Abstract
Balneotherapy includes practices and methods using medically and legally recognized mineral-medicinal waters, muds and natural gases from natural springs for therapeutic purposes. One of the most widely used method in balneotherapy is bathing with thermal mineral water. In the course of the years, scientific community has produced an increasing number of evidences that this practice is an effective method for treating signs and symptoms of several pathologies such as rheumatic, cardiovascular and dermatological diseases. This systematic review is aimed at evaluating the effect of balneotherapy with thermal water baths as a treatment to manage signs and symptoms of patients affected by all types of dermatological diseases. The systematic review was conducted according to the PRISMA Statement, and its protocol was registered on PROSPERO platform (CRD42022295913). The research was performed on the databases Pubmed, Scopus, Web of Science and Cochrane. We included clinical trials evaluating the effects of balneotherapy using thermal mineral water baths for managing dermatological diseases in humans, published in English and Italian language. Eight studies were included, seven of them enrolled adults affected by psoriasis and one studied atopic dermatitis patients. The common result of all the articles included was a clear improvement of signs and symptoms of psoriasis and eczematous diseases after use of thermal mineral water baths. These effects seem to be strictly related to physical and chemical properties of thermal water used for balneotherapy. However, studies in this field are still limited to support robust evidence of the effectiveness of balneotherapy using thermal mineral water baths and often their quality is low. Thus, new clinical studies need to be carried out, using more correct methods for conducting the studies and for processing statistical data.
Keywords: Balneotherapy, Dermatological diseases, Systematic review as topic, Mineral water
Introduction
Balneotherapy includes practices and methods using medically and legally recognized mineral-medicinal waters, muds and natural gases from natural springs for therapeutic purposes (Gálvez et al. 2018). One of the most widely used method in balneotherapy is bathing with thermal mineral water (Uzunoglu et al. 2017). This practice has proven positive effects on health depending on its physical and chemical-physical properties, such as temperature, composition and concentration of minerals contents, osmotic pressure and electrical conductivity (Fioravanti et al. 2011). For example, a high temperature of water can trigger anti-inflammatory and immunomodulating effects due to the release of mediators as β-endorphins, enkephalins and irisin (Borroni et al. 2013). Particularly, β-endorphins and enkephalins influence pain perception and regulate the proliferation of the immune cells (Nissen et al. 1998), whereas irisin improves metabolic and cognitive skills (Sacerdote et al. 2001). Besides, when the temperature of thermal water is high, it can act on dilatation of capillaries, increasing the blood flow and decreasing fibrinogen levels, finally improving the thrombotic profile of those undergoing balneotherapy (Aydin et al. 2013; Qiu et al. 2014). In addition, there are several positive outcomes related to the specific chemical contents (and their concentrations) of thermal water, such as sulfur, manganese, magnesium, selenium, strontium, silicon and bicarbonates (Lee et al. 2014; Rodrigues et al. 2017). Given these properties, in the course of the years, scientific community has focalized the attention on the positive effects of balneotherapy, producing an increasing number of evidences that balneotherapy is an effective method for managing pain (Antunes et al. 2019) and for treating signs and symptoms of several pathologies such as rheumatic (Bernetti et al. 2020), cardiovascular (Oyama et al. 2013) and dermatological diseases (Liang et al. 2015). In particular, dermatological diseases are one of the most common pathologies for which balneotherapy involving thermal mineral water baths is used (Huang et al. 2018). This is of great concern for public health because skin conditions are the most common cause for general practice consultation. Indeed, there are more than 3,000 skin diseases (both acute and chronic) affecting until to 70% of people worldwide and posing on patients a relevant burden in terms of quality of life loss and sanitary costs. The high prevalence of dermatological diseases together with their costs has to be carefully considered in planning dermatological care of patients (Richard et al. 2022), and effective treatments are needed in order to manage these diseases. Balneotherapy results an effective treatment for several skin conditions. For example, scientific evidence demonstrated a positive effect of this practice on psoriasis both in term of reducing collateral effects, as skin irritation and pruritus, as in term of safety, since it is a treatment not interfering with any metabolic comorbidities nor drugs, as typically occurs with pharmacological therapy (Timis et al. 2021). In this context, multiple studies reported as an effective balneotherapeutic treatment should last three to four weeks (Péter et al. 2017; Darlenski et al. 2021), although a significant improvement of the PASI index (Psoriasis Area Severity Index – severity score of psoriatic affected area) together with an improvement of life quality can be observed since the first session (Peroni et al. 2008). Besides, a recent narrative review evidenced a great positive effect of balneotherapy on psoriasis and atopic dermatitis and other dermatological conditions and diseases such as pruritus, prurigo, lichen ruber planus, acne vulgaris, and seborrheic dermatitis (Cacciapuoti et al. 2020). In addition, a recent systematic review demonstrated the potential positive effects of balneotherapy on dermatological diseases, but it was focalized on specific conditions such as psoriasis and atopic dermatitis (Moini Jazani et al. 2023). In our knowledge, no recent systematic review summarizes the scientific evidence on balneotherapy and all the known dermatological diseases. This systematic review is aimed at evaluating the effect of balneotherapy using thermal mineral water baths as a treatment to manage signs and symptoms of patients affected by all type of dermatological diseases.
