Abstract
Background
The relationship between 24-hour rest-activity rhythms (RARs) and risk for dementia or mild cognitive impairment (MCI) remains an area of growing interest. Previous studies were often limited by small sample sizes, short follow-ups, and older participants. More studies are required to fully explore the link between disrupted RARs and dementia or MCI in middle-aged and older adults.
Objective
We leveraged the UK Biobank data to examine how RAR disturbances correlate with the risk of developing dementia and MCI in middle-aged and older adults.
Methods
We analyzed the data of 91,517 UK Biobank participants aged between 43 and 79 years. Wrist actigraphy recordings were used to derive nonparametric RAR metrics, including the activity level of the most active 10-hour period (M10) and its midpoint, the activity level of the least active 5-hour period (L5) and its midpoint, relative amplitude (RA) of the 24-hour cycle [RA=(M10-L5)/(M10+L5)], interdaily stability, and intradaily variability, as well as the amplitude and acrophase of 24-hour rhythms (cosinor analysis). We used Cox proportional hazards models to examine the associations between baseline RAR and subsequent incidence of dementia or MCI, adjusting for demographic characteristics, comorbidities, lifestyle factors, shiftwork status, and genetic risk for Alzheimer's disease.
Results
During the follow-up of up to 7.5 years, 555 participants developed MCI or dementia. The dementia or MCI risk increased for those with lower M10 activity (hazard ratio [HR] 1.28, 95% CI 1.14-1.44, per 1-SD decrease), higher L5 activity (HR 1.15, 95% CI 1.10-1.21, per 1-SD increase), lower RA (HR 1.23, 95% CI 1.16-1.29, per 1-SD decrease), lower amplitude (HR 1.32, 95% CI 1.17-1.49, per 1-SD decrease), and higher intradaily variability (HR 1.14, 95% CI 1.05-1.24, per 1-SD increase) as well as advanced L5 midpoint (HR 0.92, 95% CI 0.85-0.99, per 1-SD advance). These associations were similar in people aged <70 and >70 years, and in non–shift workers, and they were independent of genetic and cardiovascular risk factors. No significant associations were observed for M10 midpoint, interdaily stability, or acrophase.
Conclusions
Based on findings from a large sample of middle-to-older adults with objective RAR assessment and almost 8-years of follow-up, we suggest that suppressed and fragmented daily activity rhythms precede the onset of dementia or MCI and may serve as risk biomarkers for preclinical dementia in middle-aged and older adults.
Keywords: circadian rhythm, dementia, actigraphy, cognitive decline, RAR, rest-activity rhythms, cognitive impairment
Introduction
Dementia represents a major public health concern with profound social, economic, and health care implications, and it is a leading cause of disability and dependency among the older adult population. It is estimated that over 55 million individuals worldwide are affected by dementia [1]. As the global population ages, understanding the etiology and potential risk factors associated with dementia has become a critical area of research. While the pathogenesis of dementia remains multifactorial and complex, recent studies have underscored the link of disrupted daily rest-activity rhythms (RARs) to cognitive decline and the development of dementia in older adults [2,3].
The RAR is governed by the circadian system and interacts with the daily cycles of behavioral and environmental changes, which is crucial for maintaining optimal physiological functioning and coordination of bodily processes [4]. The circadian system consists of a network of circadian clocks in the brain and peripheral organs, and these clocks can be affected or reset by environmental conditions, work schedules and social patterns via different time cue inputs including light exposure, food intake, and physical activity [5]. The importance of well-functioning circadian regulation in overall health has been widely recognized. Studies have demonstrated that disruptions in the RAR are associated with various adverse health conditions, including cancer [6], cardiovascular diseases [7], digestive diseases [6], respiratory diseases [6,8], and depression [9]. In recent years, emerging evidence has suggested that disruptions in the RAR could contribute to neurodegenerative processes and cognitive impairment [2,10,11]. However, there are notable limitations in previous studies such as small sample size [12-17], cross-sectional design [10,18-27], focusing on only older population [12,14-17], and short follow-up duration [14,15].
In this study, we used data from more than 94,000 participants aged 43-79 years in a large prospective cohort study, the UK Biobank (UKB), with at least 6 continuous days of wrist actigraphy recording and up to 7.5 years of follow-up to examine the association of RAR measures with future risk of dementia or mild cognitive impairment (MCI). We also explored the potential effects of age, genetics, and shiftwork on this association. We hypothesized that disrupted RAR patterns such as suppressed and fragmented 24-hour activity rhythms are associated with a higher risk of developing dementia or MCI.
Methods
Study Population and Data Source
We used longitudinal data on UKB participants (age range at baseline 43-79 years; 54% female) [28]. Upon enrollment, UKB participants completed a series of questionnaires that collected their demographic, lifestyle, and medical history information. Participants consented to releasing their electronic health records from the United Kingdom’s centralized National Health Service (NHS), which were then stored in the UKB’s Hospital Inpatient Data library [29]. In the UKB cohort, 103,711 participants completed actigraphy assessments between 2013 and 2015 (2.8 to 9.7 years after enrollment) [29]—the baseline of this study. We used follow-up data until September 2021 (maximum and median follow-up after actigraphy: 7.5 and 5 years, respectively). After excluding those participants with poor calibration of activity counts, significant gaps in data likely due to off-wrist periods, <6 days of collected data, dementia or MCI at baseline, or any missing covariate, 91,517 participants were included in this study.
Ethical Considerations
The UKB received approval from the North West Multi-centre Research Ethics Committee (11/NW/03820; 16/NW/0274; 21/NW/0157). This study was conducted under the terms of the UKB (33883) and Mass General Brigham Institutional Review Board (#2018P000356).
Assessment of RARs
Participants wore triaxial accelerometer devices (Axivity AX3; Axivity Ltd) for up to 7 days during the collection period. Prior actigraphy assessment of older adults [30,31] and existing criteria from the UKB [32] were used to perform quality checks. Activity counts in each 15-second epoch were derived from accelerometer data sampled at ~100 Hz (see Multimedia Appendix 1 [29,33]). The first 6 days of activity counts were used to obtain the following nonparametric RAR measures [34]: (1) activity counts during the most active 10-hour period of the 24-hour cycle (M10) and (2) the midpoint of the M10 period (M10 midpoint); (3) activity counts during the least active 5-hour period of the 24-hour cycle (L5)—likely representing hours during sleep, and (4) the timing midpoint of the L5 period (L5 midpoint); (5) relative amplitude (RA) calculated as (M10-L5)/(M10+L5)—representing the robustness of a 24-hour rest-activity cycle; (6) interdaily stability (IS) that quantifies the stability of the 24-hour rhythm between different days (Multimedia Appendix 2); and (7) intradaily variability (IV) that describes the fragmentation of the rhythm (Multimedia Appendix 2). Cosinor analysis was also performed to derive 2 additional measures of 24-hour activity rhythms: the amplitude (midline to peak) and acrophase (time of the peak) of the 24-hour rhythm. All RAR data analyses were performed using the eZActi2 software [35,36].
