Abstract
Retroperitoneal spindle cell neoplasms are diagnostically challenging. Malignant peripheral nerve sheath tumours (MPNSTs) can sometimes present as sporadic primary retroperitoneal tumours. MPNSTs are usually high-grade and highly aggressive tumours and are associated with a poor prognosis. Low-grade MPNSTs are very rarely described. This current case report describes a case of sporadic primary low-grade MPNST presenting as retroperitoneal spindle cell neoplasm. The diagnosis, imaging and immunohistopathological findings, as well as its successful surgical management, are presented.
Keywords: MPNST, low-grade, spindle cell neoplasm, retroperitoneal
Introduction
Malignant peripheral nerve sheath tumours (MPNSTs) are rare tumours of the peripheral nerves, with an estimated incidence of 0.001% in the general population. 1 MPNSTs account for approximately 5% of all soft tissue sarcomas, with over half of these cases arising in the context of neurofibromatosis type 1 (NF1). 1 Unlike MPNSTs associated with NF1, sporadic MPNSTs usually affect patients aged 40–50 years and affect both males and females equally. 2 These tumours frequently affect the limbs, and more uncommonly the head and neck, as well as the retroperitoneal region. Most MPNSTs are high grade and aggressive tumours. Low-grade MPNSTs are rare (<10% of all MPNSTs), difficult to diagnose and are thus poorly characterized due to their rarity. This current case report describes a case of sporadic primary low-grade MPNST presenting as retroperitoneal spindle cell neoplasm.
Case report
In September 2022, a 61-year-old female presented to the Emergency Department of Gandaki Medical College Teaching Hospital, Pokhara, Nepal with a 2-day history of acute epigastric pain and multiple episodes of vomiting. She reported having intractable hiccups, anorexia and apparent weight loss during the previous months. She was a known case of hypertension and rheumatoid arthritis under medication and had undergone myomectomy for fibroid uterus 30 years previously. A physical examination revealed a cachectic build and a body mass index of 17 kg/m2. There were no other apparent findings on the physical examination; and except for slightly deranged liver enzymes, routine laboratory investigations were within normal limits.
