Abstract
Testicular tumors are the most common tumors in adolescent and young men and germ cell tumors (TGCTs) account for most of all testicular cancers. Increasing incidence of TGCTs among males provides strong motivation to understand its biological and genetic basis. Gains of chromosome arm 12p and aneuploidy are nearly universal in TGCTs, but TGCTs have low point mutation rate. It is thought that TGCTs develop from premalignant intratubular germ cell neoplasia that is believed to arise from the failure of normal maturation of gonocytes during fetal or postnatal development. Progression toward invasive TGCTs (seminoma and nonseminoma) then occurs after puberty. Both inherited genetic factors and environmental risk factors emerge as important contributors to TGCT susceptibility. Genome-wide association studies have so far identified more than 30 risk loci for TGCTs, suggesting that a polygenic model fits better with the genetic landscape of the disease. Despite high cure rates because of its particular sensitivity to platinum-based chemotherapy, exploration of mechanisms underlying the occurrence, progression, metastasis, recurrence, chemotherapeutic resistance, early diagnosis and optional clinical therapeutics without long-term side effects are urgently needed to reduce the cancer burden in this underserved age group. Herein, we present an up-to-date review on clinical challenges, origin and progression, risk factors, TGCT mouse models, serum diagnostic markers, resistance mechanisms, miRNA regulation, and database resources of TGCTs. We appeal that more attention should be paid to the basic research and clinical diagnosis and treatment of TGCTs.
Keywords: Spermatogenesis, Teratoma, Risk factors, Platinum resistance, Serum makers, MiRNA, Mouse models, Database
Introduction
TGCTs are rare tumors in the general population, but are the most commonly occurring malignancy among males between ages 15 and 44 years [1]. The diagnosis of TGCTs primarily depends on physical examination, ultrasonography, magnetic resonance imaging, measurement of serum tumor markers and pathological examination. Standard treatment for TGCTs is radical orchiectomy and/or combination with chemotherapy or radiotherapy or retroperitoneal lymph node dissection. Furthermore, small interfering RNA therapy [2, 3], microRNA therapy [4, 5] and immunotherapy [6] are suggested to be potential therapeutic strategies; however, there is a long road ahead for such treatments to prove their clinical value. Significant parameters, such as angiolymphatic invasion, degree of extra testicular invasion, rete testis invasion and serum tumor marker levels [7], oncogenes [8], promoter methylation [9], polymorphism [10] and tumor-infiltrating immunocytes [11] are suggested as potential prognostic factors for TGCT patients.
TGCTs are characterized by frequent chromosomal anomalies and low rates of somatic mutations. Chromosome arm 12p amplification, such as isochromosome 12p and chromosome 12p overrepresentation, is the most common genetic hallmark that accounts for many types of TGCTs [12, 13]. The exact mechanisms of 12p gain in TGCTs are unclear, but the ubiquitous gain of 12p-derived sequences implies a significant role for some genes on 12p, such as CCND2, KRAS, TNFRSF1A, GLUT3, REA, NANOG, DPPA3, and GDF3 [14–17], in the development, pluripotency maintenance and/or progression of TGCTs.
It is not accurate to say that TGCTs are completely curable malignancies. According to the European Association of Urology (EAU) testis cancer guidelines, approximately 15–30% of TGCT patients will relapse after first-line chemotherapy and will require additional salvage therapies [18, 19]. Primary TGCTs have been reported to metastasize to the retroperitoneal lymph nodes [20], brain [21, 22], neck [23, 24], heart [25, 26], pulmonary arteries [27], inferior vena cava and aorta [28], lung [29], liver [30], stomach [31, 32] and cartilage [33]. Long-term relative survival after diagnosis of TGCTs generally continued to decline with increasing follow-up time, particularly beyond 15–30 years [34]. The side effect of TGCT therapy on other organs also offers insight into the long-term risks of TGCT survivorship. Kidney disease [35], cerebrovascular accidents, secondary leukemia, internal carotid artery occlusion and stroke associated with chemotherapy in TGCT patients have been occasionally described in the literature [36–42].
More recently, focus has expanded beyond survival to emphasize the quality of life issues when optimizing treatment algorithms. Attention should be paid toward persisting physical symptoms and psychosocial needs. Patients with TGCTs and azoospermia, submitted to onco-testicular sperm extraction and sperm cryopreservation, had the delivery of a healthy baby after intracytoplasmic sperm injection, which emphasizes the importance of fertility preservation in oncology patients [43, 44]. For patients with bilateral TGCTs, testis-sparing surgery provides a better quality of life (e.g., sufficient endogenous testosterone production) and may be considered a safe, feasible alternative treatment [45, 46]. Testicular self-examination (TSE) practices are found to be inadequate and efforts should be made to develop programs that can increase knowledge related to testicular cancer as well as the practice of TSE [47].
Herein, we present a comprehensive review on origin, progression, histological types, risk factors, TGCT mouse models, serum diagnostic markers, resistance mechanisms, miRNA regulation and database resources of TGCTs.
Origin, progression and histological types of TGCTs
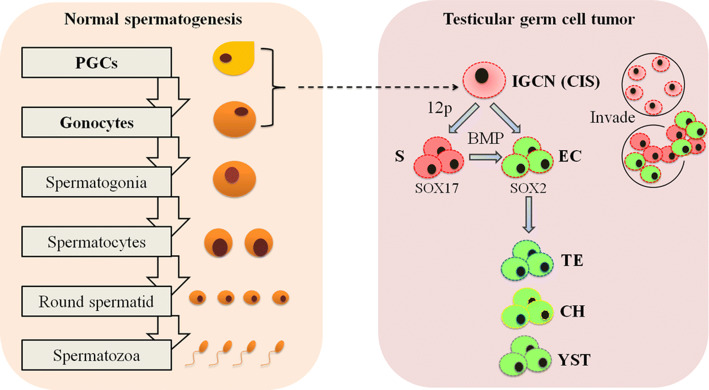
Spermatogenesis is fundamental to the establishment and maintenance of male fertility. Given that TGCTs are believed to arise from failure of normal maturation of gonocytes, understanding the process and regulatory controls of spermatogenesis will provide valuable insights into the occurrence and features of TGCTs. It is generally considered that mammalian spermatogenesis is a complex sequential process of germ cell differentiation from primordial germ cells (PGCs) or spermatogonial stem cells (SSCs) to functional haploid sperm [48, 49] (Fig. 1, left). Spermatogenesis further requires intricate interaction between germ cells (spermatogonia, spermatocytes, round/elongating spermatids) and supporting somatic cells (Sertoli cells, Leydig cells, peritubular myoid cells, endothelial cells, macrophage and newly discovered innate lymphoid and mesenchymal cells) [50–54]. Recent single-cell RNA sequencing of murine or human spermatogenesis reveals a continuous developmental trajectory of germ cells from spermatogonia to spermatids (12 or 14 germ cell states) and identifies cell type-specific markers and candidate transcription regulators in each cell component [55, 56], representing a community resource and foundation to in-depth study of spermatogenesis.
Fig. 1.
Model of normal spermatogenesis and occurrence of TGCTs. Spermatogenesis is a tightly regulated process of the continuous supply of spermatozoa. Differentiation of primordial germ cells (PGCs) into gonocytes, self-renewal and differentiation of spermatogonial stem cells, and subsequent commitment to meiotic spermatocytes and haploid round/elongating spermatids are the key events of spermatogenesis. Under pathological conditions, gonocytes that fail to undergo correct spermatogenic differentiation, but develop into intratubular germ cell neoplasia (IGCN) or carcinoma in situ (CIS) represent the precursor cells for TGCTs during early stage of germline development. CIS can further progress into invasive seminoma (S) and (or then) nonseminoma, including undifferentiated EC, as well as differentiated teratoma (TE), choriocarcinoma (CH) and yolk sac tumor (YST)
The histogenesis of TGCTs is complex. It is thought that TGCTs develop from premalignant intratubular germ cell neoplasia (IGCN), also known as carcinoma in situ (CIS), that are believed to arise from failure of normal maturation of fetal germ cells from PGCs into pre-spermatogonia [57]. Expression profiling studies reveal that IGCN cells closely parallel PGCs and maintain their genome in a demethylated and undifferentiated state [58, 59]. IGCN progresses toward invasive TGCTs then after puberty, when IGCN cells begin to proliferate, likely involving the influences of hormones. TGCTs are classified broadly into two major histologic groups: seminoma and non-seminoma germ cell tumors. Non-seminoma can be further subdivided into undifferentiated embryonal carcinoma (EC), as well as differentiated teratoma, choriocarcinoma and yolk sac tumor [60] (Fig. 1, right). Both IGCN and TGCT cells are typically aneuploid, but premalignant IGCN does not gain chromosomal material from 12p, which are pathognomonic for malignant IGCN and TGCTs [61, 62]. Transition from IGCN to invasive TGCTs is associated with the loss of PTEN and P21 as well as gain of MDM2 expression [63, 64]. KRAS mutations are exclusive to the primary TGCT tumors and not in the patient-matched pre-invasive IGCN [65]. Seminoma and EC present significant differences in clinical features, therapy and prognosis, and they show characteristics of the PGCs and embryonic stem cells (ESCs), respectively [66]. For proper diagnosis of the different histological subgroups of TGCTs, immunological staining is required using distinctive molecular markers. POU class 5 homeobox 1 (POU5F1, also known as OCT3/4), is positive in IGCN, seminoma and EC, but not in any choriocarcinoma, teratoma or YST [67]. KIT proto-oncogene receptor tyrosine kinase (KIT, also known as CD117), is positive in IGCN and seminoma and negative in EC [68]. TNF receptor superfamily member 8 (TNFRSF8, also known as CD30) expression helps pathologists to identify sites of EC in the tumors [69]. Furthermore, Glypican 3 (GPC3) is useful as an immunohistochemical marker for TGCTs differentiated to extraembryonic tissue, especially YST [70, 71]. Moreover, Sal-like protein 4 (SALL4) is a more sensitive marker than α-fetoprotein (AFP) and GPC3 for YST [72]. Integration of tumor characteristics and high-dimensional assays of genomic, epigenomic, transcriptomic and proteomic features [73] recently reveals novel distinctive molecular landscapes of TGCT histologic types and identifies previously unappreciated diversity within each component, including a separate subset of seminoma defined by KIT mutations.
