Abstract
This article describes a community–academic partnership designed and implemented to address disparities in accessing COVID-19 testing in Arizona, from November 2020 through March 2023. An equitable community-academic partnership, the involvement of local leaders, and the engagement of community health workers were critical for the success of the intervention. More than 5000 previously underserved patients were tested and received COVID-19 related services. A profile comparison with a matched group documents the success of the program in reaching the targeted population. (Am J Public Health. 2024;114(S5):S388–S391. https://doi.org/10.2105/AJPH.2024.307684 )
COVID-19 exposed systemic health disadvantages across the United States.1 In the Southwest, Latinx/Hispanic and other minoritized communities faced major barriers to COVID-19 testing.2 Vulnerable communities demonstrated high levels of resilience by adhering to mitigating behaviors and through their collective efforts to care for relatives and neighbors.3–5 This article reports on a project that capitalized on existing community partnerships to overcome barriers and increase health equity.
INTERVENTION AND IMPLEMENTATION
Grounded in 2 decades of community-academic collaboration, the project engaged community members in its design and implementation. The intervention, named RAPID (Respectful, Action-oriented, Proactive, Inclusive, and Direct-resources) for its guiding values, was spearheaded by Equality Health Foundation (EHF). EHF coordinated a multisectoral coalition and engaged community health workers (CHWs) for their deep community knowledge, trust, and patient engagement capabilities.6
The cross-sector alignment theory of change7 and a community-based participatory research orientation8 guided the project. Arizona State University (ASU) joined the effort through NIH’s Rapid Acceleration of Diagnostics-Underserved Populations (RADx-UP) initiative, providing methodological and logistical support.
In phase 1, communities were identified using state-level surveillance data publicly available from the Arizona Department of Health Services.9 We identify underserved communities through zip code tabulation areas (ZCTAs) with a higher positivity rate than the state median and lacking local testing sites. The Community and Scientific Advisory Board (CSAB) ranked those communities in order of priority. CSAB members leveraged their networks to gauge socio-cultural and other barriers to accessing COVID-19.
During phase 2, the team promoted and implemented testing events in coordination with local partners. Coalition members and the CSAB identified local community partners (churches, social services, etc.). Together with CHWs they identified and addressed specific community needs and chose culturally appropriate and accessible locations for the testing.
In phase 3, CHWs provided a warm welcome to all (including walk-ins), administered noninvasive saliva-based rapid COVID-19 tests (qPCR molecular), provided patient education, and administered the intake survey. A biomedical unit at ASU analyzed test samples and posted results on a secure online site. Patients were able to check their results immediately, but many did not have Internet access. CHWs followed-up with those who had not checked their results within 48 hours.
In phase 4, CHWs made follow-up calls to ensure that patients understood their test results and provided wraparound services (e.g., food and housing assistance) as needed. A medical provider from the local federally qualified community health center provided consultation calls to those who tested positive, guiding them through the isolation period and addressing medical questions.
PLACE, TIME, AND PERSONS
Central to the intervention were 10 bilingual/bicultural CHWs trained in public health from a Phoenix-based agency called Helping Families in Need,10 who participated in the intervention design and trained CHWs across Arizona and tribal communities to assist at local testing sites. CHWs training included the CDC’s COVID-19 mitigating behaviors, patient recruitment, follow-up protocols with patients who tested positive, and conducting saliva tests and social determinants of health surveys, after attaining CITI certification. CHWs addressed questions and dispelled myths or rumors circulating in the community regarding COVID-19 testing and vaccination, and helped overcome language, technological, and health literacy barriers, such as navigating online services. The team designed and implemented a publicity and outreach plan tailored to each community, including flyers, PSAs on social media and radio, and presentations at local institutions.
The 4-phase RAPID intervention was implemented 60 times in 20 low socioeconomic status (SES), predominantly Latinx underserved communities across Arizona, testing over 5000 individuals by March 2023. Table 1 highlights characteristics of the 20 targeted communities as compared with other ZCTAs in Arizona (n = 258). Of these communities, 60% were in Maricopa County.
