Abstract
The field of tissue engineering (TE) experiences its most exciting time in the current decade. Recent progresses in TE have made it able to translate into clinical applications. To regenerate damaged tissues, TE uses biomaterial scaffolds to prepare a suitable backbone for tissue regeneration. It is well proven that the cell–biomaterial crosstalk impacts tremendously on cell biological activities such as differentiation, proliferation, migration, and others. Clarification of exact biological effects and mechanisms of a certain material on various cell types promises to have a profound impact on clinical applications of TE. Chitosan (CS) is one of the most commonly used biomaterials with many promising characteristics such as biocompatibility, antibacterial activity, biodegradability, and others. In this review, we discuss crosstalk between CS and various cell types to provide a roadmap for more effective applications of this polymer for future uses in tissue engineering and regenerative medicine.
Keywords: Chitosan, Cell interaction, Intracellular signaling, Molecular pathways, Regulation, Immune system, Nerve system, Cancer, Stem cell
Introduction
Tissue engineering (TE) is a broad and important area of modern medicine. Every day, researchers are exploring new ways to enhance the efficacy of disabled tissues or even full restoration of missing organs. In this direction, using various biomaterials is considered as a promising approach. Biomaterial interaction with different cells is one of the most exciting and challenging issues in this regard. Understanding how biomaterials alert the biological activities of a special cell type is a critical step to design better strategies in TE filed. To date, several natural and synthetic biomaterials have been introduced for TE applications. To design a suitable scaffold, the researchers may use more than one material for fabrication of biomaterials and scaffolds for TE.
An optimal TE scaffold should have a proper impact on cell behaviors such as cell adhesion [1], cell proliferation [2, 3], cell migration [4] and cell differentiation [5]. In addition, the antibacterial properties of the biomaterials used in TE should be considered as a critical point to avoid post-implant infections [6]. Among the biomaterials utilized in TE applications, chitosan (CS) or CS-blended scaffolds have many excellent characteristics that attract the attention of the researchers [5, 7]. CS exhibits great biocompatibility, biodegradability, antimicrobial properties and remarkable compositional properties with different materials which make it an excellent candidate in TE applications [8]. One of the major concerns of researchers in deleveraging of CS in TE is how CS changes and impacts the biological behaviors of different cell types. It is important from this perspective that this information can help researchers to design more effective strategies. In this review article, we discuss the CS crosstalk with various cell types.
Chitosan
CS is a polysaccharide polymer consisted of randomly repeated units of β-(1-4)-linked N-acetyl-d-glucosamine and d-glucosamine [9]. This polymer naturally finds in the invertebrate shelves [10]. But, at the industrial scale, CST is derived from partial deacetylation of chitin (more than 60%) [11]. Chitin is one of the most abundant natural polymers. In fact, it is the second natural polysaccharide after cellulose [12]. In spite of magnificent properties, there are some limitations regarding the use of chitin in TE. For instance, chitin is not soluble in aqueous and routine natural solvents at pH < 6 because of its high hydrophobicity, resulting from the expanded hydrogen-bounded semicrystalline structure. But, CS exhibits appropriate solubility in aqueous solutions. The deacetylation process produces free amino groups in the structure of CS that makes this polysaccharide soluble at pH < 6 [13]. In addition, free protonated amino groups on d-glucosamine units endow CS the capability of binding to a wide range of natural and syntactic materials [14]. CS is utilized in various fields such as food industry [15], water waste treatment [16], paper and automotive industries [17, 18], agriculture uses, and medical and pharmaceutical applications [19]. Moreover, CS has some remarkable characteristics such as biodegradability, non-toxicity and antibacterial properties which can be used as an appropriate candidate in TE and drug control release systems (Fig. 1) [20].
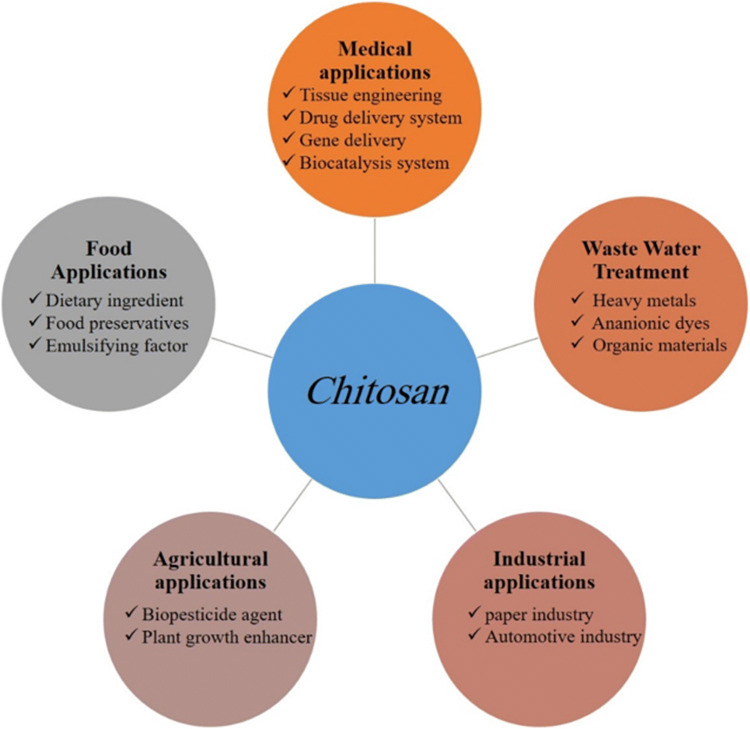
Fig. 1.
A schematic picture of the widespread applications of chitosan. This polymer is widely used in different fields such as medical and food applications, agriculture filed, wastewater treatment and even paper and automotive industries
Chitosan preparation
The first attempt to produce CS from chitin goes back to 1859 where Rouget boiled chitin in a concentrated potassium hydroxide solution [21]. But basic studies on CS production started in 1934 by Rigby [22]. Nowadays, CS is mainly produced by deacetylation of chitin using alkylation method in which sodium hydroxide and water are exploited as reagent and solvent, respectively [23]. The average molecular weight of commercially produced CS is between 3800 and 20,000 Da [24]. Generally, CS with molecular weight up to 10 kDa is known as CS oligosaccharide (COS) [25]. In this respect, various methods have been developed for the production of CS oligosaccharides. These methods are derived from two chemical and enzymatic approaches. Acidic hydrolysis, as a chemical method, is a dominant approach for COS production at the industrial scale [26].
Deacetylation degree (DD) is a critical parameter of CS which has a great effect on biological and biomechanical activities of the polysaccharide [27]. The DD represents free amino groups in the CS structure and plays an important role in its physical, chemical and mechanical properties. This parameter is determined using different methods such as IR spectrometry, UV spectrophotometry, dye absorption, 1H/13C NMR, and gas chromatography [28, 29]. Generally, depending on deacetylation degree, there are four different forms of CS. The low deacetylation degree of CS with DD between 55 and 70%, medium with DD between 70 and 85%, high with DD between 85 and 95% and ultrahigh CS with DD between 95 and 100%. In the traditional method for production CS, chitin in a strict condition process is added to the concentrated alkali at the 95 °C and stirring for 6–7 h. The DD obtained from this method is nearly 80% [26]. Production of fully deacetylation CS at the industrial scale is difficult. Therefore, various studies have been conducted to improve the traditional method and production of CS with the higher DD. Recently, Xiaofei et al. [26] developed an approach using the low concentration of alkali solution and high-pressure conditions. The results showed that ultrahigh DD value (up to 95%) is obtained when the alkali concentration varied from 5 to 15%.
Chemical parameters
Biological behaviors of a scaffold deeply depend on its mechanical and biomechanical properties such as water absorption, pore size, mechanical strength [30]. An appropriate scaffold effectively mimics the natural ECM and accelerates the regeneration process of the damaged tissue [31]. Mechanical and biological properties of chitosan-based scaffolds are affected by various chemical parameters such as DA (degree of N-acetylation), molecular weight, distribution of the acetyl groups along the chain and even preparation methods. It has been reported by many studies that the lower DA degree is associated with smaller pore size, higher cellular activities and increased water content due to enhanced hydrophilicity when compared to those with higher DA [32–36]. Moreover, DD parameter can change the cell adhesion and proliferation properties of CS scaffolds. An increase of free amino groups within the backbone of chitosan-based scaffolds remarkably promotes their adhesion capability to the mucosal surfaces with negative charges [37]. The DD also has a direct correlation with crystallinity so that CS with higher DD shows higher crystallinity. On the other hand, it has also reported that the maximum crystallinity of CS is achieved when the DD of chitosan is 0% (chitin) or 100% (fully deacetylated) [38]. Deacetylation of CS decreases its biodegradation rate. In the aqueous environment, highly deacetylated scaffolds show poor biodegradability index and are not fully degraded even after few months [39, 40]. To explain this phenomenon, two critical points should be noted. First, CS is a semi-crystalline polymer [41]. There is a relationship between the increase of crystallinity and decrease of biodegradability rate. Indeed, the maximum crystallinity is achieved when the DD of CS is 0% (chitin) or 100% (fully deacetylated). Hence, the crystallinity decreases along with the decrease of DD, resulting in an increased biodegradability rate. Second, the distribution of acetyl groups within the CS chain is another critical factor which has a great role in the biodegradability rate of scaffolds [42]. Molecular weight (MW) shows a direct effect on the CS polymer. It is obvious that the fluidity behaviors of the polymer which has an important role in the tissue interaction can be controlled by altering viscosity. In addition, MW is inversely proportional to the swelling properties of CS scaffolds so that the CS membranes with the higher MW indicate more permeability in the aqueous environments [43].
One of the other parameters that affects the chemical structure of chitosan is the pH. The pKa range for CS, which usually is from 6 to 7 (~ 6.5), depends on the various parameters such as DD, the global dissociation constant of glucosamine groups, and the cationic or anionic buffers. These factors profoundly affect the physicochemical properties of CS nanoparticles [44–46]. For example, in the acidic pH, CS nanoparticles become bigger due to intramolecular electrostatic repulsion. Given that the most CS-based complexes are made in acidic pH, there are concerns about the stability of these complexes in the physiological state. One of the most popular methods to design CS-based carriers for drug delivery is the ionically crosslinked CS/tripolyphosphate (CS/TPP). Despite the favorable results of using CS/TPP system in various studies [47–50], the stability of this complex seems to be controversial in the physiological pH. Recently, Mazancová et al. [46] evaluated the stability of the CS/TPP particles in a wide range of pH values. According to their findings, the CS/TPP complexes showed instability in the physiological pH and, in general, any pH higher than the pH in which the particles were prepared. In this circumstance, the CS/TPP complex is dissociated into the free CS and residual TPP. So, the clinical uses of the complex may face serious challenges. Moreover, the CS nanoparticles intended to aggregate in pH > 9 [44, 51]. However, further studies are needed to elucidate the exact behavior of the CS-based complexes in vivo.
Biological behaviors
Biological behaviors of TE scaffolds such as cell adhesion, proliferation, migration, cytotoxicity, stem cells differentiation, and bioactivity directly affect their healing ability. In this light, cell adhesion property is a pivotal characteristic of a scaffold. Cell adhesion is defined as the ability of a cell to attach another cell or extracellular matrix (ECM). This innate behavior of the cells plays an important role in the regulation of cell communication via stimulation of the cell signaling pathways. Thus, the effects of TE scaffolds on the cell functions deeply depend on the cell adhesion property of the scaffold’s composition [52]. The cell adhesion and mucoadhesion properties of CS and CS-based polymers have been well documented in several studies (Fig. 2) [53–56]. It has been shown that there is a direct correlation between the DD of CS and cell attachment. Cui et al. [57] demonstrated that the higher deacetylated CS exhibits better cell adhesion property.
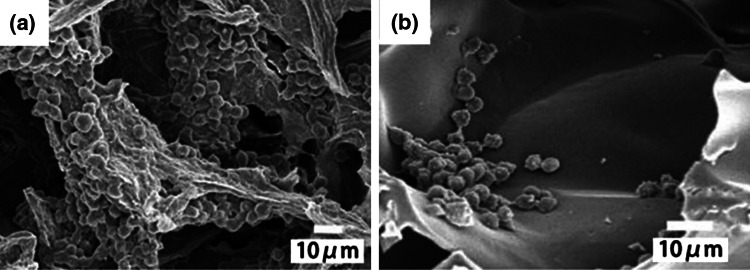
Fig. 2.
The scanning electron microscope (SEM) images show a suitable cell attachment of chondrocytes on a chitosan–alginate and b chitosan scaffolds after 14 days
(reprinted from Ref. [56] with permission from Wiley InterScience)
CS also shows a positive effect on cell proliferation and migration [58]. Cell proliferation and cell migration are two critical steps in the tissue repair process [59]. Nowadays, there is particular attention to the design of scaffolds to highly support cell proliferation and attract the cells involved in tissue repair into the damaged site. For instance, in the early phase of the wound healing process, fibroblasts move from the margins of the wound to the center area to produce new ECM [60]. CS shows the positive impact on the proliferation of fibroblasts and thereby accelerates wound healing [61, 62]. In contrast to molecular mass which exhibits no remarkable effect on proliferation rate, DD rate of CS plays a critical role in the proliferation of cells. Howling et al. [63] showed that highly deacetylated (86–89%) CS solution at a concentration range of 5–500 µg/ml stimulated the proliferation rate of human primary fibroblasts. But, the effects of CS’s DD on the proliferation of keratinocytes are controversial. So, the highly deacetylated CS has an inhibitory effect (26% at initial concentrations of 5 and 50 g/ml) on the proliferation of HaCaT and primary cultured keratinocytes, while Chatelet et al. [33] reported that CS films with lower DA increase proliferation of keratinocytes.
The effect of CS on cell migration is relatively controversial and it depends on the cell types and the used form of CS. For example, CS solution at the concentration of 0.1 and 1.0 mg/ml has been reported to reduce the migration ability of the fibroblasts (3T6) while inducing human umbilical vascular endothelial cell (HUVEC) ones at the same concentrations. In contrast to CS, the monomer and oligomer forms of CS reduced the migration of the HUVECs. Therefore, it should be noted that different forms of CS can be chosen depending on their applications [64].
CS has a broad-spectrum antimicrobial activity for bacteria, algae, yeasts, and fungi. CS is considered as both bactericidal and bacteriostatic agent; nevertheless, there is a tendency to consider CS as a bacteriostatic agent [65]. Although the exact antimicrobial mechanism of this polymer is not completely understood, several mechanisms have been suggested to describe its antimicrobial property such as attachment to the negative charges on the microbial cell surface and changing the permeability of cell wall, binding to the microbial DNA and nutrition blacking [66]. Antimicrobial property of the CS is deeply affected by DA and MW parameters in which MW has a greater role in the antimicrobial activity of CS [65]. It has been proven that the CS with lower MW better inhibits the microorganism growth and proliferation. Size and conformation are two important parameters which may explain the inhibitory effects of low molecular weight (LMW) CS on the proliferation of microorganisms. A possible description is that the LMW may facilitate the attraction and ionic interactions which eventually cause an effectively extended conformation on the cell membrane [65].
Chitosan and cell surface interaction
So far, several studies have been conducted to clarify how CS interacts with the cell surface. Most of our knowledge in this context has been obtained by studying the interactions between CS and immune cells. The role of various immune cell receptors such as Toll-like receptor (TLR-4), mannose receptor, CD14, CR3, and Dectin-1 in binding to the CS has been identified [67–69]. CS, in a phagocytosis dependent manner, activates the pyrin domain containing 3 (NLRP3) inflammasome in macrophages which has a main role in the release of IL-1β in these cells [70]. It seems that other receptors are also involved in CS–cell interaction. For example, Yuan et al. [71] reported that the presence of the megalin receptor on the renal proximal tubule cells plays a pivotal role in the receptor-mediated endocytosis of LMWC. However, the presence of a specific receptor for CS has not been identified yet and further studies are needed in this regard.