Assessment of Dementia and MCI
Study participant hospitalization records were kept within the UK’s NHS during the follow-up period before being released by the UKB. The UKB provided algorithmically defined incidence of health matters from ICD-10 (International Classification of Disease, 10th Revision) codes. We obtained data from clinical coding of dementia (ICD-10 code: F05) and MCI (ICD-10 code: F0.67), and from the UKB algorithm “date of all-cause dementia” (field 42018). Age at death or the date of death was based on the death certificates in the NHS. The first occurrence of dementia or MCI (time-to-event) was the first date of diagnosis relative to the actigraphy assessment date.
Assessment of Covariates
The following covariates that may affect RARs were considered in this study: (1) demographics, including age at actigraphy, male or female designated sex of individuals, self-reported ethnicity as European or non-European, college-level education (reported as yes or no), and the Townsend deprivation index; (2) comorbidities, including sleep apnea (based on ICD-10 code G47.30), circulatory disease (based on reports of high cholesterol, diabetes, hypertension, ischemic heart disease, smoking, and peripheral vascular disease), BMI >30, and morbidity burden (classified at the time of actigraphy as none, moderate, or high based on previously used methods that summed the presence of diseases or disorders of the endocrine, connective tissue, gastrointestinal, hematological, musculoskeletal, immune, renal, and respiratory systems as well as any cancers) [37-40]; (3) lifestyle, including alcohol intake (categorized by daily use, 3-4 times per week, 1-2 times per week, a few times per month, and never), smoking status (categorized as current, previous, and never); (4) shiftwork (yes or no); and (5) genetics based on the polygenic risk score (PRS) for Alzheimer disease. We calculated the single PRS for Alzheimer disease using the PRS continuous shrinkage [41] method. This method calculates posterior effect size from genome-wide association study summary statistics with models comprising information of local linkage disequilibrium patterns, and thus reduces PRS error and improves performance. In this study we used genome-wide association study summary statistics from a recent study for Alzheimer disease [42], and the linkage disequilibrium reference panel matrices from the UKB. The PRS continuous shrinkage default settings were used, and after deriving the posterior summary statistics, we used PLINK2 [43,44].
Statistical Analysis
Cox proportional hazard models were used to assess the associations of RAR measures with the subsequent incidence of dementia or MCI. The results were reported as hazard ratios (HRs) with corresponding 95% CIs. For each RAR measure (except M10 midpoint, L5 midpoint, and phase), participants were divided into 4 quartiles (Q1-Q4). The highest quartile (Q4) was used as a reference for RA, M10, IS, and 24-hour amplitude; the lowest quartile (Q1) was used as a reference for L5 and IV. These reference levels were chosen based on prior findings and our hypothesis regarding the direction of the association of each RAR measure with the risk of dementia and MCI, that is, the level of the RAR measure that is hypothesized to be linked to the lowest risk of developing dementia was considered as the reference [37]. Acrophase, M10 midpoint, and L5 midpoint were categorized into 3 tertiles: earlier (6:00 AM-1:34 PM for acrophase, 6:00 AM-12:58 PM for M10 midpoint, and noon-2:47 AM for L5 midpoint), middle (1:34 PM-2:25 PM for acrophase, 12:58 PM-2:01 PM for M10 midpoint, and 2:47 AM-3:44 AM for L5 midpoint), and later (2:25 AM-6:00 AM for acrophase, 2:01 AM-6:00 AM for M10 midpoint, and 3:44 AM-noon for L5 midpoint) groups, and the middle groups were used as the reference [14,15,17]. Separate Cox models were also used to obtain HRs for 1 SD change in each RAR measure. Secondary analyses were performed to investigate (1) the associations between RAR measures and the risk of developing dementia (by excluding participants who only developed MCI); (2) the associations between RAR measures and risk of developing dementia or MCI after excluding those participants who were shift workers at baseline; (3) the interaction effects of Alzheimer disease PRS (<median PRS vs >median PRS) and RAR measures on the risk of developing dementia or MCI (by including interaction terms and also stratifying participants based on their PRS values); and (4) the interaction effects of age (<70 vs ≥70 years) and RAR measures on the risk of developing dementia or MCI (by including interaction terms and also stratifying participants based on their age). All statistical analyses were performed using JMP Pro (version 16, SAS Institute).
Results
Participant Characteristics
Table 1 describes the demographic, lifestyle, and clinical comorbidity data gathered from the 91,517 UKB participants who were included in this study. Most participants were of White European descent (>95%). In comparison to the 90,962 participants who did not develop dementia or MCI, those who did (n=555) were older (69.6 vs 62.4 years) and more likely to be male (n=308, 55.5% vs n=39,758, 43.7%), had lower levels of education (n=215, 38.7% vs n=39,372, 43.3% attended college), had a higher prevalence of sleep apnea (n=10, 1.8% vs n=771, 0.8%), and circulatory system disease (n=261, 47% vs n=22,273, 24.4%), had a higher morbidity burden (2.0, SD 1.8 vs 1.1, SD 1.3), and were more likely to be current or past smokers (n=40, 7.2% vs n=6271, 6.9% and n=342, 61.6% vs n=48,428, 53.2%).
Table 1.
Baseline demographics, lifestyle, and clinical comorbidities of participants (n=91,517), by dementia or MCIa status at follow-upb.
|
|
Participants who developed dementia or MCI (n=555) | Participants who did not develop dementia or MCI (n=90,962) | ||||||
| Demographicsc | ||||||||
|
|
Age at actigraphy (years), mean (SD) | 69.6 (5.4) | 62.4 (7.8) | |||||
|
|
Sex, n (%) | |||||||
|
|
|
Male | 308 (55.5) | 39,758 (43.7) | ||||
|
|
|
Female | 247 (44.5) | 51,204 (56.3) | ||||
|
|
Attended college, n (%) | 215 (38.7) | 39,372 (43.3) | |||||
|
|
Townsend deprivation index (higher)d, n (%) | 274 (49.4) | 45,007 (49.5) | |||||
|
|
European ethnic background | 535 (96.4) | 87,951 (96.7) | |||||
| Rest-activity rhythmicity characteristics, mean (SD) | ||||||||
|
|
Relative amplitude | 0.953 (0.047) | 0.956 (0.035) | |||||
|
|
Amplitude (24-hour, AUe) | 28.0 (15.9) | 33.3 (15.9) | |||||
|
|
M10f (countg) | 127,003 (58,873) | 149,468 (61,082) | |||||
|
|
L5h (count) | 2708 (2622) | 2367 (2565) | |||||
|
|
Phase (hours after midnight) | 13.79 (1.18) | 14.02 (1.24) | |||||
|
|
IVh, AU | 0.95 (0.24) | 0.91 (0.24) | |||||
|
|
ISi, AU | 0.54 (0.13) | 0.52 (0.13) | |||||
| Comorbidities | ||||||||
|
|
Sleep apnea, n (%) | 10 (1.8) | 771 (0.8) | |||||
|
|
Circulatory system disease, n (%) | 261 (47) | 22,273 (24.4) | |||||
|
|
BMI > 30 kg/m2, n (%) | 125 (22.5) | 17,586 (19.3) | |||||
|
|
Morbidity burden (number of diagnoses), mean (SD) | 2.0 (1.8) | 1.1 (1.3) | |||||
|
|
Alcohol intake, n (%) | |||||||
|
|
|
Daily | 160 (28.8) | 20,833 (22.9) | ||||
|
|
|
3 to 4 times per week | 117 (21.1) | 23,643 (26.0) | ||||
|
|
|
Once or twice per week | 104 (18.7) | 22,830 (25.1) | ||||
|
|
|
Few times per month | 114 (20.5) | 18,522 (20.4) | ||||
|
|
|
Never | 60 (10.8) | 5134 (5.6) | ||||
|
|
Smoking status, n (%) | |||||||
|
|
|
Current | 40 (7.2) | 6271 (6.9) | ||||
|
|
|
Previous | 342 (61.6) | 48,428 (53.2) | ||||
|
|
|
Never | 173 (31.2) | 36,263 (39.9) | ||||
|
|
Shiftwork, n (%) | 18 (3.2) | 7351 (8.1) | |||||
aMCI: mild cognitive impairment.
