Abstract
Background
The short-term efficacy of combined lifestyle and behavioural interventions led by nurses in the management of urinary incontinence has not been rigorously evaluated by randomized controlled trial. We conducted a 6-month randomized controlled trial to determine whether a model of service delivery that included lifestyle and behavioural interventions led by “nurse continence advisers” in collaboration with a physician with expertise in continence management could reduce urinary incontinence and pad use in an outpatient population. We also aimed to evaluate the impact of this approach on subjects' knowledge about incontinence and their quality of life.
Methods
We used advertising in the mainstream media, newsletters to family physicians and community information sessions in 1991 to invite volunteers who were 26 years of age or older and suffered from incontinence to participate in a randomized controlled trial. Men and women who met the eligibility criteria were randomly allocated to receive either counselling from specialized nurses to manage incontinence using behavioural and lifestyle modification sessions every 4 weeks for 25 weeks or usual care. Symptoms of incontinence and the use of incontinence pads were the primary outcome measures.
Results
Using sealed envelopes, 421 patients were randomly allocated to the treatment or control groups. On average, patients in the treatment group experienced 2.1 “incontinent events” per 24 hours before treatment and 1.0 incontinent event per 24 hours at the end of the study. Control patients had an average of 2.4 incontinent events per 24 hours before the study and 2.2 incontinent events per 24 hours at the end of the study. The mean decrease in events in the treatment group was 1.2 and in the control group 0.2 (p = 0.001). Pad use declined from a mean of 2.2 per 24 hours before randomization in the treatment group to 1.2 per 24 hours at the end of the study, compared with 2.6 pads per 24 hours in the control group at the start of the study and 2.4 per 24 hours at the end. Pad use per 24 hours decreased on average by 0.9 pads in the treatment group and 0.1 in the control group (p = 0.021).
Interpretation
Behavioural and lifestyle counselling provided by specialized nurses with training in managing incontinence reduces incontinent events and incontinence pad use.
Urinary incontinence primarily affects young-to-middle-aged women and elderly men and women. The prevalence of urinary incontinence in people aged 65 years and older living in the community ranges from 8% to 30%.1,2,3,4,5,6 Urinary incontinence is underrecognized and those affected are often embarrassed and ashamed, thus, the problem frequently remains hidden.1,2
North American and Canadian practice guidelines for the effective management of adult urinary incontinence have advocated thorough initial assessment, then staged multidisciplinary approaches beginning with the least invasive and reversible (lifestyle and behavioural) interventions, before drug therapy (reversible) and surgery (invasive and irreversible).1,2,3 The role of continence advisers in the management of urinary incontinence has evolved from its early beginnings in the United Kingdom7,8,9,10,11 and is now increasingly recognized in North America.12,13,14 There has been some evaluation of the short-term efficacy of multidisciplinary incontinence management by nurse practitioners or “nurse continence advisers” in community and outpatient settings.15,16,17,18,19,20 However, the short-term efficacy of combined lifestyle and behavioural interventions led by nurse continence advisers has not been rigorously evaluated using randomized controlled trials.
Urinary incontinence has many causes, particularly in elderly people,21 and the potential for overall clinical improvement is greater when multiple interventions target several factors. Each intervention effects a small positive change, and these small changes cumulatively have a large positive outcome.21 Individual components of lifestyle and behavioural interventions are increasingly being shown to be effective. For example, behavioural training, including pelvic muscle exercises, has reduced urinary incontinence significantly,22,23,24 in some cases up to 57%.25 A combined approach consisting of both bladder training and pelvic muscle exercises, provided by trained registered nurses, has resulted in significantly fewer incontinent episodes than either approach alone.26 Pelvic floor exercises have been shown to be equally effective in women with stress, urge and mixed urinary incontinence.27 Adherence to pelvic floor muscle exercises has been shown to be sustained for up to 5 years in 70% of women who have intensive exercise training.28 Decreasing caffeine intake has also been shown to reduce episodes of incontinence.29 Reducing fluid intake in people with detrusor instability, but not those with genuine stress incontinence, reduces the number of “incontinent events.” Increasing fluid intake makes the urinary incontinence worse.30
Our 6-month randomized controlled trial was conducted to determine whether a model of service delivery that included lifestyle and behavioural interventions led by nurse continence advisers in collaboration with a physician with expertise in continence management could reduce urinary incontinence and pad use. Our secondary aim was to investigate the impact of incontinence management led by nurse continence advisers on subjects' knowledge about incontinence and their quality of life.
