Abstract
Background
Gangrenous sigmoid volvulus has a significant impact on morbidity and mortality. This study was conducted to compare sigmoid resection and primary anastomosis (RPA) with sigmoid resection and end colostomy (Hartmann's procedure) for gangrenous sigmoid volvulus.
Methods
A systematic review and meta-analysis study design was employed to summarize retrospective cohort, prospective cohort, and randomised control trial studies published from inception to march 31, 2023. Searching was performed on Medline, CINAHAL, Web of Science, Google Scholar, the Cochrane Library, and ClinicalTrials.gov to locate eligible articles. Data searching, selection and screening, quality assessment of the included articles, and data extraction were done by two separate reviewers. RevMan 5.4 software with a fixed-effect Mantel-Haenszel model and Stata version 14 were used to analyze the data. The protocol registered on PROSPERO registration website (CRD42023413367).
Results
Ten cohort studies and one randomised control trial with 724 patients were found; all of them were rated as being of moderate quality. The overall mortality after RPA was 15% (95%CI: 11-19%), and after Hartmann's procedure it was 19% (95%CI: 15-23%). Resection and primary anastomosis (RPA) for gangrenous sigmoid volvulus had slightly lower mortality rate than stoma (OR=0.98(95%CI: 0.68-1.42), p=0.07, I2=43%), which had no statistically significant difference. Resection and primary anastomosis (RPA) had a slightly higher morbidity rate than Hartmann's procedure (OR=1.01(95%CI: 0.66-1.55), p=0.30, I2=18%), which had no statistically significant difference.
Conclusion
Sigmoid resection and primary anastomosis (RPA) and Hartmann's procedure had no significant differences in mortality and morbidity for the treatment of gangrenous sigmoid volvulus. Choice of the intervention for gangrenous sigmoid volvulus should be individualized with consideration of different detrimental factors.
Keywords: sigmoid volvulus, gangrenous bowel, Primary resection and anastomosis, Stoma, Hartmann's procedure
Introduction
Sigmoid volvulus has a significant impact on morbidity, mortality, health-care costs, and emergency surgical burden. It is the third leading cause of large bowel obstruction in the western world, after colorectal cancer and diverticular disease, but it accounts for 50-80% of large bowel obstruction in the volvulus belt area such as Middle East, South America, Africa and Russia (1-5).
Meso-sigmoid twisting of upto1800 in sigmoid volvulus is considered physiological (6). Torsion beyond 1800 can lead to colonic ischemia, obstruction and perforation, and only 2% of cases can spontaneously derotate while 70% of cases occur in the counter clockwise direction (7,8).
More than one-third of sigmoid volvulus patients had gangrenous bowel (9). The significant aspect of gangrenous bowel is its high mortality, morbidity, and length of hospital stay (4). Evidence from hospital-based retrospective studies indicated that the incidence of mortality in gangrenous sigmoid volvulus ranged from 17-100% compared to 10-30% in non-gangrenous sigmoid volvulus (10).
Management of sigmoid volvulus depends on the viability of the bowel. For sigmoid volvulus patients with viable bowel and no signs of ischemia or perforations, sigmoidoscopic guided or rectal tube deflation have been advised as the first line treatment (8). Different investigations noted that urgent surgical intervention for sigmoid volvulus is required in 5-22% of patients when the deflation is not possible and 5-25% of patients presented with gangrenous bowel (11).
Urgent sigmoid resection has been advised in cases of gangrenous colon or when sigmoid volvulus deflation is unsuccessful (8). However, bowel continuity following resection has been a topic of debate for surgeons due to lack of highlevel evidences. After removing the gangrenous portion of the sigmoid colon, the decision to perform primary anastomosis or Hartmann's stoma should be individualized, taking into account both the patient's overall condition and the colon (11). As a result, this meta-analysis was conducted to compare resection and primary anastomosis versus Hartmann's stoma on mortality and morbidity among patients with gangrenous sigmoid volvulus.
Research question: Is resection and primary anastomosis more effective than stoma at preventing morbidity and mortality when treating gangrenous sigmoid volvulus?
Our meta-analysis question was based on PICOS approach.
