Abstract
Objective
Evaluate the effects of 10 min/day of yoga for 1 month on musculoskeletal discomfort and mood disturbance of home-office workers.
Background
The COVID-19 pandemic forced many people to switch to teleworking. The abrupt change from an office setting to an improvised home-office may negatively affect the musculoskeletal and emotional health of workers. By providing mental and physical exercises, yoga may be effective in reducing adverse effects.
Method
Fifty-four participants (42 women, 12 men) followed a 1-month yoga program, while 40 participants (26 women, 14 men) continued with their common work routine. The Cornell Musculoskeletal Discomfort Questionnaire was used to evaluate severity, interference with work and frequency of pain, and to obtain a total discomfort score for 25 body areas. Mood disturbance was evaluated with the Profile of Mood States questionnaire. Both groups completed both questionnaires, before and after the experimentation period.
Results
After 1 month, for the yoga group only, significant reductions were observed in the discomfort of eyes, head, neck, upper and lower back, right wrist, and hips/buttocks, as well as reductions in discomfort severity, frequency and interference for the neck, upper and lower back. Total mood disturbance was also significantly reduced for the yoga group only. No favorable changes occurred for the control group.
Conclusion
The yoga intervention program appears to reduce musculoskeletal discomfort and mood disturbance of home-office workers.
Application
Sedentary workers may benefit from 10 min/day of yoga during the workday to attenuate potential physical and emotional discomfort during the current pandemic and beyond.
Keywords: yoga, musculoskeletal discomfort, emotional state, office workers, teleworking
The outbreak of COVID-19 infections was classified as a pandemic by the World Health Organization in March 2020 (WHO). In an effort to slow infection rates, particularly in groups predisposed to high risks of morbidity and mortality, extensive social distancing and isolation policies were adopted worldwide (Pinto et al., 2020). In the United States, about half of people employed pre-COVID-19 are now working from home (Brynjolfsson et al., 2020). In Ecuador home-based working increased from 0.47% (12,800 registered employees) pre-pandemic to about 10% (436,484 employees; Echeverria, 2020; Torres, 2020). Although these restrictions are effective at preventing the spread of COVID-19 (Nussbaumer-Streit et al., 2020), they might negatively affect physical and mental health (Brooks et al., 2020; Pieh et al., 2020; Slater et al., 2020). Moreover, the challenge of an abrupt transition to isolation in a home-office setting, coupled with the pandemic-induced stress (Birditt et al., 2021; Dos Santos et al., 2020), is likely to adversely influence the risk of musculoskeletal disorders (MSDs). It is well established that MSDs are a leading cause of work disability, absenteeism, and loss of productivity (BLS, 2020), and they are a significant economic and psychosocial burden (Bevan, 2015; Bhattacharya, 2014). Psychosocial factors are known to influence the development of work-related MSDs in various occupational settings (Bongers et al., 1993; Deeney & O’Sullivan, 2009; Ilić et al., 2017; Sprigg et al., 2007), including office work (Smith & Carayon, 1996).
The prevalence of MSDs in office workers remains high. The body parts corresponding to the largest number of complains (>50%) are the low back (Bontrup et al., 2019; Celik et al., 2018; Piranveyseh et al., 2016) and neck (Celik et al., 2018; Collins & O’Sullivan, 2015; Harcombe et al., 2009) followed by upper extremities (Coenen et al., 2018; Harcombe et al., 2009). Moreover, visual problems, such as visual fatigue, dry eyes, tired eyes, redness, blurred vision, double vision, and irritation have been related to frequent computer use (Gowrisankaran & Sheedy, 2015), as commonly performed during office work. Numerous factors may influence work-related musculoskeletal symptoms in office workers, including psychosocial and organizational factors (Piranveyseh et al., 2016; Smith & Carayon, 1996), the use of a mouse and keyboard, time spent working on a computer, workstation design (Celik et al., 2018; Harcombe et al., 2009; Rodrigues et al., 2017), low physical capacity (Cabral et al., 2019), prolonged sitting (Bontrup et al., 2019; Daneshmandi et al., 2017; Waongenngarm et al., 2020), and sitting in combination with awkward postures (Kwon et al., 2018; Lis et al., 2007).
Due to the health impact and risk factors present in office work, several workplace interventions have been proposed to reduce the risk of MSDs and symptoms (Callaghan et al., 2015; Van Eerd et al., 2016). Musculoskeletal symptoms affecting office workers are significantly reduced by implementation of resistance training (Andersen et al., 2008, 2012; Blangsted et al., 2008), physical exercise (Sjögren et al., 2005), or stretching exercise programs at the workplace (Galinsky et al., 2007; Jepsen & Thomsen, 2008; Lacaze et al., 2010). Yoga-related exercises have been considered as an intervention in the workplace for both physical (Joshi & Bellad, 2011; Telles et al., 2006) and mental (Axén & Follin, 2017; Casey et al., 2018) benefits.
Yoga is an ancient practice that seeks to improve physical, mental, and spiritual health through exercises that focus on strength, posture, flexibility, breathing, and meditation (Feuerstein, 2001). Several literature reviews highlight the positive effect of yoga on low back pain (Chou et al., 2017; Cramer et al., 2013; Zhu et al., 2020), sleep quality (Wang et al., 2020), stress management (Cocchiara et al., 2019; Wang & Szabo, 2020), and neck pain (Cramer et al., 2017; Li et al., 2019). However, most of these studies have been performed on patients evaluating yoga as a treatment and not particularly as a preventive workplace intervention. Recent reviews concluded that yoga programs at the workplace can reduce stress (Bischoff et al., 2019; Della Valle et al., 2020; Puerto Valencia et al., 2019); however, the authors stated that further studies are needed to strengthen the validity of these findings. These work-related yoga studies have evaluated diverse working populations including nurses (Axén & Follin, 2017), wellness employees (Casey et al., 2018), and the general working population (de Bruin et al., 2017), but few focus only on office workers (Abdin et al., 2018; Maddux et al., 2018) and none on home-office work. So far, the influence of yoga on home-office work due to COVID-19 has not been explored. Therefore, the purpose of the present study was to evaluate whether or not a yoga program has a physical and emotional effect on office workers, forced into home-offices due to the COVID-19 pandemic. Physical activities aimed at disrupting the monotony of prolonged static muscle contractions are successful at reducing muscle fatigue (Falla & Farina, 2007), which is considered as a precursor of MSDs (see for review Côté, 2014). Hence, it is presumed that yoga exercises requiring changes in muscle activities will have beneficial effects on musculoskeletal symptoms. In this context, validated questionnaires were used to address whether a 1-month yoga program, with short 10-min sessions per day, (a) influences the perception of musculoskeletal discomfort of home-office workers, and (b) influences the emotional state of home-office workers?
Method
Study Design and Participants
This study focused on adults required to work from home due to COVID-19 confinement. Inclusion criteria were working at least 5 days a week, spending at least 6 hr a day working with a desktop, tablet, or laptop computer, and being older than 18 years of age. The exclusion criteria included current pregnancy, any neurological, vascular, or acute musculoskeletal condition or any disease or symptom (including COVID-19) that could interfere with the study. The study was approved by the Ethics Committee of the Universidad San Francisco de Quito (# 2020–059IN) and participants signed an informed consent form prior to data collection. The present study complied with the tenets of the Declaration of Helsinki. Participants were recruited through a nonprobabilistic snowball sampling, which consists of recruiting several members to participate in the study, who then recruit more participants among their acquaintances/social network (Etikan & Bala, 2017). The method was obligated by the difficulty of remotely reaching individuals in specific organizations and the lack of response when a general invitation was sent to all administrative personnel within the organizations.
Through this sampling method, responses were received from 147 survey invitations. Only eight (5.44%) invitees did not agree to participate in the program, and 37 (25.17%) did not meet the inclusion criteria. Hence, the 139 volunteers were pseudo randomly assigned to two groups, as a few adjustments were made to comply with subject’s participation conditions (“only if in control” [5 participants] or “only if in yoga” [1 participant]). Statistical results were not influenced by the exclusion or inclusion of these six participants; thus, it is unlikely the randomization procedure biased the results. Group 1 (yoga group) included 90 participants following the 1-month yoga program, and Group 2 (control group) included 49 participants performing only their regular work routine. However, to motivate participants to be part of the control group, full access to the yoga program was offered at the end of the study period.
During the study period, 36 participants from the yoga group did not follow the yoga program and/or fill out the questionnaires (32) or formally dropped (4), and nine participants from the control group formally withdrew from the study. The yoga group, therefore, comprised of 54 participants (42 women and 12 men) with a mean age of 37.8 ± 11.5 years old, height of 161.26 ± 8.64 cm, weight of 62.5 ± 10.8 kg, and BMI of 24.00 ± 3.60. The control group included 40 participants (26 women and 14 men) with a mean age of 39.4 ± 11.2 years old, height of 163.43 ± 8.74 cm, weight of 66.2 ± 12.4 kg, and BMI of 24.51 ± 4.01. The absence of significant difference between groups for age, height, weight, and BMI was verified (p = .48, p = .23, p = .14, and p = .37 respectively). Participants from both groups were requested to maintain their common daily routines regarding food intake, leisure activities, physical activities, sports, work, and other daily habits during the experimental period. All data were collected during the COVID-19 pandemic period from May 10, 2020, to August 11, 2020.
Questionnaires and Outcome Measures
Two validated and extensively used questionnaires were administered to all participants. The Cornell Musculoskeletal Discomfort Questionnaire (CMDQ) was selected to estimate the physical status of each participant, including MSD complaints (Hedge et al., 1999). The Profile of Mood States (POMS) questionnaire was used to assess transient, distinct mood states (McNair et al., 1971).
