Abstract
Objective
To assess longitudinal estimates of inpatient costs through early childhood in patients with critical congenital heart defects (CCHDs), for whom reliable estimates are scarce, using a population-based cohort of clinically validated CCHD cases.
Study design
Longitudinal retrospective cohort of infants with CCHDs live born from 1997 to 2012 in Utah. Cases identified from birth defect registry data were linked to inpatient discharge abstracts and vital records to track inpatient days and costs through age 10 years. Costs were adjusted for inflation and discounted by 3% per year to generate present value estimates. Multivariable models identified infant and maternal factors potentially associated with higher resource utilization and were used to calculate adjusted costs by defect type.
Results
The final statewide cohort included 1439 CCHD cases among 803 509 livebirths (1.8/1000). The average cost per affected child through age 10 years was $136 682 with a median of $74 924 because of a small number of extremely high cost children; costs were highest for pulmonary atresia with ventricular septal defect and hypoplastic left heart syndrome. Inpatient costs increased by 1.6% per year during the study period. A single birth year cohort (~50 000 births/year) had estimated expenditures of $11 902 899 through age 10 years. Extrapolating to the US population, inpatient costs for a single birth year cohort through age 10 years were ~$1 billion.
Conclusions
Inpatient costs for CCHDs throughout childhood are high and rising. These revised estimates will contribute to comparative effectiveness research aimed at improving the value of care on a patient and population level.
Critical congenital heart defects (CCHDs) account for approximately 25% of all congenital heart disease (CHD),1–4 but because they require lifelong complex care, they are associated with disproportionately high resource use.5 With increasing investment on improving detection and care of CCHDs, it is important to understand the return in terms of outcomes and resource use.
Current cost estimates for CCHDs are uncertain and likely underestimated. Most published studies address the surgical or index hospitalization but rarely extend beyond the first year of life.5 The few assessments beyond infancy are typically based on convenience patient cohorts (eg, single center or payer), or on administrative data sources that rely on diagnoses codes without independent clinical validation,6–11 and which are generally unable to track individual patient data over time. To address these limitations, we collected individually linked hospital utilization data for a statewide, population-based, and clinically validated cohort of children with CCHDs. Our aims were to estimate average inpatient medical costs in children with CCHDs through age 10 years and assess the contribution of individual CCHD types to population-level inpatient costs.
Methods
This longitudinal retrospective population-based cohort study included all live born infants diagnosed with a CCHD in Utah from January 1997 through December 2012. We excluded only cases with severely life-limiting chromosomal aneuploidies (eg, trisomies 18 and 13). Patients were followed through December 2013.
The CCHD cohort was identified from the Utah Birth Defect Network (UBDN), a state-wide population-based surveillance system that prospectively and actively monitors all birth outcomes (livebirths, stillbirths, and terminations) for major birth defects, including CCHDs, identified from 20 weeks of gestation to 2 years of age.12 The system’s comprehensive case ascertainment uses a combination of methods to identify potential cases. Trained abstractors review records in all birth hospitals and Primary Children’s Hospital–Utah’s only quaternary children’s hospital and sole center with pediatric congenital heart surgery for Utah and the Intermountain West. Utah state law also mandates hospitals and laboratories to report all cases of suspected birth defects. All potential cases of CHD are reviewed by expert clinicians (geneticist and pediatric cardiologist) to confirm diagnoses and ensure correct classification. For all confirmed cases, extensive data on the child’s diagnostic and clinical evaluation and maternal history and demographics are included in registry records. For prenatally diagnosed livebirths, this information includes confirmatory postnatal imaging.
For consistency with public health practice, we defined CCHDs as the 12 diagnoses used by newborn screening programs and recommended by the Centers for Disease Control and Prevention (Appendix 1 [available at www.jpeds.com] and Table I)13: hypoplastic left heart syndrome and variants (HLHS), tricuspid atresia, other single ventricles, pulmonary atresia with intact ventricular septum (PA/IVS), truncus arteriosus (truncus), Ebstein anomaly, pulmonary atresia with ventricular septal defect (PA/VSD) also known as tetralogy of Fallot (TOF) with pulmonary atresia, double outlet right ventricles (DORV) with malposed great arteries (DORV/TGA) and DORV with normally related great arteries (DORV), d-transposition of the great arteries, TOF, interrupted aortic arch, total anomalous pulmonary venous return, and coarctation of the aorta. For children with >1 major CHD, a primary CHD diagnosis was assigned using a hierarchical coding algorithm based on embryologic origin,14 type of intervention required, and associated mortality and morbidity (Appendix 1). For example, a patient with PA/IVS and Ebstein anomaly would be coded as PA/IVS, which is higher in the hierarchy. For analyses, the presence of additional major CHD was defined as an additional major heart defect (with the exception of atrial and ventricular septal defects and minor valve abnormalities) not part of the primary diagnosis. Complex cases were reviewed by 2 independent investigators.
Table I.
Demographics of children born with CCHD in Utah from 1997 to 2012 (n = 1434)*
| Characteristics | n | % or SD, as appropriate |
|---|---|---|
| Prenatal diagnosis (yes) | 423 | 29.5 |
| Type of CCHD | ||
| HLHS | 223 | 15.6 |
| TA | 80 | 5.6 |
| Other SVs | 24 | 1.7 |
| PA/IVS | 33 | 2.3 |
| Truncus | 48 | 3.4 |
| Ebstein anomaly | 46 | 3.2 |
| PA/VSD | 66 | 4.6 |
| DORV/TGA | 31 | 2.2 |
| DTGA | 134 | 9.3 |
| TOF | 191 | 13.3 |
| DORV | 20 | 1.4 |
| IAA | 30 | 2.1 |
| TAPVR | 49 | 3.4 |
| Coarctation | 459 | 32.0 |
| Gestational age at birth (wk) | 37.9 | ±2.4 |
| Female | 560 | 39.1 |
| Additional major CHD | 187 | 13.0 |
| Additional noncardiac anomaly | 351 | 24.5 |
| Year of birth | ||
| 1997-2001 | 407 | 28.2 |
| 2002-2006 | 508 | 35.3 |
| 2007-2012 | 524 | 36.5 |
| Small for gestational age (yes) | 191 | 13.3 |
| Complex chronic condition (extracardiac) | ||
| 0 | 879 | 61.3 |
| 1 | 273 | 19.0 |
| ≥2 | 282 | 19.6 |
| Private insurance (yes) | 743 | 51.8 |
| Tertiary/quaternary facility | 1285 | 89.3 |
| Maternal race nonwhite | 245 | 17.1 |
| Maternal age, y | ||
| <25 | 606 | 42.3 |
| 25-30 | 458 | 32.0 |
| 30-35 | 257 | 17.9 |
| >35 | 113 | 7.9 |
| Maternal education | ||
| <High school | 170 | 11.9 |
| High school | 435 | 30.8 |
| >High school | 740 | 51.6 |
| Missing | 89 | 6.2 |
| % Population below poverty level in census tract | ||
| <5% | 460 | 32.1 |
| 5%-9.9% | 442 | 30.8 |
| 10%-19.9% | 336 | 23.4 |
| ≥20% | 168 | 11.7 |
| Missing | 28 | 2.0 |
| Maternal residence rurality | ||
| Urban | 998 | 69.6 |
| Rural | 209 | 14.6 |
| Highly rural | 11 | 0.8 |
| Missing | 216 | 15.1 |
Coarctation, coarctation of the aorta; DTGA, d-transposition of the great arteries; IAA, interrupted aortic arch; SVs, single ventricles; TA, tricuspid atresia; TAPVR, total anomalous pulmonary venous return.
Excludes 5 patients missing inpatient cost data.
The Utah Population Database (UPDB) was the main source of data on hospital utilization, inpatient costs, and survival. The UPDB is linked annually to the UBDN using birth certificate number when available or demographic data in the rare instance it is not. These linkages have been successfully used in previous birth defect studies.15 The UPDB also maintains ongoing data linkages that include extensive demographic information from vital records and hospital discharges provided by the Utah Department of Health beginning in 1996. Further information on the linkage process can be found in Appendix 2 (available at www.jpeds.com). For our study, because of the small numbers, manual linkages for inpatient data were attempted using available identifiers if usual linkage methods failed. Data on inpatient hospitalizations are extracted from the Utah State Inpatient Discharge Abstracts. These discharge abstracts contain inpatient event data for all hospitals with all levels of care in the state (55 in 2013). Specifically, the abstracts include all inpatient stay data, regardless of the length of stay (even if <24 hours), but do not include same day procedures, observational stays, or emergency department visits that do not result in an inpatient admission. These multiple sources can be used to generate comprehensive individual-level longitudinal medical and demographic records for all state residents.16,17
The final analytic data set included the following domains: maternal and child demographics; vital status of the child; census tract of maternal residence (based on address from the birth certificate) with associated geographic income indicators and household education (2010 US Census data); child’s clinical information (eg, additional major CHD, noncardiac birth anomalies, and noncardiac chronic conditions)18; longitudinal hospital encounter histories (with associated diagnoses, procedures, and length of stay); encounter facility (tertiary/quarternary vs nontertiary/quaternary center, defined by the Utah Department of Health); and payer type (public or private by encounter; Appendix 3 [available at www.jpeds.com]). Utah’s state hospital discharge records included the total facility charges billed for each inpatient encounter (without professional fees) and are the same data reported to and used by Healthcare Cost and Utilization Project for their reports on costs and utilization.19,20 Total facility charges are inclusive of room and all services, including pharmacy charges but do not include specific detailed charges.