Population = adult patient with diagnosis of gangrenous sigmoid volvulus
Intervention = Resection and primary anastomosis
Comparison = resection and primary anastomosis Vs stoma
Outcome = Mortality and morbidity
Studies = Cohort and randomized control trials
Methods
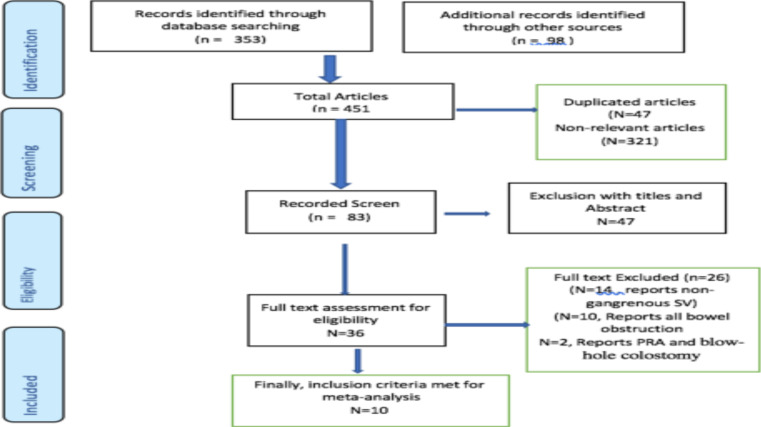
Study design: A systematic review and meta-analysis was conducted to summarize prospective cohort, retrospective cohort, and randomised control trial studies published from inception to march 31, 2023. This review was carried out in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (12,13) Figure 1). The protocol of this meta-analysis was registered at PROSPERO (CRD42023413367).
Figure 1.
Flow chart for selection of papers. Charts the selection of articles in the review in line with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) Framework
Eligibility criteria: Retrospective cohort, prospective cohort, and randomized controlled trial studies published from inception to March 31, 2023 on patients with gangrenous sigmoid volvulus who underwent primary resection and anastomosis versus stoma were considered to be eligible for inclusion. Systematic review studies, case reports, case series, and studies with unclearly reported results were excluded from the analysis. The English language restriction and time frame were chosen for convenience and sufficiency for demonstrating a trend of events (14,15)
Searching strategies and sources: Searching was performed at Medline, CINAHAL, Web of Science, Google Scholar, the Cochrane Library, and ClinicalTrials.gov to locate eligible articles. Two separate reviewers conducted the electronic data base search and selection of eligible articles. Disagreements between two reviewers were resolved through discussion, consensus, and, if necessary, the involvement of a third party. Our searching strategy was based on the Population, Interventions, Comparison, Outcomes, and Studies (PICOS) approach. Eligible articles were identified using key words and MeSH words in an electronic database, and hand searching using bibliographic or reference information from identified studies. Boolean operator, Wild cards, and splinting words and phrases were employed to widen our search. Terms such as “sigmoid”, “volvulus”, “gangrenous”, “intestinal obstruction”, “bowel obstruction”, “sigmoid volvulus”, “cohort”, “randomized control trial” “stoma”, “Hartman procedure”, and “colostomy” were used to search the eligible articles.
Screening and study selection: Two authors independently screened articles using the inclusion criteria. Duplicate studies from various electronic databases obtained through the search strategy were removed using the EndNote program. The titles and abstracts of the articles found through the search strategy were independently screened by two reviewers to eliminate obvious non-relevant papers. The full-text versions of the remaining potentially eligible articles were then retrieved and independently assessed by two reviewers to determine if they met the inclusion criteria. Disagreements are resolved through consensus and discussion. The corresponding author was contacted in order to obtain copies of papers whose full text was not available online. The reasons for exclusion at the full-text screen level were documented in accordance with the PRISMA framework. The total number of unique studies from all sources that meet the inclusion criteria have been recorded.
Data extraction and management: Data were extracted using a piloted standardized data extraction form adapted and customized from the Cochrane data extraction of randomized and non-randomized studies (16,17). The publication details, language of the paper, study period, study location, geographic setting, study design, study period, characteristics of participants, sample size and sampling technique, explanatory and outcome variables, data analysis, and the major findings were extracted.
Risk of bias assessment: The included studies' qualities were assessed using Cochrane RCT assessing tools that were specifically designed and validated for RCT studies (18). The JBI quality checklist was used for assessing the quality of observation studies (19). As with the study selection, two different investigators independently evaluated the quality of the included papers and characterized them as having high, moderate or low risk of bias.