Materials and methods
Research strategy
The present review has been performed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement (Page et al. 2021). The protocol of the review was registered on PROSPERO platform with the following ID: CRD42022295913.
We interrogated the following databases: PubMed (Medline), Scopus, Web of Science (Science and Social Science Citation Index) and Cochrane Library. The research was performed using the keywords and MeSH terms using Boolean operators as AND–OR utilizing the following string: “Balneotherapy” OR “thermal water” OR “mineral water” AND derm*. We choose these keywords and MeSH terms because we focalized the attention on the effect of balneotherapy using thermal mineral water baths. The research included all the articles published up to June 15th 2023.
Inclusion and exclusion criteria
All the articles, regardless of the language, aimed at evaluating the effect of balneotherapy using thermal mineral water baths for the management of dermatological diseases in human beings were included in the present review. Any experimental study on humans was considered eligible, whereas case reports, case series, letters to editors, commentaries, editorials, reviews and observational studies were excluded. All the references cited, both in critical and systematic review and/or in meta-analysis, have been screened in order to detect further references worth mentioning. Any article not matching the inclusion criteria was excluded.
PICOS model was used for structuring the research question, as follows:
Population: Patients having a dermatological disease.
Intervention: Balneotherapy using thermal mineral water baths.
Control: Bathing in drinking water or procedures other than balneotherapy.
Outcomes: Improvement of one or more symptoms and signs of the studied dermatological disease.
Study: experimental study on humans.
The exclusion criteria led to reject all reports not fulfilling both the requirements of this review and the predetermined inclusion criteria.
The references of the selected articles have been copied on Zotero citation management software (RRID:SCR_013784) to delete any duplicate and to evaluate the relevance of each article. Titles and abstracts of potentially eligible studies were independently screened by four investigators (M.V., A.D.G., D.M., C.P.). The group of the four investigators included two content experts (M.V. and C.P.) that assisted with the screening and reviewing process and two graduate students (A.D.G. and D.M.) that assisted with searching, screening, evaluating process. Hereafter, the four researchers focused independently on the full version of the potentially relevant articles. Any disagreement about the selection has been discussed and resolved. In particular, the same four investigators discussed each conflict until agreement was reached or asked to the subject matter expert of the team (M.F.) to resolve the conflict.
Quality evaluation of single study
The eligible full texts resulting at the end of the review process were almost all controlled clinical trials with the exception of one, concerned a not controlled clinical study (open, with no control group) (Costantino and Filippelli 2014).
To date, there is not a universally accepted checklist to assess the methodological quality of clinical studies dealing with any other therapeutic treatments but pharmacological one. Following the methodology previously used by other systematic reviews in this field (Santos et al. 2016), evaluating not pharmacological treatment (Alkaduhimi et al. 2018; Kamioka et al. 2011; Liu et al. 2020), we assessed the quality of any single study using the CLEAR NPT checklist (Checklist to Evaluate a Report of a Non pharmacological Trial). This checklist was specifically thought to evaluate not pharmacological clinical trials by a group of experts, using the Delphi method. It consists of 10 questions having dichotomous answers (yes/not) plus a “not reported” option. In particular, the questions of the checklist investigated the standardization of the intervention, care provider influence, and other measures for minimizing the potential bias deriving from lack of blinding of participants, care providers, and outcome assessors (Boutron et al. 2005). Moreover, we assessed the statistical validity and the quality of adverse /collateral events evaluation using the checklist used by Forestier et al (2016).
Four investigators (M.V., A.D.G., D.M., C.P.) independently evaluated the risk of bias for each single study and the quality of any article included in the review using the above-described checklists. Any incoming disagreement was discussed and resolved. In particular, the same four investigators discussed each conflict until agreement was reached or asked to the subject matter expert of the team (M.F.) to resolve the conflict. According to what pre-established by the authors of both checklists (Forestier et al. 2016): a score ranging from 10 to 8 corresponds to a low risk of bias, a score ranging from 7 to 5 represents a moderate risk and a score lower than 5 stands for a high risk of bias.
Regarding the uncontrolled clinical study (open, no control group), comparing the effects of balneotherapy using thermal mineral water baths on a group of patients before and after treatment, the quality assessment and the evaluation of the bias risk were performed considering the scientific value of the journal, the sample size and the methods used to evaluate patients, in accordance to previous systematic review in this field (Fraioli et al. 2018). However, due to the lack of a control group, the risk of bias has been considered higher.