The CMDQ used was the validated Spanish version (Carrasquero, 2015). This adaptation requires the rating of discomfort/pain in 25 body parts, both right and left side, in the upper and lower extremities, along three dimensions: frequency (Never = 0; 1–2 times last week = 1.5; 3–4 times last week = 3.5; once a day = 5 or several times a day = 10); severity (a little uncomfortable = 1, moderately uncomfortable = 2, very uncomfortable = 3); and interference with work (Not at all = 1, interferes slightly = 2, interferes forcefully = 3). Each body part, identified on a full body diagram, was associated with the three category rating scales to be marked. The frequency category corresponded to the question “How often did you experience pain or discomfort during the last week of work?”; the severity category to “If you experienced pain/discomfort, how uncomfortable was this?”; and the interference category to “If you experience pain/discomfort, did this interfere with your ability to work?” (Hedge et al., 1999). The total scores (weighted rating scores mean) from frequency, severity, and interference were used to obtain the Discomfort Score, by multiplying the three dimensions for each body part (Hedge et al., 1999).
The POMS questionnaire was the validated Spanish reduced version (Andrade et al., 2013). Thirty items are used to rate six first-order factors named anger, fatigue, vigor, friendliness, tension, and depressed mood (five items each). Ratings were indicated on a five-point scale ranging from 0 = not at all to 4 = extremely. The value of each factor was obtained by adding the ratings of the five corresponding items. Then the outcome measure, Total Mood Disturbance (TMD) score, which is a general indicator of emotional disturbance, corresponded to the difference of the respective sums of negative factors (anger, fatigue, tension and depressed mood) and the positive factor (vigor; Lin et al., 2014). Friendliness is a dummy factor, not used for the total score. Overall, the higher the TMD score, the higher the degree of mood disturbance or psychological distress. Therefore, a reduction of TMD is desired (Yoshihara et al., 2011).
Procedure
A 1-month yoga program was created for this study and made available to each participant through a web platform. This platform was built using the PHP hypertext processor (PHP.Net) and JavaScript (Oracle Corp.) programing language with its database in MySQL (Oracle Corp.) and Linux (Linux Foundation) operating system. The software was developed in collaboration with AEM Solutions (Quito, Ecuador). Each participant received an access link to the platform to create their private access. The platform contained the CMDQ and POMS questionnaires, which had to be filled out by each participant at the beginning (T1) and at the end (T2) of the 1-month experiment. Access to the exercise routines was granted to the yoga group only after completion of the initial questionnaires at T1, and to the control group only after completing the questionnaires at T2. All participants were encouraged to start on the same day, but a 5-day window period from our original start day was allowed. Thus, the initial measurement at T1 for all participants before undergoing the experimental period was estimated to be homogeneous.
The yoga program consisted of daily (Monday–Friday) 10-min routines that focused on (1) mindfulness (repeating positive affirmations), (2) breathing regulation (pranayama), (3) postures (asanas), and (4) relaxation (concentrating on the state of the body; de Manincor et al., 2015). Since yoga is a holistic practice, the daily focus of the program varied in areas of the body without neglecting any. Monday’s and Wednesday’s routines focused on the upper body, Tuesday’s and Thursday’s on the lower body, and Friday’s on the whole body.
Each daily yoga routine was accessible to each participant for only 24 hr, then replaced by a newly assigned routine. Hence, participants had access only to the preestablished daily routine presented in the same order to all. The exercises were described through digital manuals and videos containing a clear explanation and demonstration of the posture sequences to be performed. At the end of the practice, each user was required to register the routine of the day, with the option to rate and comment on the routine. This procedure helped to keep track of the participants who completed the routine successfully. The participants were encouraged to perform the routine as a break within the teleworking period of the day.
All yoga routines were developed in collaboration with a certified yoga instructor. Exercises were based on Vinyasa Yoga. This yoga is known to require dynamic body movements while maintaining conscious breathing and is usually guided with different levels of difficulty (Tsopanidou et al., 2020). For the present yoga program, routines were aimed at beginners to limit difficulty to a minimum. Hence, high levels of strength and flexibility were not required for the proposed exercises. The program contained five different breathing techniques (pranayama), aiming at different benefits on a physical and mental level (deep breathing, Nadi Shodhana, Ujjayi, Kapalabhati, and Kumbhaka) and different postures and exercises, including neck movements (Greeva Sanchalana), mountain pose (Tadasana), chair pose (Utkatasana), standing clamp (Uttanasana), and warrior position I (Virabhadrasana I).
Data Analysis
All data analysis was performed with SPSS (SPSS Inc.). The normality assumption was checked for POMS and CMDQ data with the Shapiro-Wilk test. Since POMS data fulfilled the normality assumption, TMD scores were analyzed with linear mixed models. The independent variables, fixed effects, for the models were measurement time (T1, T2) and group (intervention, control), while participants were considered as a random variable. Post-hoc multiple comparisons were performed with the Bonferroni Procedure. The CMDQ data were analyzed with Mann-Whitney U test. First, differences between pre and post measurement times (T1-T2) were calculated for each group and statistically compared. Then, discomfort scores, frequency, severity, and interference differences from T1 to T2 were explored to compare the outcomes before and after the experimentation period for both groups. The level of significance was set at p < .05.
Results
CMDQ Discomfort Score Yoga and Control
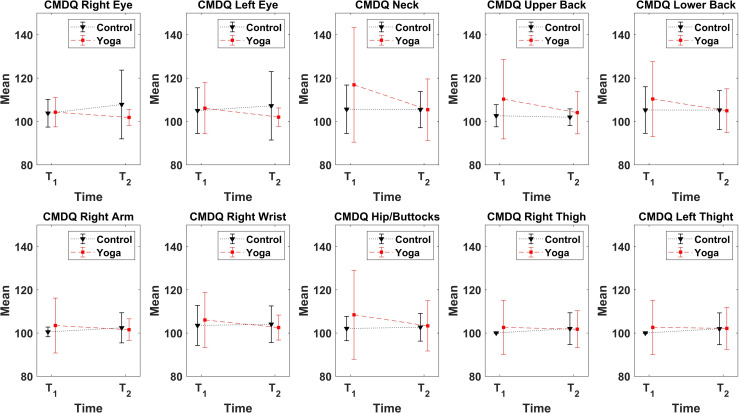
Table 1 shows that discomfort score differences (T1-T2) are significantly different between the yoga and the control group for both eyes, neck, upper back, lower back, right arm, right wrist, hips/buttocks, and both thighs (p < .05). Discomfort scores for the control group remained similar or were higher (negative values in Table 1) at T2 than T1 (Figure 1), while the discomfort scores are generally lower at T2 than T1 (positive values in Table 1) for the yoga group. Furthermore, most of the discomfort scores were not significantly different (p > .05) between groups at T1, except for the neck (p = .03), upper back (p = .01), thighs (p = .02), right wrist (p = .02), and right arm (p = .01).
Table 1.
Group Comparison of CMDQ Discomfort Score Differences (T1-T2)
| Body Regions | Yoga Group Difference (T1-T2) | Control Group Difference (T1 -T2) | p value | ||
|---|---|---|---|---|---|
| M | ±SD | M | ±SD | ||
| Right eye | 2.41 | 6.47 | −4.03 | 15.50 | .002* |
| Left eye | 4.12 | 11.78 | −2.24 | 12.77 | .01* |
| Head | 0.58 | 8.83 | −1.09 | 9.46 | .20 |
| Neck | 11.47 | 27.02 | 0.18 | 10.24 | .002* |
| Right shoulder | 4.58 | 17.24 | −.74 | 9.48 | .22 |
| Left shoulder | 1.07 | 5.57 | −.43 | 5.72 | .30 |
| Upper back | 6.21 | 15.41 | 0.68 | 5.73 | .03* |
| Lower back | 5.42 | 16.75 | 0.01 | 13.79 | .05* |
| Right arm | 1.93 | 13.33 | −1.89 | 6.78 | .04* |
| Left arm | 0.02 | 3.41 | −1.83 | 6.58 | .30 |
| Right elbow | 1.13 | 6.26 | −.70 | 4.18 | .54 |
| Left elbow | 0.50 | 6.13 | −1.25 | 3.43 | .43 |
| Right forearm | 2.42 | 13.78 | −1.76 | 7.05 | .14 |
| Left forearm | −.13 | 2.28 | −1.09 | 4.71 | .49 |
| Right wrist | 3.51 | 12.38 | −.56 | 8.40 | .01* |
| Left wrist | 0.66 | 6.66 | −.75 | 2.95 | .43 |
| Hips/buttocks | 5.11 | 19.62 | −.60 | 8.29 | .02* |
| Right thigh | 0.83 | 13.10 | −2.00 | 7.34 | .01* |
| Left thigh | 0.46 | 11.26 | −1.95 | 7.34 | .01* |
| Right knee | 2.30 | 9.47 | −1.08 | 5.80 | .16 |
| Left knee | 1.07 | 4.60 | −2.23 | 6.74 | .10 |
| Right calf | −.59 | 2.89 | −.70 | 2.47 | .72 |
| Left calf | −.53 | 2.86 | −.74 | 2.47 | .54 |
| Right ankle/foot | 1.78 | 11.33 | 1.15 | 12.97 | .08 |
| Left ankle/foot | −.47 | 2.28 | −1.64 | 7.47 | .36 |
Note. Mean (M) ± standard deviation (SD) of pre (T1) and post (T2) measurement differences are compared between yoga and control groups. Bold font and * indicate significant values, α = .05. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
Figure 1.
