.6% (54/140) of cats. At referral, 54.3% (25/46) of cats with mild, 66.7% (42/63) with moderate and 80.6% (25/31) with severe hyperthyroidism were unstable despite ongoing medical or dietary management. The prevalence of cardiac abnormalities was significantly increased in cats with severe hyperthyroidism (P = 0.014) compared with those with mild or moderate hyperthyroidism. There was no significant difference in the likelihood of renal disease (P = 0.708) or hypertension (P = 0.328) between the groups.
Conclusions and relevance
Incidental diagnosis of hyperthyroidism occurs commonly, potentially owing to increased disease screening. Cats with severe hyperthyroidism at referral were more likely to be chronically hyperthyroid with a history of poor stabilisation. This subset of patients was significantly more likely to have cardiac abnormalities. Thyrotoxic cardiomyopathy may ultimately affect patient suitability for curative treatments (radioiodine or thyroidectomy) owing to higher anaesthetic risks and potential for decompensation into congestive heart failure with the stress of travel and hospitalisation. Curative therapy should be considered before the development of severe hyperthyroidism.
Introduction
Hyperthyroidism, the most common feline endocrinopathy, has typically been associated with disease in senior (>10 years old) or geriatric (>15 years old) cats.1,2 It is a progressive condition usually resulting from functional thyroid adenomatous hyperplasia or adenoma.3,4
Feline hyperthyroidism was first reported in 1979; however, knowledge of the condition, its diagnosis and management are continually evolving. 5 It has been hypothesised that the disease is more prevalent now than previously described.6,7 Greater awareness among veterinarians may result in earlier diagnosis and thus reduced severity of clinical signs at initial presentation.1,6 With earlier diagnoses, increasing numbers of cats will likely receive chronic medical (anti-thyroid drugs [methimazole and carbimazole]) or dietary (iodine-restricted diet [IRD]) therapy, 8 resulting in progressive goitre growth and increased severity of hyperthyroidism. 9 The resultant wide spectrum of disease severity, ranging from very early and mild disease to chronic and severe disease, is potentially different to early reports. It is well recognised that various comorbidities occur with hyperthyroidism, including cardiac and renal abnormalities, hypertension and dyspnoea (eg, secondary to respiratory muscle weakness and hypercapnea); however, their frequency in relation to disease severity has not been specifically described. 10
Curative treatments (radioiodine, thyroidectomy) are often pursued only after first-line medical treatment has failed; reasons for failure include poor owner or patient compliance, adverse drug reactions and ever-increasing drug doses necessary to maintain euthyroidism. 11 Radioiodine offers several advantages over thyroidectomy, including an ability to address ectopic thyroid tissue, preservation of parathyroid gland function and lack of anaesthesia requirement. 12 Considered the gold standard, radioiodine therapy resulted in success rates of up to 94% following a single treatment in one study. 13
The aim of the present study was to explore the current spectrum of hyperthyroidism by documenting the clinicopathological features of cats classified as mildly, moderately or severely hyperthyroid in a radioiodine referral population. A secondary aim was to determine the prevalence of concurrent renal and cardiac abnormalities, hypertension and dyspnoea in these groups of cats.
Materials and methods
Criteria for case selection
Medical records for cats undergoing assessment for radioiodine treatment at the Feline Centre, Langford Vets, between January 2009 and May 2013 were reviewed. Hyperthyroidism was diagnosed prior to referral based on a serum total thyroxine (TT4) concentration above the upper limit of the reference interval (RI). Cats were excluded owing to incomplete medical records or blood work, or the presence of significant comorbidities precluding radioiodine treatment.
Procedures
Retrospective data were collected regarding signalment, clinical signs at diagnosis, physical examination findings, previous management for hyperthyroidism (medical, dietary [IRD] or surgical), and TT4 levels at diagnosis and immediately prior to radioiodine treatment (when anti-thyroid medication or IRD had been withdrawn). Cats were classified according to TT4 levels at both time points (diagnosis and referral) as mildly (TT4 60.1–124.9 nmol/l), moderately (TT4 125–250 nmol/l) or severely (TT4 >250 nmol/l) hyperthyroid. 13 It was noted whether hyperthyroidism had been incidentally diagnosed (eg, at vaccination or when investigating another unrelated illness). The time interval between diagnosis and referral for radioiodine treatment was recorded. Additional data collected during radioiodine assessment (performed 4–6 weeks before radioiodine treatment prior to withdrawal of medical or dietary management) were presence of dyspnoea and heart murmur, serum biochemistry (urea and creatinine), urinalysis (urine specific gravity [USG]), systolic blood pressure (SBP) measurements (taken using cat-friendly techniques with a Doppler method in a quiet, isolated room and not at the time of physical examination or blood sampling), abdominal ultrasonography, thoracic radiography and echocardiography findings.