bCardiovascular disease means the presence of any of the following: hypertension, high cholesterol, smoking, diabetes, ischemic heart disease, and peripheral vascular disease.
cData come from recruitment between 2.8 and 9.7 years before actigraphy.
dParticipants that scored above the median Townsend deprivation index.
eAU: arbitrary unit.
fM10: activity level of the most active 10-hour period.
gCount: relative mean change in acceleration.
hL5: activity level of the least active 5-hour period.
iIV: intradaily variability.
jIS: interdaily stability.
RARs and Incident Dementia or MCI
Table 2 presents multivariable-adjusted HRs for dementia or MCI associated with RAR metrics when considered as quartiles of exposure or per SD difference. Figure 1 shows survival plots for incident dementia or MCI associated with RAR metrics. The risk of dementia or MCI was statistically higher in those with more suppressed and fragmented 24-hour activity rhythms as quantified by lower RA (multivariable-adjusted HR per 1-SD decrease=1.23, 95% CI 1.16-1.29; Q1 vs Q4, HR 1.88, 95% CI 1.46-2.41; Figure 1A), lower M10 (multivariable-adjusted HR per 1-SD decrease=1.28, 95% CI 1.14-1.44; Q1 vs Q4, HR 1.69, 95% CI 1.30-2.19; Figure 1B), higher L5 (multivariable-adjusted HR per 1-SD increase=1.15, 95% CI 1.10-1.21; Q4 vs Q1, HR 1.51, 95% CI 1.19-1.91; Figure 1C), and larger IV (multivariable-adjusted HR per 1-SD increase=1.14, 95% CI 1.05-1.24; Q4 vs Q1, HR 1.56, 95% CI 1.20-2.02; Figure 1D). Consistently, the risk of dementia or MCI was statistically higher in those with smaller 24-hour amplitude based on cosinor analysis (multivariable-adjusted HR per 1-SD decrease=1.32, 95% CI 1.17-1.49; Q1 vs Q4, HR 1.86, 95% CI 1.42-2.42; Figure 1E). In addition, participants with delayed L5 midpoint had a lower risk for dementia or MCI (multivariable-adjusted HR per 1-SD increase or ~75 min delay in L5 midpoint=0.92, 95% CI 0.85-0.99; Figure 1G). IS (Figure 1F), M10 midpoint (Figure 1H), and acrophase (Figure 1I) had no significant associations with the risk of dementia or MCI.
Table 2.
Relationships of RARa measures with risk of developing dementia or MCIb,c.
| RAR characteristics | Adjusted hazard ratio (95% CI) | |
| Relative amplitude | ||
|
|
Q1d | 1.88 (1.46-2.41) |
|
|
Q2 | 1.29 (0.99-1.67) |
|
|
Q3 | 0.94 (0.71-1.26) |
|
|
Q4 | Reference |
|
|
Per 1-SD decrease | 1.23 (1.16-1.29) |
| M10e | ||
|
|
Q1 | 1.69 (1.30-2.19) |
|
|
Q2 | 1.11 (0.83-1.47) |
|
|
Q3 | 1.03 (0.76-1.38) |
|
|
Q4 | Reference |
|
|
Per 1-SD decrease | 1.28 (1.14-1.44) |
| M10 midpoint | ||
|
|
Earlier | 1.10 (0.90-1.34) |
|
|
Middle | Ref |
|
|
Later | 1.03 (0.83-1.27) |
|
|
Per 1-SD increase | 0.93 (0.84-1.03) |
| L5f | ||
|
|
Q1 | Reference |
|
|
Q2 | 1.23 (0.96-1.57) |
|
|
Q3 | 1.00 (0.78-1.30) |
|
|
Q4 | 1.51 (1.19-1.91) |
|
|
Per 1-SD increase | 1.15 (1.10-1.21) |
| L5 midpoint | ||
|
|
Earlier | 1.06 (0.87-1.30) |
|
|
Middle | Reference |
|
|
Later | 0.86 (0.70-1.06) |
|
|
Per 1-SD increase | 0.92 (0.85-0.99) |
| IVg | ||
|
|
Q1 | Reference |
|
|
Q2 | 1.64 (1.27-2.12) |
|
|
Q3 | 1.37 (1.05-1.78) |
|
|
Q4 | 1.56 (1.20-2.02) |
|
|
Per 1-SD increase | 1.14 (1.05-1.24) |
| ISh | ||
|
|
Q1 | 1.00 (0.78-1.27) |
|
|
Q2 | 0.82 (0.64-1.05) |
|
|
Q3 | 1.01 (0.81-1.26) |
|
|
Q4 | Reference |
|
|
Per 1-SD decrease | 0.98 (0.89-1.07) |
| Amplitude | ||
|
|
Q1 | 1.86 (1.42-2.42) |
|
|
Q2 | 1.28 (0.96-1.70) |
|
|
Q3 | 1.22 (0.91-1.63) |
|
|
Q4 | Reference |
|
|
Per 1-SD decrease | 1.32 (1.17-1.49) |
| Acrophase | ||
|
|
Earlier | 0.99 (0.81-1.20) |
|
|
Middle | Reference |
|
|
Later | 0.90 (0.73-1.13) |
|
|
Per 1-SD increase | 0.93 (0.85-1.02) |
aRAR: rest-activity rhythm.
bMCI: mild cognitive impairment.
cModels are adjusted for age at the time of actigraphy, sex, education, Townsend deprivation index, ethnic background, obesity, sleep apnea, morbidity burdens, circulatory disorders, night shiftwork status, alcohol intake, smoking status, and polygenic risk score of Alzheimer disease.
dQ: quartile.
eM10: activity level of the most active 10-hour period.
fL5: activity level of the least active 5-hour period.
gIV: intradaily variability.
hIS: interdaily stability.