TABLE 1—
Comparison of Communities With and Without RAPID Testing Sites: Arizona, November 2020–March 2023
| Demographic Variables | ZCTA with RAPID Testing Sites (n = 20) | ZCTA without RAPID Testing Sites (n = 258) |
| Mean % of Residents (SD) | Mean % of Residents (SD) | |
| Female | 50.1 (2.4) | 49.9 (5.6) |
| Non-Hispanic Whites | 23.0 (20.4) | 64.2 (22.5) |
| Completed high school or more education | 73.3 (11.4) | 88.9 (9.5) |
| Foreign-born | 19.6 (12.6) | 10.2 (7.9) |
| Speaking another language at home & Speaking English less than “very well” | 15.8 (10.5) | 6.2 (7.5) |
| Speak Spanish at home & Speaking English less than “very well” | 13.7 (11.6) | 5.1 (7.5) |
| Residents with health coverage | 82.7 (6.2) | 90.8 (6.9) |
| Household income below federal poverty line | 13.5 (6.3) | 11.6 (12.3) |
| Work from home | 6.0 (4.4) | 9.4 (7.1) |
Note. RAPID = Respectful, Action-oriented, Proactive, Inclusive, and Direct-resources; ZTCA = zip code tabulation area. Only zip code areas in Arizona for which biweekly COVID-19 case numbers were published by the Arizona Department of Health Services are compared. Excludes 123 zip code areas whose COVID-19 case numbers were not published from the analyses.
Source. The data analyzed are from the 5-y Estimates of the American Community Survey, with the final year being 2020.
PURPOSE
The partnership aimed to reduce health inequities in the context of the COVID-19 pandemic by reducing disparities in accessing testing, public health education, wraparound social services, and primary care.
EVALUATION AND ADVERSE EFFECTS
The project succeeded in increasing access to testing by underserved communities. Thirty-three percent of participants received or were referred to social services, 27% received vaccination registration assistance, and 5% were scheduled for vaccination appointments. Initially, only patients who tested positive received follow-up calls offering wrap-around services, but this was later extended to include all participants.
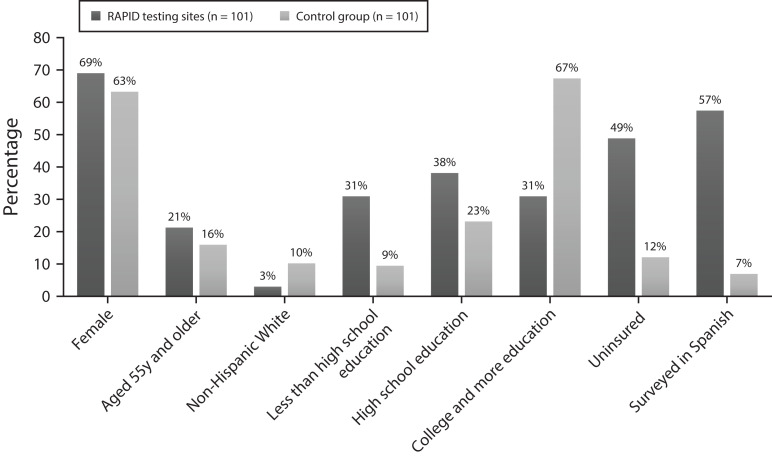
Figure 1 highlights social determinants of health among survey participants from the RAPID testing sites (n = 101) and the matched comparison group (n = 101) recruited from a list provided by the university-run testing sites (the standard of care within designated ZCTAs) operating near the RAPID testing sites. The university sites required online registration, a car, and English proficiency, lacking culturally and linguistic congruent services, wraparound services or public health information.
FIGURE 1—
Social Determinants of Health among Survey Participants of RAPID Testing Sites (n = 101) and Control Group Recruited from Geographically Adjacent University-Run Testing Sites (n = 101), Arizona, November 2020–March 2022
The majority (80%) of the 202 survey participants lived within the 20 targeted communities. The communities were distributed across the state, they were urban, semiurban, rural and tribal. More than 5000 participants took the COVID-19 saliva rapid test, 1000 completed the intake survey, and a subgroup of 101 completed the more extensive common data elements (CDEs) survey. During the first months of testing, the intervention team was not able to conduct the longer survey due to delays in receiving the results. CDEs surveys were conducted over the phone or online; the absence of working phones and unanswered calls in part explain the lower number of completed CDEs surveys. During the first 12 months of the project, only participants with a positive test result were invited to complete the CDEs survey.
In comparison with those from the university-sponsored sites, the RAPID participants were more likely to be: female (69.0% versus 63.3%); older than 54 years old (21.3% versus 16.0%), non-White (97.0% versus 89.8%); lacking a high school diploma (30.9% versus 9.5%); and without health insurance (48.8% versus 12.1%). By deploying bilingual CHWs, the RAPID model served a significantly higher percentage of participants who completed the survey in Spanish (57.4% versus 6.9%).
