Abstract
The study aimed to investigate the basic data to derive plans for snack provision to improve the nutritional status of older adults living in long-term care facilities (LFs) or long-term care hospitals (LHs). The 252 respondents (118 from LHs and 134 from LFs) were included in the study. The questionnaire of nationwide cross-sectional survey was developed by the authors and registered dietitians. The written questionnaire was sent to the food service managers across 800 LFs or LHs. The online survey was introduced using the online platform and network site for dietitians. More than 70% of live-in and non-live-in LFs provided snacks, which were mainly provided one to two times a day. Most institutions provided fruits one to three times a week. The main considerations when providing fruit were in the order of residents’ preference, cost, and ease of consumption. The reasons for not serving fruit included cost and differences in the residents’ eating and mastication abilities. Most institutions also provided dairy products at a frequency of one to three times a week. The reasons for not serving dairy products included cost and the lack of awareness of the need to provide them. To improve the quality of life and the offer benefits of fruits and dairy products to older people, efforts are needed to propose a plan to expand the provision of snacks in appropriate quantities and varieties.
Keywords: Long-term care, Nursing homes, Food service, Meals, Fruits
INTRODUCTION
A super-aged society, where more than 20% of their total population is aged 65 years and older, represents an emerging global challenge [1]. Currently, Korea has the fastest aging population in the world because of improvements in the national income and living standards and the development of medical technology and is expected to become a super-aged society by 2025 [2]. By 2050, it is predicted that 40.1% of its population will be ≥ 65 years, up from 18.4% in 2023 [3]. Providing special care services to individuals who are unable to live independently is essential to prepare for a healthy aging society and is a major strategy for establishing a healthy society with older people [4].
The rapid increase in the number of the elderly population also increases the demand for and utilization of long-term care facilities (LFs) [5,6,7,8]. The number of long-term care hospitals (LHs) increased from 868 in 2010 to 1,582 in 2020 [9], and that of LFs also increased from 69,214 in 2010 to 82,294 in 2020 [10]. In addition, the utilization rate of LFs increased by approximately 2% compared with that in 2016, accounting for 84.3% in 2017 [11]. In particular, it is reported that the rate of long-term care bed use in Korea is increasing the fastest among the Organization for Economic Co-operation and Development member countries [12]. The number of the users of long-term care beds increased by 25.6 per 1,000 people aged ≥ 65 years over the past 11 years [12].
A well-balanced nutrition for older people is important for improving their quality of life, managing chronic diseases, and preventing and delaying frailty [13]. Older adults often have difficulty eating due to functional loss, such as changes in taste and smell, deterioration of digestive and salivary gland function, and tooth damage [14]. Meals provided in LFs and LHs are closely related to the nutritional status and health of residents and can further affect their lives because the older adults living in LFs and LHs have a long residence period. Therefore, management and support for high-quality, balanced meal in LFs and LHs are essential in an aging society [15].
The prevalence of chewing and swallowing problems is higher in individuals in residential care facilities than in community-dwelling older people [16]. Older nursing home residents are frequently malnourished with the estimates of those affected ranging from 19% to > 50% [17]. Most of the nutrient intakes among older adults living in facilities did not meet the nutritional intake standards, particularly with regard to dairy products and protein, as well as micronutrient [18,19]. Considering the expense of fruits, milk, and other dairy products rich in vitamins and minerals [20], it may be expected that it is difficult to provide various kinds of snacks in an appropriate amount. Although there have been reports on oral health that can affect food intake and nutritional status of the older people living in facilities, there has been no survey on the meals provided by the facilities.
Nutritional supplementation for older people through snacks is important; however, because of physiological and functional aging, it is difficult for the elderly people to take in enough nutrients with three meals a day. The researchers conducted the survey to understand the provision of meals, especially snacks, in LFs and LHs, as basic data to improve the nutritional status and quality of life of the elderly people in care facilities.
MATERIALS AND METHODS
Study design
This nationwide cross-sectional survey study was conducted to investigate snack provision in LHs and LFs in South Korea. The survey was conducted through postal mail and online from July to December 2020. The written questionnaire was sent to the food service managers across 800 LFs or LFs (approximately 11.6% of the total of 6,885 LFs for the elderly people in Korea) throughout the country (Seoul, Gyeonggi, Incheon, Jeolla, Gyeongsang, Gangwon, and Jeju). The responses to the survey were recommended to be made by those responsible for food service. The online survey was introduced using the online platform and network site for dietitians (https://www.kdclub.com/, http://cafe.naver.com/lovenutri etc.). A total of 295 respondents participated in the survey. The 252 respondents (118 from LHs and 134 from LFs) were included in the study, excluding the data of 43 people who gave inadequate responses.
Questionnaire
The questionnaire was developed by the authors and reviewed by three registered dietitians. The final questionnaire consisted of four parts (39 items) with mostly predefined answer categories.
1. Characteristics of the food service managers, including age, sex, education, certificate, responsibilities (task), work experience, and credentials (registered dietitian, clinical dietitian, culinary staff or cook, caregiver, nurse, or social worker). The food service managers were asked to answer on their tasks (i.e., menu planning and management, ingredient selection and ordering, food preparation and distribution, and nutrition education and counseling).
2. The food service operation status, including the following six items: location of LH or LF, type of operation (self-operated or contract-managed), food service subsidies, number of food service staff, number of permitted beds, and number of patients or residents.
3. The status of the food service provision, including the number of meals served per day, type of diet (general, soft minced, moist, smooth pureed, or liquid), meal price, serving size provided by food groups, availability of texture-modified food, recognizing the need to provide texture-modified food, educational experience on texture-modified food, and necessity awareness for education on texture-modified food.
4. Snack provision-related information, including the presence of fruits, frequency and number of fruit servings, type of fruits served (e.g., fresh fruits, canned fruits, frozen fruits, commercial fruit juice with or without sugar, homemade fruit juice, and fruit puree), factors associated with fruit providing, fruits with high or low serving frequency and the reason, fruits preferred by residents and the reason (e.g., swallowing and/or chewing problem; cumbersome preparation process, such as washing and slicing fruits; and expensive price), and difficulties in providing fruits, whether dairy product and nutritional supplement drinks were provided and number, type, method of provision (at meal or between meals) and reasons for not serving dairy products.