Transabdominal ultrasound showed a heteroechoic mass lesion just inferior to the right kidney. On a contrast-enhanced computed tomography (CT) scan, a well-defined (7.6*6.5*5.1 cm), hypodense lesion was seen in the proximal insertion of the right psoas muscle that caused splaying of the psoas muscle fibres (Figure 1). The lesion showed heterogeneous peripheral enhancement with central non-enhancing component in the late arterial phase. On magnetic resonance imaging (MRI) (Figure 2), the retroperitoneal lesion was well-defined, centred on the right psoas but was not infiltrating the muscular plane. It had altered signal intensity and showed T1 isointense, T2 iso to hyperintensity with multiple internal T2 hyperintense cystic components. On contrast administration, the lesion showed mild enhancement in the arterial phase with a nonenhancing cystic component. A CT-guided biopsy was undertaken. On histopathology, cores of bundles and fascicles of spindle cells without any evidence of necrosis or increased mitotic activity was observed. Immunohistochemistry was positive for S100, SOX-10 (Figure 3) but negative for SMA, desmin, CD34 and β-catenin. Based on all of the clinical, radiological and pathological findings, a diagnosis of low-grade malignant peripheral nerve sheath tumour (MPNST) was made according to the Fédération Nationale des Centres de Lutte Contre le Cancer grading system. 3
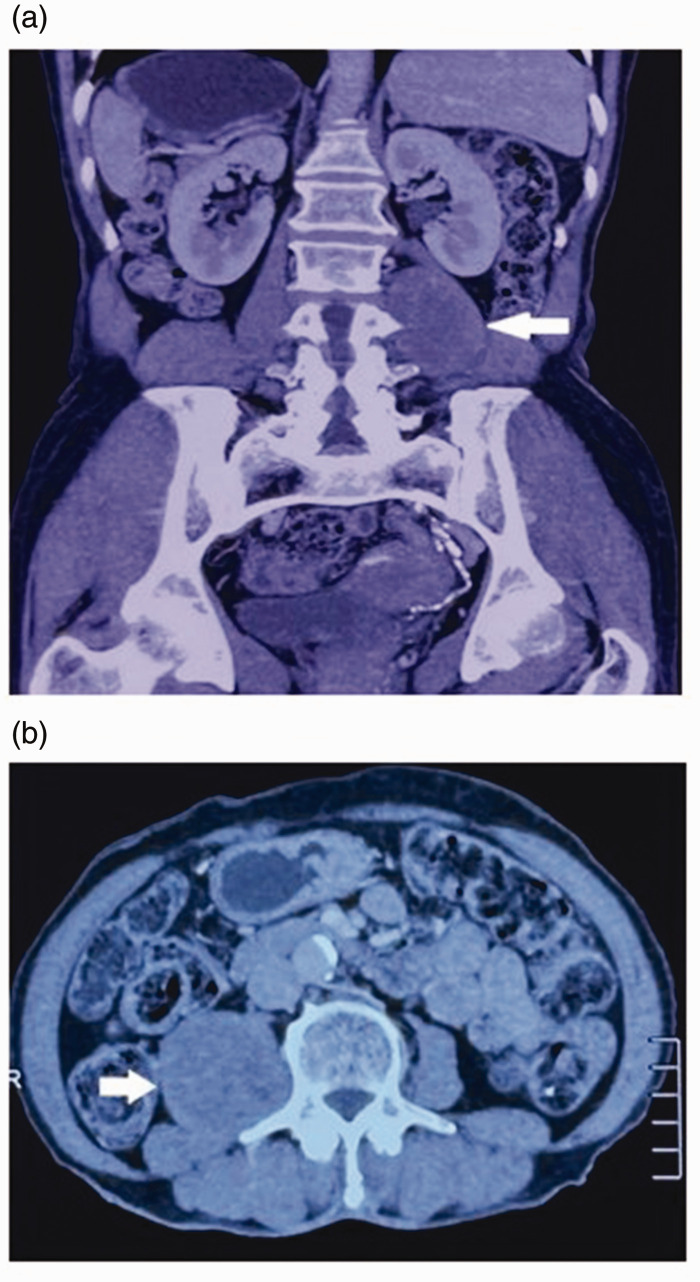
Figure 1.
Contrast-enhanced computed tomography scans of a 61-year-old female who presented with a 2-day history of acute epigastric pain and multiple episodes of vomiting: coronal (a) and axial (b) images showing a well-defined hypodense lesion on the proximal insertion of right psoas muscle (arrows).
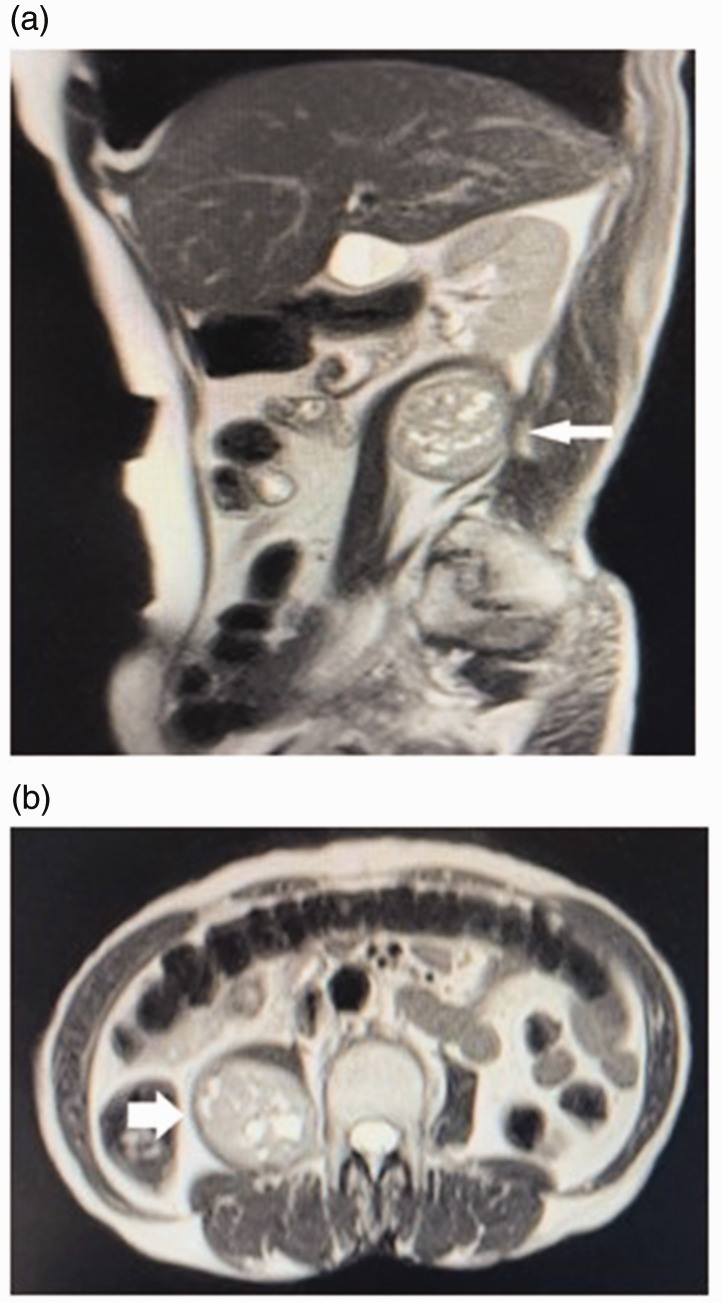
Figure 2.
