Introduction
The authors have observed fibrolipomatous growths in avid shortboard surfers that develop at the points on the chest wall of repetitive contact with the surfboard while prone paddling. The proposed etiology of these growths is incessant low-intensity traumatic compression of subcutaneous tissue, squeezed between the costal margin and the hard deck of a surfboard while paddling in the prone position.1, 2, 3, 4 These masses gradually increase in size with increased surfing activity and slowly diminish in size with prolonged surfing inactivity.1,3,5 These lesions are rather common in surfers, as most “older, long-time” surfers know of someone with these soft symmetric growths on the chest.5 However, the existing descriptions of these entities have be limited to isolated case reports.1, 2, 3, 4 Additionally, the literature lacks a consistent and clear nomenclature for these tumors.1, 2, 3, 4,6 We propose the term “Liposurfoma” (an infixation neologism) as a new, descriptive, and unambiguous designation for the subcutaneous chest wall fibrolipomas that uniquely affect shortboard surfers. Liposurfomas should not be mistaken for “Surfers’ knots,” which are symmetric rock-hard dense fibrotic callus-like masses on the lower extremity that affect longboard surfers.4,5,7
This case series describes 7 surfers with liposurfoma: 3 cases underwent surgical removal and subsequent histologic analysis; 2 cases underwent tumescent liposuction accomplished under tumescent epinephrine (0.1 mg/100 mL), lidocaine (100 mg/100 mL), sodium bicarbonate (10 mEq/L) (TEL) local anesthesia; and 2 opted for no treatment.
Surgical removal
Case 1
A 55-year-old male surfer presented with 2 large mobile chest wall masses, which he reported to have had for many years. However, he complained of recent onset of a gradually enlarging, firm, mildly tender singular nodule embedded within the central portion of the right-sided chest wall mass. The nodule became increasingly tender during and after surfing, yet became less tender after not surfing for a week.
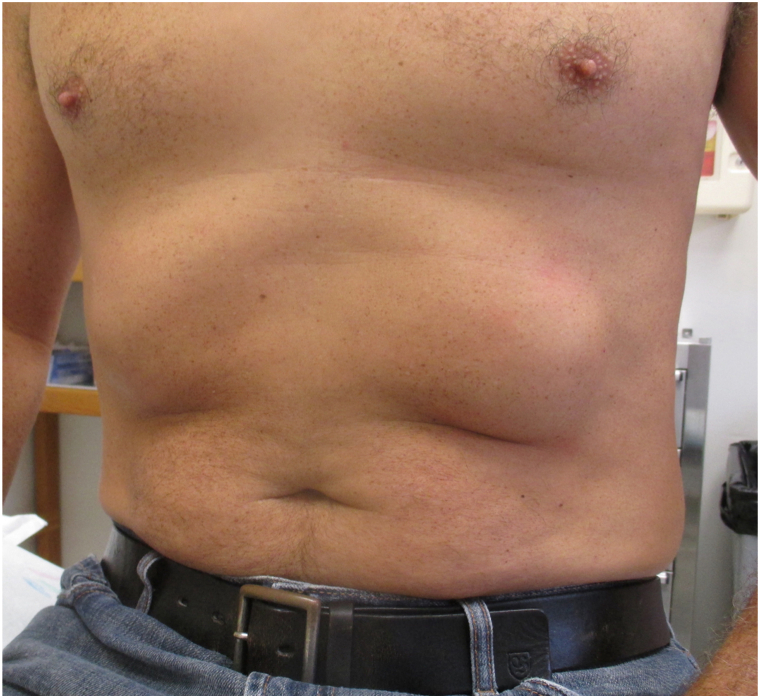
Physical examination revealed 2 bilateral, symmetric, nontender 10 cm by 12 cm chest wall masses, which were compressible and clinically consistent with lipofibromatous growths (Fig 1, A). A small 2 cm by 3 cm slightly tender nodule, seemingly adherent to the dermis, could be palpated within the central portion of the large right-sided lipomatous mass.
