Abstract
Introduction:
Smaller hand size has been shown to affect ease of instrument use and surgeon injury rates in multiple surgical subspecialties. Women have a smaller average hand size and are more often affected by this issue than men. The goal of this resident survey was to investigate whether hand size and gender impact self-reported difficulty with instrument use among orthopaedic surgery residents.
Methods:
Residents were surveyed about how often they experience difficulty using common orthopaedic instruments. Self-reported difficulty using surgical instruments was compared between residents with small glove (SG, outer ≤7.0) vs. large glove (LG, ≥ 7.5) sizes and between male and female residents.
Results:
One hundred forty-five residents (118 males and 27 females) completed the survey for a response rate of 3.7%. The SG group contained 35 residents, with 26 females and 9 males. The LG group contained 110 residents, with 1 female and 109 males. The SG group reported more difficulty than the LG group when using 3/6 instruments: the wire-cutting pliers (71.4% vs. 25.5%), universal T-handle chuck (65.7% vs. 21.4%), and large wire driver (60.0% vs. 24.8%). Female residents reported more difficulty than males for 5/6 instruments. Within the SG group, however, there was no difference in self-reported difficulty between female SG and male SG residents for 4/6 instruments.
Conclusions:
The predominantly male LG group reported significantly less difficulty than the more gender mixed though still predominantly female SG group. A subanalysis comparing males and females within the SG group found that there was no difference between SG female and SG male residents for 4/6 of the instruments, suggesting that glove size might impact reported difficulty independently from gender. Although the effect of glove size vs. gender is difficult to differentiate in this study, the high rate of difficulty experienced by male and female residents in the SG group should be considered by residency programs, surgeon educators, and instrument manufacturers as the field of orthopaedic surgery continues to become more diverse.
Level of Evidence:
III.
Introduction
Although hand size among surgeons varies significantly, the size of most instruments in orthopaedic surgery does not. As gender, ethnic, and racial diversity increases among new surgical residents, the variation in surgeon hand size will increase as well1-5. Surgeon hand size is important for 2 reasons. First, smaller surgeon hand size has been shown to affect ease of instrument of use, compensatory muscle activation, and surgeon injury rates in laparoscopic, endoscopic, and orthopaedic surgery6-10. Second, most surgeons with smaller hands are female. How hand size affects instrument use and surgeon performance was first studied in the field of laparoscopic surgery, where surgeons and trainees with smaller hands (largely but not exclusively women) frequently reported more difficulty using single-size laparoscopic instruments9,11-18. In addition to causing instruments to feel awkward or uncomfortable to use, instruments that are not properly sized can lead to overuse injuries and impact surgeon satisfaction and career longevity19,20. Just as poorly sized surgical instruments can negatively impact performance, the use of appropriately sized grips in laparoscopic surgery has been shown to significantly improve simulated surgical performance15. Finally, a significant proportion of men may also experience difficulty with instrument use related to hand size when a broader range of ethnic or racial groups are considered3-5,21-23.
Part of training an increasingly diverse generation of orthopaedic residents requires understanding the challenges they encounter while acquiring surgical skills and developing strategies and techniques to overcome these challenges. The goal of this resident survey was to describe how much difficulty orthopaedic surgery residents report using common orthopaedic instruments and investigate how hand size and gender impact difficulty with instrument use.
Materials and Methods
The study was deemed exempt from review by our Institutional Review Board before initiating the study. An online survey was developed (Qualtrics, Seattle, Washington) to collect information about residents' demographics, glove size (GS), and experiences using a variety of common orthopaedic surgical instruments. The first battery of questions asked residents how often they experienced difficulty using 6 surgical instruments commonly used in orthopaedic surgery: the large wire driver, large universal T-handle chuck, periarticular reduction forceps, rongeur, wire-cutting pliers, and arthroscope. Instruments for the survey were chosen based on a collaborative discussion between resident and attending authors by reviewing the most common instruments used on each of the subspecialty rotations, with a preference given to instruments used in the care of fractures because of the significant amount of time residents at various levels of training participate in fracture cases. Difficulty using instruments was categorized as never, sometimes, about half the time, most of the time, or always. The second battery of questions asked residents to report how often they experienced hand fatigue and how difficulty with instrument has affected or might affect in the future their choice of subspecialty. Third, residents were asked to rate how much they agreed with the following statements: “I feel that the difficulties I encounter using certain instruments are related to my lack of skill based on level of training,” and “I feel that the difficulties I encounter using certain instruments are related to design flaws.” The entire survey appears in Appendix 1, http://links.lww.com/JBJSOA/A628. The survey was sent to 199 orthopaedic surgery residency program coordinators across the United States through email and posted in a private Facebook group page “Women in Orthopaedics.” Responses were collected in May 2020 after consent was obtained and contained reassurance of voluntary and anonymous participation.
