Abstract
Introduction
Cluster headache is a severe and debilitating neurological condition characterized by intense, excruciating pain with a significant impact on patients' wellbeing. Although different treatment options are available, many patients continue to experience inadequate relief. Therefore, experimental strategies are increasingly studied. One of the more promising approaches is the use of ketamine. We present the currently available evidence and our own data.
Methods
In this mixed-methods paper, we first summarize the available evidence of ketamine for treatment of cluster headache based on a systematic review of literature in MEDLINE, EMBASE and the Cochrane library of systematic reviews. As the level of evidence is quite limited, we report our own cohort study with ten patients treated with ketamine infusions for cluster headache. They were followed up to investigate the patients’ experience of treatment success and quality of life.
Results
The search and review of literature identified four reports with a total of 68 patients. All were uncontrolled case series. The current literature suggests that ketamine might decrease cluster headache. However, as the applied regimes and reported outcomes are highly heterogeneous, further analysis was futile. Our own data show high patient satisfaction with ketamine treatment.
Conclusion
Despite the limited evidence, ketamine might be considered a potential therapeutic approach for cluster headache. Therefore, further research including randomized controlled trials should be encouraged.
Keywords: Cluster headache, Ketamine, Treatment, Systematic review, Quality of life
Plain Language Summary
This article discusses the potential use of ketamine for the treatment of cluster headache, a severe neurological condition that can have a significant impact on patients' quality of life. The authors conducted a systematic review of the existing literature on ketamine for the treatment of cluster headache. Additionally, they also presented their own cohort study of ten patients receiving ketamine infusions. The review of the literature revealed four reports with a total of 68 patients, all of which were uncontrolled case series. While the current literature suggests that ketamine may be effective in relieving cluster headache symptoms, the heterogeneity of treatment regimens and reported outcomes makes it difficult to draw definitive conclusions. The authors' own cohort study found that patients were very satisfied with ketamine treatment, indicating a potential benefit of this approach. However, due to the limited evidence available, further research, including randomized controlled trials, is needed to better understand the efficacy of ketamine in the treatment of cluster headaches.
Key Summary Points
| Why carry out this study? |
| Cluster headache is a severe and debilitating neurological condition characterized by intense, excruciating pain with a significant impact on patients' wellbeing. |
| Although different treatment options are available, many patients continue to experience inadequate relief. |
| This study evaluates the body of evidence regarding ketamine for the treatment of cluster headache. Furthermore, the authors add data from their own cohort. |
| Despite the limited evidence, ketamine might be considered a potential therapeutic approach for cluster headache. |
| Further research including randomized controlled trials should be encouraged. |
Introduction
Cluster headache is a severe and debilitating neurological condition characterized by intense, excruciating pain with a significant impact on patients' wellbeing [1]. Patients suffering from cluster headache experience tremendously decreased quality of life compared to a healthy population [2] and often show self-directed aggression, depression [3] and increased suicidality [4]. Although a combination of genetic and environmental factors seems to play a role, the exact causes of cluster headaches remain unclear [5]. About 85–90% of patients are typically categorized as having episodic cluster headaches, which are characterized by attacks that last for a few weeks to months, followed by periods of remission that can last for several months to years. On the other hand, chronic cluster headaches are distinguished by attacks that either occur without a remission period or have a remission period of < 3 months, lasting for at least 1 year. The treatment of chronic cluster headaches is generally more challenging because of various factors, including the need for concurrent long-term use of multiple treatment options and their adverse effects [6]. Acute and prophylactic treatment is used for both entities, but prophylactic medication is considered the mainstay of treatment. For acute treatment, triptans (sumatriptan and zolmitriptan) are preferably applied intranasally or subcutaneously, as oral triptans have slow onset. They should however only be used twice a day, leaving patients and practitioners in need of alternatives if attacks occur more often. Inhalation of 100% oxygen is also an established treatment but impractical to use outside patients’ homes [7]. For transition treatment, prednisolone and greater occipital nerve blockade are recommended. Verapamil, topiramate and lithium can be used for maintenance prophylaxis but require ECG (topiramate) or regular serum level monitoring (lithium) [7, 8]. Many patients continue to experience inadequate relief [8], and a recent consensus statement has advocated the need for novel treatment modalities [9].
Experimental treatment strategies are currently being investigated, e.g., somatostatine [10]. However, the effect is extremely short-lived, which is why the somatostatin analog octreotide, featuring a longer half-life, has been proposed as an alternative [11, 12]. Overall, available data are inadequate, and thus far, triptans seem superior. Therefore, somatostatin analogs should only be used as an alternative if there are contraindications to triptans [13]. Occipital nerve block is a further therapy option, which is increasingly studied in patients with cluster headache. Despite a lack of large randomized clinical trials, a recent meta-analysis suggests potential benefits [14].
