Abstract
The gastrointestinal epithelium forms the boundary between the body and external environment. It effectively provides a selective permeable barrier that limits the permeation of luminal noxious molecules, such as pathogens, toxins, and antigens, while allowing the appropriate absorption of nutrients and water. This selective permeable barrier is achieved by intercellular tight junction (TJ) structures, which regulate paracellular permeability. Disruption of the intestinal TJ barrier, followed by permeation of luminal noxious molecules, induces a perturbation of the mucosal immune system and inflammation, and can act as a trigger for the development of intestinal and systemic diseases. In this context, much effort has been taken to understand the roles of extracellular factors, including cytokines, pathogens, and food factors, for the regulation of the intestinal TJ barrier. Here, I discuss the regulation of the intestinal TJ barrier together with its implications for the pathogenesis of diseases.
Keywords: Tight junction, Intestinal epithelium, Cytokine, Pathogen, Nutrient
Introduction
The gastrointestinal epithelium forms the body’s largest interface with the external environment. The epithelium allows the absorption of nutrients while providing a physical barrier to the permeation of proinflammatory molecules, such as pathogens, toxins, and antigens, from the luminal environment into the mucosal tissues and circulatory system (see Fig. 1). The epithelial cells create this selective permeability by two pathways: the transcellular and the paracellular pathway. The transcellular pathway is involved in the absorption and transport of nutrients, including sugars, amino acids, peptides, fatty acids, minerals, and vitamins. As the cell membrane is impermeable, this process is predominantly mediated by specific transporters or channels located on the apical and basolateral membranes [1–3]. The paracellular pathway is associated with transport in the intercellular space between the adjacent epithelial cells. It is regulated by an apical junctional complex, which is composed of tight junctions (TJs) and adherence junctions (AJs) [4–7]. The AJ, along with desmosomes, provides strong adhesive bonds between the epithelial cells and also aids intercellular communication, but does not determine paracellular permeability [6, 7]. The TJs encircle the apical ends of the lateral membranes of epithelial cells and determine the selective paracellular permeability to solutes [4, 5]. In this regard, the TJs provide both a barrier to noxious molecules and a pore for the permeation of ions, solutes, and water as appropriate. TJs are multiple protein complexes composed of transmembrane proteins, such as claudins and occludin, and a wide spectrum of cytosolic proteins. The modification of TJ barrier function and paracellular permeability is dynamically regulated by various extracellular stimuli and is closely associated with our health and susceptibility disease [8–10]. TJ barrier disruption and increased paracellular permeability, followed by permeation of luminal proinflammatory molecules, can induce activation of the mucosal immune system, resulting in sustained inflammation and tissue damage. Evidence from basic science and clinical studies indicate that the intestinal TJ barrier has a critical role in the pathogenesis of intestinal and systemic diseases [8, 10, 11]. Under pathophysiological conditions, pro-inflammatory cytokines, antigens, and pathogens contribute to barrier impairment [9, 12]. In contrast, food factors and nutrients also participate in intestinal TJ regulation, and some of these could be developed as preventive and therapeutic tools for defective barrier-associated diseases [13, 14]. Experimentally, TJ barrier integrity and permeability in intestinal tissues and cells are evaluated by measurement of transepithelial electrical resistance (TER) and the paracellular passage of small molecules, such as mannitol, dextran, and inulin. This review first describes the molecular structure of intestinal TJs, then summarizes the regulation of the intestinal TJ structure and permeability by extracellular factors, such as cytokines, growth factors, pathogens, nutrients, and food factors, and finally discusses the involvement of intestinal TJs in health and disease pathogenesis.
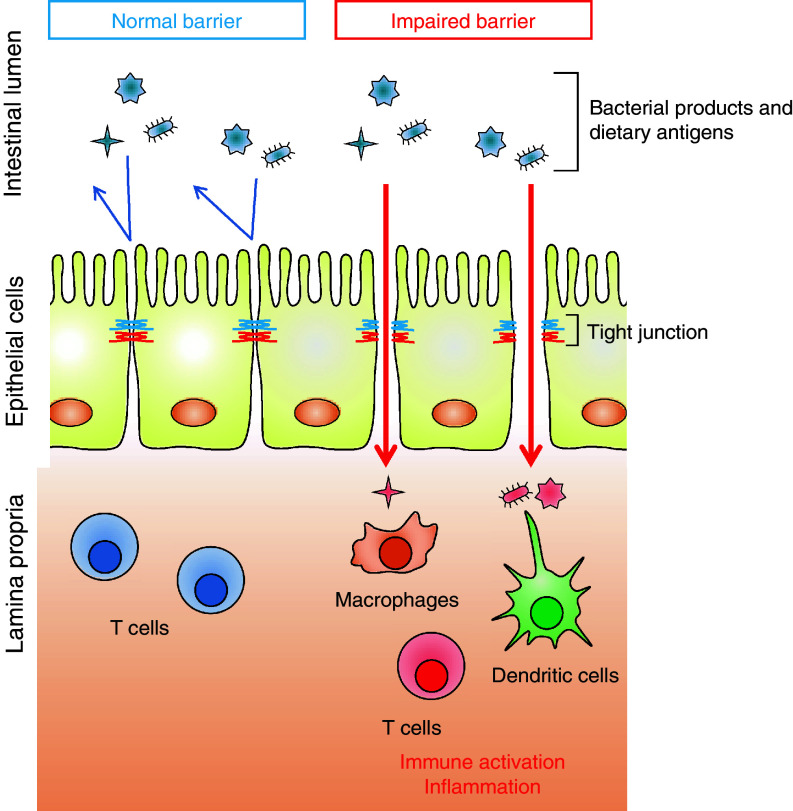
Fig. 1.
Barrier function of intestinal tight junctions (TJs). The intestinal epithelium provides a physical barrier to luminal bacteria, toxins, and antigens. The barrier is organized by different barrier components, including the TJs. The TJs regulate the paracellular passages of ions, solutes, and water between adjacent cells. Luminal noxious macromolecules cannot penetrate the epithelium because of the TJ barrier; however, TJ barrier impairment allows the passage of noxious molecules, which can induce the excessive activation of mucosal immune cells and inflammation. Therefore, intestinal barrier defects are associated with the initiation and development of various intestinal and systemic diseases
Molecular structure of TJs
TJs are multiple protein complexes located at the apical ends of the lateral membranes of intestinal epithelial cells (see Fig. 2). They regulate the paracellular passage of ions, solutes, and water, and are also known to act as a fence to maintain cell polarity by blocking the free diffusion of proteins and lipids between the apical and basolateral domains of the plasma membrane [8, 11]. Four integral transmembrane proteins, occludin [15], claudins [16], junctional adhesion molecule (JAM) [17], and tricellulin [18], have been identified, with the claudin family consisting of at least 24 members. The extracellular domains of the transmembrane proteins form the selective barrier by hemophilic and heterophilic interactions with the adjacent cells [19]. The intracellular domains of these transmembrane proteins interact with cytosolic scaffold proteins, such as zonula occludens (ZO) proteins, which in turn anchor the transmembrane proteins to the perijunctional actomyosin ring. The interaction of TJ proteins with the actin cytoskeleton is vital to the maintenance of TJ structure and function. In addition, the interaction of the TJ complex with the actomyosin ring permits the cytoskeletal regulation of TJ barrier integrity. The circumferential contraction and tension in the perijunctional actomyosin ring is regulated by myosin light chain (MLC) activity (phosphorylation) [20]. Induction of MLC phosphorylation by kinases such as myosin light chain kinase and Rho-associated kinase (ROCK) causes the contraction of the actomyosin ring, resulting in the opening of the paracellular pathways. This section summarizes the structures and functions of the integral TJ proteins [20–22].
Fig. 2.
Molecular structure of the intercelluar junction of intestinal epithelial cells. The intercellular junctions of intestinal epithelial cells are sealed by different protein complexes, including TJs, adherens junctions (AJs), and desmosomes. The TJs, multiple protein complexes, locate at the apical ends of the lateral membranes of intestinal epithelial cells. The TJ complex consists of transmembrane and intracellular scaffold proteins. The extracellular loops of the transmembrane proteins (occludin, claudins, JAMs, and tricellulin) create a permselective barrier in the paracellular pathways by hemophilic and heterophilic interactions with adjacent cells. The intracellular domains of the transmembrane proteins interact with the intracellular scaffold proteins such as zonula occludens (ZO) proteins and cingulin, which in turn anchor the transmembrane proteins to the actin cytoskeleton. Myosin light chain kinase (MLCK) is associated with the perijuctional actomyosin rings and regulates paracellular permeability through myosin contractility. The AJs along with desmosomes provide strong adhesive bonds between the epithelial cells and also intercellular communication, but do not determine paracellular permeability
Occludin
Occludin (~65 kDa) was the first integral membrane TJ protein identified in 1993 [15]. Confocal immunofluorescence microscopy, immunoelectron microscopy, and freeze-fracture immunoreplica electron microscopy specifically visualize occludin at the TJs in the epithelia. Occludin is a tetraspanin membrane protein with 4 transmembrane domains, 2 extracellular loops, and 1 intracellular loop: a short N-terminal and a long C-terminal domain project into the cytoplasm. The homophilic interaction of the extracellular loops of occludin with the adjacent cells appears to create a barrier against macromolecules, but not against small ions [23]. The long C-terminal domain interacts with several intracellular TJ proteins, such as ZO proteins, which are required to link occludin to the actin cytoskeleton [24]. The function of occludin is not yet fully understood, but numerous studies using animals and cell cultures indicate that it has crucial roles in the TJ structure and permeability in the intestinal epithelia [23, 25].
In earlier studies using embryonic stem cells, occludin depletion was shown not to prevent the TJ assembly or differentiation into polarized epithelial cells [26]. Occludin knockout mice also showed a density and organization of TJs in the intestinal epithelium equivalent to those seen in wild-type mice [26]. Further, intestinal barrier function and ion transport in the knockout mice appeared electrophysiologically normal [27]. These studies raised the question of whether occludin is required for TJ assembly and barrier integrity. However, a recent study demonstrated that histological and functional abnormalities are present in several tissues in occludin knockout mice [28]. For example, the occludin knockout mice showed chronic inflammation and hyperplasia of the gastric epithelium, testicular atrophy, and loss of cytoplasmic granules in striated duct cells of the salivary gland, suggesting that the function of occludin is more complex than previously supposed [28]. In addition, synthetic peptides with a sequence corresponding to the occludin extracellular loops, which inhibit the interaction of occludin extracellular domains with adjacent cells, disrupt TJs, and increase paracellular permeability [25]. In a more recent study using intestinal Caco-2 cells and mouse intestines, occludin knockdown was found to induce an increase in paracellular permeability to macromolecules [23]. These data consistently indicate that occludin plays a role in the maintenance and assembly of TJs.
In vitro studies demonstrate that phosphorylation of occludin regulates occludin localization and TJ permeability. This phosphorylation is regulated by the balance between kinases and phosphatases responsible for the phosphorylation sites. In the intact epithelium, occludin is highly phosphorylated on the Ser and Thr residues [29], and the phosphorylation has a role in the maintenance and assembly of the TJ structure [30]. Some kinases, such as protein kinase C (PKC) η and ζ, and casein kinase I and II, have been identified as responsible for the phosphorylation [31–35]. Depletion and inhibition of PKCη and ζ induce occludin dephosphorylation resulting in TJ disruption [31, 32]. Protein phosphorylation detection by mass spectrometry and site-directed mutagenesis reveal that T403, T404, T424, and/or T436 in the C-terminal domain of occludin are the phosphorylation sites targeted by PKCη and ζ. The mutation of these threonine residues to alanine, which prevents the phosphorylation, delays occludin assembly into the TJs. Conversely, occludin undergoes dephosphorylation on Ser and Thr residues during TJ disassembly [29, 36]. Protein phosphatase (PP) 1 and 2A have been reported to directly interact with occludin to dephosphorylate it at Ser and Thr residues [37, 38]. Experimentally, TJs can be disassembled by extracellular calcium depletion, and reassembly is induced after calcium repletion. The calcium-induced reassembly of TJs is accelerated by the knockdown of PP1 and 2A [37]. Interestingly, PP1 dephosphorylates occludin preferentially on Ser residues, while PP2A was more active in dephosphorylating occludin at the Thr residues. On the other hand, the level of tyrosine-phosphorylated occludin is very low in the intact epithelium; however, several studies have shown that tyrosine phosphorylation is caused during disassembly by various stimuli [39–41]. Hydrogen peroxide induces TJ disruption via a tyrosine kinase-dependent mechanism. In hydrogen peroxide-mediated TJ disruption, Y398 and Y402 in the C-terminal domain of occludin are phosphorylated by c-Src tyrosin kinase, and the tyrosine phosphorylation induces TJ disassembly [39]. Underlying this mechanism, the tyrosine phosphorylation of occludin attenuates the interaction with ZO-1, leading to dissociation from the junctional complex [41]. Like hydrogen peroxide, acetaldehyde, a biological metabolite of ethanol, also induces TJ disruption in Caco-2 cells in an occludin tyrosine phosphorylation-dependent manner [42, 43]. Interestingly, acetaldehyde does not affect cellular tyrosine kinase activity, but directly inhibits protein tyrosine phosphatase (PTP) 1B, resulting in occludin phosphorylation on the Tyr residues.
Claudins
Claudins (20–27 kDa) are tetraspanin membrane proteins with 1 intracellular and 2 extracellular loops, and C-terminal and N-terminal cytoplasmic domains [16]. Claudins do not have any sequence similarity to occludin. The extracellular loops of claudin molecules make homophilic and heterophilic interactions with adjacent cells, and the interactions create either barriers against or pores for the passage of selective molecules in the paracellular pathways [5, 44]. The post-synaptic density 95/Drosophila discs large/zona-occludens 1 (PDZ) binding domain in the claudin C-terminal domains interacts with intracellular TJ proteins such as ZO proteins, which in turn anchor the claudins to the actin cytoskeleton. Numerous studies have demonstrated that claudins are the key component and backbone of TJs. When claudins are expressed in fibroblasts, they are incorporated into TJ strands and form paired strands at the cell–cell contacts [16]. Recent studies using claudin knockout mice have shown that claudins have critical roles in barrier formation and paracellular permselectivity in various tissues [45–50]. As a prominent example, claudin-1 knockout mice die within 24 h of birth because of a dramatic loss of fluid and electrolytes through the impaired epidermal barrier [45].
Claudins are a multigene family with at least 24 members in humans and mice, and each isoform shows a unique expression pattern in tissues and cell lines. In mouse intestines, claudin-1, -2, -3, -4, -5, -7, -8, -10, -12, -13, -14, -15, -17, and -18 are detected at the gene expression level, but the relative expression of each isoform varies throughout the segments of the intestine [51]. In contrast to their structural similarities, claudins perform different functions and can be roughly divided into two types: those involved in barrier formation (decreasing paracellular permeability) and those playing a role in channel pores (increasing paracellular permeability) [5, 44]. To our knowledge, in the intestines, claudin-1, -3, -4, -5, -8, -9, -11, and -14 can be categorized as barrier-forming claudins, while claudin-2, -7, -12, and -15 are pore-forming claudins [5, 52–60]. Importantly, the functional properties of each claudin depend on the numbers and positions of charged amino acids in the 1st extracellular loop of the molecule [61]. For example, claudin-2 and -12, pore-forming isoforms, have 3 (positions 53, 65 and 75) and 4 (positions 62, 66, 71 and 74) negatively charged amino acids, respectively, and form selective cation pores [53, 54, 62]. It is suggested that the distribution and orientation of negatively charged residues in the extracellular loop work to repel negatively charged ions (anions) and favor positively charged ions (cations) [61]. Barrier-forming claudins, on the other hand, such as claudin-1 and -3, block the permeability of charged and uncharged molecules according to differences in the distribution and orientation of charged amino acids. However, no detailed information at the atomic level is available because of a lack of x-ray or NMR analysis of claudins.
