Abstract
Reconstruction of through-and-through defects of cheek and commissure resulting from cancer resection are challenging. The specialized function of oral competence that the oral commissure and lip play is difficult to replicate with flap only reconstruction. Static slings play an important role in improving the functional and aesthetic outcome. The asymmetric “y” fascial sling helps in achieving the goals of oral competence along with adequate mouth opening. A total of 10 patients were operated by this technique. The results were satisfactory in terms of functional and aesthetic outcome postsurgery and were maintained 6 months postradiation.
Keywords: asymmetric y sling, oral commissure reconstruction, oral competence
Introduction
Goals of reconstruction of oral commissure after cancer resection are functional and aesthetic. The functional aspect is adequate mouth opening and oral competence. The aesthetic aspect is to match the commissure angle, lip length, and angle elevation to the opposite side. Postoperatively most of the patients require radiation therapy, which further compromises the outcome of the reconstruction. Drooling of saliva from the angle of the mouth is a very undesirable outcome in patients with commissure reconstruction. Static slings 1 2 3 4 have been used in various designs to improve the functional and aesthetic outcome of commissure reconstruction. Striking a balance between oral competence and adequate mouth opening remains a challenge. We present here a novel technique to replicate the function and aesthetics of oral commissure in patients with defects postcancer resection. The design is specifically focused on maintaining stomal size, shape, and oral competence.
Material and Method
We use the fascial sling in the shape of the English letter Y. The oblique limbs of the Y are equivalent to the length to be resected from either lip. The straight limb of the Y is then attached 1 cm inferior to the center of the predetermined commissure points of the Y. The attachment resembles the English letter Y in a small case (y) with the lower limb being shorter by 1 cm than the calculated length as per the defect ( Figs. 1 and 2 ).
Fig. 1.
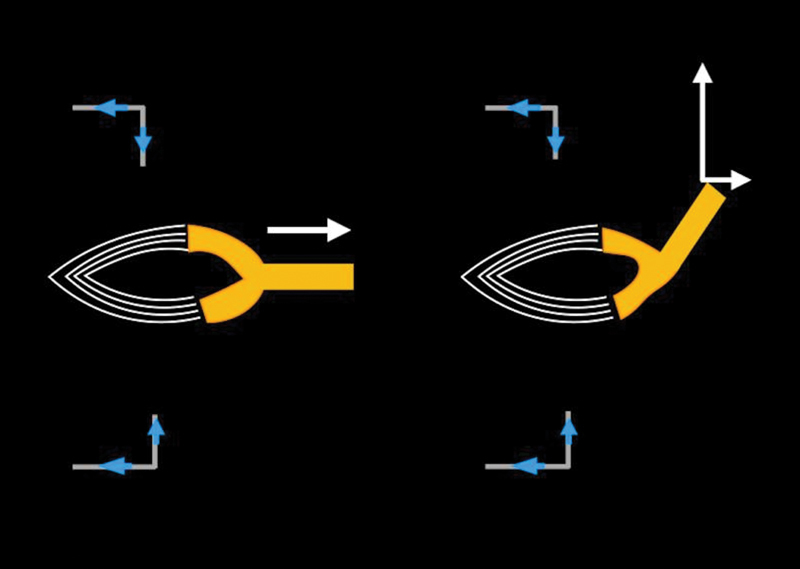
Asymmetric Y design oriented obliquely upward attached to malar prominence traction pull compared with simple y design oriented horizontally.
Fig. 2.