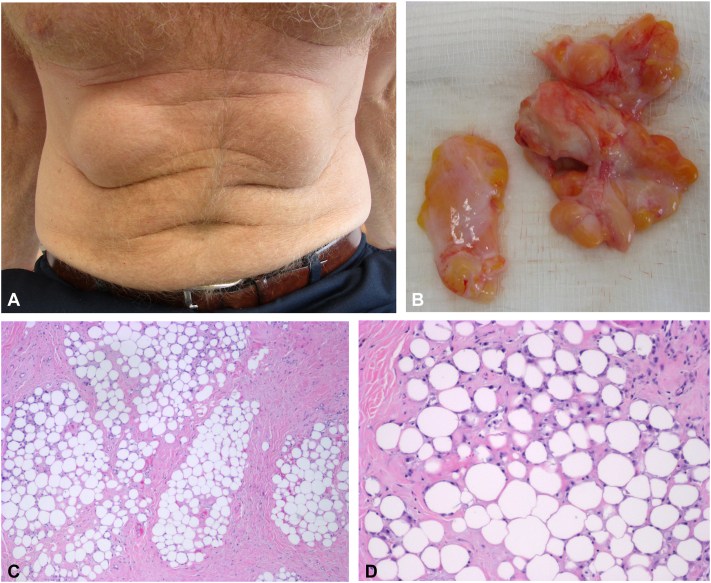
Fig 1.
A, Preoperative bilateral fibrolipomas on the chest wall of a surfer. B, Incised fibrofatty lobulated nodule. C, Photomicrograph (hematoxylin-eosin (H&E) stain; original magnification: ×4 of fatty lobules, surrounded by hyalinized collagen. There is notable variation in the size and shape of the individual entrapped adipocytes. D, Photomicrograph (H&E stain; original magnification: ×10 of hypertrophy and sclerosis of normal lipomatous septa.
An incisional biopsy of the tender subcutaneous nodule (not the entire fibrolipoma) was performed using TEL local anesthesia. After allowing 30 minutes to achieve adequate detumescence and optimal capillary vasoconstriction, the nodule was incised without bleeding or any need for cautery. The gross appearance was that of a firm fibro-fatty mass having several discrete smooth grape-like fibrous lobules (Fig 1, B). Compared with the broadly distributed mild-to-moderate fibrosis present throughout the surrounding fibrolipoma, the incised nodule was densely fibrotic. This augmented degree of fibrosis appeared to be the result of more intensely focused subacute compression between a rib and a hard place.
The histologic specimen consisted of hyalinized collagen with scattered fibroblasts, and foci of entrapped islands of fat. Fibrosis extended into the reticular dermis. Fatty lobules were surrounded by hyalinized collagen and variable fatty necrosis. There was notable variation in the size and shape of the individual entrapped adipocytes. There were no significant acute or chronic inflammatory infiltrates. There was hypertrophy and sclerosis of normal septa, consistent with chronic traumatized subcutaneous fat (Fig 1, C, D).
Case 2
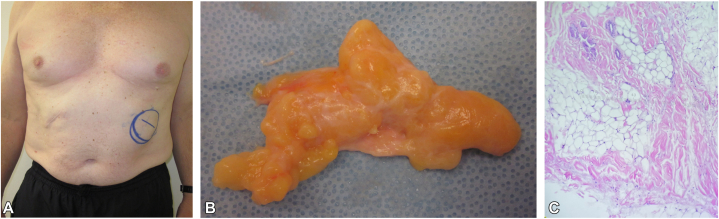
A 55-year-old man surfer previously had what was thought to be a lipoma excised from the right upper abdomen by another physician. Years later, he presented to our clinic and inquired about treatment options for a similar lesion on the left upper abdomen. Upon examination there was a well-defined, 3 cm by 6 cm subcutaneous mass symmetrically located with respect to the prior excision site (Fig 2, A). Excisional biopsy revealed a somewhat encapsulated mildly fibrous lipoma (Fig 2, B). The histopathology showed multiple circumscribed nodules of mature adipose tissue with focal fibrous bands associated with myxoid degeneration consistent with previous trauma (Fig 2, C).
Fig 2.