As is the case with occludin, some claudin isoforms are phosphorylated in the cells, and this phosphorylation is associated with localization and paracellular permeability. Claudin-1 phosphorylation on the serine residues is regulated by a protein phosphatase, PP2A, and a protein kinase, PKCζ [38]. The pharmacological inhibition of PP2A promotes recruitment of ZO-1 and occludin as well as claudin-1 to the TJs after calcium repletion. Similarly, claudin-1 phosphorylation at T203 increases claudin-1 insolubility and TJ integrity in rat lung endothelial cells [63]. Phosphorylation at T207 in claudin-5 also plays an analogous role to that at T203 in claudin-1 [64]. In contrast, some phosphorylation sites have been characterized as negatively regulating TJ barrier integrity. cAMP-dependent kinase (PKA) phosphorylates claudin-3 at T192, and the phosphorylation leads to TJ disruption in ovarian cancer OVCA433 cells [65]. An ephrin receptor tyrosine kinase, EphA2, which is largely expressed in various tumor cells, interacts with and phosphorylates claudin-4 at Y208, leading to an increase in paracellular permeability [66]. A pull-down assay using recombinant Eph2 proteins revealed that the tyrosine phosphorylation attenuates the interaction with ZO-1.
Another example of post-translational regulation of claudin function and localization is palmitoylation [67], although information on this is limited. In kidney epithelial MDCK cells, incorporation of [3H]-palmitic acid into claudin-2, -4, and -14 is observed, indicating palmitoylation [67]. The palmitoylation of claudin-14 at two sets of cysteines in the second intracellular loop and intracellular C-terminal tail, which are well conserved in all claudin isoforms, is required for efficient localization of claudin-14 at the TJ.
Junctional adhesion molecule
The JAM family belongs to the immunoglobulin (Ig) superfamily and is characterized by 2 extracellular Ig domains, one transmembrane domain, and one intracellular C-terminal domain. They are divided into 2 subfamilies based on sequence similarities in the cytoplasmic domains. JAM-A [17], -B [68] and -C [69] (or JAM-1, -2, and -3) have class II PDZ-binding motifs in the intracellular C-terminal domain, which interact with ZO-1 and Par-3, a polarity-related protein. In contrast, JAM-4 [70], coxsackievirus and adenovirus receptor (CAR) [71], endothelial selective adhesion molecule (ESAM) [72], and the brain- and testis-specific immunoglobulin superfamily (BT-IgSF) [73] have class I PDZ-binding motifs. The extracellular N-terminal domains of the JAM family members bind to various ligands through homophilic and heterophilic interactions [74]. The homophilic interactions involving the JAM members have a role in the formation of TJs and the cell–cell border. In contrast, the heterophilic interactions function in cell–cell adhesion, association between leukocytes and epi-/endothelial cells, platelet activation, and virus recognition. JAM members are expressed in various cell types including epithelial, endothelial, and immune cells, and exhibit different expression patterns in both a tissue- and cell type-specific manner. In intestinal epithelial cells, JAM-A, JAM-4, and CAR are expressed and involved in TJ regulation.
In vitro and in vivo studies demonstrate that JAM-A (~43 kDa) participates in the regulation and maintenance of the TJ barrier. In Chinese hamster ovary (CHO) cells, exogenously expressed JAM-A is concentrated at the intercellular junctions [17]. Treatment of intestinal T84 cells with monoclonal JAM-A antibodies inhibits the resealing of the TJs, indicated by delays in TER recovery and occludin assembly [75]. Recent studies using JAM-A knockout mice have also shown the importance of JAM-A in intestinal barrier function [76]. The JAM-A knockout mice exhibit higher permeability to dextran and myeloperoxidase activity in the colon compared to wild-type mice. Further, the colonic injury and inflammation induced by dextran sodium sulfate (DSS) are more severe in the JAM-A knockout mice than in wild-type mice.
JAM-4 (~40 kDa) protein expression is seen in the liver and skeletal muscle as well as in epithelial cells [70]. A study indicates that JAM-4 has a role in epithelial barrier function although there is an absence of direct evidence in the intestinal epithelium. In kidney epithelial MDCK cells, JAM-4 is localized at the intercellular junctions, where it is co-localized with ZO-1 and MAGI-1, and in vitro binding assays show that JAM-4 directly interacts with MAGI-1, but not ZO-1. In CHO cells, JAM-4 overexpression decreases dextran paracellular permeability [70].
CAR (~46 kDa) is a JAM family protein, and the heterophilic interaction of its extracellular domain with coxsackievirus and adenovirus appears to limit virus invasion [71]. CAR is concentrated at cell-cell contacts and is co-localized with ZO-1 in intestinal T84 cells [77]. The recombinant soluble CAR protein, which encodes the extracellular domain and inhibits the intercellular interaction of CAR, delays the recovery of TER after calcium repletion [77]. In CHO and MDCK cells, CAR overexpression decreases dextran permeability and increases TER [77]. This evidence indicates that CAR contributes to epithelial TJ regulation.
Tricellulin
Epithelial and endothelial cells form not only bicellular junctions between two adjacent cells but also tricellular junctions at the cell-cell contacts of 3 adjacent cells. Tricellulin is preferentially localized at tricellular junctions, although it is also observed at bicellular junctions along with occludin and claudins [18]. Tricellulin (~64 kDa) is a tetratranspan membrane protein with one intracellular and two extracellular loops, and C- and N-terminal cytoplasmic domains. The amino acid sequence of the C-terminal domain is ~32 % identical to that of occludin, while the N-terminal domain is longer than that of occludin. An in vitro study using the site-mutagenesis technique suggests that the C-terminal domain of tricellulin is important for the lateral translocation of tricellulin, whereas the N-terminal domain appears to be involved in directing tricellulin to tricellular contacts [78].
Recent studies have indicated that tricellulin plays an important role in epithelial TJ barrier regulation at both tricellular and bicellular junctions, although with different permselective properties. Krug et al. [79] closely examined the permeselectivity of tricellulin at bicellular and tricellular junctions in MDCK cells exogenously expressing tricellulin at low and high levels. When tricellulin is exogenously expressed at low levels in cells, tricellulin localized at the tricellular junctions, but not at the bicellular junction. In these cells, the paracellular permeability of macromolecules, but not small ions, is decreased, indicating that tricellulin limits macromolecule movement at the tricellular junctions. Whereas, when tricellulin is exogenously expressed at high levels, tricellulin localizes at all TJs (bicellular and tricellular), and decreases their permeability to both macromolecules and small ions. These data suggest that tricellulin forms an effective barrier to macromolecules at the tricellular junctions and to all solutes at the bicellular junctions. Interestingly, occludin and tricellulin seem to affect each other’s cellular localization, although the mechanism is unknown. In MDCK cells, occludin knockdown induces the mislocalization of tricellulin to bicellular rather than tricellular junctions, and remedial occludin expression abolishes bicellular tricellulin [80]. Further, in mammary epithelial Eph4 cells, the knockdown of tricelluin remarkably decreases the TER and increases dextran flux with decreased occludin localization at both bicellular and tricellular junctions [18].
Zonula occludens
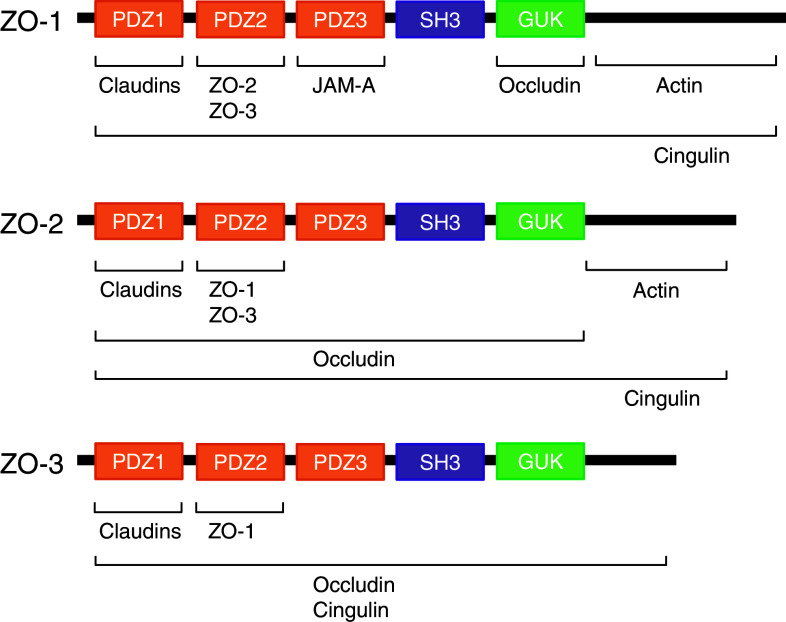
The ZO proteins were the first TJ-specific proteins indentified and 3 ZO proteins, ZO-1 (~220 kDa), -2 (~160 kDa), and -3 (~130 kDa), have been identified to date [81–83]. According to sequence analysis, these ZO proteins are categorized as members of the membrane-associated guanylate kinase homolog (MAGUK) family [19]. They are multi-domain proteins carrying 3 PDZ domains, a Src homology-3 (SH3) domain and a region of homology to GUK from the side of the N-terminus (see Fig. 3). These multi-domain structures provide an intracellular scaffold in the TJs and are required for regulation and maintenance of TJ structure. Interestingly, many TJ proteins bind to the N-terminal half region of ZO proteins, while the C-terminal region interacts with the actin cytoskeleton and cytoskeleton-associated proteins [84]. For example, claudins bind to the first PDZ domains of ZO-1, -2, and -3 [85]; JAM-A binds to the 3rd PDZ domain of ZO-1 [86], and occludin binds to the GUK domain of ZO-1 [24]. The 2nd PDZ domains are used for interactions between ZO proteins [81, 83, 84, 87, 88].
Fig. 3.
Interaction of proteins with the integral scaffold tight junction (TJ) proteins, zonula occludens (ZO)-1, -2, and -3. ZO proteins carry 3 post-synaptic density 95/Drosophila disc large/zona-occludens 1 (PDZ) domains, a Src homology-3 (SH3) domain, and a region of homology to guanylate kinase (GUK) from the side of the N-terminus. Several TJ proteins and cytoskeletal actin interact with the ZO proteins
Among the ZO proteins, the biochemical function and property of ZO-1 have been well-examined. ZO-1 localizes to the nascent cell-cell contacts in both cell cultures and animal models. Therefore, it has been proposed that ZO proteins may mediate the early assembly of TJ proteins into cell-cell contacts. To date, intensive efforts have been made to clarify the functional role of ZO proteins, but it has been difficult to obtain clear evidence showing the importance of ZO proteins in TJ regulation. For example, the exogenous expression of full-length or truncated ZO-1 has only a slight effect on the distribution of other TJ proteins and the formation of TJs [89]. Tsukita et al. [90] have suggested that the unexpected results described above are due in part to the functional redundancy in ZO proteins, and they have generated epithelial Eph cells lacking both ZO-1 alleles to validate their hypothesis. These ZO-1-deficient cells are still able to form normal TJ structures and show normal permeability; however, an obvious delay in the assembly of other TJ proteins including occludin and claudins into the TJ is observed, indicating that ZO proteins have an important role in the regulation of TJ assembly.
Cingulin
Cingulin (~140 kDa) is a component of intracellular plaque proteins in the TJs and has been identified as an actin cytoskeleton-associated protein. Sequence analysis shows that cingulin forms a homodimer with a large globular N-terminal head, a small globular C-terminal tail, and coiled-coil rod domain [19]. Studies demonstrate that cingulin localizes at the TJs and directly or indirectly interacts with several TJ proteins, indicating a role in TJ assembly [86, 91, 92]; however, its functional role has not yet been fully understood. A GST pull-down assay demonstrated that the head domain of cingulin interacts with ZO-1, -2, and -3 [91]. Further, an in vitro binding assay detected the direct binding of cingulin to JAM-A and occludin [86, 92]. However, embryoid bodies lacking the cingulin gene did not show any signs of a barrier formation defect, although the expression of TJ proteins, such as ZO-1, ZO-2, occludin, and claudin-6, was altered [93].
Intestinal TJ regulation by cytokines and growth factors
The roles of cytokines in intestinal TJ regulation under pathophysiological conditions have been well investigated using cell cultures and animal models. The cytokine-mediated dysfunction of the TJ barrier, resulting in immune activation and tissue inflammation, is thought to be important in the initiation and/or development of several intestinal and systemic diseases [8, 11]. In contrast, some growth factors play roles in the protection and maintenance of TJ integrity. This section summarizes recent knowledge regarding the cytokine- and growth factor-mediated regulation of intestinal TJ barrier function. Tables 1 and 2 provide lists of cytokines and growth factors that increase and decrease the intestinal TJ barrier and their molecular mechanisms, respectively. Although there are a number of reports showing their effects on the barrier function in other cell types, such as kidney epithelial cells, vascular endothelial cells and the blood–brain barrier, those will not be discussed here.
Table 1.
Cytokines and growth factors which increase intestinal TJ permeability
| Cytokine and growth factor | Permeabilitya | Cell | Mechanismb |
|---|---|---|---|
| IFN-γ | Increase | T84 | Myosin II-dependent vacuolarization, internalization of JAM-A, occludin, claudin-1 and claudin-4 [96, 97] |
| TNF-α | Increase | Caco-2 | ZO-1 ↓ [103] |
| Increase | Caco-2 | MLCK ↑, pMLC ↑ [104, 106] | |
| Increase | HT29/B6 | Claudin-2 ↑ [107] | |
| TNF-α/IFN-γ | Increase | Caco-2 | MLCK ↑, pMLC ↑ [109, 110] |
| LIGHT/IFN-γ | Increase | Caco-2 | MLCK ↑, pMLC ↑, Caveolar endocytosis (occludin, ZO-1 and claudin-1) [111] |
| IL-1β | Increase | Caco-2 | Occludin ↓ [116] |
| Increase | Caco-2 | MLCK ↑, pMLC ↑ [117] | |
| IL-4 | Increase | T84 | Claudin-2 ↑ [121] |
| IL-6 | Increase | Caco-2, T84 | Claudin-2 ↑ [128] |
| IL-13 | Increase | T84 | Claudin-2 ↑ [142] |
| Increase | HT29/B6 | Claudin-2 ↑ [141] | |
| Increase | Caco-2 | Potentiate oxidant [150] |
aPermeability is based on results for TER and the paracellular passage of molecules
bSymbols ↑ and ↓ indicate increases and decreases in the protein or mRNA expression, respectively
Table 2.