The change in TT4 concentration between diagnosis and referral for individual cats was calculated using TT4 ratios, as multiple laboratories were utilised at diagnosis. The ratio of the TT4 level:upper limit of the RI provided by the laboratory was calculated at both diagnosis and referral (ie, a ratio >1 indicated a TT4 level above the upper RI). The percentage change between these two ratios was determined. Cases were excluded from these analyses if the TT4 value at diagnosis was unknown (ie, recorded as >90 nmol/l).
The presence of comorbidities (cardiac abnormalities, renal disease [chronic kidney disease; CKD], dyspnoea and hypertension) was recorded and relationships between disease severities investigated.
CKD was defined (and staged) according to International Renal Interest Society (IRIS) guidelines based on serum creatinine concentrations, USG and accompanying ultrasonographic evidence of chronic renal changes (chronic degenerative changes, including loss of corticomedullary distinction, reduced renal size or altered renal shape). Serum urea and creatinine concentrations were recorded at the assessment visit (prior to withdrawal of dietary or medical management). Renal azotaemia was defined as a serum creatinine concentration >177 µmol/l in conjunction with inadequate urine-concentrating ability (USG <1.035). 14
Tachycardia was defined as a heart rate of >220 beats per min. The presence of a heart murmur was recorded (severity grading was not included owing to multiple observers and known variability of heart murmur grades in cats). 15 Cardiac abnormalities were defined as echocardiographic or radiographic evidence of cardiomyopathy ± congestive heart failure (CHF). Echocardiography was performed following standard procedure, using a GE vivid 7 and 7.5 or 12 MHz transducer as applicable, by a cardiology certificate (RCVS) and diploma holder. Cats were placed in right and left lateral recumbency with manual restraint. Left ventricular (LV) wall measurements were obtained from the right parasternal long axis five-chamber view in diastole, using the leading edge-to-leading edge method. Cardiomyopathy was defined as diastolic LV wall measurement >6 mm. Left atrial (LA) size was measured from the right-sided parasternal four-chamber view and the right-sided parasternal short-axis view at the level of the aortic valve. LA enlargement was defined as a LA size of >1.5 cm and/or a LA: aortic ratio of >1.5.15,16 A LA diameter of >2.1 cm was considered as severe enlargement. 17 A minimum of three measurements were obtained for each variable, and the average recorded. Pulmonary oedema and/or pleural effusion with associated cardiac changes were suspected to be caused by CHF.
Hypertension was defined as a mean SBP ⩾160 mmHg measured on two or more separate occasions. 18 Dyspnoea was defined as difficult or laboured breathing.
Statistical analysis
Statistical analyses were performed using a computerised statistical software package (SPSS Version 21; IBM). Data were analysed descriptively and presented as median (interquartile range [IQR]; 25th–75th percentile) or mean ± SD, where appropriate. Significance was defined as a P value of <0.05. χ2 test (with manual post-hoc Bonferroni correction) of the major comorbidities (cardiac abnormalities, renal disease, dyspnoea and hypertension) was performed to identify significant differences between disease severity groups, with the critical value adjusted for multiple testing (P = 0.017).
Results
Following initial recruitment of 154 client-owned cats; 14 were excluded (incomplete medical records [n = 10], significant comorbidity resulting in unsuitability for radioiodine treatment [n = 3: neoplasia, n = 2, thyrotoxicosis resulting in euthanasia, n = 1], owner declined radioiodine treatment [n = 1]); leaving a study population of 140 cats. Forty-six cats had mild hyperthyroidism, 63 cats had moderate hyperthyroidism and 31 cats had severe hyperthyroidism at referral (Table 1; distribution according to severity at diagnosis also included in table). Ninety-six percent of cats were non-pedigree breeds (pedigree breeds included Bengal [n = 1], British Shorthair [n = 2], Ragdoll [n = 1]); there were 79 female and 61 male cats. At referral the age range of the cats was 6.2–18.0 years (median 12.0 years; IQR 10.0–14.0 years).
Table 1.