Patients were followed until death, administrative censoring, or end of study in December 2013. Administrative censoring was based on date of last assumed residence in Utah, defined by the UPDB as either the last date seen in Utah at a health facility or 6 years from the date of latest renewal of the maternal driver’s license.21 Because the cohort only included births for mothers residing in the state, it did not include children with CCHD who moved to Utah after birth.
Statistical Analyses
The primary study outcomes were mean inpatient healthcare costs and inpatient days as estimates of hospital/healthcare resource utilization. Median costs were also calculated as a supplement. Costs were constructed from hospital charges, which represent what a hospital bills for services, using internal hospital cost-to-charge ratios when available and Medicare cost report when not available. Costs were inflation adjusted to 2013 dollars using the Producer Price Index for general medical and surgical hospitals weighted by source of payment.22 To generate present value estimates of inpatient costs for future costs of our population cohort estimates, average costs over 10 years of life were also discounted 3% per year back to the birth year.23,24 For this discounting, each future year’s cost was reduced using the formula: where r is the annual discount rate (3% in our case) and n is the year. For example, a child whose year 4 cost was equal to $10 505 would have discounted costs of .
Individual-Level Estimates.
To account for variable followup periods, average per patient costs and inpatient days were calculated for 3 discrete age periods: first year of life; age 2-5 years; and age 6-10 years. For each period, all cases alive at the beginning of the period contributed to estimates. Mean inpatient costs and inpatient days, both unadjusted and adjusted for comorbidities, insurance and socioeconomic status, were generated for each CCHD type and each age period. Because results were unstable when sample sizes were small, we report adjusted calculations only when the number of cases for a CCHD type within a specific age period was >10.
We conducted multivariable analyses to identify predictors of inpatient costs and inpatient days in each period with potential predictors chosen a priori based on the current literature.25,26 These predictors included severity of CCHD, Pediatric Quality Indicators in cardiac surgery from the Agency for Healthcare Research and Quality,27 and socioeconomic and geographic risk factors that may impact utilization.28,29 Inpatient costs and inpatient days for the first year of life were modeled using generalized linear models with gamma distribution and log link. For age 2-5 and age 6-10 years, 2-part models were used because a large proportion of the cohort had no encounters in these periods. The first part of these 2-part models was a logistic regression that modeled whether the child incurred any inpatient costs (or days). In the second part, a generalized linear model with a gamma distribution and log link was used to model inpatient costs/days conditional on the patient have incurred any of these outcomes.30 In the primary analysis, we included all cases alive at the beginning of the period regardless of whether they died during the analyzed period. However, deaths can have a variable but significant influence on healthcare costs (higher costs at end of life or lower costs secondary to early death). Death was not included in multivariate models as a risk factor because it is an intermediate outcome rather than a baseline covariate in longitudinal analysis. Instead, additional sensitivity analyses were performed with models excluding nonsurvivors during the relevant time periods.
Population-Level Estimates.
Population (statewide) inpatient costs were assessed by CCHD type by combining prevalence and per-patient costs estimates from this study. For the first year of life, estimates were assessed by multiplying the average per patient inpatient costs by the average birth prevalence (calculated using UBDN data from 1997-2012). For later ages, estimated prevalence by age incorporated death rates by year of life as assessed by the study. A Pareto analysis was used to assess the contribution of CCHD types to population inpatient costs for a single birth year cohort of children with CCHD through age 10 years.
The study was approved with a waiver of consent by the Institutional Review Boards of the University of Utah, the UPDB, and the Utah Department of Health.
Results
Among a total birth population of 803 509 delivered from 1997 through 2012, 2135 had some type of major CHD (excluding VSDs, ASDs, and isolated valve defects). Of these, 14 were homebirths and an additional 15 did not link to an inpatient discharge record (<1%). After excluding stillbirths or terminations (n = 207) and cases with severe life limiting trisomies (n = 34), and restricting cases to the 12 CCHD diagnoses, the final cohort included 1439 infants (birth prevalence 1.8/1000 births or 0.18%). Of these, 13% (n = 187) had additional major cardiac defects and 25% (n = 351) had a noncardiac anomaly or syndrome (Table I). Overall mortality for the cohort was 16.7% (n = 241): 14.5% in infancy, 2.6% for ages 2-5 years, and 1.7% for ages 6-10 years. Mortality by CCHD type and age is summarized in Table II (available at www.jpeds.com).
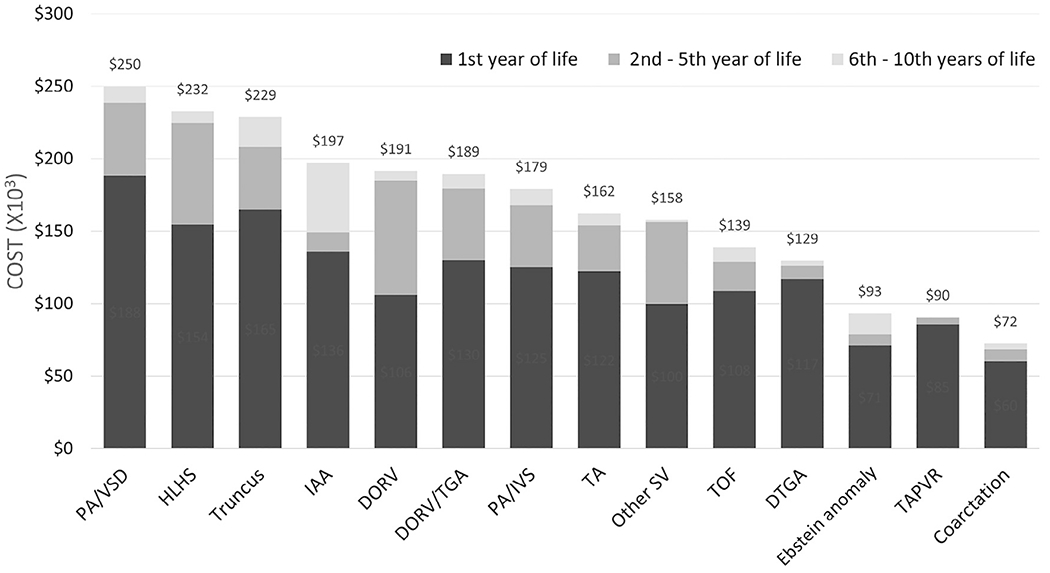
Cost data were missing for 5 patients (0.3%) who had a birth hospitalization as their only inpatient encounter. These patients were not included in the resource utilization analyses (costs and length of stay [LOS]). In the first 10 years of life, average inpatient cost for a child with a CCHD was $136 682 (median $74 924), with an average of 33 inpatient days. Average aggregate costs are presented in Figure 1 (available at www.jpeds.com) and average aggregate costs and inpatient days by age are presented in Table III. Over the first 10 years of life, children with PA/VSD had the highest average inpatient costs ($255 393) and inpatient days, followed closely by HLHS and truncus both with average costs >$200 000. PA/VSD, truncus, and DORV ranked first through third for inpatient days (58, 49, and 47 days, respectively). For CCHDs as a group, inpatient costs in the first year of life averaged $106 430 per child and exceeded $100 000 for most types of CCHD. From ages 2-5 years, HLHS, other single ventricles, and DORV had the highest average costs ($70 000, $56 000, and $79 000, respectively) and others had significantly lower averages because of a low number of hospitalizations (Table IV; available at www.jpeds.com) and hospital days at older ages (Table III). After age 5 years, inpatient costs and inpatient days were substantially lower for most types of CCHDs. However, children with interrupted aortic arch and truncus incurred substantial inpatient costs in later childhood (age 6-10 years, $48 000 and $21 000, respectively). Adjusted inpatient costs and inpatient days by CCHD type generated by regression modeling are presented in Table V (available at www.jpeds.com).
Table III.