Methods
The study protocol received approval from the University of Western Ontario Research Ethics Review Board. Subjects were recruited using advertising in the mainstream media, newsletters to family physicians and community information sessions. Volunteers were seen in an outpatient incontinence clinic. Most of the volunteers were self-referred. Subjects included both men and women who were 26 years of age or older, resided in the community, experienced urinary incontinence at least once per week and communicated in English. Those excluded were pregnant women, residents of long-term care institutions and people with dementia who lived alone. Subject enrolment began in January 1991. Subjects were enrolled up until September 1991, and the 6-month randomized controlled trial was completed in April 1992.
When potential subjects contacted the research project for an appointment, the study secretary reviewed the inclusion criteria to ensure eligibility. An appointment was made for a baseline assessment with one of 3 nurse continence advisers. A brochure describing the project and the baseline questionnaire were mailed to subjects for completion before their appointment. A 7-day, 24-hour “bladder diary” with detailed instructions was included in the package and used by subjects to record the frequency of voiding and incontinent events during the week before the potential subject's baseline assessment.
The baseline assessment comprised a history and physical examination. At this assessment, the 3 nurse continence advisers also answered any remaining questions, reviewed the completed questionnaire and bladder diary, and obtained written, informed consent from all subjects. The continence history included risk factors for incontinence and the volume of all oral fluids including caffeinated beverages taken over a typical 24-hour period. The examination included a focused neurological assessment, vaginal inspection and digital assessment of circumvaginal muscle strength,31 a rectal examination, a prostate examination, examination of sacral nerve sensation, in- and out-catheterization to measure postvoid residual urine and a Folstein Mini-Mental State Examination.32 Laboratory tests included urinalysis and measurement of serum glucose and creatinine. From the baseline assessment, the nurse continence adviser's diagnosis characterized the predominant type of incontinence as stress, urge, combined stress and urge, overflow (incomplete emptying) or functional.
We independently generated random permuted blocks, with a block size of 4, such that in each block 2 subjects were randomly assigned to treatment and control groups. Each assignment was concealed in its own envelope. After completing the initial assessment and obtaining consent, the nurse continence advisers opened the envelope to determine subject assignment to the treatment or the control group.
The nurse continence advisers were all registered nurses who had a bachelor of science in nursing degree. Before the entry of subjects into the study, all the nurses received training that included both in-depth small group education and hands-on supervised training in an already established outpatient continence clinic. This training was provided by all 3 investigators who had extensive clinical experience in the assessment and management of urinary incontinence in an adult population. As the first subjects entered the study, twice-weekly reviews of the assessments, conducted by the investigators with the nurse continence advisers, helped solve any clinical or research problems. Each nurse continence adviser carried an equal caseload and followed the same subjects from initial assessment to the 25-week final assessment, thus providing continuity for each subject. One of the investigators was also the project manager and was on-site and available daily to deal with any immediate issues.
Intervention
At week 1, the nurse continence adviser's diagnosis of incontinence was explained to the treatment group, and treatment was initiated with lifestyle and behavioural interventions. No drug treatment was initiated concomitantly. Subjects with abnormal incontinence-related findings including a true postvoid residual urine that was greater than 150 mL on 2 occasions, difficult in-catheterization and out-catheterization, or microscopic hematuria were referred to the collaborating study urologist for additional investigation and treatment.
Treatment subjects returned every 4 weeks for review of their bladder diaries for the previous week and their adherence to behavioural interventions and pelvic muscle exercises. At the midpoint of the trial, that is, at 13 weeks, each treatment subject's progress was reviewed by the 3 nurse continence advisers and investigators (M.J.B., A.K., M.B.) to determine the degree of improvement or resolution. For those subjects whose condition had not improved, secondary treatments were considered using an a priori study management algorithm. Possible actions included continuing with nurse continence adviser interventions alone, dual-channel water cystometry or referral to the study physician (M.J.B.), the study urologist or the study urogynecologist for further interventions, or some combination of these. Treatment subjects seen by the study medical staff continued with their regular visits to their nurse continence adviser. Subjects whose urinary incontinence was unresolved at the end of the 25-week trial could return to the regular continence clinic for further treatment or to consider other treatment options. Control subjects were offered treatment at the end of the 25 weeks at the regular continence clinic.
Each subject's family physician was informed of any significant abnormal findings from the baseline assessment. At 25 weeks, the baseline questionnaire, a 1-week bladder diary and an estimate of 24-hour fluid and caffeine intake were repeated. Bladder diaries were completed by subjects in the treatment group for one week before each 4-weekly review visit with the nurse continence adviser. Those in the control group completed bladder diaries at weeks 1, 13 and 25.
Outcome measures
The primary outcome variables were incontinent events (measured using bladder diaries) and pad use (measured using the questionnaire) per 24 hours at the end of 25 weeks of treatment.