Statistical analysis was performed using SPSS, version 25 (IBM), with a significance level set at p < 0.05. Perceived difficulty using surgical instruments was compared between residents with small glove (SG) vs. large glove (LG) sizes, with SG defined as outer glove size ≤ 7.0 and LG ≥ 7.5. Perceived difficulty was also compared between female and male residents and between junior vs. senior residents (Postgraduate Year [PGY] 1-3 vs. PGY4-5). For analysis, difficulty using instruments and hand fatigue responses were collapsed into binary variables of “never” vs. “sometimes” to allow for comparison using χ2 testing. To analyze residents' level of agreement with the 3 statements pertaining to difficulty with instrument use (difficulty with instrument use is due to lack of training, difficulty with instrument use is due to design flaws, and difficulty admitting trouble using instruments), “strongly agree” and “agree” responses were collapsed and compared against “strongly disagree” and “disagree” responses.
Results
A total of 145 residents completed the survey, with 118 residents (81.4%) identifying as male and 27 residents (18.6%) identifying as female. The survey response rate was 3.7%. The full demographics of the respondents are displayed in Table I. The SG group (size 7.0 outer glove or smaller) contained 35 residents, with 26 females (96.3% of all females) and 9 males (7.6% of all males). The LG group contained 110 residents, with 1 female and 109 males. The SG group was 74.3% female, and the LG group was 98.3% male. Eighty-five residents (58.6%) were in their PGY1, 2, or 3 years of training and classified as the junior resident group, with 60 residents in the senior resident group. The proportion of junior and senior residents was similar in the SG vs. LG groups (65.7% junior vs. 56.4% junior, p = 0.96). Ninety-three percent of residents were right-handed, whereas 6.9% were left-handed.
TABLE I.
Survey Respondent Demographics*
| Gender n (%) | |
|---|---|
| Male | 118 (81.4) |
| SG (≤7.0) | 9 (7.6) |
| LG (≥7.5) | 109 (92.4) |
| Female | 27 (18.6) |
| SG (≤7.0) | 26 (96.3) |
| LG (≥7.5) | 1 (3.7) |
| Glove size n (%) | |
|---|---|
| SG (≤7.0) | 35 (24.1) |
| Female | 26 (74.3) |
| Male | 9 (25.7) |
| LG (≥7.5) | 110 (75.9) |
| Female | 1 (1.7) |
| Male | 109 (98.3) |
| Training level n (%) | |
|---|---|
| Junior (PGY1-3) | 85 (58.6) |
| Senior (PGY4-5) | 60 (41.4) |
SG = small glove (≤7.0). LG = large glove (≥7.5). Junior = PGY1-3. Senior = PGY4-5.
Reported Difficulty with Instrument Use
The SG group reported more difficulty than the LG group when using 3 instruments: the wire-cutting pliers (71.4% vs. 25.5%, p < 0.001), universal T-handle chuck (65.7% vs. 21.4%, p < 0.001), and large wire driver (60.0% vs. 24.8%, p < 0.001), Fig. 1 and Table II. There was no significant difference in reported difficulty for the arthroscope, periarticular reduction forceps, or rongeur. Female residents reported significantly more difficulty than males for 5/6 instruments: (arthroscope: 85.2% vs. 63.8%, p = 0.032; periarticular reduction forceps: 87.0% vs. 55.6%, p = 0.005; wire-cutting pliers: 85.2% vs. 25.4%, p < 0.001; T-handle chuck: 74.1% vs. 29.9%, p < 0.001; and large wire driver: 66.7% vs. 25.6%, p < 0.001) but not for the rongeur (48.1 vs. 36.8%, p = 0.274), Fig. 2.
Fig. 1.