More recently, psychotropic substances were evaluated for their effect on cluster headache [15–17]. Sewell et al. published a case series that provides promising results, showing that lysergic acid diethylamide (LSD) could be prophylactically effective for treatment of cluster headache [18]. Two placebo-controlled studies are currently underway to investigate the efficacy of LSD on cluster headache. One study examines the effect of particularly low doses on chronic cluster headache, whereas the other study is investigating higher doses and the effect on unspecified cluster headache [19, 20]. Likewise, psilocybin, the psychoactive ingredient in psilocybin mushrooms, is said to be effective not only for prophylactic but also acute treatment of cluster headache [18]. Recently, a first exploratory study showed moderate effects; however, due to the low sample size, its results failed to achieve significance [21]. Another study investigating the prophylactic effect of psilocybin on chronic cluster headache was discontinued because not enough patients could be recruited because of the Covid-19 pandemic [22].
Ketamine shares clinical similarities with substances like LSD and psilocybin [23]. Introduced as an alternative to phencyclidine, it has been used in clinical practice since 1970. Due to its combination of hypnotic, analgesic and amnestic effects, ketamine is unique in its clinical use. Ketamine mainly acts on glutamate binding sites and NMDA and non-NMDA receptors. The allosteric antagonism of the NMDA receptor is responsible for the specific properties of ketamine (amnestic and psychosensory effects, analgesia and neuroprotection). There are also other mechanisms that are independent of glutamate. These include binding sites such as opioid, GABA-monoaminergic, cholinergic, nicotinic and muscarinic receptors [24]. The anesthetic effect of S( +)-ketamine is approximately three to four times more potent than R(-)-ketamine [25].
Beyond ketamine’s fundamental role in the field of anesthesia, emergency medicine and intensive care, it is widely used for its anti-hyperalgesic and anti-neuropathic effects in perioperative medicine and pain medicine [26, 27]. More recently, depression and suicidal ideation have been identified as novel indications [28, 29]. Based on these observations, it is reasonable to assume that ketamine could also have a positive effect in the treatment of cluster headaches.
In this paper, we will examine the effect of ketamine on cluster headaches. We conducted a systematic review of the available literature and will provide a summary of our findings. Second, we will present a case series based on our own experiences, as we were especially interested in patients’ quality of life and their satisfaction with treatment, which to the best of our knowledge has not been investigated.
Methods
Systematic Review of the Literature on the Treatment of Cluster Headache with Ketamine
Search Strategy
We carried out a systematic literature search in the following databases: MEDLINE, EMBASE and the Cochrane library of systematic reviews. We searched for clinical studies, case series and case reports in which the usage of ketamine on cluster headache was described. The exemplary search strategy for MEDLINE is described in Table 1.
Table 1.
Search strategy for MEDLINE
| ((ketamine[MeSH Terms]) OR (ketamine)) AND ((cluster headache) OR (cluster headache[MeSH Terms]) OR (Trigeminal Autonomic Cephalalgias[MeSH Terms])) |
Publications of case reports, case series, retrospective analyses as well as uncontrolled and controlled studies were included. Proceedings, systematic reviews and meta-analyses were excluded as were publications which did not provide original data. The reference lists of systematic reviews were manually inspected to identify further relevant publications.
Our Own Case Series
Since 2019, patients suffering from refractory cluster headaches have been treated "off-label" with ketamine at the interdisciplinary pain clinic at the Medical University Graz. If conventional treatment options have been exhausted with unsatisfactory results, patients are offered treatment with S-ketamine. We present a case series of patients treated with S-ketamine for cluster headache, which were followed up to assess treatment success and effect on quality of life.
Patients diagnosed with cluster headache and confirmation of diagnosis by at least two different pain physicians were included in this study. They were treated with S-ketamine infusions in an outpatient clinical setting at the interdisciplinary pain clinic at the Medical University of Graz from 2020 to 2023. Participants were informed about the "off-label" nature of this therapy and about the fact that, apart from a few studies or case reports and good clinical experience, there are no available data proving the benefits of this therapy. If patients agreed to this therapy, they received 0.25 mg*kg−1 S-ketamine intravenously over a 1-h period.
Pulse oximetry, ECG and interval non-invasive blood pressure measurement were applied to maintain patient safety. Patients were observed for 1 h after the intervention if they had no adverse events. The decision as to whether one or more S-ketamine infusions should be administered was made by both the patients and the practitioners on a case-by-case basis: patients with full success and patients not responding at all were given a single infusion; infusion was repeated for patients experiencing some degree of alleviation.