Cytokines and growth factors which decrease and restore intestinal TJ permeability
| Cytokine and growth factor | Permeabilitya | Cell | Mechanismb |
|---|---|---|---|
| IL-10 | Decrease | T84 | Neutralize IFN-γ [134] |
| IL-17 | Decrease | T84 | Claudin-1 ↑, Claudin-2 ↑ [146] |
| TGF-α antibody | Decrease | Caco-2 | Neutralize hydrogen peroxide [149] |
| TGF-β | Decrease | T84 | Claudin-1 ↑ [151] |
| Decrease | HT29/B6 | Claudin-4 ↑ [152] | |
| Decrease | T84 | Neutralize EHEC, restoration of occludin, claudin-2 and ZO-1 expression [151] | |
| Decrease | T84 | Neutralize IFN-γ [152] | |
| Decrease | T84 | Neutralize cryptosporidium parvum [153] | |
| EGF | Decrease | Caco-2 | Neutralize hydrogen peroxide, restoration of occludin and ZO-1 distribution [155] |
| Decrease | Caco-2 | Neutralize hydrogen peroxide, restoration of actin cytoskeleton assembly [157, 292] | |
| Decrease | Caco-2 | Neutralize ethanol, restoration of microtubule assembly and oxidation/nitration of tubulin [158] | |
| Decrease | Caco-2 | Neutralize acetaldehyde, restoration of occludin and ZO-1 distribution [42, 159] |
aPermeability is based on results for TER and the paracellular passage of molecules
bSymbols ↑ and ↓ indicate increases and decreases in the protein or mRNA expression, respectively
Interferon-γ
Interferon-γ (IFN-γ) is a Th1 proinflammatory cytokine that is predominantly secreted by T cells and natural killer cells. IFN-γ is mainly involved in the regulation of inflammatory immune responses, and levels are elevated in the intestinal mucosa in patients with inflammatory bowel disease (IBD) [94, 95]. Recent studies have also demonstrated that this cytokine increases paracellular permeability in intestinal epithelial cells through the redistribution and expression of TJ proteins and the rearrangement of the actin cytoskeleton. In intestinal T84 cells, IFN-γ induces the cellular internalization of transmembrane TJ proteins (occludin, claudin-1, claudin-4, and JAM-A) from the junctional region, resulting in a decrease in TER and increase in dextran flux [96, 97]. Immunofluorescence microscopy has revealed that this protein internalization is mediated by large actin-coated vacuoles that originate from the apical plasma membrane. Importantly, the internalization of occludin and JAM-A into the subapical cytosolic compartment is observed in the mucosal biopsies of patients with ulcerative colitis (UC) [97]. The vacuoles are co-localized with active myosin and are suppressed by inhibition of ROCK, but not myosin light chain kinase (MLCK). IFN-γ activates a ROCK regulator, small GTPase RhoA, and also increases ROCK expression. Taken together, these facts indicate that IFN-γ increases acto-myosin contractility in a ROCK-dependent manner and induces TJ protein internalization, resulting in intestinal TJ disruption.
Tumor necrosis factor-α
Tumor necrosis factor-α (TNF-α) is a proinflammatory cytokine that is produced mainly by activated T cells and macrophages. As the efficacy of TNF-α antibodies for the treatment of IBD has shown, TNF-α, like IFN-γ, has a crucial role in the pathogenesis of IBD [98, 99]. Clinical studies show that this cytokine is elevated in the intestinal mucosa, serum, and stools of IBD patients [95, 100, 101]. TNF-α is known to induce apoptosis and inflammatory response in intestinal epithelial cells [102], and recent studies have also demonstrated that it impairs the intestinal TJ barrier through different mechanisms.
In intestinal Caco-2 cells, treatment with TNF-α decreases the TER and increases the inulin permeability by 48 h post-treatment; however, the alterations delayed the TNF-α-induced decrease in ZO-1, a TJ integral protein, suggesting the presence of additional mechanisms [103]. The authors then revealed that the MLCK expression, which has an important role in TJ regulation, was interrelated with the TNF-α-induced barrier defect. The TNF-α-induced decrease in TER is well correlated with MLCK expression and MLC phosphorylation, and is inhibited by a MLCK inhibitor [104]. Further, mice injected with TNF-α show increased MLCK expression in the colon [105]. A series of their studies shows that the NF (nuclear factor)-κB signaling mediates TNF-α-induced MLCK expression and barrier defect [106]. In intestinal HT29/B6 cells, TNF-α was seen to decrease TER through claudin-2 expression [107]. Claudin-2 is expressed throughout the intestines and forms a pore for cations such as Na+. These TNF-α-induced alterations are blocked by the pharmacological inhibition of phosphatidyl inositol-3 kinase (PI3K), indicating the involvement of PI3K/Akt signaling. Collectively, TNF-α directly impairs the intestinal TJ barrier through cytoskeletal rearrangement and TJ protein expression.
Combination of TNF-α and IFN-γ
Under inflammatory conditions, tissues including the intestinal epithelium are exposed to multiple cytokines [95, 100, 108]. Both TNF-α and IFN-γ are often increased in intestinal mucosa under inflammatory conditions including IBD [95]. Although the application of multiple cytokines to the experimental model complicates the mechanistic interpretation, it may more faithfully reflect pathophysiological conditions. The achievement in understanding the combined effect of TNF-α and IFN-γ is a good example.
As described above, TNF-α and IFN-γ independently cause intestinal barrier dysfunction. Furthermore, studies have revealed that these 2 cytokines synergistically impair intestinal barrier function. In intestinal Caco-2 cells, TNF-α only induces a decrease in TER and an increase in dextran flux after treatment with IFN-γ, indicating that IFN-γ primes the intestinal cells to regulate TJ integrity in response to TNF-α [109]. The TNFα/IFN-γ-induced barrier dysfunction is caused by actomyosin contractility, resulting from MLCK expression and MLC phosphorylation. It is known that TNF-α activates the signaling pathways leading to various cellular responses through TNF-α receptor (TNFR) 1 and 2 on the membrane surface. IFN-γ increases both TNFR1 and 2 in the cells, but a blocking antibody for TNFR2, but not TNFR1, inhibits the TNFα/IFN-γ-induced barrier dysfunction, indicating that IFN-γ primes the cells by increasing TNFR2 in response to TNFα [110]. In addition, the same research group has reported that another TNF-α family member, lymphotoxin-like inducible protein (LIGHT), synergizes with IFN-γ to induce intestinal barrier dysfunction [111]. This LIGHT/IFN-γ-mediated barrier dysfunction requires MLCK activation and internalization of TJ proteins. Consistent with these observations, TNF-α and IFN-γ synergistically induce intestinal barrier defects through cytoskeletal rearrangement.
Interleukin-1β
Interleukin-1β (IL-1β), an IL-1 family member, is one of the first cytokines to be discovered. It has been reported that IL-1β is markedly elevated in intestinal mucosa under inflammatory conditions, such as in Crohn’s disease (CD) patients [108, 112]. A direct correlation has been found between increased levels of IL-1β and increases in the severity of intestinal inflammation in CD patients [108, 113]. In clinical studies, an IL-1 receptor antagonist is currently being developed for therapeutic usage [114, 115]. Thus, IL-1β plays a central role in the intestinal inflammatory process, and recent studies show that IL-1β causes increased intestinal TJ permeability.
In intestinal Caco-2 cells, IL-1β decreases TER and increases inulin flux [116, 117]. This barrier defect is in part mediated by the decreased expression and redistribution of occludin, an integral transmembrane TJ protein [116]. The IL-1β-induced decrease in occludin expression occurs at a transcription level. As another mechanism, the reduction of TER by IL-1β is associated with MLCK expression and MLC phosphorylation [117]. The authors show that the knockdown of NF-κB p65 inhibits the decrease in occludin and increases in MLCK expression, indicating NF-κB-dependent transcriptional regulation by IL-1β. Further, MEKK1 activity is required for IL-1β-induced NF-κB activation [118]. Collectively, IL-1β impairs the intestinal TJ barrier through decreases in occludin and cytoskeletal rearrangement.
Interleukin-4
Interleukin-4 (IL-4), which is predominantly secreted by T cells, basophils, and mast cells, plays a central role in humoral and adaptive immune responses. IL-4 is regarded as a major mediator of allergic diseases, because it promotes the differentiation of naïve helper T-cells into Th2 cells, the proliferation and differentiation of B cells, B cell class switching to IgE, and the expression of MHC class II antigens and low-affinity IgE receptors [119, 120]. Furthermore, IL-4 leads to intestinal barrier impairment, although the mechanism remains unclear.
In intestinal T84 cells, IL-4 decreases TER and increases dextran flux [121, 122]. Immunoblot analysis and immunofluorescence microscopy reveal that IL-4 induces pore-forming claudin-2 expression and localization at the TJs [121]. Claudin-2, however, is characterized as forming pores for cations, but not for macromolecules such as dextran, suggesting the presence of additional mechanisms. Another research group demonstrated that the pharmacological inhibition of PI3K blocks the IL-4-induced reduction in TER in T84 cells, indicating the involvement of the PI3K pathways in IL-4-induced barrier impairment [123]. However, claudin-2 expression was not examined by that group.
Interleukin-6
Interleukin-6 (IL-6) is a pleiotropic cytokine whose expression is important for the host response to a number of infections, and which exerts antigen-specific immune responses and has both pro- as well as anti-inflammatory effects [124, 125]. Excessive secretion of IL-6 and dysregulation of the signaling pathway may play a major role in the pathogenesis of many diseases, including IBD. A clinical study showed that IL-6 is produced in substantially higher amounts in both the serum and tissues of IBD patients [108, 126]. The major source of IL-6 seen in IBD has been shown to be intestinal epithelial cells and lamina propria mononuclear cells [127]. Recent studies also indicate the involvement of IL-6 in intestinal TJ regulation.
IL-6 increases paracellular permeability selectively to cations, but not to macromolecules, with an increase in pore-forming claudin-2 in intestinal Caco-2 cells [128]. These alterations are also observed in T84 cells and mouse colons. This IL-6-mediated claudin-2 expression and barrier defect require the MEK/ERK and PI3K/Akt signaling activations. IL-6 binds to cell surface IL-6 receptors, which in turn initiate intracellular signaling via gp130, a signal-transducer subunit. The claudin-2 expression induced by IL-6 is caused at a transcription level in a Cdx2-dependent mechanism. In addition, IL-6 is necessary for the development of gut barrier dysfunction after hemorrhagic shock and resuscitation (HS/R) in mice [129]. HS/R increases intestinal permeability to dextran flux and bacterial translocation to mesenteric lymph nodes along with increased mucosal IL-6 expression and decreased occludin and ZO-1 expression in the intestinal epithelium. However, these alterations are not observed in IL-6 knockout mice, indicating that IL-6 has a central role in barrier defect formation after HS/R.
Interleukin-10
Interleukin-10 (IL-10), a homodimeric cytokine mainly produced by Th2 cells, regulatory T cells, monocytes/macrophages, and dendritic cells, is regarded as an anti-inflammatory cytokine [130, 131]. In vitro studies have demonstrated that IL-10 opposes the cellular functions induced by TNF-α and Th1 cytokines such as IFN-γ [132]. IL-10 knockout mice, which are widely used as a model of spontaneous colitis, show increased intestinal permeability with elevated TNF-α, IL-1β, and IL-6 expression prior to exhibiting histologic signs of intestinal inflammation [133]. These observations suggest that IL-10 has a role in the protection of the intestinal barrier. Consistent with this hypothesis, in vivo and in vitro studies have shown that IL-10 exhibits protective effects on the intestinal TJ barrier. In intestinal T84 cells, IL-10 prevents INF-γ-induced increases in mannitol and inulin flux [134]. Clinical and animal studies have demonstrated that a major physiological consequence of total parenteral nutrition (TPN) is the loss of intestinal barrier integrity [135–137]. Mice administered with TPN show increased intestinal paracellular permeability and decreased levels of TJ proteins (ZO-1, ZO-2 and occludin), concomitantly with a decrease in mucosal IL-10 expression [138]. In these mice, IL-10 treatment restores the intestinal barrier defect.
Interleukin-13
Interleukin-13 (IL-13) is an immunoregulatory cytokine that plays a key role in the pathogenesis of allergic asthma and atopy. It is mainly secreted by Th2 cells, natural killer cells, visceral smooth muscle cells, eosinophils, mast cells, and basophils. It has been reported that IL-13 expression is elevated under inflammatory conditions, such as in the colonic mucosa of UC and CD patients [139, 140], and that this elevation possibly contributes to intestinal barrier dysfunction.
In intestinal T84 and HT29/B6 cells, IL-13 increases pore-forming claudin-2 expression and the paracellular permeability with little effect on other TJ proteins [139, 141, 142]. The colonic epithelium of mice administered with IL-13 also exhibits increased claudin-2 expression and permeability to Na+ [142]. IL-6-mediated claudin-2 expression and TJ permeability require activation of the PI3K/Akt signaling pathways.
Interleukin-17
Th17 has recently received considerable attention as it exhibits effector functions distinct from those of Th1 and Th2 cells. Interleukin-17 (IL-17) is mainly produced in Th17 cells, potently induces tissue inflammation, and is associated with the pathogenesis a variety of autoimmune conditions including rheumatoid arthritis, multiple sclerosis, and IBD [143–145]. Information regarding intestinal barrier regulation by IL-17 is limited, but one study has demonstrated that this cytokine induces claudin expression. In intestinal T84 cells, IL-17 increases 2 claudin isoforms, claudin-1 and -2, which have opposing effects on TJ integrity [146]: claudin-1 is categorized as a barrier-forming isoform, while claudin-2 forms cation-selective pores. As a consequence of the increases in claudin-1 and -2 induced by IL-17, the cells exhibit increased TER and decreased mannitol permeability [146]. Interestingly, the induction of claudin-1 and -2 is mediated through distinct signaling pathways. The pharmacological inhibition of MEK blocks IL-17-induced claudin-2, but not claudin-1 expression. The MEK pathway is also required for the claudin-2 expression induced by other cytokines, such as IL-6 and IL-13, as described above [128, 142]. However, the mechanisms underlying IL-17-mediated claduin-1 expression are yet to be elucidated.
Transforming growth factor-α
Transforming growth factor-α (TGF-α) is a member of the EGF family and is synthesized as a transmembrane precursor with EGF structural units in the extracellular domain [147]. The soluble form of TGF-α is released from the transmembrane protein by proteolytic cleavage. TGF-α binds to the EGF receptor on the cell surface and activates cellular signaling. Accordingly, TGF-α is known to show a similar potency to that of EGF, demonstrating, for example, promotive effects on cell proliferation and differentiation [148]. However, the effects of TGF-α on the intestinal barrier are reportedly controversial. Forsyth et al. [149] demonstrated that hydrogen peroxide-mediated barrier defects are blocked by a TGF-α antibody in intestinal Caco-2 cells, indicating that the oxidative stress induces cleavage and release of endogenous TGF-α and that the released TGF-α contributes to barrier impairment. This effect is mediated by the EGFR-MEK/ERK pathway. In contrast, Rao et al. [150] demonstrate that oxidative stress-induced barrier disruption, which is induced by xanthine oxidase and xanthine, is potentiated by the TGF-α antibody in Caco-2 cells.