Statistical analysis
Statistical analyses were performed using Statistical Package for the Social Sciences (version 26.0; IBM, Seoul, Korea). Statistical significance was set at 0.05 based on a two-sided test. The data file was controlled for outliers, inconsistencies, and normality. The demographic characteristics of participants are presented as means and standard deviations for continuous variables and frequencies and percentages (%) for categorical variables. The data were analyzed separately for LH and LF. Before conducting comparative analysis between groups, we identified that data were normally distributed. Group comparisons were performed using the chi-square tests for qualitative variables and one-way analysis of variance for quantitative variables. Residential facilities and non-residential facilities may have differences in the frequency of providing meals and snacks, so this study analyzed them separately.
Ethics statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Ethics Committees of the Institutional Review Boards of Kyung Hee University in July 2020 (No. KHGIRB-20-262).
RESULTS
General characteristics of the respondents
The general characteristics of the respondents are presented in Supplementary Table 1. There were a total of 252 respondents, of whom 46.8% (n = 118), 40.9% (n = 103), and 12.3% (n = 31) worked at LHs, live-in LFs, and non-live-in LFs, respectively.
The questionnaires were distributed across the country; 46.0% of the collected surveys were from the metropolitan area, and 51.6% were from the rest of the area. The respondents included a high proportion of females (94.8%), most were aged between 20 and 39 years (61.5%), and those working in LHs were significantly younger than those in live-in and non-live-in LFs (p = 0.011). More than half of the respondents had a university degree (LHs, 53.4%; live-in LFs, 61.2%; and non-live-in LFs, 71.0%), and most of them had > 10 years of work experience (26.2%).
More than 80% of the respondents from LHs and live-in LFs were dietitians (92.4% in LHs and 83.5% in live-in LFs), and approximately 50% of respondents at non-live-in LFs were social workers or caregivers, culinary staff, and nurses (19.4% were social workers or caregivers and culinary staff, and 9.7% were nurses). The respondents from LHs and live-in LFs were mainly responsible for diet management and ingredient selection and ordering (LHs, 25.2%, diet management, and 24.5%, ingredient selection and ordering; live-in LFs, 27.4%, diet management, and 25.9%, ingredient selection and ordering), and those from non-live-in LFs were mainly responsible for diet management and meal serving (20.2%, diet management and ingredient selection and ordering).
General characteristics of the institutions
Table 1 shows the general characteristics of the institutions surveyed. The surveyed institutions were mainly self-operated (84.5%); most had < 10 food service employees (67.4%) and 100–199 (40.7%) licensed beds.
Table 1. General characteristics of the institutions surveyed.
| Variables | Total (n = 252) | Long-term care hospital (n = 118) | Live-in long-term care facility (n = 103) | Non-live-in long-term care facility (n = 31) | p value* | |
|---|---|---|---|---|---|---|
| Type of food service operation | 0.000† | |||||
| Self-operated management | 213 (84.5) | 111 (94.1) | 80 (77.7) | 22 (71.0) | ||
| Consigned management | 35 (13.9) | 6 (5.1) | 23 (22.3) | 6 (19.4) | ||
| Others | 3 (1.2) | 1 (0.8) | 0 (0.0) | 2 (6.5) | ||
| No answer | 1 (0.4) | 0 (0.0) | 0 (0.0) | 1 (3.2) | ||
| Number of food service manpower | 0.000† | |||||
| < 5 | 85 (33.7) | 20 (16.9) | 46 (44.7) | 19 (61.3) | ||
| 5–9 | 85 (33.7) | 45 (38.1) | 32 (31.1) | 8 (25.8) | ||
| 10–14 | 59 (23.4) | 42 (35.6) | 15 (14.6) | 2 (6.5) | ||
| 15–19 | 10 (4.0) | 7 (5.9) | 2 (1.9) | 1 (3.2) | ||
| ≥ 20 | 7 (2.8) | 4 (3.4) | 3 (2.9) | 0 (0.0) | ||
| No answer | 6 (2.4) | 0 (0.0) | 5 (4.9) | 1 (3.2) | ||
| Number of beds | 0.000† | |||||
| < 50 | 19 (8.6) | 5 (4.2) | 14 (13.6) | - | ||
| 50–99 | 37 (16.7) | 5 (4.2) | 32 (31.1) | - | ||
| 100–149 | 44 (19.9) | 27 (22.9) | 17 (16.5) | - | ||
| 150–199 | 46 (20.8) | 35 (29.7) | 11 (10.7) | - | ||
| 200–249 | 27 (12.2) | 17 (14.4) | 10 (9.7) | - | ||
| 250–299 | 7 (3.2) | 6 (5.1) | 1 (1.0) | - | ||
| ≥ 300 | 18 (8.1) | 16 (13.6) | 2 (1.9) | - | ||
| No answer | 23 (10.4) | 7 (5.9) | 16 (15.5) | - | ||
| Meal served* | 0.000† | |||||
| Breakfast | 220 (31.4) | 117 (33.2) | 95 (32.9) | 8 (13.6) | ||
| Lunch | 250 (35.7) | 118 (33.5) | 101 (34.9) | 31 (52.5) | ||
| Dinner | 230 (32.9) | 117 (33.2) | 93 (32.2) | 20 (33.9) | ||
| Type of diet‡ | 0.000† | |||||
| General diet | 214 (15.4) | 104 (13.8) | 90 (16.0) | 20 (27.8) | ||
| Soft diet | 195 (14.0) | 99 (13.1) | 83 (14.7) | 13 (18.1) | ||
| Soft diet-minced | 177 (12.7) | 101 (13.4) | 69 (12.2) | 7 (9.7) | ||
| Liquid diet | 173 (12.5) | 97 (12.9) | 70 (12.4) | 6 (8.3) | ||
| Diabetic diet | 172 (12.4) | 96 (12.7) | 68 (12.1) | 8 (11.1) | ||
| Blended diet | 166 (12.0) | 91 (12.1) | 70 (12.4) | 5 (6.9) | ||
| Tube feeding | 162 (11.7) | 95 (12.6) | 62 (11.0) | 5 (6.9) | ||
| Low-salt diet | 121 (8.7) | 63 (8.4) | 50 (8.9) | 8 (11.1) | ||
| Others | 9 (0.6) | 7 (0.7) | 2 (0.4) | 0 (0.0) | ||
| Cost per meal§ | 0.000† | |||||
| < 1,000 won | 8 (3.2) | 6 (5.1) | 2 (1.9) | 0 (0.0) | ||
| 1,000–1,999 won | 116 (46.0) | 80 (67.8) | 32 (31.1) | 4 (12.9) | ||
| 2,000–2,999 won | 68 (27.0) | 18 (15.3) | 39 (37.9) | 11 (35.5) | ||
| 3,000–3,999 won | 32 (12.7) | 10 (8.5) | 14 (13.6) | 8 (25.8) | ||
| ≥ 4,000 won | 14 (5.6) | 3 (2.5) | 5 (4.9) | 6 (19.4) | ||
| No answer | 14 (5.6) | 1 (0.8) | 11 (10.7) | 2 (6.5) | ||
Values are presented as number (%).