Results
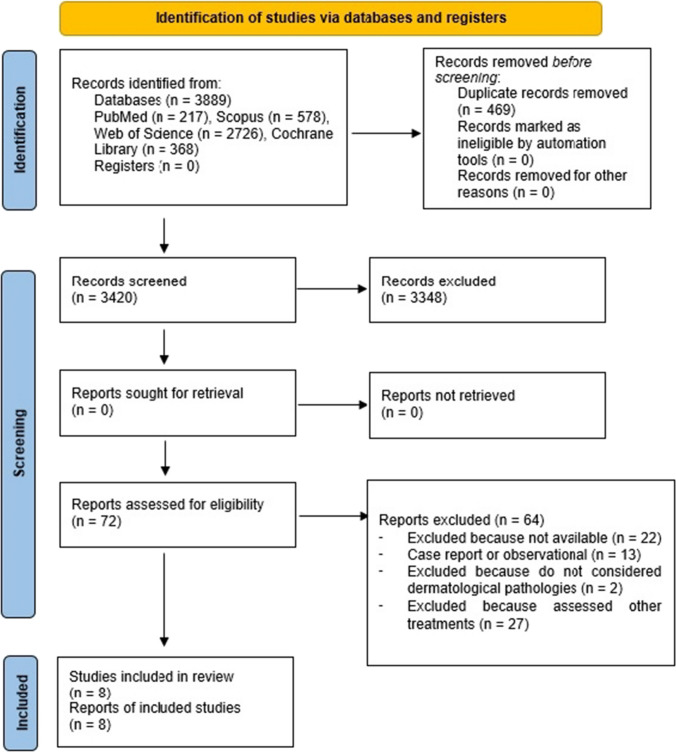
Figure 1 reports the details of the review process.
Fig. 1.
Flow chart describing the research strategy
Eight studies have been finally included in the review and undergone to the quality synthesis. The initial research performed on the databases Pubmed, Scopus, Web of Science and Cochrane produced 3,889 bibliographic citations; 3,420 left after the duplicates removal, of which 3,348 were further excluded because titles and abstracts not responded to the eligibility criteria. 22 articles resulted not available, 42 were excluded because they reported observational studies or not evaluating dermatological diseases or because coupling balneotherapy using thermal mineral water baths to other treatments (UV radiations, Dead Sea salts, topic application or parenteral consumption of thermal water). The references of the selected articles were further assessed for any other relevant citations, but no articles met the inclusion criteria.
Data related to each included article are summarized on Table 1. In particular, we reported the bibliographic references, the thermal centre, the country in which the study was set, the source of funding, the study design, the type of dermatological disease, features of the population studied in terms of gender and age, description of the balneotherapy intervention, description of the control intervention, main results, authors’ conclusions, risk of bias.
Table 1.
Features of the studies included in the review
| Study Country Study design Source of funding Dermatological diseases |
Sample Size and sample features | Balneotherapeutic treatment | Interventions on other groups/controls | Original Authors’ results and conclusions | Quality evaluation according to CLEAR NTP checklist |
|---|---|---|---|---|---|
|
Even-Paz et al. 1996 Israel Controlled clinical study Not reported Psoriasis |
81 (47 cases, 34 controls); age ranging from 16 e 80 years |
Four consecutive weeks of bathing in Dead Sea water or bathing + sun exposition | Just sun light exposure | The PASI significantly improved at the end of all the three tested treatments | High risk of bias |
|
Zumiani et al. 2000 Italy Randomized controlled clinical study Not reported Eczematous dermatitis (atopic and contact dermatitis) |
48 (25 cases, 23 controls); 23 M e 25F mean age equal to 24,5 years | 20 min/day of bathing in warm thermal water (37 °C) for 12 times within 20 days since treatment beginning | 20 min/day of bathing in warm potable water (37 °C) for 12 times within 20 days since treatment beginning | Positive improvement of the clinical index in both groups, with a significant improvement for patients treated with thermal water than those treated with potable water. Skin moisture rapidly increased after bathing in thermal water | Moderate risk of bias |
|
Léauté-Labrèze et al. 2001 France Randomized controlled clinical study Not reported Psoriasis |
71 (22 cases with thermal waters, 21 cases with thermal water and UVB, 24 cases with UVB, 4 “dropped out”); 46 M e 25 F; age ranging from 19 e 76 years (mean 49 years) | 20 min/day of immersion in warm thermal water (35 °C-37°C) for five days a week for three consecutive weeks + intervention group bathing in thermal water + phototherapy with UVB rays | Phototherapy with UVB rays only | A certain improvement of the PASI was described at the end of the three tested treatments and after one year | Moderate risk of bias |
|
Brockow et al. 2007 Germany Single blind controlled clinical study Not reported Psoriasis |
143; 53 F e 90 M; mean age equal to 49,9 ± 13,3 | 20 min/day of immersion in thermal water for three days up to symptoms remission or at maximum for six weeks (18 sessions), each session followed by UVB phototherapy | Use of phototherapy only with UVB, once a day for three days/week up to symptomatology remission or maximum up to six weeks (18 sessions) |
Significant improvement of the PASI at the end of both tested treatments Higher reduction of dermatological symptomatology for the combination balneotherapy + phototherapy than for phototherapy only |
Low risk of bias |
|
Battaglia et al. 2008 Italy Not randomized controlled clinical study Not reported Psoriasis |
100 (50 cases with balneotherapy + phototherapy, 50 cases with balneotherapy only); 44 F e 56 M; age ranging from 21 to 75 years | 20 min/day of immersion in warm thermal water (36 °C) resting the further 15 min, once a day for 12 days + phototherapy with UVB narrow band with increasing dosage | 20 min/day of bathing in warm thermal water (36 °C) resting the further 15 min, once a day for 12 days | Significant improvement of psoriatic symptomatology, with erythema, desquamation, and hyperkeratosis reduction at the end of the treatments. Significant improvement of the PASI at the end of both tested treatments | High risk of bias |