Figure 1.
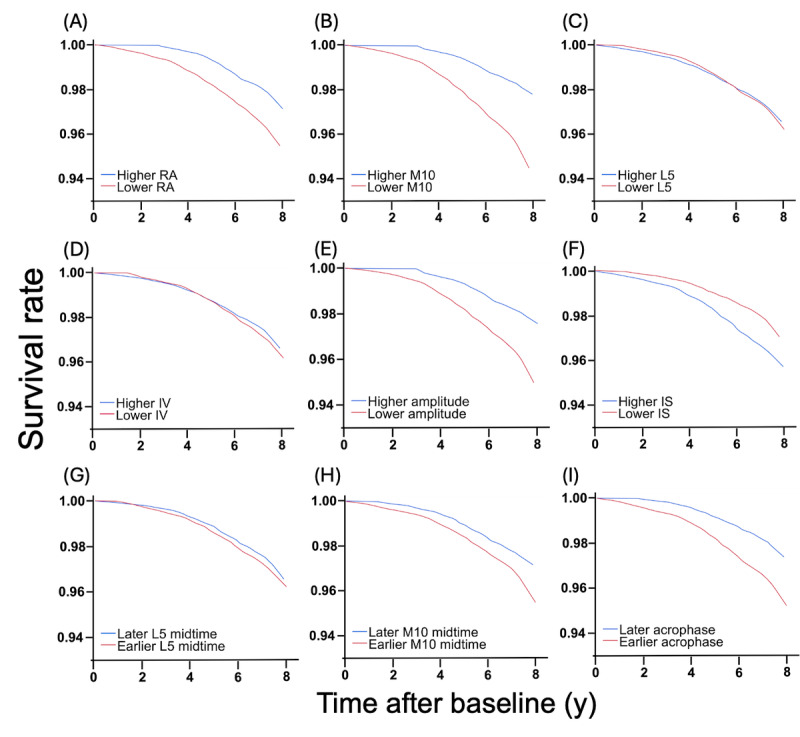
Rest-activity rhythm and risk of developing dementia or MCI. Survival curves for dementia or MCI since baseline (actigraphy assessment) for (A) participants with lower RA (1st quartile) and higher RA (4th quartile), (B) participants with lower M10 (1st quartile) and higher M10 (4th quartile), (C) participants with lower L5 (1st quartile) and higher L5 (4th quartile), (D) participants with lower IV (1st quartile) and higher IV (4th quartile), (E) participants with lower amplitude (1st quartile) and higher amplitude (4th quartile), (F) participants with lower IS (1st quartile) and higher IS (4th quartile), (G) participants with earlier L5 midpoint (1st tertile) and later L5 midpoint (3rd tertile), (H) participants with earlier M10 midpoint (1st tertile) and later M10 midpoint (3rd tertile), and (I) participants with earlier acrophase (1st tertile) and later acrophase (3rd tertile). IS: interdaily stability; IV: intradaily variability; L5: activity level of the least active 5-hour period; M10: activity level of the most active 10-hour period; MCI: mild cognitive impairment; RA: relative amplitude.
In addition, we found that the risk was higher for older participants (multivariable-adjusted HR for each year older at baseline=1.17, 95% CI 1.15-1.19) and male participants (multivariable-adjusted HR 1.33, 95% CI 1.11-1.58).
The associations between RAR measures and incident dementia or MCI remained similar when including only participants who developed dementia (Multimedia Appendix 3) or when excluding those shift workers (Multimedia Appendix 4). In addition, the associations between RAR metrics and risk of dementia or MCI were independent of PRS (P values >.10 for the interaction terms of PRS and all RAR measures; Multimedia Appendix 5) while higher PRS was associated with an increased risk of dementia or MCI (multivariable-adjusted HR per 1-SD increase=1.48, 95% CI 1.36-1.60). Moreover, the RAR-dementia or MCI associations appeared to be similar for the younger (<70 years old) and older (≥70 years old) participants (P values >.10 for the interaction terms of age group and all RAR measures, except M10; Multimedia Appendix 6).
Discussion
Principal Findings
In this large, prospective cohort study, we evaluated the association between RAR metrics, derived from wrist actigraphy, and incidence of dementia or MCI during a follow-up of up to 7.5 years. Our results underscore the significance of specific RAR metrics, notably RA, M10, amplitude, L5, L5 midpoint, and IV in delineating the dementia or MCI risk, independent of previously identified risk factors for dementia or cognitive decline.
Unlike previous studies, our analysis is based on a notably large sample size of >94,000 participants, using objective actigraphy assessments for RAR and spanning a broad age range of 43-79 years. This study adopted a longitudinal design with nearly 8 years of follow-up and comprehensively adjusted for known confounders, including demographic, shiftwork status, lifestyle, comorbidity, and genetics, to enhance the robustness of the results. Specifically, we showed that suppressed 24-hour rhythmicity (lower RA and 24-hour amplitude), accompanied by reduced activity levels (M10) during the active phase and increased activity levels during the resting phase (L5) as well as fragmented 24-hour rhythms (greater IV), were linked to the higher risk for dementia or MCI. These results are consistent with previous studies. For instance, using the Rush Memory and Aging Project data, the risk for Alzheimer dementia was higher in those with lower 24-hour amplitude and greater IV [12]; a longitudinal study of 2496 older men indicated that a larger increase in IV over a span of 7.5 years was associated with a steeper decline in Modified Mini-Mental State Examination scores [16]; and another study of 763 older women showed that reduction in RA was associated with elevated risks for MCI and probable dementia [17]. It is worth noting that our study showed consistent adverse impacts of disrupted rest-active rhythms across different age groups (≥70 years and <70 years).
Regarding the mechanisms underlying the RAR-dementia link, disturbances in circadian regulation and sleep-wake cycles have been proposed as one of the common pathological pathways [3]. Supporting this concept, shift work, an established major cause of circadian or sleep disturbances, has been linked to a higher risk for developing dementia [45-47]; and Musiek et al [22] identified a relationship between increased IV and amyloid plaque pathology in preclinical Alzheimer disease. Clearly, circadian disturbances not only occur in shift workers but also may be caused by other factors such as traveling in different time zones and social jet lag [48,49]. Consistently, we found that the associations of RAR disturbances with dementia risk remained in non–shift workers.
One “unexpected” result was the nonsignificant association of the stability measure (IS) of 24-hour rhythms with the risk for dementia or MCI because the reduction in IS has been linked to aging and dementia [12,26]. Notably, while other studies have similarly reported a lack of significant associations [13,14,17], our research contributes to more definitive insights into these complex associations with a substantially larger sample size. In a related study, Park et al [50] reported higher IS in older adults when compared to younger adults, and interpreted the results as the consequence of changes in daily schedules. This study raises a potential concern about the masking effect of daily schedules on RAR measures, especially IS [51]. An important follow-up question is how reliable IS can be in reflecting intrinsic changes in circadian regulation or predicting or capturing the long-term impacts of acute disturbed 24-hour behavioral cycles on circadian health and related cognitive changes. Future studies including circadian rhythms of other physiological variables or mathematical modeling for estimation of circadian rhythms [52-56] are needed to address the question.