Mean inpatient costs and inpatient hospital days by CCHD type and age (n = 1434)
| CCHD types | Year 1 |
Year 2 |
Year 3 |
Year 4 |
Year 5 |
Years 6-10* |
10 year total |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cost $ (SD × 103) |
LOS (SD) |
Cost $ (SD × 103) |
LOS (SD) |
Cost $ (SD × 103) |
LOS (SD) |
Cost $ (SD × 103) |
LOS (SD) |
Cost $ (SD × 103) |
LOS (SD) |
Cost $ (SD × 103) |
LOS (SD) |
Cost $ mean/median |
LOS | |
| Overall | 106 430 (130) | 27.6 (34.6) | 9348 (44) | 2.0 (9.6) | 6119 (27) | 1.1 (5.3) | 4157 (21) | 0.8 (4.2) | 3009 (16) | 0.5 (3.3) | 7619 (27) | 0.7 (4.7) | 126 159 74 924 | 32.6 |
| HLHS | 154 320 (17 4) | 32.1 (36.8) | 14 960 (74) | 2.4 (14.2) | 21 821 (64) | 2.4 (9.5) | 16 612 (15) | 2.0 (6.9) | 9589 (28) | 1.0 (4.2) | 7860 (18) | 0.5 (2.1) | 211 906 180 082 | 40.1 |
| TA | 122 159 (109) | 33.3 (34.5) | 2609 (7) | 0.9 (2.2) | 12 066 (27) | 2.4 (6.5) | 10 282 (19) | 1.8 (4.4) | 6291 (15) | 1.0 (2.7) | 8315 (17) | 1.0 (3.6) | 152 753 114 191 | 40.4 |
| Other SV | 99 853 (90) | 24.2 (23) | 20 067 (80) | 3.1 (13.9) | 22 482 (40) | 2.8 (6.0) | 6752 (13) | 0.8 (1.8) | 4614 (14) | 1.5 (5.7) | 1399 (3) | 0.2 (0.8) | 140 034 83 928 | 32.6 |
| PA/IVS | 125 221 (109) | 31.4 (34.5) | 22 349 (97) | 4.5 (14.7) | 18 807 (53) | 2.2 (8.5) | 3157 (9) | 0.5 (1.5) | 2495 (10) | 0.5 (2.5) | 11 404 (21) | 0.3 (1.1) | 169 025 91 417 | 39.3 |
| Truncus | 164 885 (128) | 42.0 (37.0) | 11 335 (42) | 1.8 (6.8) | 13 941 (21) | 1.7 (4.4) | 10 505 (39) | 1.7 (8.6) | 1797 (6) | 0.2 (0.9) | 20 878 (26) | 1.6 (3.8) | 206 561 171 749 | 49.0 |
| Ebstein anomaly | 70 859 (201) | 16.1 (33.6) | 6511 (16) | 1.2 (2.9) | 409 (1) | 0.1 (0.4) | 1397 (7) | 0.2 (1.2) | 0 (0) | 0.0 (0.0) | 14 378 (41) | 0.7 (4.7) | 74 000 17 514 | 18.3 |
| PA/VSD | 188 136 (185) | 47.9 (51.1) | 43 337 (41) | 7.5 (18.7) | 5589 (13) | 0.7 (1.9) | 2179 (7) | 0.4 (1.3) | 4816 (15) | 0.5 (2.4) | 11 337 (21) | 0.9 (3.0) | 238 868 172 267 | 57.9 |
| DORV/TGA | 129 980 (117) | 34.7 (34.3) | 15 590 (34) | 3.6 (9.0) | 3183 (10) | 0.8 (2.8) | 13 483 (36) | 2.5 (7.7) | 12 350 (42) | 2.3 (9.5) | 10 268 (8) | 1.8 (6.2) | 186 396 130 850 | 45.7 |
| DTGA | 116 728 (96) | 26.1 (21.0) | 1326 (6) | 0.4 (1.3) | 2858 (12) | 0.5 (2.4) | 1023 (4) | 0.3 (1.2) | 3350 (22) | 0.5 (3.5) | 3436 (14) | 0.3 (2.1) | 118 075 106 108 | 28.1 |
| TOF | 108 427 (128) | 31.7 (43.9) | 11 339 (26) | 2.4 (5.6) | 4570 (22) | 0.9 (5.6) | 941 (4) | 0.2 (1.1) | 1530 (6) | 0.3 (1.6) | 10 017 (16) | 0.9 (2.4) | 125 010 84 089 | 36.5 |
| DORV | 105 815 (71) | 33.3 (25.6) | 54 588 (162) | 10.4 (30.8) | 552 (1) | 0.4 (1.1) | 2740 (10) | 0.5 (2.0) | 8968 (21) | 1.8 (6.6) | 6645 (16) | 0.5 (1.5) | 172 207 81 394 | 46.8 |
| IAA | 135 948 (119) | 36.6 (29.3) | 6904 (26) | 1.6 (5.1) | 3091 (9) | 0.5 (1.6) | 895 (3) | 0.5 (2.0) | 1240 (5) | 0.2 (0.9) | 47 629 (93) | 4.5 (14.6) | 169 931 119 761 | 44.0 |
| TAPVR | 85 288 (81) | 19.2 (16.0) | 989 (4) | 0.4 (1.5) | 1447(6) | 0.4 (1.8) | 1786 (8) | 0.2 (1.3) | 59 (0.3) | 0.0 (0.1) | 258 (1) | 0.1 (0.2) | 84 656 67 248 | 20.4 |
| Coarctation | 60 046 (88) | 19.4 (29.0) | 3685 (18) | 1.0 (6.4) | 1328 (8) | 0.4 (2.9) | 1583 (15) | 0.4 (3.5) | 825 (9) | 0.2 (3.0) | 3978 (26) | 0.6 (6.2) | 64 620 34 177 | 22.0 |
On multivariable analysis, infant factors associated with increased inpatient costs in the first year of life included lower gestational age (per week), being small for gestational age, and having additional major cardiac defects (increases of 7%, 19%, and 28%, respectively, P < .05 for all, Table VI). In the first year of life, using HLHS as a reference group, only TOF, Ebstein anomaly, and coarctation had significantly lower costs (lower by $40 000, $100 000, and $82 000, respectively). Care at a tertiary/quarternary facility was associated with higher costs although private insurance was not. Prenatal diagnosis was associated with higher inpatient costs in the first year. When considering only survivors in this age group, prenatal diagnosis and the presence of noncardiac anomaly were no longer significantly associated with costs.
Table VI.
Multivariable regression model of factors associated with inpatient costs in children with CCHD by age*
| Factors | 0-Year 1 (n = 1434) |
Years 2-5 (n = 943) |
Years 6-10 (n = 432) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total cohort |
Survivors only |
Total cohort |
Survivors only |
Total cohort |
Survivors only |
|||||||
| Marginal Δ (Coeff)† | P value | Marginal Δ (Coeff)† | P value | Marginal Δ | P value | Marginal Δ | P value | Marginal Δ | P value | Marginal Δ | P value | |
| Prenatal diagnosis | $20 869 (0.192) | .008 | $2517 (0.025) | .72 | $2348 | .57 | $1808 | .61 | $2518 | .42 | $4249 | .19 |
| Additional major CHD | $30 313 (0.278) | .013 | $21 206 (0.21) | .06 | $14 225 | .02 | $14 280 | .01 | $11 786 | .008 | $9123 | .03 |
| Year of birth | $1704 (0.016) | .043 | $991 (0.010) | .18 | −$1236 | .02 | −$697 | .14 | −$734 | .22 | −$732 | .22 |
| Small for gestational age | $20 341 (0.187) | .03 | $22 262 (0.22) | .01 | −$2295 | .63 | $1041 | .81 | $4922 | .15 | $3532 | .28 |
| Tertiary facility | $55 336 (0.51) | <.001 | $74 057 (0.731) | <.001 | $58 762 | <.001 | $48 759 | <.001 | $0 | $0 | ||
| Diagnosis (ref HLHS) | ||||||||||||
| Other SV | −$17 981 | .45 | −$28 552 | .19 | $7964 | .44 | $6290 | .48 | −$7951 | .45 | −$9319 | .37 |
| TA | −$19 809 | .18 | −$26 006 | .06 | −$11 780 | .10 | −$10 439 | .08 | $2745 | .59 | $4341 | .42 |
| PA/IVS | $4822 | .82 | −$8287 | .66 | −$6372 | .56 | −$13 346 | .18 | −$2181 | .80 | $1995 | .82 |
| Truncus | $19 648 | .29 | −$12 495 | .49 | −$15 823 | .09 | −$15 060 | .07 | $2777 | .68 | $2062 | .76 |
| Ebstein anomaly | −$99 925 | <.001 | −$174 653 | <.001 | −$29 291 | .02 | −$25 653 | .03 | $9445 | .40 | $9844 | .38 |
| PA/VSD | $15 317 | .34 | −$5974 | .70 | $6368 | .451 | $1997 | .79 | −$176 | .98 | $4114 | .56 |
| DORV/TGA | $1544 | .94 | −$9336 | .62 | −$5713 | .56 | −$2965 | .73 | $2520 | .74 | $4807 | .53 |
| DTGA | $23 734 | .07 | −$3450 | .78 | −$36 208 | <.001 | −$31 563 | <.001 | −$7592 | .22 | −$5363 | .38 |
| TOF | −$40 265 | .001 | −$69 896 | <.001 | −$26 791 | <.001 | −$22 443 | <.001 | $1166 | .80 | $2278 | .63 |
| DORV | −$48 680 | .07 | −$73 478 | .002 | $499 | .97 | −$17 362 | .15 | $2300 | .85 | $5376 | .66 |
| IAA | $3205 | .89 | −$28 734 | .16 | −$43 460 | <.001 | −$36 321 | <.001 | $12 704 | .10 | $15 171 | .07 |
| TAPVR | −$15 862 | .39 | −$38 894 | .02 | −$40 522 | .001 | −$34 476 | .001 | −$30 506 | .02 | −$29 797 | .02 |
| Coarctation | −$81 843 | <.001 | −$105 868 | <.001 | −$44 072 | <.001 | −$42 836 | <.001 | −$9548 | .08 | −$9109 | .09 |
| Noncardiac anomaly | $18 826 (0.173) | .09 | $10 551 (0.104) | .29 | $8917 | .12 | $8562 | .08 | $8413 | .03 | $7807 | .05 |
| Gestational age (wk) | −$7904 (−0.073) | <.001 | −$9064 (−0.089) | <.001 | −$833 | .25 | −$345 | .58 | $1195 | .04 | $1293 | .03 |
| Chronic conditions | ||||||||||||
| +1 | $60 075 (0.55) | <.001 | $50 130 (0.513) | <.001 | $12 558 | .003 | $10 699 | .003 | $4561 | .16 | $4242 | .17 |
| >+2 | $118 021 (1.08) | <.001 | $102 724 (1.05) | <.001 | $39 798 | <.001 | $31 495 | <.001 | $12 503 | .002 | $11 536 | .003 |
Bold values indicate significance P <.05 in model.
Additional predictors included in the model were sex, maternal race, maternal age, insurance and geographic poverty, and rurality based on census tract of maternal address at birth.
Coefficients for multivariable regression only presented for model for first year of life. Because 2-part models were used for older age groups, only the marginal change in cost is presented.