The precise mechanism of the progression from premalignant IGCN to subtypes of invasive tumors is not completely understood. IGCN gives rise to seminoma and EC separately or seminoma is the intermediate stage between IGCN and EC remains a matter of debate. The first hypothesis is supported by the observation that IGCN is a phenotypically heterogeneous lesion containing cells in different stages of progression [74, 75], and KIT mutations are observed in a subset of seminoma, but not in EC [73]. The latter model is set up mainly on the basis of the phenotypic resemblance of seminoma to IGCN, learning from the studies of ploidy [76], cytogenetics [77] and pathomorphology [78]. Several studies support the common clonal origin of metastatic mature teratoma with other components of a mixed germ cell tumor [79, 80]. Intriguingly, transplantation of seminoma-like cell line TCam-2 into the seminiferous tubules results in the formation of an IGCN/seminoma, while transplantation into the flank or corpus striatum will trigger TCam-2 cells to adopt an EC-like fate. This model suggests that transition of seminoma to ECs relies on signals from the tumor microenvironment [81]. During this reprogramming, the microenvironment inhibition of bone morphogenetic protein (BMP) signaling is the initial event, resulting in activation of NODAL signaling, upregulation of pluripotency factors (e.g., SOX2) and downregulation of seminoma markers (e.g., SOX17) [82, 83]. It will be interesting to further investigate whether EC can transit into seminoma upon interference with microenvironment factors.
Risk factors of TGCTs
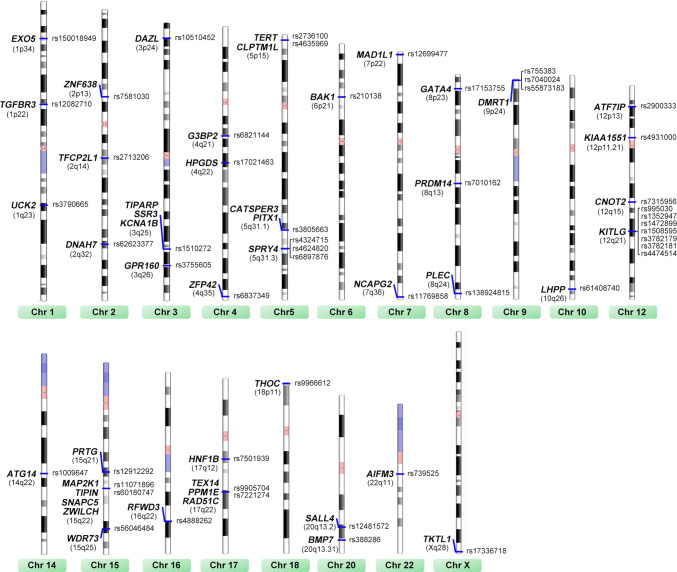
The increased (4- to 10-fold) risk of TGCTs among brothers and sons of affected men together with findings in twin studies supports a strong genetic component contributing to TGCT susceptibility [84–88]. Genome-wide association studies (GWAS) have been particularly effective in identifying multiple common variants with strong contribution to TGCT risk. Initial GWAS studies identified allele variation within the c-KIT ligand (KITLG) on 12q22 as the strongest genetic risk factor for TGCTs (per-allele OR > 2.6) [89, 90]. Approximately, 40 identified allele variations on chromosomes conferring TGCT susceptibility [91–101] are summarized in Fig. 2. Pathway-based analysis of GWAS data reveals the association of PGC formation, sex determination/differentiation, spermatogonial maintenance genes (e.g., KITLG [102], PRDM14 [103], DMRT1 [104], GATA4 [50] and DAZL [105]) with susceptibility to TGCTs. TGCT GWAS to date have been fairly small compared with those seen for other diseases, and multiple additional TGCT susceptibility loci and their functional characteristics remain to be identified.
Fig. 2.
The current known TGCT susceptibility loci that have been identified through GWAS. Single nucleotide polymorphisms, locus on chromosome (Chr) and candidate gene or genes are listed
In addition to genetic susceptibility loci, significate risk factors for the development of TGCTs include cryptorchidism [106], disorders of sex development [107], hypo/infertility [108], contralateral germ cell tumors [109] and endogenous and exogenous hormones [110]. Although the sample size is insufficient and reliable correlation should be established, environmental risk factors are currently estimated to account for half of TGCT predisposing reasons. If necessary, patients with high risks of TGCT occurrence such as family history of TGCTs, infertility and environmental risk exploration may be notified to take physical and genetic screening for the genetic susceptibility loci, credible prognosis markers or premalignant IGCN lesion.
Mouse models for TGCT study
Animal models, such as mouse models, provide novel insights into the molecular mechanisms underlying the origin, progression and development of TGCTs. Mouse strains with low versus high teratoma incidence (129 versus 129.MOLF-Chr 19 (M19)) provide original in-depth research of TGCTs in mice. M19 carries chromosome (Chr) 19 from the MOLF, whereas all other chromosomes are from the 129 strain. Approximately, 70% of M19 males develop TGCTs in contrast to approximately 5% in the 129 strain, suggesting that Chr 19 contains susceptibility loci of TGCTs [111, 112]. However, potential loci on Chr 19 have not been identified by GWAS yet.
The origin of TGCT cells predicts that developmental pathways that control germ cell pluripotency or differentiation may be involved in the malignant transformation of these cells. Using mouse strains of 129, M19 and FVB (resistant to teratoma formation), a previous study suggests that ectopic germ cell proliferation and dysexpression of germ cell pluripotency and differentiation-associated factors at a specific developmental time point, E15.5, are directly correlated with increased teratoma risk [113]. Nodal-knockout mice show premature differentiation and reduced pluripotency marker expression, and NODAL signaling components are overexpressed in human TGCT samples [114]. In contrast, germ cell expression of male sex determination gene Nanos2 is relatively low in teratoma-susceptible mouse strains and deficiency for Nanos2 increases teratoma incidence in 129 mice [115]. Furthermore, DMRT1 controls the mitosis–meiosis switch in mice and humans and loss of Dmrt1 in 129 strain mice results in a > 90% incidence of testicular teratomas [104, 116]. These genetic studies in mouse models further advance our understanding that delayed male germ cell specification and retained pluripotency may cause gonocytes to form IGCN, EC foci and teratoma on a susceptible genetic background.
An increase in tumor incidence in mice has proven to be relevant to understanding genetic risk factors for TGCTs in humans. One good example is that loss of the transmembrane Kit ligand (kitl) increases TGCT susceptibility in 129 mice [117]. GWAS have identified KITLG as a solid TGCT risk gene in humans accordingly [89]. TGCT occurrence is observed at higher incidence in mice mutant for Dnd1 [118] or Pten [119] or A1cf/Ago2 [120] in 129 inbred strains. Furthermore, spindle-associated Rhamm acts as a gatekeeper preventing IGCN initiation, because seminoma occurred in 3.7% of Rhamm mutant male mice [121]. Pierpont et al. recently developed a novel mouse TGCT model by germ cell-specific Kras activation and Pten inactivation in 129 backgrounds that developed malignant and metastatic TGCTs composed of teratoma and EC [122]. Mouse models provide biological insight into TGCT development, but their relevance to human tumorigenesis is limited, as no mutations of genes such as RHAMM and ALCF/AGO2 have been shown in human TGCTs. Whether mouse TGCT models precisely reflect the biology of human TGCTs requires to be determined.
Serum diagnostic tests for TGCTs
Compared to other solid organ malignancies, the role of serum tumor markers in TGCTs is unprecedented; these markers are fully used in the diagnosis, staging, risk stratification and surveillance of patients with TGCTs [123]. The most common serum tumor markers for TGCTs include α-fetoprotein (AFP) and human chorionic gonadotropin (hCG) [123]. They are relatively sensitive, specific and clinically useful tumor markers for TGCTs, providing value on diagnosis, classification, staging and prediction. Some progresses have been achieved to find novel serum biomarkers with good sensitivity and accuracy. MicroRNAs (miRNAs) are short non-coding RNAs that show exciting promise as a new-style biomarker of TGCTs [124]. The sensitivity and specificity of miR-371a-3p alone is ~ 90% for the diagnosis of malignant TGCTs [125], but that value can be increased further by using a combination of other miRNAs, including miR-372-3p, miR-373-3p and miR-367-3p [126–128]. Furthermore, miR-371a-3p serum level is increased in recurrence of TGCT patients, indicating its additional value as a biomarker for detecting disease relapse in TGCT patients [129]. The value of miRNA serum markers needs to be validated in more studies or a prospective clinical trial. Moreover, patients in the yolk sac seminoma subgroup have the poorest clinical outcome, tending to undergo somatic transformation and chemoresistance [130]; however, identification of subtype-specific serum biomarkers is still a big challenge.
Resistance of TGCTs
TGCTs are highly curable tumors in most cases, because of the exquisite sensitivity of seminoma and EC to DNA damaging agents; however, teratomas are mostly resistant to chemotherapeutic drugs [131]. Given that TGCTs are unique in their responsiveness to platinum-based chemotherapy, they are considered as a model for exploring the molecular mechanisms behind the exceptional sensitivity of TGCT cells to DNA damaging chemotherapeutics. At present, various hypotheses on the platinum hypersensitivity of TGCT cells have been reported. An easily activated apoptotic response and the deficiency of the DNA damage response/repair activation may account for this behavior [132, 133]. The tumor-suppressor gene TP53 commonly mutated in solid tumors is rarely mutated in TGCTs (~ 1.29%) [134] and silencing of TP53 is sufficient to abrogate the hypersensitivity of TGCT cells to cisplatin [135]. A recent clinical whole-exome and transcriptome sequencing study proposes that the basis of chemosensitivity in TGCTs with a wild-type TP53 genomic background is a result of a fundamental apoptotic propensity caused by increased mitochondrial priming [65]. HMGB4, a protein preferentially expressed in testes, uniquely blocks excision repair of cisplatin–DNA adducts, 1,2-intrastrand cross-links, to potentiate the sensitivity of TGCT cells to cisplatin therapy [136]. Furthermore, chemoresistant teratomas or transformed carcinomas are associated with continued progression of reciprocal loss of heterozygosity (RLOH) copy number and reduction of pluripotency markers (NANOG and OCT3/4) [65]; however, it is uncertain whether the loss of pluripotency markers is a driver of chemoresistance.
