Summary:
For autologous breast reconstruction using the deep inferior epigastric perforator flap, the internal mammary vessels are a common choice for recipient vessels. However, if these vessels are discovered to be inadequate, this may require the utilization of alternative vessels for successful salvage. Here, we demonstrate the use of a venous conduit for flap salvage in a patient undergoing bilateral deep inferior epigastric perforator flap breast reconstruction. Intraoperative venous congestion was identified on the left side. A contributing factor was an unresolvable size discrepancy between the deep inferior epigastric and the internal mammary venae comitantes. A saphenous vein graft can be used to drain the donor inferior epigastric vein to the contralateral internal mammary venae comitantes. In this discussion, adequate venous drainage was obtained with this approach, and the flap remained viable with good Doppler signals without further complications over a year postoperatively.
Takeaways
Question: How can venous congestion of a deep inferior epigastric perforator flap be managed when discovered on the table, when the ipsilateral vessels are inadequate for salvage?
Findings: A saphenous vein graft can be used to drain the donor inferior epigastric vein to the contralateral internal mammary venae comitantes.
Meaning: The case presented contributes evidence of successful utilization of a saphenous vein graft to bridge the donor and recipient vessels during an occurrence of an unsuitable left-sided vein in the setting of intraoperative venous congestion.
CASE PRESENTATION
The deep inferior epigastric perforator (DIEP) flap has become a mainstay for autologous reconstruction with generally low complications and risk of flap failure. The internal mammary vessels, which are a popular recipient vessel choice, can occasionally be found to be suboptimal intraoperatively. A common reason for recipient vessel concern is related to size mismatch resulting in turbulent flow.1 Irradiation is a common reason for the smaller diameter of the internal mammary vessels in this population, but this can also be a normal anatomical finding or variant.1–4 Attempts to use these suboptimal vessels can lead to a higher risk of complications. When suboptimal recipient vessels are encountered, early identification and intervention are key to flap salvage and a successful reconstruction. Here, we reengage this principle by discussing a case in which a tunneled, cross-thoracic, saphenous vein graft was used to successfully manage intraoperative venous flap congestion.
A 47-year-old woman with a history of right invasive mammary carcinoma previously treated with neoadjuvant chemotherapy, bilateral skin-sparing mastectomy, right sentinel lymph node biopsy, and radiation therapy presented for autologous breast reconstruction (Fig. 1), and was offered bilateral DIEP flap reconstruction. The perforator flap dissection proceeded uneventfully. Recipient site preparation was notable for very small, approximately 1.5-mm diameter left internal mammary venae comitantes (IMVCs). Following anastomoses of the deep inferior epigastric vein to the left medial IMVC, venous congestion of the flap was apparent within minutes. The contralateral radiated IMVCs were both of adequate size, the anastomoses proceeded uneventfully, and the right flap was well perfused without evidence of venous congestion. With the persistence of inadequate left-sided venous outflow, the decision was made to create a tunneled saphenous vein conduit to reach the unused right lateral IMV, which was of adequate caliber to provide antegrade venous drainage from the congested left-sided flap. The saphenous vein was harvested, and a presternal subcutaneous tunnel was developed to pass the vein graft from the left to the right flap recipient site. To maintain patency of the graft itself, the adipose layer was cored out until it was wide enough to ensure that the graft would be both tension and compression-free yet narrow enough to prevent a contour deformity or symmastia. Coupled end-to-end anastomoses were performed between the flap vein and vein graft (3-mm coupler), and between the vein graft and the right lateral IMV (2.5-mm coupler; Fig. 2). (See figure, Supplemental Digital Content 1, which displays insetting of the DIEP flaps following saphenous vein graft anastomoses. http://links.lww.com/PRSGO/D216.) There was no immediate or delayed venous congestion noted, and both flaps demonstrated adequate perfusion and drainage (Fig. 3). An implantable venous Doppler was placed to monitor flap viability in the postoperative period. The patient’s immediate postoperative course was uncomplicated, with reassuring flap skin paddle appearance and Doppler signals bilaterally. She was discharged unremarkably on postoperative day 4 and continues to do well over 6 months and 1 year after her reconstruction (Fig. 4). She has since undergone revision for asymmetry with fat grafting to the right radiated reconstructed breast and reduction/uplift of the left flap.
Fig. 1.
Preoperative photograph of the 47-year-old woman following bilateral skin-sparing mastectomy with right sentinel lymph node biopsy.
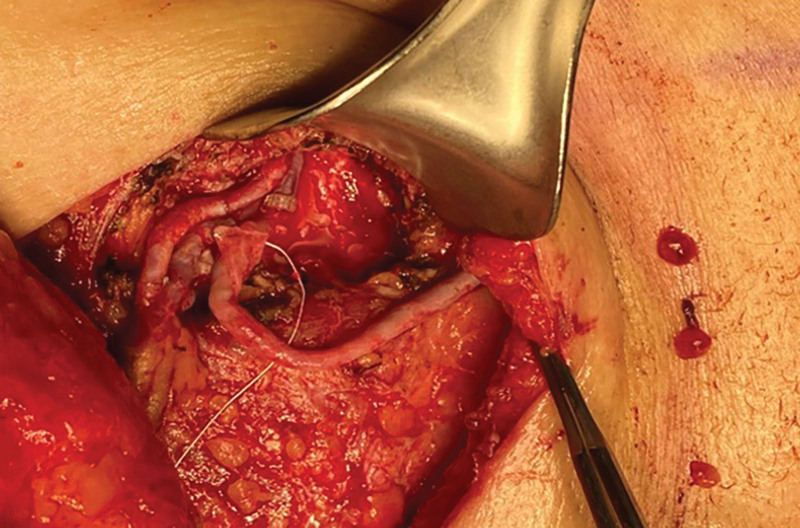
Fig. 2.