Patients treated with S-ketamine were asked about the perceived success of the therapy and possible side effects using five statements.
The treatment has a positive influence on the quality of life.
I would repeat the treatment.
The treatment was satisfactory.
The treatment was superior to occipital blockade.
The side effects exceeded the positive effect.
Answers were given on a 6-point Likert scale ranging from "absolutely agree" (6 points) to "absolutely disagree" (1 point).
Written consent was obtained from all patients for using their data for scientific evaluation. The institutional review board of the Medical University of Graz approved the study protocol (Ethics committee no. 35–146 ex 22/23). Preparation of the manuscript adhered to the PRISMA and the CARE guidelines.
Results
Systematic Review
The last search was carried out in March 2024. The initial search resulted in 252 hits. After removal of duplicates, two independent reviewers screened the literature. In the case of diverging assessment, a third reviewer was consulted.
Five publications could be isolated that investigated the effect of ketamine on cluster headache. One publication on the use of ketamine in patients with refractory headaches included two cases with cluster headache; however, as no specific data were given for these two patients, we excluded this publication [30]. Therefore, four publications remained for further analysis [31–34]. The study flow chart is displayed in Fig. 1. The study characteristics are summarized in Table 2.
Fig. 1.
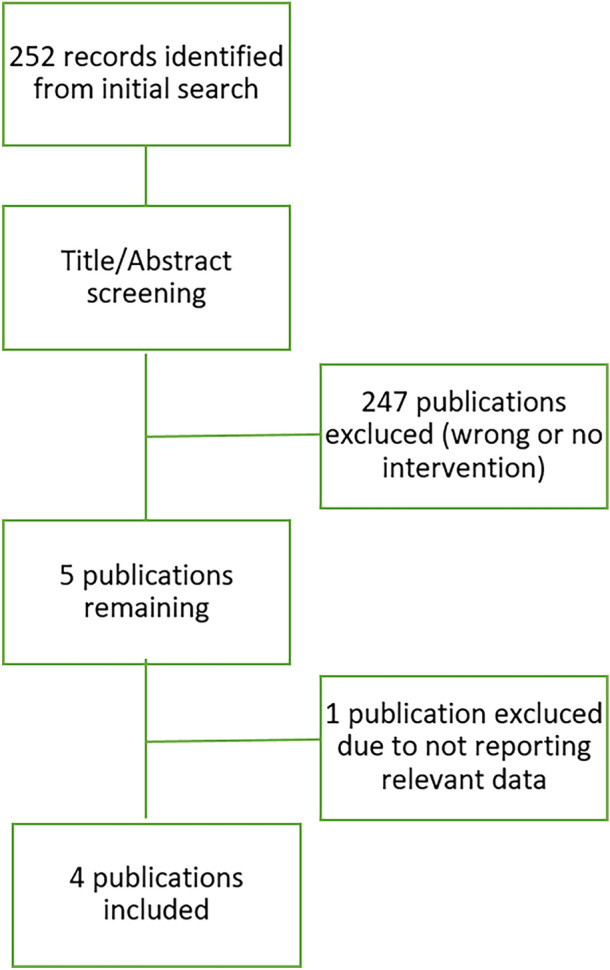
Study flow chart
Table 2.
Characteristics of the studies included in the systematic review. Abbreviations: cluster headache (CH), chronic cluster headache (cCH), episodic cluster headache (eCH)
| Study | Type | Participants | Endpoints | Intervention | Results | Side effects |
|---|---|---|---|---|---|---|
| Granata [31] | Single center observational study | 29 patients (13 cCH, 16 eCH) | Rate of complete pain free patients |
0.5 mg*kg−1 ketamine iv every 2 weeks - 1 to 4 repetitions |
54% of cCH patients were pain free within 2 weeks after the infusion, 100% of eCH patients | Mild psychomimetic side effects with a duration of seconds to minutes |
| Moisette [32] | Single center case series | 2 patients with cCH | Pain relief | 0.5 mg*kg−1 ketamine iv, single infusion plus 3000 mg magnesium | 1 patient was completely pain free, 1 had a 50% reduction of pain, both lasting 6 weeks | No side effects |
| Moisette [33] | Two center case series | 17 patients with cCH | Number of daily attacks | 0.5 mg*kg−1 ketamine iv, single infusion plus 3000 mg magnesium | Significant reduction of daily attacks (-3.1 per day), responder rate 76% | Transient or mild side effects in 41% |
| Petersen [34] | Single center open label pilot study | 23 cCH patients with more than 2 CH attacks per week | 50% reduction in pain intensity after 15 min |
15 mg of intranasal ketamine every 6 min maximum of 75 mg (5 doses) |
Reduction in pain intensity of 1.1 NRS (15%) (95% CI − 0.6 to 2.7, p = 0.188) after 15 min | No serious adverse events |
All included publications were case series. In total, 68 patients were reported to be treated with ketamine for cluster headache. No controlled studies are available yet.
