INTRODUCTION
The landscape of pediatric critical care has changed since the establishment of pediatric intensive care units (PICUs) in the 1950s. The number of children who become critically ill each year in the United States has been steadily increasing by approximately 3% each year.1 More than two-thirds of children admitted to the PICU have a previously diagnosed condition, and half have impaired or abnormal functioning at their baseline.2,3 Although PICU mortalities have decreased drastically to 2% to 3% in high-resource countries, rates of new morbidity and readmission have increased.2,3 This evolution has driven a paradigm shift in pediatric critical care from a focus on surviving pediatric critical illness to examining trajectories of recovery and promoting child and family functioning in the longer term.4
POST–INTENSIVE CARE SYNDROME IN PEDIATRICS
The persistence of PICU-acquired impairments across physical, cognitive, or mental health domains experienced by survivors of pediatric critical illness has been termed post-intensive care syndrome in pediatrics (PICS-p).5,6 Manning and colleagues7 created a conceptual model of PICS-p to depict this phenomenon and describe the impact on components unique to pediatrics, such as the impact on their continued development and family. PICS-p impairments are reported across domains of physical health (health status, mobility, activities of daily living, fatigue, and pain), cognition (attention, memory, executive functioning), emotional/mental health (anxiety, depression, acute- and posttraumatic stress, behavior), and social and family functioning (reintegration in the home, community, and school/work, family communication and cohesion).8–10
Fig. 1 is a version of the PICS-p framework, depicting the impact of critical illness on the child and their family, the types of impairments experienced, and modified with author consent to highlight the association between post-PICU impairments and hospital readmission, and how all these components are impacted by their social and political context.
Fig. 1.
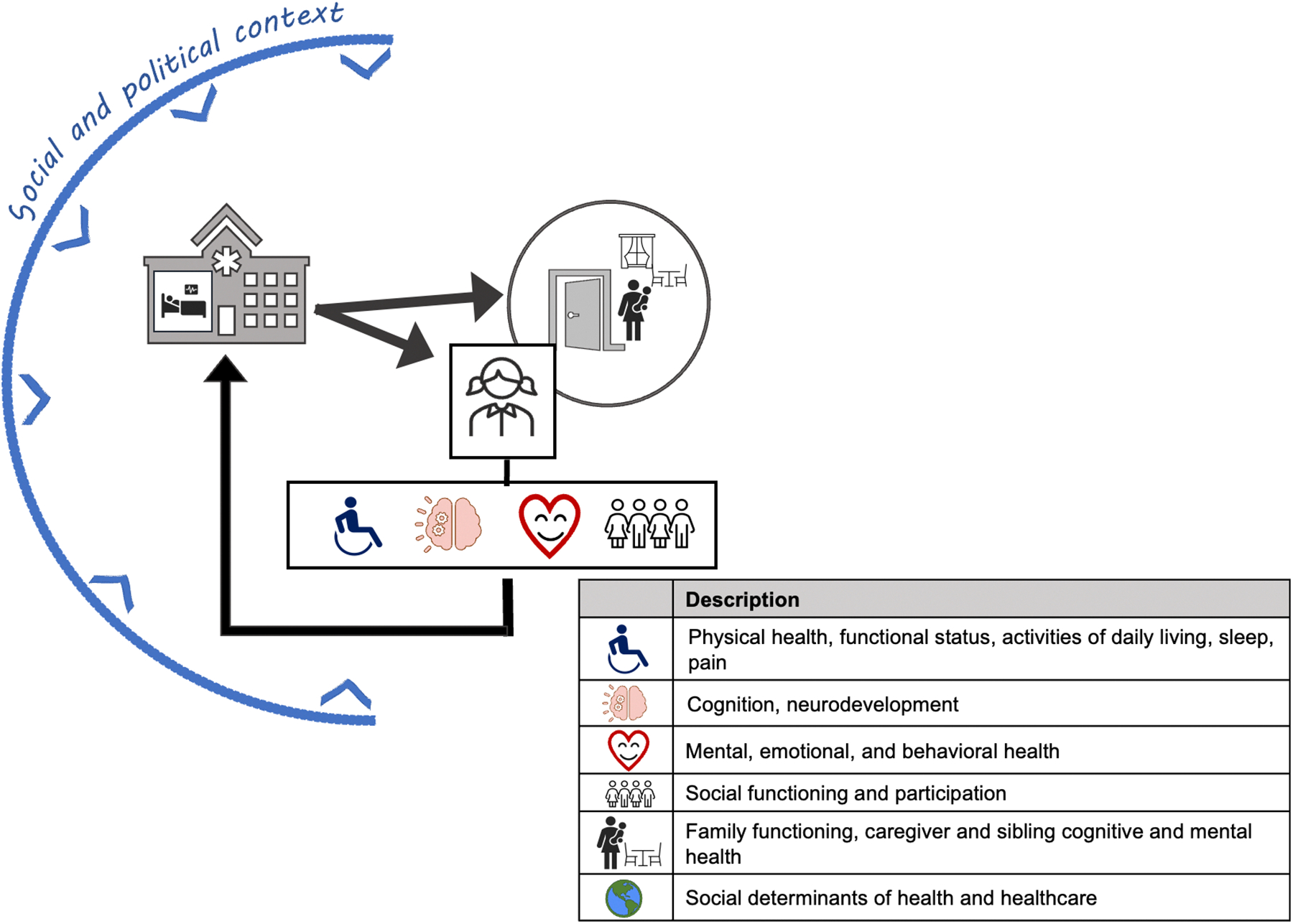
PICS-p.
Physical Functioning
The World Health Organization developed the International Classification of Functioning, Disability, and Health to provide a common framework to conceptualize functional health and disabilities.11 This framework considers functioning in 3 different ways: functional status and physical structures (eg, muscle strength); activities (eg, ability to complete tasks such as brushing teeth or transferring from bed to chair); and participation (eg, engagement in sets and sequences of meaningful life events, such as school field trips or family celebrations). Rates of impaired physical functioning range from 10% to 82% at PICU discharge, depending on how functioning was conceptualized and measured.12–17 When using the Pediatric Evaluation of Disability Inventory, a proxy/patient-reported outcome measure of children’s ability to perform activities across physical, social, and cognitive domains, to compare level of functioning pre-PICU, impairments were reported in 82% and 28% of children at PICU discharge and 6 months after, respectively. Using the Functional Status Scale, trajectories of recovery differ between survivors; for example, although approximately two-thirds of survivors report impairments persist for several months to years after discharge,16,18 in a prospective cohort study by Pinto and colleagues,6 morbidities and mortalities increased in the initial 3 years after discharge.