In addition to the receptor-mediated endocytosis, CS nanoparticles enter the cells through the other mechanisms such as clathrin-mediated endocytosis. The results of different studies showed that because of the positive charge of these particles in body fluids, they can change the conformation of the cell membrane and its embedded proteins, such as clathrin. Clathrin-mediated endocytosis is an energy-dependent pathway which is responsible for internalization of the most amounts of these nanoparticles [72]. Obviously, this type of internalization terminates into the lysosomal pathway which eventually causes the acidic and enzymatic degradation of CS nanoparticles [72]. Moreover, a few studies indicated that the caveolae-mediated endocytosis and macropinocytosis also are the other mechanisms involved in the cellular uptake of CS nanoparticles. In contrast to clathrin-mediated endocytosis, these internalization pathways do not end in the lysosomal destination and the cargo is transported from basolateral to apical side of cells which is called transcytosis [73].
Chitosan and cell signaling
Chitosan and immunity system
CS can regulate innate and adaptive immune responses. There are some promising reports about the ability of CS in stimulating the immune response against tumors and also using it as an adjuvant in the preparation of various vaccines [74, 75].
CS as a nanoparticle has been shown to have the contradictory effects on cytokine production. For instance, Lee et al. indicated that the diluted CS at the concentration of 0.001 and 0.005% increased the expression of IL-2 and IFN-γ in porcine spleen cells via affecting the Th1 cells. They also reported that CS had no effect on expression of Th2-related cytokines including IL-4, IL-5, IL-6, and IL-10 [76]. But, in another study, CS nanoparticles could considerably up-regulate the mRNA expression of Th1 (IL-2 and IFN-γ) and Th2 (IL-10) cytokines in the splenocytes of immunized mice [77]. In an in vivo experiment, CS-adjuvanted H. pylori vaccine increased the Th1 (IL-4) and Th2 (IL-10) cytokines levels in H. pylori-infected Balb/c model [78]. CS-based adjuvants also were reported to enhance Th1 and Th17 responses [75]. It seems that more investigations should be carried out to clarify how exactly CS affects lymphocytes.
It is reported that CS enhanced migration and activation of polymorphonuclear cells (PMN) and consequently led to some positive consequences such as wound healing (Fig. 3) [79–84]. In this regard, two possible mechanisms have been suggested: (1) inducing IL-8 secretion from neutrophils; (2) complement activation. It is found that neutrophils in the presence of CS showed an overexpressed level of IL-8. The IL-8 has known to be the main chemotactic agent for neutrophils. It is interesting that the degree of acetylation has a direct effect on IL-8 secretion from neutrophils. In this light, Park et al. [85] reported that the acetylation of CS increased the expression of IL-8 from these cells. They suggested that N-acetylation increased the CS film hydrophobicity which could prolong the physical interaction between CS and PMNs. Simard et al. [86] evaluated the chemotactic effect of two CS solutions with different DD (80% and 95%) on PMNs at the concentration range of 10–100 µg/ml. They found that only the 80% deacetylated CS successfully attracted the PMNs in a dose-dependent manner. According to their reports, neither 80% nor 95% deacetylated CS had the activator role in degranulation and superoxide production of PMNs. In another mechanism, CS indirectly causes neutrophil chemotaxis through interaction with complement proteins such as C3a and C5a in circulation [85].
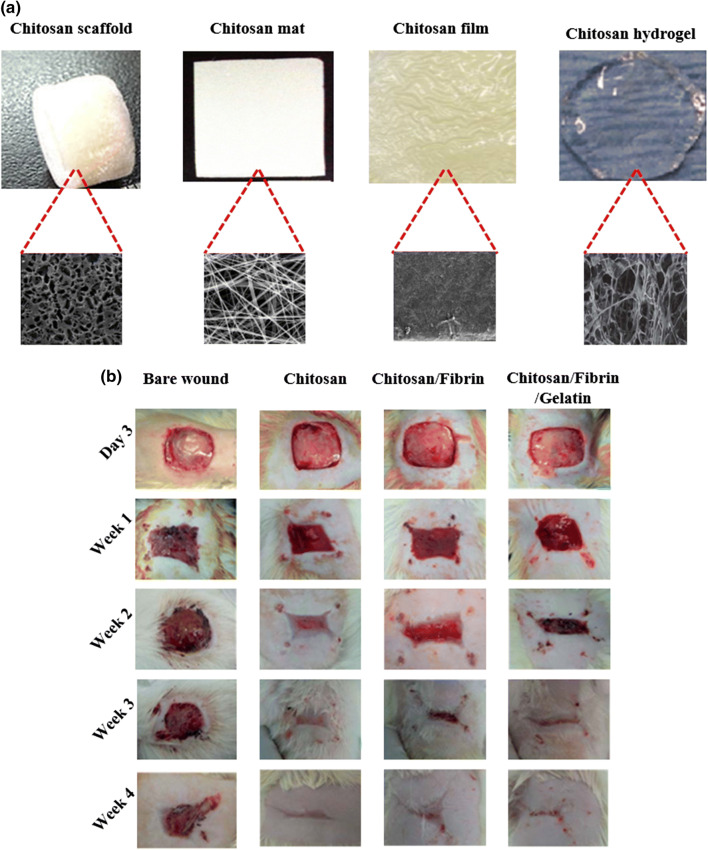
Fig. 3.
a Chitosan is a flexible material that can be used in various forms, including scaffold (reprinted from Ref. [79] with permission from springer), mat [81], film (reprinted from Ref. [80] with permission from Elsevier B.V.) and hydrogel (reprinted from Ref. [84] with permission from Royal Society of Chemistry). Each form possesses a unique characteristic that allows researchers to use them for different purposes. b The hydrogel form of chitosan and chitosan-blended materials for the treatment of burn wounds in the rat model. As shown in the picture, chitosan exhibits a high potential for use as the wound dressing
(reprinted from Ref. [82] with permission from Royal Society of Chemistry)
CS enhances the function of macrophages. Macrophages are the dominant infiltrating cells that respond rapidly to the implanted biomaterials. In the inflammatory response, macrophages possess three main functions: antigen presentation, phagocytosis, and production of various cytokines and active substances such as TNF-α, IL-1β and nitric oxide (NO). Macrophages also play critical roles in tissue regeneration via secretion a wide spectrum of cytokines and growth factors to regulate cell recruitment, proliferation, and differentiation. The way macrophages respond to biomaterials depends on the size of materials [87, 88]. Da Silva et al. [89] reported the size-dependent effect of chitin in murine macrophages. They showed that chitin induces IL-17A and IL-17A receptor expression in macrophages. They also found that these responses deeply depend on Toll-like Receptor 2 (TLR-2) and MyD88 functions. CS oligosaccharide also mediates its biological impacts on macrophages through toll-like receptor 4 (TLR-4) [90]. In a study, the COS solution (at the concentration range of 50, 100, and 500 μg/ml) inhibited the production of active molecules, including NO, IL-1β and TNF-α in LPS-stimulated RAW264.7 cells (in vitro macrophage model system) through the NF-κB (nuclear factor kappa B) signaling pathway. These cytokines have an important role in the pro-inflammatory stage of wound healing. Thus, CS could be used as a suppressive biomaterial in this stage [91].
There are also a few controversial studies about the impact of CS on mast cells function. Mast cells are associated with inflammatory responses and originated from pluripotent precursors of the bone marrow. These cells are very important to initiate inflammatory interaction and immediate allergic reactions [92]. There are different pathways that activate these cells and eventually cause the releasing of α-granules from mast cells [93]. Vo et al. [94] reported the suppressive effect of the COS solutions (200, 500, and 1000 μg/ml) on the RBL-2H3 mast cells activation in a dose-dependent manner. But these findings were not in line with those obtained from Farrugia et al. [95] investigation which shown the CS in the solution form (0.1 and 0.4 mg/ml) caused the release of beta-hexosaminidase from mast cells. However, the molecular details about the effect of CS on mast cells are unclear, and it is important to find the molecular mechanism of interaction between CS and mast cells.
Chitosan and cancer cells
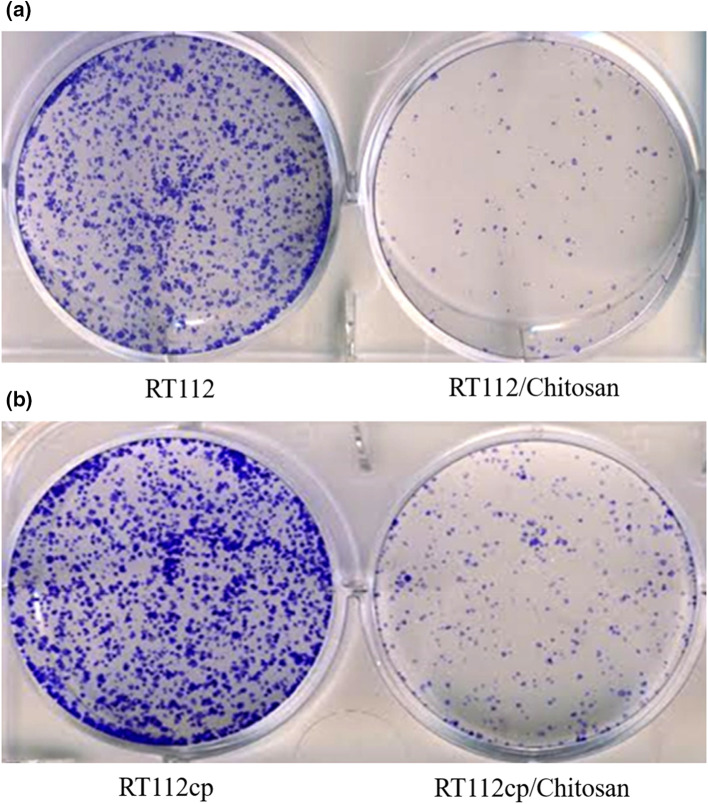
In the recent past, the anti-cancer property of CS has been well investigated by evaluating its effect on different cancer cell lines (Fig. 4). It is found that different CS parameters such as DD and MW can profoundly affect its anti-cancer characteristic [25]. In a study, the effect of various solutions of HMWC-derived products obtained from enzymatic hydrolysis was investigated on three different cancer cell lines including Human PC3 (prostate cancer cell), A549 (carcinomic human alveolar basal epithelial cell), and HepG2 (hepatocellular carcinoma cell) at a concentration range of 0.75–50 µg/ml. It was reported that the products with lower molecular weight and higher solubility, and DD showed better anti-cancer effects [25]. However, the effect of these CS parameters on cancer cell viability may vary based on the type of cancer cell lines. For instance, evaluating the cytotoxicity of the CS solution (500 µM) with different DA and MW on bladder carcinoma cells (RT112 and RT112cp) showed that the MW exhibited no significant effect on CS anti-cancer property, while DA played an undeniable role in the context [96].
Fig. 4.
a Clonogenic assay results of RT112 cell line with and without chitosan and b chitosan could remarkably diminish the number of colonies of cisplatin-resistant RT112 cell lines
(reprinted from Ref. [96] with permission from Elsevier B.V.)
The sensitivity of different cancer cell lines to CS is not similar (Table 1). Zou et al. [97] studied the anti-cancer effect of the COS solution on ten different cancer cell lines including BGC-823, SGC-7901, A549, NCI-H460, KCC-853, 786-O, HCT-116, HT-29, MCF-7, and Bcap-37. In that study, COS exhibited a wide-spectrum anti-cancer activity against all the aforementioned cells with various IC50, depending on the cell line. According to their report, the highest and lowest IC50 value of COS was observed for HCT-116 (1329.9 ± 93.4 µg/ml) and MCF-7 (48.6 ± 7.0 µg/ml), respectively. So far, different mechanisms have been suggested for the anti-cancer effect of CS. Induction of apoptosis and cell cycle arrest are two main involved mechanisms in the context [98]. Exposure of the LMWC solution to Ca9-22 (oral squamous cell carcinoma) and HaCaT (non-cancer keratinocyte) showed the cytotoxic effect of CS on Ca9-22 (IC50 = 800 ± 131.45), but not HaCaT cells. The G1/S cell cycle arrest and increased number of apoptotic cells with elevated caspase activity were found in the LMWC-treated Ca9-22 cells [98]. One possible explanation for the opposite effect of LMWC on Ca9-22 and HaCaT is differences in cytotoxic mechanism due to a higher negative charge of the cancer cell membrane compared with normal cells [99]. The positive charge of CS amino groups effectively forms the electrostatic interaction between the polymer and the negative charge of the cell membrane. Targeting cancer cells by CS may occur through a direct attack on the cell membrane, receptor-mediated manner or via endocytosis [72]. The electrostatic interaction between CS and cell membrane may disrupt it and lead to secretion of some inflammation-related cytokines such as IL-6 and IL-8. The mitogenic effect of these cytokines on normal keratinocytes and fibroblasts has been well proved [100]. In the cancer cells, IL-6 and IL-8 secretion in response to cell membrane damages may be impaired which gives another reason for differences in the cytotoxic effect of CS on cancer and normal cells. In the aforementioned study, LMWC-treated Ca9-22 showed a higher population of the cells arrested in G1/S, as well as a higher percentage of the cells in G1 phase [98]. In these circumstances, various cell signaling pathways such as ATM/ATR-Chk1/Chk2-Cdc25A-Cdk2 and TGF β-p15/p27-Cdk4/Cdk6 may play a role. Treatment the cells with LMWC may increase the expression of TGF-β which eventually causes cell cycle arrest in G1 and S phase. TGF-β activates a cascade of intercellular signaling such as Smads 2/3, Smad 4, p15, and p21 that activates the secretion of reactive oxygen species (ROS) and ultimately cell senescence [101].
Table 1.