A, Surgical scar on a surfer’s right upper abdomen following a prior “lipoma” excision. Symmetrically located fibrolipoma on the left upper abdomen. B, Gross appearance of excised lipoma. C, Photomicrograph of excised fibrolipoma (hematoxylin-eosin stain; original magnification: ×4.
Case 3
A 53-year-old man surfer presented for routine skin examination which revealed 2 bilaterally symmetric scars on the upper abdomen (Fig 3). Eight years previously, a surgeon diagnosed common subcutaneous lipomas which were excised under general anesthesia.
Fig 3.
Surfer with prominent bilaterally symmetric scars following surgical excision of chest wall lipomatous masses.
Tumescent epinephrine lidocaine (TEL) liposuction
Case 4
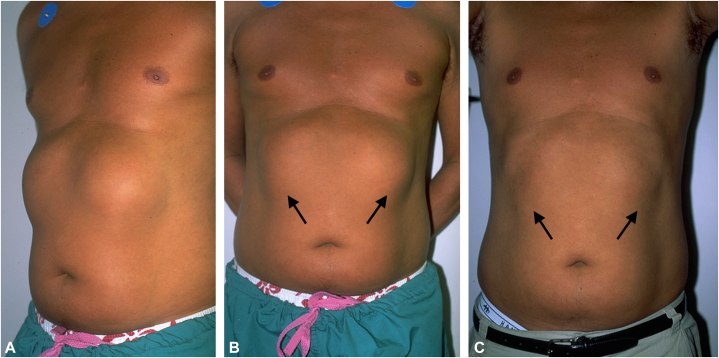
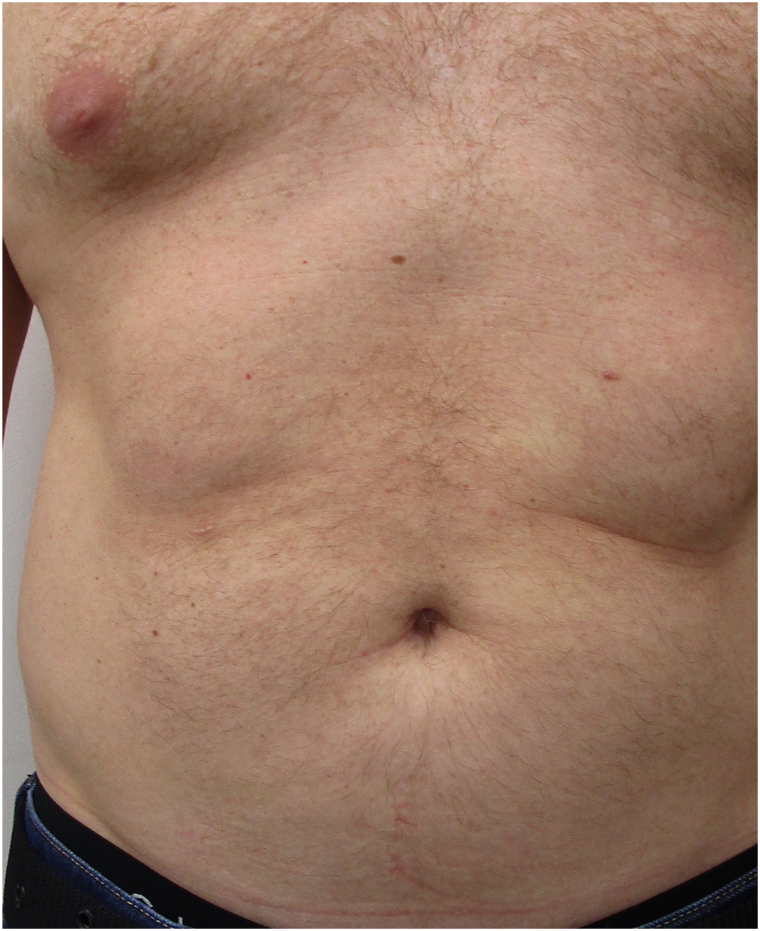
A 44-year-old man surfer presented with remarkably prominent bilateral subcutaneous tumors located on the upper abdomen and extending over the anterior-inferior costal margin (Fig 4, A, B). Successful treatment required 2 sequential liposuctions accomplished under TEL local anesthesia. Liposuction was unusually challenging because of the fibrous consistency and the large size of the fibrolipomas. Liposuction was accomplished using microcannulas with sequentially increasing gauge sizes, starting with a 16 gauge, then 14 gauge, and then 12 gauge cannula. Larger gauged cannulas should be avoided as they cannot effectively penetrate through the dense fibrous stroma of chest wall fibrolipomas. The first liposuction achieved a 50% improvement. The patient continued to surf regularly. When the patient returned 12 months later, the fibrolipomas had slightly increased in size. A second liposuction yielded more satisfactory results (Fig 4, C).