Transforming growth factor-β
Transforming growth factor-β (TGF-β) is a highly pleiotropic cytokine that is apparently secreted by all cell types. This growth factor is proposed to act as a cellular switch to regulate immune function, proliferation, and epithelial mesenchymal transition. Previous studies have demonstrated that TGF-β has protective or promotive effects on intestinal barrier function. In intestinal T84 cells, TGF-β increases the basal TER in both a dose- and time-dependent manner [151]. This increase in TER is mediated by claudin-1 expression through MEK/ERK signaling. In intestinal HT29/B6 cells, TGF-β decreases the paracellular permeability with increased claudin-4 expression [152]. Further, TGF-β protects the intestinal TJ barrier against noxious stimuli including IFN-γ [152], cryptosporidium parvum [153], and enterohemorrhagic Escherichia coli (EHEC) [151]. For example, in T84 cells, EHEC disrupts the TJ barrier by disturbing the expression and distribution of TJ proteins (ZO-1, claudin-2, and occludin). Pre-treatment of the cells with TGF-β attenuates the EHEC-induced TJ disruption [151].
Epidermal growth factor
Epidermal growth factor (EGF) is largely produced in and secreted from the submandibular glands, kidney, lactating mammary glands, and pancreas. The activity derived from EGF secreted by submandibular glands can be detected in the intestinal contents. EGF is initially synthesized as a 130-kDa precursor transmembrane protein, and the mature and soluble form is released by proteolytic cleavage. The EGF receptor is expressed on the membrane surface of most cell types, and EGF mediates various biological functions, including cellular proliferation, differentiation, and survival through the receptor. Further, recent studies have shown that EGF protects intestinal barrier function against noxious stimuli including oxidative stress, ethanol, and acetaldehyde.
Numerous studies have demonstrated that oxidative stress impairs intestinal barrier function [154]. In intestinal Caco-2 cells, pre-treatment with EGF inhibits oxidative stress-induced barrier disruption, as indicated by TER, macromolecule flux, and TJ protein (occludin and ZO-1) distributions [155]. EGF is known to activate several signaling pathways such as PKC and MAPK. The activation of the MEK/ERK pathway seems to be required for the EGF-mediated protection of the intestinal barrier against the oxidative stress, because pre-treatment of cells with a MEK inhibitor blocks the EGF-mediated effect [155]. In cells treated with EGF, ERK directly interacts with occludin, although the specific role is still unknown. Another research group has demonstrated that PKC-β and -ζ isoforms also have an important role in the EGF-mediated protection of barrier integrity against oxidative stress [156, 157]. On the other hand, ethanol and its oxidized metabolite, acetaldehyde, also induce intestinal hyperpermeability, which contributes to the development of alcoholic liver disease (ALD) (see “Alcoholic liver disease”). EGF prevents the microtubule disassembly and paracellular hyperpermeability induced by ethanol in Caco-2 cells [158]. Acetaldehyde, which is produced from ethanol by alcohol dehydrogenase, disrupts barrier function, as indicated by TER, macromolecule flux, and TJ protein (occludin and ZO-1) redistributions in Caco-2 cells. Pretreatment of cells with EGF inhibits these alterations through the activation of EGFR-phospholipase (PLC)-γ-PKCβ1/ε and EGFR-MEK/ERK signaling pathways [42, 159].
Intestinal TJ regulation by pathogens
A variety of exogenous bacteria symbiotically live in our intestinal lumen. They contribute to the maintenance of intestinal function and health; however, on occasion, pathogenic bacteria intrude into the intestines and tissues to cause infectious diseases. The interaction of enteric pathogens with intestinal epithelial cells often disturbs the intestinal TJ barrier, leading to abnormal electrolyte and fluid transport and tissue inflammation. The pathogens disrupt the barrier through direct binding to epithelial cells or the secretion of toxins. This section provides examples of barrier disruption by enteric pathogens and describes the underlying molecular mechanisms.
Vibrio cholerae
Enteric infection with V. cholerae, a gram-negative pathogenic bacterium, induces diarrhea leading to dehydration. Studies suggest that intestinal barrier impairment contributes in part to the pathogen-induced disaster. The major reservoirs of V. cholerae are aquatic sources, and infections are often associated with copepods, shellfish, and aquatic plants. V. cholerae produces several toxins, such as Cholerae toxin, hemmagglutinin/protease (HA/P), Zonula occludens toxin (ZOT), and accessary cholerae enterotoxin. ZOT and HA/P have been reported to disrupt intestinal barrier function.
ZOT has been found as a second enterotoxin produced in V. cholerae [160, 161]. It decreases TER in the small intestines of rats, rabbits, and intestinal Caco-2 cells [161]. ZOT is synthesized in the V. cholerae outer membrane and has a molecular mass of ~45 kDa (~399 a.a.), and the C-terminal fragment of 12 kDa (a.a. 288–399) is excreted in the intestinal host milieu. The C-terminal fragment seems to be responsible for the disruptive effect on the TJs, as the reduction in TER caused by a truncated mutant named ΔG-ZOT, which retains a.a. 264–399, is nearly comparable to that by full-length ZOT in intestinal Caco-2 cells [162]. The ZOT and ΔG-ZOT induce the redistribution of TJ proteins (occludin and ZO-1) and cytoskeletal rearrangement, resulting in barrier disruption [163]. This process requires PKCα activation. Further, structure–function analysis has identified a hexapeptide (FCIGRL, a.a. 288–293) as one of the biologically active domains of ΔG-ZOT [162]. This hexapeptide, FCIGRL, is structurally similar to a motif (SLIGRL) contained in the ligand for proteinase activated receptor (PAR) 2, which has a role in TJ regulation. The FCIGRL-mediated disruptive effects on the TJs are not observed in the small intestines of PAR2 knockout mice, indicating that PAR2 is one of the receptors for ΔG-ZOT and that the hexapeptide at least partially contributes to ZOT-induced TJ disruption [163]. However, additional mechanisms and receptors are also suggested as a higher concentration of FCIGRL is required for biological activity than that of ΔG-ZOT [163], and a glycine residue at 298 (referred to the full-length ZOT) has a critical role in the binding of ΔG-ZOT to the intestinal membrane [162].
The HA/P produced by V. cholerae is a zinc-binding metalloprotease that disrupts the intestinal barrier through occludin degradation. The HA/P was identified from results showing that the culture supernatants of toxin-attenuated vaccine strains still exhibit a disruptive effect on intestinal TJs [164]. The HA/P activity cleaves the extracellular domain of occludin, resulting in the dissociation of ZO-1 from the intracellular domain of occludin [165]. This dissociation finally results in actin cytoskeletal rearrangement and hyperpermeability.
Enteropathogenic E. coli
EPEC, a noninvasive enteric pathogen, causes acute watery diarrhea and is of great medical importance in developing countries. This pathogen disrupts the barrier through attachment to the intestinal epithelial cells. EPEC infection induces paracellular hyperpermeability in the mouse intestines (ileum and colon) and intestinal T84 cells, as indicated by decreased TER [166–170]. In T84 cells infected with EPEC, cytoskeletal rearrangement, and aberrant distributions of TJ proteins (ZO-1, occludin, and claudin-1) are observed [166]. Faroll et al. demonstrated that EPEC-induced barrier disruption is attenuated by the pharmacological inhibition of either PKCζ or MLCK [171]. MLCK inhibition did not inhibit the EPEC-induced PKCζ translocation to intercellular junctions, but it remains unclear whether these 2 pathways independently affect the TJ barrier or whether PKCζ acts proximally in the MLCK pathway. Recently, Dean et al. [172] have revealed that the EPEC-induced barrier disruption is mediated by two effector molecules, E. coli-secreted protein F (EspF) and mitochondrial-associated protein (Map), and a bacterial surface protein, intimin. EspF is required for the barrier disruption at an early time point after EPEC infection in mice [168], but the precise roles of the 3 proteins are still unclear.
Enterohemorrhagic E. coli
EHEC, also referred to as verotoxin-producing E. coli or Shiga toxin-producing E. coli, is a pathogenic bacterium. Enteric infection causes diarrhea and hemorrhagic colitis, and can lead to life-threatening systemic effects including hemolytic-uremic syndrome and thrombotic thrombocytopenic purpura. Although EHEC organisms produce Shiga toxins or verotoxins, which inhibit cell protein synthesis, these toxins do not appear to play a role in the diarrheal illness induced by EHEC [173]. In intestinal T84 cells, live EHEC, but not dead cells or a conditioned medium, disrupt the TJ barrier with redistribution of TJ proteins (ZO-1 and occludin), suggesting that the direct interaction of bacteria with the intestinal cells triggers barrier disruption [173]. The EHEC-induced hyperpermeability is attenuated by a MLCK inhibitor, indicating that MLC activation and cytoskeletal contraction is one of the underlying mechanisms [173]. Although EHEC translocates PKCζ to the intercellular junction, as is the case in EPEC, PKCζ does not seem to be involved in the EHEC-induced barrier disruption [171].
Clostridium perfringens
Clostridium perfringens is a gram-positive, anaerobic, and spore-forming bacterium of the genus Clostridium. C. perfringens is ever present in nature and can be found as a normal component of decaying vegetation, marine sediment, the intestinal tract of humans and other vertebrates and insects, and soil. Therefore, this pathogen is the third most common cause of food poisoning in the UK, and the US [174]. C. perfringens induces diarrhea through enterotoxin (CPE, ~35 kDa) secretion [175]. CPE consists of two functional domains, an N-terminal cytotoxic region and a C-terminal receptor-binding region (C-CPE) [176, 177]. Two functional receptors for CPE expressed in the various cell types, including the intestinal epithelial cells, have been identified as CPE-R and RVP-1 [178, 179]. Interestingly, the 2 receptors were designated as claudin-3 and -4, because the amino acid sequences of the receptors are similar to claudin-1 and -2, which were the only claudin members identified at that time [180]. CPE and C-CPE induce intestinal hyperpermeability in animals and cell cultures, as indicated by macromolecule flux and TER [181]. The direct binding of C-CPE to the extracellular domains of claudin-3 and -4 causes the internalization of claudins from the junctions [180]. Further, CPE becomes associated with occludin during the internalization [182]. Freeze fracture replica images also show disintegrated TJ strands in cells exposed to CPE [180].
Intestinal TJ regulation by nutrients and food factors
Although information is still limited, food factors and nutrients have been speculated to participate in intestinal TJ regulation. Studies suggest that several food factors, such as glutamine, polyphenols, and probiotics, enhance and protect TJ barrier integrity and could be developed as therapeutic tools for diseases associated with barrier defects. In contrast, alcohol and its metabolite, acetaldehyde, impair the TJ barrier, and this impairment may play a role in disease pathogenesis. This section summarizes the evidence from experimental and clinical studies showing intestinal TJ regulation by food factors and nutrients. Tables 3 and 4 presents lists of nutrients and food factors known to increase and decrease the intestinal TJ barrier and their molecular mechanisms, respectively.
Table 3.
Nutrients and food factors increase intestinal TJ permeability
| Nutrients and food factorsa | Permeability | Cell | Mechanismb |
|---|---|---|---|
| Amino acid | |||
| Gln deprivation | Increase | Caco-2 | Occludin ↓, claudin-1 ↔, ZO-1 ↔ [187, 188] |
| Fatty acid | |||
| EPA, DHA, γ-LA | Increase | Caco-2 | Unknown [195, 196] |
| Capric acid | Increase | Caco-2 | Occludin ↔, ZO-1 ↔, MLCK activation [198, 199] |
| Lauric acid | Increase | Caco-2 | MLCK activation [198, 199] |
| Other | |||
| Ethanol | Increase | Caco-2 | ZO-1 ↔, occludin ↔, pMLC ↑ [244] |
| Acetaldehyde | Increase | Caco-2 | ZO-1 ↔, occludin ↔, E-cadherin ↔, β-catenin ↔ [43, 220, 246] |
aPermeability is based on TER and the paracellular passage of molecules
bSymbols ↑ and ↓ indicate increases and decreases in the protein or mRNA expression, respectively. The symbol ↔ indicates alterations in the cellular distribution of the proteins
Table 4.
Nutrients and food factors decrease and restore intestinal TJ permeability
| Nutrients and food factorsa | Permeability | Cell | Mechanismb |
|---|---|---|---|
| Amino acid | |||
| Gln | Not determined | Caco-2 | Claudin-1 ↔ [187] |
| Gln | Decrease | Caco-2 | Neutralize acetaldehyde, restoration of occludin and ZO-1 distribution [189] |
| Trp | Decrease | Caco-2 | Unknown [191] |
| Peptide | |||
| Casein peptide | Decrease | Caco-2 | Occludin ↑ [194] |
| Cheese peptide | Decrease | Caco-2 | Unknown [192] |
| Fatty acid | |||
| EPA, DHA, arachidonic acid, γ-LA, di-homo-γ-LA | Decrease | T84 | Unknown [197] |
| EPA, DHA, arachidonic acid, di-homo-γ-LA | Decrease | T84 | Neutralize IL-4 [197] |
| Acetic acid | Decrease | Caco-2, T84 | Unknown [206] |
| Propionic acid | Decrease | Caco-2, T84 | Unknown [206] |
| Butyric acid | Decrease | Caco-2 | Promotion of occludin and ZO-1 assembly in Ca-induced TJ reassembly [205] |
| Vitamin | |||
| Vitamin A | Decrease | Caco-2 | Neutralize Clostridium difficile toxin A [213] |
| Vitamin D | Not determined | SW480 | ZO1 ↑, claudin-1 ↑, claudin-2 ↑, E-cadherin ↑ [214] |
| Decrease | Caco-2 | Neutralize DSS [214] | |
| Polyphenol | |||
| Quercetin | Decrease | Caco-2 | Claudin-4 ↑, ZO-2 ↔, claudin-1 ↔, occludin ↔ [217] |
| Kaempferol | Decrease | Caco-2 | ZO-2 ↑, claudin-4 ↑ occluidn ↔, claudin-1 ↔, claudin-3 ↔ [218] |
| Myricetin | Decrease | Caco-2 | Unknown [217] |
| Genistein | Decrease | Caco-2 | Neutralize hydrogen peroxide, occludin ↔, ZO-1 ↔ [40] |
| Decrease | Caco-2 | Neutralize acetaldehyde, occludin ↔, ZO-1 ↔ [43] | |
| Curcumin | Decrease | Caco-2 | Neutralize TNF-α [106] |
| Decrease | Caco-2 | Neutralize IL-1β [116] | |
| EGCG | Decrease | T84 | Neutralize IFN-γ [221] |
| Probiotics | |||
| ECN | Decrease | T84 | Unknown [225] |
| Decrease | T84 | Neutralize EPEC, ZO-2 ↔ [225] | |
| Streptococcus thermophilus | Decrease | Caco-2 | Unknown [226] |
| Lactobacillus acidophilus | Decrease | Caco-2 | Unknown [226] |
| Spreptococcus thermophiles/Lactobacillus acidophilus | Decrease | HT29/cl.19A | Neutralize enteroinvasive E. coli, restoration of occludin and ZO-1 phosphorylation [226] |
| Decrease | HT29 cl.19A | Neutralize TNF-α/IFN-γ [226] | |
| VSL#3 | Decrease | HT29 | Neutralize TNF-α [228] |
| Lactobacillus plantarum | Decrease | Caco-2 | Neutralize TNF-α [231] |
| Decrease | Caco-2 | Neutralize phorbol ester [232] | |
| Lactobacillus rhamnosus OLL2838 | Decrease | Caco-2 | Neutralize TNF-α, normalization of MLCK and ZO-1 expressions [234] |
| Lactobacillus rhamnosus GG | Decrease | Caco-2 | Neutralize TNF-α/IFN-γ, restoration of ZO-1 distribution [235] |
| Decrease | T84 | Neutralize EHEC, restoration of ZO-1 expression and distribution [236] | |
| Lactobacillus rhamnosus GG (soluble proteins) | Decrease | Caco-2 | Neutralize hydrogen peroxide, restoration of occludin and ZO-1 distributions [238] |
| Bifidobacterium infantis Y1 (conditioned medium) | Decrease | T84 | ZO-1 ↑, occludin ↑, claudin-4 ↑, claudin-2 ↓ [240] |
| Decrease | T84 | Neutralize TNF-α/IFN-γ, restoration of occludin and claudin-1 distributions [240] | |
aPermeability is based on TER and the paracellular passage of molecules
bSymbols ↑ and ↓ indicate increases and decreases in the protein or mRNA expression, respectively. The symbol ↔ indicates alterations in the cellular distribution of the proteins
Amino acids and peptides
Among the many amino acids, glutamine (Gln) and tryptophan (Trp) have been reported to maintain, promote, and protect intestinal barrier function. Gln, one of the non-essential amino acids, is a primary energy source for intestinal epithelial cells. In vivo, the protective effects of Gln on the intestinal barrier have been shown in highly stressed patients [183] and rodents subjected to total parental nutrition [184–186]. In intestinal Caco-2 cells, exogenous Gln increases claudin-1, but not occludin or ZO-1, in the detergent-insoluble fraction of cells [187]. Further, Gln deprivation by a combination of Gln-free media and Gln synthase inhibition decreases TER and increases mannitol permeability [187]. The barrier impairment is caused by the perturbation of TJ protein (ZO-1, occludin and claudin-1) expression and distribution. The Gln deprivation-induced TER reduction is restored by PI3K inhibition or knockdown, indicating the involvement of the PI3K/Akt pathway [188]. Another research group demonstrates that Gln protects the intestinal TJ barrier from acetaldehyde, which is an oxidized metabolite of ethanol, in Caco-2 cells [189] and human intestinal biopsy specimens [190]. Pre-treatment of cells and intestinal tissues with Gln attenuates the acetaldehyde-induced redistribution of ZO-1 and occludin. The Gln-mediated protective effect requires EGF receptor activation.