CMDQ discomfort scores. Mean ± SD of pre (T1) and post (T2) measurement times. The difference in discomfort between pre and post measurement times was significant between groups for the 10 body areas presented. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
For the yoga group, the discomfort score was significantly different between T1 and T2 for both eyes, head, neck, upper back, lower back, and hips/buttocks (p < .05), as presented in Table 2. For all these body areas, discomfort scores after the yoga program (at T2) were significantly lower than at baseline (T1). However, when evaluating the difference between T1 and T2 for the control group, no significant differences were observed in body areas except for both thighs, where the discomfort scores were significantly higher (p = .003) at T2 than T1. Similar results were obtained when evaluating CMDQ categories alone for the control group, where frequency (p = .003), severity (p = .01), and interference (p = .01) were significantly higher for thighs only, but not significant for all other body areas. Due to the lack of significant results in the control group, CMDQ tables for frequency, severity, and interference are presented only for the yoga group.
Table 2.
Yoga Group Comparison of CMDQ Discomfort Scores (T1 Versus T2)
| Body Regions | T1 Score | T2 Score | p value | ||
|---|---|---|---|---|---|
| M | ±SD | M | ±SD | ||
| Right eye | 104.26 | 6.75 | 101.87 | 3.7 | .03* |
| Left eye | 105.83 | 11.35 | 102.01 | 4.23 | .03* |
| Head | 105.26 | 7.9 | 104.38 | 13.09 | .01* |
| Neck | 117.15 | 25.74 | 105.44 | 14.18 | .002* |
| Right shoulder | 106.38 | 20.07 | 101.79 | 5.15 | .57 |
| Left shoulder | 102.43 | 4.73 | 101.52 | 3.98 | .34 |
| Upper back | 110.86 | 18.17 | 104.09 | 9.8 | .005* |
| Lower back | 111.18 | 19.38 | 104.95 | 10.1 | .009* |
| Right arm | 104.16 | 14.01 | 101.56 | 5.02 | .15 |
| Left arm | 100.93 | 2.9 | 101.01 | 2.6 | .94 |
| Right elbow | 102.08 | 6.47 | 100.85 | 2.92 | .48 |
| Left elbow | 101.03 | 5.32 | 100.67 | 2.05 | .09 |
| Right forearm | 104.3 | 15.61 | 101.33 | 3.63 | .86 |
| Left forearm | 100.39 | 1.34 | 100.57 | 1.66 | .33 |
| Right wrist | 107.1 | 16.24 | 102.55 | 5.79 | .04* |
| Left wrist | 101.62 | 7.84 | 100.99 | 2.51 | .19 |
| Hips/buttocks | 108.43 | 19.9 | 103.33 | 11.64 | .01* |
| Right thigh | 102.33 | 11.83 | 101.8 | 8.54 | .66 |
| Left thigh | 102.33 | 11.83 | 102.17 | 9.7 | .79 |
| Right knee | 103.32 | 8.36 | 101.26 | 3.63 | .25 |
| Left knee | 101.66 | 4.32 | 100.62 | 1.28 | .89 |
| Right calf | 100.2 | 0.68 | 100.76 | 2.9 | .18 |
| Left calf | 100.18 | 0.66 | 100.73 | 2.9 | .17 |
| Right ankle/foot | 102.48 | 10.78 | 100.89 | 2.55 | .68 |
| Left ankle/Foot | 100.25 | 0.87 | 100.76 | 2.15 | .12 |
Note. Mean (M) ± standard deviation (SD) differences between pre (T1) and post (T2) measurement times are compared withing the yoga group. Bold font and * indicate significant values, α = .05. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
CMDQ Frequency, Severity, and Interference for the Yoga Group
For the yoga group, the frequency of musculoskeletal discomfort before and after the end of the intervention program is presented in Table 3. Body areas for which a statistically significant reduction (p < .05) in complaints frequency between T1 and T2 was observed were the neck (75.4% vs. 66.7%), upper back (67.2% vs. 53.7%), and lower back (75.4% vs. 57.4%). Overall, very frequent complaints (“several times every day”) were reduced by more than 80% at the end of the yoga program.
Table 3.
Frequency of Symptoms Reported by the Yoga Group in the CMDQ
| Body Regions | Never | 1–2 Times Last Week | 3–4 Times Last Week | Once Every Day | Several Times Every Day | p value | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | ||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| Right eye | 28 | 45.9 | 31 | 57.4 | 19 | 31.2 | 15 | 27.8 | 2 | 3.3 | 1 | 1.9 | 12 | 19.7 | 6 | 11.1 | 0 | 0 | 1 | 1.9 | .20 |
| Left eye | 30 | 49.2 | 32 | 59.3 | 15 | 24.6 | 13 | 24.1 | 5 | 8.2 | 3 | 5.6 | 5 | 8.2 | 5 | 9.3 | 6 | 9.8 | 1 | 1.9 | .18 |
| Head | 19 | 31.2 | 26 | 48.2 | 33 | 54.1 | 21 | 38.9 | 7 | 11.5 | 6 | 11.1 | 2 | 3.3 | 0 | 0 | 0 | 0 | 1 | 1.9 | .11 |
| Neck | 15 | 24.6 | 18 | 33.3 | 17 | 27.9 | 22 | 40.7 | 11 | 18.0 | 7 | 13.0 | 7 | 11.5 | 5 | 9.3 | 11 | 18.0 | 2 | 3.7 | .02* |
| Right shoulder | 40 | 65.6 | 37 | 68.5 | 12 | 19.7 | 10 | 18.5 | 1 | 1.6 | 3 | 5.6 | 2 | 3.3 | 4 | 7.4 | 6 | 9.8 | 0 | 0 | .62 |
| Left shoulder | 36 | 59.0 | 35 | 64.8 | 17 | 27.9 | 13 | 24.1 | 3 | 4.9 | 5 | 9.3 | 3 | 4.9 | 1 | 1.9 | 2 | 3.3 | 0 | 0 | .48 |
| Upper back | 20 | 32.8 | 25 | 46.3 | 19 | 31.2 | 17 | 31.5 | 4 | 6.6 | 8 | 14.8 | 8 | 13.1 | 2 | 3.7 | 10 | 16.4 | 2 | 3.7 | .03* |
| Lower back | 15 | 24.6 | 23 | 42.6 | 24 | 39.3 | 16 | 29.6 | 8 | 13.1 | 10 | 18.5 | 7 | 11.5 | 4 | 7.4 | 7 | 11.5 | 1 | 1.9 | .04* |
| Right arm | 38 | 62.3 | 40 | 74.1 | 18 | 29.5 | 9 | 16.7 | 0 | 0 | 3 | 5.6 | 3 | 4.9 | 2 | 3.7 | 2 | 3.3 | 0 | 0 | .22 |
| Left arm | 45 | 73.8 | 41 | 75.9 | 14 | 23.0 | 8 | 14.8 | 0 | 0 | 4 | 7.4 | 2 | 3.3 | 1 | 1.9 | 0 | 0 | 0 | 0 | .93 |
| Right elbow | 52 | 85.3 | 41 | 75.9 | 2 | 3.3 | 9 | 16.7 | 4 | 6.6 | 3 | 5.6 | 1 | 1.6 | 1 | 1.9 | 2 | 3.3 | 0 | 0 | .32 |
| Left elbow | 55 | 90.2 | 42 | 77.8 | 3 | 4.9 | 9 | 16.7 | 1 | 1.6 | 3 | 5.6 | 1 | 1.6 | 0 | 0 | 1 | 1.6 | 0 | 0 | .09 |
| Right forearm | 45 | 73.8 | 40 | 74.1 | 10 | 16.4 | 9 | 16.7 | 3 | 4.9 | 2 | 3.7 | 0 | 0 | 3 | 5.6 | 3 | 4.9 | 0 | 0 | .95 |
| Left forearm | 53 | 86.9 | 42 | 77.8 | 8 | 13.1 | 11 | 20.4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1.9 | .19 |
| Right wrist | 28 | 45.9 | 30 | 55.6 | 17 | 27.9 | 14 | 25.9 | 6 | 9.8 | 5 | 9.3 | 4 | 6.6 | 4 | 7.4 | 6 | 9.8 | 1 | 1.9 | .21 |
| Left wrist | 51 | 83.6 | 37 | 68.5 | 6 | 9.8 | 12 | 22.2 | 2 | 3.3 | 3 | 5.6 | 1 | 1.6 | 1 | 1.9 | 1 | 1.6 | 1 | 1.9 | .07 |
| Hips/buttocks | 30 | 49.2 | 35 | 64.8 | 17 | 27.9 | 10 | 18.5 | 4 | 6.6 | 3 | 5.6 | 4 | 6.6 | 4 | 7.4 | 6 | 9.8 | 2 | 3.7 | .10 |
| Right thigh | 51 | 83.6 | 41 | 75.9 | 6 | 9.8 | 9 | 16.7 | 0 | 0 | 1 | 1.9 | 2 | 3.3 | 1 | 1.9 | 2 | 3.3 | 2 | 3.7 | .34 |
| Left thigh | 50 | 82.0 | 43 | 79.6 | 7 | 11.5 | 8 | 14.8 | 0 | 0 | 1 | 1.9 | 2 | 3.3 | 0 | 0 | 2 | 3.3 | 2 | 3.7 | .79 |
| Right knee | 39 | 63.9 | 37 | 68.5 | 11 | 18.0 | 12 | 22.2 | 5 | 8.2 | 3 | 5.6 | 3 | 4.9 | 2 | 3.7 | 3 | 4.9 | 0 | 0 | .42 |
| Left knee | 45 | 73.8 | 39 | 72.2 | 10 | 16.4 | 12 | 22.2 | 1 | 1.6 | 3 | 5.6 | 5 | 8.2 | 0 | 0 | 0 | 0 | 0 | 0 | .99 |
| Right calf | 55 | 90.2 | 44 | 81.5 | 5 | 8.2 | 7 | 13.0 | 1 | 1.6 | 2 | 3.7 | 0 | 0 | 1 | 1.9 | 0 | 0 | 0 | 0 | .17 |
| Left calf | 56 | 91.8 | 44 | 81.5 | 4 | 6.6 | 7 | 13.0 | 1 | 1.6 | 2 | 3.7 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1.9 | .10 |
| Right ankle/foot | 50 | 82.0 | 40 | 74.1 | 6 | 9.8 | 8 | 14.8 | 2 | 3.3 | 2 | 3.7 | 1 | 1.6 | 2 | 3.7 | 2 | 3.3 | 2 | 3.7 | .32 |
| Left ankle/foot | 55 | 90.2 | 42 | 77.8 | 5 | 8.2 | 8 | 14.8 | 0 | 0 | 2 | 3.7 | 1 | 1.6 | 0 | 0 | 0 | 0 | 2 | 3.7 | .06 |
Note. Sample size (n) and percentage of responses (%) are presented for pre (T1) and post (T2) measurement times for each response category. p values correspond to the comparison of total frequency scores between pre (T1) and post (T2) measurement times. Bold font and * indicate significant values, α = .05. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
The severity of musculoskeletal discomfort pre and post yoga program is presented in Table 4. Body areas for which a statistically significant difference (p < .05) in complaint severity between T1 and T2 was observed were the head, neck, upper back, lower back, and hips/buttocks. Most of the participants rated severity symptoms of moderately uncomfortable and very uncomfortable at baseline (T1), which were later reduced at the end of the yoga program for neck (56.5% vs. 31.4%), upper back (48.7% vs. 36.0%), lower back (53.3% vs. 33.3%), and hip/buttocks (46.7% vs. 31.3%).