The relationship between the RAR phase and dementia or MCI risk is still inconclusive. Our study identified earlier L5 mid-time as a risk factor for dementia or MCI, but not changes in acrophase or M10 mid-time. L5 mid-time is usually related to the timing of sleep, whereas M10 mid-time and acrophase are usually related to the timing of peak activity. Previous research has yielded varied results. For example, Lysen et al [13] did not observe any association between the circadian phase measured by L5 onset and risk of dementia or MCI, whereas Posner et al [14] observed an association between earlier L5 midpoint (but not M10 midpoint) with higher risk for dementia (but not MCI) [14]. Xiao et al [17] reported a significant linear association of delayed acrophase, M10, and L5 midpoints with a higher risk for dementia or MCI in older women. These inconsistent findings might be explained by unadjusted confounders that influence sleep timing, such as chronotype (ie, preferred sleep time), sleep disorders (eg, insomnia), use of sleep medication, and photoperiod. Future studies should consider controlling for such factors when clarifying relationships between the RAR phase and dementia or MCI.
Clinical Implications and Future Research
Our findings provide insights into the clinical practice and future research in dementia and MCI prevention, screening, and intervention. Specifically, incorporating assessments of sleep and rest-activity patterns into routine health evaluations might be beneficial for middle-aged and older adults. In geriatric care, routine monitoring and management of RAR may help evaluate the factors affecting cognitive health. Educating caregivers and family members about the importance of consistent rest-activity patterns could be incorporated into the home-based care for individuals at risk. Tailoring preventive and therapeutic strategies to individuals based on their RAR characteristics, especially in populations like shift workers, could also be effective. Future research should further clarify the causality of the associations between RAR and cognition, and test whether interventions that improve sleep hygiene, modify light exposure, or adjust physical activity levels can positively impact RAR and, consequently, help prevent or slow cognitive decline.
Strengths and Limitations
The strengths of this study include having a large sample size of more than 94,000 participants; using objective assessments of RAR using actigraphy; controlling for a large number of confounders, including demographic, lifestyle, comorbidity, genetics, and morbidity burden; large age range of participants (aged between 43 and 79 years); and the longitudinal study design with nearly 8 years of follow-up. Limitations of our study are as follows: (1) the majority of participants were of White European descent (>95%), limiting our ability to investigate racial or ethnic differences in the associations; (2) the rate of dementia or MCI events (~550 out of 94,000) appeared to be relatively low due to the overall young age of the participants (median age 63.5 years); (3) we were unable to differentiate between different types of dementia. However, this provides a great opportunity for future studies, when the participants became older, to investigate the long-term association of RAR and different types of dementia or MCI; (4) single-time assessment of actigraphy and covariates did not allow us to examine changes in RAR and dementia risk; (5) internal circadian clocks and environmental factors such as light exposure and social obligations were not assessed or controlled such that it is not possible to separate intrinsic and extrinsic influences on RAR.
Conclusions
We found that altered daily rest-activity patterns were linked to future risk of dementia or MCI, independent of other known risk factors. Monitoring of ambulatory daily motor activity or rest-activity patterns with wearable devices may provide a unique opportunity to identify people at higher risk of dementia or MCI.
Acknowledgments
This research has been conducted using the UK Biobank Resource (33883). This work is supported by the National Institutes of Health (NIH) grant RF1AG059867 to KH; KH is also partially supported by RF1AG064312; SH is partially supported by 5T32HL007901-25; PL is supported by the BrightFocus Foundation (A2020886S); LG is supported by the Alzheimer’s Association Clinician Scientist Fellowship (AACSF-23-1148490); CG is supported by the Alzheimer’s Association (AARFD-22-928372) and the American Academy of Sleep Medicine Foundation (290-FP-22). MKR was in part supported by the National Institute for Health and Care Research Manchester Biomedical Research Centre. AI is partially supported by the Multi-Partner Consortium to Expand Dementia Research in Latin America (ReDLat, supported by Fogarty International Center and the NIH National Institutes of Aging [R01 AG057234, R01 AG075775, R01 AG21051, R01 AG083799, CARDS-NIH], Alzheimer’s Association [SG-20-725707], Rainwater Charitable foundation—Tau Consortium, the Bluefield Project to Cure Frontotemporal Dementia, and Global Brain Health Institute), grants from ANID/FONDECYT Regular (1210195, 1210176, and 1220995); ANID/FONDAP/15150012; and ANID/PIA/ANILLOS ACT210096. The contents of this publication are solely the responsibility of the authors and do not represent the official views of these institutions. The funders had no role in the study design, data collection and analysis, and decision to publish or preparation of this paper. LG and KH are co-senior authors of the manuscript.
Abbreviations
- HR
hazard ratio
- ICD-10
International Classification of Disease, 10th Revision
- IS
interdaily stability
- IV
intradaily variability
- L5
activity level of the least active 5-hour period
- M10
activity level of the most active 10-hour period
- MCI
mild cognitive impairment
- NHS
National Health Service
- PRS
polygenic risk score
- Q
quartile
- RA
relative amplitude
- RAR
rest-activity rhythm
- UKB
UK Biobank
Activity count calculation.
Nonparametric analysis of circadian rest-activity rhythms.
Effects of rest-activity rhythm (RAR) measures on the risk for developing dementia (excluding those with only mild cognitive impairment; MCI). Among those with no dementia or MCI at baseline (N=91,517), 489 participants developed dementia during the follow-up.
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in non–shift workers.
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in participants with lower polygenic risk score (PRS) for Alzheimer disease (<median PRS) and participants with higher PRS (>median PRS).
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in the younger group (<70 years) and older group (≥70 years).
Footnotes
Conflicts of Interest: SH reports receiving consulting fees from Achaemenid LLC, unrelated to this project. The other authors declare no competing interests.
References
- 1.Dementia. World Health Organization. 2023. [2023-05-23]. https://www.who.int/news-room/fact-sheets/detail/dementia .