|
Peroni et al. 2008 Italy Not randomized controlled clinical study Private Psoriasis |
280 (156 cases with balneotherapy only, 124 cases with balneotherapy + phototherapy); age ranging from 18 to 85 years | 20 min/day of bathing in warm thermal water (36°-37 °C) once or twice a day on a group of 77 patients for one week and a group of 79 for two weeks | 20 min, once -twice a day, of bathing in warm thermal water (36–37 °C) followed by 15 min of UVB irradiation with increasing intensity, a group of 40 patients for one week and a group of 84 for two weeks | Significant improvement of the PASI at the end of both the treatments tested, after one and two weeks. The improvement of the results has been confirmed by the SAPASI and by the questionnaire on life quality Skindex-29 | Moderate risk of bias |
|
Morri et al. 2012 Italy Randomized controlled clinical study Not reported Psoriasis |
60 (divided into 3 groups of 20); age ranging from 18 to 65 years | 20 min/day of bathing in thermal water, followed by 15 min of rest using cotton towels + a group having balneotherapy and phototherapy using UVB rays, twice a week for 24 times | 24 applications, twice a week of phototherapy only with UVB rays | The PASI resulted significantly improved at the end of tested treatments | Moderate risk of bias |
|
Costantino and Filippelli 2014 Italy Uncontrolled clinical study Not reported Psoriasis |
35; 23% M, 77% F; mean age: 56 ± 19 years (min–max: 17–85 years) | 15 min/day of bathing in warm thermal water (37 °C) 12 times, followed by 15–20 min of controlled, once a day for six days resting the seventh | Not performed | Significant reduction of pruriginous symptomatology, improvement of the NRS score and PASI, improvement of quality of life, improvement of the anxiety-depressive symptomatology related to the dermatological disease | High risk of bias |
PASI index = Psoriasis Area Severity Index; SAPASI index = Self-Administered Psoriasis Area and Severity Index; NRS = Numerical Rating Scale
All the eight studies included in the review were clinical trial, seven of them were controlled (Battaglia et al. 2008; Brockow et al. 2007; Even-Paz et al. 1996; Léauté-Labrèze et al. 2001; Morri et al. 2012; Peroni et al. 2008; Zumiani et al. 2000), while one was open, without a control group (Costantino and Filippelli 2014). Almost all the studies enrolled adults affected by psoriasis and one (Zumiani et al. 2000) involved patients affected by eczematous dermatitis (atopic or contact dermatitis). In this case, balneotherapy were used as an intervention characterized by 20–30 min of bath, once or twice a day for 2–3 weeks’ duration, coupled or not with Sun exposure or UV radiations both for cases and controls (otherwise, the studies have been rejected). The PASI index (Psoriasis Area Severity Index) is considered the outcome index in most of the studies. Some studies considering even the VAS index (Visual Analogue Scale), the NRS index (Numerical Rating Scale), several dermatological symptoms, clinical objective evaluation of patient’s subjective one, skin moisture, quality of life. Some outcomes have been evaluated just at the end of the treatment and/or at the end of up to 3 months’ follow-up period, and compared to the pre-treatment situations or to a control group.
According to the checklist CLEAR NTP or Forestier et al. (2016) for the risk of bias and quality of the studies, three studies have a high risk of bias (included the uncontrolled one), four have a moderate risk and one has a low risk. Moreover, some improvable methodological aspects been underlined by quality, statistical and the significance evaluation. The agreement expressed by the outcomes reached by all the studies allow to lower the bias burden while strengthening the scientific evidences. All the studies showed a significant improvement of one or more signs and/or peculiar symptoms of psoriasis and eczematous dermatitis. Psoriasis is probably the most investigated dermatological disease; seven studies of the review report an improvement of patient’s status after balneotherapy expressed in term of:
PASI index improvement (7/7 articles);
reduction of dermatological symptoms (2/7);
SAPASI index (self-administered psoriasis area and severity index) improvement (1/7);
VAS index (Visual Analogue Scale) improvement (1/7);
improved quality of life (2/7).