Table 4.
Severity Symptoms Reported by the Yoga Group in the CMDQ
| Body Regions | Slightly Uncomfortable | Moderately Uncomfortable | Very Uncomfortable | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Right eye | 23 | 69.7 | 17 | 77.3 | 9 | 27.3 | 5 | 22.7 | 1 | 3.0 | 0 | 0 | .12 |
| Left eye | 20 | 66.7 | 14 | 73.7 | 9 | 30.0 | 5 | 26.3 | 1 | 3.3 | 0 | 0 | .11 |
| Head | 20 | 50.0 | 16 | 59.3 | 14 | 35.0 | 9 | 33.3 | 6 | 15.0 | 2 | 7.4 | .06 |
| Neck | 20 | 43.5 | 24 | 68.6 | 13 | 28.3 | 7 | 20.0 | 13 | 28.3 | 4 | 11.4 | .02* |
| Right shoulder | 14 | 66.7 | 13 | 76.5 | 4 | 19.1 | 2 | 11.8 | 3 | 14.3 | 2 | 11.8 | .66 |
| Left shoulder | 18 | 72.0 | 15 | 79.0 | 6 | 24.0 | 2 | 10.5 | 1 | 4.0 | 2 | 10.5 | .49 |
| Upper back | 21 | 51.2 | 16 | 64.0 | 14 | 34.2 | 7 | 28.0 | 6 | 14.6 | 2 | 8.0 | .01* |
| Lower back | 21 | 46.7 | 20 | 66.7 | 17 | 37.8 | 6 | 20.0 | 7 | 15.6 | 4 | 13.3 | .01* |
| Right arm | 14 | 63.6 | 11 | 78.6 | 7 | 31.8 | 1 | 7.1 | 1 | 4.6 | 2 | 14.3 | .21 |
| Left arm | 12 | 92.3 | 10 | 76.9 | 1 | 7.7 | 2 | 15.4 | 0 | 0 | 1 | 7.7 | .65 |
| Right elbow | 4 | 44.4 | 11 | 84.6 | 4 | 44.4 | 2 | 15.4 | 1 | 11.1 | 0 | 0 | .29 |
| Left elbow | 5 | 83.3 | 11 | 91.7 | 1 | 16.7 | 1 | 8.3 | 0 | 0.0 | 0 | 0 | .08 |
| Right forearm | 11 | 68.8 | 10 | 71.4 | 3 | 18.8 | 3 | 21.4 | 2 | 12.5 | 1 | 7.1 | .95 |
| Left forearm | 6 | 85.7 | 11 | 84.6 | 1 | 14.3 | 2 | 15.4 | 0 | 0 | 0 | 0 | .08 |
| Right wrist | 20 | 60.6 | 17 | 70.8 | 10 | 30.3 | 5 | 20.8 | 3 | 9.1 | 2 | 8.3 | .23 |
| Left wrist | 6 | 60.0 | 13 | 86.7 | 4 | 40.0 | 2 | 13.3 | 0 | 0 | 0 | 0 | .19 |
| Hips/buttocks | 16 | 53.3 | 11 | 68.8 | 10 | 33.3 | 2 | 12.5 | 4 | 13.3 | 3 | 18.8 | .02* |
| Right thigh | 6 | 60.0 | 8 | 72.7 | 3 | 30.0 | 2 | 18.2 | 1 | 10.0 | 1 | 9.1 | .63 |
| Left thigh | 7 | 63.6 | 9 | 75.0 | 3 | 27.3 | 2 | 16.7 | 1 | 9.1 | 1 | 8.3 | .62 |
| Right knee | 13 | 59.1 | 15 | 83.3 | 8 | 36.4 | 2 | 11.1 | 1 | 4.6 | 1 | 5.6 | .55 |
| Left knee | 9 | 56.3 | 15 | 93.8 | 7 | 43.8 | 1 | 6.3 | 0 | 0 | 0 | 0 | .96 |
| Right calf | 6 | 100.0 | 9 | 90.0 | 0 | 0 | 1 | 10.0 | 0 | 0 | 0 | 0 | .17 |
| Left calf | 5 | 100.0 | 10 | 100.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | .10 |
| Right ankle/foot | 8 | 72.7 | 12 | 85.7 | 1 | 9.1 | 2 | 14.3 | 2 | 18.2 | 0 | 0 | .36 |
| Left ankle/foot | 5 | 83.3 | 12 | 100.0 | 1 | 16.7 | 0 | 0 | 0 | 0 | 0 | 0 | .08 |
Note. Sample size (n) and percentage of responses (%) are presented for pre (T1) and post (T2) measurement times for each response category. p values correspond to the comparison of total severity scores between pre (T1) and post (T2) measurement times. Bold font and * indicate significant values, α = .05. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
The interference with work due to musculoskeletal discomfort pre and post yoga program is presented in Table 5. Overall, more than half of the participants (58.0%) reported that at least one musculoskeletal symptom slightly or substantially interfered with work. However, after the yoga program, interference was reduced to 32.5%. The body areas for which interference was significantly (p < .05) reduced at the end of the intervention period were head, neck, upper back, and lower back. For these body areas, the perception that symptoms substantially interfered with work decreased by more than 60%.
Table 5.
Interference With Work Reported by the Yoga Group in the CMDQ
| Body Regions | Not at All | Slightly Interfered | Substantially Interfered | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Right eye | 7 | 21.2 | 11 | 47.8 | 26 | 78.8 | 10 | 43.5 | 0 | 0 | 2 | 8.7 | .10 |
| Left eye | 9 | 30.0 | 10 | 50.0 | 21 | 70.0 | 9 | 45.0 | 0 | 0 | 1 | 5.0 | .12 |
| Head | 10 | 23.8 | 12 | 46.2 | 23 | 54.8 | 12 | 46.2 | 9 | 21.4 | 2 | 7.7 | .003* |
| Neck | 15 | 32.6 | 20 | 55.6 | 21 | 45.7 | 13 | 36.1 | 10 | 21.7 | 3 | 8.3 | .03* |
| Right shoulder | 11 | 52.4 | 14 | 82.4 | 7 | 33.3 | 2 | 11.8 | 3 | 14.3 | 1 | 5.9 | .50 |
| Left shoulder | 14 | 56.0 | 13 | 72.2 | 9 | 36.0 | 5 | 27.8 | 2 | 8.0 | 0 | 0 | .28 |
| Upper back | 14 | 34.2 | 13 | 46.4 | 23 | 56.1 | 14 | 50.0 | 4 | 9.8 | 1 | 3.6 | .04* |
| Lower back | 13 | 28.9 | 14 | 43.8 | 28 | 62.2 | 18 | 56.3 | 4 | 8.9 | 0 | 0 | .02* |
| Right arm | 9 | 39.1 | 11 | 73.3 | 11 | 47.8 | 4 | 26.7 | 3 | 13.0 | 0 | 0 | .13 |
| Left arm | 8 | 57.1 | 10 | 76.9 | 6 | 42.9 | 3 | 23.1 | 0 | 0 | 0 | 0 | 1.00 |
| Right elbow | 2 | 22.2 | 11 | 91.7 | 6 | 66.7 | 1 | 8.3 | 1 | 11.1 | 0 | 0 | .48 |
| Left elbow | 2 | 33.3 | 10 | 83.3 | 4 | 66.7 | 2 | 16.7 | 0 | 0 | 0 | 0 | .10 |
| Right forearm | 7 | 43.8 | 11 | 78.6 | 7 | 43.8 | 3 | 21.4 | 2 | 12.5 | 0 | 0 | .74 |
| Left forearm | 3 | 42.9 | 10 | 83.3 | 3 | 42.9 | 2 | 16.7 | 1 | 14.3 | 0 | 0 | .17 |
| Right wrist | 12 | 38.7 | 14 | 63.6 | 17 | 54.8 | 8 | 36.4 | 2 | 6.5 | 0 | 0 | .11 |
| Left wrist | 6 | 60.0 | 12 | 75.0 | 3 | 30.0 | 4 | 25.0 | 1 | 10.0 | 0 | 0 | .12 |
| Hips/buttocks | 14 | 46.7 | 9 | 56.3 | 13 | 43.3 | 7 | 43.8 | 3 | 10.0 | 0 | 0 | .02 |
| Right thigh | 7 | 70.0 | 10 | 90.9 | 2 | 20.0 | 1 | 9.1 | 1 | 10.0 | 0 | 0 | .66 |
| Left thigh | 8 | 80.0 | 10 | 83.3 | 1 | 10.0 | 2 | 16.7 | 1 | 10.0 | 0 | 0 | .45 |
| Right knee | 14 | 63.6 | 14 | 82.4 | 8 | 36.4 | 3 | 17.7 | 0 | 0 | 0 | 0 | .46 |
| Left knee | 11 | 68.8 | 15 | 93.8 | 5 | 31.3 | 1 | 6.3 | 0 | 0 | 0 | 0 | .87 |
| Right calf | 5 | 83.3 | 8 | 80.0 | 1 | 16.7 | 2 | 20.0 | 0 | 0 | 0 | 0 | .18 |
| Left calf | 4 | 80.0 | 8 | 80.0 | 1 | 20.0 | 2 | 20.0 | 0 | 0 | 0 | 0 | .10 |
| Right ankle/foot | 6 | 54.6 | 11 | 84.6 | 5 | 45.5 | 2 | 15.4 | 0 | 0 | 0 | 0 | .54 |
| Left ankle/foot | 5 | 83.3 | 11 | 91.7 | 1 | 16.7 | 1 | 8.3 | 0 | 0 | 0 | 0 | .08 |
Note. Sample size (n) and percentage of responses (%) are presented for pre (T1) and post (T2) measurement times for each response category. p values correspond to the comparison of total Interference scores between pre (T1) and post (T2) measurement times. Bold font and * indicate significant values, α = .05. CMDQ = Cornell Musculoskeletal Discomfort Questionnaire.