Outcome of interest: Mortality and morbidity were the main outcomes of this review. Mortality was defined as a death that occurred prior to hospital discharge, and morbidity was defined as complication of Clavien Dindo Grades II–IV, which occurred after surgery and before discharge of the patient from the hospital.
Data synthesis and analysis: A standard pairwise meta-analysis was preformed using RevMan 5.4 software and STATA version 14. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated using fixed -effect Mantel-Haenszel model because our results would not make generalization beyond the included studies. Heterogeneity across the included studies were measured using Higgins (I2) test, which represents the percentage of variability in effect estimates among the included studies. Higgins (I2) test values of 25%-50%, 50-75% and above 75% were considered to have low, moderate, or high heterogeneity, respectively (20,21). Once heterogeneity was identified, sensitivity analysis was carried out by excluding one study at a time and assessing the impact on the final result. Publication biases for the mortality and morbidity was assessed using funnel plot.
Results
Ten retrospective and prospective cohort studies and one RCT studies involving 724 patients were found, all of which were labeled as having a moderate level of quality (22-31) (Figure 1). All studies reported that gangrenous SV was found predominantly in men. Management of gangrenous sigmoid volvulus is one of the clinical dilemmas due to absent high-level evidences.
Emergency surgical treatment for gangrenous sigmoid volvulus is associated with significant mortality and morbidity, regardless of whether it involves stoma or primary resection and anastomosis (8). Numerous small-scale clinical studies indicate that factors such as age, the presence of shock, comorbid conditions, Ileo sigmoid knotting, delayed presentation, and history of volvulus attacks affect mortality after emergency surgical intervention (8,22,32,33).
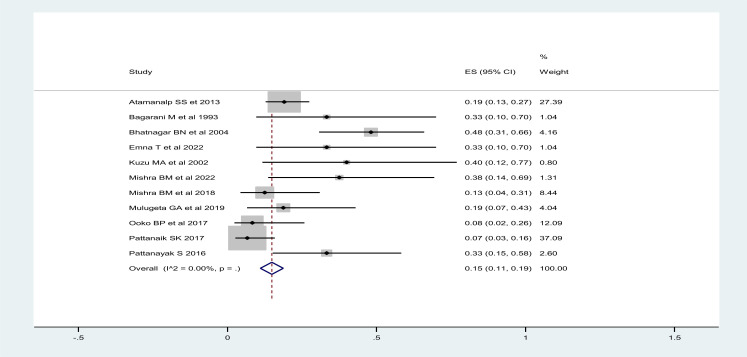
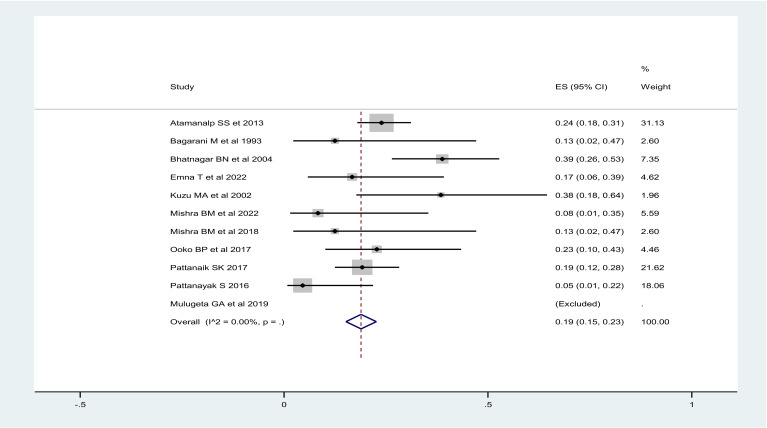
The mortality rate for gangrenous sigmoid volvulus was ranging from 9-42%, with overall mortality rate after surgical intervention being 19% (95%CI: 16-22%), regardless of the type of surgical interventions. Mortality after resection and primary anastomosis ranged from 8-48%, with overall mortality after RPA of 15% (95%CI: 11-19%) (Figure 2) and mortality after stoma ranged from 0-39%, with overall mortality rate of 19% (95%CI: 15-23%) (Figure 3).
Figure 2.
Overall mortality after resection and primary anastomosis for gangrenous sigmoid volvulus
Figure 3.