A promotive effect of Trp on the intestinal barrier has been found in the analysis of intestinal contents of ovoalubumin-induced food allergy model mice [191]. Trp increases basal TER in Caco-2 cells in a dose-dependent manner; however, the underlying molecular mechanism for this increase is totally unknown [191].
Peptides derived from food proteins such as milk and cheese have been shown to suppress intestinal permeability [192–194]. A casein-derived octapeptide (Asn-Pro-Trp-Asp-Gln) increases both occludin expression and TER in Caco-2 cells [194].
Fatty acids
Long chain fatty acids (LCFAs) have roles as cell membrane components, cellular energy sources, and precursors of eicosanoids in our body, and contribute to cellular functions. The regulation of paracellular permeability by LCFAs, such as eicosapentaenoic, docosahexaenoic, and γ-linoleic acids (EPA, DHA and γ-LA), has been demonstrated in vitro, although the results are controversial. In intestinal Caco-2 cells, treatment with EPA, DHA, or γ-LA decreases TER and increases permeability to FITC-sulfonic acids [195, 196]. In contrast, EPA, DHA, arachidonic acid, γ-LA, and di-homo-γ-LA increase TER in T84 cells [197]. Except for γ-LA, these LCFAs attenuate IL-4-induced increases in dextran flux. Incorporation of these LCFA into epithelial membrane phospholipids has been observed, but the molecular mechanisms underlying their barrier regulation remain unclear.
Medium chain fatty acids (MCFAs) are less commonly found in nature and foods, but are relatively common in milk and coconut oil as triglyceride forms. It is not clear whether food-derived MCFAs affect intestinal permeability, but two MCFAs, capric (C10) and lauric (C12) acids, which are known drug absorption enhancers, increase paracellular permeability [198–200]. In Caco-2 cells, C10 and C12 rapidly decrease TER and increase mannitol flux. C10, but not C12, induces the redistribution of TJ proteins (occludin and ZO-1) and rearrangement of the actin cytoskeleton, indicating that the two MCFAs operate via different molecular mechanisms [199]. Both the C10- and C12-induced paracellular permeability requires intracellular Ca2+-dependent MLCK activation. C10, but not C12, mobilizes Ca2+ from the inositol 3-phosphate-sensitive intracellular Ca2+ store via phospholipase C activation.
The levels of short chain fatty acids (SCFAs), mainly acetic, propionic, and butyric acids (C4), are limited in foods, being mainly found in vinegar and fermented foods such as kimchi and cheese. In contrast, the intestinal microflora metabolizes undigested carbohydrates and produces a large amount of SCFAs in the large intestines. The production of SCFAs is important for normal intestinal biology such as energy salvage, cell proliferation, and barrier function [201, 202]. Some studies conclude that SCFAs regulate the intestinal barrier as a consequence of stimulated cell proliferation and differentiation [203, 204], but mechanisms independent from these stimulations have also been reported. Different research groups have consistently demonstrated that butyric acid enhances intestinal barrier integrity. Peng et al. [205] have reported that butyric acid increases basal TJ integrity and promotes Ca2+-induced TJ assembly, as indicated by TER and/or inulin flux, in intestinal Caco-2 cells. In Ca2+-induced TJ assembly, butyric acid facilitates ZO-1 and occludin localization at the intercellular junctions. The activation of AMP-activated protein kinase (AMPK) is involved in the butyric acid-mediated effect. The promotive effects of acetic and propionic acids on barrier integrity have also been shown. Acetic and propionic acids increase TER and decrease permeability to lucifer yellow in a dose-dependent manner in the rat colon and intestinal cells (Caco-2 and T84) [206]. The acetic acid-mediated increase in TER is suppressed by the pharmacological inhibition of PI3K and Gq protein [206]. Recently, two functional receptors for SCFAs, GPCR41, and 43, have been identified [207, 208]. GPCR43 is expressed in the colon [209, 210] and is associated with Gq and Gi/o proteins [208], although the implications of these associations for intestinal barrier regulation are unknown.
Vitamins
Vitamins are essential nutrients needed in small amounts for a variety of cellular functions. They are categorized into water- and fat-soluble groups. There have been very few reports on the roles of two fat-soluble vitamins, A and D, in intestinal barrier regulation. Vitamin A and D receptors belong to the nuclear receptor superfamily of steroid/thyroid hormone receptors [211, 212]. These receptors are expressed in most organs, including the intestinal epithelium, and transcriptionally regulate gene expressions. Retinol, an alcohol form of vitamin A, partially attenuates Clostridium difficile toxin A-induced decreases in TER in intestinal Caco-2 cells [213]; however, the underlying mechanism remains to be elucidated. The protective effect of vitamin D on the intestinal barrier has been seen in the observation that vitamin D receptor (VDR) knockout mice exhibit more severe colitis compared with wild-type mice [214]. In this colitis model using DSS, VDR knockout mice exhibit intestinal barrier defects, as indicated by TER and TJ protein (claudin-1 and occludin) expression, at an earlier phase than in the wild-type mice. In intestinal SW480 cells, vitamin D treatment enhances the expression of TJ (ZO-1, claudin-1 and claudin-2) and adherens junction (E-cadherin) proteins [214]. Further, vitamin D prevents DSS-induced decreases in TER across Caco-2 cells in a VDR-dependent manner [214].
Polyphenols
Polyphenols are secondary metabolites ubiquitously distributed throughout the plant kingdom. The major sources of polyphenols in the human diet are fruits, vegetables, and beverages such as tea and coffee. Polyphenols represent a vast group of compounds having aromatic ring(s), and are characterized by the presence of one or more hydroxyl groups of varying structural complexity. Based on their chemical structures, polyphenols are divided into a number of subgroups including flavonoids and curcuminoids. Recently, considerable attention has been given to the physiological effects of polyphenols, including their anti-oxidative, anti-inflammatory, and anti-carcinogenic effects [215, 216]. Information about their roles in intestinal barrier function is limited, but recent studies have demonstrated that some polyphenols (quercetin, kaempferol, myricetin, genistein, catechin, and curcumin) participate in barrier regulation. Quercetin, myricetin, and kaempferol are categorized into the flavonoid subgroup, flavonol, and enhance barrier integrity in intestinal Caco-2 cells [217–219]. Quercetin increases TER and decreases permeability to lucifer yellow, and the effect is involved in the transcriptional regulation of claudin-4 and the assembly of ZO-2, occludin and claudin-1 at the TJs [217, 219]. Direct inhibition of PKCδ by quercetin seems to be the proximal event in relation to barrier regulation [217]. The kaempferol-mediated promotion of TJ integrity is involved in the increases in the expression (ZO-2 and claudin-4) and redistribution (occludin, claudin-1 and claudin-3) of TJ proteins [218].
Genistein, curcumin, and epigallocatechin gallate protect the intestinal barrier against noxious stimuli such as acetaldehyde, oxidative stress, and cytokines. Genistein and curcumin activity result from their potential as inhibitors of tyrosine kinase and NFκB, respectively. In Caco-2 cells, oxidative stress and acetaldehyde separately disrupt the epithelial barrier in a tyrosine kinase-dependent manner [40, 43, 220]. Pretreatment of the cells with genistein inhibits the tyrosine phosphorylation of occludin and ZO-1 and their dissociation from the junctional complex, and protects barrier integrity against acetaldehyde and oxidative stress [40, 43, 220]. Curcumin protects the intestinal barrier from two proinflammatory cytokines, TNF-α and IL-1β. In Caco-2 cells, TNF-α and IL-1β separately impair the TJ barrier, as indicated by the increase in macromolecule flux and decrease in TER [104, 106, 116, 117]. These cytokines induce NF-κB-dependent MLCK expression and the phosphorylation of MLC, resulting in actin cytoskeletal contraction [106, 116, 117]. Pre-treatment of the cells with curcumin blocks cytokine-induced NF-κB activation and intestinal hyperpermeability [106, 116]. A green tea flavonoid, EGCG, also ameliorates the intestinal barrier dysfunction provoked by IFN-γ, as indicated by TER and macromolecule flux, in T84 cells, but the precise mechanism is unclear [221].
Probiotics
Probiotics are defined as “live microorganisms which when administered in adequate amounts confer a health benefit on the host” [222]. Accumulating evidence in basic sciences and clinical studies has indicated ameliorative and preventive effects of probiotics on systemic as well as intestinal disorders. To exert beneficial effects on the intestines, probiotics often regulate and improve microbial ecology, epithelial cell survival, immune function, and barrier function. Both in vivo and in vitro studies have demonstrated that probiotics protect the intestinal barrier from stress, infection, and cytokines.
E. coli Nissle1917 (ECN) is widely used as a probiotic in Europe. Ingestion of ECN restores hyperpermeability and the loss of ZO-1, an integral TJ protein, in the colons in an experimental mouse model of colitis [223, 224]. In intestinal T84 cells, treatment with ECN enhances basal TJ integrity, as indicated by TER [225]. Further, ECN inhibits EPEC-induced decreases in TER and the dissociation of ZO-2 from the intercellular junctions [225]. Activation of PKCζ is required for EPEC-induced barrier disruption, but ECN prevents PKCζ translocation to the intercellular regions.
Streptococcus thermophilus and Lactobacillus acidophilus separately increase basal TER in Caco-2 cells [226]. Further, the combination of two probiotics attenuates the barrier disruption induced by enteroinvasive E. coli in intestinal HT29/cl.19A cells [226]. The promotion and maintenance of phosphorylation in ZO-1 and occludin seem to be involved in the protective effects of the combined probiotics, although they did not alter TJ protein expression [226]. The combined probiotics also restore TNF-α- and IFN-γ-induced decreases in TER in HT29/cl.19A cells [227].
VSL#3, a probiotic formula, is a mixture of S. thermophilus, 4 Lactobacillus species, and 3 Bifidobacterium species, and is often used in clinical treatment. In the experimental mouse model of colitis induced by DSS, VSL#3 administration prevents hyperpermeability and inflammation in the colon [228]. This prevention is accompanied by normalization of the expression and localization of TJ proteins (ZO-1, occludin and claudins). In HT-29 cells, VSL#3 restores TNF-α-induced barrier impairment, as indicated by TER and TJ protein expression [229]. The protective effect of VSL#3 is mediated through the activation of the p38 MAPK and ERK signaling pathways.
Lactobacillus plantarum (L. plantarum) is a lactic acid bacterium used in fermented products, including sauerkrant, kimuchi, and pickles. Both in vivo and vitro studies have shown the protective effects of L. plantarum on the intestinal barrier. In IL-10 knockout mice, a mouse model of spontaneous colitis, the ingestion of L. plantarum improves TER and mannitol flux in the colon, accompanied with restoration of TJ protein (ZO-1, occludin, and claudin-1) expression [230]. In Caco-2 cells, L. plantarum prevents TNF-α- and phorbol ester-induced decreases in TER by suppressing the NF-κB signal pathway [231, 232]. Extracellular L. plantarum is recognized by the membrane surface toll-like receptor 2 (TLR2) and evokes protective signaling [232]. TLR2, a member of the TLR family, recognizes conserved molecular patterns associated with both gram-negative and -positive bacteria, including lipoproteins, peptidoglycans, lipoteichoic acid, and zymosan. TLR2 signaling is known to protect intestinal barrier integrity both in vivo and in vitro [233].
Lactobacillus rhamnosus (L. rhamnosus) is a gram-negative, lactic acid bacterium that was first isolated from healthy human stools. Studies demonstrate that different strains of L. rhamnosus have protective effects on the intestinal barrier. In the mouse model of DSS-induced colitis, ingestion of live or heat-killed L. rhamnosus OLL2838 ameliorates intestinal inflammation and barrier defects, as indicated by dextran permeability and ZO-1 expression [234]. The OLL2838 strain also prevents TNF-α induced decreases in TER in Caco-2 cells, accompanied with the normalization of ZO-1 and MLCK expression. Another strain, L. rhamnosus GG, protects the intestinal barrier against infection and cytokines in vitro. Costimulation by TNF-α and IFN-γ impairs barrier integrity in Caco-2 cells, as indicated by decreased TER and redistributed ZO-1 [235]. Pretreatment of the cells with L. rhamnosus GG inhibits these alterations. In addition, pretreatment with L. rhamnosus GG prevents EHEC-induced decreases in TER and decreases in or the redistribution of ZO-1 in T84 cells [236].