Cognitive Health
Cognitive dysfunction following critical illness in children includes difficulties with attention, memory, and executive function, increased cognitive fatigue, delayed neurodevelopment, and worsened academic performance.19,20 Reported prevalence of new cognitive dysfunction in children following critical illness ranges from 3% to 73%, depending on the specificity of the measure, timing of assessment, and cohort characteristics.21 Among children with sepsis and meningitis requiring critical care, up to 42% report cognitive impairment or neurodevelopmental delays following illness.22 After cardiac arrest, 47% of children requiring extracorporeal membrane oxygenation report persistent learning difficulties.23 Furthermore, there is emerging evidence cognitive impairments may persist or worsen over the first year.24
Emotional Health
Children receive a median of 11 stressful and painful procedures in a single PICU day.25 Unsurprisingly, 64% of children demonstrate the symptoms for acute stress disorder during their PICU admission.26 Emotional dysfunction after PICU admission can manifest as anxiety, depression, behavior difficulties, and posttraumatic stress disorder (PTSD).19,27–30 PTSD is the most common psychiatric diagnosis after PICU. Prevalence of PTSD among critically ill children varies from 13% to 32% within 12 months of discharge.31,32 Other post-PICU psychiatric comorbidities include hyperactivity, depression, sleep disturbance, cognitive fatigue, and conduct disorders.33–35
Social/Familial Health
Pediatric critical illness is a highly stressful experience for caregivers and siblings of the patient and can negatively impact their mental health and family cohesion.36–38 A third of caregivers report moderate to severe anxiety or moderate to severe depression after PICU.30 One study reported 10% of caregivers receive a new mental health diagnosis within 6 months of their child’s critical illness, 110% higher than projected.39 Critical illness also impacts child and family social networks, relationship functioning, and work or school attendance. One prospective cohort study reported 43% of children had missed 7 or more days of school and 14% had missed 30 or more days of school 3 months after PICU.40
Risk Factors and Social Determinants of Health
Individual risk factors for PICS-p are outlined in Table 1. Although an in-depth review of the PICU care equity and related health disparities is out of the scope of this review, it is necessary to briefly discuss the impact of the social and political factors that influence health and health care when discussing trajectories of functional recovery.41–43 Access to care is the opportunity to have health needs fulfilled through timely and appropriate care.44 Access to care opportunities results from the interaction between an individual’s abilities/resources (eg, mobility, transportation) and the health care system characteristics (eg, geographic location, physical layout), both of which are influenced by social and political policies and norms. Unfortunately, there is an abundance of literature demonstrating access to care is inequitable, that is, access differences that are unjust, for children with disabilities, children of color, and children with lower-socioeconomic status in both the hospital and the community.45–47 The Conceptual Model of Disability and Disparities demonstrates the impact of disability on access to care and how access to care experiences influence the abling/disabling process.48 Thus, given the complexity and vulnerability of the PICU population, the authors posit that it is crucial to include examination of and support for access to care for all services developed and implemented to assure equitable care and recovery for all children.
Table 1.
Risk factors for post–intensive care syndrome in pediatrics
| Risk Factor | Description | Reference |
|---|---|---|
| Caregiver language and ethnicity | Non-English speaking is associated with worse outcomes, for example, increased mortality | 59,98 |
| Socioeconomic status | Lower income, education, and geographic location increase risk for PICU admission and poor PICU outcome | 41 |
| Child’s baseline status | Prior chronic condition | 23,47 |
| Admitting diagnosis | Neurologic conditions, sepsis, multiorgan dysfunction | 48 |
| Invasive procedures | Invasive mechanical ventilation, receipt of extracorporeal membrane oxygenation | 49 |
| Sedation requirements | Length of deep sedation | 27,58 |
MANAGEMENT OF POST–INTENSIVE CARE SYNDROME IN PEDIATRICS
Given the breadth of the impact of PICS-p, there are several approaches emerging to optimize the functioning of PICU survivors. These approaches include prevention, identification, and intervention during and after the PICU and may be targeted at the level of the individual/family or health care system. Fig. 2 illustrates the existing approaches across the care continuum, and components are summarized in later discussion.
Fig. 2.
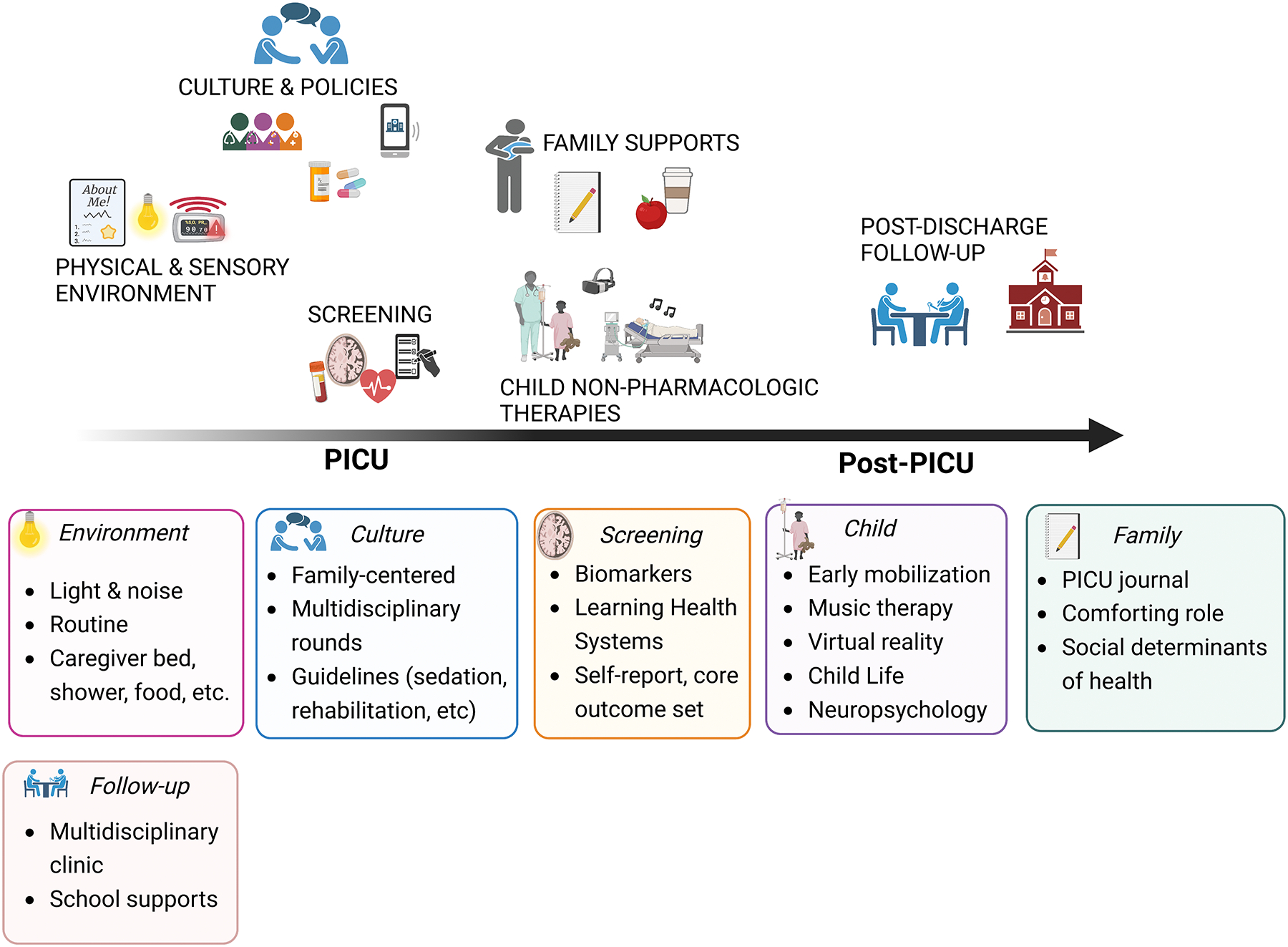
Overview of system- and individual-level approaches to remediate PICS-p.