Although the majority of TGCTs will respond with excellent cure rates, some (more than 10%) patients will relapse or demonstrate refractory disease after operation and chemotherapy. Limited options exist for patients with platinum refractory disease [137]. Exploring the mechanisms underlying platinum resistance and identifying novel treatment options that are effective in the platinum-refractory patients require an urgent priority. Both activation of the PDGFRβ-AKT pathway [138] and overexpression of MAD2γ [139] or cytoplasmic p21 [140] are explored to contribute to cisplatin-acquired resistance in TGCT cells. In contrast, disrupting MDM2-TP53 interaction [141] or stimulating expression of miR-302a [142] or miR-383 [143] increases the sensibility of TGCT cells to cisplatin exposure. Notably, compound HP-14 and poly(ADP-ribose) polymerase (PARP) inhibitor restrain the growth of cisplatin-resistant TGCT cells [144, 145].
The mutation rate is uniformly low in TGCTs [73] and no significant difference is observed in the mutational rate between seminoma and non-seminoma cases [146]. Intriguingly, several clinical studies of TGCT patients with different response to chemotherapy indicate that some gene mutations exhibit discrepancy between resistance and sensitivity. There is a significantly higher incidence of BRAF [147] and XRCC2 [146] mutation in chemotherapy-resistant TGCTs compared with sensitive controls. Furthermore, mutations in AKT1 and PIK3CA are observed exclusively in cisplatin-resistant tumors [148]. Polymorphisms of BLMH [149], PAI-1 [150], GSTP1 [151], ARVCF [152], TPMT and COMT [153] are associated with reduced survival, higher prevalence of early relapses, platinum refractory and chemotherapy-related organ toxicity after chemotherapy for TGCT patients. Although TP53 mutations rarely occur in TGCTs, a recent study of whole-exome and targeted sequencing of cisplatin-sensitive and -resistant TGCTs suggests that TP53 alterations (16.3% vs. 0%) and combined MDM2/TP53 alterations (24.0% vs. 2.6%) are more common among cisplatin-resistant TGCTs than sensitive ones [154]. Unlike testicular primary tumors, mediastinal primary nonseminoma has frequent TP53 alterations (72.2% vs. 2.5%) and an increased rate of platinum-based therapy resistance, resulting in survival of only ~ 50% [154]. It is noteworthy that several studies support the common clonal origin of metastatic mature teratoma with other components of a mixed germ cell tumor [79, 80]. It’s still an open question why different subtypes of a mixed TGCT show the diversity of the above identified mutations and how genetics determine cisplatin resistance. In phase II studies, the combination of gemcitabine, oxaliplatin and paclitaxel achieves long-term overall survival (> 2 years) in ~ 20% of patients with cisplatin-refractory or multiply relapsed TGCTs [137, 155]. By contrast, limited effects are reported in patients treated with sunitunib [156], oxaliplatin plus bevacizumab [157] or everolimus [158].
Emerging role of miRNAs
MiRNAs recently emerge as an important regulator of TGCT cells. MiRNA expression profiles of TGCTs and normal testis tissues using small RNA sequencing reveal numerous dysregulated miRNAs in TGCTs [159, 160]. Compared with normal testes, the expression of some miRNAs (e.g., miR-199a-5p/3p, miR-514a-3p) is downregulated, while others, such as miR-223-3p, is overexpressed in TGCT tissues. Recent research has confirmed the role of miRNAs as either tumor suppressors or activators (oncomiRs) in TGCT cells. Subsequent identification of functional miRNAs–mRNAs interactions in TGCT cells helps delineate post-regulatory mechanisms and may lead to new therapies.
Forced expression of miR-199a-5p/3p in TGCT cells leads to suppression of cell growth, cancer migration, invasion and metastasis [161], indicating that miR-199a-5p/3p may act as a tumor-suppressor miRNA. Tumor cell suppression activity of the miR-199a-5p is mediated by its target PODXL [161] and MAFB [4], while miR-199a-3p inhibits tumor cell growth and migration via targeting transcription factor SP1 and glucose metabolism [5]. Furthermore, miR-199a-5p/3p and miR-214 can form a self-regulatory network via PSMD10-TP53-DNMT1 in TGCT cells [162]. MiR-514a-3p induces apoptosis through direct regulation of PEG3 and PEG3-mediated activation of the NF-kappa B pathway [159]. High miR-223-3p expression in TGCT cells targets FBXW7 to promote cell growth and inhibit apoptosis in TGCT cell lines [163]. OncomiR miR-1297 promotes growth of TGCT cells via targeting tumor-suppressor gene PTEN [164] and long-noncoding RNA MEG3 contradicts the inhibitory effects of miR-1297 on PTEN [165]. In vivo evidence should be included in miRNA studies to validate the involvement of miRNAs in TGCT progression in future.
Database to stimulate TGCT study
Gene Expression Omnibus (GEO) is an international public repository that archives and freely distributes microarray, next-generation sequencing and other forms of high-throughput functional genomics data submitted by researchers. The GEO database can be searched using many different attributes including keywords (e.g., testicular germ cell tumor) and GEO accession (e.g., GSE1818). Furthermore, the GEO2R in GEO website allows us to compare two or more groups of samples in a GEO series to identify differentially expressed items and thus provides a simple interface that allows users to perform analysis without R statistical expertise. Taking the advantage of the GEO database, we can obtain informative knowledge about TGCTs. For example, GSE1818 provides RNA profiling of normal testis (n = 3), IGCN (n = 3), seminoma (n = 3), EC (n = 5), yolk sac (n = 4), teratoma (n = 4) and choriocarcinoma (n = 1). Using GEO2R to perform multiple comparisons, a series of predominant genes are observed for normal testis (e.g., KIF2A, DDEF2, and TBPL1), IGCN (e.g., CYP17A1 and ACE2), seminoma (e.g., CAPNS1, ZKSCAN3, and EIF3F), EC (e.g., GAL, BCAT1, and CALB1), yolk sac (e.g., APOA2 and CYP26A1), teratoma (e.g., COL1A1, COL61, and MFAP4) and choriocarcinoma (e.g., INSL4, CRH, and HTRA4) (Fig. 3a). It will be interesting to identify specific marker genes that mark the formation of IGCN and transition from IGCN to invasive TGCTs, because measures can be taken before IGCN progression toward malignant and invasive TGCTs or their relapse. Furthermore, RNA profiling of relapsed seminoma (n = 15), non-relapsed seminoma (n = 15), relapsed non-seminoma (n = 12) and non-relapsed non-seminoma (n = 15) is included in GSE99420. Differentially expressed genes (DEGs) are obtained by GEO2R analysis between relapsed TGCTs and non-relapsed TGCTs (Fig. 3b). Moreover, GSE14231 identifies significant changes of RNA profiling in three human TGCT cell lines (833 K, GCT27 and Susa) and their cisplatin-resistant variants (n = 2 each group), and these DEGs are considered to participate in cisplatin sensitivity or resistance of TGCT cells (Fig. 3c).
Fig. 3.
GEO datasets representing a community resource to study TGCTs. a The dataset GSE1818 is particularly useful for comparisons between various histological subtypes of TGCTs versus each other or versus normal testis. b DEGs between relapsed and non-relapsed TGCTs are obtained by analyzing GSE99420. c Noel et al. provided an expression profiling of parental and cisplatin-resistant TGCT cell lines under accession no. GSE14231
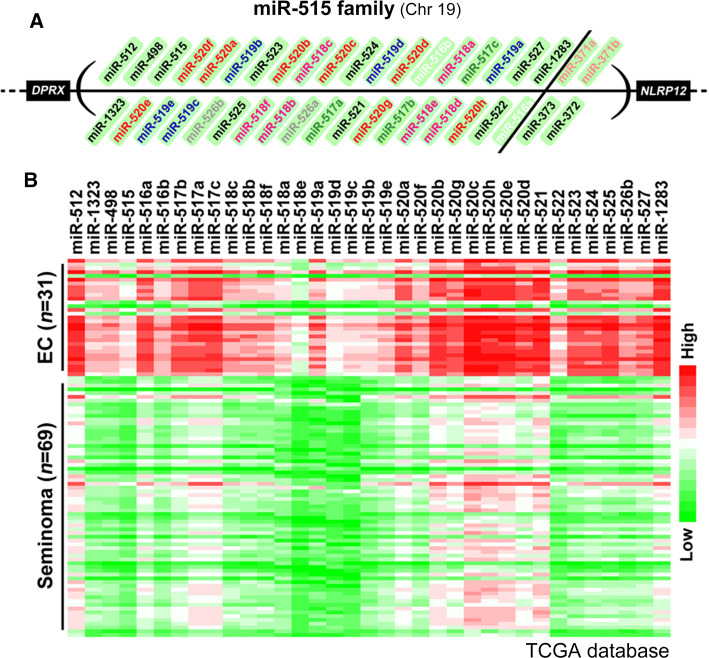
The Cancer Genome Atlas (TCGA) provides comprehensive and multi-dimensional maps of the key genomic changes in 33 types of cancer, including TGCTs. The genomic information of TCGA helps to improve the prevention, diagnosis and treatment of cancer. The cBioPortal for Cancer Genomics (http://cbioportal.org/) provides visualization, analysis and download of large-scale cancer genomics data sets, including TCGA [166, 167]. A recent systematic analysis of TCGA database concludes that TGCTs exhibit high aneuploidy and a markedly low rate of somatic mutation (mean 0.5 mutations per Mb) [73], consistent with previous exome-wide sequencing studies [146, 168, 169]. Somatic mutation of only three genes (KIT, KRAS, and NRAS) achieves significance in TGCTs, whereas large-scale copy number variation such as gain of chromosomal material from 12p is frequently observed [73]. Using TCGA and cBioPortal, a comparison of seminoma (n = 69) and EC (n = 31) samples obtains a list of differentially expressed miRNAs. Notably, miR-515 family that lists between DPRX and NLRP12 gene in Chr 19 accounts for approximately 55% of predominantly expressed genes in EC as compared with seminoma (Fig. 4). The role of miR-515 family in the distinction of EC from seminoma deserves further investigation.
Fig. 4.