Presence of additional major CHD, chronic comorbidities, and treatment in a tertiary hospital were the only consistent factors associated with higher inpatient costs for older age groups. Ebstein anomaly, TOF, d-transposition of the great arteries, total anomalous pulmonary venous return, and coarctation continued to have significantly lower costs compared with HLHS at ages 2-5 years. At ages 6-10 years, lower gestational age and the presence of a noncardiac anomaly were associated with increased costs (the latter was no longer significant after excluding deaths).
Finally, even after controlling for other covariates and correcting for inflation, costs for inpatient care in the first year of life increased over time during the study period, with an average annual growth rate of 1.6% (Table VI) without significant change in LOS (Table VII; available at www.jpeds.com). At age 2-5 years, both costs and LOS decreased significantly over time. There was no significant change in inpatient costs or LOS for older ages over time.
For a single birth year cohort of infants born with CCHDs the total unadjusted inpatient costs through age 10 years was $11 902 899 (Figure 2). The contribution of individual CCHD types to total cost was driven not only by the cost per case, but also by the birth prevalence of the condition. The 2 leading contributors to population inpatient costs were HLHS, a high cost, low prevalence condition ($2 699 508), and coarctation, a low cost but high prevalence condition ($2 080 784). Assuming a similar CCHD distribution, survival, and birth prevalence in the US as in this study and an estimated 4 million yearly US births compared with 50 000 in Utah,31 and applying Medicare’s hospital wage and capital geographic indices for the Salt Lake Metropolitan area hospitals (multiplying our costs by approximately 1.07 [1/0.938]), the national inpatient costs for a single birth year cohort of CCHDs through age 10 years in the US would be approximately $1 billion.
Figure 2.
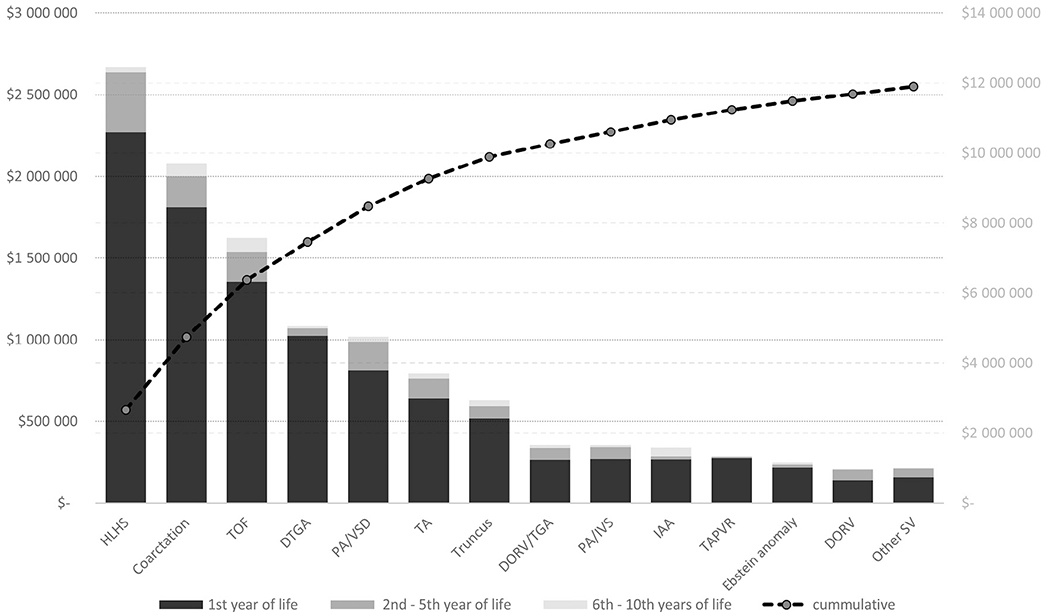
Population costs for a single year birth cohort of children with CCHD in Utah through age 10 years. Line represents cumulative costs.
Discussion
CCHDs are particularly resource intensive because complex surgical and life-long care are required for affected patients.7 In this longitudinal study, the average inpatient costs for a child with a CCHD was ~$137 000 over the first 10 years of life, with PA/VSD, HLHS, and truncus accruing markedly higher costs (>$200 000). When considering population-level estimates, costs are also driven by less expensive but high prevalence CCHDs (ie, coarctation of the aorta). Notably, inpatient costs per case rose 1.6% annually during the study period, even after accounting for concurrent changes in clinical complexity and demographic factors.
There are no comparable estimates currently in the literature for this length of follow-up and by defect type. Our study confirms that costs are the highest in the first year of life for most CCHDs in childhood,9 though our estimates were slightly lower than some previous reports.7,11,32 Our results also underscore how inpatient costs associated with CCHDs2,33,34 are high across nearly all subtypes of CCHDs, though different CCHD types drive the highest costs at different ages. These new cost estimates are important for several reasons. First, from a healthcare perspective, they provide benchmarks of the per-patient inpatient cost burden by age and type of CCHD, which can be used when evaluating the economic impact of interventions. Second, from a population perspective, the cost estimates begin to provide global state-level data for resource planning, which we hope can be expanded to additional states and regions. Third, both the per-patient and the population estimates provide a baseline for ongoing monitoring and assessment of inpatient costs for CCHDs.
Our study expands on a report by Waitzman et al on the costs of birth defects by examining CCHD specific estimates through childhood.3,35 Though the prior study used similar data sources (birth defect registry, discharge abstract, and claims data) to examine a small subset of CHD, these data sources were unlinked requiring calculated estimates rather than actual tracking of individual patients over time. Subsequent studies of CCHD costs using the Health Care Utilization Project Kid’s Inpatient Database (KID) provide longitudinal estimates, but rely on successive cross-sectional age groups and on diagnoses based exclusively on administrative International Classification of Diseases, Ninth Revision, Clinical Modification discharge diagnoses codes.7,11,32 The latter is an important limitation, as using encounter data to identify and define a case fails to include individuals who did not require inpatient care at a given age, and likely explains why their estimates are higher than in our study. Unlike administrative diagnoses codes, which can also often be incorrect,10 our granular clinical data allowed us to assign 1 primary, mutually exclusive diagnosis to each person. Although Boulet et al used MarketScan claims data to track individuals with heart defects over time, patients were still defined using International Classification of Diseases, Ninth Revision, administrative codes and their cost data included only private insurance reimbursements.6 Our approach enabled us to follow a cohort with clinically verified CCHDs from birth, account for deaths and censoring, and include individuals regardless of insurance provider or inpatient encounter at a given age. This approach has been used for other type of birth defects, but had not been previously applied to cardiac defects.36–38
The study population-level estimates of cost provide an important complement to per patient costs by taking into account the prevalence of CCHD types and represent a crucial metric for population health assessment and planning. For example, because of its high prevalence, coarctation of the aorta, which ranks low in the per-case cost ranking, is the second-highest contributor to population-level CCHD inpatient costs in early childhood, behind only HLHS.
The granular patient-level available from linked data sources also allowed us to determine factors associated with higher cost at different ages. The association of prenatal diagnosis with increased costs is likely related to its relationship with severity of disease,39 given that this association is no longer apparent when considering only surviving infants. The association of higher costs with the presence of additional co-morbidities is expected, but understanding the magnitude of these incremental costs is important for health systems and providers, and helps caretakers provide families with realistic expectations.
We documented rising costs of CCHD care25,40 even after accounting for inflation and adjusting for potential confounders such as variations in disease severity over time. Our annual rate of increase for inpatients costs in infancy over the period of 1997-2012 approximately tracked the 1.5% annual increase in real per capita general medical expenditures in the US attributable to residual use and intensity of care between 2004 and 2008.41 That such an increase in costs may relate to increased intensity of care driven by technological advances and interventions not previously available for CCHDs is suggested by the fact that we did not find a similar increased in number of inpatient days over time.42 This is similar to previous work linking increased inpatient costs to forces outside of longer hospital stays in neonates both with and without CHD.40,43–45 Although costs decreased in early childhood outside of the neonatal period, this may be attributed to the parallel decrease in inpatient hospital days. Though similar to overall healthcare spending, identifying particular drivers of increased costs in early life for our population remains important.
Our study has several limitations. The costs data we use are comprehensive but not complete; inpatient discharge abstracts included total inpatient costs without professional fees, a common limitation. Based on a recent study, such fees would add an estimated 18%-26% to inpatient facility costs.19 Our analysis did not include outpatient costs, indirect nonmedical costs, or family costs. However, previous studies found that such costs are dwarfed by inpatient resource use for CHD.46,47 Nevertheless, future inclusion of these costs should provide a more comprehensive assessment of the impact of CCHDs on resource utilization. In addition, because only total charges are available on discharge abstracts, we were unable to provide details of components of costs. Patients who moved out of state may have been missed despite our censoring methods. From an analytic perspective, cost estimates tend to be right skewed (that is, mean costs are higher than median costs) because healthcare utilization is often driven by a small percentage of very high-cost patients.48 However, we presented mean estimates of cost because they are a more realistic reflection of hospital costs and population-level healthcare resource use.
Finally, the estimates of this study are meant to complement those from other sources, such as, in the US, Healthcare Cost and Utilization Project’s KID database, and payer claims databases. Though case ascertainment remains a challenge for the latter data sources, the cross-sectional estimates generated from KID reflect a diverse population and large number of facilities. Our study, like other state estimates, reflects a unique population distribution and model of care which in our case included a single major pediatric cardiac surgical center. However, we assessed all state-level outcomes and inpatient costs. Although state level data may be more challenging to generalize, granular data provided on the association of demographic and clinical features with costs will allow other states to extrapolate grossly based on their population makeup. For example, the birth prevalence of CCHDs of ~0.2% in our cohort is similar to other published US cohorts though our racial distribution is not.49 Such estimates would also need to account for the geographic variation of costs and the relative cost of other facilities compared with our center which falls just above the first quartile in costs of care for CHD among Pediatric Health Information System hospitals.