Classification of hyperthyroidism severity and population characteristics at the time of diagnosis vs the time of referral for radioiodine treatment
| Hyperthyroid classification at diagnosis* |
Hyperthyroid classification at referral |
|||||
|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | |
| Number of cats | 79 | 40 | 10 | 46 | 63 | 31 |
| TT4 (nmol/l) | 85.0 (74.2–105.0) |
166.5 (149.8–189.0) |
304.5 (258.8–367.5) |
98.9 (77.0–111.8) |
198.0 (154.4–216.7) |
388.3 (298.5–495.0) |
| Age (years) | 11.8 (10–13.8) |
11.7 (9.9–12.8) |
10.4 (9.6–11.5) |
12.8 (11.0–14.0) |
12.0 (10.3–13.2) |
12.0 (10.0–14.0) |
| Time between
diagnosis and referral (months) |
– | – | – | 4 (3–5) |
4 (2–7) |
16 (4–26) |
Data are median (interquartile range)
Cats were excluded from hyperthyroid classification at diagnosis if their actual total thyroxine (TT4) level was not quantified and had been recorded as >90 nmol/l; mild group (n = 1), moderate group (n = 6), severe group (n = 4)
Diagnosis of hyperthyroidism was made incidentally in 24.3% of cats (n = 34). An incidental diagnosis was more frequent in the mildly (23.9%) or moderately (29.0%) hyperthyroid groups than the severely (15.6%) hyperthyroid group.
Thirty percent of the cats were <10 years old at diagnosis. The median age between groups at referral was similar; however, the median age at diagnosis of cats with severe hyperthyroidism was younger than those with mild or moderate hyperthyroidism (Table 1). The time interval between diagnosis and referral was significantly longer in cats with severe hyperthyroidism compared with cats with mild or moderate hyperthyroidism (P = 0.004).
Fifty-four of the 140 cats (38.6%) moved up at least one severity group (from mildly to moderately or severely, or from moderately to severely hyperthyroid) between the time of diagnosis and referral (Table 2).
Table 2.
Change in severity status of hyperthyroidism between diagnosis and referral for radioiodine treatment: number of cats with mild, moderate and severe hyperthyroidism at the time of diagnosis vs referral for radioiodine treatment
| Diagnosis mild hyperthyroidism (n = 79)* |
Diagnosis moderate hyperthyroidism (n = 40)* |
Diagnosis severe hyperthyroidism (n = 10)* |
|
|---|---|---|---|
| Referral mild hyperthyroidism (n = 45) | 45 | 0 | 0 |
| Referral moderate hyperthyroidism (n = 57) | 27 | 30 | 0 |
| Referral severe hyperthyroidism (n = 27) | 7 | 10 | 10 |
Cats were excluded from hyperthyroid classification at diagnosis if their actual total thyroxine level was not quantified and had been recorded as >90 nmol/l; mild group (n = 1), moderate group (n = 6), severe group (n = 4)
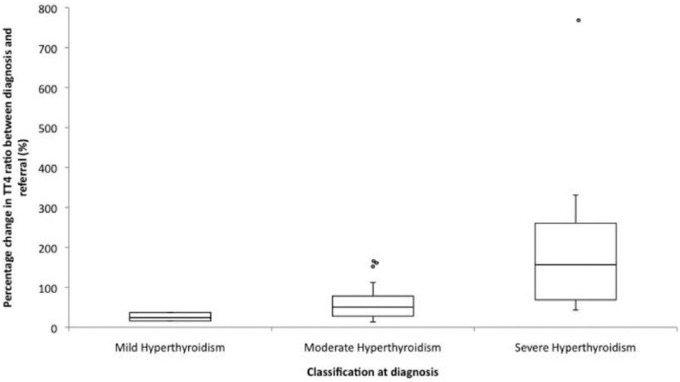
The percentage increase in the TT4 ratio between diagnosis and referral increased as the severity of hyperthyroidism increased. Cats with mild hyperthyroidism at diagnosis had a median increase in the TT4 ratio of 24.3% (IQR 15.8–37.1%) by the time of referral, those with moderate hyperthyroidism had a median increase in the TT4 ratio of 50.4% (IQR 27.8–78.4%) and those with severe hyperthyroidism had a median increase in the TT4 ratio of 156.5% (IQR 68.8–260.6%) (Figure 1).
Figure 1.