Prognostication and Screening
Identifying those at risk for PICS-p presents several challenges. First, functional impairments can be difficult to detect in very young children until they are older or after resuming home and family life, emphasizing the need for repeated screening, including after hospital discharge.14 Second, there is currently no validated measure to assess PICS-p. Existing measures of functional outcomes tend to be validated only for a specific diagnosis or narrow age group and may not detect all of the deficiencies associated with PICS-p.27,49 Given the importance of early identification to guide resource distribution and care coordination, multimodal approaches to screening and prognostication may be necessary, such as sing both caregiver/patient-reported outcome measures and clinical data, including serum, physiologic, and imaging biomarker data. For example, serum-derived vascular endothelial growth factor 1 day after PICU admission was associated with decreased functional status at hospital discharge for 44 children with acquired brain injury; heart rate variability metrics within the first 24 hours of admission predicted organ dysfunction and mortality in a cohort of more than 7000 critically ill children, and decreased connectivity strength in paralimbic tracks identified via resting state functional MRI and diffusion tensor imaging was associated with neurocognitive impairment among 12 children with cardiac arrest.50–52
Pediatric Intensive Care Unit–Based Care
System level
Environmental modifications, such as limiting noise from alarms and shift change, keeping the child on a familiar routine, and decorating the room with familiar items, are suggested to prevent some of the psychological sequalae of critical care.53–57 Interventions to optimize PICU culture include approaches to care delivery, such as providing family-centered care, the equity in care allocation and care quality, availability of translators, and educational materials and resources in non-English languages.57–63 Policies and training to promote family-centered care include protocols to improve communication (Table 2), incorporating caregivers in goal setting and care planning, provision of resources that support caregiver presence, for example, a place to sleep and nutritious food, and remote/telehealth options to engage caregivers in care planning when they cannot be at the PICU bedside.58,64–66 Implementation of multidisciplinary rounds within the PICU facilitates referral of necessary services and care coordination (Fig. 3). Last, adherence to pediatric critical care guidelines for pain and sedation management, mechanical ventilation, and delirium prevention may prevent development of PICS-p.63,67–70
Table 2.
Improving communication during pediatric critical care through the acronym HICCC
| Component | Description |
|---|---|
| Honest | Straightforward, upfront, and candid |
| Inclusive | Listening to and implementing caregiver feedback and concerns |
| Compassionate | Caring about the patient and family |
| Comprehensive & Clear | Concise descriptions and rationales |
| Coordinated | Care team roles are defined and expectations listed |
Fig. 3.
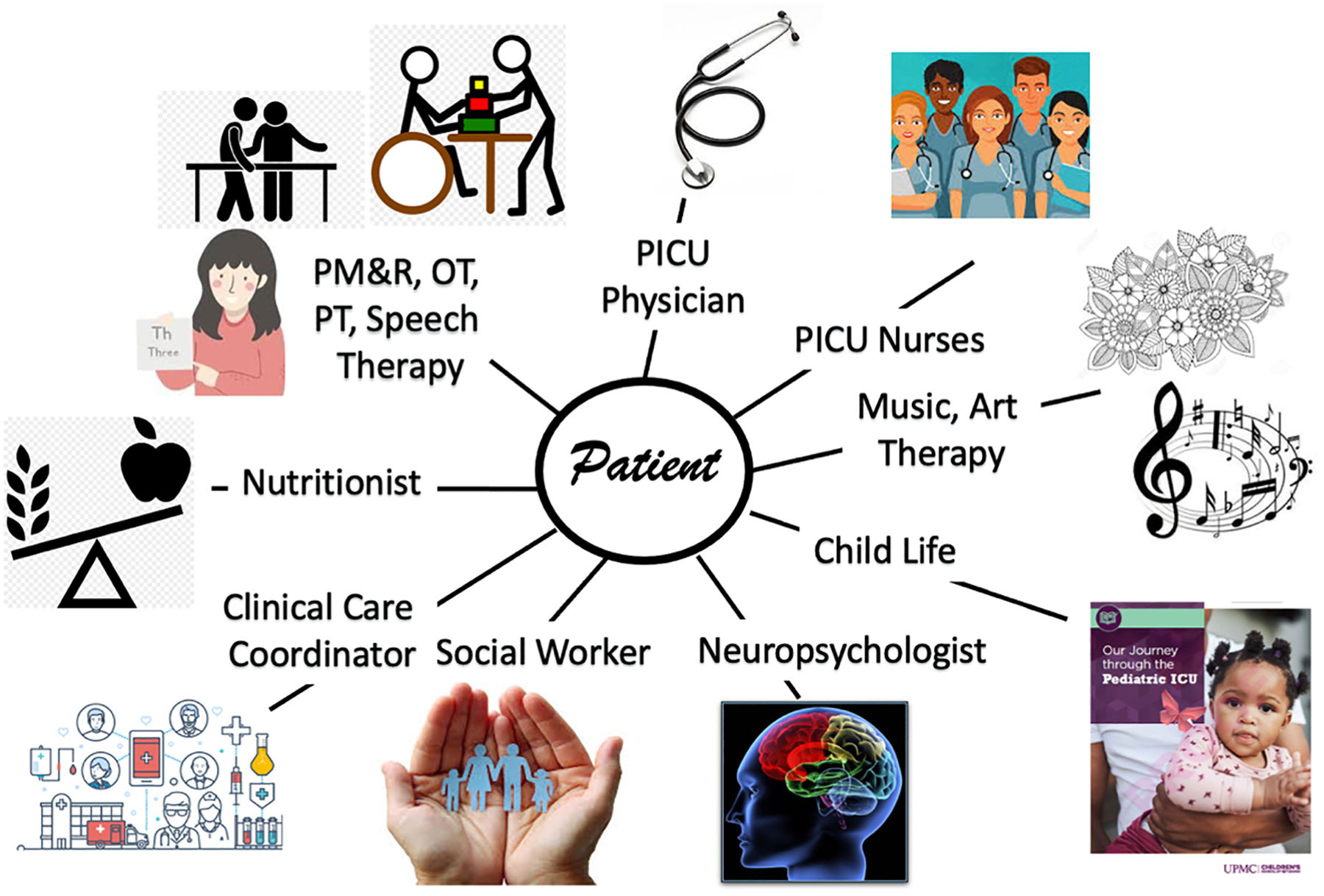
Disciplines involved in multidisciplinary PICU care. OT, occupational therapy; PM&R, physical medicine and rehabilitation; PT, physical therapy.