A summary of anti-cancer activities of chitosan and its derivatives
| CS/CS-derived products | In vitro/in vivo | Reported results | MW/DA | References | Year |
|---|---|---|---|---|---|
| COS | MDA-MB-231 (in vitro) | Reduction in MMP-9 secretion and activities | 1 kDa < MW < 3 kDa | Kyung et al. [196] | 2009 |
| COS |
LLC (in vitro) HepG2 (in vivo) |
Inhibition of MMP-9 secretion Inhibition of the tumor growth |
MW = 23.99 kDa | Shen et al. [103] | 2009 |
| COS | PC-3, A549 (in vitro) | Suppression of cancer cell growth |
DD = 85–100% MW = 360–2625 m/z |
Park et al. [25] | 2011 |
| CSO–SA | MCF-7, A549, Bel-7402 (in vitro) | Discovered anti-cancer activities of podophyllotoxin loaded on CSO–SA micelles |
DD = 95% MW = 15.0 kDa |
Huang et al. [197] | 2012 |
| Sulfated polysaccharide | SKOV3 and ECV304 cells (in vitro) | Inhibition of MMP-2 expression | MW = 11.3 kDa | Zong et al. [198] | 2013 |
| O-Carboxymethyl-chitosan | Human normal liver cell L02, human hepatoma cell Bel-7402, human gastric cancer cell SGC-7901 and human cervical carcinoma cell Hela | Cytokine levels were compatible in vitro. In vivo, nontoxic to body and enhanced body immune response, serum levels of IL-2 and TNF-α in sarcoma-180-bearing mouse |
DD = 78.0% MW = 340 kDa |
Zheng et al. [199] | 2011 |
| CSOSA-g-PEI | Hela and MCF-7 | Comparable transfection efficiency level of CSOSA-g-PEI to lipofectamine 2000 |
DD = 95.0% MW = 17.5 kDa |
Hu et al. [200] | 2013 |
| CSOAA (conjugate for doxorubicin (DOX) delivery) | FaDu cells (in vitro) and FaDu tumor xenografted mouse model (in vivo) | Control drug release profile. In addition, cellular uptake |
DD = > 90% MW = 5 kDa |
Termsarasab et al. [201] | 2013 |
| FA–PEG–COL | BALB/c mice bearing OVK18 #2 tumor xenograft (in vivo) | Showing much potential for effective ovarian cancer treatment via gene therapy |
DD = > 90% MW = 3–5 kDa |
Li et al. [202] | 2014 |
| CTS | RT112 bladder cancer cell lines (In vitro) | CS exhibited a remarkable reduction in proliferation of RT112 cell line. CTS with lower MW found to be more effective than higher MW ones |
DD = 70–90% MW = 5800 and 19,800 g/mol |
Younes et al. [203] | 2014 |
| CTS (LMWC) | Ca922 cells (in vitro) | G1/S cell cycle arrest subtle increases of caspase activity |
DD = 75–85% MW = 50–190 kDa |
Wimardhani et al. [98] | 2014 |
| CS | Bladder carcinoma cells (RT112 and RT112cp) |
Cytotoxic effect of chitosan increased with increasing DA and decreasing pH MW had no effect on toxicity of CS |
DD = 39–98% MW = 75,000–110,000 g/mol |
Younes et al. [96] | 2015 |
| CS | IMR 32/Hep G2 cells (in vitro) | Moderate anti-proliferative effect |
DD = 90.2–93.3% MW = 382.73–423.43 kDa 212.93–548.75 kDa |
Chien et al. [204] | 2016 |
| COS |
10 tumor cell lines (In vitro) S180-bearing mice (in vivo) |
HCT-116 cells were the least sensitive to COS MCF-7 cells were the most sensitive to COS Stimulation of M1 type macrophage and production of TNF-α |
DD = 90–93% MW = 1–2 kDa |
Zou et al. [97] | 2016 |
| COS | HeLa cells (in vitro) | At concentration of 40 mg/ml, an abnormal morphology was found in HeLa cells |
DD = 80% MW = 1.44 kDa |
Chokradjaroen et al. [205] | 2017 |
| CS | Ovarian cancer cell line—PA-1 (in vitro) | 100% growth suppression of the of PA-1 tumor cells at low concentration at 10 µg/ml | Not reported | Srinivasan et al. [206] | 2018 |
COS chitosan oligosaccharide, CS chitosan, CSO–SA stearic acid-g-chitosan oligosaccharide, CSOSA-g-PEI polyethylenimine-conjugated stearic acid-g-chitosan oligosaccharide micelles, FA–PEG–COL folic acid–poly(ethylene glycol)–chitosan oligosaccharide lactate, CSOAA chitosan oligosaccharide–arachidic acid, LMWC low molecular weight chitosan, MMP matrix metalloproteinase, DA degree of acetylation
However, other mechanisms have also been suggested for cancer cytotoxicity of CS. MMP-9 is a well-known enzyme which is associated with metastasis risk [102]. This enzyme digests the extracellular matrix and makes the cancer cell susceptible to escape from a solid tumor. It is obvious that targeting MMP-9 could be an effective strategy to reduce the invasiveness of cancer cells. In this direction, Shen et al. [103] reported the dose-dependent inhibitory effect of the COS (100, 500, and 1000 µg/ml) on MMP-9 secretion in Lewis lung carcinoma (LLC) cells. The LLC mice model treated by COS showed regression of tumor growth, decreased number of metastatic colonies in the lung, and lengthened survival time compared to controls.
In addition to the mentioned mechanisms, it seems the immune system has a part in the anti-cancer effect of CS. CS exerts its anti-tumor impact by activating the cells involved in the immune system such as lymphocytes, natural killer cells (NK), and macrophages [104]. For instance, oral administration of COS can effectively promote intraepithelial lymphocytes to secrete some macrophage activator cytokines such as interferon (IFN)-γ and interleukin (IL)-12. Further studies show the ability of COS to increase lymphocyte cytokines by accelerating T cell proliferation. Besides these, intraperitoneal injection of COS has been associated with an increased number of tumor suppressor M1 macrophages producing TNF-α. These findings suggest that TNF signaling pathway may also have a critical role in the anti-cancer effect of CS [105].
Chitosan and platelet
CS hemostatic effect has been well investigated in the literature [106–108]. Studies show that CS through binding, activation, and aggregation of platelets can cause hemostasis, and accelerate the healing process of damaged tissue [109]. It is reported that the presence of CS causes remarkable changes in platelets at both morphological and gene expression levels. CS induces filopodia and lamellipodia in platelets and promotes them to generate a grapes shape structure which eventually decreases hemostasis time. CS also induces the gene expression of platelet activation markers such as P-selectin and glycoprotein IIb/IIIa. These cell surface proteins facilitate platelet accumulation around the damaged area. In addition, CS induces secretion of various cytokines from activated platelets such as EGF, TGF-β1, and PDGF-AB [107, 109, 110]. CS significantly diminishes the blood coagulation time (BCT). Okamoto et al. [111] reported that the canine whole blood exhibited a decreased BCT in the presence of the CS micro-particle suspension (0.3 mg/ml). Moreover, CS mixed platelet-rich plasma (PRP) showed a promoted platelet aggregation (PA) in a dose-dependent manner (0.01–2 mg/ml). Change in intracellular calcium concentration is one of the proposed mechanisms for the effect of CS on platelets. Non-activated platelets maintain a low intracellular calcium ion concentration (0.1 µM). Platelet contact with the extracellular matrix such as collagen causes an increased cytosolic concentration of calcium, which in turn increases the expression of glycoprotein IIb/IIIa. It is reported that CS similarly increases intracellular calcium concentration in platelets.
Chitosan and chondrocytes
Osteoarthritis (OA) is the most common age-related degenerative disease which is generally identified by joint dysfunction due to various factors such as articular cartilage degradation, chondrocyte apoptosis, extracellular matrix damage and a remarkable loss in tissue cellularity [112, 113]. IL-1β seems to play a key role in the pathogenesis of OA. It is found that the expression of this protein is remarkably increased in patients with OA. IL-1β protein, directly or indirectly, involves in a series of biological events which eventually cause cartilage degradation [114]. Chondrocytes, as the main population cells of cartilage, are responsible for the production and maintenance of the extracellular matrix of cartilage [115]. Due to the presence of a large quantity of IL-1β receptors on chondrocyte surface, it is a basic target for this cytokine. It is conceivable that the inhibition of the IL-1β pathway can be a promising therapy to prevent cartilage degradation during OA pathological process. In vitro study on IL-1β-induced chondrocytes showed the dose-dependent anti-apoptosis property of the COS solution on such cells at a concentration range of 50–200 µg/ml. The COS could greatly increase the cell viability of IL-1β-induced chondrocytes as compared to controls. Morphological analysis exhibited a strong impact of COS on the overall integrity of nuclear chromatin in the IL-1β-induced chondrocytes. The COS also stabilized the integrity of the mitochondrial membrane and prevented the destruction of the mitochondrial membrane potential. It is suggested that the cationic charge of this polysaccharide may have a part in the membrane stabilizing property of CS due to binding to the various cell surface glycoproteins. In that study, COS strongly shifted the Bcl-2/Bax balance in favor of Bcl-2. It is found that the polysaccharide effectively induced the expression of Bcl-2 in the IL-1β-induced chondrocytes which were significantly higher compared with the controls. Expression of Cas-3, as the main trigger of apoptosis cascade, was also remarkably diminished in the COS-treated IL-1β-induced chondrocytes [116, 117].
The NO, as a critical factor in chondrocytes apoptosis, is found to be increased in synovial tissue and articular cartilage of patients with OA [118]. Indeed, IL-1β provokes chondrocytes to up-regulate the expression of iNOS [119, 120]. NO increasing in IL-1β-induced chondrocytes leads to the activation of the p38/MAPK pathway. As mentioned before, p38/MAPK cell signaling involves many inflammatory and apoptosis-related responses (e.g., up-regulation of Cas-3 and downregulation of Bcl-2) [121, 122]. The p38/MAPK also regulates the expression of MMP and TIMP proteins. COS treatment of IL-1β-induced chondrocytes revealed to decrease the expression of iNOS via decreasing the p38/MAPK phosphorylation. In addition, COS up-regulated the expression of TIMP proteins which have inhibitory effects on MMP function [117]. To confirm the in vitro findings, Xi Lu et al. [123] reported the therapeutic potential of the CS solution on rat knee cartilage. They revealed that the injection of 0.2 ml of 0.1% CS solution inside the articular cavity of the rat knee caused the growth of epiphyseal cartilage and positively affected the proliferation of fibrous tissue.
Chitosan and osteoblasts
CS accelerates bone regeneration. It is commonly used as a biomimetic material for treatment of bone trauma [124]. Due to its biocompatibility, biodegradability, and porosity, CS has been considered as a popular biomaterial for orthopedic TE [125–127]. The underlying mechanism by which CS governs its effect on bone mineralization has not yet been elucidated in detail. A wide range of cellular and molecular events participate in controlling bone growth and fracture repair. It is found that osteocalcin (OCN) and alkaline phosphatase (ALP) are two typical osteoblast biomarkers involved in regulating ECM mineralization in osteogenesis and osteoblast function during bone regeneration [128]. These biomarkers would be up-regulated during differentiation and maturation of osteoblasts [129, 130]. CS is able to enhance the ALP activity on osteoblasts in vitro. Ohara et al. [131] reported that COS solution at the optimized concentration of 0.005% w/v elevated the ALP activity of cultured osteoblasts. It seems that COS directly speeds up cell proliferation of osteoblasts via up-regulating gene expression of some cell binding and adhesion molecules such as neural cell adhesion molecule (CD56) and tissue-type plasminogen activator (t-PA). It may explain why ALP activity is increased in such cells while there is no significant difference between ALP mRNA expressions of COS-treated cells and controls. Beside this, COS remarkably enhances BMP-2 gene expression in osteoblasts [131]. It is proven that BMP-2 protein initiates differentiation of osteogenic lineage from multipotent mesenchymal progenitor cell lines [132]. In brief, CS can stimulate both differentiation and proliferation in osteoblasts through BMP-2 mediated pathway.
Runt-related transcription factor 2 (Runx2) is a crucial transcription factor for osteoblast differentiation and mineralization [133, 134]. Overexpression of this protein leads to osteogenesis and bone regeneration [135]. Furthermore, it is reported that Runx2 mediates nitric oxide-induced osteoblast protection against apoptosis via controlling Bcl-2 expression [136]. CS also promotes differentiation of osteoblasts by activation Runx2 signaling pathway [137]. Ho et al. [138] note that seeding osteoblasts on chitosan nanofiber scaffold caused activation of Runx2 signaling pathway followed by maturation of osteoblasts. In view of this property, using CS nanofiber scaffold in vivo exhibits a powerful effect on promoting bone regeneration via improving production, connectivity, and thickness of the trabecular bone.
Chitosan and retinal cells
The eye has specific vulnerabilities due to constant contact with harmful environmental factors. Ocular diseases such as glaucoma, diabetic retinopathy, and age-related macular degeneration are often the result of oxidative stress. Using new approaches, such as antioxidant biomaterials, can be a strategy to treat such diseases. Recently, a lot of attention is given to CS as an antioxidant biomaterial. It is found that CS dramatically increases intracellular GSH (Glutathione) level in various cell lines [139, 140]. GSH directly interacts with the redox system (ROS) as a cofactor of the glutathione peroxidase enzyme to protect cells from oxidative stress [141]. Several studies show the inhibitory effect of COS on (NF-κB) signal transduction pathway which can be activated in response to oxidative stress [142–144].
CS reduces oxidative-induced retinal damage through the inhibition of apoptotic pathways. Fang et al. reported that the COS solution (100 µg/ml) improved the activity of antioxidant enzymes including catalase, GSH, and SOD, and also decreased ROS levels in the retina. In the transcription level, COS attenuated the DNA-binding ability of NF-κB by decreasing expression of the p65 protein which is responsible for initiation of transcription activity of NF-κB heterodimer. On the other hand, COS enhanced the expression level of IκB protein which plays an inhibitory role for NF-κB heterodimer in the cytosol. COS also effectively decreased Bax/Bcl ratios where they have an important role in cell apoptosis regulation [145]. Bax is a proapoptotic protein that leads to an apoptotic cascade, whereas Bcl-2 prevents apoptosis [146].
Fang et al. [147] reported that COS effectively protected the retinal cells from ischemia and reperfusion (I/R) injury in the rat model. According to their findings, intraperitoneal injection of the COS solutions (5 and 10 mg/kg), before inducing ischemia and reperfusion, attenuated oxidative stress by decreasing various factors such as inflammatory mediators (TNF-a, IL-1b, MCP-1, iNOS, ICAM-1), P53, and Bax. Moreover, COS affected two signaling pathways involved in oxidative stress by reducing the phosphorylation of JNK and ERK. They also showed that COS improved the phosphorylation level of P38 protein which is known as the main member of mitogen-activated protein kinase (MAPK). MAPK family consists of different factors which are involved in the secretion of various pro-inflammatory cytokines. It is suggested that the neuroprotective effect of P38 may be exerted via activation of Bcl-2 factor.
Chitosan and stem cells
CS’s effect on cell differentiation and proliferation of stem cells has been well documented in many studies [148–150]. Wang et al. [151] reported the great capacity of CS on proliferation and differentiation of rat’s neural stem cells (NSCs). According to their finding, chitosan film changed the morphological properties of the attached NSCs into the neural-like cells. Mesenchymal stem cells seeded on the CS film exhibited an increased expression level of Oct4, Sox2, and Nanog compared with 2D culture systems. Besides this, the mesenchymal stem cells interestingly tend to differentiate into the nerve cells and chondrocytes in the presence of CS film [152]. It is also reported that using blended chitosan and alginate (CA) scaffold enhances self-renewal of human embryonic stem cells (hESCs) without requiring of fibroblast-conditioned media or feeder cell layer. Using a feeder layer is associated with an increased risk of environmental contamination. Therefore, developing CS scaffold based-cell culture system for hESCs can be widely utilized in TE applications [153].
The lack of an efficient cell delivery system is one of the main concerns of researchers regarding cell-based myocardial regeneration [154]. Improving the myocardial infarction (MI) microenvironment to enhance the engraftment, survival and homing of stem cells, has become a serious challenge in myocardial TE field. In this respect, Liu et al. developed an injectable CS hydrogel for delivery of adipose-derived mesenchymal stem cells (ADSC) into the ischemic heart. They reported that the presence of ROS in damaged tissue may have a negative effect on ADSC adhesion molecules (αV, β1, p-FAK, and p-Src) involved in engraftment and homing of such cells. On the other hand, ROS may impair some host myocardium ligands such as ICAM1 and VCAM1 which are involved in stem cell engraftment. The developed CS hydrogel could improve the cell engraftment via removing ROS and also increases some cytokines involved in stem cell homing such as SDF-1 protein [155].
According to the literature, topographical structures of CS scaffolds can interestingly affect the behavior of stem cells. For instance, micro-hills on CS scaffold promote the proliferation and alignment of MSCs [156]. It is also reported that the chondrogenesis of MSCs on CS microfiber scaffolds is significantly higher compared to CS macroporous sponge scaffolds. COS is also able to influence the gene expression and cytokine secretion of hMSC but no significant impact on mineralization [157].