Eczematous dermatitis, as demonstrated by studies focusing on this disease, showed some positive variation of clinical indexes when treated with thermal water rather than with potable water. Moreover, skin moisture rapidly improved after thermal bathing.
Discussion
The main finding of the present systematic review is that all the articles included demonstrated a clear improvement of signs and symptoms of psoriasis and eczematous diseases after the treatment with balneotherapy using thermal mineral water baths. According to the authors of the considered articles and to the scientific literature in this field, thermal bathing triggers its clinical effects through a double mechanism: the former, non-specific (hydrotherapy) due to mechanical influences and hydrostatic pressure (crenotherapy) linked to physical and chemical properties of thermal water (Fioravanti et al. 2011; Forestier et al. 2016; Fraioli et al. 2018; O’Hare et al. 1985). As regards to crenotherapy, immersion in thermal waters, particularly in saline (sodium-chloride rich waters) and sulphurous waters, is widely considered an integrative and complementary dermatological treatment due to its keratolytic, regenerative and anti-oxidative effects (Soroka et al. 2008; Peinemann et al. 2020). Besides, several studies reported that chemicals such as sulfur, manganese, magnesium, selenium, strontium, silicon and bicarbonates in thermal water has immunomodulatory effect on skin disorders, especially on atopic dermatitis, contact dermatitis and psoriasis (Lee et al. 2014; Rodrigues et al. 2017). For example, the sulphur can inhibit T-cells proliferation and the production of interleukin -2, interleukin -8, interleukin -23, interleukin -17 and interferon-γ, finally improving inflammation related to the skin disorders previously mentioned (Mirandola et al. 2011). Besides, sulfur and magnesium have bactericide effect against Staphylococcus aureus, which is a typical strain colonizing and complicating skin lesions of atopic dermatitis (Akiyama et al. 2000; Scala et al. 2019), by reinforcing the skin barrier and the immune system, speeding up skin regeneration. An in vitro study demonstrated as thermal water rich in selenium and strontium when in contact with epidermidis cells, can inhibit the production of pro-inflammatory cytokines, particularly of interleukin 6 (Wollenberg et al. 1992). In a systematic review by Khalilzadeh et al. (2019) on the therapeutic effects of thermal water, has been observed as saline waters (sodium-chloride rich) presenting a high content of minerals, can reduce the enzyme leukocyte esterase, involved in psoriasis, the transforming growth factor-β (TGF-β), increased in psoriatic patients, the Langerhans cells of the epidermis and skin infections trough the removal of bacteria that contribute to seborrheic dermatitis and other dermatological diseases.
The present systematic review has some limitations. First of all, statistical analysis of the results of the studies included in the review was not performed because we considered all the dermatological diseases and, thus, it is not possible to compare changes in symptoms and signs of different pathologies. Besides, each included studies used different approaches both for conducting the trial and for evaluating changes in clinical symptoms and signs of the dermatological disease studied. However, this systematic review is the first giving a picture of the positive effects of balneotherapy using thermal mineral water baths on symptoms and signs of all type of dermatological diseases. Secondly, the quality of the studies resulted overall low, with three studies have a high risk of bias, four have a moderate risk and one has a low risk. Nevertheless, the findings of the studies included agree and evidenced a significant improvement of one or more specific signs and/or symptoms of the studied dermatological diseases after the balneotherapy treatments.
Conclusion
The results of the present systematic review evidences that all the included studies demonstrated a significant improvement in signs and/or symptoms of the studied dermatological diseases. However, the quality of the studies included is not so high in several cases because the methodological approaches used to perform the study and/or the elaboration of the results were not completely appropriate. Therefore, it is necessary to carry out further clinical trials with more proper methods to conduct this kind of studies and more advanced techniques to perform statistical elaboration of data.