Fig 4.
A,B, Preoperative oblique and frontal view of unusually large bilateral chest wall fibrolipomas in a surfer before first liposuction procedure. C, Postoperative frontal view 12 months after second liposuction procedure.
Case 5
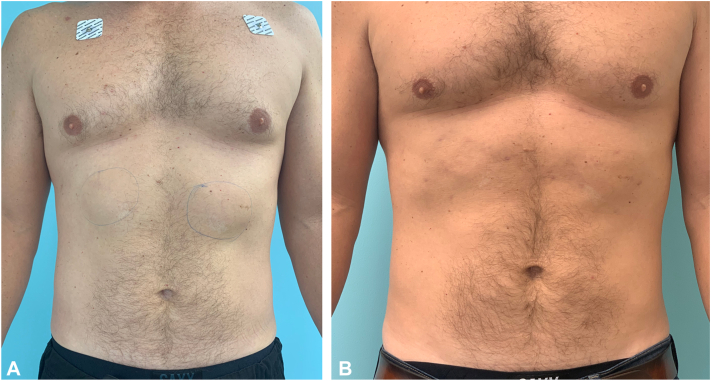
A 41-year-old man presented with moderately sized bilateral chest wall fibrolipomas (Fig 5, A). After injection of TEL local anesthesia and 90-minutes of detumescence, liposuction was accomplished with the use of microcannulas. The 10-week follow-up photograph documents the efficacy of TEL liposuction in reducing the size of chest wall fibrolipomas in surfers (Fig 5, B).
Fig 5.
A, Preoperative appearance of moderate bilateral fibrolipomas (faint drawn blue circles) on the chest wall of a surfer. B, Postoperative appearance 10-weeks after microcannula liposuction.
No treatment
Cases 6 and 7
Two surfers with prominent bilateral chest wall fibrolipomas were seen in consultation about their condition and treatment options (Figs 6 and 7). After learning that these fibrolipomas may recur posttreatment if shortboard surfing is continued, both surfers chose to forego any treatments.
Fig 6.
Surfer with bilateral chest wall fibrolipomas who opted for no treatment.
Fig 7.
Surfer with bilateral chest wall fibrolipomas who opted for no treatment.
Discussion
“Liposurfoma”: Proposed designation for chest wall fibrolipomas in surfers
Avid surfers may acquire bilateral fibrolipomas overlying the upper abdomen and anterior costal margin at the points of repetitive contact with the surfboard while prone paddling. The literature lacks consistent and clear nomenclature for these tumors, and their abundant fatty composition is not well described.1, 2, 3, 4,6 Therefore, we propose adopting the designation “Liposurfoma,” as it is a descriptive and unambiguous term that conveys both the histologic and epidemiologic features of this unique littoral dermatologic disease.