Acknowledgments
We thank the University of Utah Department of Geography’s Digitally Integrated Geographic Information Technologies laboratory for providing the geographic socioeconomic data from the 2010 Census.
We thank the Pedigree and Population Resource of the Huntsman Cancer Institute, University of Utah (funded in part by the Huntsman Cancer Foundation) for its role in the ongoing collection, maintenance, and support of the Utah Population Database. We thank the University of Utah Center for Clinical and Translational Science (funded by National Institutes of Health Clinical and Translational Science Awards), the Pedigree and Population Resource, University of Utah Information Technology Services and Biomedical Informatics Core for establishing the Master Subject Index between the Utah Population Database, the University of Utah Health Sciences Center, and Intermountain Health Care.
Acknowledgments available at www.jpeds.com
Funded by the American Heart Association Western Affiliates Mentored Clinical and Population Research Award (14CRP18200023 [to N.P.]) and supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (5UL1TR001067-02 [formerly 8UL1TR000105 and UL1RR025764]). The authors declare no conflicts of interest.
Glossary
- CCHD
Critical congenital heart defect
- CHD
Congenital heart disease
- DORV/TGA
Double outlet right ventricles with malposed great arteries
- DORV
Double outlet right ventricle
- HLHS
Hypoplastic left heart syndrome and variants
- KID
Kid’s Inpatient Database
- LOS
Length of stay
- PA/IVS
Pulmonary atresia with intact ventricular septum
- PA/VSD
Pulmonary atresia with VSD
- TOF
Tetralogy of Fallot
- Truncus
Truncus arteriosus
- UBDN
Utah Birth Defect Network
- UPDB
Utah Population Database
- VSD
Ventricular septal defect
Appendix 1
Birth Defect Codes Included by Type of CCHD and Hierarchy of CCHD Diagnosis Assigned for Study
-
Hypoplastic Left Heart Syndrome (HLHS)
746700
Hypoplastic Left Heart Variants (HLHS)
745620/745630/745690 CAVC + (746700 HLHS or +746881 HLV)
745186/745189/745185 DORV + (746700 HLHS or 746881 HLV or 746505 or 746500 Mitral atresia or 746110)
746505/746500 Mitral atresia and/or 747200 aortic atresia + 746881 HLV
- 2. Other single ventricles (SV)
- 745310/745300/745320/745380/746883
- 745620/745630/745690 (CAVC) + (746882/746883/all other SV codes)
-
3. Tricuspid atresia (TA)
746100
-
4. Pulmonary atresia/Intact Ventricular Septum (PA/IVS)
746000 Exclusion: VSD codes or d-transposition of the great arteries (DTGA) or CAVC codes
-
5. Truncus arteriosus (Truncus)
745000
-
6. Ebstein anomaly
746200
-
7. Pulmonary atresia with ventricular septal defect (PA/VSD)
747310 Exclusions: DORV or DTGA codes
-
8. Double outlet right ventricle with transposed great arteries (DORV/TGA)
745186/745189 DORV + (745100/745110TGA) or 745186 DORV/TGA
-
9. D-transposition of the great arteries (DTGA)
745100/745110/745180/745190
-
10. Tetralogy of Fallot (TOF)
745200/745210
-
11. Double outlet right ventricle (DORV)
745189/745185
-
12. Interrupted aortic arch (IAA)
747217 (IAA type B) or 747216/747215 (IAA type A)
-
13. Total anomalous pulmonary venous return (TAPVR)
747420
-
14. Coarctation (Coarct)
747100/747110/747120/747190
Appendix 2
Data Linkages
The UPDB was the main source of data on hospital utilization, inpatient costs, and survival. The UPDB maintains ongoing data linkages that include extensive demographic information from vital records and hospital discharges provided by the Utah Department of Health.
Discharge abstracts may have varying levels of identifiers for linkages purposes. If data is insufficient, the Utah Department of Health provides each facility with a masked ID for the abstract. This ID along with patient identifiers is sent from the facility to the UPDB so allow for linkage of data with other UPDB data sources including vital records.
Further details on the inpatient record linkages can be found at the UPDB website (https://healthcare.utah.edu/huntsmancancerinstitute/research/updb/) and are summarized below:
Claims data represents patient events in the hospital. Data are available in UPDB beginning with 1996. Each record contains identifying information (for record linking), demographic information, hospital code, principal diagnosis and principal procedure codes, 8 (maximum) other diagnosis and other procedure codes, admit and discharge information, mortality risk codes, and payer category.
More than 91% of these records have been linked to an individual within the UPDB. One or more inpatient events are recorded for 2.3 million individuals with records in UPDB.
Appendix 3
Insurance Categories
Public:
Medicare
Medicaid
Other government
Children’s Health Insurance Plan
Charity/unclassified
Private:
Blue Cross/Blue Shield
Other commercial
Managed care
Self-pay
Figure 1.
Average per patient inpatient hospital costs by type of CCHD through age 10 years.
Table II.
Mortality by diagnosis and age
| CCHD types | n | Year 1 |
Years 2-5 |
Years 6-10 |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | (%) | n | Deaths | (%) | n | Deaths | (%) | ||
| Overall | 1439 | 208 | (14.5) | 944 | 25 | (2.6) | 480 | 8 | (1.7) |
| HLHS | 225 | 85 | (37.8) | 97 | 5 | (5.2) | 38 | 3 | (7.9) |
| TA | 80 | 14 | (17.5) | 50 | 0 | (0.0) | 5 | 0 | (0.0) |
| Other SVs | 24 | 4 | (16.7) | 17 | 0 | (0.0) | 29 | 0 | (0.0) |
| PA/IVS | 33 | 5 | (15.2) | 21 | 2 | (9.5) | 7 | 1 | (14.3) |
| Truncus | 49 | 13 | (27.1) | 26 | 2 | (7.7) | 12 | 1 | (8.3) |
| Ebstein anomaly | 47 | 9 | (19.1) | 26 | 2 | (7.7) | 8 | 0 | (0.0) |
| PA/VSD | 66 | 13 | (19.7) | 42 | 3 | (7.1) | 13 | 0 | (0.0) |
| DORV/TGA | 31 | 2 | (6.5) | 22 | 1 | (4.5) | 12 | 1 | (8.3) |
| DTGA | 135 | 8 | (6.0) | 98 | 0 | (0.0) | 63 | 0 | (0.0) |
| TOF | 192 | 18 | (9.4) | 140 | 5 | (3.6) | 79 | 1 | (1.3) |
| DORV | 20 | 3 | (15.0) | 13 | 1 | (7.7) | 6 | 0 | (0.0) |
| IAA | 31 | 4 | (12.9) | 23 | 1 | (4.3) | 13 | 0 | (0.0) |
| TAPVR | 49 | 6 | (12.2) | 31 | 0 | (0.0) | 13 | 0 | (0.0) |
| Coarctation | 461 | 24 | (5.2) | 338 | 3 | (0.9) | 182 | 1 | (0.5) |
Coarctation, coarctation of the aorta; DTGA, d-transposition of the great arteries; IAA, interrupted aortic arch; SVs, single ventricles; TA, tricuspid atresia; TAPVR, total anomalous pulmonary venous return.
Table IV.