Chitosan and nerve cells
Neurodegenerative diseases include a wide range of progressive diseases with the destruction of neurons (nerve cells) in the central nervous system (CNS) that led to cognitive and motor disabilities in patients [158]. Alzheimer’s, Parkinson’s, and Huntington’s diseases are the most well known of such diseases [159]. These disorders can also appear as secondary complications in brain tumors, multiple sclerosis (MS), ALS, and spinal cord injury. Oxidative stress has been proven to play a pivotal role in their emergence [160]. The brain damages can elevate the oxidative stress via activating and producing the pro-inflammatory cytokines by microglial cells [161]. Beside this, increased oxidative stress can occur through other pathological conditions, such as increased glutamate concentration and miss-folded proteins accumulation in neurons [162, 163]. Until now, many efforts have been made to treat neurodegenerative diseases. CS has been shown to possess a promising neuroprotective effect. In general, CS exerts its protecting influence on neurons through various mechanisms, most notably the anti-oxidative stress effect [164]. For instance, a study on glutamate-induced PC12 cells showed that the use of pre-acetylated chitosan (PACOS) at the optimized concentration of 200 µg/ml significantly reduced the production of ROS in these cells [112]. In another study, Wei et al. [165] found that the COS had a protective effect on Cu (II)-induced cortical neuronal cells by reducing the production of ROS. The role of Cu (II) and another metal ions such as Fe(II) accumulation in initiating oxidative stress in neuronal cells and its association with neurodegenerative disease such as Alzheimer have been well proven [166]. In Wei’s study, treatment of Cu (II)-induced cells with the COS solutions at concentrations of 0.1–0.4 mg/ml could increase cell viability in a dose-dependent manner. Using the LDH assay, they also showed that the COS significantly reduced the Cu (II)-mediated cell membrane damages in the rat cortical neuronal cells [165].
Oxidative stress can occur as a result of increased glutamate concentrations in cells. Two different mechanisms are involved in glutamate-mediated oxidative stress: the massive influx of extracellular Ca2+ and preventing of cysteine uptake [112, 167]. So, targeting these pathways provide a suitable strategy to prevent glutamate-mediated oxidative stress. It is reported that COS treatment of glutamate-induced rat hippocampal neurons could effectively improve their cell viability as compared with controls. Meanwhile, the measurement of intracellular Ca2+ concentration using Fluo-4-AM fluorescence dye showed that the COS (at the concentration of 1.0 mg/ml) remarkably diminished the entrance of Ca2+ into the hippocampal neurons and significantly decreased the percentage of proapoptotic cells [168].
As previously mentioned, chronic inflammation can play a major role in the onset and progression of neurodegenerative diseases [161]. Anti-neuroinflammatory characteristic of CS suggests it as a therapeutic option to reduce inflammation and symptoms of neurodegenerative diseases such as Alzheimer’s. Kim et al. [169] investigated the effect of CS on the IL-1b and Ab fragment 25–35-induced human astrocytoma cell line (CCF-STTG1). According to their results, the CS solution (10 µg/ml) significantly decreased the secretion of IL-6 and TNF-α in the stimulated cells. CS treatment also reduced the expression level of iNOS in the cells. In another study, Pangestuti et al. [170] showed that CS derivatives decreased the microglial activity. According to their reports, the COS solution (500 µg/ml) attenuated the production of nitric oxide and prostaglandin E2 and had a suppressive effect on the release and expression levels of IL-1β, IL-6, TNF-α, and JNK/MAPK2 phosphorylation.
The anti-apoptotic effect is another protective mechanism of CS on neuronal cells. Since neuronal cell apoptosis plays an important role in the clinical manifestations of neurodegenerative diseases, its prevention can be an effective way of reducing the progression of such diseases [171]. So far, the anti-apoptotic effect of CS on neuronal cells has been reported in several studies [172, 173]. Most of the findings are related to the reduction of caspases activities and increasing the Bax/Bcl-2 ratio. For instance, glutamate-induced PC12 cells in the presence of pre-acetylated chitosan (PACO) exhibited lower expression of Bax protein. These cells also showed less activated Cas-3 and 9, as well as a lower percentage of cytochrome c release from mitochondria compared with those not treated with PACO [112]. Similar results were found in another study where the effect of CS on dibutyltin (DBT)-induced-PC12 cells was investigated. In that study, gene expression evaluation indicated that the CS solution (50–200 µg/ml) significantly reduced the expression of Bax, Bad, Apaf-1 and cytochrome c genes, and increased the expression of Bcl-2 and Bcl-xL genes in the DBT-stimulated PC12 cells in a dose-dependent manner. This study also showed that the Cas-3 and -9 showed a significant reduction in the presence of CS in both genes and proteins level in the DBT-induced PC12 cells [172]. Prevention of apoptosis can also occur by inactivating the p53 protein [174]. CS has been shown to prevent apoptosis in the human astrocytes by inhibiting the activation of P53. Koo et al. [173] indicated that high-weight water-soluble chitosan (WSC) at the concentration of 10 µg/ml could suppress the serum starvation-induced activation of P53 in the astrocytes which eventually protected them from apoptosis.
The accumulation of β amyloid proteins, which form senile plaques, is a characteristic of some neurodegenerative diseases, especially Alzheimer’s. The presence of these plaques in patients with Alzheimer’s disease is one of the main causes of clinical manifestations in these patients [175]. Significant failures in reducing symptoms of Alzheimer despite current treatments have led researchers to seek out alternative therapeutic choices using natural ingredients. Regarding the non-toxicity of CS, this polymer has been studied as a therapeutic option to prevent the formation of amyloid plaques in several studies [142, 176]. For example, the COS solutions (2.5 and 5 mg/ml), in a dose-dependent manner, inhibited the aggregation of Aβ42 and the formation of β-sheet structures in the rat hippocampal neuron cells. CS also prevented the formation of Aβ42 fibrils and even disrupted the preformed fibrils in the hippocampal neuron cells [176]. Khodagholi et al. [142] reported that CS due to its anti-oxidative effect can inhibit the amyloid plaque formation in the NT2 cells. According to their findings, CS at a concentration of 0.1–0.5 w/v could remarkably elevate the production of proteins involved in oxidative stress response including HO-1, c-GCS, Hsp-70 through activation of the Keap1–Nrf2 signaling pathway. These proteins are reported to have a protecting effect against oxidative stress. They also showed that CS reduced the expression of the NF-κB, which plays a major role in the production of pro-inflammatory cytokines. These results indicate the ability of CS to be applied in the treatment of patients suffering from Alzheimer’s disease.
The application of CS for developing a suitable scaffold in neural TE has been associated with positive results. It is reported that CS improves the cell adhesion and cell growth of neural cells. According to Cao et al. [177] reports, neural cells exhibited better attachment and growth in the presence of a blended hydrogel containing agarose and CS. They suggested that a steric hindrance effect of CS may play a part in morphological differences and desired cell attachment and outgrowth of such cells.
Chitosan and epithelial cells
Epithelial tissue contains different types of epithelial cell, covering various part of human organs such as skin, pancreas, salivary glands and digestive and respiratory tract [178]. Epithelial tissue is arranged in single or multiple layers which are characterized by tight intercellular connection and keratin-based cytoskeleton [179, 180]. Despite the overall similarity, different epithelial cells show various responses to biomaterials. So far, the impact of CS on the different types of epithelial cells has been investigated.
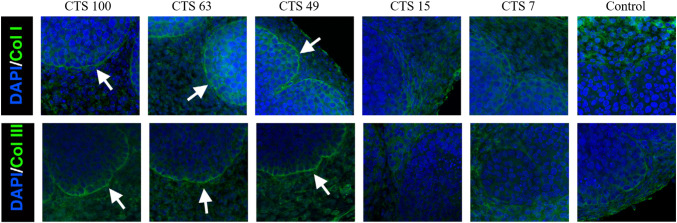
Branch morphogenesis plays an important role in the formation of glandular organs such as salivary and mammary glands. This phenomenon occurs due to the interconnection between epithelial cells, ECM and different signaling molecules [181]. Using CS as a scaffold for inducing branch morphogenesis has been accompanied by considerable results. It is reported that both CS parameters, DD and MW, have a direct effect on branch morphogenesis. DD directly influences the expression of ECM’s components such as COL I and COL III (Fig. 5) [182]. Hsiao et al. [182] used the CS solutions (0.3 mg/ml) with different DD for the culture of embryonic salivary glands. After 48 h, they assessed the formation of the branching structure. They found that the cells cultured on CS with DD of 49% showed the highest number of branching structures. It seems that the morphogenesis inducing the effect of CS strongly depends on FGF10–FGF2Rb signaling pathway. Study on explanted murine embryonic mammary gland cells on CS indicated that the interaction between FGF family, especially FGF 10, and CS has a strong impact on the formation of branching structures. CS, because of its cationic nature, provides a suitable anchorage for attaching and immobilizing various growth factors with the negative charge. Therefore, CS with higher MW better induces branching formation compared with the lower ones as a result of better interaction between chitosan chains themselves and also between chitosan and various growth factors [183].
Fig. 5.
Expression pattern of type I and III collagens in the embryonic murine submandibular gland in the presence of CS with different degrees of deacetylation. The highest expression rate of both type I and III collagens was observed in the chitosan groups
(reprinted from Ref. [182] with permission from Elsevier B.V.)
The epithelium of the nasal cavity consists of two main cell types including stratified squamous epithelium and columnar ciliated epithelium which prevent the entry of small and large particles to the body by entrapping them in the cilia. Moreover, mucus-producing glands in the nasal cavity help it to keep its moisture and also entrap the air-suspended particles and pathogens. In some situations such as sinus surgery, restoring the mucociliary mucosa and avoiding post-surgery adhesion formation must be considered. To avoid postoperative difficulties, different chitosan-based polymers have been applied to enhance the healing process. However, some interesting results have been obtained from the treatment of nasal epithelial cells (NECs) with CS [184]. Huang et al. [185] reported that CS solution (1% w/v) significantly diminished migration, proliferation, and mucociliary differentiation of the NECs. Morphological examination revealed that CS-treated NECs were found in an irregular shape without the formation of the tight junction. According to their results, CS via inducing TGF-β1/Smad2/Smad3 signaling decreases the expression of ZO-1 and changes the morphological structures of NECs. The CS also increased the expression of AQP3 and AQP5 which are involved in water balance and secretion of periciliary fluid in the nasal cavity. The effect of CS on the tight junctions has been investigated by several other studies. For example, CS via CaSR–Gq–PLC–IP3-receptor channel-dependent pathway increased the release of Ca2+ from endoplasmic reticulum which activated the AMPK signaling pathway in the T84 cells as a model for epithelial cells. Following AMPK activation, the tight junction assembly elevated, which decreased the secretion of chloride ion (Cl−) by suppressing the CFTR channel. Hence, it seems that COS shows great potential as a therapeutic strategy in the treatment of colorectal cancer chemoprevention and secretary diarrhea disorders [181]. In another study, Smith et al. [186] investigated the effect of CS on barrier characteristics of Caco-2 cell monolayers such as transepithelial electrical resistance (TEER). They reported that CS by translocation of ZO-1 in a dose-dependent manner (0.05–0.5% w/v), significantly decreased the transepithelial electrical resistance of Caco-2 up to 83%. According to cellular fraction analysis results, the concentration of both ZO-1 and occludin decreased at cytosol and cell membrane and increased at cytoskeleton fraction of the CS-treated cells. These data show the role of CS in the translocation of ZO-1 from cell membrane to the cytoskeleton, resulting in disruption of epithelial cell tight junctions.
In a few studies, the positive impact of CS in the treatment of inflammatory intestinal diseases such as inflammatory bowel disease (IBD) has been reported. Inflammatory bowel disease results from defection in the intestinal barrier and uncontrolled inflammatory responses to the damaged gastrointestinal tract. It is found that oral administration of COS may be an effective way in the treatment of IBD. In this respect, CS derivatives prevent NF-ƘB activation and also TNF-α and IL-6 production in the epithelial barrier. CS also contributes to the amelioration of diabetes by increasing of glucagon-like peptide-1 (GLP-1) production and secretion by intestinal cells. It is reported that CS via p38/MAPK-dependent signaling pathway can effectively elevate the production of glucagon-like peptide-1. Secretion of GLP-1 by intestinal L cells plays an important role in glucose homeostasis via inducing of insulin secretion, suppressing glucagon production, and decreasing food intake. These findings suggest CS as a suitable alternative for the treatment of diabetic patients [187].
Chitosan and endothelial cells
One of the most important reasons for the onset of the cardiovascular disease is the increased oxidative damages in the vascular endothelial cells [188]. The production of ROS by vascular endothelial cells plays an undeniable role in the development of some critical clinical diseases such as atherosclerosis and hypocholesteremia [189, 190]. Increasing ROS in cells can cause irreparable harm through various ways such as inactivation of vital enzymes for the cell, oxidation of membrane lipids, and induction of apoptosis [191]. Therefore, the use of substances with the ability to reduce free radicals may have a preventative effect on oxidative stress. CS is one of the biomaterials which help to reduce the oxidative stress damages. A study on the effect of chitosan on H2O2-treated ECV304 cells showed that the concentration of 100–200 µg/ml CS remarkably reduced the amount of the ROS in the treated cells [140]. One possible reason for this phenomenon is the protection of the endogenous antioxidants, such as SOD and GSH-Px, as well as the reduction of oxidation of lipids by CS. CS also significantly increased the NO levels in the treated cells. NO has an important role in regulating the functions of endothelial cells, in turn, reducing NO levels can increase the oxidative flow in cells [140]. This finding was not in line with other studies in which CS prevented NO production in HT-29 and RAW264.7 cells [69, 192]. This controversy appears to be due to the differences in the cell types and variability in the pro-inflammatory cytokines. The effect of CS on H2O2-treated ECV304 cells showed that these cells exhibited a less pre-apoptotic phase compared with the control. Based on the flow cytometry results, the H2O2-treated cells showed a high percentage of cells arrested in the G0/G1 stage, which was different for CS-treated cells, so that the treatment with CS increased cell arrest in the G1/S and M phase. CS also promoted the proliferation rate of these cells compared with the control group [140]. The findings regarding the effect of CS on the induction of apoptosis in the aforementioned study were not consistent with the results obtained in other studies. For example, Wang et al. [193] reported that the N-acetyl-COS at a concentration of 250–1000 µg/ml decreased the proliferation rate and showed an increased pre-apoptotic effect on the HUVECs cells. One explanation for this controversy can be differences in the applied doses of CS. The anti-apoptotic effect of this substance appears to be completely dose dependent, so at the high doses, it even has an apoptotic effect on the endothelial cells.
CS influences the secretion of cytokines in endothelial cells. For instance, COS at the concentrations of 50–200 μg/ml inhibited the LPS-induced IL-8 production in endothelial cells. This phenomenon occurs due to blockade of p38/MAPK and PI3k/Akt signaling pathways [194]. Moreover, COS down-regulated the ICAM-1 (at the concentrations of 50–200 µg/ml) and E-selectin (only at the concentration of 200 µg/ml) expression in endothelial cells by inhibiting the phosphorylation of MAPK and activation of NF-ƘB [195] (Fig. 6). Liu et al. [153] found that the COS (50–200 µg/ml) decreased the IL-6 levels in endothelial cells after exposure to the LPS. It seems that NF-ƘB-independent P38/MAPK activation and NF-ƘB-dependent ERK1/2 are the two signaling pathways involved in the context.
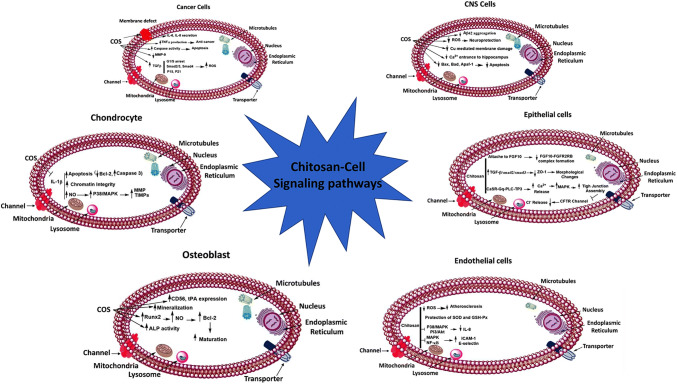
Fig. 6.