Individual level
Early mobility has been a primary focus of rehabilitation therapies of PICU-based interventions to prevent impairment and promote recovery.71,72 Although feasibility, acceptability, and safety of early mobilization and rehabilitation therapies in the PICU has been demonstrated, there is a lack of evidence on efficacy.73–77 However, among adults, early mobility resulted in improved outcomes, such as increased strength and shorter durations of mechanical ventilation and lengths of intensive care unit (ICU) stay.78 Furthermore, caregivers report less stress 6 months after discharge if their child received PICU-based rehabilitation therapies, compared with those who did not.79 Thus, the 2022 Society of Critical Care Medicine Clinical Practice Guidelines for critically ill pediatric patients recommend incorporation of a standardized early mobility protocol outlining criteria to participate in early mobility, the contraindications, and mobility activities and goals.70
Nonpharmacologic approaches to supporting children’s comfort and mental health, such as providing music or music therapy, virtual reality, and comfort-care holding, are emerging as potentially effective alternatives to decreasing stress and pain without the potentially deleterious effects associated with analgesics and sedatives.80–86 These studies primarily demonstrate feasibility, acceptability, and safety. However, there is promising results among critically ill adults to encourage continued exploration of these approaches. For example, listening to music during mechanical ventilation resulted in decreased self-reported anxiety and less medication use, compared with usual care in a randomized control trial of 373 patients across 12 different ICUs.87 Additional interventions to support both child and caregiver include caregivers reading to their child and PICU diaries.88,89 The latter involves working with families to create a written record detailing daily events about their child’s condition and care during the PICU hospitalization in their own words. These diaries may address gaps in a child’s memory regarding their critical illness hospitalization and provide clarity and context about their experience. Among adults, ICU diaries have been associated with a reduction in the incidence of PTSD, anxiety, and depression, as well as improve health-related quality of life.90 Last, but possibly most importantly for addressing PICS-p, are approaches of bundled care. The ABCDEF Bundle (Fig. 4), also known as “A2F Care” and “PICU Liberation,” aims to minimize pain and sedation, decrease unnecessarily prolonged mechanical ventilation, prevent immobility, and facilitate family engagement.91
Fig. 4.
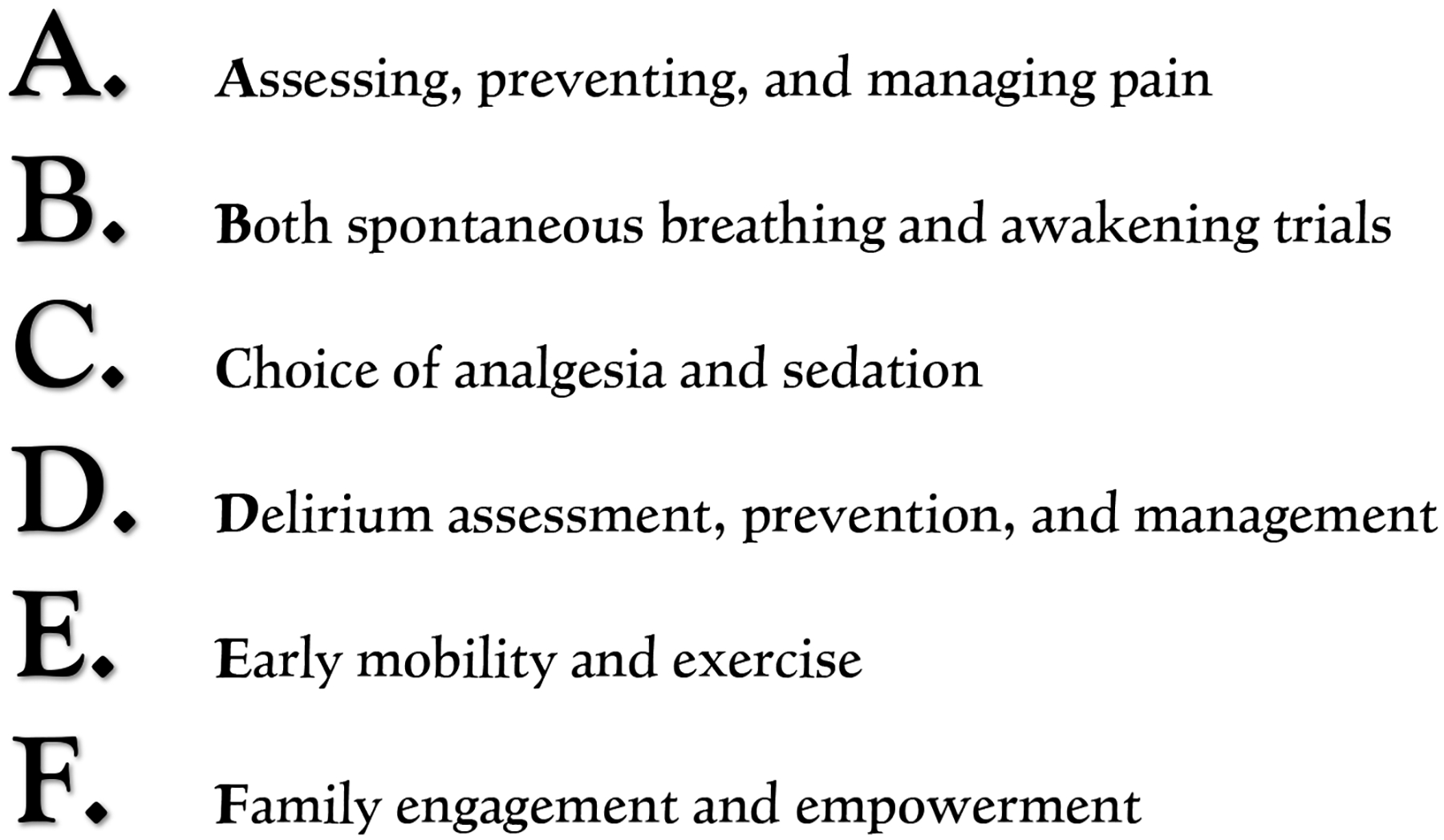
Components of the ABCDEF Bundle for addressing PICS-p.