Author contribution
Conception and design of the work, CP and MV; acquisition of data for the work, CP, ADG, DM, SC, MF and MV; analysis of data for the work, ADG, DM, SC; interpretation of data, CP, MV and MF; drafting the work, ADG, DM, SC; reviewing it critically for important intellectual content, CP, MV and MF. All co-authors have read and agreed to the published version of the manuscript. All co-authors take full responsibility that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Informed consent
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
References
- Akiyama H, Yamasaki O, Tada J, Kubota K, Arata J (2000) Antimicrobial effects of acidic hot-spring water on Staphylococcus aureus strains isolated from atopic dermatitis patients. J Dermatol Sci 24:112–118. 10.1016/s0923-1811(00)00091-8 10.1016/s0923-1811(00)00091-8 [DOI] [PubMed] [Google Scholar]
- Alkaduhimi H, Saarig A, van der Linde JA, Willigenburg NW, van Deurzen DFP, van den Bekerom MPJ (2018) An assessment of quality of randomized controlled trials in shoulder instability surgery using a modification of the clear CLEAR-NPT score. Shoulder Elbow 10:238–249. 10.1177/1758573218754370 10.1177/1758573218754370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antunes JDM, Daher DV, Giaretta VMDA, Ferrari MFM, Posso MBS (2019) Hydrotherapy and crenotherapy in the treatment of pain: Integrative review. BrJP 2:87–98. 10.5935/2595-0118.20190033 10.5935/2595-0118.20190033 [DOI] [Google Scholar]
- Aydin S, Aydin S, Kuloglu T, Yilmaz M, Kalayci M, Sahin I, Cicek D (2013) Alterations of irisin concentrations in saliva and serum of obese and normal-weight subjects, before and after 45 min of a Turkish bath or running. Peptides 50:13–18. 10.1016/j.peptides.2013.09.011 10.1016/j.peptides.2013.09.011 [DOI] [PubMed] [Google Scholar]
- Battaglia E, Marletta F, Meo R, De Luca S, e Nappi G (2008) Photo-balneotherapy vs. balneotherapy in the treatment of psoriatic dermatitis in a thermal environment. Medicina Clinica e Termale 20:13–20 [Google Scholar]
- Bernetti A, Mangone M, Alviti F, Paolucci T, Attanasi C, Murgia M, Di Sante L, Agostini F, Vitale M, Paoloni M (2020) Spa therapy and rehabilitation of musculoskeletal pathologies: a proposal for best practice in Italy. Int J Biometeorol 64:905–914. 10.1007/s00484-019-01731-z 10.1007/s00484-019-01731-z [DOI] [PubMed] [Google Scholar]
- Borroni G, Brazzelli V, Fornara L, Rosso R, Paulli M, Tinelli C, Ciocca O (2013) Clinical, pathological and immunohistochemical effects of arsenical-ferruginous spa waters on mild-to-moderate psoriatic lesions: a randomized placebo-controlled study. Int J Immunopathol Pharmacol 26:495–501. 10.1177/039463201302600223 10.1177/039463201302600223 [DOI] [PubMed] [Google Scholar]
- Boutron I, Moher D, Tugwell P, Giraudeau B, Poiraudeau B, Nizard R, Ravaud P (2005) A checklist to evaluate a report of a nonpharmacological trial (CLEAR NPT) was developed using consensus. J Clin Epidemiol 58:1233–1240. 10.1016/j.jclinepi.2005.05.004 10.1016/j.jclinepi.2005.05.004 [DOI] [PubMed] [Google Scholar]
- Brockow T, Schiener R, Franke A, Resch KL, Peter RU (2007) A pragmatic randomized controlled trial on the effectiveness of low concentrated saline spa water baths followed by ultraviolet B (UVB) compared to UVB only in moderate to severe psoriasis. J Eur Acad Dermatol Venereol 21:1027–1037. 10.1111/j.1468-3083.2007.02152.x 10.1111/j.1468-3083.2007.02152.x [DOI] [PubMed] [Google Scholar]
- Cacciapuoti S, Luciano MA, Megna M, Annunziata MC, Napolitano M, Patruno C, Scala E, Colicchio R, Pagliuca C, Salvatore P, Fabbrocini G (2020) The role of thermal water in chronic skin diseases management: a review of the literature. J Clin Med 9:3047. 10.3390/jcm9093047 10.3390/jcm9093047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantino M, Filippelli A (2014) Impact of SPA therapy with sulphureous mineral water on quality of life and psychological distress in chronic plaque psoriasis. Clin Ter 165:e277–e284. 10.7417/CT.2014.1743 10.7417/CT.2014.1743 [DOI] [PubMed] [Google Scholar]
- Darlenski R, Bogdanov I, Kacheva M, Zheleva D, Demerdjieva Z, Hristakieva E, Fluhr JW, Tsankov N (2021) Disease severity, patient-reported outcomes and skin hydration improve during balneotherapy with hydrocarbonate- and sulphur-rich water of psoriasis. J Eur Acad Dermatol Venereol 35:e196–e198. 10.1111/jdv.16908 10.1111/jdv.16908 [DOI] [PubMed] [Google Scholar]