Overall mortality after stoma for gangrenous sigmoid volvulus
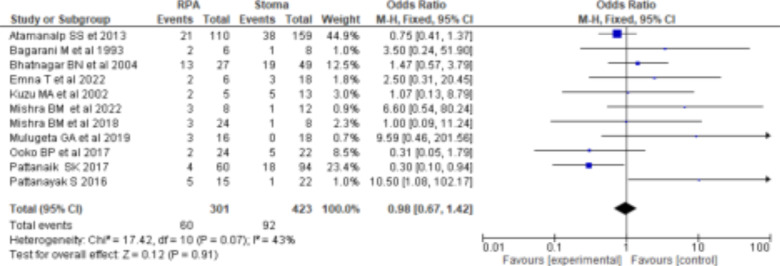
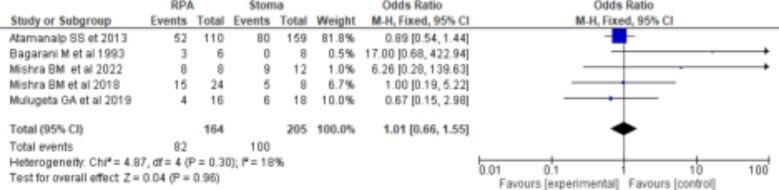
The mortality rate for gangrenous sigmoid volvulus ranged from 9-42%, with overall mortality rate after surgical intervention being 19% (95%CI: 16-22%). Resection and primary anastomosis for gangrenous sigmoid volvulus had a higher mortality rate than stoma (OR=0.98(95%CI: 0.68-1.42), p=0.07, I2=43%), which had no statistically significant difference (Figure 4). Five studies reported morbidity. Resection and primary anastomosis had a higher morbidity rate than stoma (OR=1.01(95%CI: 0.66-1.55), p=0.30 I2=18%), which had no statistically significant difference (Figure 5). Low levels of heterogeneity were found in the included studies (I2 for mortality and morbidity was 43% and 18%, respectively) (Figure 4 and 5) with no significant publication biases (Figures 6). Figure 4: Forest plot comparing RPA and Stoma mortality rates.
Figure 4.
Forest plot comparing RPA and Stoma mortality rates
Figure 5.
Forest plot comparing RPA and Stoma morbidity rates
Figure 6.
Funnel plot for Morbidity (A) and mortality (B)
The included articles did not find any evidence of mortality and morbidity with statistical significance associations with the type of procedure. However, the advice given in each of the articles included was not consistent. Some of the included articles suggested primary resection and anastomosis for gangrenous sigmoid volvulus with specific prerequisites like intraoperative hemodynamic stability, absence of gross contamination, capability to achieve a tensionfree anastomosis, presence of viable and well-vascularized bowel ends after resection, and good functional status (22,24-26,31). In contrast, some of the included studies in this review recommended stoma due to low mortality rates, fear of anastomotic leaks, quick procedure time, and short hospital stays (23,27,30).
Discussion
To the best of our knowledge, this is the first meta-analysis to provide evidence on the comparative safety of resection and primary anastomosis and Hartmann's stoma for the treatment of gangrenous sigmoid volvulus. This meta-analysis, which included 724 patients, was conducted using ten prospective and retrospective cohort studies and one RCT, which all were of moderate quality. Low levels of heterogeneity were found in the included studies (I2 for mortality and morbidity was 43% and 18%, respectively).
The findings of this review revealed that mortality rate after resection and primary anastomosis for gangrenous sigmoid volvulus was approximately 19%, which was fairly close to previous research findings based on clinical data collected over four decades with 393 emergency sigmoid volvulus surgeries, where mortality rate after primary anastomosis was 22% (4).
This study also found that mortality from resection and primary anastomosis and Hartmann's stoma had no statistically significant difference. Gangrenous sigmoid volvulus has a poor prognosis. Evidence from various studies indicated that the mortality rate for gangrenous sigmoid volvulus ranged from 11 to 80% compared to 6 to 24% for non-gangrenous sigmoid volvulus (4,10,33).
We also found that resection and primary anastomosis had slightly higher morbidity rate as compared with Hartmann's stoma, but this difference was not statistically significant. Emergency resection of sigmoid volvulus had a higher rate of postoperative complications (34). The most common morbidity conditions were anastomotic leaks and surgical site infections (4). Retrospective studies showed that a modified RPA and a modified blow-hole colostomy provide satisfactory results and help to avoid these morbid complications (35,36).