*The p values were analyzed using the χ2 test; †p < 0.001; ‡Multiple response analysis; §The cost per meal is the unit price of pure ingredients, excluding, for example, the labor and maintenance costs. 1,300 KRW (South Korean Won) = 0.77 USD (United States dollar) (Jun 22, 2023 18:22 UTC).
The majority of institutions provided breakfast, lunch, and dinner (31.4%, 35.7%, and 32.9%, respectively), and non-live-in LFs showed lower rates of providing breakfast than did other institutions (13.6% in non-live-in LFs vs. 33.2% in LHs and 32.9% in live-in LFs; p = 0.000). General (15.4%) and soft (14.0%) diets were mainly provided, and therapeutic diets were provided at a similar level (soft diet-minced, 12.7%; liquid diet, 12.5%; diabetic diet, 12.4%; blended diet, 12.0%; tube feeding, 11.7%; and low-salt diet, 8.7%). In general, the cost per meal was 1,000–2,999 won (46.0% at 1,000–1,999 won and 27.0% at 2,000–2,999 won).
Overall snack provision
The snack provision status is presented in Table 2. More than 70% of live-in and non-live-in LFs provided snacks (live-in LFs, 81.3%, and non-live-in LFs, 74.2%), whereas < 50% of LHs provided snacks. Snacks were mainly provided one to two times a day (49.0% at one time/day and 35.7% at two times/day) outside of mealtimes (62.4%) and generally cost 500–1,499 won (29.9% at 500–999 won and 23.6% at 1,000–1,499 won).
Table 2. Snack provision status.
| Variables | Total (n = 252) | Long-term care hospital (n = 118) | Live-in long-term care facility (n = 103) | Non-live-in long-term care facility (n = 31) | p value* | |
|---|---|---|---|---|---|---|
| Providing snacks | 0.000† | |||||
| Yes | 157 (62.3) | 50 (42.4) | 84 (81.3) | 23 (74.2) | ||
| No | 95 (37.7) | 68 (57.6) | 19 (18.4) | 8 (25.8) | ||
| Frequency of providing snacks if answered “Yes” (n = 157) | 0.088 | |||||
| 1 time/day | 77 (49.0) | 25 (50.0) | 39 (46.4) | 13 (56.5) | ||
| 2 times/day | 56 (35.7) | 12 (24.0) | 37 (44.0) | 7 (30.4) | ||
| > 3 times/day | 9 (5.7) | 3 (6.0) | 5 (6.0) | 1 (4.3) | ||
| Whenever residents want | 9 (5.7) | 6 (12.0) | 1 (1.2) | 2 (8.7) | ||
| No answer | 6 (3.8) | 4 (8.0) | 2 (2.4) | 0 (0.0) | ||
| Way of providing snacks if answered “Yes” (n = 157) | 0.000† | |||||
| Provided with each meal | 36 (22.9) | 27 (54.0) | 7 (8.3) | 2 (8.7) | ||
| Provided between meals | 98 (62.4) | 9 (18.0) | 71 (84.5) | 18 (78.3) | ||
| Others | 19 (12.1) | 11 (22.0) | 5 (6.0) | 3 (13.0) | ||
| No answer | 4 (2.5) | 3 (6.0) | 1 (1.2) | 0 (0.0) | ||
| Cost of snacks if answered “Yes” (n = 157)‡ | 0.000† | |||||
| < 500 won | 30 (19.1) | 20 (40.0) | 7 (8.3) | 3 (13.0) | ||
| 500–999 won | 47 (29.9) | 11 (22.0) | 33 (39.3) | 3 (13.0) | ||
| 1,000–1,499 won | 37 (23.6) | 4 (8.0) | 25 (29.8) | 8 (34.8) | ||
| 1,500–1,999 won | 11 (7.0) | 3 (6.0) | 6 (7.1) | 2 (8.7) | ||
| ≥ 2,000 won | 10 (6.4) | 3 (6.0) | 4 (4.8) | 3 (13.0) | ||
| No answer | 22 (14.0) | 9 (18.0) | 9 (10.7) | 4 (17.4) | ||
Values are presented as number (%).
*The p values were analyzed using the χ2 test; †p < 0.001; ‡The cost per meal is the unit price of pure ingredients, excluding, for example, the labor and maintenance costs. 1,300 KRW (South Korean Won) = 0.77 USD (United States dollar) (Jun 22, 2023 18:22 UTC).