Secondary outcomes that we examined included the impact of incontinence management led by nurse continence advisers on subjects' knowledge about incontinence and their quality of life. These were measured using 10 questions from the Incontinence Impact Questionnaire (IIQ)33 and selected items from the York Incontinence Perceptions Scale (YIPS), both of which could be answered by both men and women.34 The latter, under development at the time of the study, has been subsequently validated in a similar population.34 The IIQ consisted of 26 items that measured the impact of incontinence in 3 domains (daily activities, social interaction and self-perception). The reliability of the modified IIQ was verified in our sample. Internal consistency as measured by Cronbach's α reliability coefficient was extremely high (α = 0.97). The selected items from the YIPS measured subjects' knowledge, control and acceptance of urinary incontinence, their coping and their quality of life. Each of these items was rated on a 7-point Likert scale, ranging from most negative (1) to most positive (7), with 4 being neutral.
Statistical analysis
An intention-to-treat analysis was used to test the effect of incontinence management led by nurse continence advisers. The 2 х 3 ANOVA method was used to assess the main effects of treatment group and type of incontinence (stress, urge, and combined stress and urge), and their first-order interaction, on the primary response variables of incontinent events and pad use. These 3 primary types of incontinence were used, because they accounted for 94% of the sample. In the absence of a main effect due to incontinence type and no evidence of interaction, the analysis proceeded using an examination of change scores as described by Pocock.35 Within-group changes were evaluated by subtracting scores at 25 weeks from baseline scores for each subject. Between-group differences in effect were then compared using independent t-tests of the change scores. A 95% confidence interval was also calculated for the between-group difference in change scores.
Results