Despite a lack of high-quality evidence on the management of gangrenous sigmoid volvulus, this review found that the choice of stoma versus RPA had no different effect on morbidity or mortality, but stoma formation required a relatively less operation time. Low-level evidence and expert opinion suggest that, as long as the patient is stable and tension-free anastomosis is feasible, resection and primary anastomosis can be carried out with acceptable morbidity, mortality, and length of hospital stay.
Although high-level evidence is lacking, numerous small-sample and low-level evidences support resection and primary anastomosis for gangrenous sigmoid volvulus when certain conditions are met, such as intraoperative hemodynamic stability, the absence of gross peritoneal contamination, the ability to achieve a tension-free anastomosis, the presence of viable and well-vascularized bowel ends after resection, and good functional status (22,24-26,31). Gangrenous sigmoid volvulus is classified as group III in the Atamanalp 2020 sigmoid classification, which has the highest risk of mortality (10-60%) and morbidity (5-30%) (32). Atamanalp 2020 recommends resection and anastomosis for patients under the age of 70, ASA I-III, and intact bowel, whereas stoma is recommended for patients over the age of 70, ASA IV-V, and perforated bowel, or borderline ischemia (32). We devised a new protocol considering age, symptom duration, ASA, ECOG, organ dysfunction, cable tension free anastomosis, and the presence of septic shock. We recommended resection and primary anastomosis for patients aged less than 60 years, with ASA I-II, ECOG 0-II, symptom duration less than 72 hours, no organ dysfunction, no septic shock, and WBC count less than 18,000/mm3, whereas stoma was recommended for patients aged greater than 60 years, with ASA III-IV, ECOG III-IV, symptom duration more than 72 hours, septic shock with organ dysfunction, and WBC greater than 18,000/mm3 (Table1).
Table 1.
Atalel-Zelalem Proposed a new protocol for management of gangrenous sigmoid volvulus
| Resection and Anastomosis | Stoma | Definitions | |
| Age | <60years | >60years | |
| ASA class | I-II | III-V | |
| ECOG | 0-II | III-IV | |
| Duration | <72 hours | >72 hours | |
| Septic shock | No | Yes | SBP < 90mmHg and which is not responding to 20ml/kg fluid for the first one hour OR requiring vasopressor to maintain SBP above 90mmHg |
| Organ Dysfunction | No | Yes | Organ Dysfunction defined as Cardiovascular dysfunction: hypotension requiring treatment with dopamine ≥5 ug/kg per min, or any dose of norepinephrine OR Respiratory dysfunction: PaO2/FiO2 ratio <300 OR Neurological dysfunction: decreased level of consciousness OR Renal dysfunction: oliguria, creatinine >2.0 mg/dl OR Hepatic dysfunction: PT-INR >1.5 OR Hematological dysfunction: platelet count <100,000/mm3 |
| Bowel | Intact | Perforated and gross contamination bowel | |
| Anastomosis | Tension free and well vascular after 5-10cm resection distal to gangrenous bowel | Impossible | |
| WBC | <18,000 | >18,000 |
This review is the largest study with acceptable quality to provide clinically significant important information. First, it disproves the dogma that resection and primary anastomosis is associated with high mortality and morbidity in treatment of gangrenous sigmoid volvulus. Increased mortality and morbidity after surgical interventions have been linked to more heinous factors than just the specific surgical procedure. However, high level evidences are needed for further recommendations.
This review has some limitations. First, this meta-analysis as well as the included articles did not address the contributing factors for mortality and morbidity in each intervention. Second, high quality evidence was lacking in the included articles, which may be due to an ethical conflict in conducting randomized control trials.
In conclusion, this meta-analysis showed that resection and primary anastomosis and Hartmann's stoma had no significant difference in mortality and morbidity for the treatment of gangrenous sigmoid volvulus when performed with selection criteria. Resection and primary anastomosis is advised as the first line treatment for gangrenous sigmoid volvulus under certain conditions such as intraoperative hemodynamic stability, the absence of gross contamination, the capacity to achieve a tension-free anastomosis, the absence of comorbidity, the presence of viable and well-vascularized bowel ends after resection, and good functional status. The findings from this review have a better quality compared with previously available evidences on the management of gangrenous sigmoid volvulus. However, the area requires further extensive research in order to get a high level of evidence especially on examining the contributing factors for morbidity and mortality.