Summary of inpatient hospital costs by type of CCHD and year of life
| CCHD types | Year of life | Mean | Discounted mean | SD | % with cost | Median for those with cost |
|---|---|---|---|---|---|---|
| Overall | 1 | $106 430 | — | $130 652 | 100% | $66 685 |
| 2 | $9348 | $8812 | $43 649 | 23.3% | $15 074 | |
| 3 | $6119 | $5600 | $27 490 | 15.8% | $20 512 | |
| 4 | $4157 | $3693 | $21 234 | 12.3% | $19 408 | |
| 5 | $3009 | $2595 | $15 598 | 8.6% | $24 869 | |
| 6 | $1595 | 1336 | $8702 | 7.0% | $12 668 | |
| 7 | $993 | $808 | $5424 | 6.2% | $10 329 | |
| 8 | $1406 | $1110 | $9274 | 5.6% | $13 805 | |
| 9 | $1264 | $969 | $13 944 | 3.7% | $13 268 | |
| 10 | $1857 | $1381 | $11 147 | 6.1% | $17 775 | |
| HLHS | 1 | $154 320 | — | $174 393 | 100% | $120 750 |
| 2 | $14 960 | $14 102 | $74 385 | 25.2% | $16 466 | |
| 3 | $21 821 | $19 969 | $64 430 | 31.1% | $45 545 | |
| 4 | $16 612 | $14 759 | $48 260 | 30.6% | $34 358 | |
| 5 | $9589 | $8272 | $27 764 | 21.5% | $30 510 | |
| 6 | $3262 | $2732 | $12 671 | 14.1% | $9477 | |
| 7 | $1440 | $1171 | $5219 | 13.6% | $6859 | |
| 8 | $845 | $667 | $3821 | 8.6% | $6412 | |
| 9 | $337 | $259 | $1693 | 4.4% | $7593 | |
| 10 | $531 | $395 | $2626 | 5.7% | $9288 | |
| TA | 1 | $122 159 | — | $108 700 | 100% | $95 427 |
| 2 | $2609 | $2459 | $7087 | 30.8% | $4930 | |
| 3 | $12 066 | $11 042 | $26 786 | 27.4% | $37 652 | |
| 4 | $10 282 | $9135 | $18 940 | 31.5% | $31 884 | |
| 5 | $6291 | $5427 | $15 099 | 24.0% | $29 758 | |
| 6 | $2703 | $2263 | $9003 | 15.6% | $7801 | |
| 7 | $1114 | $905 | $4855 | 5.1% | $21 714 | |
| 8 | $1483 | $1171 | $7726 | 6.1% | $24 477 | |
| 9 | $1169 | $896 | $6402 | 3.3% | $35 067 | |
| 10 | $1300 | $967 | $5473 | 6.9% | $18 848 | |
| SV | 1 | $99 853 | — | $89 668 | 100% | $75 550 |
| 2 | $20 067 | $18 915 | $80 140 | 15.8% | $27 861 | |
| 3 | $22 482 | $20 574 | $40 440 | 27.8% | $85 862 | |
| 4 | $6752 | $5999 | $13 174 | 22.2% | $31 821 | |
| 5 | $4614 | $3980 | $14 401 | 11.8% | $39 219 | |
| 6 | $437 | $366 | $1749 | 6.3% | $6997 | |
| 7 | $2180 | $1772 | $6751 | 13.3% | $16 346 | |
| 8 | $0 | $0 | $0 | 0.0% | ||
| 9 | $0 | $0 | $0 | 0.0% | ||
| 10 | $0 | $0 | $0 | 0.0% | ||
| PA/IVS | 1 | $125 221 | — | $109 095 | 100% | $94 389 |
| 2 | $22 349 | $21 066 | $67 481 | 28.6% | $38 133 | |
| 3 | $18 807 | $17 211 | $52 517 | 19.2% | $77 839 | |
| 4 | $3157 | $2805 | $8977 | 13.0% | $28 687 | |
| 5 | $2495 | $2152 | $10 354 | 10.5% | $23 699 | |
| 6 | $0 | $0 | $0 | $0 | 0.0% | |
| 7 | $0 | $0 | $0 | $0 | 0.0% | |
| 8 | $5249 | $4144 | $16 600 | 10.0% | $52 493 | |
| 9 | $0 | $0 | $0 | $0 | 0.0% | |
| 10 | $4556 | $3390 | $11 160 | 16.7% | $27 335 | |
| Truncus | 1 | $164 885 | — | $136 124 | 100% | $136 124 |
| 2 | $11 335 | $10 685 | $42 037 | 21.2% | $27 250 | |
| 3 | $13 941 | $12 758 | $21 228 | 45.2% | $26 207 | |
| 4 | $10 505 | $9334 | $38 542 | 22.2% | $16 804 | |
| 5 | $1797 | $1550 | $5662 | 16.0% | $7471 | |
| 6 | $5985 | $5012 | $19 733 | 19.0% | $19 537 | |
| 7 | $3998 | $3250 | $9840 | 20.0% | $21 444 | |
| 8 | $5212 | $4115 | $13 603 | 16.7% | $41 752 | |
| 9 | $5446 | $4174 | $13 916 | 14.3% | $38 123 | |
| 10 | $2949 | $2194 | $9779 | 9.1% | $32 434 | |
| Ebstein anomaly | 1 | $70 859 | — | $200 863 | 100% | $11 183 |
| 2 | $6511 | $6137 | $16 141 | 19.4% | $31 736 | |
| 3 | $409 | $374 | $1364 | 10.3% | $2886 | |
| 4 | $1397 | $1241 | $7259 | 3.7% | $37 720 | |
| 5 | $0 | $0 | $0 | $0 | 0.0% | |
| 6 | $0 | $0 | $0 | $0 | 0.0% | |
| 7 | $5324 | $4329 | $21 296 | 6.3% | $85 185 | |
| 8 | $0 | $0 | $0 | $0 | 0.0% | |
| 9 | $2487 | $1906 | $8615 | 8.3% | $29 842 | |
| 10 | $0 | $0 | $0 | $0 | 0.0% | |
| PA/VSD | 1 | $188 136 | — | $185 055 | 100% | $120 865 |
| 2 | $43 337 | $40 849 | $89 096 | 54.0% | $52 982 | |
| 3 | $5589 | $5115 | $12 884 | 28.9% | $14 990 | |
| 4 | $2179 | $1936 | $7364 | 17.1% | $5739 | |
| 5 | $4816 | $4154 | $14 663 | 12.8% | $38 320 | |
| 6 | $851 | $713 | $4832 | 5.7% | $14 900 | |
| 7 | $1558 | $1267 | $6207 | 8.8% | $18 686 | |
| 8 | $1605 | $1267 | $6863 | 12.0% | $3314 | |
| 9 | $481 | $368 | $2305 | 4.3% | $11 055 | |
| 10 | $8287 | $6166 | $19 678 | 30.8% | $18 428 | |
| DORV/TGA | 1 | $129 980 | — | $116 502 | 100% | $113 076 |
| 2 | $15 590 | $14 695 | $33 596 | 35.7% | $33 931 | |
| 3 | $3183 | $2913 | $9559 | 12.5% | $32 471 | |
| 4 | $13 483 | $11 980 | $35 520 | 21.7% | $44 017 | |
| 5 | $12 350 | $10 654 | $42 103 | 9.5% | $129 679 | |
| 6 | $6110 | $5117 | $20 674 | 15.0% | $28 110 | |
| 7 | $147 | $120 | $607 | 5.9% | $2501 | |
| 8 | $3321 | $2622 | $11 974 | 7.7% | $43 173 | |
| 9 | $0 | $0 | $0 | $0 | 0.0% | |
| 10 | $4721 | $3513 | $11 123 | 18.2% | $25 964 | |
| DTGA | 1 | $116 728 | — | $96 265 | 100% | $94 866 |
| 2 | $1326 | $1250 | $5700 | 9.7% | $9048 | |
| 3 | $2858 | $2616 | $11 670 | 10.5% | $23 727 | |
| 4 | $1023 | $909 | $4189 | 10.2% | $7190 | |
| 5 | $3350 | $2890 | $21 845 | 5.1% | $50 873 | |
| 6 | $45 | $37 | $438 | 1.0% | $4290 | |
| 7 | $31 | $26 | $290 | 1.2% | $2675 | |
| 8 | $167 | $132 | $1485 | 1.3% | $13 200 | |
| 9 | $722 | $553 | $5007 | 2.7% | $26 359 | |
| 10 | $2279 | $1696 | $12 272 | 6.3% | $24 850 | |
| TOF | 1 | $108 427 | — | $128 237 | 100% | $59 572 |
| 2 | $11 339 | $10 688 | $25 798 | 33.1% | $30 443 | |
| 3 | $4570 | $4182 | $22 361 | 13.8% | $25 586 | |
| 4 | $941 | $836 | $4371 | 8.8% | $4312 | |
| 5 | $1530 | $1320 | $6337 | 8.1% | $17 208 | |
| 6 | $2394 | $2,005 | $8933 | 9.7% | $25 366 | |
| 7 | $1751 | $1423 | $6766 | 9.6% | $13 690 | |
| 8 | $2802 | $2212 | $8935 | 12.5% | $27 486 | |
| 9 | $1252 | $960 | $6256 | 5.7% | $16 448 | |
| 10 | $1624 | $1208 | $7612 | 5.1% | $28 299 | |
| DORV | 1 | $105 815 | — | $71 445 | 100% | $89 102 |
| 2 | $54 588 | $51 454 | $161 768 | 35.3% | $28 187 | |
| 3 | $552 | $506 | $1170 | 20.0% | $2586 | |
| 4 | $2740 | $2435 | $10 252 | 7.1% | $38 361 | |
| 5 | $8968 | $7736 | $20 991 | 16.7% | $53 811 | |
| 6 | $3832 | $3210 | $11 972 | 18.2% | $21 078 | |
| 7 | $996 | $810 | $2988 | 11.1% | $8964 | |
| 8 | $0 | $0 | $0 | $0 | 0.0% | |
| 9 | $0 | $0 | $0 | $0 | 0.0% | |
| 10 | $0 | $0 | $0 | $0 | 0.0% | |
| IAA | 1 | $135 948 | — | $118 585 | 100% | $103 300 |
| 2 | $6904 | $6508 | $26 181 | 19.2% | $13 728 | |
| 3 | $3091 | $2828 | $8583 | 20.0% | $16 267 | |
| 4 | $895 | $795 | $2796 | 16.7% | $3320 | |
| 5 | $1240 | $1070 | $4563 | 9.1% | $13 639 | |
| 6 | $6459 | $5409 | $23 678 | 20.0% | $9757 | |
| 7 | $2358 | $1918 | $5570 | 18.8% | $13 008 | |
| 8 | $15 663 | $12 365 | $47 048 | 14.3% | $109 641 | |
| 9 | $0 | $0 | $0 | $0 | 0.0% | |
| 10 | $18 375 | $13 673 | $49 283 | 15.4% | $119 437 | |
| TAPVR | 1 | $85 288 | — | $81 269 | 100% | $67 248 |
| 2 | $989 | $932 | $3974 | 9.8% | $6847 | |
| 3 | $1447 | $1324 | $5530 | 8.3% | $14 923 | |
| 4 | $1786 | $1587 | $8012 | 6.3% | $28 583 | |
| 5 | $59 | $51 | $329 | 3.2% | $1832 | |
| 6 | $119 | $99 | $616 | 3.7% | $3202 | |
| 7 | $174 | $141 | $778 | 5.0% | $3479 | |
| 8 | $186 | $147 | $791 | 5.6% | $3356 | |
| 9 | $0 | $0 | $0 | $0 | 0.0% | |
| 10 | $0 | $0 | $0 | $0 | 0.0% | |
| Coarctation | 1 | $60 046 | — | $87 937 | 100% | $32 122 |
| 2 | $3685 | $3474 | $17 789 | 18.6% | $9335 | |
| 3 | $1328 | $1215 | $7734 | 8.1% | $9205 | |
| 4 | $1583 | $1406 | $14 540 | 4.9% | $13 931 | |
| 5 | $825 | $711 | $8778 | 3.3% | $6031 | |
| 6 | $658 | $551 | $4608 | 3.6% | $13 332 | |
| 7 | $331 | $269 | $2665 | 2.5% | $9046 | |
| 8 | $282 | $222 | $3652 | 2.0% | $3299 | |
| 9 | $1797 | $1377 | $21 609 | 3.3% | $9043 | |
| 10 | $505 | $376 | $3562 | 3.9% | $9723 |
Table V.