Proposed etiologic mechanism
Liposurfomas in shortboard surfers are likely associated with chronic repetitive low-intensity-trauma induced by prone paddling. This form of trauma-induced fibro-lipomatous proliferation has also been reported to occur below the clavicle of a violinist (which correlates with the anatomic location upon which a violin rests) and along the perineum of an equestrian.8,9 A reasonable explanation for the cause of chronic mild trauma induced fibrolipomas is the regular, prolonged and frequent exposure to focal low-grade traumatic compression affecting subcutaneous tissue as it is pinched between costal margin and surfboard, clavicle and violin, or perineum and saddle.1, 2, 3, 4,8,9 A plausible lipogenesis pathway for liposurfoma formation in surfers may involve (1) repeated subcutaneous microtraumas, (2) induction of aberrant repair pathways, (3) release of proinflammatory cytokines, (4) chronic inflammation, (5) preadipocyte differentiation, and (6) proliferation of fibroblasts and adipocytes.10,11 The risk of malignant transformation in such lesions is not known, but based on the current literature, and in the experience of the authors, the long-term prognosis of this entity appears benign.4
Liposurfomas versus surfer’s knots
Longboard surfboards (typically 8-10.5 feet long) were the ubiquitous standard throughout the late 1950s and 1960s. The shortboard revolution began around 1967, when surfers realized that smaller boards (6-7 feet long) allowed for more radical turns on the face of a wave.4,12 The larger longboards provide far superior floatation which allows for paddling while kneeling. When paddling in this position, only the knee (anterior tibial plateau), dorsal midfoot (tarsal-metatarsal) and dorsal toes are in constant contact with the longboard deck. These areas are the sites of Surfers’ knots, also known as Surfers’ nodules, Surf bumps, or Surfer’s knobs.4,6,13 In contrast, the decreased buoyancy of short boards requires prone paddling with much of the board slightly submerged, the back arched, and neck extended to keep the face above the water. In this position, continuous pressure is applied to the anterior costal margin, with the potential to induce liposurfomas.1,2 With the advent of shortboards, the prevalence of lower extremity surfer’s knots declined, whereas the prevalence of liposurfomas increased.4 Back in the day, however, surfer’s knots were marks of distinction and prestige among the surfing cognoscenti.5,14
Liposurfomas and surfer’s knots are nosologically distinct entities, with different mechanical etiologies, compositions, and anatomic locations. Liposurfomas are bilaterally symmetric chest wall swellings induced by prone paddling on shortboards, while Surfers’ knots are symmetrical lower extremity masses (typically affecting the knees, dorsal midfoot, and toes) induced by knee paddling on long boards.1,2,4, 5, 6, 7,12, 13, 14 Liposurfomas are subcutaneous fibrolipomas composed of fibrous tissue with abundant adipocytes (Figs 1, C, D and 2, C). Surfers’ knots are somewhat mobile hypertrophic avascular callus-like masses affecting the subcutaneous tissue composed of rock-hard dense fibrotic connective dermal tissue, completely devoid of fat.4,5,7 The diameter of surfers’ knots can range from 1 to 6 cm, with a height of as much as ≥2.5. During the Vietnam war, individuals with surfer’s knots that were too large to permit the wearing of combat boots were excused from conscription in the military draft. Both surfers’ knots and liposurfomas increase in size with increased surfing activity and decrease in size with surfing inactivity.1,3,5 In contrast to surfer’s knots, which have been reported to occasionally become infected or ulcerate, liposurfomas do not appear to cause complications beyond soreness.4,12 Despite their stark differences, reports in the literature have seemingly lumped longboard-associated lower extremity surfer’s knots together with shortboard-associated chest wall fibrolipomas.1, 2, 3, 4
Another littoral disease that may be mistaken for a liposurfoma is a surfer’s bursa, which was described in a single case as a large, recurrent, soft tissue mass on the chest wall of a surfer with a distinctive histologic appearance of a cyst partially lined by synoviocytes and a dense fibrotic wall.15 Although most physicians are unaware of liposurfoma as a diagnostic entity, liposurfomas should be considered as a possible diagnosis when an avid surfer presents with bilateral chest wall growths. Additionally, if a dedicated surfer exhibits a unilateral lipomatous chest wall growth accompanied by a symmetric scar from a prior “lipoma” removal (Fig 2, A), or bilateral symmetric chest wall scars from previous surgical removal of lipomatous masses (Fig 3), the possibility of liposurfoma should be considered.