- Even-Paz Z, Gumon R, Kipnis V, Abels DJ, Efron D (1996) Dead sea sun versus dead sea water in the treatment of psoriasis. J Dermatol Treat 7:83–86. 10.3109/09546639609089534 10.3109/09546639609089534 [DOI] [Google Scholar]
- Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8. 10.1007/s00296-010-1628-6 10.1007/s00296-010-1628-6 [DOI] [PubMed] [Google Scholar]
- Forestier R, Forestier FBE, Alain Francon A (2016) Spa therapy and knee osteoarthritis: A systematic review. Ann Phys Rehabil Med 59:216–226. 10.1016/j.rehab.2016.01.010 10.1016/j.rehab.2016.01.010 [DOI] [PubMed] [Google Scholar]
- Fraioli A, Mennuni G, Fontana M, Nocchi S, Ceccarelli F, Perricone C, Serio A (2018) Efficacy of spa therapy, mud-pack therapy, balneotherapy, and mud-bath therapy in the management of knee osteoarthritis. A systematic review. Biomed Res Int 2018:1042576. 10.1155/2018/1042576 10.1155/2018/1042576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gálvez I, Torres-Piles S, Ortega-Rincón E (2018) Balneotherapy, immune system, and stress response: a hormetic strategy? Int J Mol Sci 19:1687. 10.3390/ijms19061687 10.3390/ijms19061687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang A, Seité S, Adar T (2018) The use of balneotherapy in dermatology. Clin Dermatol 36:363–368. 10.1016/j.clindermatol.2018.03.010 10.1016/j.clindermatol.2018.03.010 [DOI] [PubMed] [Google Scholar]
- Kamioka H, Tsutani K, Mutoh Y, Okuizum H, Ohta M, Handa S, Okada S et al (2011) A systematic review of nonrandomized controlled trials on the curative effects of aquatic exercise. Int J Gen Med 4:239–260. 10.2147/IJGM.S17384 10.2147/IJGM.S17384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalilzadeh S, Shirbeigi L, Naghizadeh A, Mehriardestani M, Shamohammadi S, Tabarrai M (2019) Use of mineral waters in the treatment of psoriasis: Perspectives of Persian and conventional medicine. Dermatol Ther 32:e12969. 10.1111/dth.12969 10.1111/dth.12969 [DOI] [PubMed] [Google Scholar]
- Léauté-Labrèze C, Saillour F, Chêne G, Cazenave C, Luxey-Bellocq ML, Sanciaume C, Toussaint JF, Taïeb A (2001) Saline spa water or combined water and UV-B for psoriasis vs conventional UV-B: lessons from the Salies de Béarn randomized study. Arch Dermatol 137:1035–1039 [PubMed] [Google Scholar]
- Lee YB, Lee JY, Lee HJ, Yun ST, Lee JT, Kim HJ, Yu DS, Woo SY, Kim JW (2014) Immunomodulatory effects of balneotherapy with hae-un-dae thermal water on imiquimod-induced psoriasis-like murine model. Ann Dermatol 26:221–230. 10.5021/ad.2014.26.2.221 10.5021/ad.2014.26.2.221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J, Kang D, Wang Y, Yu Y, Fan J, Takashi E (2015) Carbonate ion-enriched hot spring water promotes skin wounf healing in nude rats. PLoS ONE 10:e0117106. 10.1371/journal.pone.0117106 10.1371/journal.pone.0117106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu F, Cui J, Liu X, Chen KW, Chen X, Li R (2020) The effect of tai chi and Qigong exercise on depression and anxiety of individuals with substance use disorders: a systematic review and meta-analysis. BMC Complement Med Ther 20:161. 10.1186/s12906-020-02967-8 10.1186/s12906-020-02967-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirandola P, Gobbi G, Micheloni C, Vaccarezza M, Di Marcantonio D, Ruscitti F, de Panfilis G, Vitale M (2011) Hydrogen sulfide inhibits IL-8 expression in human keratinocytes via MAP kinase signaling. Lab Invest 91:1188–1194. 10.1038/labinvest.2011.76 10.1038/labinvest.2011.76 [DOI] [PubMed] [Google Scholar]
- Moini Jazani A, Ayati MH, Nadiri AA, Nasimi Doost Azgomi R (2023) Efficacy of hydrotherapy, spa therapy, and balneotherapy for psoriasis and atopic dermatitis: a systematic review. Int J Dermatol 62:177–189. 10.1111/ijd.16080 10.1111/ijd.16080 [DOI] [PubMed] [Google Scholar]
- Morri M, Norat M, Canzi P, Viti S, Mascherpa MA, Angeli P, Angeli F, Romani G (2012) Balneotherapy and narrow-band phototherapy in the treatment of psoriasis: A comparative study. Gazz Med Ital Arch Sci Med 171:739–748 [Google Scholar]
- Nissen JB, Avrach WW, Hansen ES, Stengaard-Pedersen K, Kragballe K (1998) Increased levels of enkephalin following natural sunlight (combined with salt water bathing at the Dead Sea) and ultraviolet A irradiation. Br J Dermatol 139:1012–1019. 10.1046/j.1365-2133.1998.02557.x 10.1046/j.1365-2133.1998.02557.x [DOI] [PubMed] [Google Scholar]