Granata et al. 2016
In 2016, Granata et al. [31] published an observational study of 29 patients (2 women) with refractory cluster headache treated with ketamine. Sixteen patients had a diagnosis of episodic cluster headache and 13 had a diagnosis of chronic cluster headache. The patients were treated with intravenous R/S ketamine 0.5 mg*kg−1. Depending on the success of the therapy, the infusions were repeated up to four times. To prevent possible side effects, one third of the patients received 2.5 mg midazolam i.v. before ketamine was infused.
The treatment was well tolerated by all patients, and only mild or well-treatable side effects occurred. These included mild derealization, transient hypertension, bradycardic phases and mild to severe fatigue.
As a result of the therapy, 54% of patients with chronic cluster headache were free of attacks, with the effect lasting between 3 to 18 months. In all patients with episodic cluster headache, a termination of the episode was achieved.
Moisset et al. 2017
Moisset et al. [32] published a case report on two patients whom they treated with ketamine and magnesium. Patient 1 was 45 years old at the time of treatment. He had been suffering from cluster headache for 6 years, with the disease having taken on a chronic form for 1 year. In an outpatient setting, the patient received a single dose of ketamine 0.5 mg*kg−1 in an infusion over 2 h. In addition, he was infused with 3 g magnesium sulfate within 30 min. The patient did not experience any side effects during this therapy. The next day, the patient was in complete remission, which lasted for 6 weeks. After these 6 weeks, the patient again had 6–10 attacks daily, which were successfully treated by electrical stimulation of the greater occipital nerve.
Patient 2 was 28 years old. This patient also received ketamine and magnesium sulfate in an outpatient setting the same way as patient 1, which improved his symptoms. The daily attacks were reduced by 50%. The remaining attacks were treated with oxygen only. Since then, the patient has received an infusion of ketamine and magnesium sulfate every 8 weeks.
Moisset et al. 2020
In 2020, Moisset et al. [33] published data from a retrospective case series including 17 patients (14 men). All patients had been diagnosed with chronic cluster headache before, were > 18 years old and had suffered from the disease for at least 1 year. They were all treatment-refractory to at least three different preventive methods. All patients had an average of more than two attacks per day. Treatment with ketamine took place in a day clinic setting. The patients received a single dose of ketamine (0.5 mg*kg−1) as an infusion over 2 h. In addition, 3 g magnesium sulfate was infused over 30 min. The primary endpoint was the overall difference in the frequency of mean daily attacks between days 7 and 8 after the ketamine-magnesium infusion compared to the mean daily attacks for 2 weeks prior to the treatment. The main secondary endpoint was the proportion of patients with a ≥ 50% reduction in the frequency of daily acute episodes on days 7 and 8 post-infusion.
The number of daily attacks before the infusion was 4.3 ± 2.4. Seven and 8 days after a single infusion of the ketamine-magnesium combination, the number of daily attacks decreased clinically significantly (– 2.75 [95% CI: – 4.0 to – 1.75], P < 0.001) to 1.3 ± 1.0 attacks per day, corresponding to a reduction of 63.2% overall and 78.4% in responders. The analgesic effect started 1 to 6 (median = 3) days after infusion and lasted 2 to 68 (median = 4) weeks. Of these 17 patients, 13 (76.5%; 95% CI 56.3–96.6) had a ≥ 50% reduction in the frequency of daily episodes. In seven patients, the headaches disappeared completely (between 75 and 100% reduction), and in six patients the burden was reduced by at least 50%, measured by the average number of attacks per day. Of the four patients who did not respond to treatment, two showed no response within the first week and two experienced a reduction of 20.0–33.3% but failed to meet the study’s criteria for success.
None of the patients experienced hallucinations during the infusion, and although transient sedation was common (7/17 or 41.2%), none of the patients showed debilitating sedation 1 hour after the end of infusion. No bradycardia or high blood pressure was observed.