An example of data analysis using TCGA and cBioPortal. MiRNA profiling data of 31 patients with EC and 69 patients with seminoma was extracted from the TCGA database and DEGs were analyzed. Notably, miR-515 family that lists between DPRX and NLRP12 gene in Chr 19 accounts for approximately 55% of predominantly expressed genes in ECs
Concluding remarks
In summary, we described the developmental (origin and progression), genetic (susceptibility loci) and molecular (resistance mechanisms, miRNA involvement) aspects of TGCTs, and discussed the emerging TGCT mouse models, public database resources and serum diagnostic markers with application prospects.
TGCTs are histologically heterogeneous and distinctly curable with chemotherapy. One major challenge is the development of therapeutic approaches for cisplatin-refractory or multiply relapsed TGCTs. TGCTs are highly curable tumors in most cases, because of their exquisite sensitivity of seminoma and EC to DNA damaging agents; however, teratoma are mostly resistant to chemotherapeutic drugs [131]. In most cases, surgical resection is specifically required for teratomas and identifying ways to discern teratomas from nonviable tissues after chemotherapy is important to avoid unnecessary invasive surgeries. Malignant transformation of TGCTs into somatic malignancy is uncommon [170]. Patients whose primary TGCTs contain yolk sac tumor and seminoma have a poor clinical outcome, tending to undergo chemoresistance and somatic transformation within their metastatic lesions after chemotherapy [130]. Similarly, teratoma with malignant transformation had a worse prognosis than other types of TGCTs [171].
Patient-derived xenografts (PDX) are models of cancer where the tissue or cells from a patient’s tumor are implanted into immunodeficient or humanized mice. PDX provides unique opportunities for cancer research, treatment evaluation and drug discovery. However, understanding the limitations of PDX models and the difference between PDX and human tumors in their natural environment is required for optimal application. Firstly, it is vital to ensure that appropriate PDX tumor model is used, because several studies suggest that human tumors engrafted in immunodeficient mice are susceptible to the formation of lymphocytic neoplasms [172, 173]. Secondly, PDX undergo mouse-specific tumor evolution and show genomic instability; for instance, the copy number alteration landscapes of PDX change continuously and differ from those acquired in patients [174, 175]. Moreover, further development and use of mouse genetic TGCT models will provide novel insight into the underlying molecular mechanisms of TGCTs, as well as useful tools to test therapeutic strategies. Nevertheless, whether mouse TGCT models precisely reflect the biology of various subtypes of human TGCTs requires to be determined.
Targeting of tumor cells is not equivalent to targeting tumor tissues. Tumor cells display extensive and dynamic cross-talk with the microenvironment, mainly containing tumor-infiltrating lymphocytes, tumor-associated macrophages, cancer-associated fibroblasts, surrounding stroma and tumor vasculature [176]. TGCTs are frequently characterized by T lymphocyte infiltration [177]. Deep immune characterization of TGCTs shows that activated T cell infiltration is closely correlated with seminoma histology, early stage and good prognosis. Seminomas show increased T cell infiltration, decreased regulatory T cells, increased program death-ligand 1 (PD-L1) and increased program-death 1 (PD-1)/PD-L1 spatial interaction compared with non-seminoma [73, 178, 179]. EMMPRIN secreted by EC cells via membrane vesicles exerts its matrix metalloproteinase-inducing effect on fibroblasts within the tumor microenvironment to promote tumor invasion [180]; thus, EMMPRIN may predict an unfavorable prognosis in patients with TGCTs [181]. MiR-125b in TGCT tumor cells promotes TGCT xenograft growth through stimulating the recruitment of tumor-associated macrophages [182]. In addition to the intrinsic properties of tumor cells, more attention should be paid to tumor microenvironment and corresponding therapeutics directing against ‘tumor’ rather than ‘tumor cells’.
Anti-PD-1 is standard immunotherapy for multiple cancers, and the expression of its ligand, PD-L1, has been described in TGCTs [6, 183]. Immunotherapy using PD-1/PD-L1 inhibitors (e.g., pembrolizumab) has been performed to treat platinum-refractory TGCTs [184, 185]. However, a phase II study of anti-PD-1 in refractory TGCTs (Clinicaltrials.gov, NCT02499952) was terminated due to lack of efficacy. Pembrolizumab is well tolerated, but does not appear to have clinically meaningful single-agent activity [186]. brentuximab vedotin (BV) is an antibody–drug conjugate consisting of the chimeric anti-CD30 antibody conjugated to an antimitotic drug monomethylauristatin E [187–189]. A phase II trial of BV in refractory CD30-positive TGCTs (ClinicalTrials.gov, NCT01851200) has been completed; however, the clinical outcomes have not been reported.
Acknowledgements
This work was supported by the Young Elite Scientists Sponsorship Program by CAST (Grant no. YESS20160118 to SR Chen); National Natural Science Foundation of China (31501198 to SR Chen); CAS-TWAS President’s Fellowship for International PhD Students (to A Batool).
Compliance with ethical standards
Conflict of interest
The authors declare that there are no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aalia Batool, Najmeh Karimi and Xiang-Nan Wu contributed equally to this review.
References
- 1.Ghazarian AA, et al. Future of testicular germ cell tumor incidence in the United States: forecast through 2026. Cancer. 2017;123(12):2320–2328. doi: 10.1002/cncr.30597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ushida H, et al. Therapeutic potential of SOX2 inhibition for embryonal carcinoma. J Urol. 2012;187(5):1876–1881. doi: 10.1016/j.juro.2011.12.058. [DOI] [PubMed] [Google Scholar]
- 3.Yamada Y, et al. A novel prognostic factor TRIM44 promotes cell proliferation and migration, and inhibits apoptosis in testicular germ cell tumor. Cancer Sci. 2017;108(1):32–41. doi: 10.1111/cas.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gu S, et al. Molecular mechanisms of regulation and action of microRNA-199a in testicular germ cell tumor and glioblastomas. PLoS One. 2013;8(12):e83980. doi: 10.1371/journal.pone.0083980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu X, et al. microRNA-199a-3p functions as tumor suppressor by regulating glucose metabolism in testicular germ cell tumors. Mol Med Rep. 2016;14(3):2311–2320. doi: 10.3892/mmr.2016.5472. [DOI] [PubMed] [Google Scholar]
- 6.Fankhauser CD, et al. Frequent PD-L1 expression in testicular germ cell tumors. Br J Cancer. 2015;113(3):411–413. doi: 10.1038/bjc.2015.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vogt AP, Chen Z, Osunkoya AO. Rete testis invasion by malignant germ cell tumor and/or intratubular germ cell neoplasia: what is the significance of this finding? Hum Pathol. 2010;41(9):1339–1344. doi: 10.1016/j.humpath.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Pinto F, et al. Brachyury oncogene is a prognostic factor in high-risk testicular germ cell tumors. Andrology. 2018;6(4):597–604. doi: 10.1111/andr.12495. [DOI] [PubMed] [Google Scholar]
- 9.Martinelli C, et al. MGMT and CALCA promoter methylation are associated with poor prognosis in testicular germ cell tumor patients. Oncotarget. 2017;8(31):50608–50617. doi: 10.18632/oncotarget.11167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu Y, et al. The polymorphic hMSH5 C85T allele augments radiotherapy-induced spermatogenic impairment. Andrology. 2016;4(5):873–879. doi: 10.1111/andr.12203. [DOI] [PubMed] [Google Scholar]
- 11.Yamada Y, et al. Prognostic value of CD66b positive tumor-infiltrating neutrophils in testicular germ cell tumor. BMC Cancer. 2016;16(1):898. doi: 10.1186/s12885-016-2926-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkin NB, Baker MC. Specific chromosome change, i(12p), in testicular tumours? Lancet. 1982;2(8311):1349. doi: 10.1016/S0140-6736(82)91557-4. [DOI] [PubMed] [Google Scholar]
- 13.Stock C, et al. Isochromosome 12p and maternal loss of 1p36 in a pediatric testicular germ cell tumor. Cancer Genet Cytogenet. 1996;91(2):95–100. doi: 10.1016/0165-4608(95)00190-5. [DOI] [PubMed] [Google Scholar]
- 14.Juric D, et al. Gene expression profiling differentiates germ cell tumors from other cancers and defines subtype-specific signatures. Proc Natl Acad Sci USA. 2005;102(49):17763–17768. doi: 10.1073/pnas.0509082102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez S, et al. Expression profile of genes from 12p in testicular germ cell tumors of adolescents and adults associated with i(12p) and amplification at 12p11.2-p12.1. Oncogene. 2003;22(12):1880–1891. doi: 10.1038/sj.onc.1206302. [DOI] [PubMed] [Google Scholar]
- 16.Ezeh UI, et al. Human embryonic stem cell genes OCT4, NANOG, STELLAR, and GDF3 are expressed in both seminoma and breast carcinoma. Cancer. 2005;104(10):2255–2265. doi: 10.1002/cncr.21432. [DOI] [PubMed] [Google Scholar]
- 17.Korkola JE, et al. Down-regulation of stem cell genes, including those in a 200-kb gene cluster at 12p13.31, is associated with in vivo differentiation of human male germ cell tumors. Cancer Res. 2006;66(2):820–827. doi: 10.1158/0008-5472.CAN-05-2445. [DOI] [PubMed] [Google Scholar]
- 18.Albers P, et al. Guidelines on testicular cancer: 2015 update. Eur Urol. 2015;68(6):1054–1068. doi: 10.1016/j.eururo.2015.07.044. [DOI] [PubMed] [Google Scholar]
- 19.Albers P, et al. EAU guidelines on testicular cancer: 2011 update. Eur Urol. 2011;60(2):304–319. doi: 10.1016/j.eururo.2011.05.038. [DOI] [PubMed] [Google Scholar]