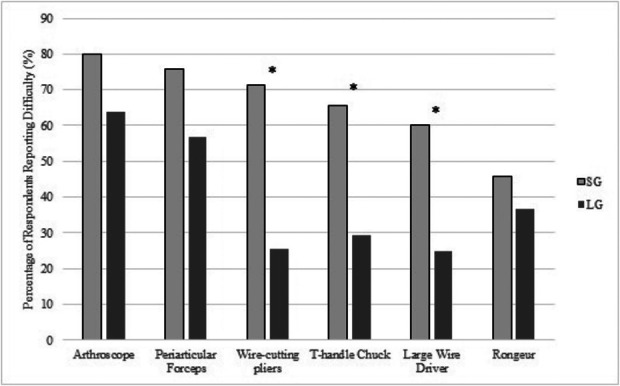
Percentage of residents who reported encountering difficulty using 6 common orthopaedic instruments (arthroscope, periarticular forceps, wire-cutting pliers, T-handle chuck, large wire driver, and rongeur). SG = small glove (≤7.0). LG = large glove (≥7.5). Asterisks indicate p < 0.05.
Fig. 2.
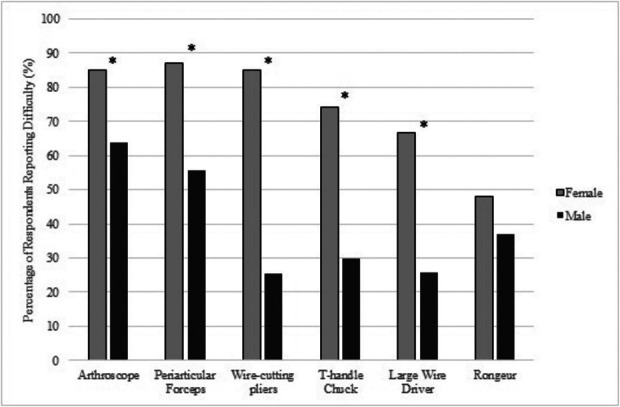
Percentage of residents who reported encountering difficulty using 6 common orthopaedic instruments (arthroscope, periarticular forceps, wire-cutting pliers, T-handle chuck, large wire driver, and rongeur). Asterisks indicate p < 0.05.
TABLE II.
Number of Residents Who Reported Never Experiencing Difficulty Vs. Those Who Reported Some or More Difficulty Using 6 Orthopaedic Instruments*
| SG n (%) | LG n (%) | p value | Female n (%) | Male n (%) | p value | Junior n (%) | Senior n (%) | p value | |
|---|---|---|---|---|---|---|---|---|---|
| Arthroscope | |||||||||
| No difficulty | 7 (20) | 39 (36.1) | 0.076 | 4 (14.8) | 42 (36.2) | 0.032 | 22 (26.5) | 24 (40) | 0.088 |
| Difficulty | 28 (80) | 69 (63.9) | 23 (85.2) | 74 (63.8) | 61 (73.5) | 36 (60) | |||
| Periarticular reduction forceps | |||||||||
| No difficulty | 7 (24.1) | 44 (43.1) | 0.064 | 3 (13) | 48 (44.4) | 0.005 | 24 (33.8) | 27 (45) | 0.19 |
| Difficulty | 22 (75.9) | 58 (56.9) | 20 (87) | 60 (55.6) | 47 (66.2) | 33 (55) | |||
| Wire-cutting pliers | |||||||||
| No difficulty | 10 (28.6) | 82 (74.5) | <0.001 | 4 (14.8) | 88 (74.6) | <0.001 | 51 (60) | 41 (68.3) | 0.305 |
| Difficulty | 25 (71.4) | 28 (25.5) | 23 (85.2) | 30 (25.4) | 34 (40.5) | 19 (31.7) | |||
| T-handle chuck | |||||||||
| No difficulty | 12 (34.3) | 77 (70.6) | <0.001 | 7 (25.9) | 82 (70.1) | <0.001 | 50 (59.5) | 39 (65) | 0.505 |
| Difficulty | 23 (65.7) | 32 (29.4) | 20 (74.1) | 35 (29.9) | 34 (40.5) | 21 (35) | |||
| Large wire driver | |||||||||
| No difficulty | 14 (40) | 82 (75.2) | <0.001 | 9 (33.3) | 87 (74.4) | <0.001 | 47 (56) | 49 (81.7) | 0.001 |
| Difficulty | 21 (60) | 27 (24.8) | 18 (66.7) | 30 (25.6) | 37 (44) | 11 (18.3) | |||
| Rongeur | |||||||||
| No difficulty | 19 (54.3) | 69 (63.3) | 0.341 | 14 (51.9) | 74 (63.2) | 0.274 | 44 (52.4) | 44 (73.3) | 0.011 |
| Difficulty | 16 (45.7) | 40 (36.7) | 13 (48.1) | 43 (36.8) | 40 (47.6) | 16 (26.7) |
SG = small glove (≤7.0). LG = large glove (≥7.5). Junior = PGY1-3. Senior = PGY4-5.