Interestingly, metabolites and secretion products from probiotics often exert protective effects on intestinal barrier function. Two soluble proteins, p40 and p70, from L. rhamnosus GG inhibit cytokine-induced apoptosis [237] and oxidative stress-induced barrier disruption [238]. In Caco-2 cells, the combination of p40 and p75 attenuates hydrogen oxide-induced barrier disruption, as indicated by TER and inulin flux, accompanied with normalization of TJ and AJ protein (ZO-1, occludin, E-cadherin, and β-catenin) distribution. This protective effect is mediated through the activation of the PKCβ/ε and ERK pathways. In mice, delivery of p40 to the colon using a hydrogel bead system ameliorates the DSS-induced intestinal barrier defect, indicated by dextran permeability and ZO-1 localization [239]. Interestingly, the p40-mediated ameliorative effect was not observed in EGF receptor-deficient mice, indicating the involvement of EGF receptor in the p40-mediated signal transduction. Similarly, secreted bioactive factors from Bifidobacterium infantis Y1, which is contained in VSL#3, exhibit protective and promotive effects on the intestinal barrier. The conditioned medium of B. infantis (BiCM) enhances basal TJ integrity in T84 cells, as indicated by TER and mannitol flux [240]. This enhancing effect of BiCM is accompanied by increases in ZO-1, occludin, and claudin-4 and a decrease in claudin-2. Further, BiCM prevents TNF-α- and IFN-γ-induced decreases in TER and the redistribution of TJ proteins (occludin and claudin-1). These effects of BiCM are mediated by the MEK/ERK signaling pathway. In addition, BiCM ingestion was found to attenuate colitis in IL-10 knockout mice [240], although intestinal permeability was not examined.
Alcohol and acetaldehyde
Alcohol and its oxidized metabolite, acetaldehyde, impair the intestinal barrier, and this impairment is involved in the development of ALD (see “Alcoholic liver disease”). In animal models, acute and chronic administrations of alcohol induce intestinal hyperpermeability [241–243]. However, the hyperpermeability observed in the duodenum and jejunum upon acute administration seems to result from histological injury induced by the high concentration of alcohol [243]. In intestinal Caco-2 cells, ethanol decreases TER and increases mannitol flux [244]. Immunofluorescence microscopy shows the ethanol-induced redistribution of TJ proteins, ZO-1 and occludin. Barrier impairment is caused by a MLCK-dependent mechanism.
Acetaldehyde accumulates in the large intestinal lumen upon alcohol drinking [245]. Exposure of the rat colon to acetaldehyde impairs barrier integrity, as indicated by TER and dextran permeability [242]. Studies using Caco-2 cells reveal that acetaldehyde induces barrier disruption via a tyrosine kinase-dependent mechanism [43, 246]. Acetaldehyde does not change the overall tyrosine kinase activity in cells, but effectively suppresses the PTP-1B, 1C, and 1D [43]. The acetaldehyde-induced suppression of PTP activity causes tyrosine phosphorylation of TJ and AJ proteins (ZO-1, occludin, E-cadherin, and β-catenin), and their dissociation from the respective TJ and AJ complexes, finally leading to increased paracellular permeability [43, 220].
Clinical implications of intestinal TJ regulation
As described above, the intestinal TJs provide a physical barrier against luminal noxious molecules such as pathogens, toxins, and allergens [8, 11]. Increased diffusion of these noxious molecules through the defective barrier can cause excessive activation of the immune system and inflammation. Therefore, barrier defects are closely associated with the pathogenesis of various intestinal and systemic inflammatory diseases. Although multiple factors are involved in disease pathogenesis, and barrier defects can be the consequence of disease development, evidence from basic science and clinical studies suggests that barrier defects can play roles in both the initiation and development of diseases. The final section describes the implications of intestinal TJ barrier defects for disease pathogenesis, focusing mainly on clinical data.
Inflammatory bowel disease
IBDs, including UC and CD, are chronic and relapsing-remitting inflammatory diseases. These diseases afflict millions of people throughout the world, and impair their daily functions and quality of life. Accumulating evidence from basic science and clinical studies suggests 3 essential factors for IBD pathogenesis: (1) disruption of the intestinal barrier, (2) exposure of the luminal content to mucosal immune cells, and (3) an abnormal immune response [10]. Although the factor responsible for initiating the disease has not been specified, some evidence suggests that intestinal barrier impairment can initiate IBD. For example, hyperpermeability is observed in the non-involved intestinal segments of IBD patients [247]. A subset of first-degree relatives of patients with CD has increased intestinal permeability despite being apparently healthy [248]. The possible mechanism underlying hyperpermeability in apparently healthy subjects is subclinical immune activation and cytokine secretion. Hyperpermeability resulting in the permeation of luminal bacterial products and antigens into the intestinal mucosa induces an abnormally robust inflammatory response. Further, the immune activation stimulates cytokine production from macrophages, T cells, and mast cells, leading to a substantial barrier defect. Clinical studies show that the levels of inflammatory cytokines, including TNF-α [100, 101], IFN-γ [94, 95], IL-1β [108, 112], IL-6 [108, 126], and IL-17 [143, 144], are elevated in the intestines of IBD patients. These cytokines are known to disturb intestinal barrier function as mentioned above (see “Intestinal TJ regulation by cytokines and growth factors”). In particular, TNF-α may have an important role in the initiation and development of intestinal barrier defects in IBD, because anti-TNF-α treatment suppresses the inflammatory response and improves intestinal permeability [249]. As a consequence of perturbation by multiple cytokines, the alterations to the intestinal TJ structures in IBD patients could be complicated. Clinical studies show decreased expression and redistribution of barrier-forming proteins (occludin, claudin-3, claudin-5, claudin-8, and JAM-A), and increased expression of pore-forming claudin-2 in CD patients [250, 251]. In UC patients, decreased expression and redistribution of occludin, claudin-1, claudin-4, tricellulin, and JAM-A, and increased claudin-2 expression are observed [139, 251]. In addition, MLCK expression and MLC phosphorylation are also observed in the intestines of both UC and CD patients, indicating cytoskeletal dysregulation of intestinal permeability [252].
Celiac disease
Celiac disease is an immune-mediated disorder of the small intestine, triggered by an inappropriate T cell-mediated response to gliadin found in the wheat protein, gluten. Although celiac disease pathogenesis is complicated and remains obscure, some evidence suggests that intestinal barrier defects have a role in initiating celiac disease. For example, a symptomatic patient on a gluten-free diet continues to display intestinal hyperpermeability [253, 254]. Many healthy first-degree relatives of patients also show hyperpermeability [255]. These observations suggest that intestinal hyperpermeability occurs prior to disease onset in celiac disease. Clinical and experimental studies indicate that gliadin induces intestinal barrier defects through the direct stimulation of epithelial cells and excessive activation of mucosal immune cells.
Recently, a functional gliadin receptor, CXCR3, has been identified, and evidence suggests its involvement in intestinal hyperpermeability and inflammation in celiac disease [256]. CXCR3 is expressed in both epithelial cells and the lamina propria of the human intestines, although the expression level in the lamina propria is higher than that in the epithelial cells [256]. The binding of gliadin to CXCR3 on the epithelial cells induces zonulin secretion in a MyD88-dependent manner. Zonulin is a human intestinal ZOT homolog [257, 258] and is known to disrupt epithelial barrier function via a mechanism similar to that of ZOT (see “Vibrio cholerae”). Clinical studies demonstrate that the expression of CXCR3 and zonulin in the intestinal mucosa of patients with celiac disease is highly elevated. Further, the treatment of intestinal biopsy specimens from celiac disease patients with gliadin induces zonulin release and barrier impairment [259]. Gliadin permeation through the lamina propria may be negligible under healthy conditions because of barrier integrity, but barrier impairment results in the substantial exposure of immune cells to gliadin. The binding of gliadin to CXCR3 expressed in T cells induces an inflammatory cascade and further increases intestinal permeability. Clinical studies show the downregulation of occludin and ZO-1 and upregulation of claudin-2 and -3 in the intestines of patients with celiac disease [259, 260]. On the other hand, inherited factors are also associated with celiac disease pathogenesis. Gene mapping in the human leukocyte antigen (HLA) region has identified genes encoding class II molecules DQ2 and DQ8 as key genetic risk factors in celiac disease [261]. However, it is unknown if the class II HLA genotype is associated with intestinal barrier function and gluten tolerance.
Type I diabetes
Type I diabetes (T1D) is characterized by the loss of insulin-producing β-cells from the islets of Langerhans in the pancreas resulting in insulin deficiency. T1D is an autoimmune disorder and the loss of the β-cells occurs through a T cell-mediated autoimmune attack. It is believed that genetically predisposed individuals develop T1D after encountering one or more environmental factors associated with the disease. In 1986, Mooradian et al. [262] first reported the increased intestinal permeability in diabetic patients. The interplay between increased intestinal permeability and the initiation of T1D is still unclear, but evidence from experimental and clinical studies indicates that intestinal barrier defects have a role in T1D pathogenesis.
In a clinical study, intestinal permeability was examined in diabetic patients at different disease stages [263, 264]. All diabetic groups showed increased permeability, but notably the prediabetic group exhibited the greatest increase, indicating that increased permeability occurs prior to disease onset and that the increased exposure to luminal antigens leads to the autoimmune distraction of β-cells. Further, elevated TNF-α and IFN-γ levels were observed in small intestinal biopsy specimens from T1D patients, indicating an intestinal inflammatory response [265].
Similar to in celiac disease, the gliadin-zonulin axis possibly plays a role in the intestinal barrier defects in T1D [266, 267]. In a study using biobreeding diabetes-prone (BBDP) rats, elevated zonulin levels in the sera and intestinal contents were coincident with hyperpermeability in the small intestines [266]. These alterations precede the production of autoantibodies against pancreatic β-cells and the elevation of blood glucose levels. Importantly, a zonulin inhibitor is known to suppress intestinal hyperpermeability and the development of diabetes in the BBDP rats [266]. In clinical studies, T1D patients and their relatives exhibit elevated serum levels of zonulin, which is correlated with intestinal permeability [268].
Alcoholic liver disease
ALD is a disorder that encompasses many hepatic manifestations of alcohol overconsumption including hepatic steatosis, hepatitis, chronic hepatitis with hepatic fibrosis, and cirrhosis. Although hepatic steatosis develops in all individuals who consume a large amount of alcohol beverages for a long period of time, this process is transient and reversible. Of all chronic heavy drinkers, only 15–20 % develop hepatitis or cirrhosis, which can occur concomitantly or in succession. A striking observation is that endotoxemia and endotoxin-mediated alteration of the liver cell functions plays a crucial role in the pathogenesis of ALD [269]. Indeed, high levels of endotoxin are observed in the serum of alcoholics [270, 271] and alcohol-fed animals [241]. In animal models, a significant correlation is known to exist between endotoxin levels and the severity of alcohol-induced liver damage [272, 273]. Further, treatment with antibiotics or lactobacillus species that lower blood endotoxin levels suppresses the liver damage in alcohol-fed rats [274, 275]. Endotoxins derived from luminal bacteria are highly immunogenic and induce the production of proinflammatory cytokines such as IL-1β and TNF-α in liver cells, suggesting that endotoxins from luminal bacteria induce liver inflammation leading to hepatitis and cirrhosis in ALD. One postulated mechanism of the endotoxemia observed in ALD patients is intestinal barrier defects, although bacterial overgrowth in the intestines could also increase the penetration of endotoxins [276]. A clinical study showed that intestinal permeability to macromolecules with a comparable molecular size to that of endotoxins was higher in alcoholics than in normal subjects [277]. Further, alcohol administration increases intestinal permeability in both the normal subjects and ALD patients [278].
Possible candidates for the induction of intestinal barrier impairment after alcohol consumption are ethanol and its oxidized metabolite, acetaldehyde. Acetaldehyde is produced from ethanol in the large intestines by alcohol dehydrogenase in the mucosa and luminal bacteria, while the capacity of the colonic mucosa and microbes to oxidize acetaldehyde to acetate is low compared to that of other tissues. Therefore, a considerable amount of acetaldehyde could be accumulated in the colon after alcohol consumption. A study by Visapää et al. [245] demonstrated that the intracolonic acetaldehyde level in rats after alcohol consumption may reach as high as 3 mM. The dysregulation of intestinal barrier function by ethanol and acetaldehyde are described in “Alcohol and acetaldehyde.” Collectively, the endotoxemia resulting from the intestinal barrier defects induced by ethanol and acetaldehyde is closely associated with ALD pathogenesis.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a disorder most commonly characterized by cramping, abdominal pain, bloating, constipation, and diarrhea, but the symptoms vary among the patients. IBS has been regarded as a disorder of the psychological sphere associated with gut motor abnormalities and increased sensory perception. However, recent studies suggest that mucosal inflammation, which is linked to enhanced exposure of mucosal immune cells to antigens because of increased intestinal permeability, also participates in the initiation and development of IBS [279]. In IBS patients, the intestinal mucosa appears normal at endoscopic or conventional histologic examination, but contains a greater number of immune cells, including mast cells and T cells, indicating increased cytokine production and inflammation [280, 281]. In a clinical study, paracellular permeability was found to be increased in the colonic biopsies of IBS patients compared to that in healthy subjects [282]. The hyperpermeability is accompanied with decreased ZO-1 expression [282]. According to evidence from clinical and experimental studies, the barrier impairment in IBS patients is possibly caused by psychological and environmental stress. In a clinical study, jejunal permeability was examined by intestinal albumin output in healthy subjects experiencing low and moderate stress [283]. The moderate stress group showed higher permeability than did the low stress group, and, furthermore, additional cold stress increased permeability in both groups [283]. In animal studies, rodents exposed to different stresses showed increased intestinal permeability, coincidently with the disturbance of TJ structures [284–286]. One possible mechanism for stress-induced hyperpermeability is the activation of mucosal immune cells, particularly mast cells. The mast cells release a variety of inflammatory substances such as TNF-α, IL-4, IL-6, IL-13, and proteases, which have been shown to impair intestinal barrier function (see “Intestinal TJ regulation by cytokines and growth factors”). In human subjects, elevated release of mast cell mediators, such as tryptase and histamine, occurs in response to cold stress [283]. An animal study demonstrated that stress-induced intestinal hyperpermeability was not caused in mast cell-deficient rats [286]. Interestingly, higher serine protease activity is observed in the luminal contents of diarhhetic IBS patients, and this activity increases paracellular permeability in the mouse colon and Caco-2 cells [282].