Snack: fruits
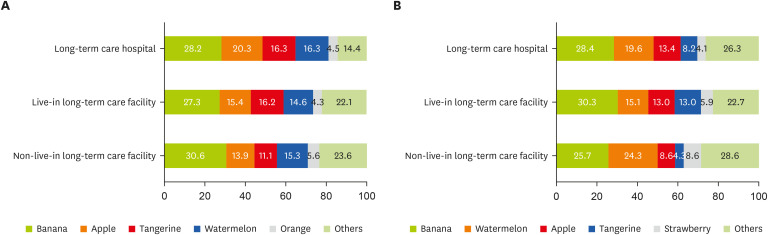
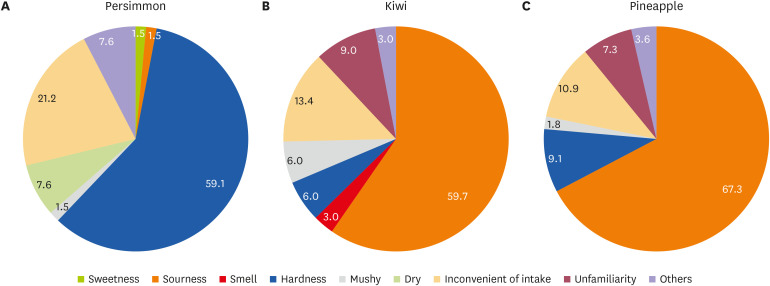
Table 3, Figures 1 and 2 shows the fruit provision status in elderly care facilities. Most institutions provided fruits (70.6%) one to three a week (19.1% at one time/week and 25.3% at two to three times/week). The main reason for the low preference for persimmons was hardness (59.1%), whereas kiwi and pineapple were less preferred because of sourness (kiwi, 59.7%, and pineapple, 67.3%). In order, the factors considered when providing fruits were the resident preference, cost, and ease of consumption (22.7%, 22.5%, and 21.2%, respectively). On the other hand, the main reasons for not providing fruits were “cost” and difficulty in providing various kinds of fruits considering their different levels of chewing abilities (27.3% and 24.5%, respectively).
Table 3. Fruit provision status.
| Variables | Total (n = 252) | Long-term care hospital (n = 118) | Live-in long-term care facility (n = 103) | Non-live-in long-term care facility (n = 31) | p value* | |
|---|---|---|---|---|---|---|
| Providing fruits | 0.000† | |||||
| Yes | 178 (70.6) | 69 (58.5) | 85 (82.5) | 24 (77.4) | ||
| No | 72 (28.6) | 48 (40.7) | 17 (16.5) | 7 (22.6) | ||
| No answer | 2 (0.8) | 1 (0.8) | 1 (1.0) | 0 (0.0) | ||
| Frequency of providing fruits if answered “Yes” (n = 178) | 0.017‡ | |||||
| > 3 times/day | 2 (1.1) | 0 (0.0) | 1 (1.2) | 1 (4.2) | ||
| 2 times/day | 15 (8.4) | 9 (13.0) | 6 (7.1) | 0 (0.0) | ||
| 1 time/day | 33 (18.5) | 14 (20.3) | 14 (16.5) | 5 (20.8) | ||
| 4–6 times/wk | 19 (10.7) | 7 (10.1) | 11 (12.9) | 1 (4.2) | ||
| 2–3 times/wk | 45 (25.3) | 11 (15.9) | 29 (34.1) | 5 (20.8) | ||
| 1 time/wk | 34 (19.1) | 9 (13.0) | 18 (21.2) | 7 (29.2) | ||
| 2–3 times/mon | 15 (8.4) | 7 (10.1) | 4 (4.7) | 4 (16.7) | ||
| Less than 1 time/mon | 10 (5.6) | 8 (11.6) | 1 (1.2) | 1 (4.2) | ||
| No answer | 5 (2.8) | 4 (5.8) | 1 (1.2) | 0 (0.0) | ||
| Factors to consider when providing fruits if answered “Yes” (n = 178)* | 0.066 | |||||
| Preference | 121 (22.7) | 41 (19.8) | 64 (25.1) | 16 (22.2) | ||
| Cost | 120 (22.5) | 60 (29.0) | 50 (19.6) | 10 (13.9) | ||
| Ease of consumption | 113 (21.2) | 36 (17.4) | 60 (23.5) | 17 (23.6) | ||
| Nutrition | 85 (15.9) | 26 (12.6) | 43 (16.9) | 16 (22.2) | ||
| Convenience of provision | 72 (13.5) | 33 (15.9) | 33 (12.9) | 6 (8.3) | ||
| Others | 8 (1.5) | 2 (1.0) | 5 (2.0) | 1 (1.4) | ||
| No answer | 15 (2.8) | 9 (4.3) | 0 (0.0) | 6 (8.3) | ||
| Barriers for providing fruits if answered “No” (n = 72)§ | 0.002∥ | |||||
| Cost | 59 (27.3) | 48 (33.3) | 6 (11.8) | 5 (23.8) | ||
| Difficulties in providing fruits considering their individual chewing abilities | 53 (24.5) | 27 (18.8) | 19 (37.3) | 7 (33.3) | ||
| Insufficient manpower | 38 (17.6) | 30 (20.8) | 6 (11.8) | 2 (9.5) | ||
| Self-consumption | 33 (15.3) | 23 (16.0) | 9 (17.6) | 1 (4.8) | ||
| No demand | 10 (4.6) | 3 (2.1) | 4 (7.8) | 3 (14.3) | ||
| Others | 6 (2.8) | 6 (4.2) | 0 (0.0) | 0 (0.0) | ||
| No answer | 17 (7.9) | 7 (4.9) | 7 (13.7) | 3 (14.3) | ||
Values are presented as number (%).
*The p values were analyzed using the χ2 test; †p < 0.001; ‡p < 0.05, §Multiple response analysis; ∥p < 0.01.
Figure 1. Ranking of the most offered and favorite fruits (%).* (A) Fruits frequently served (%). Other fruits include the following: pears > strawberries > canned fruits > grapes, soft persimmons > tomatoes > peaches > pineapples > kiwis > oriental melons, mangoes > melons > blueberries > persimmons > plums > others. (B) Fruits with high preference (%). Other fruits include the following: peaches > soft persimmons > pears > grapes > oranges > tomatoes > canned fruits > persimmons, melons > mangoes, kiwis > oriental melons, pineapples > blueberries > plums, others.
*Multiple response analysis.
Figure 2. Fruits of low preference and reasons (%).* (A) Reasons for the low preference of persimmon. (B) Reasons for the low preference of kiwi. (C) Reasons for the low preference of pineapple. The fruits with the lowest preference were persimmon (1st), kiwi (2nd) and pineapple (3rd). Other fruits include the following: apples, grapes > oriental melons > plums > oranges > pears > blueberries > tangerines, tomatoes > mangoes > others > bananas, peaches, canned fruits > soft persimmons > strawberries, watermelons > grapefruits > passionfruit, cherries.