Adjusted mean inpatient hospital costs and hospital days by CCHD type and age
| CCHD types | Additional CHD | Year 1 |
Years 2-5 |
Years 6-10 |
Total |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Costs $ | LOS* | n | Costs $ | Discounted Costs $ | LOS* | n | Cost $ | Discounted costs $ | LOS* | Cost$‡ | LOS* | ||
| HLHS | 25 (11) | 223 | 146 235 | 30.5 | 97 | 61 651 | 56 419 | 14.3 | 38 | 7364 | 5,900 | 1.7 | 215,250 | 46.4 |
| TA | 10 (13) | 80 | 106 182 | 28.9 | 50 | 29 286 | 26 801 | 8.2 | 29 | 6961 | 5,577 | 1.7 | 142,430 | 38.7 |
| Other SV | 4 (17) | 24 | 110 463 | 29.8 | 17 | 61 233 | 56 037 | 13.2 | 5 | † | † | † | † | |
| PA/IVS | 4 (12) | 33 | 124 665 | 30.5 | 21 | 44 055 | 40 316 | 8.5 | 7 | † | † | † | † | † |
| Truncus | 7 (15) | 48 | 149 806 | 36.0 | 26 | 35 750 | 32 716 | 7.6 | 12 | 17 873 | 14,319 | 3.0 | 203,428 | 46.6 |
| Ebstein anomaly | 3 (6) | 46 | 81 438 | 20.1 | 26 | 13 059 | 11 951 | 3.4 | 8 | † | † | † | † | † |
| PA/VSD | 16 (24) | 66 | 158 459 | 38.9 | 42 | 46 389 | 42 453 | 8.7 | 13 | 2094 | 1,677 | 0.2 | 206,942 | 47.8 |
| DORV/TGA | 5 (16) | 31 | 119 666 | 30.7 | 22 | 37 946 | 34 726 | 9.4 | 12 | 8123 | 6,508 | 0.9 | 165,734 | 41.0 |
| DTGA | 15 (11) | 134 | 37 453 | 32.3 | 98 | 14 024 | 12 834 | 3.6 | 63 | 3138 | 2,514 | 0.6 | 154,614 | 36.5 |
| TOF | 31 (16) | 191 | 94 030 | 27.0 | 140 | 16 944 | 15 506 | 3.9 | 79 | 10 424 | 8,351 | 1.8 | 121,398 | 32.6 |
| DORV | 5 (25) | 20 | 69 056 | 21.4 | 13 | 66 644 | 60 989 | 13.7 | 6 | † | † | † | † | † |
| IAA | 3 (10) | 30 | 123 499 | 30.6 | 23 | 7080 | 6479 | 1.6 | 13 | 49 823 | 39,916 | 10.8 | 180,402 | 43.1 |
| TAPVR | 2 (4) | 49 | 94 479 | 22.4 | 31 | 9140 | 8364 | 3.5 | 13 | 1541 | 1,235 | 0.1 | 105,160 | 25.9 |
| Coarctation | 57 (12) | 459 | 73 099 | 23.3 | 338 | 12 701 | 11 623 | 4.0 | 182 | 5236 | 4,195 | 1.7 | 91,036 | 29.0 |
Adjusted for additional major CHD, small for gestational age, gestational age, noncardiac anomaly, sex, additional chronic conditions, tertiary facility, insurance, maternal race, maternal age, census tract poverty, and census tract rurality.
LOS total inpatient hospital days.
Insufficient sample for adjusted cost/LOS calculation.
Total costs represent total absolute cost (not discounted).
Table VII.
Multivariable regression model of factors associated with inpatient hospital days/LOS in children with CCHD by age*
| Factors | 0-Year 1 (n = 1434) |
Years 2-5 (n = 943) |
Years 6-10 (n = 432) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total cohort |
Survivors only |
Total cohort |
Survivors only |
Total cohort |
Survivors only |
|||||||
| Marginal Δ† | P value | Marginal Δ† | P value | Marginal Δ† | P value | Marginal Δ† | P value | Marginal Δ† | P value | Marginal Δ† | P value | |
| Prenatal diagnosis | 2.7 | .114 | −0.6 | .71 | 1.0 | .31 | 0.8 | .33 | 1.3 | .15 | 1.7 | .11 |
| Additional major CHD | 5.1 | .061 | 4.7 | .08 | 3.2 | .03 | 3.0 | .02 | 2.7 | .04 | 2.0 | .09 |
| Year of birth | 0.2 | .238 | 0.0 | .80 | −0.3 | .04 | −0.2 | .14 | −0.1 | .56 | −0.1 | .55 |
| Small for gestational age | 6.8 | .001 | 8.3 | <.001 | −0.3 | .78 | 0.6 | .56 | 1.2 | .15 | 0.8 | .32 |
| Tertiary facility | 13.9 | <.001 | 15.3 | <.001 | 8.2 | .01 | 6.9 | .01 | 0 | 0 | ||
| Diagnosis (ref HLHS) | ||||||||||||
| Other SV | 0.6 | .91 | −5.0 | .33 | 1.7 | .50 | 1.3 | .55 | −2.9 | .26 | −3.4 | .22 |
| TA | 1.3 | .70 | −3.4 | .30 | −2.1 | .22 | −2.0 | .15 | 0.2 | .84 | 0.5 | .67 |
| PA/IVS | 2.1 | .66 | −2.1 | .63 | −2.9 | .26 | −4.7 | .05 | −1.1 | .60 | −0.3 | .88 |
| Truncus | 6.3 | .13 | −3.9 | .35 | −4.9 | .04 | −5.1 | .01 | 0.1 | .93 | 0.0 | .99 |
| Ebstein anomaly | −16.0 | <.001 | −31.5 | <.001 | −6.1 | .04 | −4.9 | .08 | 3.1 | .34 | 3.1 | .34 |
| PA/VSD | 6.8 | .07 | −0.9 | .80 | 0.0 | .99 | −1.0 | .54 | −1.1 | .50 | 0.1 | .96 |
| DORV/TGA | 1.9 | .69 | −3.9 | .38 | −2.6 | .27 | −1.9 | .35 | −0.3 | .88 | 0.4 | .83 |
| DTGA | 6.9 | .02 | −2.2 | .45 | −9.1 | <.001 | −8.1 | <.001 | −1.8 | .23 | −1.5 | .33 |
| TOF | −4.3 | .10 | −14.2 | <.001 | −7.2 | <.001 | −6.5 | <.001 | −0.2 | .84 | 0.0 | .97 |
| DORV | −5.3 | .37 | −15.1 | .01 | −0.5 | .87 | −4.1 | .15 | −2.4 | .42 | −1.5 | .62 |
| IAA | 5.7 | .26 | −3.7 | .43 | −10.5 | <.001 | −9.4 | <.001 | 3.0 | .16 | 3.7 | .13 |
| TAPVR | −2.5 | .54 | −10.5 | .01 | −7.6 | .01 | −6.6 | .01 | −5.2 | .09 | −5.6 | .10 |
| Coarctation | −10.5 | <.001 | −19.0 | <.001 | −8.7 | <.001 | −8.8 | <.001 | −1.9 | .15 | −1.9 | .15 |
| Noncardiac anomaly | 1.8 | .47 | 0.5 | .84 | 1.0 | .44 | 0.8 | .49 | 1.2 | .20 | 1.1 | .27 |
| Gestational age (wk) | −2.4 | <.001 | −2.8 | <.001 | −0.2 | .29 | −0.1 | .34 | 0.1 | .49 | 0.1 | .33 |
| Chronic conditions | 1.1 | |||||||||||
| +1 | 14.4 | <.001 | 12.2 | <.001 | 3.6 | .001 | 2.9 | .001 | 1.0 | .21 | 0.9 | .26 |
| >+2 | 31.2 | <.001 | 27.2 | <.001 | 11.0 | <.001 | 8.8 | <.001 | 2.7 | .02 | 2.5 | .03 |
Bold values represent significance of P <.05 in model.
Additional predictors included in the model were sex, maternal race, maternal age, insurance and geographic poverty, and rurality based on census tract of maternal address at birth.
Marginal change represents change in hospital days.
Footnotes
Portions of this study were presented at the American College of Cardiology Scientific Sessions, April, 2016, Chicago, IL.