Of the 446 people who contacted the clinic, 421 eligible subjects were randomized to the treatment (n = 210) and control (n = 211) groups (Table 1). No subjects were actively being treated by any other professional. Two subjects had been seen coincidently by the study gynecologist but were not receiving active treatment. Current treatment was not an exclusion criterion, but no one presented who was currently receiving treatment. Fig. 1 shows the flow of subjects through each stage of the study. The most frequently used nursing interventions provided were counselling related to fluid and caffeine intake, pelvic muscle exercises (for stress incontinence and to suppress urinary urgency) and bladder training, using regular timed voiding. Over 90% of treatment subjects received all of these interventions. All the subjects in the intervention group were seen by the nurse continence adviser every 4 weeks. Most of the subjects kept their 4-weekly appointments and saw the nurses a total of 7 times. Those who became continent (dry) before the end of the study missed some of the visits as “they were unnecessary” but returned for the final 25-week visit.
Table 1
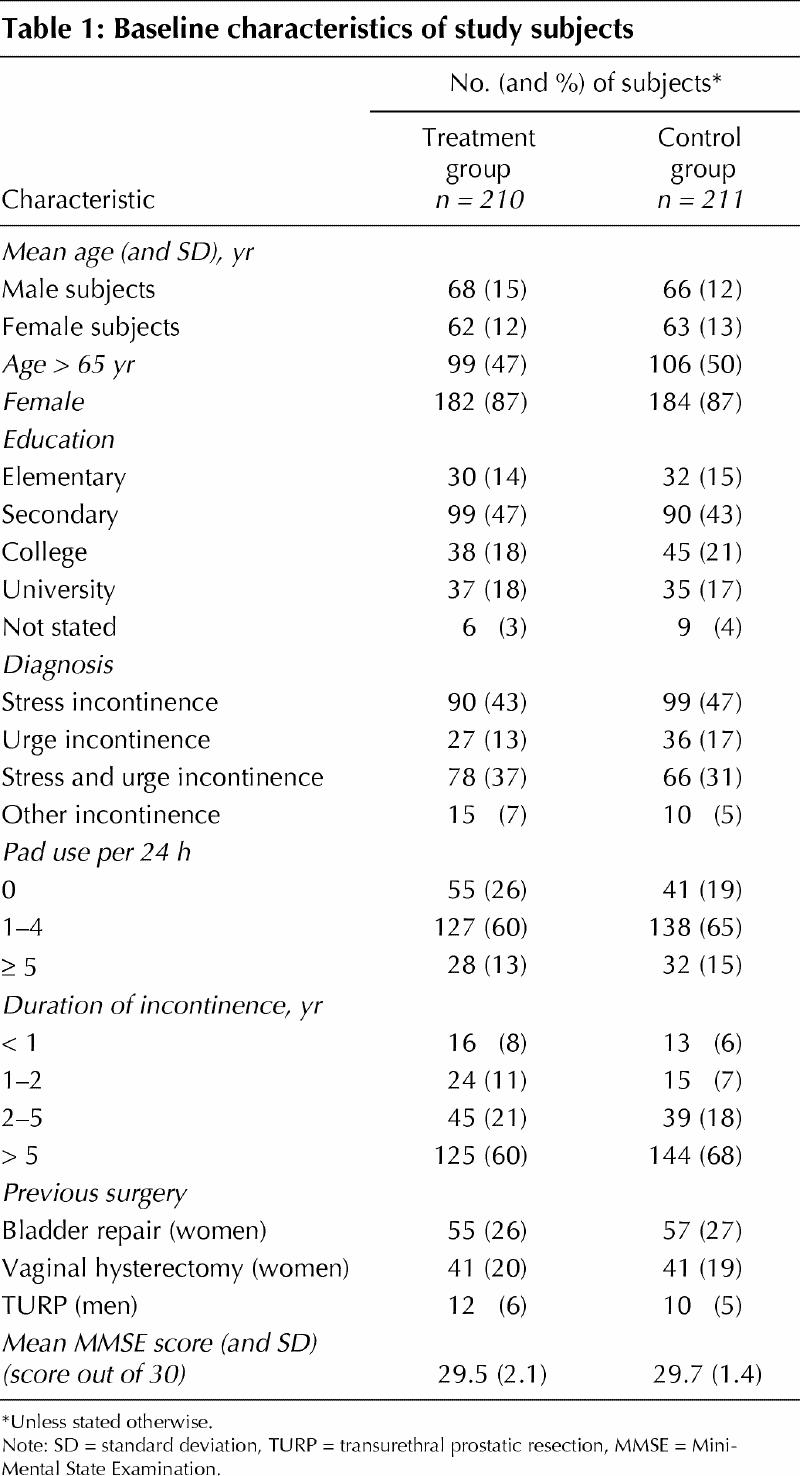
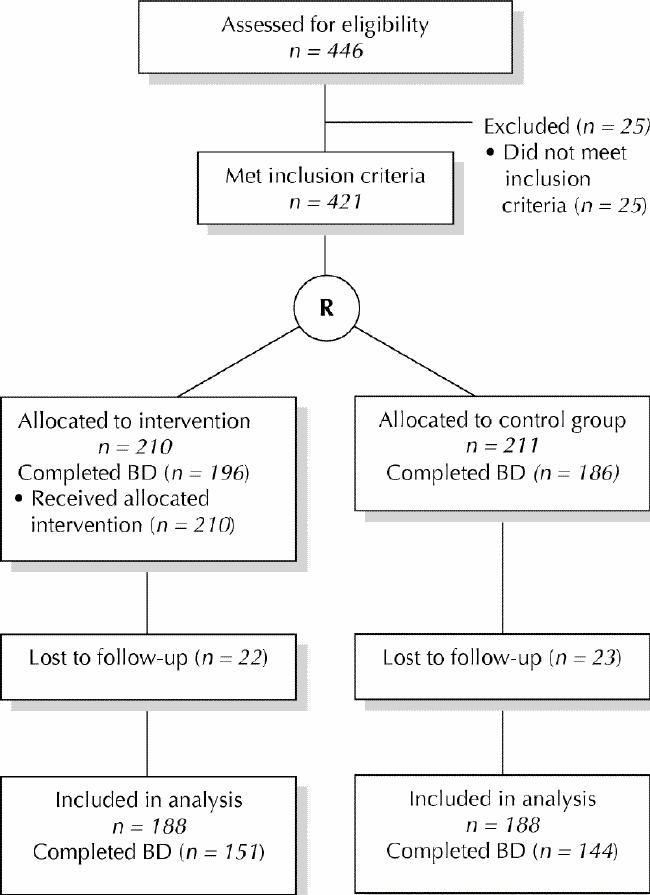
Fig. 1: Flow of participants through each stage of the randomized controlled trial. BD = bladder diaries.
Treatment and control subjects were compared for all medical history variables. There was no statistically significant difference between the groups in the use of medications that affect bladder function or incontinence, and overall their use was relatively low: anticholinergics 7.8%, cholinergics 1.0%, diuretics 17.1%, estrogen 20.2% and sedatives 16.2%.
Compared with those subjects lost to follow-up, those successfully followed at 25 weeks were more likely to be women (88% v. 77.5%), over 45 years of age (93% v. 82 %) and with more than secondary education (43% v. 22%). This pattern was consistent for both treatment and control groups, suggesting no biased dropout by group. The largest between-group difference in baseline characteristics was in pad use: those lost to follow-up in the treatment group had slightly higher 24-hour median pad use (3 pads) than control subjects lost to follow-up (2 pads), or treatment or control subjects who were successfully followed (2 pads in each group).