The reported difficulty of the 26 females and 9 males in the SG group was then compared. Female SG residents reported more difficulty with the wire-cutting pliers and the periarticular reduction forceps compared with male SG residents, but there was no difference in difficulty with the rongeur, arthroscope, universal T-handle chuck, or large wire driver. Meaningful statistical analysis by gender was not possible for the LG group, given there was only 1 female in the LG group.
When comparing the junior and senior resident groups, junior residents reported more difficulty with the large wire driver and rongeur (44.0% vs. 18.3%, p = 0.001; and 47.6% vs. 26.7%, p = 0.011; respectively) but not with the remaining instruments.
Hand Fatigue
Self-reported hand fatigue after a typical operating room day was slightly more frequent in the SG group than LG group (85.3% vs. 72.7%, p = 0.135). The frequency of hand fatigue did not significantly differ between junior and senior residents (72.6% vs. 80.0%, p = 0.309). Female residents reported hand fatigue more frequently than males (96.2% vs. 71.2%, p = 0.007).
Agreement Statements
The SG group more frequently agreed with the statement that difficulty with instrument use was related to design flaws than the LG group (50.0% SG in agreement vs. 23.1% LG, p = 0.009), with similar findings when comparing female and male residents (63.2% females in agreement vs. 22.4% males, p < 0.001) (Table III). The SG group also more frequently agreed that it was hard to disclose difficulty using an instrument (74.2% SG in agreement vs. 45.9% LG, p = 0.007), as did female residents (80.0% females vs. 46.2% males, p = 0.003).
TABLE III.
Number of Residents Who Agreed or Strongly Agreed Vs. Disagreed or Strongly Disagreed With 3 Statements Related to Instrument Use*
| SG n (%) | LG n (%) | p value | Female n (%) | Male n (%) | p value | Junior n (%) | Senior n (%) | p value | |
|---|---|---|---|---|---|---|---|---|---|
| “It is hard to admit when using certain instruments is hard for me.” | |||||||||
| Agree | 23 (74.2) | 39 (45.9) | 0.007 | 20 (80) | 42 (46.2) | 0.003 | 41 (61.2) | 21 (42.9) | 0.051 |
| Disagree | 8 (25.8) | 36 (54.1) | 5 (20) | 49 (53.8) | 26 (38.8) | 28 (57.1) | |||
| “The difficulties I encounter using certain instruments are related to my lack of skill based on level of training.” | |||||||||
| Agree | 16 (53.3) | 50 (53.8) | 0.967 | 14 (58.3) | 52 (52.5) | 0.609 | 50 (66.7) | 16 (33.3) | <0.001 |
| Disagree | 14 (46.7) | 43 (46.2) | 10 (41.7) | 47 (47.5) | 25 (33.3) | 32 (66.7) | |||
| “The difficulties I encounter using certain instruments are related to design flaws.” | |||||||||
| Agree | 13 (50) | 18 (23.1) | 0.009 | 12 (63.2) | 19 (22.4) | <0.001 | 12 (18.8) | 19 (47.5) | 0.002 |
| Disagree | 13 (50) | 60 (76.9) | 7 (36.8) | 66 (77.6) | 52 (81.3) | 21 (52.5) |
SG = small glove (≤7.0). LG = large glove (≥7.5). Junior = PGY1-3. Senior = PGY4-5.
Subspecialty Interest
The majority of residents reported that difficulty using instruments would not affect their choice of subspecialty. Junior residents reported that ease of instrument use might affect subspecialty choice more often than senior residents (31.8% vs. 10.0%, p = 0.002). When comparing the SG vs. LG and female vs. male groups, there was no difference in the proportion of residents that reported ease of instrument use might affect their subspecialty choice: (31.4% SG vs. 20.0% LG, p = 0.160; 33.3% females vs. 20.3% males, p = 0.146).