References
- 1.Heis HA, Bani-Hani KE, Rabadi DK, et al. Sigmoid volvulus in the Middle East. World J Surg. 2008;32:459–464. doi: 10.1007/s00268-007-9353-3. [DOI] [PubMed] [Google Scholar]
- 2.Avots-avotins KV, Waugh DE. Colon volvulus and the geriatric patient. Surg Clin North Am. 1982;62:248–260. doi: 10.1016/s0039-6109(16)42684-8. [DOI] [PubMed] [Google Scholar]
- 3.Halabi Wissam J, Jafari Mehraneh D, Kang Celeste Y, et al. Colonic Volvulus in the United States:Trends, Outcomes, and Predictors of Mortalit. Ann Surg. 2014;259:293–301. doi: 10.1097/SLA.0b013e31828c88ac. [DOI] [PubMed] [Google Scholar]
- 4.Oren D, Atamanalp SS, Aydinli B, Yildirgan MI, Başoğlu M, Polat KY, Onbaş O. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007;50(4):489–497. doi: 10.1007/s10350-006-0821-x. doi: 10.1007/s10350-006-0821-x. [DOI] [PubMed] [Google Scholar]
- 5.Dolejs SC, Guzman MJ, Fajardo AD, et al. Contemporary Management of Sigmoid Volvulus. J Gastrointest Surg. 2018;22:1404–1411. doi: 10.1007/s11605-018-3747-4. [DOI] [PubMed] [Google Scholar]
- 6.Ballantyne GH. Review of sigmoid volvulus: clinical patterns and pathogenesis. Dis Colon Rectum. 1982;25:823–830. doi: 10.1007/BF02553326. [DOI] [PubMed] [Google Scholar]
- 7.Shepherd JJ. The epidemiology and clinical presentation of sigmoid volvulus. Br J Surg. 1969;56:353–359. doi: 10.1002/bjs.1800560510. [DOI] [PubMed] [Google Scholar]
- 8.Tian BWCA, Vigutto G, Tan E, van Goor H, et al. WSES consensus guidelines on sigmoid volvulus management. World J Emerg Surg. 2023;18(1):34. doi: 10.1186/s13017-023-00502-x. doi: 10.1186/s13017-023-00502-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samuel JC, Akinkuotu A, Msiska N, Cairns BA, Muyco AP, Charles AG. Re-examining treatment strategies for sigmoid volvulus: An analysis of treatment and outcomes in Lilongwe, Malawi. Glob j Surg. 2010;1(2):149–153. [PMC free article] [PubMed] [Google Scholar]
- 10.Oneil N. Gangrene of Large Bowel Due to Volvulus-Etiopathogenesis, Management and Outcome. Gangrene - Current Concepts and Management Options. 2011. Aug 29, Available from: [DOI]
- 11.Vogel JD, Feingold DL, Stewart DB, Turner JS, Boutros M, Chun J, Steele SR. Clinical Practice Guidelines for Colon Volvulus and Acute Colonic Pseudo-Obstruction. Dis Colon Rectum. 2016 Jul;59(7):589–600. doi: 10.1097/DCR.0000000000000602. doi: 10.1097/DCR.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA PRISMA-P Group, author. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA PRISMA-P Group, author. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. doi: 10.1136/bmj.g7647. doi: 10.1136/bmj.g7647. Erratum in: BMJ. 2016 Jul 21;354:i4086. [DOI] [PubMed] [Google Scholar]
- 14.Edoardo Aromataris E, Riitano D. Constructing a Search Strategy and Searching for Evidence. AJN. 2014;114(5):49–56. doi: 10.1097/01.NAJ.0000446779.99522.f6. [DOI] [PubMed] [Google Scholar]
- 15.McKenzie JE, Brennan SE, Ryan RE, Thomson HJ, Johnston RV, Thomas J. Chapter 3: Defining the criteria for including studies and how they will be grouped for the synthesis. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons; 2019. pp. 33–66. [Google Scholar]
- 16.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020) Cochrane: 2020. Available from www.training.cochrane.org/handbook. [Google Scholar]
- 17.Cochrane Training. [May 29,2023]. https://training.cochrane.org/data-collection-form-rcts .