- O’Hare JP, Heywood A, Summerhayes C, Lunn G, Evans JM, Walters G, Corrall RJ, Dieppe PA (1985) Observations on the effects of immersion in Bath spa water. Br Med J (clin Res Ed) 291:1747–1751. 10.1136/bmj.291.6511.1747 10.1136/bmj.291.6511.1747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyama J, Kudo Y, Maeda T, Node K, Makino N (2013) Hyperthermia by bathing in hot spring improves cardiovascular functions and reduces the production of inflammatory cytokines in patients with chronic heart failure. Heart Vessels 28:173–178. 10.1007/s00380-011-0220-7 10.1007/s00380-011-0220-7 [DOI] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. 10.1136/bmj.n71 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peinemann F, Harari M, Peternel S, Chan T, Chan D, Labeit AM, Gambichler T (2020) Indoor salt water baths followed by artificial ultraviolet B light for chronic plaque psoriasis. Cochrane Database Syst Rev 5:CD011941. 10.1002/14651858.CD011941 10.1002/14651858.CD011941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peroni A, Gisondi P, Zanoni M, Girolomoni G (2008) Balneotherapy for chronic plaque psoriasis at Comano spa in Trentino, Italy. Dermatol Ther 21(Suppl 1):S31–S38. 10.1111/j.1529-8019.2008.00200.x 10.1111/j.1529-8019.2008.00200.x [DOI] [PubMed] [Google Scholar]
- Péter I, Jagicza A, Ajtay Z, Boncz I, Kiss I, Szendi K, Kustán P, Németh B (2017) Balneotherapy in psoriasis rehabilitation. In Vivo 31:1163–1168. 10.21873/invivo.11184 [DOI] [PMC free article] [PubMed]
- Qiu Y, Zhu Y, Jia W, Chen S, Meng Q (2014) Spa adjuvant therapy improves diabetic lower extremity arterial disease. Complement Ther Med 22:655–661. 10.1016/j.ctim.2014.05.003 10.1016/j.ctim.2014.05.003 [DOI] [PubMed] [Google Scholar]
- Richard MA, Paul C, Nijsten T, Gisondi P, Salavastru C, Taieb C, Trakatelli M, Puig L, Stratigos A, EADV burden of skin diseases project team (2022) Prevalence of most common skin diseases in Europe: a population-based study. J Eur Acad Dermatol Venereol 36:1088–1096. 10.1111/jdv.18050 10.1111/jdv.18050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues L, Ekundi-Valentim E, Florenzano J, Cerqueira AR, Soares AG, Schmidt TP et al (2017) Protective effects of exogenous and endogenous hydrogen sulfide in mast cell-mediated pruritus and cutaneous acute inflammation in mice. Pharmacol Res 15:255–266. 10.1016/j.phrs.2016.11.006 10.1016/j.phrs.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Sacerdote P, Gaspani L, Panerai AE (2001) Role of beta-endorphin in the modulation of immune responses: perspectives in autoimmune diseases. Adv Exp Med Biol 493:137–142. 10.1007/0-306-47611-8_16 10.1007/0-306-47611-8_16 [DOI] [PubMed] [Google Scholar]
- Santos I, Cantista P, Vasconcelos C (2016) Balneotherapy in rheumatoid arthritis-a systematic review. Int J Biometeorol 60:1287–1301. 10.1007/s00484-015-1108-5 10.1007/s00484-015-1108-5 [DOI] [PubMed] [Google Scholar]
- Scala E, Di Caprio R, Cacciapuoti S, Caiazzo G, Fusco A, Tortorella E, Fabbrocini G, Balato A (2019) A new T helper 17 cytokine in hidradenitis suppurativa: antimicrobial and proinflammatory role of interleukin-26. Br J Dermatol 181:1038–1045. 10.1111/bjd.17854 10.1111/bjd.17854 [DOI] [PubMed] [Google Scholar]
- Soroka Y, Ma’or Z, Leshem Y, Verochovsky L, Neuman R, Brégégère FM, Milner Y (2008) Aged keratinocyte phenotyping: morphology, biochemical markers and effects of Dead Sea minerals. Exp Gerontol 43:947–957. 10.1016/j.exger.2008.08.003 10.1016/j.exger.2008.08.003 [DOI] [PubMed] [Google Scholar]
- Timis TL, Florian IA, Mitrea DR, Orasan R (2021) Mind-body interventions as alternative and complementary therapies for psoriasis: a systematic review of the english literature. Medicina (kaunas) 57:410. 10.3390/medicina57050410 10.3390/medicina57050410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzunoglu E, Yentur S, Kayar AH, Turan M, Donmez A, Direskeneli GS, Erdogan N (2017) Effect of mild heat stress on heat shock protein 70 in a balneotherapy model. Eur J Integr Med 9:86–90. 10.1016/j.eujim.2016.11.014 10.1016/j.eujim.2016.11.014 [DOI] [Google Scholar]
- Wollenberg A, Richard A, Bieber T (1992) In vitro effect of the thermal water from La Roche-Posay on the stimulatory capacity of epidermal Langerhans cells. Eur J Dermatol 2:128–129 [Google Scholar]
- Zumiani G, Zanoni M, Agostini G (2000) Evaluation of the efficacy of Comano thermal baths water versus tap water in the treatment of eczematous dermatitis. G Ital Dermatol Venereol 135:253–258 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.