Post–Pediatric Intensive Care Unit Follow-Up
The creation of post-PICU follow-up clinics is a postacute approach to optimize recovery through recognition of PICs-p, provision of referrals for health care and school accommodations requests, care coordination, and connection with psychosocial support. There is significant variability in the design of post-ICU clinics; however, families report high satisfaction and value from attending.92–94 Common components of these clinics are multidisciplinary engagement (eg, therapists, social workers, intensivists, physiatrists, neuropsychologists) and screening for child and family functional outcomes.8,27 Developing such clinics can be complicated and time consuming, given the heterogeneity of the PICU population diagnoses, conditions, and ages coupled with the resources necessary to support multidisciplinary care.
To guide the successful development of post-PICU follow-up clinics, Butcher and colleagues95 provide the following “5 S’s” to consider when implementing a post-ICU clinic:
Space: Affordability; availability; accessibility; maximum occupancy
Staff: Disciplines; scheduling; compensation
Stuff: Funding; technology; equipment
Screening: Eligibility criteria; outcomes to assess; process to identify; timing of follow-up
Selling it: Awareness; advocacy; assuring attendance
Addressing these considerations inevitably depends on the resources and expertise available at individual institutions. Partnering between PICU physicians and established follow-up clinics provides a potentially universal solution to space and equipment. Particularly multidisciplinary, specialty clinics, such as Complex Care or Pediatric Rehabilitation Medicine clinics, can provide access to many of the support services patients require after ICU admission. Determining which patients will be offered follow-up visits may also depend on the number of staff available to participate in post-ICU clinics. Who should be involved and mode of follow-up (eg, in-person, virtual, asynchronous) require careful consideration. Beginning with a focused patient population and expanding gradually as additional funding and resources are identified may facilitate the feasibility of starting and sustaining this care. Incorporating a diverse set of stakeholders, both end users and providers, in clinic design and optimizations can optimize care, facilitate efforts to promote awareness of PICS-p, advocate for clinic attendance, and promote retention across longitudinal care.92,96,97
THE ROLE OF PEDIATRIC REHABILITATION MEDICINE
Pediatric physiatrists are well poised to champion this space of optimizing recovery for survivors of pediatric critical illness, given their unique focus on child functioning versus a specific organ system. Pediatric rehabilitation medicine spans the health care continuum from the PICU to postacute and ambulatory care, while consistently focusing on optimizing function through effective collaboration and communication with other health care professionals. Pediatric physiatrists are ideally equipped to identify and manage weakness and functional limitations in the PICU and can also help educate families about PICS-p and assist in coordination of care for patients who are able to transition home. For those pediatric patients who have more significant functional deficits, they can identify those who would benefit from transfer to a pediatric acute inpatient rehabilitation unit before discharge home.
FUTURE DIRECTIONS
There has been a rapid evolution of research aimed at characterizing and facilitating functional recovery for children and families after pediatric critical illness; however, significant hurdles still lay ahead. Resources and tools for PICS-p education and identification will be necessary to maintain momentum for improving functional recovery of survivors of pediatric critical illness.96 In addition, evidence on PICS-p intervention efficacy and guidelines for equitable implementation are necessary to drive development of health policies for clinical implementation. Last, children and families admitted into the PICU reported a higher prevalence of adverse social determinants of health and prior adverse childhood experiences compared with the general population.94,95,97 Taken together with the high proportion of children from historically marginalized communities within the PICU population, additional research on best practices to screen for and intervene on adverse social determinants of health and assure equitable opportunity to access care is crucial to assure every child has the opportunity to achieve their optimal health.
SUMMARY
Pediatric critical illness can have a long-lasting, negative impact on children and families across a variety of different functional domains. Preventing, identifying, and treating PICS-p requires coordinated care among a multidisciplinary team of health care professions and intentional development of guidelines and policies that assure equitable implementation of evidence-based care during and after the PICU admission. Clinicians and researchers should evaluate their local needs, barriers, and facilitators for addressing PICS-p and collaborate with lived experience experts to design the longitudinal support necessary for recovery in the longer term.
KEY POINTS.
Post–intensive care syndrome in pediatrics (PICS-p) is composed of new or worsening impairments in physical, cognitive, social, and mental health for the child and their family.
Addressing PICS-p requires a multilevel and longitudinal approach.
An interdisciplinary team, including intensivists, rehabilitation specialists, and social workers, is essential for the prevention and management of PICS-p.
Monitoring outcomes via validated measures of core outcomes and starting with focused patient populations can facilitate the implementation and evaluation of approaches to address PICS-p.
CLINICS CARE POINTS.
Children, their caregivers, and their siblings may experience new or worsening impairments after pediatric intensive care unit discharge, known as post–intensive care syndrome in pediatrics. Post–intensive care syndrome in pediatrics education and awareness for families, health care providers (eg, primary care physicians), and educators are necessary to improve identification and treatment.
Within the pediatric intensive care unit, there are several promising interventions addressing post–intensive care syndrome in pediatrics at an individual and a system level. Protocolizing a bundled approach may be best, given the wide range of potential impairments.
Follow-up assessment and care are necessary, but resource intensive. There is need for careful consideration of who should be a part of follow-up care, mode of delivery, and the level of specificity desired for outcome data (eg, general vs specific) to drive measure selection, although outcomes should always align with family priorities.
Efforts to promote survivorship should incorporate addressing social determinants of health and equitable access.
ACKNOWLEDGMENTS
The authors acknowledge Ericka Fink, MD, MS and Katie Hayden, MSN for their expertise, time, and guidance during this review.
DISCLOSURE
This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K23HD106011 (J.M. Jarvis). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have nothing else to disclose.