The effect of chitosan on cell signaling pathways in different cell types
Conclusion and future perspective
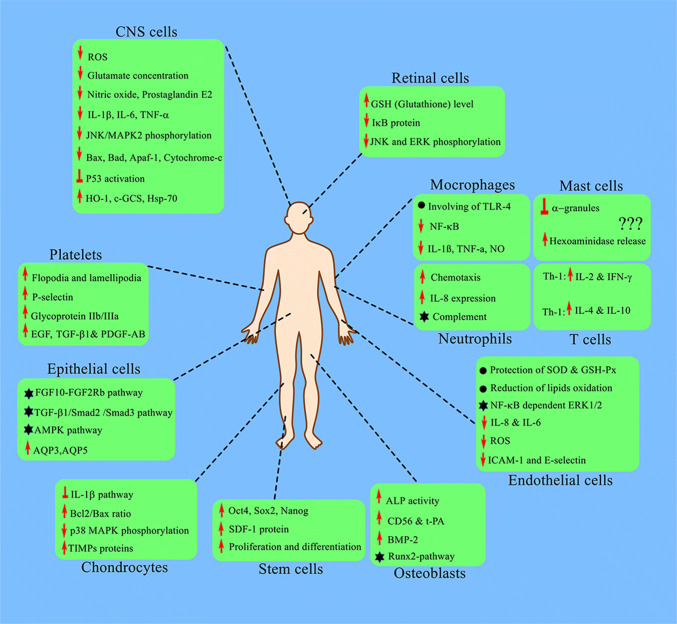
Nowadays, with the advances in the tissue engineering field, new approaches based on cell and scaffold interaction are being developed to treat the injured tissues. The increasing progress of this branch of medical sciences has opened a promising window to find definite and effective ways for the development of a whole tissue or organ in vitro to be replaced with the damaged ones in the body. To this end, researchers are studying various types of natural and synthetic materials to find suitable scaffolds in the context. CS is one of the widely used materials in various aspects of TE. The characteristics such as appropriate biodegradability, high biocompatibility, antibacterial properties, and suitable mechanical behavior make CS as a popular biomaterial among researchers. Numerous studies have been carried out to survey the effect of CS on the behaviors and biological functions of different cell types (Fig. 7). The importance of these studies is that understanding the crosstalk between cells and materials provides a vital clue for the best design of scaffolds. As the behavior and function of the various cell types are unique, their response to a certain material would be different. In the present study, we aimed to review the literature on the interaction between CS and different cell types. It is obvious that there are many undefined signaling pathways involved in CS effect on the functions of various cell types. Future studies can help to further clarify the response of different cells to this popular biopolymer to design a comprehensive map for use in various aspects of the TE field.
Fig. 7.
Chitosan induces various cell responses in different cell types. Identifying the crosstalk between chitosan and different cell types and comparison of results help researchers to more wisely use of this polymer in their studies (up arrow: increase; down arrow: decrease; star: activation; perpendicular sign: blockage)
Acknowledgements
We would like to show our gratitude to Dr. Saman Mohammadiamanab for his comments on this paper.
Compliance with ethical standards
Conflict of interest
There is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mehrdad Moosazadeh Moghaddam, Phone: (+98 21) 82482563, Email: mm.genetics@gmail.com, Email: rsr.moosazadeh@bmsu.ac.ir.
Mazaher Gholipourmalekabadi, Phone: (+98 21) 8862 2755, Email: mazaher.gholipour@iums.ac.ir, Email: mazaher.gholipour@gmail.com.
References
- 1.Gholipourmalekabadi M, et al. Optimization of nanofibrous silk fibroin scaffold as a delivery system for bone marrow adherent cells: in vitro and in vivo studies. Biotechnol Appl Biochem. 2015;62:785–794. doi: 10.1002/bab.1324. [DOI] [PubMed] [Google Scholar]
- 2.Hamidabadi HG, Shafaroudi MM, Seifi M, Bojnordi MN, Behruzi M, Gholipourmalekabadi M, Shafaroudi AM, Rezaei N. Repair of critical-sized rat calvarial defects with three-dimensional hydroxyapatite-gelatin scaffolds and bone marrow stromal stem cells. Med Arch. 2018;72:88. doi: 10.5455/medarh.2018.72.88-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gholipourmalekabadi M, Sameni M, Radenkovic D, Mozafari M, Mossahebi-Mohammadi M, Seifalian A. Decellularized human amniotic membrane: how viable is it as a delivery system for human adipose tissue-derived stromal cells? Cell Prolif. 2016;49:115–121. doi: 10.1111/cpr.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.del Mar Encabo-Berzosa M, et al. The effect of PEGylated hollow gold nanoparticles on stem cell migration: potential application in tissue regeneration. Nanoscale. 2017;9:9848–9858. doi: 10.1039/C7NR01853C. [DOI] [PubMed] [Google Scholar]
- 5.Ghasemi Hamidabadi H, et al. Chitosan-intercalated montmorillonite/poly (vinyl alcohol) nanofibers as a platform to guide neuronlike differentiation of human dental pulp stem cells. ACS Appl Mater Interfaces. 2017;9:11392–11404. doi: 10.1021/acsami.6b14283. [DOI] [PubMed] [Google Scholar]
- 6.Gholipourmalekabadi M, Chauhan NPS, Farhadihosseinabad B, Samadikuchaksaraei A. Human amniotic membrane as a biological source for regenerative medicine. In: Arjmand B, editor. Perinatal tissue-derived stem cells. New York: Springer; 2016. pp. 81–105. [Google Scholar]
- 7.Samadikuchaksaraei A, Gholipourmalekabadi M, Farhadihosseinabadi B, Rezvani Z, Mozafari M (2016) Carboxymethyl chitosan/forsterite bone tissue engineering scaffolds: correlations between composition and physico-chemical characteristics. Biointerface Res Appl Chem 6(3)
- 8.Delattre C (2017) Current opinion on chitosan and its derivatives: biological impact in antimicrobial applications from nature to chitosan and it derivatives: how it is working? Adv Biotechnol Microbiol 6(2)
- 9.Raafat D, Leib N, Wilmes M, François P, Schrenzel J, Sahl H-G. Development of in vitro resistance to chitosan is related to changes in cell envelope structure of Staphylococcus aureus. Carbohydr Polym. 2017;157:146–155. doi: 10.1016/j.carbpol.2016.09.075. [DOI] [PubMed] [Google Scholar]
- 10.Mustafa A, Sîrbu R. Studies on chitosan extraction and its biomedical properties. Eur J Pharm Med Stud. 2017;1:7–14. [Google Scholar]
- 11.Kim S-K. Chitin, chitosan, oligosaccharides and their derivatives: biological activities and applications. London: CRC Press; 2010. [Google Scholar]
- 12.Sugier K, Vacherie B, Cornils A, Jamet J-L, Wincker P, Madoui M-A (2017) Chitin distribution in the Oithona digestive and reproductive systems revealed by fluorescence microscopy. PeerJ (preprints) [DOI] [PMC free article] [PubMed]
- 13.Leedy MR, Martin HJ, Norowski PA, Jennings JA, Haggard WO, Bumgardner JD (2011) Use of chitosan as a bioactive implant coating for bone-implant applications. In: Chitosan for biomaterials II, pp. 129–165. Springer, New York
- 14.Cheung RCF, Ng TB, Wong JH, Chan WY. Chitosan: an update on potential biomedical and pharmaceutical applications. Mar Drugs. 2015;13:5156–5186. doi: 10.3390/md13085156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manigandan V, Karthik R, Ramachandran S, Rajagopal S (2018) Chitosan applications in food industry. In: Biopolymers for food design, pp 469–491. Elsevier, New York
- 16.Desbrieres J, Guibal E. Chitosan for wastewater treatment. Polym Int. 2018;67:7–14. doi: 10.1002/pi.5464. [DOI] [Google Scholar]
- 17.Song Z, Li G, Guan F, Liu W. Application of chitin/chitosan and their derivatives in the papermaking industry. Polymers. 2018;10:389. doi: 10.3390/polym10040389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ding F, Li H, Du Y, Shi X. Recent advances in chitosan-based self-healing materials. Res Chem Intermed. 2018;44:1–14. doi: 10.1007/s11164-018-3339-7. [DOI] [Google Scholar]
- 19.Silva SS, Mano JF, Reis RL. Ionic liquids in the processing and chemical modification of chitin and chitosan for biomedical applications. Green Chem. 2017;19:1208–1220. doi: 10.1039/C6GC02827F. [DOI] [Google Scholar]
- 20.Kim S-K, Rajapakse N. Enzymatic production and biological activities of chitosan oligosaccharides (COS): a review. Carbohydr Polym. 2005;62:357–368. doi: 10.1016/j.carbpol.2005.08.012. [DOI] [Google Scholar]
- 21.Riegger BR, Bäurer B, Mirzayeva A, Tovar GE, Bach M. A systematic approach of chitosan nanoparticle preparation via emulsion crosslinking as potential adsorbent in wastewater treatment. Carbohydr Polym. 2018;180:46–54. doi: 10.1016/j.carbpol.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Meraz OV (2017) Synthesis and characterization of chitosan composites reinforced with carbon nanostructures
- 23.Gavhane Y, Gurav A, Yadav A. Chitosan and its applications: a review of literature. Int J Biomed Pharm Sci. 2013;4:312–331. [Google Scholar]
- 24.Sahoo R, Sahoo S, Nayak PL (2013) Synthesis and characterization of gelatin–chitosan nanocomposite to explore the possible use as drug delivery vehicle. Eur Sci J (ESJ) 9(18)
- 25.Park JK, Chung MJ, Choi HN, Park YI. Effects of the molecular weight and the degree of deacetylation of chitosan oligosaccharides on antitumor activity. Int J Mol Sci. 2011;12:266–277. doi: 10.3390/ijms12010266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naqvi S, Moerschbacher BM. The cell factory approach toward biotechnological production of high-value chitosan oligomers and their derivatives: an update. Crit Rev Biotechnol. 2017;37:11–25. doi: 10.3109/07388551.2015.1104289. [DOI] [PubMed] [Google Scholar]
- 27.He X, Li K, Xing R, Liu S, Hu L, Li P. The production of fully deacetylated chitosan by compression method. Egypt J Aquat Res. 2016;42:75–81. doi: 10.1016/j.ejar.2015.09.003. [DOI] [Google Scholar]
- 28.Wu T (2004). Production and characterization of fungal chitin and chitosan
- 29.Wang J, Jiang J-Z, Chen W, Bai Z-W. Data of 1H/13C NMR spectra and degree of substitution for chitosan alkyl urea. Data Brief. 2016;7:1228–1236. doi: 10.1016/j.dib.2016.03.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nwe N, Furuike T, Tamura H. The mechanical and biological properties of chitosan scaffolds for tissue regeneration templates are significantly enhanced by chitosan from Gongronella butleri. Materials. 2009;2:374–398. doi: 10.3390/ma2020374. [DOI] [Google Scholar]
- 31.Gholipourmalekabadi M, Zhao S, Harrison BS, Mozafari M, Seifalian AM. Oxygen-generating biomaterials: a new, viable paradigm for tissue engineering? Trends Biotechnol. 2016;34:1010–1021. doi: 10.1016/j.tibtech.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Amaral I, Sampaio P, Barbosa M. Three-dimensional culture of human osteoblastic cells in chitosan sponges: the effect of the degree of acetylation. J Biomed Mater Res Part A. 2006;76:335–346. doi: 10.1002/jbm.a.30522. [DOI] [PubMed] [Google Scholar]
- 33.Chatelet C, Damour O, Domard A. Influence of the degree of acetylation on some biological properties of chitosan films. Biomaterials. 2001;22:261–268. doi: 10.1016/S0142-9612(00)00183-6. [DOI] [PubMed] [Google Scholar]
- 34.Chupa JM, Foster AM, Sumner SR, Madihally SV, Matthew HW. Vascular cell responses to polysaccharide materials: in vitro and in vivo evaluations. Biomaterials. 2000;21:2315–2322. doi: 10.1016/S0142-9612(00)00158-7. [DOI] [PubMed] [Google Scholar]
- 35.Dhiman HK, Ray AR, Panda AK. Characterization and evaluation of chitosan matrix for in vitro growth of MCF-7 breast cancer cell lines. Biomaterials. 2004;25:5147–5154. doi: 10.1016/j.biomaterials.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 36.Thein-Han WW, Kitiyanant Y. Chitosan scaffolds for in vitro buffalo embryonic stem-like cell culture: an approach to tissue engineering. J Biomed Mater Res B Appl Biomater. 2007;80:92–101. doi: 10.1002/jbm.b.30573. [DOI] [PubMed] [Google Scholar]
- 37.Helander I, Nurmiaho-Lassila E-L, Ahvenainen R, Rhoades J, Roller S. Chitosan disrupts the barrier properties of the outer membrane of Gram-negative bacteria. Int J Food Microbiol. 2001;71:235–244. doi: 10.1016/S0168-1605(01)00609-2. [DOI] [PubMed] [Google Scholar]
- 38.Croisier F, Jérôme C. Chitosan-based biomaterials for tissue engineering. Eur Polym J. 2013;49:780–792. doi: 10.1016/j.eurpolymj.2012.12.009. [DOI] [Google Scholar]
- 39.Muzzarelli R. Human enzymatic activities related to the therapeutic administration of chitin derivatives. Cell Mol Life Sci. 1997;53:131–140. doi: 10.1007/PL00000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tomihata K, Ikada Y. In vitro and in vivo degradation of films of chitin and its deacetylated derivatives. Biomaterials. 1997;18:567–575. doi: 10.1016/S0142-9612(96)00167-6. [DOI] [PubMed] [Google Scholar]
- 41.Prusty A, Gupta BK. Role of chitosan and eudragit in polymer-based extended release matrix tablets—a review. Int J Pharm Sci Res. 2017;8:4973–4982. [Google Scholar]
- 42.Li Q, Dunn E, Grandmaison E, Goosen MF. Applications and properties of chitosan. J Bioact Compat Polym. 1992;7:370–397. doi: 10.1177/088391159200700406. [DOI] [Google Scholar]
- 43.Singh DK, Ray AR. Biomedical applications of chitin, chitosan, and their derivatives. J Macromol Sci Part C Polym Rev. 2000;40:69–83. doi: 10.1081/MC-100100579. [DOI] [Google Scholar]
- 44.Schatz C, Viton C, Delair T, Pichot C, Domard A. Typical physicochemical behaviors of chitosan in aqueous solution. Biomacromolecules. 2003;4:641–648. doi: 10.1021/bm025724c. [DOI] [PubMed] [Google Scholar]
- 45.Lopez-Leon T, Carvalho EL, Seijo B, Ortega-Vinuesa JL, Bastos-Gonzalez D. Physicochemical characterization of chitosan nanoparticles: electrokinetic and stability behavior. J Colloid Interface Sci. 2005;283:344–351. doi: 10.1016/j.jcis.2004.08.186. [DOI] [PubMed] [Google Scholar]
- 46.Mazancová P, Némethová V, Treľová D, Kleščíková L, Lacík I, Rázga FJCP. Dissociation of chitosan/tripolyphosphate complexes into separate components upon pH elevation. Polymers. 2018;192:104–110. doi: 10.1016/j.carbpol.2018.03.030. [DOI] [PubMed] [Google Scholar]
- 47.Cruz-Filho AMD, Bordin ARDV, Souza-Flamini LE, Guedes DFDC, Saquy PC, Silva RG, Pécora JDJ. Analysis of the shelf life of chitosan stored in different types of packaging, using colorimetry and dentin microhardness. Restor Dentis Endod. 2017;42:87–94. doi: 10.5395/rde.2017.42.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ali A, Ahmed SJ. A review on chitosan and its nanocomposites in drug delivery. Int J Biol Macromol. 2018;109:273–286. doi: 10.1016/j.ijbiomac.2017.12.078. [DOI] [PubMed] [Google Scholar]