Primary outcomes
The ANOVA method revealed no evidence of a main effect of diagnosis for either the number of incontinent events per 24 hours or the number of absorbent pads used. Neither first-order interaction (incontinent events х diagnosis, pads used х diagnosis) was statistically significant. Consequently, the remainder of the analyses were based on means, mean change scores and confidence intervals.
Within-group changes
The mean change scores after 25 weeks indicated that incontinent events in the treatment group decreased by over one event (–1.2) per 24-hour period. The confidence intervals for the mean change exclude zero and suggest that the smallest statistical decrease was 0.8 events. In contrast, the control group displayed only a 0.2 reduction in incontinent events, and the confidence interval for this difference included zero. Pad use decreased in the treatment group by 0.9 pads per day, an effect that was unlikely to have occurred due to chance (95% confidence interval [CI] –1.5 to –0.3). In the control group, there was virtually no change in pad use, and the confidence intervals included zero.
Between-group differences
At 25 weeks, the treatment group had a net decrease exceeding one incontinent event (–1.2) relative to the control group (–0.2), and this difference was statistically significant (p < 0.001). For pads, the net difference in use between groups was –0.9 in favour of the treatment group (p = 0.021). The mean daily numbers of incontinent events at baseline and 25 weeks, by group, are outlined in Table 2 and Fig. 2.
Table 2
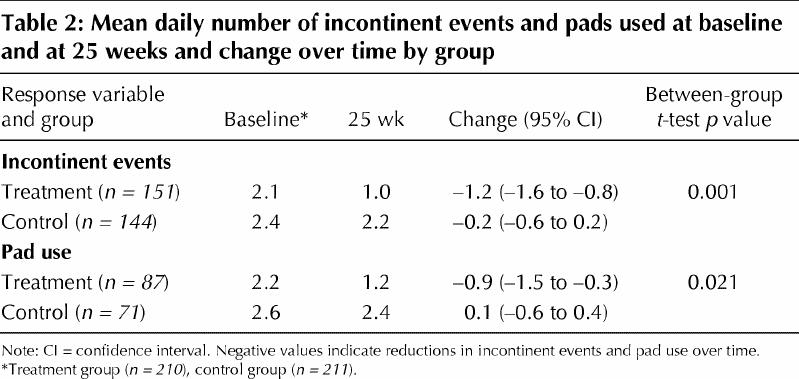
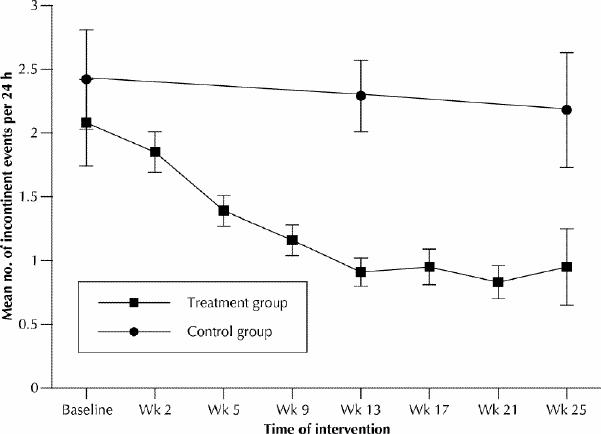
Fig. 2: Mean number of incontinent events by study group over time. Information was derived from participants' bladder diaries.
Control group improvement
During the 25-week study, some control subjects sought treatment outside the research project. However, as a group, there was no change in incontinent events or pad use. After the 25-week study, control subjects were offered and provided treatment through the continence clinic, and some received treatment from other sources such as specialist referrals initiated by their family physician.
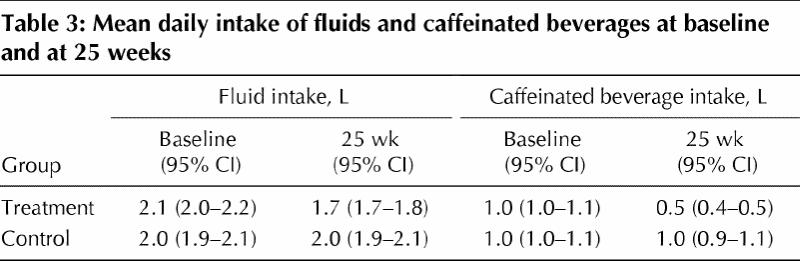
The treatment group had a significant reduction in fluid and caffeinated fluid intake at 25 weeks, whereas the control group's fluid and caffeine intake was unchanged at 25 weeks (Table 3).