REFERENCES
- 1.Heneghan JA, Rogerson C, Goodman DM, et al. Epidemiology of Pediatric Critical Care Admissions in 43 United States Children’s Hospitals, 2014–2019. Pediatr Crit Care Med 2022;23(7):484–92. [DOI] [PubMed] [Google Scholar]
- 2.Namachivayam P, Shann F, Shekerdemian L, et al. Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med 2010;11(5):549–55. [DOI] [PubMed] [Google Scholar]
- 3.Pollack MM, Holubkov R, Funai T, et al. Pediatric Intensive Care Outcomes: Development of New Morbidities During Pediatric Critical Care. Pediatr Crit Care Med 2014;15(9):821–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heneghan J, Pollack MM. Morbidity: Changing the outcome paradigm for pediatric critical care. Pediatr Clin North Am 2017;64(5):1147–65. Morbidity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: A systematic review. World J Crit Care Med 2017;6(2):124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinto NP, Rhinesmith EW, Kim TY, et al. Long-term function after pediatric critical illness: Results from the Survivor Outcomes study. Pediatr Crit Care Med 2017; 18(3):122–30. [DOI] [PubMed] [Google Scholar]
- 7.Manning JC, Pinto NP, Rennick JE, et al. Conceptualizing Post Intensive Care Syndrome in Children—The PICS-p Framework. Pediatr Crit Care Med 2018; 19(4):298–300. [DOI] [PubMed] [Google Scholar]
- 8.Fink EL, Maddux AB, Pinto N, et al. A Core Outcome Set for Pediatric Critical Care. Crit Care Med 2020;48(12):1819–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choong K. PICU-acquired complications: the new marker of the quality of care. ICU Manag 2019;19(2):84–8. [Google Scholar]
- 10.Fayed BN, Cameron S, Fraser D, et al. Priority outcomes in critically ill children. A patient and parent perspective 2020;29(5):94–103. [DOI] [PubMed] [Google Scholar]
- 11.The World Health Organization. International classification of functioning, disability, and health: children & youth version. ICF-CY; 2007. 10.1017/CBO9781107415324.004. Published online. [DOI] [Google Scholar]
- 12.Choong K, Fraser D, Al-Harbi S, et al. Functional Recovery in Critically Ill Children, the “WeeCover” Multicenter Study. Pediatr Crit Care Med 2018;19(2): 145–54. [DOI] [PubMed] [Google Scholar]
- 13.Ong C, Lee JH, Leow MKS, et al. Functional outcomes and physical impairments in pediatric critical care survivors: A scoping review. Pediatr Crit Care Med 2016; 17(5):e247–59. [DOI] [PubMed] [Google Scholar]
- 14.Khetani MA, Albrecht E, Jarvis JM, et al. Determinants of change in home participation among critically ill children. Dev Med Child Neurol 2018;60(8):793–800. [DOI] [PubMed] [Google Scholar]
- 15.Jarvis JM, Fayed N, Fink EL, et al. Caregiver dissatisfaction with their child’s participation in home activities after pediatric critical illness. BMC Pediatr 2020; 20(1):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jarvis J, Houtrow A, Treble-Barna A, et al. #442: Post pediatric neurocritical care recovery: A whole child and family perspective. Pediatr Crit Care Med 2021; 22(Supplement 1 3S):13. [Google Scholar]
- 17.Bossen D, de Boer RM, Knoester H, et al. Physical Functioning After Admission to the PICU: A Scoping Review. Crit Care Explor 2021;3(6):e0462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carlton EF, Pinto N, Smith M, et al. Overall health following pediatric critical illness: A scoping review of instruments and methodology. Pediatr Crit Care Med 2021;22(12):1061–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Als LC, Tennant A, Nadel S, et al. Persistence of neuropsychological deficits following pediatric critical illness. Crit Care Med 2015;43(8 PG-312–315):e312–5. [DOI] [PubMed] [Google Scholar]
- 20.Als LC, Nadel S, Cooper M, et al. Neuropsychologic Function Three to Six Months Following Admission to the PICU With Meningoencephalitis, Sepsis, and Other Disorders. Crit Care Med 2013;41(4):1094–103. [DOI] [PubMed] [Google Scholar]
- 21.Chaiyakulsil C . ROC and, 2021. undefined. Pediatric postintensive care syndrome: high burden and a gap in evaluation tools for limited-resource settings. ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8426094/. Accessed November 20, 2022. [DOI] [PMC free article] [PubMed]
- 22.Kachmar AG, Irving SY, Connolly CA, et al. A systematic review of risk factors associated with cognitive impairment after pediatric critical illness. Pediatr Crit Care Med 2018;19(3):e164–71. [DOI] [PubMed] [Google Scholar]
- 23.Elias MD, Achuff BJ, Ittenbach RF, et al. Long-term outcomes of pediatric cardiac patients supported by extracorporeal membrane oxygenation. Pediatr Crit Care Med 2017;18(8):787–94. [DOI] [PubMed] [Google Scholar]
- 24.Hall TA, Greene RK, Lee JB, et al. Post-Intensive Care Syndrome in a Cohort of School-Aged Children and Adolescent ICU Survivors: The Importance of Follow-up in the Acute Recovery Phase. J Pediatr Intensive Care 2022. 10.1055/s-0042-1747935. [DOI] [Google Scholar]
- 25.Baarslag MA, Jhingoer S, Ista E, et al. How often do we perform painful and stressful procedures in the paediatric intensive care unit? A prospective observational study. Aust Crit Care 2019;32(1):4–10. [DOI] [PubMed] [Google Scholar]
- 26.Nelson LP, Lachman SE, Goodman K, et al. Admission Psychosocial Characteristics of Critically Ill Children and Acute Stress. Pediatr Crit Care Med 2020;22(2): 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinto NP, Maddux AB, Dervan LA, et al. A Core Outcome Measurement Set for Pediatric Critical Care. Pediatr Crit Care Med 2022;23(11):893–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manning JC, Hemingway P, Redsell SA. Long-term psychosocial impact reported by childhood critical illness survivors: A systematic review. Nurs Crit Care 2014; 19(3):145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colville G, Kerry S, Pierce C. Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med 2008;177(9):976–82. [DOI] [PubMed] [Google Scholar]
- 30.Rodríguez-Rey R, Alonso-Tapia J, Colville G. Prediction of parental posttraumatic stress, anxiety and depression after a child’s critical hospitalization. J Crit Care 2018;45:149–55. [DOI] [PubMed] [Google Scholar]
- 31.Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: A review. Pediatr Crit Care Med 2012;13(3):338–47. [DOI] [PubMed] [Google Scholar]
- 32.Nelson LP, Lachman SE, Li SW, et al. The effects of family functioning on the development of posttraumatic stress in children and their parents following admission to the PICU. Pediatr Crit Care Med 2019;20(4):e208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kudchadkar SR, Aljohani OA, Punjabi NM. Sleep of critically ill children in the pediatric intensive care unit: A systematic review. Sleep Med Rev 2014;18(2): 103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Colville GA, Pierce CM, Peters MJ. Self-Reported Fatigue in Children Following Intensive Care Treatment. Pediatr Crit Care Med 2019;20(2):e98–101. [DOI] [PubMed] [Google Scholar]