*Multiple response analysis.
Based on the 23 most consumed fruits by Koreans, we surveyed the fruits frequently provided and those with high preference among residents (Figures 1 and 2). Bananas, apples, tangerines, watermelons, and oranges were frequently provided, and bananas, watermelons, apples, tangerines, and strawberries were preferred by residents (Figure 1). Persimmons, kiwis, and pineapples were less preferred by residents (Figure 2).
Snack: dairy products
The dairy product provision status is presented in Table 4. The majority of the facilities provided dairy products (LHs, 64.4%; live-in LFs, 79.6%; and non-live-in LFs, 77.4%). Dairy products were mostly provided one to three times a week (35.2% for normal milk, 10.4% for low-fat milk, 39.0% for Yakult, 36.8% for drinking yogurt, and 45.6% for semisolid yogurt). The main reasons for not providing dairy products were cost and the lack of perception of the necessity (29.4% and 22.1%, respectively).
Table 4. Dairy provision status.
| Variables | Total (n = 252) | Long-term care hospital (n = 118) | Live-in long-term care facility (n = 103) | Non-live-in long-term care facility (n = 31) | p value* | ||
|---|---|---|---|---|---|---|---|
| Dairy product provision status | 0.017† | ||||||
| Yes | 182 (72.2) | 76 (64.4) | 82 (79.6) | 24 (77.4) | |||
| No | 68 (27.0) | 42 (35.6) | 19 (18.4) | 7 (22.6) | |||
| No answer | 2 (0.8) | 0 (0.0) | 2 (1.9) | 0 (0.0) | |||
| Types of dairy products if answered “Yes” (n = 182) | |||||||
| Normal milk | 0.001‡ | ||||||
| 1 time/day | 43 (23.6) | 29 (38.2) | 13 (15.9) | 1 (4.2) | |||
| 1–3 times/wk | 64 (35.2) | 17 (22.4) | 36 (43.9) | 11 (45.8) | |||
| 4–6 times/wk | 5 (2.7) | 1 (1.3) | 2 (2.4) | 2 (8.3) | |||
| No answer | 70 (38.5) | 29 (38.2) | 31 (37.8) | 10 (41.7) | |||
| Low-fat milk | 0.387 | ||||||
| 1 time/day | 12 (6.6) | 7 (9.2) | 4 (4.9) | 1 (4.2) | |||
| 1–3 times/wk | 19 (10.4) | 5 (6.6) | 11 (13.4) | 3 (12.5) | |||
| 4–6 times/wk | 4 (2.2) | 0 (0.0) | 3 (3.7) | 1 (4.2) | |||
| No answer | 147 (80.8) | 64 (84.2) | 64 (78.0) | 19 (79.2) | |||
| Yakult | 0.167 | ||||||
| 1 time/day | 20 (11.0) | 11 (14.5) | 7 (8.5) | 2 (8.3) | |||
| 1–3 times/wk | 71 (39.0) | 22 (28.9) | 40 (48.8) | 9 (37.5) | |||
| 4–6 times/wk | 8 (4.4) | 2 (2.6) | 4 (4.9) | 2 (8.3) | |||
| No answer | 83 (45.6) | 41 (53.9) | 31 (37.8) | 11 (45.8) | |||
| Drinking yogurt | 0.261 | ||||||
| 1 time/day | 10 (5.5) | 2 (2.6) | 5 (6.1) | 3 (12.5) | |||
| 1–3 times/wk | 67 (36.8) | 24 (31.6) | 33 (40.2) | 10 (41.7) | |||
| 4–6 times/wk | 5 (2.7) | 1 (1.3) | 3 (3.7) | 1 (4.2) | |||
| No answer | 100 (54.9) | 49 (64.5) | 41 (50.0) | 10 (41.7) | |||
| Semisolid yogurt | 0.002‡ | ||||||
| 1 time/day | 24 (13.2) | 7 (9.2) | 15 (18.3) | 2 (8.3) | |||
| 1–3 times/wk | 83 (45.6) | 25 (32.9) | 47 (57.3) | 11 (45.8) | |||
| 4–6 times/wk | 4 (2.2) | 1 (1.3) | 2 (2.4) | 1 (4.2) | |||
| No answer | 71 (39.0) | 43 (56.6) | 18 (22.0) | 10 (41.7) | |||
| Barriers for providing dairy products if answered “No” (n = 68) | 0.587 | ||||||
| Cost | 20 (29.4) | 14 (33.3) | 5 (26.3) | 1 (14.3) | |||
| Lack of perception of necessity | 15 (22.1) | 7 (16.7) | 5 (26.3) | 3 (42.9) | |||
| Difficulty in transport/storage | 12 (17.6) | 9 (21.4) | 3 (15.8) | 0 (0.0) | |||
| Low preference | 5 (7.4) | 4 (9.5) | 1 (5.3) | 0 (0.0) | |||
| Others | 8 (11.8) | 6 (14.3) | 1 (5.3) | 1 (14.3) | |||
| No answer | 8 (11.8) | 2 (4.8) | 4 (21.1) | 2 (28.6) | |||
Values are presented as number (%).
*The p values were analyzed using the χ2 test; †p < 0.05; ‡p < 0.01.
DISCUSSION
This study was conducted to investigate the snack provision in LFs and LHs in Korea and identify the factors influencing the provision of snacks. Only approximately 60% of LFs and LHs provided snacks to residents, and the frequency was low (one to three times a week), and the snacks provided to them were limited to three to four kinds. Government subsidies are needed to provide healthy snacks, such as fruits and dairy products, considering the intake capacity of the elderly people. Educating food service staff on the cooking methods and recipes that are conducive to food intake of older people can help improve the nutritional status of the elderly living in the facility.