Table 3
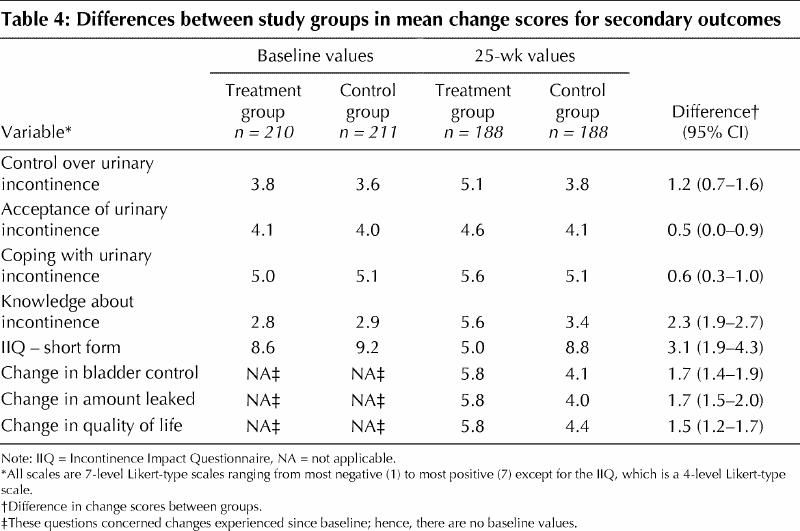
Secondary outcomes
Differences in mean change scores for secondary outcomes between study groups, their baseline values and values at 25 weeks are outlined in Table 4. After 25 weeks, all differences in change scores favoured the treatment group. For 5 of these outcome measures (control over incontinence, knowledge about incontinence, perceived changes in bladder control, amount of urine leaked and quality of life), the difference exceeded one full unit on a 7-point Likert-type scale. Except in the case of control over incontinence, the lower bounds of the 95% confidence intervals suggested that the between-group difference was at least one full unit of improvement. The net change in the IIQ favoured the treatment group by 3.1 units (95% CI 1.9–4.3) on a 30-point scale.
Table 4
By following the a priori study management algorithm, dual-channel water cystometry was used to clarify the nurses' diagnosis for treatment subjects whose condition had not improved at 13 weeks. Fifty-seven treatment subjects had not shown improvement at the midpoint of the study. Of these, 36 were referred to the study physician, 4 to the urologist and 4 to the urogynecologist. The remaining 13 continued with behavioural interventions. Three of the 4 subjects referred to the urologist had symptoms of prostatism, and 2 had more than 150 mL of residual urine on 2 occasions. Following consultation, one had a transurethral resection of the prostate. The 4 subjects referred to the study gynecologist had persisting incontinence and varying degrees of urogenital prolapse (n = 3) and in one case a large fibroid uterus (n = 1). Following consultation, one subject had a vaginal pessary inserted, whereas another had an abdominal hysterectomy and a Marshall-Marchetti-Krantz procedure.
Interpretation
The lifestyle and behavioural interventions led by nurse continence advisers resulted in a statistically and clinically significant improvement in the treatment group at 25 weeks, with a reduction in incontinent events and pad use. The 4-weekly bladder diaries indicate that a significant difference in the treatment group had already occurred by 9 weeks. This suggests that early intervention consisting of bladder training and counselling about fluid and caffeine intake contributed to this improvement. Two measurable risk factors for urinary incontinence that improved by 25 weeks were fluid and caffeine intake.
The improvement in secondary outcomes at 25 weeks paralleled and reinforced the significant improvement in primary outcomes and is consistent with other findings.36,37 The significant improvement in treatment subjects' perceived knowledge about incontinence and bladder control support the role of education provided by nurse continence advisers in incontinence management.
Our study contributes to our understanding of the effectiveness of the role of nurse continence advisers. Other investigators have demonstrated the effect of single behavioural interventions such as pelvic floor exercise and caffeine and fluid reduction. This study focused on and confirmed the validity of the practice of nurse continence advisers who use a package of behavioural interventions tailored to the individual client, in this case outpatient women and men of a wide age range.
There are several limitations to our interpretation of the data. The sample was not proportionately representative of the type of incontinence prevalent in the community but was a convenience sample, which implies certain selection biases. Furthermore, the subjects responded to active advertising and may have been motivated to implement behavioural interventions. The nurse continence advisers' package of interventions addressed multiple risk factors. As with other efficacious multifactorial interventions, it is difficult to isolate the individual or combined contributions of the separate interventions. Other studies have already evaluated the relative contributions. We felt that it was more important to evaluate an overall comprehensive management strategy to determine the short-term efficacy of reducing incontinence and pad use and to assess the change in knowledge of incontinence and quality of life of the subjects.