Box and whisker plot of the percentage change in total thyroxine (TT4) ratios in hyperthyroid groups between diagnosis and referral for radioiodine treatment for 129 cats. Boxes represent the interquartile range from the 25th to 75th percentile. The horizontal bar in each box represents the median value. Open circles represent outlying data points. Eleven cats were excluded from this data set as their exact TT4 concentration at diagnosis was unknown (ie, TT4 was reported as >90 nmol/l)
At referral, 54% of cats with mild, 67% with moderate and 81% with severe hyperthyroidism were biochemically hyperthyroid despite medical or dietary therapy (95% of all cases received medical therapy and 5% received dietary therapy).
When combining all three severity groups, the most common presenting clinical signs at diagnosis were weight loss (91%) and polyphagia (79%) (Table 3). A palpable goitre was detected in 80.7% of all cases at referral.
Table 3.
Clinical signs recorded at diagnosis of hyperthyroidism in mildly, moderately and severely hyperthyroid cats
| Clinical sign | Mildly hyperthyroid group (n = 46) | Moderately hyperthyroid group (n = 63) | Severely hyperthyroid group (n = 31) |
|---|---|---|---|
| Weight loss | 87 | 89 | 100 |
| Polyphagia | 76 | 78 | 87 |
| Polyuria/polydipsia | 39 | 43 | 77 |
| Hyperactivity | 26 | 43 | 48 |
| Vomiting | 37 | 35 | 48 |
| Tachycardia | 33 | 34 | 48 |
| Alopecia/coat changes | 22 | 30 | 23 |
| Lethargy | 13 | 17 | 19 |
| Diarrhoea | 9 | 14 | 19 |
| Muscle weakness | 13 | 6 | 10 |
| Anorexia | 4 | 8 | 7 |
Data are %
Comorbidity assessment at referral
There was a significantly increased prevalence of cardiac abnormalities in cats with severe hyperthyroidism compared with cats with mild or moderate hyperthyroidism (P = 0.014) (Table 4). Mildly hyperthyroid cats were significantly less likely to be dyspnoeic than cats with moderate or severe hyperthyroidism (P = 0.012). Dyspnoea was due to CHF in two cats with severe hyperthyroidism; no mildly or moderately hyperthyroid cats had CHF. Other non-hyperthyroid causes of dyspnoea were excluded in the remaining 10 cats (eg, thoracic or upper respiratory tract pathology, anaemia); pulmonary and upper respiratory tract auscultation revealed no abnormal sounds in these cats. There was no significant difference in the likelihood of renal disease (P = 0.708) or hypertension (P = 0.328) between groups
Table 4.
Prevalence of major comorbidities (cardiac abnormalities, hypertension, renal disease and dyspnoea) in mildly, moderately and severely hyperthyroid cats at referral for radioiodine treatment
| Comorbidity | Mildly hyperthyroid group (n = 46) | Moderately hyperthyroid group (n = 63) |
Severely hyperthyroid group (n = 31) |
|---|---|---|---|
| Cardiac abnormalities | 37* | 51* | 71* |
| Hypertension | 37 | 29 | 48 |
| Renal disease | 33 | 30 | 39 |
| Dyspnoea | 0* | 11* | 16* |
Data are %
Significant differences between the groups (mild, moderate and severe hyperthyroidism)
When combining all three groups, echocardiography revealed 51% of cats had cardiac abnormalities; 21% had LA enlargement and 1.4% had CHF (Table 5). The two cats diagnosed with CHF were severely hyperthyroid (pleural effusion, n = 1, pulmonary oedema, n = 1). Where present, LV hypertrophy was focal in 28% of cats (n = 9) and generalised in 72% of cats (n = 23). Concurrent LV hypertrophy and systemic hypertension was documented in one cat with mild, five cats with moderate and three cats with severe hyperthyroidism. A cardiac murmur was detected at referral in 63% of cats with mild, 89% with moderate and 90% with severe hyperthyroidism.
Table 5.
Prevalence of echocardiographic abnormalities in mildly, moderately and severely hyperthyroid cats at referral for radioiodine treatment
| Abnormality | Mildly hyperthyroid group (n = 46) | Moderately hyperthyroid group (n = 63) |
Severely hyperthyroid group (n = 31) |
|---|---|---|---|
| Cardiomegaly | 33 | 43 | 68 |
| LA enlargement | 11 | 22 | 32 |
| LV hypertrophy (with
concurrent LA enlargement, with concurrent increased LV end diastolic diameter) |
22 (9, 2) | 44 (22, 16) | 68 (29, 35) |
| Cardiac failure | 0 | 0 | 7 |
LA = left atrial; LV= left ventricle
CKD was diagnosed in 46 cats; in 78% of these, the diagnosis was made when hyperthyroidism was controlled (TT4 15–60 nmol/l), with the remaining 22% biochemically hyperthyroid. Of those cats without CKD, 28.3% were biochemically hyperthyroid. The median age of all cats with concurrent CKD was 13.0 years (IQR 12.0–14.8 years). No severely hyperthyroid cats were azotaemic. No cats were diagnosed with IRIS stage 3 or 4 CKD (Table 6).