The nutritional status of older adults is an important factor for improving the quality of life and maintaining a physically healthy life [21]. Most of the older people in LFs have chronic diseases [22,23,24] and receive all meals of the day at the facility; therefore, sufficient provision of meals and snacks by the facility could greatly affect the nutritional status of the residents [25]. Facilities generally provide residents with three meals a day; however, the availability, frequency, and type of snacks provided vary by facility. Because the digestive, chewing, and swallowing abilities of the older people deteriorate due to the aging of the digestive system, it is often difficult to consume enough nutrients with three meals a day; thus, nutritional supplementation through snack intake is important for proper nutritional intake [26]. It was found that 62% of elderly care facilities provided snacks. There were significantly more facilities that provided snacks than those that did not; however, it is concerning that 38% of the elderly care facilities did not provide snacks to residents. Elderly care facilities that provided snacks usually provided snacks one or two times a day between meals to residents, and the frequency and timing of snacks were found to be appropriate.
Fruits, as healthy snacks, are a major source of essential micronutrients, dietary fiber, and phytochemicals [27]. These can also play an important role in supplementing calories and nutrition that may be insufficient for the elderly people [28]. The frequency, type, and preference of fruit provision in elderly care facilities were investigated. More than 70% of facilities provided fruits, and most of them provided fruits one to three times a week. Facilities were burdened with providing fruit to residents, and only 28% of facilities provided fruits daily. This reality means that residents’ fruit consumption and nutrition may be insufficient if the family members of the elderly people do not provide additional fruit support. The fruits mainly provided by elderly care facilities were bananas, apples, tangerines, and watermelons, which matched the preferences noted in the survey results, that is, banana, watermelon, and mandarin. According to a food preference survey of the older adults living in the geriatric hospital, they preferred sweet, soft, and easy-to-eat bananas the most, followed by apples and watermelons [29]. A survey on the frequency of fruit intake among the elderly people has shown that tangerines, apples, watermelons, and bananas are frequently consumed in the order [2]. The older people had a low preference for pineapples, kiwi, and sweet persimmon because they are either hard or difficult to consume or are extremely sour. Changes in chewing function and taste affect the fruit preference in the elderly people, and the intake of hard or sour fruits gradually decreases, and these changes appear to affect the intake of various fruits by the elderly people. The findings of this study revealed that three to four kinds of fruits are mainly provided in LFs, indicating an extremely unvaried menu. It appears that two factors affect for the limited types of fruit provided: preference and price. The elderly people prefer fruits that are familiar and easy to chew and swallow, and facilities prefer fruits that are inexpensive and easy to provide, that is, banana, apples, and tangerines. The consumption of various fruits by the elderly people affects the incidence of chronic diseases and quality of life and has been reported to offer multiple health benefits [30]. Therefore, efforts and considerations are needed to provide a variety of fruits and fruit products in consideration of the older adults’ chewing ability and taste change.
Milk is a major source of protein and calcium and is a healthy snack that plays an important role in calcium intake, supplementing protein and calories, especially for the elderly people [31]. Dairy products, such as normal milk, low-fat milk, Yakult, liquid yogurt, and semisolid yogurt, were provided in more than 70% facilities; however, they were only provided one to three times a week. Considering that the frequency of providing dairy products is lower than the recommended eating pattern of the 2020 Dietary Reference Intakes for Koreans [10], it may be necessary to increase the frequency and variety of fruits and dairy products served in these facilities to improve the quality of life of the elderly people. It is useful to provide lactose-free products to the elderly people who are concerned about diarrhea and similar diseases due to reduced secretion of digestive enzymes with aging.
This study investigated the factors that make it difficult for elderly care facilities to provide snacks, such as fruits or dairy products. In providing a fruit as a snack, the cost and lack of manpower for fruit preparation according to the individual consumption ability of the elderly people were the main factors, because of the large variation in the chewing and swallowing ability of the residents. Regarding the provision of dairy products, the study found that there were high prices, lack of understanding of its necessity, and difficulties in managing short shelf life and refrigeration. Cost was found to be a major factor influencing the provision of snacks, such as fruits and dairy products, in LFs and LHs. This cost includes not only the money required to purchase snacks, such as fruits or daily products, but also labor cost for manpower required to prepare snacks according to the individual intake and mastication abilities of the residents. Therefore, if economic support is provided to expand the provision of snacks in elderly care facilities, it is judged that support for personnel recruitment and purchases will be necessary. It is also necessary to prepare a manpower system that manages and supervises whether economic support is properly used in LFs and LHs. Two additional supports are needed to provide dairy products to the elderly residents at an appropriate frequency. First, it is to educate food service personnel at LHs and LFs on the importance of dairy intake for the elderly people and the need to provide them. Second, providing recipes for various foods made using dairy products, such as milk rice cakes, risotto, pasta, steamed eggs, and cheese fried rice, will increase the intake of dairy products by residents.
Facilities registered as food service centers and LHs are obligated to employ a registered dietitian based on the Medical Service Act [32] and Food Sanitation Act [33]. On the contrary, employing a dietitian is not mandatory for facilities providing < 50 meals/day; hence, they mostly operate their own food service without a professional dietitian supervision. Investigating the general matters of meal service personnel in this study revealed that the proportion of clinical dietitians was low; however, > 80% of LHs and live-in LFs had dietitians, whereas it was < 40% for non-live-in LFs. In LHs and LFs, the elderly people are served meals three times a day while residing in the facility, whereas non-live-in LFs only provide one or two meals a day because they are visit-type facilities. The differences may be attributed to the characteristics of each facility, regardless of the presence or absence of a dietitian. Because elderly care facility users have several health problems, meals provided for the elderly people should include high-quality diets for the management of chronic diseases and maintenance of their health [34,35]. However, Kim et al. reported that the nutritional intake of the elderly living in nursing facilities is lower than the standard for nutritional intake [36,37]. Basic nutritional management services, such as proper meal therapy, have been reported to be improperly implemented when dietitians are not employed in nursing facilities, a trend which has rapidly increased in recent years [38,39]. In advanced countries, such as Japan and the United States, that have entered a super-aging society, dietary characteristics and major nutritional problems of the elderly people are analyzed, and guidelines for customized nutrition management are presented, in consideration of the health problems of the older adults [40,41]. However, in Korea, the nutritional management guidelines for the elderly people are not yet established, and there is a lack of manuals for providing meals at nursing facilities.