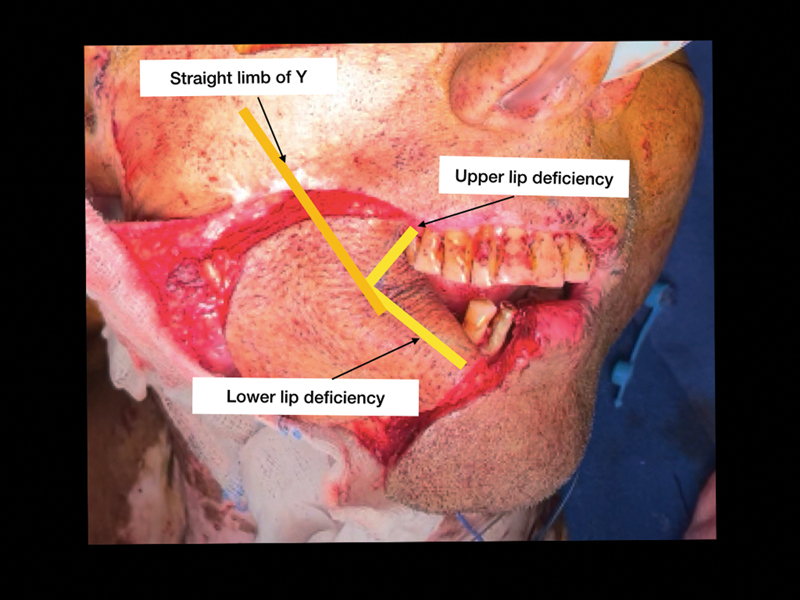
Clinical example of asymmetric Y design.
A sling of adequate size is harvested from the site of flap harvest and placed in the subdermal plane after creating a tunnel with artery forceps ( Fig. 3 ). The length is 1.5 cm more than the total defect of both upper and lower lip defects and 2 cm wide. The sling is split into two, and one slip serves as the straight limb of Y. The extra fascial length is woven into the residual orbicularis muscles of both the upper and the lower lip. Tension adjustment is done by comparison with the opposite commissure and is overcorrected. The straight limb of Y is sutured to the periosteum of the malar bone with nonabsorbable sutures (Prolene 3/0).
Fig. 3.
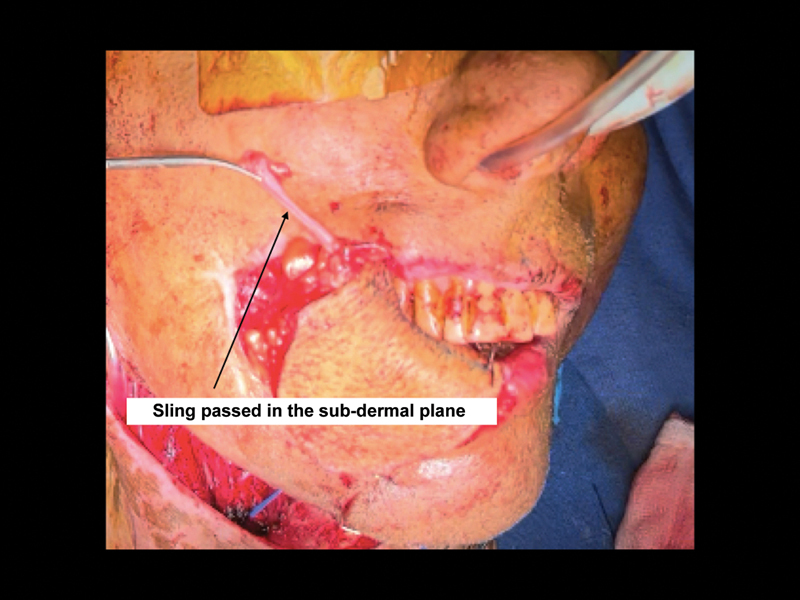
Plane of sling placement (subdermal).
This design of the fascial sling provides adequate support, restores adequate mouth opening, which is maintained postradiation, prevents drooling of saliva, and recreates the angle of the commissure.
Results
A total of 10 patients were managed using this technique. All patients were male in the age group of 47 to 57 years. The defects mostly involved the buccal mucosa, cheek skin, oral commissure, and varying lengths of both upper and lower lips ( Fig. 4 ). Anterolateral thigh (ALT) flap was used for the reconstruction of defect in all the 10 cases. Lip loss in the patients ranged from 20 to 90% of the total lip length (200%). Eight out of ten patients needed postoperative radiotherapy. The outcome was assessed for drooling of saliva, oral competence, and mouth opening. All the patients had good oral competence, occasional drooling of saliva, and adequate mouth opening. The functional outcomes were maintained over 6 months postradiation ( Figs. 5 6 ). None of the patient had any complication related to the use of nonvascularized fascial sling.