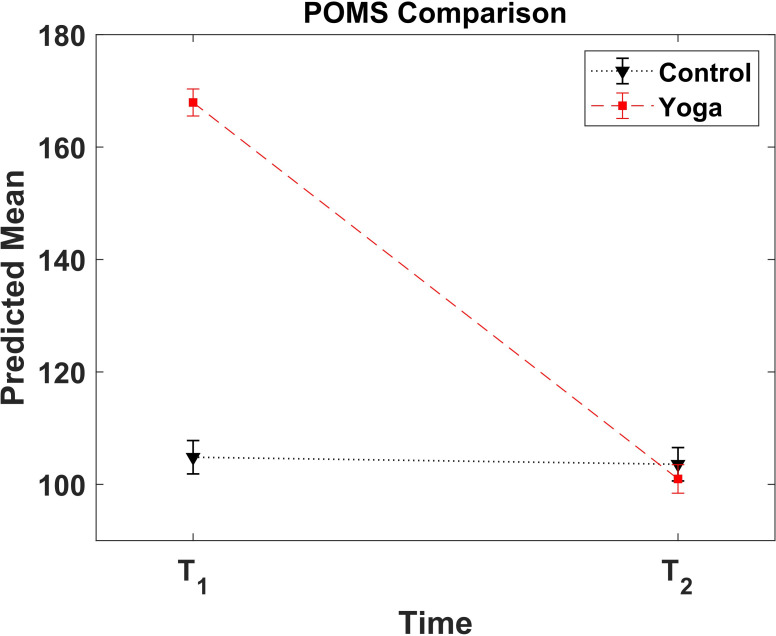
POMS Total Mood Scores
A significant interaction of time with group (F(1,92) = 283.11, p = .001) and a significant main effect for time (F(1,92) = 306.38, p = .001) and group (F(1,92) = 118.54, p = .001) were observed for the total mood scores. These scores were significantly higher for the yoga than the control group (p = .0001) at T1. For the yoga group, total mood scores were significantly lower (p = .001) at T2 than T1 (100.26 ± 19.36 vs. 166.11 ± 25.25); see Figure 2. However, for the control group, total mood scores were not significantly different (p = .66) between T2 and T1 (104.83 ± 10.40 vs. 103.53 ± 8.62).
Figure 2.
POMS score. Mean ± SD total mood score at pre (T1) and post (T2) measurement times for the yoga and control groups. POMS = Profile of Mood States questionnaire.
Discussion
The influence of daily 10-min yoga exercises on musculoskeletal discomfort and mood disturbance was evaluated after 1 month on office workers that were required to telework due to the COVID-19 pandemic. Decreases in discomfort of eyes, head, neck, upper back, lower back, right wrist, hips/buttocks, and mood disturbance indicate the mitigating influence of the yoga program on symptoms when compared to the absence of changes or even worsening of symptoms for the control group. Thus, a yoga program for home-office workers seems to have a positive impact on musculoskeletal and emotional health.
Initial Differences Between Groups
Despite some significant difference in CMDQ responses between groups (Figure 1) and an obvious difference in total mood scores (Figure 2) at T1, there may have been some kind of group difference before the period of the experiment. A few aspects were considered: many invitees (36) withdrew from the yoga group. Additionally, the control group included participants that apparently did not have time for yoga during the workday. Hence, it is highly likely that the yoga group included primarily participants that felt a stronger motivation/need to reduce their current discomfort and/or improve their well-being and benefit from a free intervention program while enduring the 1-month participation.
Musculoskeletal Discomfort
Based on the total musculoskeletal discomfort scores found in the present study, the difference between pre and post measurement was significantly greater for the yoga group than the control group for several body regions including eyes, neck, back area, right arm and wrist, thighs, and hips/buttocks. For the control group, the changes in total musculoskeletal discomfort scores from baseline (T1) to post measurement (T2) were not significant (Figure 1). However, significant reductions of total musculoskeletal discomfort scores for the eyes, head, neck, upper and lower back, right wrist, and hips/buttocks were observed for the yoga group. Similar benefits of yoga exercises for office workers have been observed. They include a reduction of back pain (Hartfiel et al., 2012) in blue collar workers, and a decrease of neck pain (Joshi & Bellad, 2011), and visual discomfort (Telles et al., 2006) in computer users. In prolonged occupational seated work, the major body areas affected by musculoskeletal discomfort, which progress onto clinical disorders, are the neck (Waersted et al., 2010), back (Lis et al., 2007; Tissot et al., 2009), and hip/thigh/buttock (Baker et al., 2018).
The present study indicates that a 1-month yoga program for home-office workers contributed to a large reduction of musculoskeletal discomfort in these body areas. Thus, ergonomic intervention strategies aiming at reducing and disrupting prolonged postures, complemented by adapted yoga exercises should be given serious consideration, as possible preventive measures for musculoskeletal discomfort. In the long term, discomfort and symptom reduction is likely to contribute to the prevention of MSDs. This perspective is supported by studies showing a reduction of muscle fatigue, an acknowledged precursor of MSDs (Côté, 2014; Gallagher & Schall, 2017; Hadrevi et al., 2019; Sejersted & Sjøgaard, 2000) by intermittent (Falla & Farina, 2007; Farina et al., 2008) or sporadic changes in muscle contraction (Martin et al., 2019). Moreover, reduction of right wrist discomfort may also be beneficial in reducing the potential risk of carpal tunnel syndrome. (Garfinkel et al., 1998). Garinkel et al. investigated the effect of yoga to alleviate the pain caused by carpal tunnel syndrome. The authors found that the yoga group exhibited a significant grip strength improvement and pain reduction, while the control group did not show any significant change. It is worth emphasizing that the asymmetric improvement, for right wrist only, is not surprising, as most humans are right-handed and use the mouse or other pointing devices with their dominant hand. They also preferentially use that hand for a range of manipulations.
The frequency of complaints was also reduced by the yoga program, particularly in the neck and back, which are areas mostly affected by prolonged seated work (Celik et al., 2018). Concurrently, the moderately and very uncomfortable levels in the severity category were also reduced by the yoga program. In addition, musculoskeletal discomfort, which slightly or substantially interfered with work performance, was also reduced. This latter effect is most likely a consequence of all the reductions indicated above and strengthens the significance of the intervention. Thus, the 1month yoga program presented a benefit in all three categories of musculoskeletal discomfort scores. As stated above, the effects on the musculoskeletal system are most likely resulting from the significant disruptions of prolonged monotonic muscle contraction (Falla & Farina, 2007; Farina et al., 2008) by yoga exercises. These changes in muscle contractions and thus muscle recruitment patterns are unlikely to be occurring in the control group, as more participants in this group mentioned a lack of time for extra activities during the workdays.
Mood Disturbance
The level of mental distortion at the beginning of the program was higher for the yoga than control group. The much lower level observed at the end of the experiment illustrates the positive mental effects of yoga exercises. Conversely, the total mood scores of the control group did not change during this period. Having a daily exercise routine, where the mind changes to a state of relaxation, has been reported to improve mental well-being and other quality of life aspects (Gard et al., 2012; Taspinar et al., 2014; Telles et al., 2019; Tulloch et al., 2018). Furthermore, meditation has been associated with the release of neurotransmitters modulating psychological disorders and anxiety (e.g., Krishnakumar et al., 2015; Sharma, 2015, for review). Consequently, our result agrees with previous studies (Gard et al., 2012; Taspinar et al., 2014; Tulloch et al., 2018), pointing out that state of mind is influenced by lack of both physical and mental rest. de Bruin et al. (2017) combined physical exercise, yoga, and mindfulness to produce beneficial effects on work-related diseases and perceived stress. Their premise concurs with the present study, as it could also produce a feeling of balance and well-being in each participant through the active 10-min break, such that their mind is temporarily free of workload and stress. The current persisting global pandemic brings a great deal of uncertainty and stress in many ways (Brooks et al., 2020; Lin et al., 2020). Pandemic crises are so fluid that plans must often change rapidly (Liang et al., 2020). Thus, implementing a yoga program to mitigate musculoskeletal discomfort and emotional stress during the prolonged COVID-19 pandemic may be of benefit to office workers working from home.