Table 6.
Prevalence of renal disease classified by International Renal Interest Society (IRIS) chronic kidney disease (CKD) stage at the time of referral for radioiodine treatment in cats with mild, moderate and severe hyperthyroidism
| Mildly hyperthyroid group (n = 46) |
Moderately hyperthyroid group (n = 63) |
Severely hyperthyroid group (n = 31) |
||||
|---|---|---|---|---|---|---|
| Number of cases affected | Number of euthyroid affected cases | Number of cases affected | Number of euthyroid affected cases | Number of cases affected | Number of euthyroid affected cases | |
| IRIS stage 1* | 12 | 12 (100) | 13 | 7 (54) | 9 | 2 (22) |
| IRIS stage 2
non- azotaemic: creatinine 140–177 μmol/l |
0 | 0 | 3 | 3 (100) | 3 | 3 (100) |
| IRIS stage 2
azotaemic: creatinine >177 μmol/l |
3 | 3 (100) | 3 | 3 (100) | 0 | 0 |
Data are n (%) unless otherwise specified
IRIS stage 1 renal disease defined as non-azotaemic (serum creatinine <140 μmol/l) with abnormal renal ultrasound findings ± dilute urine (urine specific gravity <1.035), consistent with CKD
Discussion
Hyperthyroidism has typically been associated with disease in senior or geriatric cats. The median age of 12 years in this cohort was younger than that of a large first-opinion population (15.4 years). 7 Thirty percent of cats were <10 years old at initial diagnosis, which contrasts previous studies reporting an incidence of approximately 5% in cats <10 years old.1,2,13 This may represent a changing pattern or demographic of hyperthyroidism, increased use of health-screening profiles (including TT4) 19 or more widespread use of thyroid-stimulating hormone assays allowing for earlier diagnosis of disease, even in more mild forms. 20 Conversely, this population may be biased, with owners more willing to opt for radioiodine treatment in younger cats.
A reasonable proportion (24.3%) of cats were diagnosed incidentally at a routine or unrelated assessment. Failure of owner recognition of a problem (eg, polyphagia may not be reported until weight loss develops) or detection of subtle changes by veterinarians (eg, mild weight loss or a small thyroid blip prompting testing for hyperthyroidism) may account for this. Unsurprisingly, an incidental diagnosis was more likely in cats with mild or moderate disease, than cats with severe disease.
This study further documents the wide disease spectrum of feline hyperthyroidism, ranging from mild or early disease, to severe and chronic disease. 9 Cats with severe hyperthyroidism in this cohort were diagnosed at a younger median age; however, further studies are required to ascertain if this is a common finding and not simply a reflection of the small sample size (n = 10) in this disease category. The time interval between diagnosis and referral was significantly longer in cats with severe hyperthyroidism and this group also had the greatest increase in TT4 ratios over time. Chronic medical or dietary therapy allows for continued growth of adenomatous thyroid tissue with time, resulting in increased thyroid volume and associated TT4 levels, as well as potentially carcinomatous transformation. 9 Progression of disease resulted in over one-third of cats (38.6%; n = 54) moving up a severity group between diagnosis and referral. Cats with mild disease may be successfully treated with ultra-low or low doses of radioiodine (eg, <111 MBq). 21 In contrast, severe and chronic disease typically requires much higher doses to restore euthyroidism (eg, 140–1100 MBq), which may necessitate longer hospitalisation periods. 9
Many cats had been chronically medically managed (95% received medical management prior to referral). This may reflect practitioner preference, with oral medication the most commonly preferred treatment option among general practitioners in the UK. 8 While the reported efficacy of medical management (methimazole) is >90%,22,23 a large number of cases were not stabilised with treatment and were biochemically hyperthyroid at referral. This was most frequent in severely hyperthyroid cats (81% were unstable). As the severity of hyperthyroidism increases, it may become difficult or impossible to maintain euthyroidism, despite high doses of thiamazole medications. 9 This inability to medically stabilise patients may have triggered referral and thus biased our results. However, this also raises concern that some cats may have periods between scheduled veterinary visits when hyperthyroidism is inadequately controlled.