Liposurfoma treatment
Based on our experience, a patient who presents with a liposurfoma can be counseled regarding their benign nature and the likelihood of persistence or recurrence with continued surfing. If treatment of liposurfomas is requested, then liposuction totally by TEL local anesthesia using microcannulas is a reasonable approach (Figs 4, A-C, and 5, A, B). Surgical removal is another therapeutic option, although it is unavoidably associated with visible scarring (Figs 2, A and 3).3 Patients may also opt to decline surgery in favor of observation and management via wetsuits with foam padding over the area of focal compression to lessen the soreness and discomfort associated with prolonged prone paddling.4
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
Patient consent: The authors obtained written consent from patients for their photographs and medical information to be published in print and online and with the understanding that this information may be publicly available. Patient consent forms were not provided to the journal but are retained by the authors.
IRB approval status: Not applicable.
Prior presentation: This case series has not been presented previously.
References
- 1.Baba A., Okuyama Y., Yakabe H., Yamazoe S., Kobashi Y., Mogami T. Surfers’ knots in the anterior chest. Clin Case Rep. 2019;7(3):597–598. doi: 10.1002/ccr3.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tashima C.K. Letter: surfer’s chest knots. JAMA. 1973;226(4):468. doi: 10.1001/jama.1973.03230040042024. [DOI] [PubMed] [Google Scholar]
- 3.Miguelote P.M., Barbassa T., Marchiori E. Surfers’ knots: an uncommon cause of chest wall masses. Arch Bronconeumol. 2022;58(1):86. doi: 10.1016/j.arbres.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 4.McManus L.J., Thomson A., Whan A. The magnetic resonance appearance of surfers’ knots: a case report. Radiol Case Rep. 2016;11(3):201–206. doi: 10.1016/j.radcr.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swift S. Surfers’ “knots”. JAMA. 1965;192(3):223–224. doi: 10.1001/jama.1965.03080160043011. [DOI] [PubMed] [Google Scholar]
- 6.Burdick C.O. Surfer’s knots. JAMA. 1981;245(8):823. doi: 10.1001/jama.1981.03310330013010. [DOI] [PubMed] [Google Scholar]
- 7.Gelfand D.W. Surfer’s knots. Associated bone changes and medical problems. JAMA. 1966;197(2):149–150. doi: 10.1001/jama.1966.03110020137049. [DOI] [PubMed] [Google Scholar]
- 8.Erginöz E., Çavuş G.H., Çarkman S. Post-traumatic chest wall lipoma in a violinist: fact or fiction? Interact Cardiovasc Thorac. Surg. 2022;34(3):500–501. doi: 10.1093/icvts/ivab266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devers K.G., Heckman S.R., Muller C., Joste N.E. Perineal nodular induration: a trauma-induced mass in a female equestrian. Int J Gynecol Pathol. 2010;29(4):398–401. doi: 10.1097/PGP.0b013e3181ce1341. [DOI] [PubMed] [Google Scholar]
- 10.Henderson N.C., Rieder F., Wynn T.A. Fibrosis: from mechanisms to medicines. Nature. 2020;587(7835):555–566. doi: 10.1038/s41586-020-2938-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chimenti I., Sattler S., del Monte-Nieto G., Forte E. Editorial: fibrosis and inflammation in tissue pathophysiology. Front Physiol. 2021;12 doi: 10.3389/fphys.2021.830683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cragg J. Surfers’ nodules. Br J Clin Pract. 1973;27(11):418–419. doi: 10.1111/j.1742-1241.1973.tb09086.x. [DOI] [PubMed] [Google Scholar]
- 13.Erickson J.G., von Gemmingen G.R. Surfer’s nodules and other complications of surfboarding. JAMA. 1967;201(2):134–136. doi: 10.1001/jama.1967.03130020080025. [DOI] [PubMed] [Google Scholar]
- 14.Surfer’s nodules. Br Med J. 1967;4(5577):437. [PMC free article] [PubMed] [Google Scholar]
- 15.Chaves Gomes D., Farshid G., Bruening M. Surfer’s bursa: a recurrent chest wall mass in dedicated surfers that may mimic a sarcoma. Pathology. 2021;53(4):550–552. doi: 10.1016/j.pathol.2020.08.029. [DOI] [PubMed] [Google Scholar]