As could be expected, those more affected by symptoms appear more likely to participate in an intervention and do exercises that disrupt muscular monotony and have benefits. When taken together, the reduction of headache, complaints related to the musculoskeletal system, and mood improvement support the claimed effects of yoga on physical and mental systems (de Bruin et al., 2017; Puerto Valencia et al., 2019). They are also in agreement with the ancient philosophy of yoga (Prabhu & Bhat, 2013), which emphasizes the mind–body monism proposed by the philosopher Spinoza in the 17th century (Spinoza & Curley, 2016) and now supported by neuroscience (Damasio, 1994).
Study Limitations
The results are interpreted in light of some limitations. They show that a 10-min exercise break can alleviate symptoms but do not imply that 1 month is sufficient to prevent MSDs. Thus, care should be taken in generalizing these findings to sustained/regular interventions. Further research is necessary to investigate the long terms benefits, particularly the function of adapted active breaks. Second, this study took place during a pandemic context in which the “distraction/ attraction” attributed to the intervention may not have the same effect in a “normal” situation. Moreover, factors like work–life balance, job demands, leisure activities, and household duties may have changed during the pandemic. Although participants were requested to maintain their common routines during the experimental period, the influence of these factors is unknown and would be of interest in future studies. However, since group attribution was largely randomized, it may be cautiously presumed that pandemic-induced burdens were similar between groups and did not significantly affect the results. Third, the work environment could not be controlled. Hence, large variations in equipment/tools and workstation design were expected. Beside inherent individual differences, this may have led to variations in symptom locus, frequency, and severity. The recommendations to perform yoga exercises during the work periods could not be controlled. Hence, it is possible that some participants waited till the end of the day to attend to the routine, which may have been less efficient than interruptions of the ongoing work activities. Although an initial bias may have differentiated, to some extent, the initial health status of the groups and their motivation as well as the benefits of the yoga program are consistent over all measures. The active break principle, combining mind and body, appears effective, but generalization to different types of work would require adaptation.
Conclusions
A 1-month yoga intervention program significantly reduced CMDQ discomfort scores of eyes, head, neck, upper and lower back, right wrist, and hips/buttocks, and POMS total mood scores of home-office workers during the COVID-19 pandemic. These measures were not significantly altered in the control group that performed their regular work without any intervention. Musculoskeletal discomfort and emotional disturbance seem to be effectively reduced with 10 min of daily yoga exercises during the workday. It could be speculated that enforcing exercise breaks during the work hours would produce equal outcomes. However, such intervention types do not preclude, or should be used in lieu of, standard ergonomic improvements in working conditions.
Key Points
Musculoskeletal discomfort and mood disturbance were significantly reduced after a 1-month yoga intervention program for home-office workers.
Mood disturbance scores and most musculoskeletal discomfort scores did not change for the control group, as expected.
Daily 10-min yoga exercises seem to have had a positive influence on physical and emotional discomfort of home-office workers during the COVID-19 pandemic.
Supplemental Material
Supplemental material, Online supplementary file 1, for Impact of 10-Min Daily Yoga Exercises on Physical and Mental Discomfort of Home-Office Workers During COVID-19 by Maria-Gabriela Garcia, Melany Estrella, Angie Peñafiel, Paul G. Arauz and Bernard J. Martin in Human Factors: The Journal of Human Factors and Ergonomics Society
Acknowledgments
The authors thank Edison Estrella and Jose Alvaro from AEM Solutions for their assistance with the yoga program web platform; Daniel Silva for his contribution with the yoga program exercises; and Maggie Graf for her collaboration on the final draft.
Author Biographies
Maria-Gabriela Garcia is an associate professor in the Department of Industrial Engineering at the Universidad San Francisco de Quito. She received her DSc in health sciences and technology in 2017 from ETH Zürich, Switzerland.
Melany Estrella is a research collaborator at the Department of Industrial Engineering at the Universidad San Francisco de Quito. She received her industrial engineering degree in 2020 from Universidad San Francisco de Quito, Ecuador.
Angie Peñafiel is a research collaborator at the Department of Industrial Engineering at the Universidad San Francisco de Quito. She received her industrial engineering degree in 2020 from Universidad San Francisco de Quito, Ecuador.
Paul G. Arauz is an assistant professor in the Department of Mechanical Engineering at the Universidad San Francisco de Quito. He received his PhD in mechanical engineering in 2016 from the State University of New York at Stony Brook and held a two-year Post-Doctoral Research Fellow position at the Massachusetts General Hospital and Harvard Medical School in 2017.
Bernard J. Martin is a professor in the Department of Industrial and Operations Engineering at the University of Michigan, USA, and holds a research fellow appointment in the School of Kinesiology and is an affiliate faculty of the Department of Biomedical Engineering. He was awarded a PhD in bioengineering in 1981 and a doctor of science degree in life science in 1989 from the University of Provence, France.
Footnotes
Supplemental Material: The online supplemental material is available with the manuscript on the HF website.
ORCID iD
Maria-Gabriela Garcia https://orcid.org/0000-0002-5666-2156
References
- Abdin S., Welch R. K., Byron-Daniel J., Meyrick J. (2018). The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health, 160, 70–76. 10.1016/j.puhe.2018.03.029 [DOI] [PubMed] [Google Scholar]
- Andersen C. H., Andersen L. L., Gram B., Pedersen M. T., Mortensen O. S., Zebis M. K., Sjøgaard G. (2012). Influence of frequency and duration of strength training for effective management of neck and shoulder pain: A randomised controlled trial. British Journal of Sports Medicine, 46, 1004–1010. 10.1136/bjsports-2011-090813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen L. L., Jørgensen M. B., Blangsted A. K., Pedersen M. T., Hansen E. A., Sjøgaard G. (2008). A randomized controlled intervention trial to relieve and prevent neck/shoulder pain. Medicine & Science in Sports & Exercise, 40, 983–990. 10.1249/MSS.0b013e3181676640 [DOI] [PubMed] [Google Scholar]
- Andrade E., Arce C., De Francisco C., Torrado J., Garrido J. (2013). Versión breve en español del cuestionario POMS para deportistas adultos y población general1. Revista de Psicologia Del Deporte, 22, 95–102. [Google Scholar]
- Axén I., Follin G. (2017). Medical yoga in the workplace setting-perceived stress and work ability-a feasibility study. Complementary Therapies in Medicine, 30, 61–66. 10.1016/j.ctim.2016.12.001 [DOI] [PubMed] [Google Scholar]
- Baker R., Coenen P., Howie E., Williamson A., Straker L. (2018). The short term musculoskeletal and cognitive effects of prolonged sitting during office computer work. International Journal of Environmental Research and Public Health, 15, 1678. 10.3390/ijerph15081678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan S. (2015). Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Practice & Research Clinical Rheumatology, 29, 356–373. 10.1016/j.berh.2015.08.002 [DOI] [PubMed] [Google Scholar]
- Bhattacharya A. (2014). Costs of occupational musculoskeletal disorders (MSDs) in the United States. International Journal of Industrial Ergonomics, 44, 448–454. [Google Scholar]
- Birditt K. S., Turkelson A., Fingerman K. L., Polenick C. A., Oya A. (2021). Age differences in stress, life changes, and social ties during the COVID-19 pandemic: Implications for psychological well-being. The Gerontologist, 61, 205–216. 10.1093/geront/gnaa204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff L. L., Otto A.-K., Hold C., Wollesen B. (2019). The effect of physical activity interventions on occupational stress for health personnel: A systematic review. International Journal of Nursing Studies, 97, 94–104. 10.1016/j.ijnurstu.2019.06.002 [DOI] [PubMed] [Google Scholar]
- Blangsted A. K., Søgaard K., Hansen E. A., Hannerz H., Sjøgaard G. (2008). One-year randomized controlled trial with different physical-activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scandinavian Journal of Work, Environment & Health, 34, 55–65. 10.5271/sjweh.1192 [DOI] [PubMed] [Google Scholar]
- BLS . (2020). Fact Sheet | Occupational injuries and illnesses resulting in musculoskeletal disorders (MSDs) | May 2020. [Google Scholar]
- Bongers P. M., de Winter C. R., Kompier M. A., Hildebrandt V. H. (1993). Psychosocial factors at work and musculoskeletal disease. Scandinavian Journal of Work, Environment & Health, 19, 297–312. 10.5271/sjweh.1470 [DOI] [PubMed] [Google Scholar]
- Bontrup C., Taylor W. R., Fliesser M., Visscher R., Green T., Wippert P.-M., Zemp R. (2019). Low back pain and its relationship with sitting behaviour among sedentary office workers. Applied Ergonomics, 81, 102894. 10.1016/j.apergo.2019.102894 [DOI] [PubMed] [Google Scholar]
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brynjolfsson E., Horton J. J., Ozimek A., Rock D., Sharma G., TuYe H. (2020). Covid-19 and remote work: An early look at US data (working paper # 27344). Climate Change 2013 - The Physical Science Basis, 1–30.doi:https://www.nber.org/papers/w27344 [Google Scholar]
- Cabral A. M., de Moreira R. F. C., de Barros F. C., de Sato T. O., Sato T., de O. (2019). Is physical capacity associated with the occurrence of musculoskeletal symptoms among office workers? A cross-sectional study. International Archives of Occupational and Environmental Health, 92, 1159–1172. 10.1007/s00420-019-01455-y [DOI] [PubMed] [Google Scholar]
- Callaghan J. P., De Carvalho D., Gallagher K., Karakolis T., Nelson-Wong E. (2015). Is standing the solution to sedentary office work? Ergonomics in Design: The Quarterly of Human Factors Applications, 23, 20–24. 10.1177/1064804615585412 [DOI] [Google Scholar]
- Carrasquero E. (2015). Spanish adaptation and validation of Cornell musculoskeletal discomfort questionnaire (CDMQ). [Conference session]. Conference Proceeding Universidad de las Fuerzas Armadas, Panama. [Google Scholar]
- Casey L. J., Van Rooy K. M., Sutherland S. J., Jenkins S. M., Rosedahl J. K., Wood N. G., Ebbert J. O., Lopez-Jimenez F., Egginton J. S., Sim L. A., Clark M. M. (2018). Improved self-acceptance, quality of life, and stress level from participation in a worksite yoga foundations program: A pilot study. International Journal of Yoga Therapy, 28, 15–21. 10.17761/2018-00013R2 [DOI] [PubMed] [Google Scholar]