Food allergies
Prior exposure to a food antigen by the oral route generates a regulatory T cell response that can suppress allergic sensitization to the food antigen. Food allergies are defined as an immunologically mediated adverse reaction to foods and are caused by food tolerance dysfunction. The development of a food allergy is dependent on exposure of the food antigens to mucosal immune cells, which leads to antigen sensitization and production of antigen-specific CD4+ Th2 cells and IgE [287]. Therefore, intestinal barrier defects have a role in the initiation and development of food allergies. A clinical study examined intestinal permeability in food allergic patients who had been on an allergen-free diets for at least 6 month [288]. Notably, the increase in intestinal permeability remained in the patients, indicating that increased permeability is not simply a consequence of the allergic reaction. In contrast, a similar study was conducted in patients after an allergen challenge [288, 289]. The increased permeability in response to the allergen was correlated with the severity of the clinical symptoms, suggesting the involvement of intestinal permeability in allergy development. The mechanism for hyperpermeability in the absence of antigens is obscure, but the hyperpermeability during the allergic reaction is possibly mediated by mast cells. In a mouse model of an oral ovoalubumin-induced food allergy, intestinal hyperpermeability was observed after an allergen challenge and was accompanied with marked mucosal mast cell degranulation, but no hyperpermeability was observed in mast cell-depleted mice [290], indicating that the mediators secreted from the mucosal mast cells increase intestinal hyperpermeability. In the patients with food allergies, mast cells induce degranulation and release a variety of inflammatory mediators in response to the food antigens [291]. At the very least it has been shown that inflammatory mediators, such as TNF-α, IL-4, IL-6, IL-13, and tryptases, released from mast cells on activation impair intestinal barrier integrity (see "Intestinal TJ regulation by cytokines and growth factors").
Concluding remarks
Intestinal TJ structures are organized by multiple integral proteins and signaling molecules. Clinical and experimental studies demonstrate that defects in the intestinal TJ barrier and increased permeability are observed in various intestinal and systemic diseases. Although barrier defects may be caused as a consequence of the disease development, recent studies have suggested that increased intestinal permeability resulting in excessive activation of mucosal immune cells, and inflammation could play a role in initiating and also developing diseases. In this regard, the intestinal TJ barrier is dynamically regulated by physiological and pathophysiological factors, including cytokines, pathogens, and food factors. Understanding the molecular mechanisms underlying TJ regulation by the extracellular factors will lead to the development of effective therapeutic and preventive approaches against diseases associated with intestinal barrier defects. Further, understanding of the precise associations between the TJ barrier and the innate and adaptive immune systems will help us clarify disease pathogenesis.
Acknowledgments
This work was supported by Japan Society for the Promotion of Science, a Grant-in-Aid for Young Scientists (B) 23780135 to T. Suzuki.
Abbreviations
- AJ
Adherens junction
- ALD
Alcoholic liver disease
- AMPK
AMP activated protein kinase
- BBDP
Biobreeding diabetes-prone
- BiCM
Conditioned medium of Bifidobacterium infantis
- BT-IgSF
Brain- and testis-specific immunoglobulin superfamily
- C10
Capric acid
- C12
Lauric acid
- CAR
Coxsacki and adenovirus receptor
- CD
Crohn’s disease
- CHO
Chinese hamster ovary
- CPE
Clostridium perfringen enterotoxin
- DHA
Docosahexaenoic acid
- DSS
Dextran sodium sulfate
- ECN
Escherichia coli Nissle1917
- EGF
Epidermal growth factor
- EHEC
Enterohemorrhagic Escherichia coli
- EPA
Eicosapentaenoic acid
- EPEC
Enteropathogenic Escherichia coli
- ERK
Extracellular signal-regulated kinase
- ESAM
Endothelial selective adhesion molecule
- EspF
Escherichia coli secreted protein F
- GPCR
G-protein-coupled receptor
- HA/P
Hemagglutinin/protease
- HS/R
Hemorrhagic shock and resuscitation
- IBD
Inflammatory bowel disease
- IBS
Irritative bowel syndrome
- IFN
Interferon
- Ig
Immunoglobulin
- IL
Interleukin
- JAM
Junctional adhesion molecule
- LA
Linolec acid
- LCFA
Long chain fatty acid
- LIGHT
Lymphotoxin-like inducible protein
- L. plantarum
Lactobacillus plantarum
- L. rhamnosus
Lactobacillus rhamnosus
- MAGUK
Membrane-associated guanylate kinase homolog
- MAP
Mitochondrial-associated protein
- MCFA
Medium chain fatty acid
- MEK
Mitogen-activated protein kinase
- MLC
Myosin light chain
- MLCK
Myosin light chain kinase
- NFκB
Nuclear factor-κB
- PAR
Proteinase activated receptor
- PDZ
Post-synaptic density 95/Drosophila discs large/zona-occludens 1
- PI3K
Phosphatidyl inositol-3 kinase
- PK
Protein kinase
- PKA
cAMP-dependent kinase
- PP
Protein phosphatase
- PPAR
Peroxisome proliferator-activated receptor
- PTP
Protein tyrosine phosphatase
- ROCK
Rho-associated kinase
- SCFA
Short chain fatty acid
- SH
Src homology
- T1D
Type I diabetes
- TER
Transepithelial electrical resistance
- TGF
Transforming growth factor
- TJ
Tight junction
- TLR
Toll-like receptor
- TNF
Tumor necrosis factor
- TNFR
TNF-α receptor
- TPN
Total parenteral nutrition
- VDR
Vitamin D receptor
- ZO
Zonula occludens
- ZOT
Zonula occludens toxin
References
- 1.Ferraris RP, Diamond J. Regulation of intestinal sugar transport. Physiol Rev. 1997;77:257–302. doi: 10.1152/physrev.1997.77.1.257. [DOI] [PubMed] [Google Scholar]
- 2.Broer S. Amino acid transport across mammalian intestinal and renal epithelia. Physiol Rev. 2008;88:249–286. doi: 10.1152/physrev.00018.2006. [DOI] [PubMed] [Google Scholar]
- 3.Kiela PR, Ghishan FK. Ion transport in the intestine. Curr Opin Gastroenterol. 2009;25:87–91. doi: 10.1097/MOG.0b013e3283260900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsukita S, Furuse M, Itoh M. Multifunctional strands in tight junctions. Nat Rev Mol Cell Biol. 2001;2:285–293. doi: 10.1038/35067088. [DOI] [PubMed] [Google Scholar]
- 5.Van Itallie CM, Anderson JM. Claudins and epithelial paracellular transport. Annu Rev Physiol. 2006;68:403–429. doi: 10.1146/annurev.physiol.68.040104.131404. [DOI] [PubMed] [Google Scholar]
- 6.Oda H, Takeichi M. Evolution: structural and functional diversity of cadherin at the adherens junction. J Cell Biol. 2011;193:1137–1146. doi: 10.1083/jcb.201008173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baum B, Georgiou M. Dynamics of adherens junctions in epithelial establishment, maintenance, and remodeling. J Cell Biol. 2011;192:907–917. doi: 10.1083/jcb.201009141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9:799–809. doi: 10.1038/nri2653. [DOI] [PubMed] [Google Scholar]
- 9.Nusrat A, Turner JR, Madara JL. Molecular physiology and pathophysiology of tight junctions. IV. Regulation of tight junctions by extracellular stimuli: nutrients, cytokines, and immune cells. Am J Physiol Gastrointest Liver Physiol. 2000;279:G851–G857. doi: 10.1152/ajpgi.2000.279.5.G851. [DOI] [PubMed] [Google Scholar]
- 10.Clayburgh DR, Shen L, Turner JR. A porous defense: the leaky epithelial barrier in intestinal disease. Lab Invest. 2004;84:282–291. doi: 10.1038/labinvest.3700050. [DOI] [PubMed] [Google Scholar]
- 11.Farhadi A, Banan A, Fields J, Keshavarzian A. Intestinal barrier: an interface between health and disease. J Gastroenterol Hepatol. 2003;18:479–497. doi: 10.1046/j.1440-1746.2003.03032.x. [DOI] [PubMed] [Google Scholar]
- 12.Capaldo CT, Nusrat A. Cytokine regulation of tight junctions. Biochim Biophys Acta. 2009;1788:864–871. doi: 10.1016/j.bbamem.2008.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amasheh M, Andres S, Amasheh S, Fromm M, Schulzke JD. Barrier effects of nutritional factors. Ann N Y Acad Sci. 2009;1165:267–273. doi: 10.1111/j.1749-6632.2009.04063.x. [DOI] [PubMed] [Google Scholar]
- 14.Mullin JM, Skrovanek SM, Valenzano MC. Modification of tight junction structure and permeability by nutritional means. Ann N Y Acad Sci. 2009;1165:99–112. doi: 10.1111/j.1749-6632.2009.04028.x. [DOI] [PubMed] [Google Scholar]
- 15.Furuse M, Hirase T, Itoh M, Nagafuchi A, Yonemura S, Tsukita S. Occludin: a novel integral membrane protein localizing at tight junctions. J Cell Biol. 1993;123:1777–1788. doi: 10.1083/jcb.123.6.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Furuse M, Fujita K, Hiiragi T, Fujimoto K, Tsukita S. Claudin-1 and -2: novel integral membrane proteins localizing at tight junctions with no sequence similarity to occludin. J Cell Biol. 1998;141:1539–1550. doi: 10.1083/jcb.141.7.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin-Padura I, Lostaglio S, Schneemann M, Williams L, Romano M, Fruscella P, Panzeri C, Stoppacciaro A, Ruco L, Villa A, Simmons D, Dejana E. Junctional adhesion molecule, a novel member of the immunoglobulin superfamily that distributes at intercellular junctions and modulates monocyte transmigration. J Cell Biol. 1998;142:117–127. doi: 10.1083/jcb.142.1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ikenouchi J, Furuse M, Furuse K, Sasaki H, Tsukita S. Tricellulin constitutes a novel barrier at tricellular contacts of epithelial cells. J Cell Biol. 2005;171:939–945. doi: 10.1083/jcb.200510043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gonzalez-Mariscal L, Betanzos A, Nava P, Jaramillo BE. Tight junction proteins. Prog Biophys Mol Biol. 2003;81:1–44. doi: 10.1016/S0079-6107(02)00037-8. [DOI] [PubMed] [Google Scholar]
- 20.Madara JL, Moore R, Carlson S. Alteration of intestinal tight junction structure and permeability by cytoskeletal contraction. Am J Physiol. 1987;253:C854–C861. doi: 10.1152/ajpcell.1987.253.6.C854. [DOI] [PubMed] [Google Scholar]
- 21.Turner JR, Rill BK, Carlson SL, Carnes D, Kerner R, Mrsny RJ, Madara JL. Physiological regulation of epithelial tight junctions is associated with myosin light-chain phosphorylation. Am J Physiol. 1997;273:C1378–C1385. doi: 10.1152/ajpcell.1997.273.4.C1378. [DOI] [PubMed] [Google Scholar]
- 22.Walsh SV, Hopkins AM, Chen J, Narumiya S, Parkos CA, Nusrat A. Rho kinase regulates tight junction function and is necessary for tight junction assembly in polarized intestinal epithelia. Gastroenterology. 2001;121:566–579. doi: 10.1053/gast.2001.27060. [DOI] [PubMed] [Google Scholar]
- 23.Al-Sadi R, Khatib K, Guo S, Ye D, Youssef M, Ma T. Occludin regulates macromolecule flux across the intestinal epithelial tight junction barrier. Am J Physiol Gastrointest Liver Physiol. 2011;300:G1054–G1064. doi: 10.1152/ajpgi.00055.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Furuse M, Itoh M, Hirase T, Nagafuchi A, Yonemura S, Tsukita S. Direct association of occludin with ZO-1 and its possible involvement in the localization of occludin at tight junctions. J Cell Biol. 1994;127:1617–1626. doi: 10.1083/jcb.127.6.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong V, Gumbiner BM. A synthetic peptide corresponding to the extracellular domain of occludin perturbs the tight junction permeability barrier. J Cell Biol. 1997;136:399–409. doi: 10.1083/jcb.136.2.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saitou M, Fujimoto K, Doi Y, Itoh M, Fujimoto T, Furuse M, Takano H, Noda T, Tsukita S. Occludin-deficient embryonic stem cells can differentiate into polarized epithelial cells bearing tight junctions. J Cell Biol. 1998;141:397–408. doi: 10.1083/jcb.141.2.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schulzke JD, Gitter AH, Mankertz J, Spiegel S, Seidler U, Amasheh S, Saitou M, Tsukita S, Fromm M. Epithelial transport and barrier function in occludin-deficient mice. Biochim Biophys Acta. 2005;1669:34–42. doi: 10.1016/j.bbamem.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Saitou M, Furuse M, Sasaki H, Schulzke JD, Fromm M, Takano H, Noda T, Tsukita S. Complex phenotype of mice lacking occludin, a component of tight junction strands. Mol Biol Cell. 2000;11:4131–4142. doi: 10.1091/mbc.11.12.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakakibara A, Furuse M, Saitou M, Ando-Akatsuka Y, Tsukita S. Possible involvement of phosphorylation of occludin in tight junction formation. J Cell Biol. 1997;137:1393–1401. doi: 10.1083/jcb.137.6.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rao R. Occludin phosphorylation in regulation of epithelial tight junctions. Ann N Y Acad Sci. 2009;1165:62–68. doi: 10.1111/j.1749-6632.2009.04054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain S, Suzuki T, Seth A, Samak G, Rao R. Protein kinase Czeta phosphorylates occludin and promotes assembly of epithelial tight junctions. Biochem J. 2011;437:289–299. doi: 10.1042/BJ20110587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suzuki T, Elias BC, Seth A, Shen L, Turner JR, Giorgianni F, Desiderio D, Guntaka R, Rao R. PKC eta regulates occludin phosphorylation and epithelial tight junction integrity. Proc Natl Acad Sci USA. 2009;106:61–66. doi: 10.1073/pnas.0802741106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dorfel MJ, Westphal JK, Huber O. Differential phosphorylation of occludin and tricellulin by CK2 and CK1. Ann N Y Acad Sci. 2009;1165:69–73. doi: 10.1111/j.1749-6632.2009.04043.x. [DOI] [PubMed] [Google Scholar]
- 34.McKenzie JA, Riento K, Ridley AJ. Casein kinase I epsilon associates with and phosphorylates the tight junction protein occludin. FEBS Lett. 2006;580:2388–2394. doi: 10.1016/j.febslet.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 35.Smales C, Ellis M, Baumber R, Hussain N, Desmond H, Staddon JM. Occludin phosphorylation: identification of an occludin kinase in brain and cell extracts as CK2. FEBS Lett. 2003;545:161–166. doi: 10.1016/S0014-5793(03)00525-8. [DOI] [PubMed] [Google Scholar]