- 2.Smagula SF, Gujral S, Capps CS, Krafty RT. A systematic review of evidence for a role of rest-activity rhythms in dementia. Front Psychiatry. 2019;10:778. doi: 10.3389/fpsyt.2019.00778. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.00778/full . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leng Y, Musiek ES, Hu K, Cappuccio FP, Yaffe K. Association between circadian rhythms and neurodegenerative diseases. Lancet Neurol. 2019;18(3):307–318. doi: 10.1016/S1474-4422(18)30461-7. https://europepmc.org/abstract/MED/30784558 .S1474-4422(18)30461-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta NJ. Lifestyle and circadian health: where the challenges lie? Nutr Metab Insights. 2019;12:1178638819869024. doi: 10.1177/1178638819869024. https://journals.sagepub.com/doi/10.1177/1178638819869024 .10.1177_1178638819869024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hastings MH, Maywood ES, Brancaccio M. The mammalian circadian timing system and the suprachiasmatic nucleus as its pacemaker. Biology (Basel) 2019;8(1):13. doi: 10.3390/biology8010013. https://www.mdpi.com/2079-7737/8/1/13 .biology8010013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng H, Yang L, Ai S, Liu Y, Zhang W, Lei B, Chen J, Liu Y, Chan JWY, Chan NY, Tan X, Wang N, Benedict C, Jia F, Wing YK, Zhang J. Association between accelerometer-measured amplitude of rest-activity rhythm and future health risk: a prospective cohort study of the UK Biobank. Lancet Healthy Longev. 2023;4(5):e200–e210. doi: 10.1016/S2666-7568(23)00056-9. https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(23)00056-9/fulltext .S2666-7568(23)00056-9 [DOI] [PubMed] [Google Scholar]
- 7.Xu Y, Su S, Li X, Mansuri A, McCall WV, Wang X. Blunted rest-activity circadian rhythm increases the risk of all-cause, cardiovascular disease and cancer mortality in US adults. Sci Rep. 2022;12(1):20665. doi: 10.1038/s41598-022-24894-z. https://www.nature.com/articles/s41598-022-24894-z .10.1038/s41598-022-24894-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gu W, Tian Z, Tian W, Song Y, Qi G, Qi J, Sun C. Association of rest-activity circadian rhythm with chronic respiratory diseases, a cross-section survey from NHANES 2011-2014. Respir Med. 2023;209:107147. doi: 10.1016/j.rmed.2023.107147.S0954-6111(23)00035-5 [DOI] [PubMed] [Google Scholar]
- 9.Yang HJ, Cheng WJ, Hsiao MC, Huang SC, Kubo T, Hang LW, Lee WS. Rest-activity rhythm associated with depressive symptom severity and attention among patients with major depressive disorder: a 12-month follow-up study. Front Psychiatry. 2023;14:1214143. doi: 10.3389/fpsyt.2023.1214143. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1214143/full . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gehrman P, Marler M, Martin JL, Shochat T, Corey-Bloom J, Ancoli-Israel S. The relationship between dementia severity and rest/activity circadian rhythms. Neuropsychiatr Dis Treat. 2005;1(2):155–163. doi: 10.2147/nedt.1.2.155.61043. https://europepmc.org/abstract/MED/18568061 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leng Y, Blackwell T, Cawthon PM, Ancoli-Israel S, Stone KL, Yaffe K. Association of circadian abnormalities in older adults with an increased risk of developing Parkinson disease. JAMA Neurol. 2020;77(10):1270–1278. doi: 10.1001/jamaneurol.2020.1623. https://jamanetwork.com/journals/jamaneurology/fullarticle/2767087 .2767087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li P, Gao L, Gaba A, Yu L, Cui L, Fan W, Lim ASP, Bennett DA, Buchman AS, Hu K. Circadian disturbances in Alzheimer's disease progression: a prospective observational cohort study of community-based older adults. Lancet Healthy Longev. 2020;1(3):e96–e105. doi: 10.1016/s2666-7568(20)30015-5. https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(20)30015-5/fulltext . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lysen TS, Luik AI, Ikram MK, Tiemeier H, Ikram MA. Actigraphy-estimated sleep and 24-hour activity rhythms and the risk of dementia. Alzheimers Dement. 2020;16(9):1259–1267. doi: 10.1002/alz.12122. https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.12122 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Posner AB, Tranah GJ, Blackwell T, Yaffe K, Ancoli-Israel S, Redline S, Leng Y, Zeitzer JM, Chen DM, Webber KR, Stone KL. Predicting incident dementia and mild cognitive impairment in older women with nonparametric analysis of circadian activity rhythms in the study of osteoporotic fractures. Sleep. 2021;44(10):zsab119. doi: 10.1093/sleep/zsab119. https://academic.oup.com/sleep/article/44/10/zsab119/6272553?login=false .6272553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tranah GJ, Blackwell T, Stone KL, Ancoli-Israel S, Paudel ML, Ensrud KE, Cauley JA, Redline S, Hillier TA, Cummings SR, Yaffe K. Circadian activity rhythms and risk of incident dementia and mild cognitive impairment in older women. Ann Neurol. 2011;70(5):722–732. doi: 10.1002/ana.22468. https://europepmc.org/abstract/MED/22162057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiao Q, Sampson JN, LaCroix AZ, Shadyab AH, Zeitzer JM, Ancoli-Israel S, Yaffe K, Stone K. Nonparametric parameters of 24-hour rest-activity rhythms and long-term cognitive decline and incident cognitive impairment in older men. J Gerontol A Biol Sci Med Sci. 2022;77(2):250–258. doi: 10.1093/gerona/glab275. https://academic.oup.com/biomedgerontology/article/77/2/250/6374909?login=false .6374909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao Q, Shadyab AH, Rapp SR, Stone KL, Yaffe K, Sampson JN, Chen JC, Hayden KM, Henderson VW, LaCroix AZ. Rest-activity rhythms and cognitive impairment and dementia in older women: results from the Women's Health Initiative. J Am Geriatr Soc. 2022;70(10):2925–2937. doi: 10.1111/jgs.17926. https://europepmc.org/abstract/MED/35708069 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harper DG, Stopa EG, McKee AC, Satlin A, Harlan PC, Goldstein R, Volicer L. Differential circadian rhythm disturbances in men with Alzheimer disease and frontotemporal degeneration. Arch Gen Psychiatry. 2001;58(4):353–360. doi: 10.1001/archpsyc.58.4.353. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/481749 .yoa20065 [DOI] [PubMed] [Google Scholar]