- Celik S., Celik K., Dirimese E., Taşdemir N., Arik T., Büyükkara İ. (2018). Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. International Journal of Occupational Medicine and Environmental Health, 31, 91–111. 10.13075/ijomeh.1896.00901 [DOI] [PubMed] [Google Scholar]
- Chou R., Deyo R., Friedly J., Skelly A., Hashimoto R., Weimer M., Fu R., Dana T., Kraegel P., Griffin J., Grusing S., Brodt E. D. (2017). Nonpharmacologic therapies for low back pain: A systematic review for an American College of physicians clinical practice guideline. Annals of Internal Medicine, 166, 493–505. 10.7326/M16-2459 [DOI] [PubMed] [Google Scholar]
- Cocchiara R. A., Peruzzo M., Mannocci A., Ottolenghi L., Villari P., Polimeni A., Guerra F., La Torre G. (2019). The use of yoga to manage stress and burnout in healthcare workers: A systematic review. Journal of Clinical Medicine, 8, 284. 10.3390/jcm8030284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coenen P., Healy G. N., Winkler E. A. H., Dunstan D. W., Owen N., Moodie M., LaMontagne A. D., Eakin E. A., O’Sullivan P. B., Straker L. M. (2018). Associations of office workers objectively assessed occupational sitting, standing and stepping time with musculoskeletal symptoms. Ergonomics, 61, 1187–1195. 10.1080/00140139.2018.1462891 [DOI] [PubMed] [Google Scholar]
- Collins J. D., O’Sullivan L. W. (2015). Musculoskeletal disorder prevalence and psychosocial risk exposures by age and gender in a cohort of office based employees in two academic institutions. International Journal of Industrial Ergonomics, 46, 85–97. 10.1016/j.ergon.2014.12.013 [DOI] [Google Scholar]
- Côté J. N. (2014). Adaptations to neck/shoulder fatigue and injuries. In Levin M. F. (Ed.), Progress in motor control (Vol. 826, pp. 205–228). Springer. [Google Scholar]
- Cramer H., Klose P., Brinkhaus B., Michalsen A., Dobos G. (2017). Effects of yoga on chronic neck pain: A systematic review and meta-analysis. Clinical Rehabilitation, 31, 1457–1465. 10.1177/0269215517698735 [DOI] [PubMed] [Google Scholar]
- Cramer H., Lauche R., Haller H., Dobos G. (2013). A systematic review and meta-analysis of yoga for low back pain. Clinical J Pain, 29, 1–11. [DOI] [PubMed] [Google Scholar]
- Damasio A. R. (1994). Descartes’ error : Emotion, reason, and the human brain. G.P. Putnam. [Google Scholar]
- Daneshmandi H., Choobineh A., Ghaem H., Karimi M. (2017). Adverse effects of prolonged sitting behavior on the general health of office workers. Journal of Lifestyle Medicine, 7, 69–75. 10.15280/jlm.2017.7.2.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin E. I., Formsma A. R., Frijstein G., Bögels S. M. (2017). Mindful2Work: Effects of combined physical exercise, yoga, and mindfulness meditations for stress relieve in employees. A proof of concept study. Mindfulness, 8, 204–217. 10.1007/s12671-016-0593-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Manincor M., Bensoussan A., Smith C., Fahey P., Bourchier S. (2015). Establishing key components of yoga interventions for reducing depression and anxiety, and improving well-being: A Delphi method study. BMC Complementary and Alternative Medicine, 15, 1–10. 10.1186/s12906-015-0614-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeney C., O’Sullivan L. (2009). Work related psychosocial risks and musculoskeletal disorders: Potential risk factors, causation and evaluation methods. Work, 34, 239–248. 10.3233/WOR-2009-0921 [DOI] [PubMed] [Google Scholar]
- Della Valle E., Palermi S., Aloe I., Marcantonio R., Spera R., Montagnani S., Sirico F. (2020). Effectiveness of workplace yoga interventions to reduce perceived stress in employees: A systematic review and meta-analysis. Journal of Functional Morphology and Kinesiology, 5, E33, 33. 10.3390/jfmk5020033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dos Santos C. F., Picó-Pérez M., Morgado P. (2020). COVID-19 and mental health-what do we know so far? Frontiers in Psychiatry, 11, 565698. 10.3389/fpsyt.2020.565698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeverria L. (2020). El teletrabajo aumentó en un 109%. Criterios Digital. www.criteriosdigital.com
- Etikan I., Bala K. (2017). Sampling and sampling methods. Biometrics & Biostatistics International Journal, 5, 215–217. 10.15406/bbij.2017.05.00149 [DOI] [Google Scholar]
- Falla D., Farina D. (2007). Periodic increases in force during sustained contraction reduce fatigue and facilitate spatial redistribution of trapezius muscle activity. Experimental Brain Research, 182, 99–107. 10.1007/s00221-007-0974-4 [DOI] [PubMed] [Google Scholar]
- Farina D., Leclerc F., Arendt-Nielsen L., Buttelli O., Madeleine P. (2008). The change in spatial distribution of upper trapezius muscle activity is correlated to contraction duration. Journal of Electromyography and Kinesiology, 18, 16–25. 10.1016/j.jelekin.2006.08.005 [DOI] [PubMed] [Google Scholar]
- Feuerstein G. (2001). The yoga tradition: Its history, literature, philosophy, and practice. Hohm Press. [Google Scholar]
- Galinsky T., Swanson N., Sauter S., Dunkin R., Hurrell J., Schleifer L. (2007). Supplementary breaks and stretching exercises for data entry operators: A follow-up field study. American Journal of Industrial Medicine, 50, 519–527. 10.1002/ajim.20472 [DOI] [PubMed] [Google Scholar]
- Gallagher S., Schall M. C. (2017). Musculoskeletal disorders as a fatigue failure process: Evidence, implications and research needs. Ergonomics, 60, 255–269. 10.1080/00140139.2016.1208848 [DOI] [PubMed] [Google Scholar]
- Gard T., Brach N., Hölzel B. K., Noggle J. J., Conboy L. A., Lazar S. W. (2012). Effects of a yoga-based intervention for young adults on quality of life and perceived stress: The potential mediating roles of mindfulness and self-compassion. The Journal of Positive Psychology, 7, 165–175. 10.1080/17439760.2012.667144 [DOI] [Google Scholar]
- Garfinkel M. S., Singhal A., Katz W. A., Allan D. A., Reshetar R., Schumacher H. R. (1998). Yoga-based intervention for carpal tunnel syndrome: A randomized trial. JAMA, 280, 1601–1603. 10.1001/jama.280.18.1601 [DOI] [PubMed] [Google Scholar]
- Gowrisankaran S., Sheedy J. E. (2015). Computer vision syndrome: A review. Work, 52, 303–314. 10.3233/WOR-152162 [DOI] [PubMed] [Google Scholar]
- Hadrevi J., Barbe M. F., Ørtenblad N., Frandsen U., Boyle E., Lazar S., Sjøgaard G., Søgaard K. (2019). Calcium fluxes in work-related muscle disorder: Implications from a rat model. BioMed Research International, 2019, 1–14. 10.1155/2019/5040818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcombe H., McBride D., Derrett S., Gray A. (2009). Prevalence and impact of musculoskeletal disorders in New Zealand nurses, postal workers and office workers. Australian and New Zealand Journal of Public Health, 33, 437–441. 10.1111/j.1753-6405.2009.00425.x [DOI] [PubMed] [Google Scholar]
- Hartfiel N., Burton C., Rycroft-Malone J., Clarke G., Havenhand J., Khalsa S. B., Edwards R. T. (2012). Yoga for reducing perceived stress and back pain at work. Occupational Medicine, 62, 606–612. 10.1093/occmed/kqs168 [DOI] [PubMed] [Google Scholar]
- Hedge A., Morimoto S., McCrobie D. (1999). Effects of keyboard tray geometry on upper body posture and comfort. Ergonomics, 42, 1333–1349. 10.1080/001401399184983 [DOI] [PubMed] [Google Scholar]
- Ilić I. M., Arandjelović Mirjana Ž., Jovanović J. M., Nešić M. M. (2017). Relationships of work-related psychosocial risks, stress, individual factors and burnout - Questionnaire survey among emergency physicians and nurses. Medycyna Pracy, 68, 167–178. 10.13075/mp.5893.00516 [DOI] [PubMed] [Google Scholar]
- Jepsen J. R., Thomsen G. (2008). Prevention of upper limb symptoms and signs of nerve afflictions in computer operators: The effect of intervention by stretching. Journal of Occupational Medicine and Toxicology, 3, 1. 10.1186/1745-6673-3-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi V. S., Bellad A. S. (2011). Effect of yogic exercises on symptoms of musculoskeletal disorders of upper limbs among computer users: A randomised controlled trial. Indian Journal of Medical Sciences, 65, 424–428. 10.4103/0019-5359.109256 [DOI] [PubMed] [Google Scholar]
- Krishnakumar D., Hamblin M. R., Lakshmanan S. (2015). Meditation and yoga can modulate brain mechanisms that affect behavior and Anxiety-A modern scientific perspective. Ancient Science, 2, 13–19. 10.14259/as.v2i1.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon Y., Kim J.-W., Heo J.-H., Jeon H.-M., Choi E.-B., Eom G.-M. (2018). The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technology and Health Care, 26, 409–418. 10.3233/THC-174717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacaze D. H. C., Sacco C. N., Rocha L. E., Pereira C. B., Casarotto R. A. (2010). Stretching and joint mobilization exercises reduce call-center operators’ musculoskeletal discomfort and fatigue. Clinics, 65, 657–662. 10.1590/S1807-59322010000700003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Li S., Jiang J., Yuan S. (2019). Effects of yoga on patients with chronic nonspecific neck pain; A prisma systematic review and meta-analysis. Medicine, 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Z. C., Ooi S. B. S., Wang W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95, 1359–1361. 10.1097/ACM.0000000000003441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin D., Friedman D. B., Qiao S., Tam C. C., Li X., Li X. (2020). Information uncertainty: A correlate for acute stress disorder during the COVID-19 outbreak in China. BMC Public Health, 20, 1867. 10.1186/s12889-020-09952-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S., Hsiao Y.-Y., Wang M. (2014). Test review: The profile of mood states 2nd edition. Journal of Psychoeducational Assessment, 32, 273–277. 10.1177/0734282913505995 [DOI] [Google Scholar]
- Lis A. M., Black K. M., Korn H., Nordin M. (2007). Association between sitting and occupational LBP. European Spine Journal, 16, 283–298. 10.1007/s00586-006-0143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux R. E., Daukantaité D., Tellhed U. (2018). The effects of yoga on stress and psychological health among employees: An 8- and 16-week intervention study. Anxiety, Stress, & Coping, 31, 121–134. 10.1080/10615806.2017.1405261 [DOI] [PubMed] [Google Scholar]
- Martin B. J., Botter A., Soedirdjo S. D. H., Kim D. G., Nicolletti C., Wild P., Laubli T. (2019). Pain in the neck: A likely neuromuscular control issue; trapezius contraction patterns. Annual Australian Institute of Health and Safety Conference. [Google Scholar]
- McNair D., Lorr M., Droppleman L. (1971). Manual for the profile of mood states. Educational and Industrial Testing Service. [Google Scholar]
- Nussbaumer-Streit B., Mayr V., Dobrescu A., Chapman A., Persad E., Klerings I., Gartlehner G. (2020). Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database of Systematic Reviews, 4, 1–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. (2020). Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company ’ S public news and information, (January).