Discussion
The purpose of this study was to describe how often orthopaedic surgery residents perceive difficulty using common orthopaedic instruments and to analyze how GS and gender impacted self-reported difficulty with instrument use. We also investigated whether reported difficulty with instrument use might impact residents' choice of subspecialty. We found that the predominantly male (98.3% male) LG group reported significantly less difficulty than the more gender mixed though still predominantly female (74.3% female) SG group for the wire-cutting pliers, large wire driver, and T-handle chuck. When male and female residents were compared, female residents reported more difficulty with all instruments except the rongeur. A subanalysis within the SG group found that there was no difference between SG female and SG male residents for 4/6 of the instruments, suggesting that hand size might impact difficulty using orthopaedic instruments independently from gender, although the sample size for this comparison was small. Although the close correlation between GS and gender makes it challenging to separate these 2 variables statistically, the high rate of difficulty experienced by male and female residents in the SG group is an important consideration for residency programs, surgeon educators, and instrument manufacturers as the field of orthopaedic surgery continues to become more diverse. Although nearly a third of junior residents reported that difficulty with instrument use might impact their choice of orthopaedic subspecialty, only 10% of senior residents agreed, indicating that most orthopaedic residents are not deterred from their specialty of interest because of instrument-specific issues.
In 2018, the American Academy of Orthopaedic Surgeons made increasing diversity and closing the gender gap among orthopaedic surgeons 1 of its top strategic goals24. In 2021, women made up 16.6% of the orthopaedic surgery residents in the United States, despite women making up 55.6% of new medical school matriculants1,2,25. One of the most common reasons reported by women for not pursuing orthopaedic surgery is the perception that too much physical strength is required26. Poorly sized orthopaedic instruments may contribute to this perception. Ruiz-Ruiz et al.23 found that a grip span (the amount of hand spread when generating force) proportionate to hand size was required for women to achieve maximum grip strength. Fram et al. found that female orthopaedic surgeons and trainees were significantly more likely to report that orthopaedic surgical instruments were difficult or uncomfortable to use and that nearly half of orthopaedic surgeons required medical treatment for symptoms related to using orthopaedic instruments19,27. This demonstrates that discomfort and difficulty with instrument use can lead to clinically significant symptoms that might impact surgeon productivity, satisfaction, and career longevity. In this study, we found that SG and female residents more often reported that difficulty using instruments was related to design flaws in the instruments than their LG and male counterparts. Although the orthopaedic literature concerning this issue is relatively sparse, more extensive research has been conducted in the field of endoscopic and laparoscopic surgery. Berguer and Hreljac.14 found that practicing surgeons using size 6.5 or smaller gloves had significantly more difficulty with one-size laparoscopic instruments and that increased difficulty with instrument use was associated with higher rates of musculoskeletal injuries. Adams et al.12 compared male and female general surgery residents and found that women more often described laparoscopic instruments as “always awkward” and more often were forced to use 2 hands rather than 1 to perform key tasks. In addition to causing instruments to feel awkward, Wong et al.9 found surgeons with smaller hand size experienced a greater grip strength decline and greater ergonomic workload during repetitive laparoscopic tasks. Interestingly, we found no difference in hand fatigue between the SG and LG groups, although female residents reported more hand fatigue than males. Similarly, Armijo et al.13 found that female attending surgeons had significantly higher hand, wrist, and shoulder muscle activation while using laparoscopic instrumentation and concluded that although this increased muscle activation might represent a successful adaption strategy to the tools, it could also put female surgeons at risk of overuse injuries. Collectively, the above studies suggest that tools that are not ergonomically designed or appropriately sized can affect both surgical performance and surgeon health. Our study adds important data regarding orthopaedic residents' experience using common orthopaedic instruments and suggests that both men and women with smaller hand sizes may have greater difficulty with certain orthopaedic instruments.