- 49.Bernkop-Schnürch A, Dünnhaupt SJ. Chitosan-based drug delivery systems. Eur J Pharm Biopharm. 2012;81:463–469. doi: 10.1016/j.ejpb.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 50.Rampino A, Borgogna M, Blasi P, Bellich B, Cesàro AJ. Chitosan nanoparticles: preparation, size evolution and stability. Int J Pharm. 2013;455:219–228. doi: 10.1016/j.ijpharm.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 51.Salatin S, Yari Khosroushahi AJ. Overviews on the cellular uptake mechanism of polysaccharide colloidal nanoparticles. J Cell Mol Med. 2017;21:1668–1686. doi: 10.1111/jcmm.13110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khalili AA, Ahmad MR. A review of cell adhesion studies for biomedical and biological applications. Int J Mol Sci. 2015;16:18149–18184. doi: 10.3390/ijms160818149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bernkop-Schnürch A, Guggi D, Pinter Y. Thiolated chitosans: development and in vitro evaluation of a mucoadhesive, permeation enhancing oral drug delivery system. J Control Release. 2004;94:177–186. doi: 10.1016/j.jconrel.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 54.Bravo-Osuna I, Vauthier C, Farabollini A, Palmieri GF, Ponchel G. Mucoadhesion mechanism of chitosan and thiolated chitosan-poly (isobutyl cyanoacrylate) core-shell nanoparticles. Biomaterials. 2007;28:2233–2243. doi: 10.1016/j.biomaterials.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 55.Patel V, Prajapati B, Patel M. Design and characterization of chitosan-containing mucoadhesive buccal patches of propranolol hydrochloride. Acta Pharm. 2007;57:61–72. doi: 10.2478/v10007-007-0005-9. [DOI] [PubMed] [Google Scholar]
- 56.Li Z, Zhang M. Chitosan-alginate as scaffolding material for cartilage tissue engineering. J Biomed Mater Res Part A. 2005;75:485–493. doi: 10.1002/jbm.a.30449. [DOI] [PubMed] [Google Scholar]
- 57.Cui YL, Di Qi A, Liu WG, Wang XH, Wang H, Ma DM, De Yao K. Biomimetic surface modification of poly (l-lactic acid) with chitosan and its effects on articular chondrocytes in vitro. Biomaterials. 2003;24:3859–3868. doi: 10.1016/S0142-9612(03)00209-6. [DOI] [PubMed] [Google Scholar]
- 58.Patrulea V, Ostafe V, Borchard G, Jordan O. Chitosan as a starting material for wound healing applications. Eur J Pharm Biopharm. 2015;97:417–426. doi: 10.1016/j.ejpb.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 59.Gholipourmalekabadi M et al (2018) 3D protein-based bilayer artificial skin for the guided scarless healing of third-degree burn wounds in vivo. Biomacromolecules [DOI] [PubMed]
- 60.Branco A, Saraswathibhatla A, Notbohm J, Thibeault S. Migration and contraction of fibroblasts from normal and scar vocal folds with applications to wound healing. Biophys J. 2018;114:517a. doi: 10.1016/j.bpj.2017.11.2824. [DOI] [Google Scholar]
- 61.Behera SS, Das U, Kumar A, Bissoyi A, Singh AK. Chitosan/TiO2 composite membrane improves proliferation and survival of L929 fibroblast cells: application in wound dressing and skin regeneration. Int J Biol Macromol. 2017;98:329–340. doi: 10.1016/j.ijbiomac.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 62.Patrulea V, Hirt-Burri N, Jeannerat A, Applegate L, Ostafe V, Jordan O, Borchard G. Peptide-decorated chitosan derivatives enhance fibroblast adhesion and proliferation in wound healing. Carbohydr Polym. 2016;142:114–123. doi: 10.1016/j.carbpol.2016.01.045. [DOI] [PubMed] [Google Scholar]
- 63.Howling GI, Dettmar PW, Goddard PA, Hampson FC, Dornish M, Wood EJ. The effect of chitin and chitosan on the proliferation of human skin fibroblasts and keratinocytes in vitro. Biomaterials. 2001;22:2959–2966. doi: 10.1016/S0142-9612(01)00042-4. [DOI] [PubMed] [Google Scholar]
- 64.Okamoto Y, Watanabe M, Miyatake K, Morimoto M, Shigemasa Y, Minami S. Effects of chitin/chitosan and their oligomers/monomers on migrations of fibroblasts and vascular endothelium. Biomaterials. 2002;23:1975–1979. doi: 10.1016/S0142-9612(01)00324-6. [DOI] [PubMed] [Google Scholar]
- 65.Goy RC, Britto DD, Assis OB. A review of the antimicrobial activity of chitosan. Polímeros. 2009;19:241–247. doi: 10.1590/S0104-14282009000300013. [DOI] [Google Scholar]
- 66.Li B, Shan C, Ge M, Wang L, Fang Y, Wang Y, Xie G, Sun G. Antibacterial mechanism of chitosan and its applications in protection of plant from bacterial disease: mini review. Asian J Chem. 2013;25:10033. doi: 10.14233/ajchem.2013.15217. [DOI] [Google Scholar]
- 67.Han Y, Zhao L, Yu Z, Feng J, Yu QJ. Role of mannose receptor in oligochitosan-mediated stimulation of macrophage function. Int Immunopharmacol. 2005;5:1533–1542. doi: 10.1016/j.intimp.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 68.Otterlei M, Vårum KM, Ryan L, Espevik T. Characterization of binding and TNF-α-inducing ability of chitosans on monocytes: the involvement of CD14. Vaccine. 1994;12:825–832. doi: 10.1016/0264-410X(94)90292-5. [DOI] [PubMed] [Google Scholar]
- 69.Wu GJ, Tsai GJ. Chitooligosaccharides in combination with interferon-γ increase nitric oxide production via nuclear factor-κB activation in murine RAW264.7 macrophages. Food Chem Toxicol. 2007;45:250–258. doi: 10.1016/j.fct.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 70.Bueter CL, Lee CK, Rathinam VA, Healy GJ, Taron CH, Specht CA, Levitz SMJ. Chitosan but not chitin activates the inflammasome by a mechanism dependent upon phagocytosis. J Biol Chem. 2011;286:35447–35455. doi: 10.1074/jbc.M111.274936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuan Z-X, Zhang Z-R, Zhu D, Sun X, Gong T, Liu J, Luan C-T. Specific renal uptake of randomly 50% N-acetylated low molecular weight chitosan. Mol Pharm. 2008;6:305–314. doi: 10.1021/mp800078a. [DOI] [PubMed] [Google Scholar]
- 72.Huang M, Khor E, Lim LY. Uptake and cytotoxicity of chitosan molecules and nanoparticles: effects of molecular weight and degree of deacetylation. Pharm Res. 2004;21:344–353. doi: 10.1023/B:PHAM.0000016249.52831.a5. [DOI] [PubMed] [Google Scholar]
- 73.Behzadi S, et al. Cellular uptake of nanoparticles: journey inside the cell. Chem Soc Rev. 2017;46:4218–4244. doi: 10.1039/C6CS00636A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jia L, Gao X, Wang Y, Yao N, Zhang X. Structural, phenotypic and functional maturation of bone marrow dendritic cells (BMDCs) induced by chitosan (CTS) Biologicals. 2014;42:334–338. doi: 10.1016/j.biologicals.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 75.Mori A, et al. The vaccine adjuvant alum inhibits IL-12 by promoting PI3 kinase signaling while chitosan does not inhibit IL-12 and enhances Th1 and Th17 responses. Eur J Immunol. 2012;42:2709–2719. doi: 10.1002/eji.201242372. [DOI] [PubMed] [Google Scholar]
- 76.Deog-Yong L, Jeong-Hee H, Han-Sang Y. Chitosan and d-glucosamine induce expression of Th1 cytokine genes in porcine spleen cells. J Vet Med Sci. 2002;64:645–648. doi: 10.1292/jvms.64.645. [DOI] [PubMed] [Google Scholar]
- 77.Wen Z-S, Xu Y-L, Zou X-T, Xu Z-R. Chitosan nanoparticles act as an adjuvant to promote both Th1 and Th2 immune responses induced by ovalbumin in mice. Mar Drugs. 2011;9:1038–1055. doi: 10.3390/md9061038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gong Y, et al. Chitosan as an adjuvant for a Helicobacter pylori therapeutic vaccine. Mol Med Rep. 2015;12:4123–4132. doi: 10.3892/mmr.2015.3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Feng X, et al. 3D porous chitosan scaffolds suit survival and neural differentiation of dental pulp stem cells. Cell Mol Neurobiol. 2014;34:859–870. doi: 10.1007/s10571-014-0063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bof MJ, Bordagaray VC, Locaso DE, García MA. Chitosan molecular weight effect on starch-composite film properties. Food Hydrocolloids. 2015;51:281–294. doi: 10.1016/j.foodhyd.2015.05.018. [DOI] [Google Scholar]
- 81.Dou Y, Sun X, Guo G, Dong J, Lu M, Zhang W (2016). Electrospun pure chitosan nanofibrous mats with high structural stability for dura mater regeneration. Front Bioeng Biotechnol
- 82.Kumar PS, Praveen G, Raj M, Chennazhi K, Jayakumar R. Flexible, micro-porous chitosan–gelatin hydrogel/nanofibrin composite bandages for treating burn wounds. RSC Adv. 2014;4:65081–65087. doi: 10.1039/C4RA11969J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chakrabarti A, Talukdar D, Pal A, Ray M. Immunomodulation of macrophages by methylglyoxal conjugated with chitosan nanoparticles against Sarcoma-180 tumor in mice. Cell Immunol. 2014;287:27–35. doi: 10.1016/j.cellimm.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 84.Valmikinathan CM, Mukhatyar VJ, Jain A, Karumbaiah L, Dasari M, Bellamkonda RV. Photocrosslinkable chitosan based hydrogels for neural tissue engineering. Soft Matter. 2012;8:1964–1976. doi: 10.1039/C1SM06629C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Park CJ, Gabrielson NP, Pack DW, Jamison RD, Johnson AJW. The effect of chitosan on the migration of neutrophil-like HL60 cells, mediated by IL-8. Biomaterials. 2009;30:436–444. doi: 10.1016/j.biomaterials.2008.09.060. [DOI] [PubMed] [Google Scholar]
- 86.Simard P, Galarneau H, Marois S, Rusu D, Hoemann CD, Poubelle PE, El-Gabalawy H, Fernandes MJ. Neutrophils exhibit distinct phenotypes toward chitosans with different degrees of deacetylation: implications for cartilage repair. Arthritis Res Ther. 2009;11:R74. doi: 10.1186/ar2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li H, Shi B, Yan S, Zhao T, Li J, Guo X. Effects of chitosan on the secretion of cytokines and expression of inducible nitric oxide synthase mRNA in peritoneal macrophages of broiler chicken. Braz Arch Biol Technol. 2014;57:466–471. doi: 10.1590/S1516-8913201401903. [DOI] [Google Scholar]
- 88.Xia Z, Triffitt JT. A review on macrophage responses to biomaterials. Biomed Mater. 2006;1:R1. doi: 10.1088/1748-6041/1/1/R01. [DOI] [PubMed] [Google Scholar]
- 89.Da Silva CA, Hartl D, Liu W, Lee CG, Elias JA. TLR-2 and IL-17A in chitin-induced macrophage activation and acute inflammation. J Immunol. 2008;181:4279–4286. doi: 10.4049/jimmunol.181.6.4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhang P, Liu W, Peng Y, Han B, Yang Y. Toll like receptor 4 (TLR4) mediates the stimulating activities of chitosan oligosaccharide on macrophages. Int Immunopharmacol. 2014;23:254–261. doi: 10.1016/j.intimp.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 91.Zhu J, Zhang Y, Wu G, Xiao Z, Zhou H, Yu X. Inhibitory effects of oligochitosan on TNF-α, IL-1β and nitric oxide production in lipopolysaccharide-induced RAW264.7 cells. Mol Med Rep. 2015;11:729–733. doi: 10.3892/mmr.2014.2643. [DOI] [PubMed] [Google Scholar]
- 92.Wernersson S, Pejler G. Mast cell secretory granules: armed for battle. Nat Rev Immunol. 2014;14:478–494. doi: 10.1038/nri3690. [DOI] [PubMed] [Google Scholar]
- 93.Amin K. The role of mast cells in allergic inflammation. Respir Med. 2012;106:9–14. doi: 10.1016/j.rmed.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 94.Vo T-S, Kim J-A, Ngo D-H, Kong C-S, Kim S-K. Protective effect of chitosan oligosaccharides against FcɛRI-mediated RBL-2H3 mast cell activation. Process Biochem. 2012;47:327–330. doi: 10.1016/j.procbio.2011.10.036. [DOI] [Google Scholar]
- 95.Farrugia BL, Whitelock JM, Jung M, McGrath B, O’Grady RL, McCarthy SJ, Lord MS. The localisation of inflammatory cells and expression of associated proteoglycans in response to implanted chitosan. Biomaterials. 2014;35:1462–1477. doi: 10.1016/j.biomaterials.2013.10.068. [DOI] [PubMed] [Google Scholar]
- 96.Younes I, Frachet V, Rinaudo M, Jellouli K, Nasri M. Cytotoxicity of chitosans with different acetylation degrees and molecular weights on bladder carcinoma cells. Int J Biol Macromol. 2016;84:200–207. doi: 10.1016/j.ijbiomac.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 97.Zou P, Yang X, Zhang Y, Du P, Yuan S, Yang D, Wang J. Antitumor effects of orally and intraperitoneally administered chitosan oligosaccharides (COSs) on S180-bearing/residual mouse. J Food Sci. 2016;81:H3035–H3042. doi: 10.1111/1750-3841.13538. [DOI] [PubMed] [Google Scholar]
- 98.Wimardhani YS, Suniarti DF, Freisleben HJ, Wanandi SI, Siregar NC, Ikeda M-A. Chitosan exerts anticancer activity through induction of apoptosis and cell cycle arrest in oral cancer cells. J Oral Sci. 2014;56:119–126. doi: 10.2334/josnusd.56.119. [DOI] [PubMed] [Google Scholar]
- 99.Zhang J, Xia W, Liu P, Cheng Q, Tahi T, Gu W, Li B. Chitosan modification and pharmaceutical/biomedical applications. Mar Drugs. 2010;8:1962–1987. doi: 10.3390/md8071962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wiegand C, Winter D, Hipler U-C. Molecular-weight-dependent toxic effects of chitosans on the human keratinocyte cell line HaCaT. Skin Pharmacol Physiol. 2010;23:164–170. doi: 10.1159/000276996. [DOI] [PubMed] [Google Scholar]
- 101.Senturk S, Mumcuoglu M, Gursoy-Yuzugullu O, Cingoz B, Akcali KC, Ozturk M. Transforming growth factor-beta induces senescence in hepatocellular carcinoma cells and inhibits tumor growth. Hepatology. 2010;52:966–974. doi: 10.1002/hep.23769. [DOI] [PubMed] [Google Scholar]