The findings of this study support the model of a nurse-led continence clinic. We were surprised at the degree of success with behavioural nursing interventions alone. The need for consultation with the study physician for further treatment, such as with medication, was infrequent. A nurse with at least a baccalaureate, and preferably a master's degree, in nursing and specialized training in the assessment and management of urinary incontinence could provide clinic-based care for those with urinary incontinence. Because of the potential complexity of continence problems with varying causes, particularly in the case of elderly patients, medical collaboration and an interdisciplinary approach ensure comprehensive management.
This intervention led by nurse continence advisers is an effective, low-cost management strategy that is consistent with the models and guidelines of continence management recommended by the Canadian Continence Foundation Consensus Conference in May 2000.2
Acknowledgments
We would like to thank Dr. Liliane Richardson for her contribution as research assistant, consultant study urologist, Dr. John Vallely, consultant study urogynecologist, Dr. James King, and Ms. Barbara Kudo for her secretarial support. This project is dedicated to the late Dr. Alfreda Kartha, friend and colleague, who was a co-investigator for the study and provided support and encouragement to continue with the follow-up phase.
Footnotes
This article has been peer reviewed.
Contributors: Dr. Michael Borrie was responsible for study conceptualization, design of the RCT, health data analysis and interpretation of the data. Ms. Mary Bawden was responsible for RCT conceptualization and design and data collection. Dr. Mark Speechley was responsible for the statistical design of the RCT and analysis and interpretation of data. Dr. Marita Kloseck analyzed and interpreted data. All authors contributed to drafting the manuscript and critical revisions of the intellectual content of the manuscript.
This study was funded by the Ontario Ministry of Health Assistive Devices Branch (grant no. M695A2), Parkwood Hospital, London, Ont., and the University of Western Ontario, London, Ont.
Competing interests: None declared.
Correspondence to: Dr. Michael J. Borrie, Division of Geriatric Medicine, Parkwood Hospital, 801 Commissioners Rd. E, London ON N6C 5J1; fax 519 685-4093; michael.borrie@sjhc.london.on.ca
References
- 1.National Institutes of Health. Urinary incontinence in adults: consensus conference. JAMA 1989;261:2685-90. [DOI] [PubMed]
- 2.The Canadian Continence Foundation. Promoting a collaborative consumer-focused approach to continence care in Canada. Westmount (QC): The Foundation; 2001. Available: www.continence-fdn.ca (accessed 2002 Feb 15).
- 3.Fantl JA, Newman DK, Colling J, DeLancey JOL, Keeys C, Loughery R, et al. Urinary incontinence in adults: acute and chronic management. Clinical Practice Guideline No. 2, 1996 Update. Rockville (MD): US Department of Health and Human Services, Agency for Health Care Policy and Research; 1996. AHCPR publication no. 96-0682.
- 4.Mohide EA. The prevalence and scope of urinary incontinence. Clin Geriatr Med 1986;2:639-55. [PubMed]
- 5.Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol 1991;146:1255-9. [DOI] [PubMed]
- 6.Steeman E, Defever M. Urinary incontinence among elderly persons who live at home. A literature review. Nurs Clin North Am 1998;33:441-55. [PubMed]
- 7.Duffin HM, Castleden CM. The continence adviser's role in the British health care system. Clin Geriatr Med 1986;2:841-55. [PubMed]
- 8.Roe BH. Development of continence advisory services in the United Kingdom. Scand J Caring Sci 1990;4:51-4. [DOI] [PubMed]
- 9.Roe BH. A comparison of nursing approaches for the promotion and management of continence in the U.K. and Denmark. Int J Nurs Stud 1993;30:25-35. [DOI] [PubMed]
- 10.Rhodes P, Parker G. Profile of an adviser. Nurs Times 1994;90:75-8. [PubMed]
- 11.Shields N, Thomas C, Benson K, Major K, Tree J. Development of a community nurse-led continence service. Br J Nurs 1998;7:824-30. [DOI] [PubMed]
- 12.Newman DK. Urinary incontinence management in the USA: the role of the nurse. Br J Nurs 1996;5:78-88. [DOI] [PubMed]
- 13.Jacobs M, Wyman JF, Rowell P, Smith D. Continence nurses: a survey of who they are and what they do. Urol Nurs 1998;18:13-20. [PubMed]
- 14.Dougherty MC, Dwyer JW, Pendergast JF, Tomlinson BU, Boyington AR, Vogel WB, et al. Community-based nursing: continence care for older rural women. Nurs Outlook 1998;46:234-44. [DOI] [PubMed]
- 15.Brink C, Wells T, Diokno A. A continence clinic for the aged. J Gerontol Nurs 1983;9:651-5. [DOI] [PubMed]
- 16.McDowell BJ, Burgio KL, Dombrowski M, Locher JL, Rodriquez E. An interdisciplinary approach to the assessment and behavioral treatment of urinary incontinence in geriatric outpatients. J Am Geriatr Soc 1992;40:370-4. [DOI] [PubMed]
- 17.O'Brien J. Evaluating primary care interventions for incontinence. Nurs Stand 1996;10:40-3. [PubMed]
- 18.McGhee M, O'Neill K, Major K, Twadolle S. Evaluation of a nurse led continence service in the southwest of Glasgow, Scotland. J Adv Nurs 1997; 26:723-8. [DOI] [PubMed]
- 19.Skelly J, Kenny K. The impact of the nurse continence advisor on continence care. Clin Effect Nurs 1998;2:4-10.