Limitations
An important methodological limitation to consider when interpreting the results of this study is that we did not evaluate whether self-reported difficulty with instrument use correlated with actual surgical proficiency. Flyckt et al.28 found that female residents self-rated their laparoscopic proficiency approximately 50% lower than their male colleagues did, but performed equivalently on a standardized objective test of laparoscopic skill. In a study comparing 97 male and female orthopaedic surgery residents at the University of Minnesota, there was no difference in any of the 8 Accreditation Council for Graduate Medical Education competencies, technical skills, or overall competency based on faculty evaluations29. Another limitation is related to selection bias. Residents who participate in a survey about difficulty with surgical instruments may be different from nonrespondents. By advertising the survey in a social media group oriented toward female residents, residents who participated in the study may be systematically different from residents as a whole and from female residents as a whole. Because of the very low proportion of female residents in orthopaedics, this was deemed necessary to gather sufficient responses from female residents. Another significant limitation is the small sample size of our study and the low survey response rate. Because surveys were sent to program coordinators, it is possible not all surveys were received by individual residents. In our review of the cited references, the number of respondents is similar to other survey studies assessing surgical performance. Another limitation is that the almost entirely male LG group and predominantly female SG group made it difficult to differentiate the effect of gender vs. GS on ease of instrument use. However, given the significant differences in mean GS between male and female residents, differentiating the effect of gender vs. GS on difficulty with instrument would be difficult regardless of sample size. Finally, although surgeon GS correlates well with hand circumference, it is an imperfect surrogate for more exact measures of hand anthropometry and is affected by individual preferences with regard to glove sizing, the use of inner and outer gloves, and differences between glove manufacturers16.
As gender diversity in orthopaedic surgery increases, there is an opportunity for surgeon educators and residents to scrutinize and improve on orthopaedic surgical education. In this study, we demonstrated that orthopaedic residents with SG sizes, both male and female, reported increased difficulty using common orthopaedic surgical instruments. For residents, particularly those without colleagues and mentors similar to themselves with respect to gender or hand size, this study provides confirmation that experiencing difficulty with certain instruments is a common, shared experience rather than a personal deficiency. For resident educators, we hope this study highlights the different experiences residents have using orthopaedic instruments and spurs consideration of how to help all trainees excel in orthopaedics. Increasing the availability of instruments that are appropriately sized should be part of the solution. The other is to look to the many excellent surgeons who have developed techniques and adaptations to succeed with the instruments available and ensure that these skills are passed on to those who need them.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A628). This content was not copyedited or verified by JBJS.
Footnotes
Investigation performed at the Kirk Kerkorian School of Medicine, University of Nevada Las Vegas
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A627).
Contributor Information
Jessica Albanese, Email: jessicaalbanesemd@gmail.com.
Gayle Allenback, Email: gayle.allenback1@optum.com.
Karen Nelson, Email: karengoldman503@gmail.com.
References
- 1.Ranson R, Mao H, Saker C, Lehane K, Gianakos A, Stamm M, Mulcahey MK. The demographic make-up of orthopaedic surgery residents in the United States post ACGME merger. J Orthop Exp Innov. 2023. [Google Scholar]
- 2.Association of American Medical Colleges. Applicants, first-time applicants, acceptees, and matriculants to U.S. MD-granting medical schools by gender, 2013-2014 through 2022-2023; 2022. Available at: https://www.aamc.org/data-reports/students-residents/data/2022-facts-applicants-and-matriculants-data. Accessed February 3, 2023.
- 3.Davies BT, Benson AK, Courtney A, Minto I, Minto I. A comparison of hand anthropometry of females in three ethnic groups. Ergonomics. 1980;23(2):179-82. [DOI] [PubMed] [Google Scholar]
- 4.Garrett JW. The adult human hand: some anthropometric and biomechanical considerations. Hum Factors. 1971;13(2):117-31. [DOI] [PubMed] [Google Scholar]
- 5.White RM. Comparative anthropometry of the hand. Army natick research and development labs ma clothing equipment and. Mater Eng Lab. 1980:192. [Google Scholar]