Fig. 4.
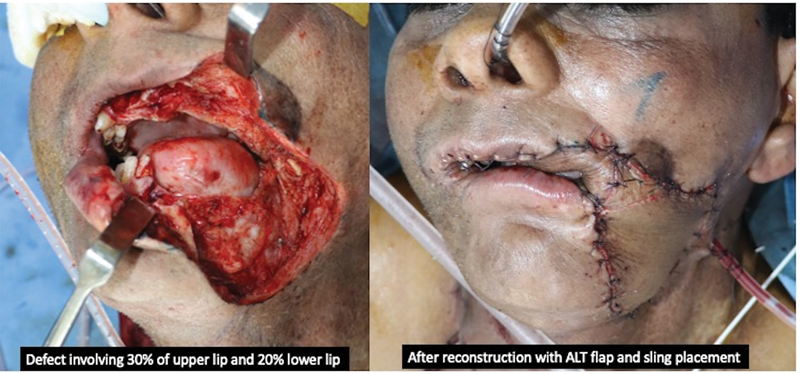
Defect postresection of tumor with defect involving the 30% of upper and 20% of lower lip commissure and buccal mucosa and segmental mandibulectomy. Reconstruction done with anterolateral thigh (ALT) free flap.
Fig. 5.

Long-term follow-up (2 years postsurgery) showing no leak of air and excellent lip competence.
Fig. 6.

Long-term follow-up (5 years postsurgery and radiation therapy.
Discussion
Excision performed for squamous cell carcinoma of buccal mucosa may involve excision of a minor or major part of the upper and the lower lip and/or oral commissure along with the buccal mucosa and cheek skin. This leads to discontinuity of the orbicularis orris muscle and its attachment to the modiolus. These defects are mostly reconstructed using free flaps. The ALT free flap is the workhorse flap for head and neck reconstruction. These flaps cover the defect but fail to restore the oral competency and shape of the oral commissure, leading to asymmetry, drooping of the angle of the mouth, oral incompetence, and drooling of saliva.
Oral competence can be achieved by coaptation of the residual lip edges in defects up to one-third of the total lip length. For defects between one-third to two-third local flaps are an option. 5 Reconstruction using a local flap in postcancer resection may not be a good option due to unavailability of sufficient local tissue. 6 Jeng et al 7 have reconstructed (combined defects up to 60% out of 200%, considering the normal length of both the lips combined as 200%) by lip advancement and primary closure with good outcomes in terms of oral competence and adequate oral stoma size. These techniques can restore oral competence but may lead to varying degrees of microstomia. 8 Microstomia may lead to poor oral and dental hygiene, inability to use dentures, difficulty in dental rehabilitation, and feeding difficulties. 9
In postcancer patients receiving adjuvant radiotherapy, microstomia may worsen and become even more debilitating. Adequate stoma size and oral competence are equally crucial in reconstruction after cancer resection.
Design modifications to address these problems have been done in the past. Fascial sling designs to address oral competence have been proposed and proven to be successful. Since the fascial sling is a static sling with no contractile ability, the onus of competence is on the residual muscle.
Radiotherapy has an adverse effect on the mouth opening due to reduced pliability of the tissue postradiation. An essential aspect of the reconstruction of oral competence is restoring the continuity of the orbicularis orris. Adding a C-sling restores the continuity of the oral commissure, but is not sufficient to restore the competence. Adding an extra limb shaped like the letter Y replicates the natural orientation and attachment of the orbicularis orris muscles ( Fig. 1 ). Sasaki et al 1 have tried to recreate the natural oral commissure and competence by the v/y design of fascial sling attached to masseter muscle replicating the modiolus of a normal lip. A symmetric Y design fails to overcome the effect of gravity and the weight of the flap ( Fig. 1 ), which leads to rounding and drooping of the angle of the mouth, leading to drooling of saliva. Defects from mandibular resection further add to the drag on the oral commissure. The above design is useful for different combinations of defects, which need commissure reconstruction. So far, we have come across no article that stresses upon the importance of stoma size and oral competence while considering the fascial sling design.