- 20.Borrie MJ, Lyteynec S, Griffiths N, Knezic Z, Gagnon M. Outcomes of a new community-nurse continence service. Ann R Coll Physicians Surg Can 1999;32:346-51.
- 21.Resnick NM, Yalla SV. Management of urinary incontinence in the elderly. N Engl J Med 1985;313:800-5. [DOI] [PubMed]
- 22.McDowell BJ, Engberg S, Sereika S, Donovan N, Jubeck ME, Weber E, et al. Effectiveness of behavioral therapy to treat incontinence in homebound older adults. J Am Geriatr Soc 1999;47:309-18. [DOI] [PubMed]
- 23.Bo K, Talseth T, Holme I. Single blind, randomized controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999;318(7182):487-93. [DOI] [PMC free article] [PubMed]
- 24.Boyington AR, Dougherty MC. Pelvic muscle exercise effect on pelvic muscle performance in women. Int Urogynecol J Pelvic Floor Dysfunct 2000;11(4):212-8. [DOI] [PubMed]
- 25.Fantl JA, Wyman JF, McClish DK, Harkins SW, Elswick RK, Taylor JR, et al. Efficacy of bladder training in older women with urinary incontinence. JAMA 1991;265:609-13. [PubMed]
- 26.Wyman JF, Fantl JA, McClish DK, Bump RC. Comparative efficacy of behavioural interventions in the management of female urinary incontinence. Continence program for women research group. Am J Obstet Gynecol 1998; 46:233-44. [DOI] [PubMed]
- 27.Nygaard IE, Kreder KJ, Lepic MM, Fountain KA, Rhomberg AT. Efficacy of pelvic floor muscle exercises in women with stress, urge and mixed urinary incontinence. Am J Obstet Gynecol 1996;174:120-5. [DOI] [PubMed]
- 28.Bo K. Adherence to pelvic floor muscle exercise and long-term effect stress urinary incontinence. A five-year follow-up study. Scand J Med Sci Sports 1995;5:36-9. [DOI] [PubMed]
- 29.Tomlinson BU, Dougherty MC, Pendergast JF, Boyington AR, Coffma MA, Pickens SM. Dietary caffeine, fluid intake and urinary incontinence in older rural women. Int Urogynecol J Pelvic Floor Dysfunct 1999;10:22-8. [DOI] [PubMed]
- 30.Swithinbank LV, Rogers CA, Yang Q, Shepherd AM, Abrams P. Does the amount and type of fluid intake effect urinary symptoms in women? Neurourol Urodyn 1999;18:371-2.
- 31.Wells TJ, Brink CA, Diokno AC, Wolfe R, Gillis GL. Pelvic muscle exercise for stress urinary incontinence in elderly women. J Am Geriatr Soc 1991;39(8):785-91. [DOI] [PubMed]
- 32.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12(3):189-98. [DOI] [PubMed]
- 33.Wyman JF, Harkins SW, Choi SC, Taylor JR, Frantl JA. Psychosocial impact of urinary incontinence in women. Obstet Gynecol 1987;70:378-81. [PubMed]
- 34.Lee PS, Reid DW, Saltmarche A, Linton L. Measuring the psychosocial impact of urinary incontinence: the York Incontinence Perceptions Scale (YIPS). J Am Geriatr Soc 1995;43:1275-8. [DOI] [PubMed]
- 35.Pocock SJ. Clinical trial: a practical approach. Chichester (England): John Wylie; 1983.
- 36.Fonda D, Woodward M, D'Astoli M, Chin WF. Sustained improvement of subjective quality of life in older community-dwelling people after treatment of urinary incontinence. Age Ageing 1995;24:283-6. [DOI] [PubMed]
- 37.Wyman JF, Fantl JA, McClish DK, Harkins SW, Uebersax JS, Ory M. Quality of life following bladder training in older women with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 1997;8:223-9. [DOI] [PubMed]