- 20.Tarrant WP, Czerniak BA, Guo CC. Relationship between primary and metastatic testicular germ cell tumors: a clinicopathologic analysis of 100 cases. Hum Pathol. 2013;44(10):2220–2226. doi: 10.1016/j.humpath.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Iida K, et al. Metastasectomy as optimal treatment for late relapsing solitary brain metastasis from testicular germ cell tumor: a case report. BMC Res Notes. 2014;7:865. doi: 10.1186/1756-0500-7-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ushida H, et al. Recurrent rhabdomyosarcoma after adjuvant chemotherapy for stage I non-seminomatous germ cell tumor with malignant transformation. Int J Urol. 2013;20(5):544–546. doi: 10.1111/j.1442-2042.2012.03197.x. [DOI] [PubMed] [Google Scholar]
- 23.Gavriel H, Kleid S. Benign neck metastasis of a testicular germ cell tumor. Int Surg. 2015;100(1):164–168. doi: 10.9738/INTSURG-D-13-00157.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Connor A, Dias A, Timon C. Role of neck dissection for metastatic nonseminomatous testicular carcinoma: case report and literature review. J Laryngol Otol. 2013;127(10):1038–1039. doi: 10.1017/S0022215113002090. [DOI] [PubMed] [Google Scholar]
- 25.Rascol O, et al. A proof-of-concept, randomized, placebo-controlled, multiple cross-overs (n-of-1) study of naftazone in Parkinson’s disease. Fundam Clin Pharmacol. 2012;26(4):557–564. doi: 10.1111/j.1472-8206.2011.00951.x. [DOI] [PubMed] [Google Scholar]
- 26.Talwar V, et al. Intracardiac metastases from a testicular germ cell tumor. J Assoc Physicians India. 2002;50:855. [PubMed] [Google Scholar]
- 27.do Nascimento FB, et al. Right cardiac chambers involvement by a malignant testicular germ cell tumor: an imaging-pathologic correlation. Urology. 2016;93:e9–e11. doi: 10.1016/j.urology.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 28.Hakiman H, et al. Rapid progression of a germ cell tumor encasing the inferior vena cava and aorta following a radical orchiectomy. Rare Tumors. 2013;5(2):79–82. doi: 10.4081/rt.2013.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delahunt B, et al. Testicular germ cell tumor with pineal metastases. Neurosurgery. 1990;26(4):688–691. doi: 10.1227/00006123-199004000-00023. [DOI] [PubMed] [Google Scholar]
- 30.Oing C, et al. Nodal, pulmonary and pleural gliomatosis in a 42-year-old-male with non-seminomatous testicular germ cell cancer. Histopathology. 2014;65(1):142–143. doi: 10.1111/his.12374. [DOI] [PubMed] [Google Scholar]
- 31.Aydiner A, et al. Testicular germ cell tumor with gastric metastasis. Acta Oncol. 1993;32(4):459–460. doi: 10.3109/02841869309093625. [DOI] [PubMed] [Google Scholar]
- 32.Lauro S, et al. Gastric metastases from testicular cancer: case report and review of literature. J Gastrointest Cancer. 2014;45(Suppl 1):22–24. doi: 10.1007/s12029-013-9524-4. [DOI] [PubMed] [Google Scholar]
- 33.Assimakopoulos SF, et al. A case of chondrosarcoma developing in a recurrent retroperitoneal mass after chemotherapy for testicular germ cell tumor. Urol Int. 2006;77(1):86–88. doi: 10.1159/000092942. [DOI] [PubMed] [Google Scholar]
- 34.Kvammen O, et al. Long-term relative survival after diagnosis of testicular germ cell tumor. Cancer Epidemiol Biomark Prev. 2016;25(5):773–779. doi: 10.1158/1055-9965.EPI-15-1153. [DOI] [PubMed] [Google Scholar]
- 35.Cost NG, et al. Effect of testicular germ cell tumor therapy on renal function. Urology. 2012;80(3):641–648. doi: 10.1016/j.urology.2012.04.064. [DOI] [PubMed] [Google Scholar]
- 36.Weijl NI, et al. Thromboembolic events during chemotherapy for germ cell cancer: a cohort study and review of the literature. J Clin Oncol. 2000;18(10):2169–2178. doi: 10.1200/JCO.2000.18.10.2169. [DOI] [PubMed] [Google Scholar]
- 37.Lange J, et al. Cisplatin-related cerebral infarction in testicular germ cell cancer: short report of three Cases and pathomechanism. Clin Neurol Neurosurg. 2017;152:76–77. doi: 10.1016/j.clineuro.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 38.Azak A, et al. Cerebrovascular accident during cisplatin-based combination chemotherapy of testicular germ cell tumor: an unusual case report. Anticancer Drugs. 2008;19(1):97–98. doi: 10.1097/CAD.0b013e3282f0777e. [DOI] [PubMed] [Google Scholar]
- 39.Meattini I, et al. Ischemic stroke during cisplatin-based chemotherapy for testicular germ cell tumor: case report and review of the literature. J Chemother. 2010;22(2):134–136. doi: 10.1179/joc.2010.22.2.134. [DOI] [PubMed] [Google Scholar]
- 40.Nonomura N, et al. Secondary acute monocytic leukemia occurring during the treatment of a testicular germ cell tumor. A case report and review of the literature. Urol Int. 1997;58(4):239–242. doi: 10.1159/000282992. [DOI] [PubMed] [Google Scholar]
- 41.Matsumoto S, et al. Secondary leukemia following ultra high-dose chemotherapy with peripheral blood stem cell autotransplantation for refractory testicular cancer. Nihon Hinyokika Gakkai Zasshi. 2000;91(10–11):687–691. doi: 10.5980/jpnjurol1989.91.68. [DOI] [PubMed] [Google Scholar]
- 42.Cerrud-Rodriguez RC, Quinteros MG, Azam M. Internal carotid artery occlusion and stroke as a complication of cisplatin-based chemotherapy for metastatic testicular germ cell tumour. BMJ Case Rep. 2017 doi: 10.1136/bcr-2017-220084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Furuhashi K, et al. Onco-testicular sperm extraction: testicular sperm extraction in azoospermic and very severely oligozoospermic cancer patients. Andrologia. 2013;45(2):107–110. doi: 10.1111/j.1439-0272.2012.01319.x. [DOI] [PubMed] [Google Scholar]
- 44.Roque M, et al. Onco-testicular sperm extraction: birth of a healthy baby after fertility preservation in synchronous bilateral testicular cancer and azoospermia. Andrologia. 2015;47(4):482–485. doi: 10.1111/and.12292. [DOI] [PubMed] [Google Scholar]
- 45.Kirkali Z, et al. Testis sparing surgery for the treatment of a sequential bilateral testicular germ cell tumor. Int J Urol. 2001;8(12):710–712. doi: 10.1046/j.1442-2042.2001.00395.x. [DOI] [PubMed] [Google Scholar]
- 46.Demir A, et al. Testis-sparing surgery in an adult with bilateral synchronous seminomatous tumor. Int J Urol. 2004;11(12):1142–1144. doi: 10.1111/j.1442-2042.2004.00946.x. [DOI] [PubMed] [Google Scholar]
- 47.Peltzer K, Pengpid S. Knowledge, attitudes and practice of testicular self-examination among male university students from bangladesh, madagascar, singapore, south africa and turkey. Asian Pac J Cancer Prev. 2015;16(11):4741–4743. doi: 10.7314/APJCP.2015.16.11.4741. [DOI] [PubMed] [Google Scholar]
- 48.Chen SR, Liu YX. Regulation of spermatogonial stem cell self-renewal and spermatocyte meiosis by Sertoli cell signaling. Reproduction. 2015;149(4):R159–R167. doi: 10.1530/REP-14-0481. [DOI] [PubMed] [Google Scholar]
- 49.Chen SR, et al. Disruption of genital ridge development causes aberrant primordial germ cell proliferation but does not affect their directional migration. BMC Biol. 2013;11:22. doi: 10.1186/1741-7007-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen SR, et al. Loss of Gata4 in Sertoli cells impairs the spermatogonial stem cell niche and causes germ cell exhaustion by attenuating chemokine signaling. Oncotarget. 2015;6(35):37012–37027. doi: 10.18632/oncotarget.6115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rebourcet D, et al. Sertoli cells control peritubular myoid cell fate and support adult Leydig cell development in the prepubertal testis. Development. 2014;141(10):2139–2149. doi: 10.1242/dev.107029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeFalco T, et al. Macrophages contribute to the spermatogonial niche in the adult testis. Cell Rep. 2015;12(7):1107–1119. doi: 10.1016/j.celrep.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen SR, Liu YX. Myh11-Cre is not limited to peritubular myoid cells and interaction between Sertoli and peritubular myoid cells needs investigation. Proc Natl Acad Sci USA. 2016;113(17):E2352. doi: 10.1073/pnas.1602873113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang YQ, et al. GATA4 is a negative regulator of contractility in testicular peritubular myoid cells. Reproduction. 2018 doi: 10.1530/rep-18-0148. [DOI] [PubMed] [Google Scholar]
- 55.Green CD, et al. A comprehensive roadmap of murine spermatogenesis defined by single-cell RNA-Seq. Dev Cell. 2018;46(5):651–667e610. doi: 10.1016/j.devcel.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang M, et al. Single-cell RNA sequencing analysis reveals sequential cell fate transition during human spermatogenesis. Cell Stem Cell. 2018;23(4):599–614e594. doi: 10.1016/j.stem.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 57.Skakkebaek NE. Possible carcinoma-in situ of the testis. Lancet. 1972;2(7776):516–517. doi: 10.1016/S0140-6736(72)91909-5. [DOI] [PubMed] [Google Scholar]
- 58.Kristensen DG, et al. Evidence that active demethylation mechanisms maintain the genome of carcinoma in situ cells hypomethylated in the adult testis. Br J Cancer. 2014;110(3):668–678. doi: 10.1038/bjc.2013.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mitchell RT, et al. Intratubular germ cell neoplasia of the human testis: heterogeneous protein expression and relation to invasive potential. Mod Pathol. 2014;27(9):1255–1266. doi: 10.1038/modpathol.2013.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vasdev N, Moon A, Thorpe AC. Classification, epidemiology and therapies for testicular germ cell tumours. Int J Dev Biol. 2013;57(2–4):133–139. doi: 10.1387/ijdb.130031nv. [DOI] [PubMed] [Google Scholar]
- 61.Ottesen AM, et al. High-resolution comparative genomic hybridization detects extra chromosome arm 12p material in most cases of carcinoma in situ adjacent to overt germ cell tumors, but not before the invasive tumor development. Genes Chromosomes Cancer. 2003;38(2):117–125. doi: 10.1002/gcc.10244. [DOI] [PubMed] [Google Scholar]