Conclusion
Modifying the fascial sling by making the lower limb 1 cm smaller than needed as per calculation and attachment to the malar prominence with overcorrection helps maintain good long-term functional outcomes by countering the effect of gravity and radiation. Adequate stoma matching the opposite side's dimensions helps maintain the mouth opening, commissure angle and overall symmetry of the reconstruction.
Conflict of Interest None declared.
Ethical Approval
Ethics committee approval obtained from the institutional ethics committee.
Authors' Contributions
All the authors were involved in the conception of the work, data collection, analysis and interpretation and throughout the process of the drafting and revision of the manuscript.
References
- 1.Sasaki K, Sasaki M, Oshima J, Aihara Y, Nishijima A, Sekido M. Free-flap reconstruction for full-thickness oral defects involving the oral commissure combined with oral modiolus reconstruction using a fascial sling. Microsurgery. 2020;40(05):553–560. doi: 10.1002/micr.30546. [DOI] [PubMed] [Google Scholar]
- 2.Jeng S F, Kuo Y R, Wei F C, Su C Y, Chien C Y. Reconstruction of extensive composite mandibular defects with large lip involvement by using double free flaps and fascia lata grafts for oral sphincters. Plast Reconstr Surg. 2005;115(07):1830–1836. doi: 10.1097/01.prs.0000164688.44223.75. [DOI] [PubMed] [Google Scholar]
- 3.Kuo Y R, Jeng S F, Wei F C, Su C Y, Chien C Y. Functional reconstruction of complex lip and cheek defect with free composite anterolateral thigh flap and vascularized fascia. Head Neck. 2008;30(08):1001–1006. doi: 10.1002/hed.20807. [DOI] [PubMed] [Google Scholar]
- 4.Yildirim S, Gideroğlu K, Aydogdu E, Avci G, Akan M, Aköz T. Composite anterolateral thigh-fascia lata flap: a good alternative to radial forearm-palmaris longus flap for total lower lip reconstruction. Plast Reconstr Surg. 2006;117(06):2033–2041. doi: 10.1097/01.prs.0000210663.59939.02. [DOI] [PubMed] [Google Scholar]
- 5.Matsui C, Tachibana K, Arai T et al. Combined ALT, Estlander, and upper lip flap for defects involving the oral commissure. Plast Reconstr Surg Glob Open. 2022;10(09):e4557. doi: 10.1097/GOX.0000000000004557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei F C, Tan B K, Chen I H, Hau S P, Liau C T. Mimicking lip features in free-flap reconstruction of lip defects. Br J Plast Surg. 2001;54(01):8–11. doi: 10.1054/bjps.2000.3481. [DOI] [PubMed] [Google Scholar]
- 7.Jeng S F, Kuo Y R, Wei F C, Su C Y, Chien C Y. Reconstruction of concomitant lip and cheek through-and-through defects with combined free flap and an advancement flap from the remaining lip. Plast Reconstr Surg. 2004;113(02):491–498. doi: 10.1097/01.PRS.0000100809.43453.C7. [DOI] [PubMed] [Google Scholar]
- 8.Qaisi M, Lubek J E. Complications associated with reconstruction of lip defects. Lip Cancer. 2013;x:137–145. [Google Scholar]
- 9.Ki S H, Jo G Y, Yoon J, Choi M SS. Reconstruction of microstomia considering their functional status. Arch Craniofac Surg. 2020;21(03):161–165. doi: 10.7181/acfs.2020.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]