- 18.Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:14898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 19.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P-F. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. Available from https://synthesismanual.jbi.global. [Google Scholar]
- 20.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in metaanalyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deeks JJ, Higgins JPT, Altman DG, Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester (UK): John Wiley & Sons; 2008. Chapter 9: Analysing data and undertaking meta-analyses. [Google Scholar]
- 22.Bhatnagar B N, Sharma C L, Gautum A, Kakar A, Reddy D C. Gangrenous sigmoid volvulus: a clinical study of 76 patients. Int J Colorectal Dis. 2004;19(2):134–142. doi: 10.1007/s00384-003-0534-8. [DOI] [PubMed] [Google Scholar]
- 23.Mishra BM, Guru R, Sethy S, Manoj PR. Hartman's Procedure Vs Resection and Primary Anastomosis In Gangrenous Sigmoid Volvulus. International Journal of Surgery and Medicine. 2022;8(4):12–16. [Google Scholar]
- 24.Mishra BM, Mishra S, Sahoo B. Primary Resection and Anastomosis in Gangrenous Sigmoid Volvulus- A Prospective Study. JMSCR. 2018;06(12):683–687. [Google Scholar]
- 25.Ooko BP, White R. Management of gangrenous sigmoid volvulus at Tenwek Hospital in western Kenya. East Cent Afr J Surg. 2017;22(2):17–23. [Google Scholar]
- 26.Mulugeta GA, Awlachew S. Retrospective study on pattern and outcome of management of sigmoid volvulus at district hospital in Ethiopia. BMC Surg. 2019;19(1):107. doi: 10.1186/s12893-019-0561-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pattanayak S, Saha D, Bara BK, et al. Comparison of primary resection and anastomosis with Hartmann's procedure in management of acute sigmoid volvulus. Hellenic J Surg. 2016;88:226–263. doi: 10.1007/s13126-016-0329-3. [DOI] [Google Scholar]
- 28.Pattanaik SK. Emergency Management of Sigmoid Colon Volvulus in a Volvulus Belt Population and a Review of Literature. Indian J Surg. 2018;80(6):599–605. doi: 10.1007/s12262-017-1699-7. [DOI] [Google Scholar]
- 29.Emna T, Atef M, Sarra S. Management of acute sigmoid volvulus: A Tunisian experience. Asian J Surg. 2022;45(1):148. doi: 10.1016/j.asjsur.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Bagarani M, Conde AS, Longo R, Italiano A, Terenzi A, Venuto G. Sigmoid volvulus in west Africa: a prospective study on surgical treatments. Dis Colon Rectum. 1993;36(2):186–190. doi: 10.1007/BF02051177. [DOI] [PubMed] [Google Scholar]
- 31.Atamanalp SS. Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Tech Coloproctol. 2013;17(5):561–569. doi: 10.1007/s10151-013-1019-6. [DOI] [PubMed] [Google Scholar]
- 32.Atamanalp SS. Sigmoid volvulus: An update for Atamanalp classification. Pak J Med Sci. 2020;36(5):1137–1139. doi: 10.12669/pjms.36.5.2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atamanalp SS, Kisaoglu A, Ozogul B. Factors affecting bowel gangrene development in patients with sigmoid volvulus. Ann Saudi Med. 2013;33(2):144–148. doi: 10.5144/0256-4947.2013.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee K, Oh HK, Cho JR, et al. Surgical Management of Sigmoid Volvulus: A Multicenter Observational Study. Ann Coloproctol. 2020;36(6):403–408. doi: 10.3393/ac.2020.03.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coban S, Yilmaz M, Terzi A, et al. Resection and primary anastomosis with or without modified blow-hole colostomy for sigmoid volvulus. World J Gastroenterol. 2008;14(36):5590. doi: 10.3748/wjg.14.5590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sozen S, Das K, Erdem H, Menekse E, Cetinkunar S, Karateke F. Resection and primary anastomosis with modified blowhole colostomy or Hartmann's procedure. Which method should be performed for gangrenous sigmoid volvulus? Chirurgia (Bucur) 2012;107(6):751–755. [PubMed] [Google Scholar]