- 62.Summersgill B, et al. Chromosomal imbalances associated with carcinoma in situ and associated testicular germ cell tumours of adolescents and adults. Br J Cancer. 2001;85(2):213–220. doi: 10.1054/bjoc.2001.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Di Vizio D, et al. Loss of the tumor suppressor gene PTEN marks the transition from intratubular germ cell neoplasias (ITGCN) to invasive germ cell tumors. Oncogene. 2005;24(11):1882–1894. doi: 10.1038/sj.onc.1208368. [DOI] [PubMed] [Google Scholar]
- 64.Datta MW, et al. Transition from in situ to invasive testicular germ cell neoplasia is associated with the loss of p21 and gain of mdm-2 expression. Mod Pathol. 2001;14(5):437–442. doi: 10.1038/modpathol.3880331. [DOI] [PubMed] [Google Scholar]
- 65.Taylor-Weiner A, et al. Genomic evolution and chemoresistance in germ-cell tumours. Nature. 2016;540(7631):114–118. doi: 10.1038/nature20596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sperger JM, et al. Gene expression patterns in human embryonic stem cells and human pluripotent germ cell tumors. Proc Natl Acad Sci USA. 2003;100(23):13350–13355. doi: 10.1073/pnas.2235735100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.de Jong J, et al. Diagnostic value of OCT3/4 for pre-invasive and invasive testicular germ cell tumours. J Pathol. 2005;206(2):242–249. doi: 10.1002/path.1766. [DOI] [PubMed] [Google Scholar]
- 68.Rajpert-De Meyts E, Skakkebaek NE. Expression of the c-kit protein product in carcinoma-in situ and invasive testicular germ cell tumours. Int J Androl. 1994;17(2):85–92. doi: 10.1111/j.1365-2605.1994.tb01225.x. [DOI] [PubMed] [Google Scholar]
- 69.Emerson RE, Ulbright TM. Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers. Pathology. 2010;42(4):344–355. doi: 10.3109/00313021003767355. [DOI] [PubMed] [Google Scholar]
- 70.Ota S, et al. Oncofetal protein glypican-3 in testicular germ-cell tumor. Virchows Arch. 2006;449(3):308–314. doi: 10.1007/s00428-006-0238-x. [DOI] [PubMed] [Google Scholar]
- 71.Zynger DL, et al. Glypican 3 has a higher sensitivity than alpha-fetoprotein for testicular and ovarian yolk sac tumour: immunohistochemical investigation with analysis of histological growth patterns. Histopathology. 2010;56(6):750–757. doi: 10.1111/j.1365-2559.2010.03553.x. [DOI] [PubMed] [Google Scholar]
- 72.Cao D, et al. SALL4 is a novel diagnostic marker for testicular germ cell tumors. Am J Surg Pathol. 2009;33(7):1065–1077. doi: 10.1097/PAS.0b013e3181a13eef. [DOI] [PubMed] [Google Scholar]
- 73.Shen H, et al. Integrated molecular characterization of testicular germ cell tumors. Cell Rep. 2018;23(11):3392–3406. doi: 10.1016/j.celrep.2018.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Skakkebaek NE, Berthelsen JG. Carcinoma-in situ of the testis and invasive growth of different types of germ cell tumours. A revised germ cell theory. Int J Androl. 1981;4(Suppl s4):26–33. doi: 10.1111/j.1365-2605.1981.tb00647.x. [DOI] [PubMed] [Google Scholar]
- 75.Rajpert-De Meyts E, Kvist M, Skakkebaek NE. Heterogeneity of expression of immunohistochemical tumour markers in testicular carcinoma in situ: pathogenetic relevance. Virchows Arch. 1996;428(3):133–139. doi: 10.1007/BF00200655. [DOI] [PubMed] [Google Scholar]
- 76.de Graaff WE, et al. Ploidy of testicular carcinoma in situ. Lab Investig. 1992;66(2):166–168. doi: 10.1007/s00761-005-0952-z. [DOI] [PubMed] [Google Scholar]
- 77.de Jong B, et al. Pathogenesis of adult testicular germ cell tumors. A cytogenetic model. Cancer Genet Cytogenet. 1990;48(2):143–167. doi: 10.1016/0165-4608(90)90115-Q. [DOI] [PubMed] [Google Scholar]
- 78.Srigley JR, et al. The ultrastructure and histogenesis of male germ neoplasia with emphasis on seminoma with early carcinomatous features. Ultrastruct Pathol. 1988;12(1):67–86. doi: 10.3109/01913128809048477. [DOI] [PubMed] [Google Scholar]
- 79.Kernek KM, et al. Identical allelic losses in mature teratoma and other histologic components of malignant mixed germ cell tumors of the testis. Am J Pathol. 2003;163(6):2477–2484. doi: 10.1016/S0002-9440(10)63602-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jones TD, et al. Clonal origin of metastatic testicular teratomas. Clin Cancer Res. 2006;12(18):5377–5383. doi: 10.1158/1078-0432.CCR-06-0444. [DOI] [PubMed] [Google Scholar]
- 81.Nettersheim D, et al. Establishment of a versatile seminoma model indicates cellular plasticity of germ cell tumor cells. Genes Chromosomes Cancer. 2012;51(7):717–726. doi: 10.1002/gcc.21958. [DOI] [PubMed] [Google Scholar]
- 82.Nettersheim D, et al. BMP inhibition in seminomas initiates acquisition of pluripotency via NODAL signaling resulting in reprogramming to an embryonal carcinoma. PLoS Genet. 2015;11(7):e1005415. doi: 10.1371/journal.pgen.1005415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nettersheim D, et al. SOX2 is essential for in vivo reprogramming of seminoma-like TCam-2 cells to an embryonal carcinoma-like fate. Oncotarget. 2016;7(30):47095–47110. doi: 10.18632/oncotarget.9903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hemminki K, Li X. Familial risk in testicular cancer as a clue to a heritable and environmental aetiology. Br J Cancer. 2004;90(9):1765–1770. doi: 10.1038/sj.bjc.6601714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chia VM, et al. Risk of cancer in first- and second-degree relatives of testicular germ cell tumor cases and controls. Int J Cancer. 2009;124(4):952–957. doi: 10.1002/ijc.23971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Neale RE, et al. Testicular cancer in twins: a meta-analysis. Br J Cancer. 2008;98(1):171–173. doi: 10.1038/sj.bjc.6604136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Swerdlow AJ, et al. Risks of breast and testicular cancers in young adult twins in England and Wales: evidence on prenatal and genetic aetiology. Lancet. 1997;350(9093):1723–1728. doi: 10.1016/S0140-6736(97)05526-8. [DOI] [PubMed] [Google Scholar]
- 88.Teh BT, et al. Familial testicular cancer: lack of evidence for trinucleotide repeat expansions and association with PKD1 in one family. J Med Genet. 1999;36(4):348–349. doi: 10.1046/j.1365-2788.1999.00200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kanetsky PA, et al. Common variation in KITLG and at 5q31.3 predisposes to testicular germ cell cancer. Nat Genet. 2009;41(7):811–815. doi: 10.1038/ng.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rapley EA, et al. A genome-wide association study of testicular germ cell tumor. Nat Genet. 2009;41(7):807–810. doi: 10.1038/ng.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Turnbull C, et al. Variants near DMRT1, TERT and ATF7IP are associated with testicular germ cell cancer. Nat Genet. 2010;42(7):604–607. doi: 10.1038/ng.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kanetsky PA, et al. A second independent locus within DMRT1 is associated with testicular germ cell tumor susceptibility. Hum Mol Genet. 2011;20(15):3109–3117. doi: 10.1093/hmg/ddr207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dalgaard MD, et al. A genome-wide association study of men with symptoms of testicular dysgenesis syndrome and its network biology interpretation. J Med Genet. 2012;49(1):58–65. doi: 10.1136/jmedgenet-2011-100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chung CC, et al. Meta-analysis identifies four new loci associated with testicular germ cell tumor. Nat Genet. 2013;45(6):680–685. doi: 10.1038/ng.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ruark E, et al. Identification of nine new susceptibility loci for testicular cancer, including variants near DAZL and PRDM14. Nat Genet. 2013;45(6):686–689. doi: 10.1038/ng.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schumacher FR, et al. Testicular germ cell tumor susceptibility associated with the UCK2 locus on chromosome 1q23. Hum Mol Genet. 2013;22(13):2748–2753. doi: 10.1093/hmg/ddt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Litchfield K, et al. Multi-stage genome-wide association study identifies new susceptibility locus for testicular germ cell tumour on chromosome 3q25. Hum Mol Genet. 2015;24(4):1169–1176. doi: 10.1093/hmg/ddu511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kristiansen W, et al. Two new loci and gene sets related to sex determination and cancer progression are associated with susceptibility to testicular germ cell tumor. Hum Mol Genet. 2015;24(14):4138–4146. doi: 10.1093/hmg/ddv129. [DOI] [PubMed] [Google Scholar]
- 99.Litchfield K, et al. Identification of 19 new risk loci and potential regulatory mechanisms influencing susceptibility to testicular germ cell tumor. Nat Genet. 2017;49(7):1133–1140. doi: 10.1038/ng.3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang Z, et al. Meta-analysis of five genome-wide association studies identifies multiple new loci associated with testicular germ cell tumor. Nat Genet. 2017;49(7):1141–1147. doi: 10.1038/ng.3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Paumard-Hernandez B, et al. Whole exome sequencing identifies PLEC, EXO5 and DNAH7 as novel susceptibility genes in testicular cancer. Int J Cancer. 2018;143(8):1954–1962. doi: 10.1002/ijc.31604. [DOI] [PubMed] [Google Scholar]
- 102.Runyan C, et al. Steel factor controls midline cell death of primordial germ cells and is essential for their normal proliferation and migration. Development. 2006;133(24):4861–4869. doi: 10.1242/dev.02688. [DOI] [PubMed] [Google Scholar]
- 103.Yamaji M, et al. Critical function of Prdm14 for the establishment of the germ cell lineage in mice. Nat Genet. 2008;40(8):1016–1022. doi: 10.1038/ng.186. [DOI] [PubMed] [Google Scholar]
- 104.Matson CK, et al. The mammalian doublesex homolog DMRT1 is a transcriptional gatekeeper that controls the mitosis versus meiosis decision in male germ cells. Dev Cell. 2010;19(4):612–624. doi: 10.1016/j.devcel.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gill ME, et al. Licensing of gametogenesis, dependent on RNA binding protein DAZL, as a gateway to sexual differentiation of fetal germ cells. Proc Natl Acad Sci USA. 2011;108(18):7443–7448. doi: 10.1073/pnas.1104501108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Seetharam V, et al. Bilateral cryptorchidism with bilateral synchronous abdominal testicular germ cell tumour. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-203085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chemes HE, et al. Is a CIS phenotype apparent in children with disorders of sex development? Milder testicular dysgenesis is associated with a higher risk of malignancy. Andrology. 2015;3(1):59–69. doi: 10.1111/andr.301. [DOI] [PubMed] [Google Scholar]