- 19.Hatfield CF, Herbert J, van Someren EJW, Hodges JR, Hastings MH. Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer's dementia. Brain. 2004;127(Pt 5):1061–1074. doi: 10.1093/brain/awh129. https://academic.oup.com/brain/article/127/5/1061/303080 .awh129 [DOI] [PubMed] [Google Scholar]
- 20.Hooghiemstra AM, Eggermont LHP, Scheltens P, van der Flier WM, Scherder EJA. The rest-activity rhythm and physical activity in early-onset dementia. Alzheimer Dis Assoc Disord. 2015;29(1):45–49. doi: 10.1097/WAD.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 21.Luik AI, Zuurbier LA, Hofman A, Van Someren EJW, Ikram MA, Tiemeier H. Associations of the 24-h activity rhythm and sleep with cognition: a population-based study of middle-aged and elderly persons. Sleep Med. 2015;16(7):850–855. doi: 10.1016/j.sleep.2015.03.012. https://www.sciencedirect.com/science/article/pii/S1389945715007030?via%3Dihub .S1389-9457(15)00703-0 [DOI] [PubMed] [Google Scholar]
- 22.Musiek ES, Bhimasani M, Zangrilli MA, Morris JC, Holtzman DM, Ju YES. Circadian rest-activity pattern changes in aging and preclinical Alzheimer disease. JAMA Neurol. 2018;75(5):582–590. doi: 10.1001/jamaneurol.2017.4719. https://jamanetwork.com/journals/jamaneurology/fullarticle/2670749 .2670749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oosterman JM, van Someren EJW, Vogels RLC, Van Harten B, Scherder EJA. Fragmentation of the rest-activity rhythm correlates with age-related cognitive deficits. J Sleep Res. 2009;18(1):129–135. doi: 10.1111/j.1365-2869.2008.00704.x. https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2869.2008.00704.x .JSR704 [DOI] [PubMed] [Google Scholar]
- 24.Saito Y, Kume Y, Kodama A, Sato K, Yasuba M. The association between circadian rest-activity patterns and the behavioral and psychological symptoms depending on the cognitive status in Japanese nursing-home residents. Chronobiol Int. 2018;35(12):1670–1679. doi: 10.1080/07420528.2018.1505752. [DOI] [PubMed] [Google Scholar]
- 25.Satlin A, Volicer L, Stopa EG, Harper D. Circadian locomotor activity and core-body temperature rhythms in Alzheimer's disease. Neurobiol Aging. 1995;16(5):765–771. doi: 10.1016/0197-4580(95)00059-n.019745809500059N [DOI] [PubMed] [Google Scholar]
- 26.van Someren EJ, Hagebeuk EE, Lijzenga C, Scheltens P, de Rooij SE, Jonker C, Pot AMJ, Mirmiran M, Swaab DF. Circadian rest-activity rhythm disturbances in Alzheimer's disease. Biol Psychiatry. 1996;40(4):259–270. doi: 10.1016/0006-3223(95)00370-3.0006-3223(95)00370-3 [DOI] [PubMed] [Google Scholar]
- 27.Witting W, Kwa IH, Eikelenboom P, Mirmiran M, Swaab DF. Alterations in the circadian rest-activity rhythm in aging and Alzheimer's disease. Biol Psychiatry. 1990;27(6):563–572. doi: 10.1016/0006-3223(90)90523-5.0006-3223(90)90523-5 [DOI] [PubMed] [Google Scholar]
- 28.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001779 .PMEDICINE-D-12-02351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doherty A, Jackson D, Hammerla N, Plötz T, Olivier P, Granat MH, White T, van Hees VT, Trenell MI, Owen CG, Preece SJ, Gillions R, Sheard S, Peakman T, Brage S, Wareham NJ. Large scale population assessment of physical activity using wrist worn accelerometers: the UK Biobank Study. PLoS One. 2017;12(2):e0169649. doi: 10.1371/journal.pone.0169649. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0169649 .PONE-D-16-26249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li P, Gao L, Yu L, Zheng X, Ulsa MC, Yang HW, Gaba A, Yaffe K, Bennett DA, Buchman AS, Hu K, Leng Y. Daytime napping and Alzheimer's dementia: a potential bidirectional relationship. Alzheimers Dement. 2023;19(1):158–168. doi: 10.1002/alz.12636. https://europepmc.org/abstract/MED/35297533 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao L, Li P, Gaba A, Musiek E, Ju YES, Hu K. Fractal motor activity regulation and sex differences in preclinical Alzheimer's disease pathology. Alzheimers Dement (Amst) 2021;13(1):e12211. doi: 10.1002/dad2.12211. https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/dad2.12211 .DAD212211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones SE, van Hees VT, Mazzotti DR, Marques-Vidal P, Sabia S, van der Spek A, Dashti HS, Engmann J, Kocevska D, Tyrrell J, Beaumont RN, Hillsdon M, Ruth KS, Tuke MA, Yaghootkar H, Sharp SA, Ji Y, Harrison JW, Freathy RM, Murray A, Luik AI, Amin N, Lane JM, Saxena R, Rutter MK, Tiemeier H, Kutalik Z, Kumari M, Frayling TM, Weedon MN, Gehrman PR, Wood AR. Genetic studies of accelerometer-based sleep measures yield new insights into human sleep behaviour. Nat Commun. 2019;10(1):1585. doi: 10.1038/s41467-019-09576-1. https://www.nature.com/articles/s41467-019-09576-1 .10.1038/s41467-019-09576-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Hees VT, Renström F, Wright A, Gradmark Anna, Catt Michael, Chen Kong Y, Löf Marie, Bluck Les, Pomeroy Jeremy, Wareham Nicholas J, Ekelund Ulf, Brage Søren, Franks Paul W. Estimation of daily energy expenditure in pregnant and non-pregnant women using a wrist-worn tri-axial accelerometer. PLoS One. 2011;6(7):e22922–e22984. doi: 10.1371/journal.pone.0022922. https://dx.plos.org/10.1371/journal.pone.0022922 .PONE-D-11-03109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Someren EJW, Swaab DF, Colenda CC, Cohen W, McCall WV, Rosenquist PB. Bright light therapy: improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiol Int. 1999;16(4):505–518. doi: 10.3109/07420529908998724. [DOI] [PubMed] [Google Scholar]
- 35.Li P. pliphd/Actigraphy: ezActi2. Zenodo. [2024-04-10]. https://zenodo.org/record/8411607 .