This study has a few limitations. First, in case the respondent of the survey is not a nutrition expert, there is a possibility for subjective error or improvised responses for questions that require nutritional knowledge. Second, only fruit and milk snacks were examined in detail, and the types of snacks served only occasionally were not investigated. However, when developing the questionnaire with the research team and registered dietitians, it was confirmed that fruits and milk were mainly provided when snacks were provided in elderly care facilities. To the best of our knowledge, this study is the first to investigate the provision of snacks in Korean nursing facilities, unlike previous studies that investigated only the meal intake of the elderly living in nursing facilities. The results of this study will serve as a cornerstone for reminding us of the importance of providing proper nutrition and the meaning of providing snacks in LFs. In addition, it will be a substantial report that informs what support is needed for the elderly living in elderly care facilities.
More than half of the LHs and LFs provided snacks to residents; however, 38% did not provide snacks. Even in the LHs and LFs that provided snacks, the frequency of provision was low, and the types of snacks were limited. Elderly care facilities had difficulty providing snacks, such as fruits and dairy products, because of the burden of cost, and this cost included both money for food purchase and labor cost. To improve the quality of life and the offer benefits of fruits and dairy products to the elderly people using the LHs and LFs, efforts are needed to propose a plan to expand the provision of snacks in appropriate quantities and varieties. Considering the reasons for low preference of fruits, it is necessary to provide them in a form that considers chewing and swallowing difficulties when providing fruits. Given that the main factor in providing snacks at facilities is price, improvements, such as adjusting expenses and manpower, are needed in the future.
ACKNOWLEDGEMENTS
The authors would like to thank the BK21 program “AgeTech-Service Convergence Major” through the National Research Foundation by the Ministry of Education of Korea (5120200313836).
Footnotes
Funding: This work was supported by the Ministry of Agro-food Resources, National Institute of Agricultural Sciences, Rural Development Administration in Korea.
Conflict of Interest: The authors declare that they have no competing interests.
- Conceptualization: Yeo D, Kang HJ, Ahn H, Park YK.
- Formal analysis: Yeo D, Kang HJ.
- Investigation: Yeo D, Kang HJ.
- Supervision: Ahn H, Park YK.
- Writing - original draft: Yeo D, Kang HJ.
- Writing - review and editing: Ahn H, Park YK.
SUPPLEMENTARY MATERIAL
General characteristics of the respondents
References
- 1.Suzuki T. Health status of older adults living in the community in Japan: recent changes and significance in the super-aged society. Geriatr Gerontol Int. 2018;18:667–677. doi: 10.1111/ggi.13266. [DOI] [PubMed] [Google Scholar]
- 2.Kim HY, Lee JS, Youn JC, Chang MJ. Food and nutrient intake status of Korean elderly by degree of cognitive function. J Nutr Health. 2016;49:313–322. [Google Scholar]
- 3.Statistics Korea. Statistics population Korea: future population projection [Internet] 2023. [cited 2023 June 6]. Available from https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA003&vw_cd=MT_ZTITLE&list_id=A41_10&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE.
- 4.Edwards RD, Brenowitz WD, Portacolone E, Covinsky KE, Bindman A, Glymour MM, Torres JM. Difficulty and help with activities of daily living among older adults living alone with cognitive impairment. Alzheimers Dement. 2020;16:1125–1133. doi: 10.1002/alz.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee MJ, Kim JH, Park OJ, Lee YM. A study on the needs for nutrition management program for elderly who use welfare facilities. Korean J Community Nutr. 2016;21:65–74. [Google Scholar]
- 6.Shin SH, Park JS. Factors influencing quality of life of elderly residents in long-term care facilities. J Korean Gerontol Nurs. 2017;19:113–124. [Google Scholar]
- 7.Kwon S. Future of long-term care financing for the elderly in Korea. J Aging Soc Policy. 2008;20:119–136. doi: 10.1300/J031v20n01_07. [DOI] [PubMed] [Google Scholar]
- 8.Kim SH, Kim DH, Kim WS. Long-term care needs of the elderly in Korea and elderly long-term care insurance. Soc Work Public Health. 2010;25:176–184. doi: 10.1080/19371910903116979. [DOI] [PubMed] [Google Scholar]
- 9.National Health Insurance Service. National health insurance statistical yearbook [Internet] 2021. [cited 2023 June 6]. Available from https://www.nhis.or.kr/nhis/together/wbhaec06300m01.do?mode=view&articleNo=10812384&article.offset=0&articleLimit=10&srSearchVal=%EC%9A%94%EC%96%91.
- 10.Ministry of Health and Welfare, The Korean Nutrition Society. Dietary reference intakes for Koreans. Sejong: Ministry of Health and Welfare; 2020. [Google Scholar]
- 11.Ministry of Health and Welfare. Status of long-term care facility utilization by region in 2017 [Internet] 2018. [cited 2023 June 6]. Available from https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=344487.