- 35.Rennick JE, Dougherty G, Chambers C, et al. Children’s psychological and behavioral responses following pediatric intensive care unit hospitalization: the caring intensively study. BMC Pediatr 2014;14(1):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abela KM, Wardell D, Rozmus C, et al. Impact of paediatric critical illness and injury on families: An updated systematic review. J Pediatr Nurs 2020;51:21–31. [DOI] [PubMed] [Google Scholar]
- 37.Shudy M, de Almeida ML, Ly S, et al. Impact of pediatric critical illness and injury on families: A systematic literature review. Pediatrics 2006;118(Supplement_3): S203–18. [DOI] [PubMed] [Google Scholar]
- 38.Colville G, Darkins J, Hesketh J, et al. The impact on parents of a child’s admission to intensive care: Integration of qualitative findings from a cross-sectional study. Intensive Crit Care Nurs 2009;25(2):72–9. [DOI] [PubMed] [Google Scholar]
- 39.Logan GE, Sahrmann JM, Gu H, et al. Parental mental health care after their child’s pediatric intensive care hospitalization. Pediatr Crit Care Med 2020; 21(11):941–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kastner K, Pinto N, Msall ME, et al. PICU follow-up: The impact of missed school in a cohort of children following PICU admission. Crit Care Explor 2019;1(8):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Modification of social determinants of health by critical illness and consequences of that modification for recovery: an international qualitative study. BMJ Open 2022; 12(9):e060454. Available at: https://bmjopen.bmj.com/content/12/9/e060454.abstract. Accessed November 20, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zambrano LD, Ly KN, Link-Gelles R, et al. Investigating Health Disparities Associated With Multisystem Inflammatory Syndrome in Children After SARS-CoV-2 Infection. Pediatr Infect Dis J 2022;41(11):891–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zurca AD, Suttle ML, October TW. An Antiracism Approach to Conducting, Reporting, and Evaluating Pediatric Critical Care Research. Pediatr Crit Care Med 2022;23(2):129–32. [DOI] [PubMed] [Google Scholar]
- 44.Levesque J, Harris M, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013;12(18):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitchell H, Reddy A, Perry M, et al. Racial, ethnic, and socioeconomic disparities in paediatric critical care in the USA. Lancet Child Adolesc Health 2021;5: 739–50. Available at: https://pubmed.ncbi.nlm.nih.gov/34370979/. [DOI] [PubMed] [Google Scholar]
- 46.Kuo DZ, Goudie A, Cohen E, et al. Inequities in health care needs for children with medical complexity. Health Aff 2014;33(12):2190–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McGowan SK, Sarigiannis KA, Fox SC, et al. Racial Disparities in ICU Outcomes: A Systematic Review. Crit Care Med 2022;50(1):1–20. [DOI] [PubMed] [Google Scholar]
- 48.Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil 2015;37(7):632–41. [DOI] [PubMed] [Google Scholar]
- 49.Maddux AB, Pinto N, Fink EL, et al. Postdischarge Outcome Domains in Pediatric Critical Care and the Instruments Used to Evaluate Them: A Scoping Review. Crit Care Med 2020;48(12):e1313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jarvis JM, Roy J, Schmithorst V, et al. Limbic pathway vulnerability associates with neurologic outcome in children after cardiac arrest. Resuscitation 2022; 182:109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Madurski C, Jarvis JM, Beers SR, et al. Serum Biomarkers of Regeneration and Plasticity are Associated with Functional Outcome in Pediatric Neurocritical Illness: An Exploratory Study. Neurocrit Care 2021;35(2):457–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badke CM, Marsillio LE, Carroll MS, et al. Development of a Heart Rate Variability Risk Score to Predict Organ Dysfunction and Death in Critically Ill Children. Pediatr Crit Care Med 2021;22(8):e437–47. [DOI] [PubMed] [Google Scholar]
- 53.Royka M, Unit G. Promoting Psychosocial Adjustment in Pediatric Burn Patients Through Music Therapy and Child Life Therapy.
- 54.Morrison WE, Haas EC, Shaffner DH, et al. Noise, stress, and annoyance in a pediatric intensive care unit. Crit Care Med 2003;31(1):113–9. [DOI] [PubMed] [Google Scholar]
- 55.Mazer BSE. Hospital Noise and the Patient Experience : Seven Ways to Create and Maintain a Quieter Environment.
- 56.Kawai Y, Weatherhead JR, Traube C, et al. Quality Improvement Initiative to Reduce Pediatric Intensive Care Unit Noise Pollution With the Use of a Pediatric Delirium Bundle. J Intensive Care Med 2019;34(5):383–90. [DOI] [PubMed] [Google Scholar]
- 57.Spazzapan M, Vijayakumar B, Stewart CE. A bit about me: Bedside boards to create a culture of patient-centered care in pediatric intensive care units (PICUs). J Healthc Risk Manag 2020;39(3):11–9. [DOI] [PubMed] [Google Scholar]
- 58.DeSanti RL, Brown DH, Srinivasan S, et al. Patient- and Family-Centered Video Rounds in the Pediatric Intensive Care Unit. Telehealth and Medicine Today 2020;1–14. 10.30953/tmt.v5.231. [DOI] [Google Scholar]
- 59.Anand KJS, Sepanski RJ, Giles K, et al. Pediatric intensive care unit mortality among Latino children before and after a multilevel health care delivery intervention. JAMA Pediatr 2015;169(4):383–90. [DOI] [PubMed] [Google Scholar]
- 60.Environments C, Briggs LP, Fontaine DK, et al. Designing Humanistic Critical Care Environments. Crit Care Nurse Q 2001;24(3):21–34. [DOI] [PubMed] [Google Scholar]
- 61.Chlan L Integrating nonpharmacological, adjunctive interventions into critical care practice: A means to humanize care. American journal of criti 2002; 11(1):14–6. [PubMed] [Google Scholar]
- 62.Ross-Driscoll K, Esper G, Kinlaw K, et al. Evaluating Approaches to Improve Equity in Critical Care Resource Allocation in the COVID-19 Pandemic. Am J Respir Crit Care Med 2021;204(12):1481–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Davidson JE, Aslakson RA, Long AC, et al. Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med 2017;45(1):103–28. [DOI] [PubMed] [Google Scholar]
- 64.Curfman A, Hackell JM, Herendeen NE, et al. Telehealth: Opportunities to Improve Access, Quality, and Cost in Pediatric Care. Pediatrics 2022;149(3). 10.1542/peds.2021-056035. [DOI] [PubMed] [Google Scholar]
- 65.Dale CM, Carbone S, Istanboulian L, et al. Support needs and health-related quality of life of family caregivers of patients requiring prolonged mechanical ventilation and admission to a specialised weaning centre: A qualitative longitudinal interview study. Intensive Crit Care Nurs 2020;58:102808. [DOI] [PubMed] [Google Scholar]
- 66.DeLemos D, Chen M, Romer A, et al. Building trust through communication in the intensive care unit: HICCC. Pediatr Crit Care Med 2010;11(3):378–84. [DOI] [PubMed] [Google Scholar]
- 67.Hall TA, Leonard S, Bradbury K, et al. Post-intensive care syndrome in a cohort of infants & young children receiving integrated care via a pediatric critical care & neurotrauma recovery program: A pilot investigation. Clin Neuropsychol 2022; 36(3):639–63. [DOI] [PubMed] [Google Scholar]