The saphenous vein graft is anastomosed from the left-sided DIEP flap to the right internal mammary venae comitantes.
Fig. 3.
With the patient in supine position, there is a lack of immediate venous congestion following flap insetting.
Fig. 4.
Postoperative photographs at 12 months following bilateral DIEP flap breast reconstruction salvaged with a cross-thoracic saphenous vein graft.
DISCUSSION
DIEP free tissue transfer is a commonly used and accepted method of autologous breast reconstruction. From a surgeon’s perspective, the donor site perforator anatomy and quality are consistently reliable with low donor site morbidity.5 The IMVCs are conveniently located within the recipient site, and have a relatively large diameter and high outflow, making them the most commonly used recipient veins in free flap breast reconstruction.6 However, in the setting of even subtle intraoperative venous congestion, rapid intervention to augment or identify alternate recipient vessels for optimal venous outflow is imperative in preventing flap failure.
In 2009, Flores et al7 reported their use of the saphenous vein graft as a salvage option for two cases of DIEP flap breast reconstruction complicated by flap thrombosis and venous congestion. From a broader perspective, intraoperative identification of flap compromise, as opposed to postoperative identification, generally yields a better prognosis with reduced flap complications. The prognosis is also improved with fewer salvage attempts. In the case presented here, the existence of two adequately sized right IMVCs allowed us to use this unique salvage option. If there is only one adequately sized IMVC, as is often the case, other potential recipient vessels may include the lateral thoracic vein, thoracodorsal vein, and cephalic vein turn-down, among others. Although techniques and algorithms to augment venous outflow for management of intraoperative venous congestion have been described, more data are ultimately needed to help surgeons make rapid, confident decisions.8–10 The case presented here demonstrates successful use of a saphenous vein graft to span the presternal space to reach a contralateral IMV recipient vessel, correct the venous outflow issue, and allow for tension-free anastomosis and ideal flap orientation and inset. For future patients in whom there is evidence of venous congestion due to inadequate recipient venous drainage, it may be wise to consider this option.
DISCLOSURES
The senior authors are military service members. All the other authors have no financial interest to declare in relation to the content of this article. The views expressed in the article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
Supplementary Material
Footnotes
Published online 22 May 2024.
Presented at Virginia Society of Plastic Surgeons, September 2022, Charlottesville, Virginia, and at American Society of Plastic Surgeons, Plastic Surgery the Meeting, October 2023, Austin, Texas.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;17:202–210. [DOI] [PubMed] [Google Scholar]
- 2.Changchien CH, Fang CL, Hsu CH, et al. Creating a context for recipient vessel selection in deep inferior epigastric perforator flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2023;84:618–625. [DOI] [PubMed] [Google Scholar]
- 3.López IR, Sebastián JD, Jarillo LL, et al. Análisis de las diferencias de calibre entre las venas mamarias internas derecha e izquierda y su relación con múltiples factores en reconstrucción microquirúrgica de mama. Cir. plást. iberolatinoam. 2023;49:75–79. [Google Scholar]
- 4.Tran NV, Buchel EW, Convery PA. Microvascular complications of DIEP flaps. Plast Reconstr Surg. 2007;119:1397–1405. [DOI] [PubMed] [Google Scholar]
- 5.Ludolph I, Horch RE, Harlander M, et al. Is there a rationale for autologous breast reconstruction in older patients? A retrospective single center analysis of quality of life, complications and comorbidities after DIEP or ms-TRAM flap using the BREAST-Q. Breast J. 2015;21:588–595. [DOI] [PubMed] [Google Scholar]
- 6.Saint-Cyr M, Youssef A, Bae HW, et al. Changing trends in recipient vessel selection for microvascular autologous breast reconstruction: an analysis of 1483 consecutive cases. Plast Reconstr Surg. 2007;119:1993–2000. [DOI] [PubMed] [Google Scholar]
- 7.Flores JI, Rad AN, Shridharani SM, et al. Saphenous vein grafts for perforator flap salvage in autologous breast reconstruction. Microsurgery. 2009;29:236–239. [DOI] [PubMed] [Google Scholar]
- 8.Boissiere F, Gandolfi S, Riot S, et al. Flap venous congestion and salvage techniques: a systematic literature review. Plast Reconstr Surg Glob Open. 2021;9:e3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ochoa O, Pisano S, Chrysopoul M, et al. Salvage of intraoperative deep inferior epigastric perforator flap venous congestion with augmentation of venous outflow: flap morbidity and review of the literature. Plast Reconstr Surg Glob Open. 2013;1:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehrara BJ, Santoro T, Smith A, et al. Alternative venous outflow vessels in microvascular breast reconstruction. Plast Reconstr Surg. 2003;112:448–455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.