References
- 1.Hoffman JI. Incidence of congenital heart disease: II. Prenatal incidence. Pediatr Cardiol 1995;16:155–65. [DOI] [PubMed] [Google Scholar]
- 2.Russo CA, Elixhauser A. Hospitalizations for birth defects, 2004. HCUP statistical brief #24. Rockville (MD): Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- 3.Waitzman NJ, Scheffler RM, Romano PS. The cost of birth defects: estimates of the value of protection. 1st ed. Lanham: University Press of America; 1996. [Google Scholar]
- 4.Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics 2001;107:E32. [DOI] [PubMed] [Google Scholar]
- 5.Peterson C, Dawson A, Grosse SD, Riehle-Colarusso T, Olney RS, Tanner JP, et al. Hospitalizations, costs, and mortality among infants with critical congenital heart disease: how important is timely detection? Birth Defects Res A Clin Mol Teratol 2013;97:664–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boulet SL, Grosse SD, Riehle-Colarusso T, Correa-Villasenor A. Health care costs of congenital heart defects. In: Wyszynksi D, Graham TP, Correa-Villasenor A, eds. Congenital heart defects: from origin to treatment. Oxford University Press; 2010. p. 493–501. [Google Scholar]
- 7.Simeone RM, Oster ME, Cassell CH, Armour BS, Gray DT, Honein MA. Pediatric inpatient hospital resource use for congenital heart defects. Birth Defects Res A Clin Mol Teratol 2014;100:934–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Copel JA, Tan AS, Kleinman CS. Does a prenatal diagnosis of congenital heart disease alter short-term outcome? Ultrasound Obstet Gynecol 1997;10:237–41. [DOI] [PubMed] [Google Scholar]
- 9.Garson A Jr, Allen HD, Gersony WM, Gillette PC, Hohn AR, Pinsky WW, et al. The cost of congenital heart disease in children and adults. A model for multicenter assessment of price and practice variation. Arch Pediatr Adolesc Med 1994;148:1039–45. [DOI] [PubMed] [Google Scholar]
- 10.Pasquali SK, Peterson ED, Jacobs JP, He X, Li JS, Jacobs ML, et al. Differential case ascertainment in clinical registry versus administrative data and impact on outcomes assessment for pediatric cardiac operations. Ann Thorac Surg 2013;95:197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Romley JA, Chen AY, Goldman DP, Williams R. Hospital costs and inpatient mortality among children undergoing surgery for congenital heart disease. Health Serv Res 2014;49:588–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldkamp M, Macleod L, Young L, Lecheminant K, Carey JC. The methodology of the Utah Birth Defect Network: congenital heart defects as an illustration. Birth Defects Res A Clin Mol Teratol 2005;73:693–9. [DOI] [PubMed] [Google Scholar]
- 13.Oster ME, Aucott SW, Glidewell J, Hackell J, Kochilas L, Martin GR, et al. Lessons learned from newborn screening for critical congenital heart defects. Pediatrics 2016;137:pii: e20154573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Botto LD, Lin AE, Riehle-Colarusso T, Malik S, Correa A. Seeking causes: classifying and evaluating congenital heart defects in etiologic studies. Birth Defects Res A Clin Mol Teratol 2007;79:714–27. [DOI] [PubMed] [Google Scholar]
- 15.Feldkamp ML, Carey JC, Pimentel R, Krikov S, Botto LD. Is gastroschisis truly a sporadic defect?: familial cases of gastroschisis in Utah, 1997 to 2008. Birth Defects Res A Clin Mol Teratol 2011;91:873–8. [DOI] [PubMed] [Google Scholar]
- 16.DuVall SL, Fraser AM, Rowe K, Thomas A, Mineau GP. Evaluation of record linkage between a large healthcare provider and the Utah Population Database. J Am Med Inform Assoc 2012;19:e54–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirchhoff AC, Fluchel MN, Wright J, Ying J, Sweeney C, Bodson J, et al. Risk of hospitalization for survivors of childhood and adolescent cancer. Cancer Epidemiol Biomarkers Prev 2014;23:1280–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peterson C, Xu L, Florence C, Grosse SD, Annest JL. Professional Fee Ratios for US Hospital Discharge Data. Med Care 2015;53:840–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.(HCUP) HCaUP. In: Quality AfHRa, ed. HCUP databases. Rockville (MD): Agency for Healthcare Research and Quality; 2017. [Google Scholar]
- 21.Kaul S, Barbeau B, Wright J, Fluchel M, Kirchhoff AC, Nelson RE. Statewide longitudinal hospital use and charges for pediatric and adolescent patients with cancer. J Oncol Pract 2015;11:e468–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res 2016;53:175–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA 1996;276:1253–8. [PubMed] [Google Scholar]
- 24.Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on cost-effectiveness in health and medicine. JAMA 1996;276:1339–41. [DOI] [PubMed] [Google Scholar]
- 25.Connor JA, Gauvreau K, Jenkins KJ. Factors associated with increased resource utilization for congenital heart disease. Pediatrics 2005;116:689–95. [DOI] [PubMed] [Google Scholar]
- 26.Ungerleider RM, Bengur AR, Kessenich AL, Liekweg RJ, Hart EM, Rice BA, et al. Risk factors for higher cost in congenital heart operations. Ann Thorac Surg 1997;64:44–8, discussion 9. [DOI] [PubMed] [Google Scholar]
- 27.Geppert J, Rhoda D, Morara M. Quality Indicator Empirical Methods (Revised by Battelle, under Contract No. HHSA290201200001C). Rockville, MD: Agency for Healthcare Research and Quality. September 2013. [Google Scholar]
- 28.Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 2001;87:1367–71. [DOI] [PubMed] [Google Scholar]
- 29.Epstein AM, Stern RS, Weissman JS. Do the poor cost more? A multihospital study of patients’ socioeconomic status and use of hospital resources. N Engl J Med 1990;322:1122–8. [DOI] [PubMed] [Google Scholar]
- 30.Griswold M, Parmigiani G, Potosky A, Lipscomb J. Analyzing health care costs: a comparison of statistical methods motivated by Medicare colorectal cancer charges. Biostatistics 2004;1:1–23. [Google Scholar]
- 31.Martin JA, Hamilton BE, Osterman MJ. Births in the United States. NCHS Data Brief 2015;2016:1–8. [PubMed] [Google Scholar]
- 32.Simeone RM, Oster ME, Hobbs CA, Robbins JM, Collins RT, Honein MA. Population-based study of hospital costs for hospitalizations of infants, children, and adults with a congenital heart defect, Arkansas 2006 to 2011. Birth Defects Res A Clin Mol Teratol 2015;103:814–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dawson AL, Cassell CH, Oster ME, Olney RS, Tanner JP, Kirby RS, et al. Hospitalizations and associated costs in a population-based study of children with Down syndrome born in Florida. Birth Defects Res A Clin Mol Teratol 2014;100:826–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoon PW, Bresee JS, Olney RS, James LM, Khoury MJ. Epidemiology of biliary atresia: a population-based study. Pediatrics 1997;99:376–82. [DOI] [PubMed] [Google Scholar]
- 35.Waitzman NJ, Romano PS, Scheffler RM. Estimates of the economic costs of birth defects. Inquiry 1994;31:188–205. [PubMed] [Google Scholar]
- 36.Bell J, Nassar N, Turner R, Bower C, Gillett D, McBain W, et al. Hospitalisations up to adulthood for children born with orofacial clefts. J Paediatr Child Health 2016;52:441–8. [DOI] [PubMed] [Google Scholar]
- 37.Bell JC, Nassar N, Bower C, Turner RM, Raynes-Greenow C. Long-term survival for infants born with orofacial clefts in Western Australia. Birth Defects Res A Clin Mol Teratol 2016;106:172–7. [DOI] [PubMed] [Google Scholar]
- 38.Razzaghi H, Dawson A, Grosse SD, Allori AC, Kirby RS, Olney RS, et al. Factors associated with high hospital resource use in a population-based study of children with orofacial clefts. Birth Defects Res A Clin Mol Teratol 2015;103:127–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oster ME, Kim CH, Kusano AS, Cragan JD, Dressler P, Hales AR, et al. A population-based study of the association of prenatal diagnosis with survival rate for infants with congenital heart defects. Am J Cardiol 2014;113:1036–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Islam S, Yasui Y, Kaul P, Marelli AJ, Mackie AS. Congenital heart disease hospitalizations in Canada: a 10-year experience. CanJ Cardiol 2016;32:197–203. [DOI] [PubMed] [Google Scholar]
- 41.Martin AB, Hartman M, Washington B, Catlin A, National Health Expenditure Accounts T. National health spending: faster growth in 2015 as coverage expands and utilization increases. Health Aff (Millwood) 2017;36:166–76. [DOI] [PubMed] [Google Scholar]
- 42.van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol 2011;8:50–60. [DOI] [PubMed] [Google Scholar]
- 43.Danford DA, Karels Q, Kutty S. Variabilities in the mortality-related resource utilisation for congenital heart disease. Open Heart 2016;3:e000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McDermott KW, Elixhauser A, Sun R. Trends in hospital inpatient Stays in the United States, 2005-2014. In: Quality AfHRa, ed. HCUP statistical brief. Rockville (MD): Agency for Healthcare Research and Quality; 2017. (IBM Watson Health), (AHRQ). [Google Scholar]
- 45.Smith AH, Gay JC, Patel NR. Trends in resource utilization associated with the inpatient treatment of neonatal congenital heart disease. Congenit Heart Dis 2014;9:96–105. [DOI] [PubMed] [Google Scholar]
- 46.Gerber AU, Torre AH, Buscher G, Stock SA, Graf C, Schickendantz S, et al. Direct non-medical and indirect costs for families with children with congenital cardiac defects in Germany: a survey from a university centre. Cardiol Young 2010;20:178–85. [DOI] [PubMed] [Google Scholar]
- 47.Connor JA, Kline NE, Mott S, Harris SK, Jenkins KJ. The meaning of cost for families of children with congenital heart disease. J Pediatr Health Care 2010;24:318–25. [DOI] [PubMed] [Google Scholar]
- 48.Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood) 2001;20:9–18. [DOI] [PubMed] [Google Scholar]
- 49.Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics 2013;131:e1502–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