Petersen et al. 2021
In 2021, Petersen et al. [34] published an open study investigating the effect of intranasal ketamine on acute cluster headache attacks. For this purpose, 23 patients diagnosed with chronic cluster headache were selected. Participants received 15 mg of ketamine every 6 min for a maximum of five doses, resulting in a maximum dose of 75 mg. Ketamine was only administered for attacks with an intensity of at least 6 on an 11-point numerical pain rating scale, where 0 is no pain and 10 is the worst pain imaginable. Patients received at least three doses of ketamine 6 min apart, with possibility of two additional administrations. However, if a patient was pain free or almost pain free (defined as NRS < 4), no further ketamine was administered. All participants were offered oxygen and/or sumatriptan as rescue medication 15 min after the first ketamine administration. The main finding of this study is that ketamine may be effective for acute cluster headache. After 15 min, the mean reduction of pain intensity was 15%, after 30 min 69%. Furthermore, their data suggest that intranasal application at the dosage used is probably safe from severe side effects.
Our Own Case Series
Ten patients were included in this case series. Of these, eight identified as male and two as female. Both patients with episodic cluster headache (n = 6) and chronic cluster headache (n = 4) were included. The mean time since the first diagnosis was 12 ± 6.9 years. Patients’ characteristics are summarized in Table 3. Patients received an average of 4.1 ± 1.7 S-ketamine infusions with a mean frequency of 2.4 ± 1.3 infusions per week. The total number of infusions ranged from one to seven. The study results are summarized in Table 4.
Table 3.
Clinical data of the patients presented as absolute numbers (percentages) or mean ± standard deviation
| Number of patients | 10 |
| Number of males (percentage) | 8 (80%) |
| Number of episodic cluster headache (percentage) | 6 (60%) |
| Number of chronic cluster headache (percentage) | 4 (40%) |
| Age (years) | 42.2 ± 7.0 |
| Body weight (kg) | 85.3 ± 20.6 |
| Height (cm) | 179.9 ± 12.3 |
| Years since diagnosis | 12.0 ± 6.6 |
| Number of ketamine infusion per week | 2.4 ± 1.3 |
| Number of ketamine infusions in total | 4.1 ± 1.7 |
Table 4.
Mean values and standard deviation of the responses of all patients with chronic cluster headaches and episodic cluster headaches
| All patients | Episodic cluster headache | Chronic cluster headache | P value | |
|---|---|---|---|---|
| Treatment has a positive influence on quality of life | 4.9 ± 1.5 | 5.6 ± 0.5 | 3.8 ± 1.8 | 0.05561 |
| I would repeat the treatment | 4.7 ± 1.6 | 5.5 ± 0.8 | 3.5 ± 1.7 | 0.05036 |
| The treatment was satisfactory | 4.8 ± 1.9 | 5.8 ± 0.4 | 3.3 ± 2.3 | 0.04079 |
| The treatment was superior to occipital blockade | 4.8 ± 1.7 | 5.6 ± 0.7 | 3.3 ± 2.1 | 0.06539 |
| The side effects exceeded the positive effect | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.00000 |
All responses were reported on a Likert Scale from 1 (strongly disagree) to 6 (strongly agree)
All patients except two reported a complete pain-free interval. The duration however varied considerably, ranging from 1 to 26 months. Both non-responders suffered from chronic cluster headache, resulting in a success rate of 100% in the episodic cluster headache and in 50% in chronic cluster headache population. No side effects were reported.
Discussion
Systematic Review
The most remarkable result of our literature search is that there are currently no high-quality studies on ketamine for cluster headache. All references found are only case series.
In most cases, ketamine infusion resulted in a relevant alleviation of symptoms. However, as there were no control groups, placebo effects cannot be excluded. Likewise, an underreporting of failed treatment attempts must be presumed.
The comparability of the existing studies is limited because of different endpoints, types of application and additional medications used. Comparability within individual studies is also difficult because of the heterogeneous nature of preventive and acute therapy.
Only a few mild side effects occurred in all studies. This indicates that ketamine may be a safe medication for patients with cluster headache and therefore is encouraging for further studies and possible future clinical use. Further studies with a larger number of patients and a randomized and controlled design would be useful to investigate the effect of ketamine on cluster headache. Until then, individual case series can still contribute to a better understanding of this potential treatment option. In particular, the question of subjective changes in quality of life has also not yet been examined. The subjective relationship between effect and possible side effects has hardly been addressed in the literature to date.
Interpretation of Our Own Case Series
Our case series shows that a ketamine infusion is perceived positively by patients with cluster headaches. The treatment provided a high degree of satisfaction and the quality of life increased. The side effects profile was seen as favorable. These factors have not yet been reported in previous case series. Patients with episodic cluster headache largely felt an improvement in their quality of life after treatment with S-ketamine. It is therefore not surprising that they were satisfied with the therapy and would repeat it if given the need and opportunity.
Despite the small sample size, we could demonstrate that patients with chronic cluster headache were significantly less satisfied with the S-ketamine infusion. Two out of four patients felt no improvement in quality of life and would not repeat this therapy. This pattern is consistent with previous literature, in which patients with episodic and chronic cluster headache had different success rates [31]. Future studies should therefore consider further evaluating these findings.