T2-weighted magnetic resonance imaging scans of a 61-year-old female who presented with a 2-day history of acute epigastric pain and multiple episodes of vomiting: sagittal (a) and axial (b) images showing an iso to hyperintense lesion with multiple internal hyperintense cystic components centred on the right psoas with splaying of the psoas muscle fibres (arrows).
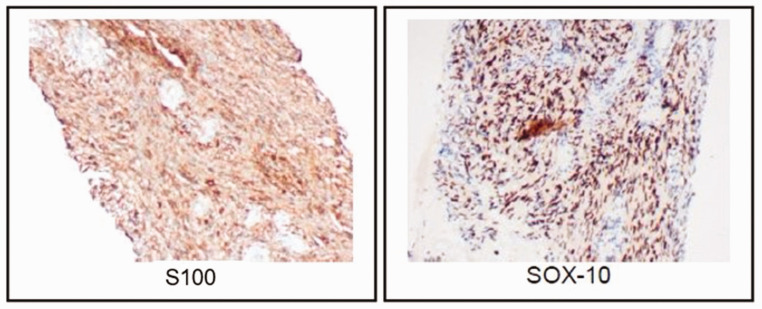
Figure 3.
Representative photomicrographs showing strong immunohistochemical staining for S100 and SOX-10 in tumour cells taken from a computed tomography-guided biopsy from a 61-year-old female who presented with a 2-day history of acute epigastric pain and multiple episodes of vomiting. Magnification, ×100. The colour version of this figure is available at: http://imr.sagepub.com.
After obtaining informed consent for treatment, the patient underwent laparotomy through an anterior midline approach and a wide local excision was carried out with the aim to achieve a potentially curative operation, as per the recommendation of our multidisciplinary tumour board team. Grossly, the capsulated mass was hard and nodular. Postoperative histopathological examination showed encapsulated tissue ensheathing spindle shaped tumour cells arranged in fascicles with predominant bits of tissue in an intersecting growth pattern without any evidence of necrosis or atypical mitoses, which was consistent with the preoperative diagnosis. The post-operative course was uneventful. Considering the highly aggressive behaviour of MPNST, the patient was subject to close clinical follow-up and is doing well as per her most recent follow-up (January 2024). Written informed consent was obtained from the patient for publication of this article and any accompanying images. The reporting of this study conforms to CARE guidelines. 4
Discussion
A wide range of tumours with spindle cell morphology can occur in the retroperitoneum and these include sarcomas and tumours showing adipocytic, smooth muscle or myofibroblastic differentiation as well as peripheral nerve tumours. 2 It is often very challenging to establish the correct diagnosis because of the highly variable clinical as well as imaging and histological findings of these tumours. One of the rare differential diagnoses of retroperitoneal spindle cell tumours include MPNSTs. These tumours are rare variety of soft tissue sarcoma of ectomesenchymal origin. 5
Malignant peripheral nerve sheath tumours are classified into low-grade or high-grade based on a combination of tumour differentiation/histology, mitotic count and tumour necrosis. 3 Most MPNSTs (approximately 90%) are aggressive, high-grade tumours and are associated with poor survival due to frequent multifocal lesions and higher rates of recurrence and metastasis. 6 Low-grade MPNSTs are rare and as a consequence they are poorly understood. A multimodal approach should be utilized in establishing the diagnosis.
Most low-grade MPSNTs are slow growing tumours and thus they often present later in life as compared with the high-grade tumours that present earlier. Classical sites include the extremities, trunk and the head and neck region. The clinical picture may comprise of nonspecific discomfort or features of mass effect. This current case had a rather subacute presentation with nonspecific features of malignancy such as weight loss and cachexia. There was no evidence of neurofibromatoses.
Conventional imaging modalities cannot reliably differentiate between the various differentials of spindle cell neoplasm. However, both CT and MRI might be effective in determining the tumour extent, distant metastases or recurrence following surgery. MRI findings that are more consistent with MPNST than other diagnoses include a large (>5 cm) tumour, heterogeneity on T1-weighted sequence, intratumoral cystic change and ill-defined margins, lack of target sign and perilesional oedema-like zones. 7 The presence of two or more of these imaging features is highly suggestive of MPNST, which was the situation in the current case.