As expected, severely hyperthyroid cats more frequently presented with classical signs of disease (weight loss, polyphagia, polyuria/polydipsia). Overall, weight loss was the most common presenting sign, followed by polyphagia (in accordance with surveys from 1983 and 1993), with little difference between the groups. 1 Apathetic hyperthyroidism (lethargy, inappetence) was infrequent in this population (similar to previous reports affecting approximately 10% of hyperthyroid cats).2,10,24 A thyroid goitre was detected in 80.7% of cats, consistent with previous studies (80–90%).1,2,10
Cardiac abnormalities were common in this cohort; the majority of cats presented with a heart murmur and 45% had evidence of cardiomegaly. This prevalence is greater than previous studies (reporting radiographic evidence of cardiomegaly in 26–40% of hyperthyroid cats) and may partially reflect use of a more sensitive imaging modality (echocardiography).25,26 A reported 14.7% of apparently healthy cats in the general population have subclinical hypertrophic cardiomyopathy and this prevalence increases with age (29.4% of cats ⩾9 years). 15 Hyperthyroid cats may be presented with concurrent primary cardiomyopathy, or cardiac disease secondary to hyperthyroidism or systemic hypertension. Although not performed in this study, repeat assessment following radioiodine treatment would be required to differentiate these. Echocardiographic findings consistent with cardiomyopathy or cardiomegaly were most frequently seen in severely hyperthyroid cats. As these cats were of a similar age as those with less severe disease at the time of echocardiography, it is likely that hyperthyroidism contributed to the observed cardiac abnormalities. Approximately one-fifth (21%) of cats had increased LA size, an important finding that implies progressed cardiac disease and is often associated with development of CHF.27,28 This would suggest cardiac assessment should be considered in hyperthyroid cats, particularly those with severe disease and/or poor stability.
The two cats diagnosed with CHF (1.4% of cases) were both severely hyperthyroid. Previous studies report a similar incidence (2–3%) of CHF in hyperthyroid cats.1,10 CHF was treated accordingly, but both cats were deemed unsuitable for radioiodine treatment owing to their daily medication requirement. Significant cardiac disease may also preclude cats from thyroidectomy due to their increased anaesthetic risk. Withdrawal of antithyroid medication prior to radioiodine treatment (standard practice) results in an acute increase in thyroxine levels with potential negative effects on cardiac function. 29 Combined with the stress associated with travel to the radioiodine facility and hospitalisation, subclinical cardiac disease may decompensate to CHF.
The prevalence of hypertension was higher in this study than in a previous reports (36% of cats vs 19% in a previous study). 30 Possible reasons include a high proportion of unstable hyperthyroid cats or the ‘white coat’ effect. Systemic hypertension may further contribute to LV hypertrophy; 16 18% of cats with systemic hypertension in the current study had LV hypertrophy.
Hyperthyroidism may exacerbate renal disease due to sustained hypertension and increased renal blood flow.14,31 There was no significant difference in the frequency of renal disease between severity groups. There was, however, a difference in the stability of hyperthyroidism between groups (severely hyperthyroid cats were more likely to be biochemically hyperthyroid). It is a well-recognised phenomenon that hyperthyroidism may mask underlying renal disease by increasing glomerular filtration rates (GFR).31,32 Along with decreased muscle mass, this results in decreased serum creatinine concentrations.14,31 Over one-quarter (28.3%) of cats without biochemical evidence of renal disease were biochemically hyperthyroid. Therefore, the prevalence of renal disease in this subset of cats (n = 26, 18.6% of the study population) could not be accurately assessed with serum biochemistry alone. GFR studies were not performed in this cohort, and performing IRIS classification at a single time point in hyperthyroid cats represent limitations of this study’s ability to assess renal function; however, this reflects common clinical practice. Furthermore, muscle condition scores were not available. Ultrasound provided additional information, despite poor control of hyperthyroidism, with cats most frequently being classified with IRIS stage 1 CKD. Further studies are required to determine whether ultrasonographic changes are predictive for the development of azotaemia following curative therapy and whether specific ultrasound findings occur with differing severities of hyperthyroidism. No cats were diagnosed with IRIS stage 3 or 4 CKD; however, this was biased by case screening before referral.