- 6.Shepherd JM, Harilingam MR, Hamade A. Ergonomics in laparoscopic surgery-A survey of symptoms and contributing factors. Surg Laparosc Endosc Percutan Tech. 2016;26(1):72-7. [DOI] [PubMed] [Google Scholar]
- 7.Filisetti C, Cho A, Riccipetitoni G, Saxena AK. Analysis of hand size and ergonomics of instruments in pediatric minimally invasive surgery. Surg Laparosc Endosc percutaneous Tech. 2015;25(5):e159-62. [DOI] [PubMed] [Google Scholar]
- 8.Cohen DL, Naik JR, Tamariz LJ, Madanick RD. The perception of gastroenterology fellows towards the relationship between hand size and endoscopic training. Dig Dis Sci. 2008;53(7):1902-9. [DOI] [PubMed] [Google Scholar]
- 9.Wong JMK, Moore KJ, Lewis P, Reid M, Saul K, Carey ET. Ergonomic assessment of surgeon characteristics and laparoscopic device strain in gynecologic surgery. J Minim Invasive Gynecol. 2022;29(12):1357-63. [DOI] [PubMed] [Google Scholar]
- 10.Alleblas CC, De Man AM, Van Den Haak L, Vierhout ME, Jansen FW, Nieboer TE. Prevalence of musculoskeletal disorders among surgeons performing minimally invasive surgery: a systematic review. Ann Surg. 2017;266(6):905-20. [DOI] [PubMed] [Google Scholar]
- 11.Sutton E, Irvin M, Zeigler C, Lee G, Park A. The ergonomics of women in surgery. Surg Endosc. 2014;28(4):1051-5. [DOI] [PubMed] [Google Scholar]
- 12.Adams DM, Fenton SJ, Schirmer BD, Mahvi DM, Horvath K, Nichol P. One size does not fit all: current disposable laparoscopic devices do not fit the needs of female laparoscopic surgeons. Surg Endosc. 2008;22(10):2310-3. [DOI] [PubMed] [Google Scholar]
- 13.Armijo PR, Flores L, Pokala B, Huang CK, Siu KC, Oleynikov D. Gender equity in ergonomics: does muscle effort in laparoscopic surgery differ between men and women? Surg Endosc. 2022;36(1):396-401. [DOI] [PubMed] [Google Scholar]
- 14.Berguer R, Hreljac A. The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc. 2004;18(3):508-12. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez-Margallo JA, Gonzalez Gonzalez A, Garcia Moruno L, Gómez-Blanco JC, Pagador JB, Sanchez-Margallo FM. Comparative study of the use of different sizes of an ergonomic instrument handle for laparoscopic surgery. Appl Sci. 2020;10(4):1526. [Google Scholar]
- 16.Stellon M, Seils D, Mauro C. Assessing the importance of surgeon hand anthropometry on the design of medical devices. J Med Devices. 2017;11(4):041004. [Google Scholar]
- 17.Hislop J, Orth D, Tirosh O, Isaksson M, Hensman C, McCormick J. Does surgeon sex and anthropometry matter for tool usability in traditional laparoscopic surgery? A systematic review and meta-analysis. Surg Endosc. 2023;37(9):6640-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin D, Pena G, Field J, Altree M, Marlow N, Babidge W, Hewett P, Maddern G. What are the demographic predictors in laparoscopic simulator performance? ANZ J Surg. 2016;86(12):983-9. [DOI] [PubMed] [Google Scholar]
- 19.Fram B, Bishop ME, Beredjiklian P, Seigerman D, Fram BR. Female sex is associated with increased reported injury rates and difficulties with use of orthopedic surgical instruments. Cureus. 2021;13(5):e14952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210(3):306-13. [DOI] [PubMed] [Google Scholar]
- 21.Gunther CM, Burger A, Rickert M, Crispin A, Schulz CU. Grip strength in healthy caucasian adults: reference values. J Hand Surg Am. 2008;33(4):558-65. [DOI] [PubMed] [Google Scholar]
- 22.Pazderka MP, Henderson M, Hallbeck MS, Span G. Gender, grip span, anthropometric dimensions, and time effects on grip strength and discomfort. Proc Hum Factors Ergon Soc Annu Meet. 1996;40(13):707-11. [Google Scholar]
- 23.Ruiz-Ruiz J, Mesa JL, Gutierrez A, Castillo MJ. Hand size influences optimal grip span in women but not in men. J Hand Surg Am. 2002;27(5):897-901. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Orthopedic Surgeons. Diversity as an AAOS strategic goal. Available at: https://www.aaos.org/about/diversity-in-orthopaedics/. Accessed June 14, 2023.
- 25.American Association Medical Colleges. Specialty Data Report. Available at: https://www.aamc.org/media/63371/download?attachment. Accessed March 2, 2023. [Google Scholar]
- 26.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016;474(9):1950-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen-Rosenblum AR, Varady NH, Leonovicz O, Chen AF. Repetitive musculoskeletal injuries: a survey of female adult reconstruction surgeons. J Arthroplasty. 2022;37(8):1474-7.e6. [DOI] [PubMed] [Google Scholar]
- 28.Flyckt RL, White EE, Goodman LR, Mohr C, Dutta S, Zanotti KM. The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int. 2017;2017:1945801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pico K, Gioe TJ, Vanheest A, Tatman PJ. Do men outperform women during orthopaedic residency training? Clin Orthop Relat Res. 2010;468(7):1804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