Microscopically, most MPNSTs are highly cellular and show a spindled, fascicular growth pattern with alternating myxoid areas and perivascular condensation. 2 Approximately 15–20% of these tumours may show heterologous differentiation including chondrosarcomatous, osteosarcomatous and rhabdomyosarcomatous components. 8 For a tumour to be classified as low-grade, it should have a mitotic index of <10/10 high power field with no evidence of necrosis. MPNSTs usually show patchy or focal staining for S100 and SOX-10. Interestingly, strong and diffuse staining for S100 and/or SOX-10 strongly suggests low-grade MPNST. 8 In this current case, the histopathology specimens showed spindle-shaped tumour cells arranged in fascicles with predominant bits of tissue in an intersecting growth pattern without any evidence of necrosis or atypical mitoses. Immunohistochemistry was strongly positive for S100 and SOX-10, effectively ruling out other tumours with spindle cell morphology at that region such as fibromyxoid sarcoma, low-grade myxofibrosarcoma and fibrosarcoma. Therefore, considering all of the clinical, radiological and pathological findings, a diagnosis of low-grade MPNST was established. Molecular/cytogenetic studies were not undertaken due to the lack of its availability in our setting.
In patients with MPNST, complete surgical excision with negative margins is the only proven curative treatment. Adjuvant chemotherapy and radiotherapy have been shown to be beneficial but the evidence is limited and hence their use in clinical practice is highly variable. 9 The current patient was subject to a wide local excision since the tumour was low-grade without any evidence of local spread or distant metastases. MPNSTs have a very poor prognosis despite optimum surgical management including adjuvant therapies, with the 5-year survival rates being 30–50%. Grading has been identified as an independent prognostic factor for overall survival in large studies and the use of adjuvant therapies have not influenced outcomes in this cohort significantly. 10 This current patient has undergone close clinical follow-up post-surgery and remains symptom free.
In conclusion, this case report has described a very unusual pathology of sporadic primary, retroperitoneal spindle cell neoplasm in the form of low-grade MPNST. Low-grade MPNST are very controversial not only in their diagnosis but also their management. This case report illustrates how this rare diagnosis can be established by using a multimodal clinico-radiologic-immunopathologic approach. In our opinion, low-grade MPNSTs are different from high-grade MPNSTs in terms of their clinical behaviour as well as their immunohistopathology, but they remain to be characterized properly due to their rarity. Surgery alone may be curative for low-grade lesions, as was in this current case. Further studies are warranted to establish the biological nature, and thus prognosis, of this rare tumour.
Footnotes
Author contributions: M.K., B.K.M., L.O., Y.T., S.B, S.S. and S.C. designed the report, reviewed the literature, edited the images and wrote the paper. S.R., B.R.N. and D.M.S. revised the paper. All the authors have read and approved the final manuscript.
The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Mitesh Karn https://orcid.org/0000-0002-3965-8884
References
- 1.Magro G, Broggi G, Angelico G, et al. Practical Approach to Histological Diagnosis of Peripheral Nerve Sheath Tumors: An Update. Diagnostics (Basel) 2022; 12: 1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaefer IM, Fletcher CD. Diagnostically Challenging Spindle Cell Neoplasms of the Retroperitoneum. Surg Pathol Clin 2015; 8: 353–374. [DOI] [PubMed] [Google Scholar]
- 3.Knight SWE, Knight TE, Santiago T, et al. Malignant Peripheral Nerve Sheath Tumors—A Comprehensive Review of Pathophysiology, Diagnosis, and Multidisciplinary Management. Children (Basel) 2022; 9: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 5.Kar M, Deo SV, Shukla NK, et al. Malignant peripheral nerve sheath tumors (MPNST) – Clinicopathological study and treatment outcome of twenty-four cases. World J Surg Onc 2006; 4: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prudner BC, Ball T, Rathore R, et al. Diagnosis and management of malignant peripheral nerve sheath tumors: Current practice and future perspectives. Neurooncol Adv 2019; 2(Suppl 1): i40–i49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wasa J, Nishida Y, Tsukushi S, et al. MRI features in the differentiation of malignant peripheral nerve sheath tumors and neurofibromas. AJR Am J Roentgenol 2010; 194: 1568–1574. [DOI] [PubMed] [Google Scholar]
- 8.Yamaguchi U, Hasegawa T, Hirose T, et al. Low grade malignant peripheral nerve sheath tumour: Varied cytological and histological patterns. J Clin Pathol 2003; 56: 826–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res 2002; 62: 1573–1577. [PubMed] [Google Scholar]
- 10.Cai Z, Tang X, Liang H, et al. Prognosis and risk factors for malignant peripheral nerve sheath tumor: a systematic review and meta-analysis. World J Surg Oncol 2020; 18: 257. [DOI] [PMC free article] [PubMed] [Google Scholar]