Further limitations include case selection from a single referral hospital (population bias), incomplete medical records (including documentation of arrhythmias) and the necessity to exclude cats from analyses involving TT4 levels at diagnosis, if the exact level was unknown (ie, reported as >90 nmol/l). Clinical signs may have been under-reported if not recorded in clinical notes or recalled by the owner. As multiple observers (not all cardiologists) performed cardiac auscultation and due to the variability of murmur grades in cats during auscultation, 15 the severity of heart murmurs (by grade) was not included.
Finally, occult or very mildly hyperthyroid cats (diagnosed by high normal TT4, high free T4 and suppressed thyroid-stimulating hormone) were not included in this population.
Conclusions
A large number of hyperthyroid cats in this cohort were initially diagnosed as an incidental finding. This likely reflects increased awareness of hyperthyroidism within the profession, resulting in increased screening for the disease. Cats with severe hyperthyroidism (TT4 >250.0 nmol/l) were more likely to be chronically hyperthyroid with a history of poor stabilisation, consistent with the progressive nature of the disease. This subset of patients are significantly more likely to suffer from cardiac abnormalities, which may affect their suitability as candidates for curative treatment. These results support the recommendation that radioiodine treatment be given where possible before severe hyperthyroidism develops, due to reduced comorbidity and potentially lower dose requirements.
Acknowledgments
We would like to thank Domingo Casamian for his cardiac assessment of the cats, the referring veterinarians and staff involved in the care of cats while at the Feline Centre, Langford Vets.
Footnotes
Author note: Data from this study were presented in abstract form at BSAVA Congress 2015.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Accepted: 3 January 2018
References
- 1. Broussard JD, Peterson ME, Fox PR. Changes in clinical and laboratory findings in cats with hyperthyroidism from 1983 to 1993. J Am Vet Med Assoc 1995; 206: 302–305. [PubMed] [Google Scholar]
- 2. Peterson ME, Kintzer PP, Cavanagh PG, et al. Feline hyperthyroidism: pretreatment clinical and laboratory evaluation of 131 cases. J Am Vet Med Assoc 1983; 206: 302–305. [PubMed] [Google Scholar]
- 3. Lucke VM. A histological study of thyroid abnormalities in the domestic cat. J Small Anim Pract 1964; 5: 351–358. [Google Scholar]
- 4. Leav I, Schiller AL, Rijnberk A, et al. Adenomas and carcinomas of the canine and feline thyroid. Am J Pathol 1976; 83: 61–122. [PMC free article] [PubMed] [Google Scholar]
- 5. Peterson ME. Hyperthyroidism in cats: what’s causing this epidemic of thyroid disease and how can we prevent it? J Feline Med Surg 2012; 14: 804–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bucknell DG. Feline hyperthyroidism: spectrum of clinical presentations and response to carbimazole therapy. Aust Vet J 2000; 78: 462–465. [DOI] [PubMed] [Google Scholar]
- 7. Stephens MJ, O’Neill DG, Church DB, et al. Feline hyperthyroidism reported in primary-care veterinary practices in England: prevalence, associated factors and spatial distribution. Vet Rec 2014; 175: 458–462. [DOI] [PubMed] [Google Scholar]
- 8. Higgs P, Murray JK, Hibbert A. Medical management and monitoring of the hyperthyroid cat: a survey of UK general practitioners. J Feline Med Surg 2014; 16: 788–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Peterson ME, Broome MR, Rishniw M. Prevalence and degree of thyroid pathology in hyperthyroid cats increases with disease duration: a cross-sectional analysis of 2096 cats referred for radioiodine therapy. J Feline Med Surg 2016; 18: 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thoday KL, Mooney CT. Historical, clinical and laboratory features of 126 hyperthyroid cats. Vet Rec 1992; 131: 257–264. [DOI] [PubMed] [Google Scholar]