- 102.Mandel A, Larsson P, Sarwar M, Semenas J, Khaja ASS, Persson JL. The interplay between AR, EGF receptor and MMP-9 signaling pathways in invasive prostate cancer. Mol Med. 2018;24:34. doi: 10.1186/s10020-018-0035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shen K-T, Chen M-H, Chan H-Y, Jeng J-H, Wang Y-J. Inhibitory effects of chitooligosaccharides on tumor growth and metastasis. Food Chem Toxicol. 2009;47:1864–1871. doi: 10.1016/j.fct.2009.04.044. [DOI] [PubMed] [Google Scholar]
- 104.Masuda S, et al. Anti-tumor properties of orally administered glucosamine and N-acetyl-d-glucosamine oligomers in a mouse model. Carbohydr Polym. 2014;111:783–787. doi: 10.1016/j.carbpol.2014.04.102. [DOI] [PubMed] [Google Scholar]
- 105.Azuma K, Osaki T, Minami S, Okamoto Y. Anticancer and anti-inflammatory properties of chitin and chitosan oligosaccharides. J Funct Biomater. 2015;6:33–49. doi: 10.3390/jfb6010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chou T-C, Fu E, Wu C-J, Yeh J-H. Chitosan enhances platelet adhesion and aggregation. Biochem Biophys Res Commun. 2003;302:480–483. doi: 10.1016/S0006-291X(03)00173-6. [DOI] [PubMed] [Google Scholar]
- 107.Lord MS, Cheng B, McCarthy SJ, Jung M, Whitelock JM. The modulation of platelet adhesion and activation by chitosan through plasma and extracellular matrix proteins. Biomaterials. 2011;32:6655–6662. doi: 10.1016/j.biomaterials.2011.05.062. [DOI] [PubMed] [Google Scholar]
- 108.Shen E-C, Chou TC, Gau CH, Tu HP, Chen YT, Fu E. Releasing growth factors from activated human platelets after chitosan stimulation: a possible bio-material for platelet-rich plasma preparation. Clin Oral Implant Res. 2006;17:572–578. doi: 10.1111/j.1600-0501.2004.01241.x. [DOI] [PubMed] [Google Scholar]
- 109.Periayah MH, Halim AS, Saad AZM, Yaacob NS, Hussein AR, Karim FA, Rashid AHA, Ujang Z. Chitosan scaffold enhances growth factor release in wound healing in von Willebrand disease. Int J Clin Exp Med. 2015;8:15611. [PMC free article] [PubMed] [Google Scholar]
- 110.Busilacchi A, Gigante A, Mattioli-Belmonte M, Manzotti S, Muzzarelli RA. Chitosan stabilizes platelet growth factors and modulates stem cell differentiation toward tissue regeneration. Carbohydr Polym. 2013;98:665–676. doi: 10.1016/j.carbpol.2013.06.044. [DOI] [PubMed] [Google Scholar]
- 111.Okamoto Y, Yano R, Miyatake K, Tomohiro I, Shigemasa Y, Minami S. Effects of chitin and chitosan on blood coagulation. Carbohydr Polym. 2003;53:337–342. doi: 10.1016/S0144-8617(03)00076-6. [DOI] [Google Scholar]
- 112.Hao C, Gao L, Zhang Y, Wang W, Yu G, Guan H, Zhang L, Li C. Acetylated chitosan oligosaccharides act as antagonists against glutamate-induced PC12 cell death via Bcl-2/Bax signal pathway. Mar Drugs. 2015;13:1267–1289. doi: 10.3390/md13031267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Urquhart DM, Soufan C, Teichtahl AJ, Wluka AE, Hanna F, Cicuttini FM. Factors that may mediate the relationship between physical activity and the risk for developing knee osteoarthritis. Arthritis Res Ther. 2008;10:203. doi: 10.1186/ar2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Daheshia M, Yao JQ. The interleukin 1β pathway in the pathogenesis of osteoarthritis. J Rheumatol. 2008;35:2306–2312. doi: 10.3899/jrheum.080346. [DOI] [PubMed] [Google Scholar]
- 115.Lin Z, Willers C, Xu J, Zheng M-H. The chondrocyte: biology and clinical application. Tissue Eng. 2006;12:1971–1984. doi: 10.1089/ten.2006.12.1971. [DOI] [PubMed] [Google Scholar]
- 116.Chen Q, Liu S-Q, Du Y-M, Peng H, Sun L-P. Carboxymethyl-chitosan protects rabbit chondrocytes from interleukin-1β-induced apoptosis. Eur J Pharmacol. 2006;541:1–8. doi: 10.1016/j.ejphar.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 117.Zhang C, Yu L, Zhou Y, Zhao Q, Liu S-Q. Chitosan oligosaccharides inhibit IL-1β-induced chondrocyte apoptosis via the P38 MAPK signaling pathway. Glycoconj J. 2016;33:735–744. doi: 10.1007/s10719-016-9667-1. [DOI] [PubMed] [Google Scholar]
- 118.Weinberg BJ, Fermor B, Guilak F (2007) Nitric oxide synthase and cyclooxygenase interactions in cartilage and meniscus. In: Inflammation in the pathogenesis of chronic diseases, pp 31–62. Springer, New York [DOI] [PubMed]
- 119.de Andrés MC, Maneiro E, Martín MA, Arenas J, Blanco FJ. Nitric oxide compounds have different effects profiles on human articular chondrocyte metabolism. Arthritis Res Ther. 2013;15:R115. doi: 10.1186/ar4295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhou PH, Liu SQ, Peng H. The effect of hyaluronic acid on IL-1β-induced chondrocyte apoptosis in a rat model of osteoarthritis. J Orthop Res. 2008;26:1643–1648. doi: 10.1002/jor.20683. [DOI] [PubMed] [Google Scholar]
- 121.Menon MB, et al. p38 MAPK/MK2-dependent phosphorylation controls cytotoxic RIPK1 signalling in inflammation and infection. Nat Cell Biol. 2017;19:1248. doi: 10.1038/ncb3614. [DOI] [PubMed] [Google Scholar]
- 122.Liu C, et al. Novel 1, 4-naphthoquinone derivatives induce apoptosis via ROS-mediated p38/MAPK, Akt and STAT3 signaling in human hepatoma Hep3B cells. Int J Biochem Cell Biol. 2018;96:9–19. doi: 10.1016/j.biocel.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 123.Lu JX, Prudhommeaux F, Meunier A, Sedel L, Guillemin G. Effects of chitosan on rat knee cartilages. Biomaterials. 1999;20:1937–1944. doi: 10.1016/S0142-9612(99)00164-7. [DOI] [PubMed] [Google Scholar]
- 124.Tan ML, et al. The potential role of free chitosan in bone trauma and bone cancer management. Biomaterials. 2014;35:7828–7838. doi: 10.1016/j.biomaterials.2014.05.087. [DOI] [PubMed] [Google Scholar]
- 125.Shao P, Wei Y, Dass CR, Zhang G, Wu Z. Systemic delivery of free chitosan accelerates femur fracture healing in rats. Curr Drug Targets. 2018;19:460–466. doi: 10.2174/1389450115666141010150255. [DOI] [PubMed] [Google Scholar]
- 126.Dhivya S, Keshav Narayan A, Logith Kumar R, Viji Chandran S, Vairamani M, Selvamurugan N. Proliferation and differentiation of mesenchymal stem cells on scaffolds containing chitosan, calcium polyphosphate and pigeonite for bone tissue engineering. Cell Prolif. 2018;51:e12408. doi: 10.1111/cpr.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bhowmick A, Banerjee SL, Pramanik N, Jana P, Mitra T, Gnanamani A, Das M, Kundu PP. Organically modified clay supported chitosan/hydroxyapatite–zinc oxide nanocomposites with enhanced mechanical and biological properties for the application in bone tissue engineering. Int J Biol Macromol. 2018;106:11–19. doi: 10.1016/j.ijbiomac.2017.07.168. [DOI] [PubMed] [Google Scholar]
- 128.Qiu J, Liu L, Chen B, Qiao Y, Cao H, Zhu H, Liu X. Graphene oxide as a dual Zn/Mg ion carrier and release platform: enhanced osteogenic activity and antibacterial properties. J Mater Chem B. 2018;6:2004–2012. doi: 10.1039/C8TB00162F. [DOI] [PubMed] [Google Scholar]
- 129.Rutkovskiy A, Stensløkken K-O, Vaage IJ. Osteoblast differentiation at a glance. Med Sci Monit Basic Res. 2016;22:95. doi: 10.12659/MSMBR.901142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jafary F, Hanachi P, Gorjipour K. Osteoblast differentiation on collagen scaffold with immobilized alkaline phosphatase. Int J Organ Transplant Med. 2017;8:195. [PMC free article] [PubMed] [Google Scholar]
- 131.Ohara N, Hayashi Y, Yamada S, Kim S-K, Matsunaga T, Yanagiguchi K, Ikeda T. Early gene expression analyzed by cDNA microarray and RT-PCR in osteoblasts cultured with water-soluble and low molecular chitooligosaccharide. Biomaterials. 2004;25:1749–1754. doi: 10.1016/j.biomaterials.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 132.Lu Z, Roohani-Esfahani S-I, Li J, Zreiqat H. Synergistic effect of nanomaterials and BMP-2 signalling in inducing osteogenic differentiation of adipose tissue-derived mesenchymal stem cells. Nanomed Nanotechnol Biol Med. 2015;11:219–228. doi: 10.1016/j.nano.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 133.Komori T. Signaling networks in RUNX2-dependent bone development. J Cell Biochem. 2011;112:750–755. doi: 10.1002/jcb.22994. [DOI] [PubMed] [Google Scholar]
- 134.Hawse JR, Subramaniam M, Ingle JN, Oursler MJ, Rajamannan N, Spelsberg TC. Estrogen-TGFβ cross-talk in bone and other cell types: role of TIEG, Runx2, and other transcription factors. J Cell Biochem. 2008;103:383–392. doi: 10.1002/jcb.21425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wohl GR, Towler DA, Silva MJ. Stress fracture healing: fatigue loading of the rat ulna induces upregulation in expression of osteogenic and angiogenic genes that mimic the intramembranous portion of fracture repair. Bone. 2009;44:320–330. doi: 10.1016/j.bone.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ho WP, Chan WP, Hsieh MS, Chen RM. Runx2-mediated bcl-2 gene expression contributes to nitric oxide protection against hydrogen peroxide-induced osteoblast apoptosis. J Cell Biochem. 2009;108:1084–1093. doi: 10.1002/jcb.22338. [DOI] [PubMed] [Google Scholar]
- 137.Ho M-H, Liao M-H, Lin Y-L, Lai C-H, Lin P-I, Chen R-M. Improving effects of chitosan nanofiber scaffolds on osteoblast proliferation and maturation. Int J Nanomed. 2014;9:4293. doi: 10.2147/IJN.S68012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ho M-H, Yao C-J, Liao M-H, Lin P-I, Liu S-H, Chen R-M. Chitosan nanofiber scaffold improves bone healing via stimulating trabecular bone production due to upregulation of the Runx2/osteocalcin/alkaline phosphatase signaling pathway. Int J Nanomed. 2015;10:5941. doi: 10.2147/IJN.S90669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mendis E, Kim M-M, Rajapakse N, Kim S-K. An in vitro cellular analysis of the radical scavenging efficacy of chitooligosaccharides. Life Sci. 2007;80:2118–2127. doi: 10.1016/j.lfs.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 140.Liu H-T, Li W-M, Xu G, Li X-Y, Bai X-F, Wei P, Yu C, Du Y-G. Chitosan oligosaccharides attenuate hydrogen peroxide-induced stress injury in human umbilical vein endothelial cells. Pharmacol Res. 2009;59:167–175. doi: 10.1016/j.phrs.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 141.Panieri E, Santoro M. ROS homeostasis and metabolism: a dangerous liason in cancer cells. Cell Death Dis. 2016;7:e2253. doi: 10.1038/cddis.2016.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Khodagholi F, Eftekharzadeh B, Maghsoudi N, Rezaei PF. Chitosan prevents oxidative stress-induced amyloid β formation and cytotoxicity in NT2 neurons: involvement of transcription factors Nrf2 and NF-κB. Mol Cell Biochem. 2010;337:39–51. doi: 10.1007/s11010-009-0284-1. [DOI] [PubMed] [Google Scholar]
- 143.Ryu B, Himaya S, Napitupulu RJ, Eom T-K, Kim S-K. Sulfated chitooligosaccharide II (SCOS II) suppress collagen degradation in TNF-induced chondrosarcoma cells via NF-κB pathway. Carbohydr Res. 2012;350:55–61. doi: 10.1016/j.carres.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 144.Wei P, Ma P, Xu Q-S, Bai Q-H, Gu J-G, Xi H, Du Y-G, Yu C. Chitosan oligosaccharides suppress production of nitric oxide in lipopolysaccharide-induced N9 murine microglial cells in vitro. Glycoconj J. 2012;29:285–295. doi: 10.1007/s10719-012-9392-3. [DOI] [PubMed] [Google Scholar]
- 145.Fang I-M, Yang C-H, Yang C-M, Chen M-S. Chitosan oligosaccharides attenuates oxidative-stress related retinal degeneration in rats. PLoS ONE. 2013;8:e77323. doi: 10.1371/journal.pone.0077323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jeng PS, Inoue-Yamauchi A, Hsieh JJ, Cheng EH (2018) BH3-dependent and independent activation of BAX and BAK in mitochondrial apoptosis. Curr Opin Physiol [DOI] [PMC free article] [PubMed]
- 147.Fang I-M, Yang C-M, Yang C-H. Chitosan oligosaccharides prevented retinal ischemia and reperfusion injury via reduced oxidative stress and inflammation in rats. Exp Eye Res. 2015;130:38–50. doi: 10.1016/j.exer.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 148.Tan K, Wang X, Zhang J, Zhuang Z, Dong T. Effect of chitosan porous scaffolds combined with bone marrow mesenchymal stem cells in repair of neurological deficit after traumatic brain injury in rats. Chinese J Reparative Reconstr Surg (Zhongguo xiufu chongjian waike zazhi) 2018;32:745–752. doi: 10.7507/1002-1892.201712047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Moattari M, Kouchesfehani HM, Kaka G, Sadraie SH, Naghdi M, Mansouri K. Chitosan-film associated with mesenchymal stem cells enhanced regeneration of peripheral nerves: a rat sciatic nerve model. J Chem Neuroanat. 2018;88:46–54. doi: 10.1016/j.jchemneu.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 150.Damas I, Zuliani C, Moraes A, Westin C, Kharmandayan P, Andrade K, Mamonei R, Coimbra I. Comparision between human amniotic fluid and adipose tissue mesenchymal stem cells induced-chondrogenesis cultured in chitosan-xanthan scaffold stimulated with TGF-β3. Osteoarthr Cartil. 2018;26:S298–S299. doi: 10.1016/j.joca.2018.02.600. [DOI] [Google Scholar]
- 151.Wang A, Ao Q, He Q, Gong X, Gong K, Gong Y, Zhao N, Zhang X. Neural stem cell affinity of chitosan and feasibility of chitosan-based porous conduits as scaffolds for nerve tissue engineering. Tsinghua Sci Technol. 2006;11:415–420. doi: 10.1016/S1007-0214(06)70210-3. [DOI] [Google Scholar]
- 152.Li Z, Tian X, Yuan Y, Song Z, Zhang L, Wang X, Li T. Effect of cell culture using chitosan membranes on stemness marker genes in mesenchymal stem cells. Mol Med Rep. 2013;7:1945–1949. doi: 10.3892/mmr.2013.1423. [DOI] [PubMed] [Google Scholar]
- 153.Liu HT, Li WM, Li XY, Xu QS, Liu QS, Bai XF, Yu C, Du YG. Chitosan oligosaccharides inhibit the expression of interleukin-6 in lipopolysaccharide-induced human umbilical vein endothelial cells through p38 and ERK1/2 protein kinases. Basic Clin Pharmacol Toxicol. 2010;106:362–371. doi: 10.1111/j.1742-7843.2010.00539.x. [DOI] [PubMed] [Google Scholar]