- 12.Organisation for Economic Co-operation and Development. Health at a glance. Paris: Organisation for Economic Co-operation and Development. 2021. [DOI] [Google Scholar]
- 13.Kwon JS, Lee SH, Lee KM, Lee Y. Study on energy and nutrient intake and food preference of the elderly in care facilities. Korean J Community Nutr. 2016;21:200–217. [Google Scholar]
- 14.Lee MS. Quality of nutrient adequacy and health-related quality of life of the rural elderly. Korean J Community Nutr. 2015;20:423–432. [Google Scholar]
- 15.Sloane PD, Ivey J, Helton M, Barrick AL, Cerna A. Nutritional issues in long-term care. J Am Med Dir Assoc. 2008;9:476–485. doi: 10.1016/j.jamda.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Burger C, Kiesswetter E, Alber R, Pfannes U, Arens-Azevedo U, Volkert D. Texture modified diet in German nursing homes: availability, best practices and association with nursing home characteristics. BMC Geriatr. 2019;19:284. doi: 10.1186/s12877-019-1286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai MR, Tsai HH, Tsai YF, Liao FY. “Tailoring homely meals”: family members’ motivations underlying nursing home visits during residents’ meals. Jpn J Nurs Sci. 2020;17:e12341. doi: 10.1111/jjns.12341. [DOI] [PubMed] [Google Scholar]
- 18.Namasivayam AM, Steele CM. Malnutrition and Dysphagia in long-term care: a systematic review. J Nutr Gerontol Geriatr. 2015;34:1–21. doi: 10.1080/21551197.2014.1002656. [DOI] [PubMed] [Google Scholar]
- 19.Power SE, Jeffery IB, Ross RP, Stanton C, O’Toole PW, O’Connor EM, Fitzgerald GF. Food and nutrient intake of Irish community-dwelling elderly subjects: who is at nutritional risk? J Nutr Health Aging. 2014;18:561–572. doi: 10.1007/s12603-014-0449-9. [DOI] [PubMed] [Google Scholar]
- 20.Barkoukis H. Nutrition recommendations in elderly and aging. Med Clin North Am. 2016;100:1237–1250. doi: 10.1016/j.mcna.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Lee HS. The factors influencing health-related quality of life in the elderly: focused on the general characteristics, health habits, mental health, chronic diseases, and nutrient intake status: data from the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V), 2010–2012. Korean J Community Nutr. 2014;19:479–489. [Google Scholar]
- 22.Xie F, Li J, Song W, Liu Q, Jiang S, Chen ZY, Shu Q. Long-term care facility and its elderly chronic diseases in Jishou: insights into underdeveloped area of China. Inquiry. 2022;59:469580221128735. doi: 10.1177/00469580221128735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell CL, Lee AS, Tamura BK. Malnutrition in the nursing home. Curr Opin Clin Nutr Metab Care. 2015;18:17–23. doi: 10.1097/MCO.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 24.Kim EM, Choi MK. An analysis of food consumption patterns of the elderly from the Korea national health and nutrition examination survey (KNHANES V-1) J Korean Soc Food Sci Nutr. 2013;42:818–827. [Google Scholar]
- 25.Park MS, Lyu ES. Importance and performance of dietitian’s task at long term care hospital foodservice in Busan · Kyungnam area. Korean J Community Nutr. 2011;16:602–612. [Google Scholar]
- 26.Toniazzo MP, Amorim PS, Muniz FW, Weidlich P. Relationship of nutritional status and oral health in elderly: systematic review with meta-analysis. Clin Nutr. 2018;37:824–830. doi: 10.1016/j.clnu.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 27.Lazzeri G, Pammolli A, Azzolini E, Simi R, Meoni V, de Wet DR, Giacchi MV. Association between fruits and vegetables intake and frequency of breakfast and snacks consumption: a cross-sectional study. Nutr J. 2013;12:123. doi: 10.1186/1475-2891-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kälviäinen N, Roininen K, Tuorila H. The relative importance of texture, taste and aroma on a yogurt-type snack food preference in the young and the elderly. Food Qual Prefer. 2003;14:177–186. [Google Scholar]
- 29.Bae MA, Kim MJ, Chang KJ. Foodservices satisfaction and food preference according to the types and cooking methods of the elderly with dementia in a geriatric hospital. J Korean Soc Food Cult. 2017;32:534–548. [Google Scholar]
- 30.Nicklett EJ, Kadell AR. Fruit and vegetable intake among older adults: a scoping review. Maturitas. 2013;75:305–312. doi: 10.1016/j.maturitas.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Givens DI. MILK symposium review: the importance of milk and dairy foods in the diets of infants, adolescents, pregnant women, adults, and the elderly. J Dairy Sci. 2020;103:9681–9699. doi: 10.3168/jds.2020-18296. [DOI] [PubMed] [Google Scholar]
- 32.Korea Legislation Research Institute. Medical service act in South Korea [Internet] 2023. [cited 2023 November 5]. Available from https://www.law.go.kr/LSW/lsInfoP.do?efYd=20211230&lsiSeq=225385#0000; https://elaw.klri.re.kr/eng_service/lawView.do?hseq=40970&lang.
- 33.Korea Legislation Research Institute. Food sanitation act in South Korea [Internet] 2023. [cited 2023 November 5]. Available from https://www.law.go.kr/LSW/lsInfoP.do?efYd=20220101&lsiSeq=234355#0000; https://www.mfds.go.kr/files/upload/eng/FOOD_SANITATION_ACT.pdf.
- 34.Buccheri C, Mammina C, Giammanco S, Giammanco M, Guardia ML, Casuccio A. Knowledge, attitudes and self-reported practices of food service staff in nursing homes and long-term care facilities. Food Control. 2010;21:1367–1373. [Google Scholar]
- 35.Kim YS, Park YS, Choi BB. Foodservice characteristics and satisfaction of the elderly with the welfare facilities in the northern Gyeonggi-do area. Korean J Food Nutr. 2014;27:872–880. [Google Scholar]
- 36.Yoon MO, Moon HK, Jeon JY, Sohn CM. Nutritional management by dietitian at elderly nursing homes in Gyeonggi-do. J Korean Diet Assoc. 2013;19:400–415. [Google Scholar]
- 37.Lim HS, Oh EB, Park YK, Chung HY. Study on the nutrient intake and dietary quality of elderly residents on various meal types in long-term care facility. J East Asian Soc Diet Life. 2020;30:172–181. [Google Scholar]
- 38.Choi JH, Kim DH, Choi EH, Chung MJ, Lee HS, Lee MJ, Chang HJ, Lee KE, Kwak TK. Assessment of foodservice management practices according to types of elderly foodservice facilities. J Korean Soc Food Sci Nutr. 2019;48:469–481. [Google Scholar]
- 39.Woo J, Park YK, Kim MH, Lee SK, Song K, Kim HK WOO J. Current status of sanitary and nutritional food service in elderly day care center. Korean J Community Nutr. 2020;25:374–385. [Google Scholar]
- 40.Ministry of Health, Labour and Welfare. Long-term care, health and welfare services for the elderly. Health and welfare bureau for the elderly [Internet] 2017. [cited 2023 November 5]. Available from https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/index.htmlhttps://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/index.html.
- 41.National Institute on Aging. Health eating after 50 [Internet] 2019. [cited 2023 November 5]. Available from https://order.nia.nih.gov/publication/healthy-eating-after-50.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
General characteristics of the respondents