- Pinto A. J., Dunstan D. W., Owen N., Bonfá E., Gualano B. (2020). Combating physical inactivity during the COVID-19 pandemic. Nature Reviews Rheumatology, 16, 347–348. 10.1038/s41584-020-0427-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piranveyseh P., Motamedzade M., Osatuke K., Mohammadfam I., Moghimbeigi A., Soltanzadeh A., Mohammadi H. (2016). Association between psychosocial, organizational and personal factors and prevalence of musculoskeletal disorders in office workers. International Journal of Occupational Safety and Ergonomics, 22, 267–273. 10.1080/10803548.2015.1135568 [DOI] [PubMed] [Google Scholar]
- Prabhu H. R. A., Bhat P. S. (2013). Mind and consciousness in yoga - Vedanta: A comparative analysis with western psychological concepts. Indian Journal of Psychiatry, 55, S182–186. 10.4103/0019-5545.105524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puerto Valencia L. M., Weber A., Spegel H., Bögle R., Selmani A., Heinze S., Herr C. (2019). Yoga in the workplace and health outcomes: A systematic review. Occupational Medicine, 69, 163–176. [DOI] [PubMed] [Google Scholar]
- Rodrigues M. S., Leite R. D. V., Lelis C. M., Chaves T. C. (2017). Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work, 57, 563–572. 10.3233/WOR-172582 [DOI] [PubMed] [Google Scholar]
- Sejersted O. M., Sjøgaard G. (2000). Dynamics and consequences of potassium shifts in skeletal muscle and heart during exercise. Physiological Reviews, 80, 1411–1481 10.1152/physrev.2000.80.4.1411 [DOI] [PubMed] [Google Scholar]
- Sharma H. (2015). Meditation: Process and effects. Ayu, 36, 233–237. 10.4103/0974-8520.182756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjögren T., Nissinen K. J., Järvenpää S. K., Ojanen M. T., Vanharanta H., Mälkiä E. A. (2005). Effects of a workplace physical exercise intervention on the intensity of headache and neck and shoulder symptoms and upper extremity muscular strength of office workers: A cluster randomized controlled cross-over trial. Pain, 116, 119–128. 10.1016/j.pain.2005.03.031 [DOI] [PubMed] [Google Scholar]
- Slater S. J., Christiana R. W., Gustat J. (2020). Recommendations for keeping Parks and green space accessible for mental and physical health during COVID-19 and other pandemics. Preventing Chronic Disease, 17, 1–5. 10.5888/pcd17.200204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M. J., Carayon P. (1996). Work organization, stress, and cumulative trauma disorder. In Moon S. (Ed.), Beyond biomechanics: Psychosocial factors and musculoskeletal disorders in office work (pp. 23–42). Taylor & Francis. [Google Scholar]
- Spinoza Bde., Curley E. (2016). The collected works of Spinoza (Vol. II). Princeton University Press. [Google Scholar]
- Sprigg C. A., Stride C. B., Wall T. D., Holman D. J., Smith P. R. (2007). Work characteristics, musculoskeletal disorders, and the mediating role of psychological strain: A study of call center employees. Journal of Applied Psychology, 92, 1456–1466. 10.1037/0021-9010.92.5.1456 [DOI] [PubMed] [Google Scholar]
- Taspinar B., Aslan U. B., Agbuga B., Taspinar F. (2014). A comparison of the effects of hatha yoga and resistance exercise on mental health and well-being in sedentary adults: A pilot study. Complementary Therapies in Medicine, 22, 433–440. 10.1016/j.ctim.2014.03.007 [DOI] [PubMed] [Google Scholar]
- Telles S., Gupta R. K., Kumar A., Pal D. K., Tyagi D., Balkrishna A. (2019). Mental wellbeing, quality of life, and perception of chronic illness in yoga-experienced compared with yoga-naïve patients. Medical Science Monitor Basic Research, 25, 153–163. 10.12659/MSMBR.914663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telles S., Naveen K., Dash M., Deginal R., Manjunath N. K. (2006). Effect of yoga on self-rated visual discomfort in computer users. Head & Face Medicine, 2, 46. 10.1186/1746-160X-2-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tissot F., Messing K., Stock S. (2009). Studying the relationship between low back pain and working postures among those who stand and those who sit most of the working day. Ergonomics, 52, 1402–1418. 10.1080/00140130903141204 [DOI] [PubMed] [Google Scholar]
- Torres W. (2020). 306.000 ecuatorianos están teletrabajando emergencia sanitaria. Primicias. [Google Scholar]
- Tsopanidou A. Α., Venetsanou F. D., Stavridis I. S., Paradisis G. P., Zacharogiannis E. G. (2020). Energy expenditure during a Vinyasa yoga session. The Journal of Sports Medicine and Physical Fitness, 60, 1110–1117. 10.23736/S0022-4707.20.10821-1 [DOI] [PubMed] [Google Scholar]
- Tulloch A., Bombell H., Dean C., Tiedemann A. (2018). Yoga-based exercise improves health-related quality of life and mental well-being in older people: A systematic review of randomised controlled trials. Age and Ageing, 47, 537–544. 10.1093/ageing/afy044 [DOI] [PubMed] [Google Scholar]
- Van Eerd D., Munhall C., Irvin E., Rempel D., Brewer S., van der Beek A. J., Dennerlein J. T., Tullar J., Skivington K., Pinion C., Amick B. (2016). Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occupational and Environmental Medicine, 73, 62–70. 10.1136/oemed-2015-102992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waersted M., Hanvold T. N., Veiersted K. B. (2010). Computer work and musculoskeletal disorders of the neck and upper extremity. A systematic review. BMC Musculoskeletal Disorders, 11, 79. 10.1186/1471-2474-11-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Szabo A. (2020). Effects of yoga on stress among healthy adults: A systematic review. Alternative Therapies in Health and Medicine, 26. [PubMed] [Google Scholar]
- Wang W. L., Chen K. H., Pan Y. C., Yang S. N., Chan Y. Y. (2020). The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry, 20, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waongenngarm P., van der Beek A. J., Akkarakittichoke N., Janwantanakul P. (2020). Perceived musculoskeletal discomfort and its association with postural shifts during 4-h prolonged sitting in office workers. Applied Ergonomics, 89, 103225. 10.1016/j.apergo.2020.103225 [DOI] [PubMed] [Google Scholar]
- Yoshihara K., Hiramoto T., Sudo N., Kubo C. (2011). Profile of mood states and stress-related biochemical indices in long-term yoga practitioners. BioPsychoSocial Medicine, 5, 6. 10.1186/1751-0759-5-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu F., Zhang M., Wang D., Hong Q., Zeng C., Chen W. (2020). Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. Plos One, 15, e0238544–21. 10.1371/journal.pone.0238544 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Online supplementary file 1, for Impact of 10-Min Daily Yoga Exercises on Physical and Mental Discomfort of Home-Office Workers During COVID-19 by Maria-Gabriela Garcia, Melany Estrella, Angie Peñafiel, Paul G. Arauz and Bernard J. Martin in Human Factors: The Journal of Human Factors and Ergonomics Society