- 11. Boland LA, Murray JK, Bovens CPV. A survey of owners’ perceptions and experiences of radioiodine treatment of feline hyperthyroidism in the UK. J Feline Med Surg 2014; 16: 663–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harvey AM, Hibbert A, Barrett EL, et al. Scintigraphic findings in 120 hyperthyroid cats. J Feline Med Surg 2009; 11: 96–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peterson ME, Becker DV. Radioiodine treatment of 524 cats with hyperthyroidism. J Am Vet Med Assoc 1995; 207: 1422–1428. [PubMed] [Google Scholar]
- 14. Williams TL, Peak K, Brodbelt D, et al. Survival and the development of azotaemia after treatment of hyperthyroid cats. J Vet Intern Med 2010; 24: 863–869. [DOI] [PubMed] [Google Scholar]
- 15. Payne JR, Brodbelt DC, Luis Fuentes V. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J Vet Cardiol 2015; 17: S244–S247. [DOI] [PubMed] [Google Scholar]
- 16. Haggstrom J, Luis Fuentes V, Wess G. Screening for hypertrophic cardiomyopathy in cats. J Vet Cardiol 2015; 17: S134–S149. [DOI] [PubMed] [Google Scholar]
- 17. Payne JR, Borgeat K, Connolly DJ, et al. Prognostic indicators in cats with hypertrophic cardiomyopathy. J Vet Intern Med 2013; 27: 1427–1436. [DOI] [PubMed] [Google Scholar]
- 18. Brown S, Atkins C, Bagley R, et al. ACVIM Consensus Statement: guidelines for the identification, evaluation and management of systemic hypertension in dogs and cats. J Vet Intern Med 2007; 21: 542–558. [DOI] [PubMed] [Google Scholar]
- 19. Paepe D, Verjans G, Duchateau L, et al. Routine health screening: findings in apparently healthy middle-aged and old cats. J Feline Med Surg 2012; 15: 8–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Peterson ME, Guterl JN, Nichols R, et al. Evaluation of serum thyroid-stimulating hormone concentration as a diagnostic test for hyperthyroidism in cats. J Vet Intern Med 2015; 29: 1327–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lucy JM, Peterson ME, Randolph JF, et al. Efficacy of low-dose (2 millicurie) vs standard-dose (4 millicurie) radioiodine treatment for cats with mild-to-moderate hyperthyroidism. J Vet Intern Med 2017; 31: 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Trepanier LA, Hoffman SB, Kroll M, et al. Efficacy and safety of once versus twice daily administration of methimazole in cats with hyperthyroidism. J Am Vet Med Assoc 2003; 222: 954–958. [DOI] [PubMed] [Google Scholar]
- 23. Sartor LL, Trepanier LA, Kroll MM, et al. Efficacy and safety of transdermal methimazole in the treatment of cats with hyperthyroidism. J Vet Intern Med 2004; 18: 651–655. [DOI] [PubMed] [Google Scholar]
- 24. Carney HC, Ward CR, Bailey SJ, et al. 2016 AAFP guidelines for the management of feline hyperthyroidism. J Feline Med Surg 2016; 18: 400–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moise NS, Dietze AE. Echocardiographic, electrocardiographic, and radiographic detection of cardiomegaly in hyperthyroid cats. Am J Vet Res 1986; 47: 1487–1494. [PubMed] [Google Scholar]
- 26. Bond BR, Fox PR, Peterson ME, et al. Echocardiographic findings in 103 cats with hyperthyroidism. J Am Vet Med Assoc 1988; 192: 1546–1549. [PubMed] [Google Scholar]
- 27. Rush JE, Freeman LM, Fenollosa NK, et al. Population and survival characteristics of cats with hypertrophic cardiomyopathy: 260 cases (1990–1999). J Am Vet Med Assoc 2002; 220: 202–207. [DOI] [PubMed] [Google Scholar]
- 28. Payne J, Luis Fuentes V, Boswood A, et al. Population characteristics and survival in 127 referred cats with hyperthrophic cardiomyopathy (1997–2005). J Small Anim Pract 2010; 51: 540–547. [DOI] [PubMed] [Google Scholar]
- 29. Connolly DJ, Guitian J, Boswood A, et al. Serum troponin I levels in hyperthyroid cats before and after treatment with radioactive iodine. J Feline Med Surg 2005; 7: 289–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stepien RL, Rapoport GS, Henik PA, et al. Effect of measurement method on blood pressure findings in cats before and after therapy for hyperthyroidism. J Vet Intern Med 2003; 17: 754. [Google Scholar]
- 31. Williams TL, Elliott J, Syme HM. Association of iatrogenic hypothyroidism with azotaemia and reduced survival time in cats treated for hyperthyroidism. J Vet Intern Med 2010; 24: 1086–1092. [DOI] [PubMed] [Google Scholar]
- 32. Wakeling J, Moore K, Elliott J, et al. Diagnosis of hyperthyroidism in cats with mild chronic kidney disease. J Small Anim Pract 2008; 49: 287–294. [DOI] [PubMed] [Google Scholar]