Our survey also revealed that no patient in this case series experienced side effects of any kind. Even though the therapies in the systematic review were carried out with R/S ketamine and were very well tolerated, S-ketamine appears to be even more favorable in this regard.
We also asked our patients to compare the effect of the S-ketamine treatment with occipital blockade. Only one patient rated the occipital nerve block superior to S-ketamine treatment, with all other patients preferring S-ketamine infusion. If these findings are reproduced in larger trials, it may be indicative for clinical management.
Limitations
Our conclusions are limited as case series represent the lowest level of evidence. Although we were able to demonstrate a positive effect in our case series, more research is needed to recommend routine use of R/S ketamine or S-ketamine to treat refractory cluster headache and improve quality of life, as several questions remain unanswered. Is there an effect beyond placebo? What is the best dosing and application method? Are multiple infusions or treatments beneficial? Is S-ketamine superior to R/S-ketamine? To answer these questions, further high-quality studies are needed.
Especially in episodic cluster headaches, treatment success is difficult to monitor. This is particularly true for uncontrolled case reports. This also demonstrates the need for methodologically properly designed clinical studies.
Ongoing Studies and Outlook
A search in the clinicaltrials.gov database, the EU clinical trials register, the WHO international clinical trials platform and the German clinical trials register revealed only a single ongoing study in this field. As of March 2024, a placebo-controlled, double-blind study to investigate the effect of ketamine plus magnesium on patients with chronic cluster headache is currently recruiting patients at ten different sites across France. According to the published protocol, patients are planned to be treated with a single dose of ketamine 0.5 mg*kg−1 and 3 g of magnesium [35]. This will be the first prospectively designed randomized-controlled trial on this topic. However, researchers should be encouraged to plan and publish further well-designed clinical trials.
Conclusions
Cluster headache is associated with great suffering and serious restrictions on quality of life. Even though there are established treatment options, there are still patients with refractory pain. It is therefore of great interest to develop further treatment options.
As the systematic review of the current literature shows, there are encouraging results but not enough high-quality evidence to provide specific treatment recommendations. However, the results of the existing case series and case studies are extremely promising, and reported side effects were mild. The results of the case series presented in this article are largely consistent with those of existing publications. The results from positive case series should spark interest in further studies for the treatment of cluster headache, even though underreporting of failed attempts might bias current knowledge. Placebo-controlled double-blind studies would be ideal to confirm the efficacy of R/S-ketamine and/or S-ketamine on cluster headache. However, further case series could also contribute to treatment advances as they could be summarized in meta-analyses.
Acknowledgements
We thank the participants of the study. Kordula Lang-Illievich added the Department of Anaesthesia and Intensive Care Medicine, State Hospital Güssing, Güssing, Austria to her affiliations.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Johannes Neumann, Gudrun Rumpold-Seitlinger and Helmar Bornemann-Cimenti. The first draft of the manuscript was written by Johannes Neumann and Helmar Bornemann-Cimenti, and all authors commented on and contributed to the final manuscript. All authors read and approved the final manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
Helmar Bornemann-Cimenti is an Editorial Board member of Pain and Therapy. Helmar Bornemann-Cimenti was not involved in the selection of peer reviewers for the manuscript or any of the subsequent editorial decisions. All other authors declare that they have no competing interests.
Ethical Approval
The institutional review board of the Medical University of Graz approved the study protocol (ethics committee number 35–146 ex 22/23). Written consent was obtained from all patients for using their data for scientific evaluation.
Footnotes
Johannes Neumann and Helmar Bornemann-Cimenti have contributed equally to this work.