- 108.Machiela MJ, et al. Mosaic chromosome Y loss and testicular germ cell tumor risk. J Hum Genet. 2017;62(6):637–640. doi: 10.1038/jhg.2017.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dieckmann KP, et al. Contralateral testicular biopsy in patients with germ cell tumors: practice patterns in Germany 2014. Urologe A. 2014;53(11):1651–1655. doi: 10.1007/s00120-014-3657-3. [DOI] [PubMed] [Google Scholar]
- 110.Morimoto LM, et al. Neonatal hormone concentrations and risk of testicular germ cell tumors (TGCT) Cancer Epidemiol Biomark Prev. 2018;27(4):488–495. doi: 10.1158/1055-9965.EPI-17-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Matin A, et al. Susceptibility to testicular germ-cell tumours in a 129.MOLF-Chr 19 chromosome substitution strain. Nat Genet. 1999;23(2):237–240. doi: 10.1038/13874. [DOI] [PubMed] [Google Scholar]
- 112.Zhu R, Matin A. Tumor loci and their interactions on mouse chromosome 19 that contribute to testicular germ cell tumors. BMC Genet. 2014;15:65. doi: 10.1186/1471-2156-15-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Heaney JD, et al. Germ cell pluripotency, premature differentiation and susceptibility to testicular teratomas in mice. Development. 2012;139(9):1577–1586. doi: 10.1242/dev.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Spiller CM, et al. Endogenous Nodal signaling regulates germ cell potency during mammalian testis development. Development. 2012;139(22):4123–4132. doi: 10.1242/dev.083006. [DOI] [PubMed] [Google Scholar]
- 115.Dawson EP, et al. Delayed male germ cell sex-specification permits transition into embryonal carcinoma cells with features of primed pluripotency. Development. 2018 doi: 10.1242/dev.156612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Krentz AD, et al. The DM domain protein DMRT1 is a dose-sensitive regulator of fetal germ cell proliferation and pluripotency. Proc Natl Acad Sci USA. 2009;106(52):22323–22328. doi: 10.1073/pnas.0905431106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Heaney JD, et al. Loss of the transmembrane but not the soluble kit ligand isoform increases testicular germ cell tumor susceptibility in mice. Cancer Res. 2008;68(13):5193–5197. doi: 10.1158/0008-5472.CAN-08-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Youngren KK, et al. The Ter mutation in the dead end gene causes germ cell loss and testicular germ cell tumours. Nature. 2005;435(7040):360–364. doi: 10.1038/nature03595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kimura T, et al. Conditional loss of PTEN leads to testicular teratoma and enhances embryonic germ cell production. Development. 2003;130(8):1691–1700. doi: 10.1242/dev.00392. [DOI] [PubMed] [Google Scholar]
- 120.Carouge D, et al. Parent-of-origin effects of A1CF and AGO2 on testicular germ-cell tumors, testicular abnormalities, and fertilization bias. Proc Natl Acad Sci USA. 2016;113(37):E5425–E5433. doi: 10.1073/pnas.1604773113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Li H, et al. Impaired planar germ cell division in the testis, caused by dissociation of RHAMM from the spindle, results in hypofertility and seminoma. Cancer Res. 2016;76(21):6382–6395. doi: 10.1158/0008-5472.CAN-16-0179. [DOI] [PubMed] [Google Scholar]
- 122.Pierpont TM, et al. Chemotherapy-induced depletion of OCT4-positive cancer stem cells in a mouse model of malignant testicular cancer. Cell Rep. 2017;21(7):1896–1909. doi: 10.1016/j.celrep.2017.10.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Barlow LJ, Badalato GM, McKiernan JM. Serum tumor markers in the evaluation of male germ cell tumors. Nat Rev Urol. 2010;7(11):610–617. doi: 10.1038/nrurol.2010.166. [DOI] [PubMed] [Google Scholar]
- 124.Murray MJ, Huddart RA, Coleman N. The present and future of serum diagnostic tests for testicular germ cell tumours. Nat Rev Urol. 2016;13(12):715–725. doi: 10.1038/nrurol.2016.170. [DOI] [PubMed] [Google Scholar]
- 125.Spiekermann M, et al. MicroRNA miR-371a-3p in serum of patients with germ cell tumours: evaluations for establishing a serum biomarker. Andrology. 2015;3(1):78–84. doi: 10.1111/j.2047-2927.2014.00269.x. [DOI] [PubMed] [Google Scholar]
- 126.Syring I, et al. Circulating serum miRNA (miR-367-3p, miR-371a-3p, miR-372-3p and miR-373-3p) as biomarkers in patients with testicular germ cell cancer. J Urol. 2015;193(1):331–337. doi: 10.1016/j.juro.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 127.Murray MJ, et al. A pipeline to quantify serum and cerebrospinal fluid microRNAs for diagnosis and detection of relapse in paediatric malignant germ-cell tumours. Br J Cancer. 2016;114(2):151–162. doi: 10.1038/bjc.2015.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gillis AJ, et al. Targeted serum miRNA (TSmiR) test for diagnosis and follow-up of (testicular) germ cell cancer patients: a proof of principle. Mol Oncol. 2013;7(6):1083–1092. doi: 10.1016/j.molonc.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Terbuch A, et al. MiR-371a-3p serum levels are increased in recurrence of testicular germ cell tumor patients. Int J Mol Sci. 2018 doi: 10.3390/ijms19103130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tu SM, et al. Intratumoral heterogeneity: role of differentiation in a potentially lethal phenotype of testicular cancer. Cancer. 2016;122(12):1836–1843. doi: 10.1002/cncr.29996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Comiter CV, et al. Prognostic features of teratomas with malignant transformation: a clinicopathological study of 21 cases. J Urol. 1998;159(3):859–863. doi: 10.1016/S0022-5347(01)63754-6. [DOI] [PubMed] [Google Scholar]
- 132.Bartkova J, et al. DNA damage response in human testes and testicular germ cell tumours: biology and implications for therapy. Int J Androl. 2007;30(4):282–291. doi: 10.1111/j.1365-2605.2007.00772.x. [DOI] [PubMed] [Google Scholar]
- 133.Cavallo F, Feldman DR, Barchi M. Revisiting DNA damage repair, p53-mediated apoptosis and cisplatin sensitivity in germ cell tumors. Int J Dev Biol. 2013;57(2–4):273–280. doi: 10.1387/ijdb.130135mb. [DOI] [PubMed] [Google Scholar]
- 134.Peng HQ, et al. Mutations of the p53 gene do not occur in testis cancer. Cancer Res. 1993;53(15):3574–3578. doi: 10.1007/BF01525437. [DOI] [PubMed] [Google Scholar]
- 135.Gutekunst M, et al. p53 hypersensitivity is the predominant mechanism of the unique responsiveness of testicular germ cell tumor (TGCT) cells to cisplatin. PLoS One. 2011;6(4):e19198. doi: 10.1371/journal.pone.0019198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Awuah SG, Riddell IA, Lippard SJ. Repair shielding of platinum-DNA lesions in testicular germ cell tumors by high-mobility group box protein 4 imparts cisplatin hypersensitivity. Proc Natl Acad Sci USA. 2017;114(5):950–955. doi: 10.1073/pnas.1615327114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Oechsle K, et al. Long-term survival after treatment with gemcitabine and oxaliplatin with and without paclitaxel plus secondary surgery in patients with cisplatin-refractory and/or multiply relapsed germ cell tumors. Eur Urol. 2011;60(4):850–855. doi: 10.1016/j.eururo.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 138.Juliachs M, et al. The PDGFRbeta-AKT pathway contributes to CDDP-acquired resistance in testicular germ cell tumors. Clin Cancer Res. 2014;20(3):658–667. doi: 10.1158/1078-0432.CCR-13-1131. [DOI] [PubMed] [Google Scholar]
- 139.Lopez-Saavedra A, et al. MAD2gamma, a novel MAD2 isoform, reduces mitotic arrest and is associated with resistance in testicular germ cell tumors. Cell Cycle. 2016;15(15):2066–2076. doi: 10.1080/15384101.2016.1198863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Koster R, et al. Cytoplasmic p21 expression levels determine cisplatin resistance in human testicular cancer. J Clin Invest. 2010;120(10):3594–3605. doi: 10.1172/JCI41939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Koster R, et al. Disruption of the MDM2-p53 interaction strongly potentiates p53-dependent apoptosis in cisplatin-resistant human testicular carcinoma cells via the Fas/FasL pathway. Cell Death Dis. 2011;2:e148. doi: 10.1038/cddis.2011.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Liu L, et al. MicroRNA-302a sensitizes testicular embryonal carcinoma cells to cisplatin-induced cell death. J Cell Physiol. 2013;228(12):2294–2304. doi: 10.1002/jcp.24394. [DOI] [PubMed] [Google Scholar]
- 143.Huang H, et al. microRNA-383 impairs phosphorylation of H2AX by targeting PNUTS and inducing cell cycle arrest in testicular embryonal carcinoma cells. Cell Signal. 2014;26(5):903–911. doi: 10.1016/j.cellsig.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 144.Nitzsche B, et al. Anti-tumour activity of two novel compounds in cisplatin-resistant testicular germ cell cancer. Br J Cancer. 2012;107(11):1853–1863. doi: 10.1038/bjc.2012.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cavallo F, et al. Reduced proficiency in homologous recombination underlies the high sensitivity of embryonal carcinoma testicular germ cell tumors to cisplatin and poly (adp-ribose) polymerase inhibition. PLoS One. 2012;7(12):e51563. doi: 10.1371/journal.pone.0051563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Litchfield K, et al. Whole-exome sequencing reveals the mutational spectrum of testicular germ cell tumours. Nat Commun. 2015;6:5973. doi: 10.1038/ncomms6973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Honecker F, et al. Microsatellite instability, mismatch repair deficiency, and BRAF mutation in treatment-resistant germ cell tumors. J Clin Oncol. 2009;27(13):2129–2136. doi: 10.1200/JCO.2008.18.8623. [DOI] [PubMed] [Google Scholar]