- 68.Ista E, Redivo J, Kananur P, et al. ABCDEF Bundle Practices for Critically Ill Children: An International Survey of 161 PICUs in 18 Countries. Crit Care Med 2022; 50(1):114–25. [DOI] [PubMed] [Google Scholar]
- 69.Ista E, Redivo J, Kananur P, et al. Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Sedation, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Engagement/Empowerment Bundle Practices for Critically Ill Children. Crit Care Med 2021;1–15. 10.1097/ccm.0000000000005168. [DOI] [PubMed] [Google Scholar]
- 70.Smith HAB, Besunder JB, Betters KA, et al. Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility. Pediatr Crit Care Med 2022;23(2):e74–110. [DOI] [PubMed] [Google Scholar]
- 71.Choong K, Awladthani S, Khawaji A, et al. Early Exercise in Critically Ill Youth and Children, a Preliminary Evaluation: The wEECYCLE Pilot Trial. Pediatr Crit Care Med 2017;18(11 PG-546–554):e546–54. [DOI] [PubMed] [Google Scholar]
- 72.Treble-Barna A, Beers SR, Houtrow AJ, et al. PICU-Based Rehabilitation and Outcomes Assessment. Pediatr Crit Care Med 2019;20(6):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Patel Rv, Redivo J, Nelliot A, et al. Early Mobilization in a PICU: A Qualitative Sustainability Analysis of PICU Up!*. Pediatr Crit Care Med 2021;E233–42. 10.1097/PCC.0000000000002619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hopkins RO, Choong K, Zebuhr CA, et al. Transforming PICU Culture to Facilitate Early Rehabilitation HHS Public Access. J Pediatr Intensive Care 2015;4(4): 204–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wieczorek B, Ascenzi J, Kim Y, et al. PICU Up!: Impact of a quality improvement intervention to promote early mobilization in critically ill children. Pediatr Crit Care Med 2016;17(12):e559–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fink EL, Beers SR, Houtrow AJ, et al. Early protocolized versus usual care rehabilitation for pediatric neurocritical care patients: A randomized controlled trial. Pediatr Crit Care Med 2019;20(6):540–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.LaRosa JM, Nelliot A, Zaidi M, et al. Mobilization Safety of Critically Ill Children. Pediatrics 2022;149(4). 10.1542/peds.2021-053432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang J, Ren D, Liu Y, et al. Effects of early mobilization on the prognosis of critically ill patients: A systematic review and meta-analysis. Int J Nurs Stud 2020; 110:103708. [DOI] [PubMed] [Google Scholar]
- 79.Jarvis J, Choong K, Khetani M. Associations of participation-focused strategies and rehabilitation service use with caregiver stress after pediatric critical illness. Arch Phys Med Rehabil 2019;100(4):703–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Liu MH, Zhu LH, Peng JX, et al. Effect of personalized music intervention in mechanically ventilated children in the PICU: A pilot study. Pediatr Crit Care Med 2020;21(1):e8–14. [DOI] [PubMed] [Google Scholar]
- 81.Bush HI, LaGasse AB, Collier EH, et al. Effect of Live Versus Recorded Music on Children Receiving Mechanical Ventilation and Sedation. Am J Crit Care 2021; 30(5):343–9. [DOI] [PubMed] [Google Scholar]
- 82.Garcia Guerra G, Joffe AR, Sheppard C, et al. Music Use for Sedation in Critically ill Children (MUSiCC trial): a pilot randomized controlled trial. J Intensive Care 2021;9(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gerber SM, Jeitziner MM, Wyss P, et al. Visuo-acoustic stimulation that helps you to relax: A virtual reality setup for patients in the intensive care unit. Sci Rep 2017; 7(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lai B, Powell M, Clement AG, et al. Examining the feasibility of early mobilization with virtual reality gaming using head-mounted display and adaptive software with adolescents in the pediatric intensive care unit: Case report. JMIR Rehabil Assist Technol 2021;8(2):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee LA, Moss SJ, Martin DA, et al. Comfort-holding in critically ill children: a scoping review. Can J Anesth 2021;68(11):1695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med 2014;370(5):444–54. [DOI] [PubMed] [Google Scholar]
- 87.Chlan LL, Weinert CR, Heiderscheit A, et al. Effects of patient-directed music intervention on anxiety and sedative exposure in critically Ill patients receiving mechanical ventilatory support: A randomized clinical trial. J Am Med Assoc 2013;309(22):2335–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rennick JE, Stremler R, Horwood L, et al. A Pilot Randomized Controlled Trial of an Intervention to Promote Psychological Well-Being in Critically Ill Children. Pediatr Crit Care Med 2018;19(7):1. [DOI] [PubMed] [Google Scholar]
- 89.Wang SH, Owens T, Johnson A, et al. Evaluating the Feasibility and Efficacy of a Pediatric Intensive Care Unit Diary. Crit Care Nurs Q 2022;45(1):88–97. [DOI] [PubMed] [Google Scholar]
- 90.McIlroy PA, King RS, Garrouste-Orgeas M, et al. The Effect of ICU Diaries on Psychological Outcomes and Quality of Life of Survivors of Critical Illness and Their Relatives: A Systematic Review and Meta-Analysis. Crit Care Med 2019;47(2): 273–9. [DOI] [PubMed] [Google Scholar]
- 91.Waak M, Harnischfeger J, Ferguson A, et al. Every child, every day, back to play: the PICUstars protocol - implementation of a nurse-led PICU liberation program. BMC Pediatr 2022;22(1). 10.1186/s12887-022-03232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hickey E, Johnson T, Kudchadkar SR, et al. Persistence Matters! Hurdles and High Points of PICU Follow-Up Clinic. Pediatr Crit Care Med 2022;23(8):397–9. [DOI] [PubMed] [Google Scholar]
- 93.Samuel VM, Colville GA, Goodwin S, et al. The value of screening parents for their risk of developing psychological symptoms after PICU: A feasibility study evaluating a pediatric intensive care follow-up clinic. Pediatr Crit Care Med 2015;16(9): 808–13. [DOI] [PubMed] [Google Scholar]
- 94.Ducharme-Crevier L, La KA, Francois T, et al. PICU Follow-Up Clinic: Patient and Family Outcomes 2 Months After Discharge. Pediatr Crit Care Med 2021;22(11): 935–43. [DOI] [PubMed] [Google Scholar]
- 95.Butcher B, Eaton T, Montgomery-Yates A, et al. 2022 undefined. Meeting the Challenges of Establishing Intensive Care Unit Follow-up Clinics. Am J Crit Care 2022;31(4):324–8. [DOI] [PubMed] [Google Scholar]
- 96.Anthony L, Hilder A, Newcomb D, et al. General practitioner perspectives on a shared-care model for paediatric patients post-intensive care: A cross-sectional survey. Aust Crit Care 2022. 10.1016/J.AUCC.2022.07.007. [DOI] [PubMed] [Google Scholar]
- 97.Madrigal V, Walter JK, Sachs E, et al. Pediatric continuity care intensivist: A randomized controlled trial. Contemp Clin Trials 2019;76(September 2018):72–8. [DOI] [PubMed] [Google Scholar]
- 98.Leimanis Laurens M, Snyder K, Davis AT, et al. Racial/Ethnic Minority Children with Cancer Experience Higher Mortality on Admission to the ICU in the United States*. Pediatric Critical Care Medicine 2020;859–68. 10.1097/PCC.0000000000002375. [DOI] [PubMed] [Google Scholar]