References
- 1.Hoffmann J, May A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 2018;17:75–83. doi: 10.1016/S1474-4422(17)30405-2. [DOI] [PubMed] [Google Scholar]
- 2.Torkamani M, Ernst L, Cheung LS, Lambru G, Matharu M, Jahanshahi M. The neuropsychology of cluster headache: cognition, mood, disability, and quality of life of patients with chronic and episodic cluster headache. Headache. 2015;55:287–300. doi: 10.1111/head.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luerding R, Henkel K, Gaul C, Dresler T, Lindwurm A, Paelecke-Habermann Y, et al. Aggressiveness in different presentations of cluster headache: results from a controlled multicentric study. Cephalalgia Int J Headache. 2012;32:528–536. doi: 10.1177/0333102412443336. [DOI] [PubMed] [Google Scholar]
- 4.Ji Lee M, Cho S-J, Wook Park J, Kyung Chu M, Moon H-S, Chung P-W, et al. Increased suicidality in patients with cluster headache. Cephalalgia Int J Headache. 2019;39:1249–1256. doi: 10.1177/0333102419845660. [DOI] [PubMed] [Google Scholar]
- 5.Waung MW, Taylor A, Qualmann KJ, Burish MJ. Family History of Cluster Headache: A Systematic Review. JAMA Neurol. 2020;77:887–896. doi: 10.1001/jamaneurol.2020.0682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suri H, Ailani J. Cluster Headache: A Review and Update in Treatment. Curr Neurol Neurosci Rep. 2021;21:31. doi: 10.1007/s11910-021-01114-1. [DOI] [PubMed] [Google Scholar]
- 7.Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V, et al. Aids to management of headache disorders in primary care (2nd edition): on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache. J Headache Pain. 2019;20:57. doi: 10.1186/s10194-018-0899-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.May A, Evers S, Goadsby PJ, Leone M, Manzoni GC, Pascual J, et al. European Academy of Neurology guidelines on the treatment of cluster headache. Eur J Neurol. 2023;30:2955–2979. doi: 10.1111/ene.15956. [DOI] [PubMed] [Google Scholar]
- 9.Lund NLT, Petersen AS, Fronczek R, Tfelt-Hansen J, Belin AC, Meisingset T, et al. Current treatment options for cluster headache: limitations and the unmet need for better and specific treatments-a consensus article. J Headache Pain. 2023;24:121. doi: 10.1186/s10194-023-01660-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sicuteri F, Geppetti P, Marabini S, Lembeck F. Pain relief by somatostatin in attacks of cluster headache. Pain. 1984;18:359–365. doi: 10.1016/0304-3959(84)90048-4. [DOI] [PubMed] [Google Scholar]
- 11.Harris AG. Somatostatin and somatostatin analogues: pharmacokinetics and pharmacodynamic effects. Gut. 1994;35:S1–4. doi: 10.1136/gut.35.3_Suppl.S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dahaba AA, Mueller G, Mattiassich G, Rumpold-Seitlinger G, Bornemann H, Rehak PH, et al. Effect of somatostatin analogue octreotide on pain relief after major abdominal surgery. Eur J Pain Lond Engl. 2009;13:861–864. doi: 10.1016/j.ejpain.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Brandt RB, Doesborg PGG, Haan J, Ferrari MD, Fronczek R. Pharmacotherapy for Cluster Headache. CNS Drugs. 2020;34:171–184. doi: 10.1007/s40263-019-00696-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ornello R, Lambru G, Caponnetto V, Frattale I, Di Felice C, Pistoia F, et al. Efficacy and safety of greater occipital nerve block for the treatment of cluster headache: a systematic review and meta-analysis. Expert Rev Neurother. 2020;20:1157–1167. doi: 10.1080/14737175.2020.1809379. [DOI] [PubMed] [Google Scholar]
- 15.Govare A, Leroux E. Licit and illicit drug use in cluster headache. Curr Pain Headache Rep. 2014;18:413. doi: 10.1007/s11916-014-0413-8. [DOI] [PubMed] [Google Scholar]
- 16.de Coo IF, Naber WC, Wilbrink LA, Haan J, Ferrari MD, Fronczek R. Increased use of illicit drugs in a Dutch cluster headache population. Cephalalgia Int J Headache. 2019;39:626–634. doi: 10.1177/0333102418804160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossi P, Allena M, Tassorelli C, Sances G, Di Lorenzo C, Faroni JV, et al. Illicit drug use in cluster headache patients and in the general population: a comparative cross-sectional survey. Cephalalgia Int J Headache. 2012;32:1031–1040. doi: 10.1177/0333102412458190. [DOI] [PubMed] [Google Scholar]
- 18.Sewell RA, Halpern JH, Pope HG. Response of cluster headache to psilocybin and LSD. Neurology. 2006;66:1920–1922. doi: 10.1212/01.wnl.0000219761.05466.43. [DOI] [PubMed] [Google Scholar]