- 148.Feldman DR, et al. Presence of somatic mutations within PIK3CA, AKT, RAS, and FGFR3 but not BRAF in cisplatin-resistant germ cell tumors. Clin Cancer Res. 2014;20(14):3712–3720. doi: 10.1158/1078-0432.CCR-13-2868. [DOI] [PubMed] [Google Scholar]
- 149.de Haas EC, et al. Variation in bleomycin hydrolase gene is associated with reduced survival after chemotherapy for testicular germ cell cancer. J Clin Oncol. 2008;26(11):1817–1823. doi: 10.1200/JCO.2007.14.1606. [DOI] [PubMed] [Google Scholar]
- 150.de Haas EC, et al. Association of PAI-1 gene polymorphism with survival and chemotherapy-related vascular toxicity in testicular cancer. Cancer. 2010;116(24):5628–5636. doi: 10.1002/cncr.25300. [DOI] [PubMed] [Google Scholar]
- 151.Oldenburg J, et al. Cisplatin-induced long-term hearing impairment is associated with specific glutathione s-transferase genotypes in testicular cancer survivors. J Clin Oncol. 2007;25(6):708–714. doi: 10.1200/JCO.2006.08.9599. [DOI] [PubMed] [Google Scholar]
- 152.Fung C, et al. Chemotherapy refractory testicular germ cell tumor is associated with a variant in armadillo repeat gene deleted in velco-cardio-facial syndrome (ARVCF) Front Endocrinol (Lausanne) 2012;3:163. doi: 10.3389/fendo.2012.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ross CJ, et al. Genetic variants in TPMT and COMT are associated with hearing loss in children receiving cisplatin chemotherapy. Nat Genet. 2009;41(12):1345–1349. doi: 10.1038/ng.478. [DOI] [PubMed] [Google Scholar]
- 154.Bagrodia A, et al. Genetic determinants of cisplatin resistance in patients with advanced germ cell tumors. J Clin Oncol. 2016;34(33):4000–4007. doi: 10.1200/JCO.2016.68.7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Seidel C, et al. Efficacy and safety of gemcitabine, oxaliplatin, and paclitaxel in cisplatin-refractory germ cell cancer in routine care—registry data from an outcomes research project of the German Testicular Cancer Study Group. Urol Oncol. 2016;34(4):167.e21–167.e28. doi: 10.1016/j.urolonc.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 156.Oechsle K, et al. Preclinical and clinical activity of sunitinib in patients with cisplatin-refractory or multiply relapsed germ cell tumors: a Canadian Urologic Oncology Group/German Testicular Cancer Study Group cooperative study. Ann Oncol. 2011;22(12):2654–2660. doi: 10.1093/annonc/mdr026. [DOI] [PubMed] [Google Scholar]
- 157.Jain A, et al. Phase II clinical trial of oxaliplatin and bevacizumab in refractory germ cell tumors. Am J Clin Oncol. 2014;37(5):450–453. doi: 10.1097/COC.0b013e31827de90d. [DOI] [PubMed] [Google Scholar]
- 158.Mego M, et al. Phase II study of everolimus in refractory testicular germ cell tumors. Urol Oncol. 2016;34(3):122.e117–122.e122. doi: 10.1016/j.urolonc.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 159.Ozata DM, et al. Loss of miR-514a-3p regulation of PEG3 activates the NF-kappa B pathway in human testicular germ cell tumors. Cell Death Dis. 2017;8(5):e2759. doi: 10.1038/cddis.2016.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rijlaarsdam MA, et al. Identification of known and novel germ cell cancer-specific (embryonic) miRs in serum by high-throughput profiling. Andrology. 2015;3(1):85–91. doi: 10.1111/andr.298. [DOI] [PubMed] [Google Scholar]
- 161.Cheung HH, et al. Methylation of an intronic region regulates miR-199a in testicular tumor malignancy. Oncogene. 2011;30(31):3404–3415. doi: 10.1038/onc.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Chen BF, et al. A miR-199a/miR-214 self-regulatory network via PSMD10, TP53 and DNMT1 in testicular germ cell tumor. Sci Rep. 2014;4:6413. doi: 10.1038/srep06413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Liu J, et al. miR2233p regulates cell growth and apoptosis via FBXW7 suggesting an oncogenic role in human testicular germ cell tumors. Int J Oncol. 2017;50(2):356–364. doi: 10.3892/ijo.2016.3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yang NQ, et al. miRNA-1297 induces cell proliferation by targeting phosphatase and tensin homolog in testicular germ cell tumor cells. Asian Pac J Cancer Prev. 2014;15(15):6243–6246. doi: 10.7314/APJCP.2014.15.15.6243. [DOI] [PubMed] [Google Scholar]
- 165.Yang NQ, et al. Crosstalk between Meg3 and miR-1297 regulates growth of testicular germ cell tumor through PTEN/PI3K/AKT pathway. Am J Transl Res. 2016;8(2):1091–1099. [PMC free article] [PubMed] [Google Scholar]
- 166.Cerami E, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gao J, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6(269):pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cutcutache I, et al. Exome-wide sequencing shows low mutation rates and identifies novel mutated genes in seminomas. Eur Urol. 2015;68(1):77–83. doi: 10.1016/j.eururo.2014.12.040. [DOI] [PubMed] [Google Scholar]
- 169.Litchfield K, et al. Rare disruptive mutations in ciliary function genes contribute to testicular cancer susceptibility. Nat Commun. 2016;7:13840. doi: 10.1038/ncomms13840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Mikuz G, Colecchia M. Teratoma with somatic-type malignant components of the testis. A review and an update. Virchows Arch. 2012;461(1):27–32. doi: 10.1007/s00428-012-1251-x. [DOI] [PubMed] [Google Scholar]
- 171.Giannatempo P, et al. Treatment and clinical outcomes of patients with teratoma with somatic-type malignant transformation: an international collaboration. J Urol. 2016;196(1):95–100. doi: 10.1016/j.juro.2015.12.082. [DOI] [PubMed] [Google Scholar]
- 172.Bondarenko G, et al. Patient-derived tumor xenografts are susceptible to formation of human lymphocytic tumors. Neoplasia. 2015;17(9):735–741. doi: 10.1016/j.neo.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wetterauer C, et al. Early development of human lymphomas in a prostate cancer xenograft program using triple knock-out immunocompromised mice. Prostate. 2015;75(6):585–592. doi: 10.1002/pros.22939. [DOI] [PubMed] [Google Scholar]
- 174.Colombo PE, et al. Ovarian carcinoma patient derived xenografts reproduce their tumor of origin and preserve an oligoclonal structure. Oncotarget. 2015;6(29):28327–28340. doi: 10.18632/oncotarget.5069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ben-David U, et al. Patient-derived xenografts undergo mouse-specific tumor evolution. Nat Genet. 2017;49(11):1567–1575. doi: 10.1038/ng.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Mazzieri R, et al. Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell. 2011;19(4):512–526. doi: 10.1016/j.ccr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 177.Hvarness T, et al. Phenotypic characterisation of immune cell infiltrates in testicular germ cell neoplasia. J Reprod Immunol. 2013;100(2):135–145. doi: 10.1016/j.jri.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 178.Siska PJ, et al. Deep exploration of the immune infiltrate and outcome prediction in testicular cancer by quantitative multiplexed immunohistochemistry and gene expression profiling. Oncoimmunology. 2017;6(4):e1305535. doi: 10.1080/2162402X.2017.1305535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cheng L, Lyu B, Roth LM. Perspectives on testicular germ cell neoplasms. Hum Pathol. 2017;59:10–25. doi: 10.1016/j.humpath.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 180.Milia-Argeiti E, et al. EMMPRIN/CD147-encriched membrane vesicles released from malignant human testicular germ cells increase MMP production through tumor-stroma interaction. Biochim Biophys Acta. 2014;1840(8):2581–2588. doi: 10.1016/j.bbagen.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 181.Bi XC, et al. Extracellular matrix metalloproteinase inducer: a novel poor prognostic marker for human seminomas. Clin Transl Oncol. 2012;14(3):190–196. doi: 10.1007/s12094-012-0783-5. [DOI] [PubMed] [Google Scholar]
- 182.Batool A, et al. A miR-125b/CSF1-CX3CL1/tumor-associated macrophage recruitment axis controls testicular germ cell tumor growth. Cell Death Dis. 2018;9(10):962. doi: 10.1038/s41419-018-1021-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cierna Z, et al. Prognostic value of programmed-death-1 receptor (PD-1) and its ligand 1 (PD-L1) in testicular germ cell tumors. Ann Oncol. 2016;27(2):300–305. doi: 10.1093/annonc/mdv574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Shah S, et al. Clinical response of a patient to anti-PD-1 immunotherapy and the immune landscape of testicular germ cell tumors. Cancer Immunol Res. 2016;4(11):903–909. doi: 10.1158/2326-6066.CIR-16-0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Loh KP, Fung C. Novel therapies in platinum-refractory metastatic germ cell tumor: a case report with a focus on a PD-1 inhibitor. Rare Tumors. 2017;9(2):6867. doi: 10.4081/rt.2017.6867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Adra N, et al. Phase II trial of pembrolizumab in patients with platinum refractory germ-cell tumors: a hoosier cancer research network study GU14-206. Ann Oncol. 2018;29(1):209–214. doi: 10.1093/annonc/mdx680. [DOI] [PubMed] [Google Scholar]
- 187.Okeley NM, et al. Intracellular activation of SGN-35, a potent anti-CD30 antibody-drug conjugate. Clin Cancer Res. 2010;16(3):888–897. doi: 10.1158/1078-0432.CCR-09-2069. [DOI] [PubMed] [Google Scholar]
- 188.Ratta R, et al. Immunotherapy advances in uro-genital malignancies. Crit Rev Oncol Hematol. 2016;105:52–64. doi: 10.1016/j.critrevonc.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 189.Schonberger S, et al. Brentuximab vedotin exerts profound antiproliferative and pro-apoptotic efficacy in CD30-positive as well as cocultured CD30-negative germ cell tumour cell lines. J Cell Mol Med. 2018;22(1):568–575. doi: 10.1111/jcmm.13344. [DOI] [PMC free article] [PubMed] [Google Scholar]