SUSTAINABILITY
NIH supplemental funding expanded the areas and populations covered by the RAPID project, including transnational populations between the Mexico-US border and asylum seekers crossing through Arizona. It also added the NIH CDE survey. The partnership evolved to include state-, county-, and city-administered funding to deliver COVID-19 education and vaccination to vulnerable and underserved residents of Arizona.11
CHWs were compensated though EHF through a subcontract with ASU’s RADx-UP award. The CHWs qualified for reimbursement toward the conclusion of the project. Arizona’s state Medicaid program (AHCCCS) started to reimburse for CHW services under its state plan in February 2023. These statutory and financial amendments were crucial for sustaining public health interventions such as the RAPID model.
PUBLIC HEALTH SIGNIFICANCE
The success of the RAPID model stemmed from strong coalitions, the community-academic partnership, skilled CHWs, and their ability to address the needs (i.e., cultural and language congruent services) of the communities they serve. CHWs involved in the intervention were bilingual, culturally competent, knowledgeable about available resources and skillful in connecting community members to those resources. The RAPID model is easily transferable across different cultural and geographic contexts as its key components are flexible and adaptable. The COVID-19 pandemic landscape continues to evolve, and the project’s ability to evolve with it into new locations and populations is significant.
The research team will continue to make adaptations to the intervention model to provide quality care to vulnerable communities that have been historically underserved. This project increased Arizona’s capacity to respond to the next public health crisis, and demonstrated that strong community-academic partnerships–when nurtured over time–provide an ideal platform to respond to health crises in an equitable manner.
ACKNOWLEDGMENTS
Research reported in this Rapid Acceleration of Diagnostics–Underserved Populations (RADx-UP) publication was supported by the National Institutes of Health (award 3U54MD002316-14S1). Application of the RAPID model was expanded to additional regions and populations by NIH supplemental funding (award 3U54MD002316-14S1; U54MD002316-15S1) and the RADx-UP pilot project (award A03-5092).
We acknowledge the participants and leaders from communities across Arizona, Helping Families in Need, the Equality Health Foundation, the entire team at ASU, participating NGOs, and governmental agencies in the coalition.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
Human subject protection protocols were approved by the Arizona State University institutional review board.
REFERENCES
- 1.MageshS , JohnD , LiWT , et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. 10.1001/jamanetworkopen.2021.34147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LopezL , HartLH , KatzMH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719–720. 10.1001/jama.2020.26443 [DOI] [PubMed] [Google Scholar]
- 3.JimenezME , Rivera-NúñezZ , CrabtreeBF , et al. Black and Latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Netw Open. 2021;4(7):e2117074. 10.1001/jamanetworkopen.2021.17074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.OromH , AllardNC , KiviniemiMT , et al. Racial/ethnic differences in prosocial beliefs and prevention behavior during the COVID-19 pandemic. J Racial Ethn Health Disparities. 2021;9(5): 1807–1817. 10.1007/s40615-021-01117-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MyersonJ , StrubeMJ , GreenL , HaleS. Individual differences in COVID-19 mitigation behaviors: The roles of age, gender, psychological state, and financial status. PLoS One. 2021;16(9):e0257658. 10.1371/journal.pone.0257658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernandez-SalinasC , MarsigliaFF , OhH , CamposAP , De La RosaK. Community health workers as puentes/bridges to increase COVID-19 health equity in Latinx communities of the southwest U.S. J Community Health. 2023;48(3):398–413. 10.1007/s10900-022-01182-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LandersGM , MinyardKJ , LanfordD , HeishmanH. A theory of change for aligning health care, public health, and social services in the time of COVID-19. Am J Public Health. 2020;110(S2): S178–S180. 10.2105/AJPH.2020.305821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WallersteinN , DuranB. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(S1):S40–S46. 10.2105/AJPH.2009.184036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arizona Department of Health Services. ADHS COVID Dashboard. 2022. Available at: https://azdhs.gov/preparedness/epidemiology-di . Accessed December 10, 2022.
- 10.Equality Health Foundation. Herozona Foundation. ONE Community Initiative Against COVID-19. 2021. Available at: https://www.onecommunityaz.com/ . Accessed July 23, 2023.
- 11.NIH. (2024). Common Data Elements (CDEs) Program. Accessed it on 03-10-2024. https://heal.nih.gov/data/common-data-elements