- 19.University Hospital, Basel, Switzerland. Safety and Efficacy of Lysergic Acid Diethylamide (LSD) as Treatment for Cluster Headache: a Randomized, Double-blind, Placebo-controlled Phase II Study [Internet]. clinicaltrials.gov; 2022 May. Report No.: NCT03781128. Available from: https://clinicaltrials.gov/ct2/show/NCT03781128
- 20.Mulleners W. Efficacy and Safety of Minidosing Lysergic Acid Diethylamide (LSD) for Chronic Cluster Headache: a Randomized Placebo-controlled Study [Internet]. clinicaltrials.gov; 2022 Jul. Report No.: NCT05477459. Available from: https://clinicaltrials.gov/ct2/show/NCT05477459
- 21.Schindler EAD, Sewell RA, Gottschalk CH, Luddy C, Flynn LT, Zhu Y, et al. Exploratory investigation of a patient-informed low-dose psilocybin pulse regimen in the suppression of cluster headache: Results from a randomized, double-blind, placebo-controlled trial. Headache. 2022;62:1383–1394. doi: 10.1111/head.14420. [DOI] [PubMed] [Google Scholar]
- 22.Knudsen GM. Prophylactic Effects of Psilocybin on Chronic Cluster Headache: an Open-label Clinical Trial and Neuroimaging Study [Internet]. clinicaltrials.gov; 2022 Aug. Report No.: NCT04280055. Available from: https://clinicaltrials.gov/ct2/show/NCT04280055
- 23.De Gregorio D, Aguilar-Valles A, Preller KH, Heifets BD, Hibicke M, Mitchell J, et al. Hallucinogens in Mental Health: Preclinical and Clinical Studies on LSD, Psilocybin, MDMA, and Ketamine. J Neurosci. 2021;41:891–900. doi: 10.1523/JNEUROSCI.1659-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mion G, Villevieille T. Ketamine Pharmacology: An Update (Pharmacodynamics and Molecular Aspects, Recent Findings) CNS Neurosci Ther. 2013;19:370–380. doi: 10.1111/cns.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinner B, Graf BM. Ketamine. Handb Exp Pharmacol. 2008;313–33. [DOI] [PubMed]
- 26.Bornemann-Cimenti H, Wejbora M, Michaeli K, Edler A, Sandner-Kiesling A. The effects of minimal-dose versus low-dose S-ketamine on opioid consumption, hyperalgesia, and postoperative delirium: a triple-blinded, randomized, active- and placebo-controlled clinical trial. Minerva Anestesiol. 2016;82:1069–1076. [PubMed] [Google Scholar]
- 27.Bornemann-Cimenti H, Dorn C, Rumpold-Seitlinger G. Early Onset and Treatment of Phantom Limb Pain Following Surgical Amputation. Pain Med Malden Mass. 2017;18:2510–2512. doi: 10.1093/pm/pnx111. [DOI] [PubMed] [Google Scholar]
- 28.Rosenbaum SB, Gupta V, Patel P, Palacios JL. Ketamine [Internet]. StatPearls Internet. StatPearls Publishing; 2022 [cited 2023 Jan 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470357/
- 29.Mischel NA, Balon R. Esketamine. J Clin Psychopharmacol. 2021;41:233–235. doi: 10.1097/JCP.0000000000001395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwenk ES, Dayan AC, Rangavajjula A, Torjman MC, Hernandez MG, Lauritsen CG, et al. Ketamine for Refractory Headache: A Retrospective Analysis. Reg Anesth Pain Med. 2018;43:875–879. doi: 10.1097/AAP.0000000000000827. [DOI] [PubMed] [Google Scholar]
- 31.Granata L, Niebergall H, Langner R, Agosti R, Sakellaris L. Ketamin i. v. zur Behandlung von Clusterkopfschmerz. Schmerz. 2016;30:286–8. [DOI] [PubMed]
- 32.Moisset X, Clavelou P, Lauxerois M, Dallel R, Picard P. Ketamine Infusion Combined With Magnesium as a Therapy for Intractable Chronic Cluster Headache: Report of Two Cases. Headache J Head Face Pain. 2017;57:1261–1264. doi: 10.1111/head.13135. [DOI] [PubMed] [Google Scholar]
- 33.Moisset X, Giraud P, Meunier E, Condé S, Périé M, Picard P, et al. Ketamine-Magnesium for Refractory Chronic Cluster Headache: A Case Series. Headache J Head Face Pain. 2020;60:2537–2543. doi: 10.1111/head.14005. [DOI] [PubMed] [Google Scholar]
- 34.Petersen AS, Pedersen AS, Barloese MCJ, Holm P, Pedersen O, Jensen RH, et al. Intranasal ketamine for acute cluster headache attacks—Results from a proof-of-concept open-label trial. Headache J Head Face Pain. 2022;62:26–35. doi: 10.1111/head.14220. [DOI] [PubMed] [Google Scholar]
- 35.University Hospital, Clermont-Ferrand. Evaluation of the Efficacy of a Single Infusion of Ketamine Combined With Magnesium Sulfate to Treat Refractory Chronic Cluster Headache [Internet]. clinicaltrials.gov; 2023 Jun. Report No.: NCT04814381. Available from: https://clinicaltrials.gov/study/NCT04814381
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