- 36.Gao C, Haghayegh S, Wagner M, Cai R, Hu K, Gao L, Li P. Approaches for assessing circadian rest-activity patterns using actigraphy in cohort and population-based studies. Curr Sleep Medicine Rep. 2023;9(4):247–256. doi: 10.1007/s40675-023-00267-4. https://link.springer.com/article/10.1007/s40675-023-00267-4 . [DOI] [Google Scholar]
- 37.Gao L, Li P, Gaykova N, Zheng X, Gao C, Lane JM, Saxena R, Scheer FAJL, Rutter MK, Akeju O, Hu K. Circadian rest-activity rhythms, delirium risk, and progression to dementia. Ann Neurol. 2023;93(6):1145–1157. doi: 10.1002/ana.26617. https://onlinelibrary.wiley.com/doi/10.1002/ana.26617 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao L, Gaba A, Li P, Saxena R, Scheer FAJL, Akeju O, Rutter MK, Hu K. Heart rate response and recovery during exercise predict future delirium risk-a prospective cohort study in middle- to older-aged adults. J Sport Health Sci. 2023;12(3):312–323. doi: 10.1016/j.jshs.2021.12.002. https://www.sciencedirect.com/science/article/pii/S209525462100140X?via%3Dihub .S2095-2546(21)00140-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gao L, Gaba A, Cui L, Yang HW, Saxena R, Scheer FAJL, Akeju O, Rutter MK, Lo MT, Hu K, Li P. Resting heartbeat complexity predicts all-cause and cardiorespiratory mortality in middle- to older-aged adults from the UK Biobank. J Am Heart Assoc. 2021;10(3):e018483. doi: 10.1161/JAHA.120.018483. https://www.ahajournals.org/doi/10.1161/JAHA.120.018483 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ulsa MC, Xi Z, Li P, Gaba A, Wong PM, Saxena R, Scheer FAJL, Rutter M, Akeju O, Hu K, Gao L. Association of poor sleep burden in middle age and older adults with risk for delirium during hospitalization. J Gerontol A Biol Sci Med Sci. 2022;77(3):507–516. doi: 10.1093/gerona/glab272. https://academic.oup.com/biomedgerontology/article/77/3/507/6374863?login=false .6374863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ge T, Chen CY, Ni Y, Feng YCA, Smoller JW. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat Commun. 2019;10(1):1776. doi: 10.1038/s41467-019-09718-5. https://www.nature.com/articles/s41467-019-09718-5 .10.1038/s41467-019-09718-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wightman DP, Jansen IE, Savage JE, Shadrin AA, Bahrami S, Holland D, Rongve A, Børte S, Winsvold BS, Drange OK, Martinsen AE, Skogholt AH, Willer C, Bråthen G, Bosnes I, Nielsen JB, Fritsche LG, Thomas LF, Pedersen LM, Gabrielsen ME, Johnsen MB, Meisingset TW, Zhou W, Proitsi P, Hodges A, Dobson R, Velayudhan L, Heilbron K, Auton A, Sealock JM, Davis LK, Pedersen NL, Reynolds CA, Karlsson IK, Magnusson S, Stefansson H, Thordardottir S, Jonsson PV, Snaedal J, Zettergren A, Skoog I, Kern S, Waern M, Zetterberg H, Blennow K, Stordal E, Hveem K, Zwart JA, Athanasiu L, Selnes P, Saltvedt I, Sando SB, Ulstein I, Djurovic S, Fladby T, Aarsland D, Selbæk G, Ripke S, Stefansson K, Andreassen OA, Posthuma D. A genome-wide association study with 1,126,563 individuals identifies new risk loci for Alzheimer's disease. Nat Genet. 2021;53(9):1276–1282. doi: 10.1038/s41588-021-00921-z. https://europepmc.org/abstract/MED/34493870 .10.1038/s41588-021-00921-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7. doi: 10.1186/s13742-015-0047-8. https://academic.oup.com/gigascience/article/4/1/s13742-015-0047-8/2707533?login=false .47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Purcell S, Chang C. Cog Genomics. [2024-04-10]. https://www.cog-genomics.org/plink/2.0/
- 45.Bokenberger K, Sjölander A, Aslan AKD, Karlsson IK, Åkerstedt T, Pedersen NL. Shift work and risk of incident dementia: a study of two population-based cohorts. Eur J Epidemiol. 2018;33(10):977–987. doi: 10.1007/s10654-018-0430-8. https://link.springer.com/article/10.1007/s10654-018-0430-8 .10.1007/s10654-018-0430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jørgensen JT, Hansen J, Westendorp RGJ, Nabe-Nielsen K, Stayner LT, Simonsen MK, Andersen ZJ. Shift work and incidence of dementia: a Danish nurse cohort study. Alzheimers Dement. 2020;16(9):1268–1279. doi: 10.1002/alz.12126. [DOI] [PubMed] [Google Scholar]
- 47.Lee KW, Yang CC, Chen CH, Hung CH, Chuang HY. Shift work is significantly and positively associated with dementia: a meta-analysis study. Front Public Health. 2023;11:998464. doi: 10.3389/fpubh.2023.998464. https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.998464/full . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. Chronotype and social jetlag: a (self-) critical review. Biology (Basel) 2019;8(3):54. doi: 10.3390/biology8030054. https://www.mdpi.com/2079-7737/8/3/54 .biology8030054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walker WH, Walton JC, DeVries AC, Nelson RJ. Circadian rhythm disruption and mental health. Transl Psychiatry. 2020;10(1):28. doi: 10.1038/s41398-020-0694-0. https://www.nature.com/articles/s41398-020-0694-0 .10.1038/s41398-020-0694-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Park JE, Lee YJ, Byun MS, Yi D, Lee JH, Jeon SY, Hwang JY, Yoon H, Choe YM, Kim YK, Shin SA, Suk HW, Lee DY. Differential associations of age and Alzheimer's disease with sleep and rest-activity rhythms across the adult lifespan. Neurobiol Aging. 2021;101:141–149. doi: 10.1016/j.neurobiolaging.2021.01.006.S0197-4580(21)00013-0 [DOI] [PubMed] [Google Scholar]
- 51.Hu K, Li P, Gao L. Sleep, rest-activity rhythms and aging: a complex web in Alzheimer's disease? Neurobiol Aging. 2021;104:102–103. doi: 10.1016/j.neurobiolaging.2021.02.017. https://europepmc.org/abstract/MED/33902941 .S0197-4580(21)00072-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Forger DB, Jewett ME, Kronauer RE. A simpler model of the human circadian pacemaker. J Biol Rhythms. 1999;14(6):533–538. doi: 10.1177/074873099129000867. [DOI] [PubMed] [Google Scholar]
- 53.Stone JE, Aubert XL, Maass H, Phillips AJK, Magee M, Howard ME, Lockley SW, Rajaratnam SMW, Sletten TL. Application of a limit-cycle oscillator model for prediction of circadian phase in rotating night shift workers. Sci Rep. 2019;9(1):11032. doi: 10.1038/s41598-019-47290-6. https://www.nature.com/articles/s41598-019-47290-6 .10.1038/s41598-019-47290-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang Y, Mayer C, Cheng P, Siddula A, Burgess HJ, Drake C, Goldstein C, Walch O, Forger DB. Predicting circadian phase across populations: a comparison of mathematical models and wearable devices. Sleep. 2021;44(10):zsab126. doi: 10.1093/sleep/zsab126. https://academic.oup.com/sleep/article/44/10/zsab126/6278480?login=false .6278480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Song YM, Choi SJ, Park SH, Lee SJ, Joo EY, Kim JK. A real-time, personalized sleep intervention using mathematical modeling and wearable devices. Sleep. 2023;46(9):zsad179. doi: 10.1093/sleep/zsad179.7221723 [DOI] [PubMed] [Google Scholar]
- 56.Hong J, Choi SJ, Park SH, Hong H, Booth V, Joo EY, Kim JK. Personalized sleep-wake patterns aligned with circadian rhythm relieve daytime sleepiness. iScience. 2021;24(10):103129. doi: 10.1016/j.isci.2021.103129. https://www.cell.com/iscience/fulltext/S2589-0042(21)01097-X?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS258900422101097X%3Fshowall%3Dtrue .S2589-0042(21)01097-X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Activity count calculation.
Nonparametric analysis of circadian rest-activity rhythms.
Effects of rest-activity rhythm (RAR) measures on the risk for developing dementia (excluding those with only mild cognitive impairment; MCI). Among those with no dementia or MCI at baseline (N=91,517), 489 participants developed dementia during the follow-up.
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in non–shift workers.
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in participants with lower polygenic risk score (PRS) for Alzheimer disease (<median PRS) and participants with higher PRS (>median PRS).
Effects of rest-activity rhythm (RAR) measures on risk of developing dementia or mild cognitive impairment (MCI) in the younger group (<70 years) and older group (≥70 years).