- 154.Segers VF, Lee RT. Stem-cell therapy for cardiac disease. Nature. 2008;451:937–942. doi: 10.1038/nature06800. [DOI] [PubMed] [Google Scholar]
- 155.Liu Z, et al. The influence of chitosan hydrogel on stem cell engraftment, survival and homing in the ischemic myocardial microenvironment. Biomaterials. 2012;33:3093–3106. doi: 10.1016/j.biomaterials.2011.12.044. [DOI] [PubMed] [Google Scholar]
- 156.Yang J, Liu A, Zhou C. Proliferation of mesenchymal stem cell on chitosan films associated with convex micro-topography. J Biomater Sci Polym Ed. 2011;22:919–929. doi: 10.1163/092050610X496396. [DOI] [PubMed] [Google Scholar]
- 157.Ragetly GR, Griffon DJ, Lee H-B, Fredericks LP, Gordon-Evans W, Chung YS. Effect of chitosan scaffold microstructure on mesenchymal stem cell chondrogenesis. Acta Biomater. 2010;6:1430–1436. doi: 10.1016/j.actbio.2009.10.040. [DOI] [PubMed] [Google Scholar]
- 158.Van Bockstaele E, Ross J. SI: Catecholamine dysregulation and neurodegenerative disease catecholamine dysregulation in neurodegenerative disease: from molecular mechanisms to circuit dysfunctioned. New York: Elsevier; 2018. [DOI] [PubMed] [Google Scholar]
- 159.Sweeney MD, Sagare AP, Zlokovic BV. Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol. 2018;14:133. doi: 10.1038/nrneurol.2017.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hao C, Wang W, Wang S, Zhang L, Guo Y. An overview of the protective effects of chitosan and acetylated chitosan oligosaccharides against neuronal disorders. Mar Drugs. 2017;15:89. doi: 10.3390/md15040089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Amor S, Peferoen LA, Vogel DY, Breur M, van der Valk P, Baker D, van Noort JM. Inflammation in neurodegenerative diseases—an update. Immunology. 2014;142:151–166. doi: 10.1111/imm.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kimura Y, Shibuya N, Kimura H (2018) Sulfite protects neurons from oxidative stress. Br J Pharmacol [DOI] [PMC free article] [PubMed]
- 163.Im H, Lim J. Oxidative stress caused by accumulation of misfolded Z-type alpha1-antitrypsin. Free Radical Biol Med. 2018;120:S71–S72. doi: 10.1016/j.freeradbiomed.2018.04.237. [DOI] [Google Scholar]
- 164.Chen B, Li J, Borgens RB. Neuroprotection by chitosan nanoparticles in oxidative stress-mediated injury. BMC Res Notes. 2018;11:49. doi: 10.1186/s13104-018-3162-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Xu W, Huang H-C, Lin C-J, Jiang Z-F. Chitooligosaccharides protect rat cortical neurons against copper induced damage by attenuating intracellular level of reactive oxygen species. Bioorg Med Chem Lett. 2010;20:3084–3088. doi: 10.1016/j.bmcl.2010.03.105. [DOI] [PubMed] [Google Scholar]
- 166.Atwood CS, Huang X, Moir RD, Tanzi RE, Bush AI (2018) Role of free radicals and metal ions in the pathogenesis of Alzheimer’s disease. In: Metal ions in biological systems, pp 309–364. Routledge, Abingdon [PubMed]
- 167.Murphy TH, Miyamoto M, Sastre A, Schnaar RL, Coyle JT. Glutamate toxicity in a neuronal cell line involves inhibition of cystine transport leading to oxidative stress. Neuron. 1989;2:1547–1558. doi: 10.1016/0896-6273(89)90043-3. [DOI] [PubMed] [Google Scholar]
- 168.Zhou S, Yang Y, Gu X, Ding F. Chitooligosaccharides protect cultured hippocampal neurons against glutamate-induced neurotoxicity. Neurosci Lett. 2008;444:270–274. doi: 10.1016/j.neulet.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 169.Kim M-S, Sung M-J, Seo S-B, Yoo S-J, Lim W-K, Kim H-M. Water-soluble chitosan inhibits the production of pro-inflammatory cytokine in human astrocytoma cells activated by amyloid β peptide and interleukin-1β. Neurosci Lett. 2002;321:105–109. doi: 10.1016/S0304-3940(02)00066-6. [DOI] [PubMed] [Google Scholar]
- 170.Pangestuti R, Bak S-S, Kim S-K. Attenuation of pro-inflammatory mediators in LPS-stimulated BV2 microglia by chitooligosaccharides via the MAPK signaling pathway. Int J Biol Macromol. 2011;49:599–606. doi: 10.1016/j.ijbiomac.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 171.Verma DK, et al. New therapeutic activity of metabolic enhancer piracetam in treatment of neurodegenerative disease: participation of caspase independent death factors, oxidative stress, inflammatory responses and apoptosis. Biochim Biophys Acta (BBA) Mol Basis Dis. 2018;1864:2078–2096. doi: 10.1016/j.bbadis.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 172.Wang X, Miao J, Yan C, Ge R, Liang T, Liu E, Li Q. Chitosan attenuates dibutyltin-induced apoptosis in PC12 cells through inhibition of the mitochondria-dependent pathway. Carbohydr Polym. 2016;151:996–1005. doi: 10.1016/j.carbpol.2016.06.053. [DOI] [PubMed] [Google Scholar]
- 173.Koo H-N, Jeong H-J, Hong S-H, Choi J-H, An N-H, Kim H-M. High molecular weight water-soluble chitosan protects against apoptosis induced by serum starvation in human astrocytes. J Nutr Biochem. 2002;13:245–249. doi: 10.1016/S0955-2863(01)00218-2. [DOI] [PubMed] [Google Scholar]
- 174.Green DR, Kroemer G. Cytoplasmic functions of the tumour suppressor p53. Nature. 2009;458:1127. doi: 10.1038/nature07986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lim YY, et al. Association of β-amyloid and apolipoprotein E ε4 with memory decline in preclinical Alzheimer disease. JAMA Neurol. 2018;75:488–494. doi: 10.1001/jamaneurol.2017.4325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dai X, Hou W, Sun Y, Gao Z, Zhu S, Jiang Z. Chitosan oligosaccharides inhibit/disaggregate fibrils and attenuate amyloid β-mediated neurotoxicity. Int J Mol Sci. 2015;16:10526–10536. doi: 10.3390/ijms160510526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cao Z, Gilbert RJ, He W. Simple agarose–chitosan gel composite system for enhanced neuronal growth in three dimensions. Biomacromolecules. 2009;10:2954–2959. doi: 10.1021/bm900670n. [DOI] [PubMed] [Google Scholar]
- 178.Blanpain C. Epidermal stem cells. Bull Mem Acad R Med Belg. 2007;162:418. [PubMed] [Google Scholar]
- 179.Chai J, Modak C, Mouazzen W, Narvaez R, Pham J (2010) Epithelial or mesenchymal: where to draw the line? Biosci Trends 4(3) [PubMed]
- 180.Paz AC, Soleas J, Poon JC, Trieu D, Waddell TK, McGuigan AP. Challenges and opportunities for tissue-engineering polarized epithelium. Tissue Eng Part B Rev. 2013;20:56–72. doi: 10.1089/ten.teb.2013.0144. [DOI] [PubMed] [Google Scholar]
- 181.Muanprasat C, Wongkrasant P, Satitsri S, Moonwiriyakit A, Pongkorpsakol P, Mattaveewong T, Pichyangkura R, Chatsudthipong V. Activation of AMPK by chitosan oligosaccharide in intestinal epithelial cells: mechanism of action and potential applications in intestinal disorders. Biochem Pharmacol. 2015;96:225–236. doi: 10.1016/j.bcp.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 182.Hsiao Y-C, Chen C-N, Chen Y-T, Yang T-L. Controlling branching structure formation of the salivary gland by the degree of chitosan deacetylation. Acta Biomater. 2013;9:8214–8223. doi: 10.1016/j.actbio.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 183.Yang T-L, Lin L, Hsiao Y-C, Lee H-W, Young T-H. Chitosan biomaterials induce branching morphogenesis in a model of tissue-engineered glandular organs in serum-free conditions. Tissue Eng Part A. 2012;18:2220–2230. doi: 10.1089/ten.tea.2011.0527. [DOI] [PubMed] [Google Scholar]
- 184.Patil SV, Nanduri LS. Interaction of chitin/chitosan with salivary and other epithelial cells—an overview. Int J Biol Macromol. 2017;104:1398–1406. doi: 10.1016/j.ijbiomac.2017.03.058. [DOI] [PubMed] [Google Scholar]
- 185.Huang TW, Wei CK, Su HW, Fang KM. Chitosan promotes aquaporin formation and inhibits mucociliary differentiation of nasal epithelial cells through increased TGF-β1 production. J Tissue Eng Regen Med. 2017;11:3567–3575. doi: 10.1002/term.2274. [DOI] [PubMed] [Google Scholar]
- 186.Smith J, Wood E, Dornish M. Effect of chitosan on epithelial cell tight junctions. Pharm Res. 2004;21:43–49. doi: 10.1023/B:PHAM.0000012150.60180.e3. [DOI] [PubMed] [Google Scholar]
- 187.Liu SH, Huang YW, Wu CT, Chiu CY, Chiang MT. Low molecular weight chitosan accelerates glucagon-like peptide-1 secretion in human intestinal endocrine cells via a p38-dependent pathway. J Agric Food Chem. 2013;61:4855–4861. doi: 10.1021/jf305410k. [DOI] [PubMed] [Google Scholar]
- 188.Montorfano I, et al. Oxidative stress mediates the conversion of endothelial cells into myofibroblasts via a TGF-β1 and TGF-β2-dependent pathway. Lab Investig. 2014;94:1068. doi: 10.1038/labinvest.2014.100. [DOI] [PubMed] [Google Scholar]
- 189.Förstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circ Res. 2017;120:713–735. doi: 10.1161/CIRCRESAHA.116.309326. [DOI] [PubMed] [Google Scholar]
- 190.Amiya E. Interaction of hyperlipidemia and reactive oxygen species: insights from the lipid-raft platform. World J Cardiol. 2016;8:689. doi: 10.4330/wjc.v8.i12.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Xu H-B, Huang Z-Q. Icariin enhances endothelial nitric-oxide synthase expression on human endothelial cells in vitro. Vasc Pharmacol. 2007;47:18–24. doi: 10.1016/j.vph.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 192.Nam K-S, Kim M-K, Shon Y-H. Inhibition of proinflammatory cytokine-induced invasiveness of HT-29 cells by chitosan oligosaccharide. J Microbiol Biotechnol. 2007;17:2042–2045. [PubMed] [Google Scholar]
- 193.Wang Z, Zheng L, Yang S, Niu R, Chu E, Lin X. N-acetylchitooligosaccharide is a potent angiogenic inhibitor both in vivo and in vitro. Biochem Biophys Res Commun. 2007;357:26–31. doi: 10.1016/j.bbrc.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 194.Liu H-T, Huang P, Ma P, Liu Q-S, Yu C, Du Y-G. Chitosan oligosaccharides suppress LPS-induced IL-8 expression in human umbilical vein endothelial cells through blockade of p38 and Akt protein kinases. Acta Pharmacol Sin. 2011;32:478–486. doi: 10.1038/aps.2011.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li Y, Xu Q, Wei P, Cheng L, Peng Q, Li S, Yin H, Du Y. Chitosan oligosaccharides downregulate the expression of E-selectin and ICAM-1 induced by LPS in endothelial cells by inhibiting MAP kinase signaling. Int J Mol Med. 2014;33:392–400. doi: 10.3892/ijmm.2013.1589. [DOI] [PubMed] [Google Scholar]
- 196.Nam K-S, Shon Y-H. Suppression of metastasis of human breast cancer cells by chitosan oligosaccharides. J Microbiol Biotechnol. 2009;19:629–633. doi: 10.4014/jmb.0805.333. [DOI] [PubMed] [Google Scholar]
- 197.Huang X, Huang X, Jiang X-H, Hu F-Q, Du Y-Z, Zhu Q-F, Jin C-S. In vitro antitumour activity of stearic acid-g-chitosan oligosaccharide polymeric micelles loading podophyllotoxin. J Microencapsul. 2012;29:1–8. doi: 10.3109/02652048.2011.621551. [DOI] [PubMed] [Google Scholar]
- 198.Zong A, et al. Anti-metastatic and anti-angiogenic activities of sulfated polysaccharide of Sepiella maindroni ink. Carbohydr Polym. 2013;91:403–409. doi: 10.1016/j.carbpol.2012.08.050. [DOI] [PubMed] [Google Scholar]
- 199.Zheng M, Han B, Yang Y, Liu W. Synthesis, characterization and biological safety of O-carboxymethyl chitosan used to treat sarcoma 180 tumor. Carbohydr Polym. 2011;86:231–238. doi: 10.1016/j.carbpol.2011.04.038. [DOI] [Google Scholar]
- 200.Hu F, Chen W, Zhao M, Yuan H, Du Y. Effective antitumor gene therapy delivered by polyethylenimine-conjugated stearic acid-g-chitosan oligosaccharide micelles. Gene Ther. 2013;20:597. doi: 10.1038/gt.2012.72. [DOI] [PubMed] [Google Scholar]
- 201.Termsarasab U, Cho H-J, Kim DH, Chong S, Chung S-J, Shim C-K, Moon HT, Kim D-D. Chitosan oligosaccharide-arachidic acid-based nanoparticles for anti-cancer drug delivery. Int J Pharm. 2013;441:373–380. doi: 10.1016/j.ijpharm.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 202.Li TSC, Yawata T, Honke K. Efficient siRNA delivery and tumor accumulation mediated by ionically cross-linked folic acid-poly (ethylene glycol)-chitosan oligosaccharide lactate nanoparticles: for the potential targeted ovarian cancer gene therapy. Eur J Pharm Sci. 2014;52:48–61. doi: 10.1016/j.ejps.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 203.Younes I, Hajji S, Frachet V, Rinaudo M, Jellouli K, Nasri M. Chitin extraction from shrimp shell using enzymatic treatment. Antitumor, antioxidant and antimicrobial activities of chitosan. Int J Biol Macromol. 2014;69:489–498. doi: 10.1016/j.ijbiomac.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 204.Chien R-C, Yen M-T, Mau J-L. Antimicrobial and antitumor activities of chitosan from shiitake stipes, compared to commercial chitosan from crab shells. Carbohydr Polym. 2016;138:259–264. doi: 10.1016/j.carbpol.2015.11.061. [DOI] [PubMed] [Google Scholar]
- 205.Chokradjaroen C, Rujiravanit R, Watthanaphanit A, Theeramunkong S, Saito N, Yamashita K, Arakawa R. Enhanced degradation of chitosan by applying plasma treatment in combination with oxidizing agents for potential use as an anticancer agent. Carbohydr Polym. 2017;167:1–11. doi: 10.1016/j.carbpol.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 206.Srinivasan H, Kanayairam V, Ravichandran R. Chitin and chitosan preparation from shrimp shells Penaeus monodon and its human ovarian cancer cell line, PA-1. Int J Biol Macromol. 2018;107:662–667. doi: 10.1016/j.ijbiomac.2017.09.035. [DOI] [PubMed] [Google Scholar]