- 36.Wong V. Phosphorylation of occludin correlates with occludin localization and function at the tight junction. Am J Physiol. 1997;273:C1859–C1867. doi: 10.1152/ajpcell.1997.273.6.C1859. [DOI] [PubMed] [Google Scholar]
- 37.Seth A, Sheth P, Elias BC, Rao R. Protein phosphatases 2A and 1 interact with occludin and negatively regulate the assembly of tight junctions in the CACO-2 cell monolayer. J Biol Chem. 2007;282:11487–11498. doi: 10.1074/jbc.M610597200. [DOI] [PubMed] [Google Scholar]
- 38.Nunbhakdi-Craig V, Machleidt T, Ogris E, Bellotto D, White CL, 3rd, Sontag E. Protein phosphatase 2A associates with and regulates atypical PKC and the epithelial tight junction complex. J Cell Biol. 2002;158:967–978. doi: 10.1083/jcb.200206114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elias BC, Suzuki T, Seth A, Giorgianni F, Kale G, Shen L, Turner JR, Naren A, Desiderio DM, Rao R. Phosphorylation of Y398 and Y402 in occludin prevents its interaction with ZO-1 and destabilizes its assembly at the tight junctions. J Biol Chem. 2008;284:1559–1569. doi: 10.1074/jbc.M804783200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rao RK, Basuroy S, Rao VU, Karnaky KJ, Jr, Gupta A. Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem J. 2002;368:471–481. doi: 10.1042/BJ20011804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kale G, Naren AP, Sheth P, Rao RK. Tyrosine phosphorylation of occludin attenuates its interactions with ZO-1, ZO-2, and ZO-3. Biochem Biophys Res Commun. 2003;302:324–329. doi: 10.1016/S0006-291X(03)00167-0. [DOI] [PubMed] [Google Scholar]
- 42.Suzuki T, Seth A, Rao R. Role of phospholipase Cgamma-induced activation of protein kinase Cepsilon (PKCepsilon) and PKCbetaI in epidermal growth factor-mediated protection of tight junctions from acetaldehyde in Caco-2 cell monolayers. J Biol Chem. 2008;283:3574–3583. doi: 10.1074/jbc.M709141200. [DOI] [PubMed] [Google Scholar]
- 43.Atkinson KJ, Rao RK. Role of protein tyrosine phosphorylation in acetaldehyde-induced disruption of epithelial tight junctions. Am J Physiol Gastrointest Liver Physiol. 2001;280:G1280–G1288. doi: 10.1152/ajpgi.2001.280.6.G1280. [DOI] [PubMed] [Google Scholar]
- 44.Tsukita S, Furuse M. Pores in the wall: claudins constitute tight junction strands containing aqueous pores. J Cell Biol. 2000;149:13–16. doi: 10.1083/jcb.149.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Furuse M, Hata M, Furuse K, Yoshida Y, Haratake A, Sugitani Y, Noda T, Kubo A, Tsukita S. Claudin-based tight junctions are crucial for the mammalian epidermal barrier: a lesson from claudin-1-deficient mice. J Cell Biol. 2002;156:1099–1111. doi: 10.1083/jcb.200110122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamura A, Hayashi H, Imasato M, Yamazaki Y, Hagiwara A, Wada M, Noda T, Watanabe M, Suzuki Y, Tsukita S. Loss of claudin-15, but not claudin-2, causes Na+ deficiency and glucose malabsorption in mouse small intestine. Gastroenterology. 2011;140:913–923. doi: 10.1053/j.gastro.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 47.Miyamoto T, Morita K, Takemoto D, Takeuchi K, Kitano Y, Miyakawa T, Nakayama K, Okamura Y, Sasaki H, Miyachi Y, Furuse M, Tsukita S. Tight junctions in Schwann cells of peripheral myelinated axons: a lesson from claudin-19-deficient mice. J Cell Biol. 2005;169:527–538. doi: 10.1083/jcb.200501154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weber S, Hoffmann K, Jeck N, Saar K, Boeswald M, Kuwertz-Broeking E, Meij II, Knoers NV, Cochat P, Sulakova T, Bonzel KE, Soergel M, Manz F, Schaerer K, Seyberth HW, Reis A, Konrad M. Familial hypomagnesaemia with hypercalciuria and nephrocalcinosis maps to chromosome 3q27 and is associated with mutations in the PCLN-1 gene. Eur J Hum Genet. 2000;8:414–422. doi: 10.1038/sj.ejhg.5200475. [DOI] [PubMed] [Google Scholar]
- 49.Gow A, Southwood CM, Li JS, Pariali M, Riordan GP, Brodie SE, Danias J, Bronstein JM, Kachar B, Lazzarini RA. CNS myelin and sertoli cell tight junction strands are absent in Osp/claudin-11 null mice. Cell. 1999;99:649–659. doi: 10.1016/S0092-8674(00)81553-6. [DOI] [PubMed] [Google Scholar]
- 50.Morita K, Sasaki H, Furuse M, Tsukita S. Endothelial claudin: claudin-5/TMVCF constitutes tight junction strands in endothelial cells. J Cell Biol. 1999;147:185–194. doi: 10.1083/jcb.147.1.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holmes JL, Van Itallie CM, Rasmussen JE, Anderson JM. Claudin profiling in the mouse during postnatal intestinal development and along the gastrointestinal tract reveals complex expression patterns. In. Gene expr patterns. 2006;6:581–588. doi: 10.1016/j.modgep.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 52.Inai T, Kobayashi J, Shibata Y. Claudin-1 contributes to the epithelial barrier function in MDCK cells. Eur J Cell Biol. 1999;78:849–855. doi: 10.1016/S0171-9335(99)80086-7. [DOI] [PubMed] [Google Scholar]
- 53.Amasheh S, Meiri N, Gitter AH, Schoneberg T, Mankertz J, Schulzke JD, Fromm M. Claudin-2 expression induces cation-selective channels in tight junctions of epithelial cells. J Cell Sci. 2002;115:4969–4976. doi: 10.1242/jcs.00165. [DOI] [PubMed] [Google Scholar]
- 54.Colegio OR, Van Itallie CM, McCrea HJ, Rahner C, Anderson JM. Claudins create charge-selective channels in the paracellular pathway between epithelial cells. Am J Physiol Cell Physiol. 2002;283:C142–C147. doi: 10.1152/ajpcell.00038.2002. [DOI] [PubMed] [Google Scholar]
- 55.Hou J, Gomes AS, Paul DL, Goodenough DA. Study of claudin function by RNA interference. J Biol Chem. 2006;281:36117–36123. doi: 10.1074/jbc.M608853200. [DOI] [PubMed] [Google Scholar]
- 56.Milatz S, Krug SM, Rosenthal R, Gunzel D, Muller D, Schulzke JD, Amasheh S, Fromm M. Claudin-3 acts as a sealing component of the tight junction for ions of either charge and uncharged solutes. Biochim Biophys Acta. 2010;1798:2048–2057. doi: 10.1016/j.bbamem.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 57.Yu AS, Enck AH, Lencer WI, Schneeberger EE. Claudin-8 expression in Madin–Darby canine kidney cells augments the paracellular barrier to cation permeation. J Biol Chem. 2003;278:17350–17359. doi: 10.1074/jbc.M213286200. [DOI] [PubMed] [Google Scholar]
- 58.Alexandre MD, Jeansonne BG, Renegar RH, Tatum R, Chen YH. The first extracellular domain of claudin-7 affects paracellular Cl- permeability. Biochem Biophys Res Commun. 2007;357:87–91. doi: 10.1016/j.bbrc.2007.03.078. [DOI] [PubMed] [Google Scholar]
- 59.Amasheh S, Schmidt T, Mahn M, Florian P, Mankertz J, Tavalali S, Gitter AH, Schulzke JD, Fromm M. Contribution of claudin-5 to barrier properties in tight junctions of epithelial cells. Cell Tissue Res. 2005;321:89–96. doi: 10.1007/s00441-005-1101-0. [DOI] [PubMed] [Google Scholar]
- 60.Van Itallie C, Rahner C, Anderson JM. Regulated expression of claudin-4 decreases paracellular conductance through a selective decrease in sodium permeability. J Clin Invest. 2001;107:1319–1327. doi: 10.1172/JCI12464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Krause G, Winkler L, Piehl C, Blasig I, Piontek J, Muller SL. Structure and function of extracellular claudin domains. Ann N Y Acad Sci. 2009;1165:34–43. doi: 10.1111/j.1749-6632.2009.04057.x. [DOI] [PubMed] [Google Scholar]
- 62.Fujita H, Chiba H, Yokozaki H, Sakai N, Sugimoto K, Wada T, Kojima T, Yamashita T, Sawada N. Differential expression and subcellular localization of claudin-7, -8, -12, -13, and -15 along the mouse intestine. J Histochem Cytochem. 2006;54:933–944. doi: 10.1369/jhc.6A6944.2006. [DOI] [PubMed] [Google Scholar]
- 63.Fujibe M, Chiba H, Kojima T, Soma T, Wada T, Yamashita T, Sawada N. Thr203 of claudin-1, a putative phosphorylation site for MAP kinase, is required to promote the barrier function of tight junctions. Exp Cell Res. 2004;295:36–47. doi: 10.1016/j.yexcr.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 64.Soma T, Chiba H, Kato-Mori Y, Wada T, Yamashita T, Kojima T, Sawada N. Thr(207) of claudin-5 is involved in size-selective loosening of the endothelial barrier by cyclic AMP. Exp Cell Res. 2004;300:202–212. doi: 10.1016/j.yexcr.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 65.D’Souza T, Agarwal R, Morin PJ. Phosphorylation of claudin-3 at threonine 192 by cAMP-dependent protein kinase regulates tight junction barrier function in ovarian cancer cells. J Biol Chem. 2005;280:26233–26240. doi: 10.1074/jbc.M502003200. [DOI] [PubMed] [Google Scholar]
- 66.Tanaka M, Kamata R, Sakai R. EphA2 phosphorylates the cytoplasmic tail of claudin-4 and mediates paracellular permeability. J Biol Chem. 2005;280:42375–42382. doi: 10.1074/jbc.M503786200. [DOI] [PubMed] [Google Scholar]
- 67.Van Itallie CM, Gambling TM, Carson JL, Anderson JM. Palmitoylation of claudins is required for efficient tight-junction localization. J Cell Sci. 2005;118:1427–1436. doi: 10.1242/jcs.01735. [DOI] [PubMed] [Google Scholar]
- 68.Cunningham SA, Arrate MP, Rodriguez JM, Bjercke RJ, Vanderslice P, Morris AP, Brock TA. A novel protein with homology to the junctional adhesion molecule. Characterization of leukocyte interactions. J Biol Chem. 2000;275:34750–34756. doi: 10.1074/jbc.M002718200. [DOI] [PubMed] [Google Scholar]
- 69.Arrate MP, Rodriguez JM, Tran TM, Brock TA, Cunningham SA. Cloning of human junctional adhesion molecule 3 (JAM3) and its identification as the JAM2 counter-receptor. J Biol Chem. 2001;276:45826–45832. doi: 10.1074/jbc.M105972200. [DOI] [PubMed] [Google Scholar]
- 70.Hirabayashi S, Tajima M, Yao I, Nishimura W, Mori H, Hata Y. JAM4, a junctional cell adhesion molecule interacting with a tight junction protein, MAGI-1. Mol Cell Biol. 2003;23:4267–4282. doi: 10.1128/MCB.23.12.4267-4282.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bergelson JM, Cunningham JA, Droguett G, Kurt-Jones EA, Krithivas A, Hong JS, Horwitz MS, Crowell RL, Finberg RW. Isolation of a common receptor for Coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275:1320–1323. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 72.Hirata K, Ishida T, Penta K, Rezaee M, Yang E, Wohlgemuth J, Quertermous T. Cloning of an immunoglobulin family adhesion molecule selectively expressed by endothelial cells. J Biol Chem. 2001;276:16223–16231. doi: 10.1074/jbc.M100630200. [DOI] [PubMed] [Google Scholar]
- 73.Suzu S, Hayashi Y, Harumi T, Nomaguchi K, Yamada M, Hayasawa H, Motoyoshi K. Molecular cloning of a novel immunoglobulin superfamily gene preferentially expressed by brain and testis. Biochem Biophys Res Commun. 2002;296:1215–1221. doi: 10.1016/S0006-291X(02)02025-9. [DOI] [PubMed] [Google Scholar]
- 74.Bazzoni G. The JAM family of junctional adhesion molecules. Curr Opin Cell Biol. 2003;15:525–530. doi: 10.1016/S0955-0674(03)00104-2. [DOI] [PubMed] [Google Scholar]
- 75.Liu Y, Nusrat A, Schnell FJ, Reaves TA, Walsh S, Pochet M, Parkos CA. Human junction adhesion molecule regulates tight junction resealing in epithelia. J Cell Sci. 2000;113(Pt 13):2363–2374. doi: 10.1242/jcs.113.13.2363. [DOI] [PubMed] [Google Scholar]
- 76.Laukoetter MG, Nava P, Lee WY, Severson EA, Capaldo CT, Babbin BA, Williams IR, Koval M, Peatman E, Campbell JA, Dermody TS, Nusrat A, Parkos CA. JAM-A regulates permeability and inflammation in the intestine in vivo. J Exp Med. 2007;204:3067–3076. doi: 10.1084/jem.20071416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cohen CJ, Shieh JT, Pickles RJ, Okegawa T, Hsieh JT, Bergelson JM. The coxsackievirus and adenovirus receptor is a transmembrane component of the tight junction. Proc Natl Acad Sci USA. 2001;98:15191–15196. doi: 10.1073/pnas.261452898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Westphal JK, Dorfel MJ, Krug SM, Cording JD, Piontek J, Blasig IE, Tauber R, Fromm M, Huber O. Tricellulin forms homomeric and heteromeric tight junctional complexes. Cell Mol Life Sci. 2010;67:2057–2068. doi: 10.1007/s00018-010-0313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Krug SM, Amasheh S, Richter JF, Milatz S, Gunzel D, Westphal JK, Huber O, Schulzke JD, Fromm M. Tricellulin forms a barrier to macromolecules in tricellular tight junctions without affecting ion permeability. Mol Biol Cell. 2009;20:3713–3724. doi: 10.1091/mbc.E09-01-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ikenouchi J, Sasaki H, Tsukita S, Furuse M. Loss of occludin affects tricellular localization of tricellulin. Mol Biol Cell. 2008;19:4687–4693. doi: 10.1091/mbc.E08-05-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gumbiner B, Lowenkopf T, Apatira D. Identification of a 160-kDa polypeptide that binds to the tight junction protein ZO-1. Proc Natl Acad Sci USA. 1991;88:3460–3464. doi: 10.1073/pnas.88.8.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Willott E, Balda MS, Fanning AS, Jameson B, Van Itallie C, Anderson JM. The tight junction protein ZO-1 is homologous to the Drosophila discs-large tumor suppressor protein of septate junctions. Proc Natl Acad Sci USA. 1993;90:7834–7838. doi: 10.1073/pnas.90.16.7834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haskins J, Gu L, Wittchen ES, Hibbard J, Stevenson BR. ZO-3, a novel member of the MAGUK protein family found at the tight junction, interacts with ZO-1 and occludin. J Cell Biol. 1998;141:199–208. doi: 10.1083/jcb.141.1.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fanning AS, Ma TY, Anderson JM. Isolation and functional characterization of the actin binding region in the tight junction protein ZO-1. FASEB J. 2002;16:1835–1837. doi: 10.1096/fj.02-0121fje. [DOI] [PubMed] [Google Scholar]
- 85.Itoh M, Furuse M, Morita K, Kubota K, Saitou M, Tsukita S. Direct binding of three tight junction-associated MAGUKs, ZO-1, ZO-2, and ZO-3, with the COOH termini of claudins. J Cell Biol. 1999;147:1351–1363. doi: 10.1083/jcb.147.6.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bazzoni G, Martinez-Estrada OM, Orsenigo F, Cordenonsi M, Citi S, Dejana E. Interaction of junctional adhesion molecule with the tight junction components ZO-1, cingulin, and occludin. J Biol Chem. 2000;275:20520–20526. doi: 10.1074/jbc.M905251199. [DOI] [PubMed] [Google Scholar]
- 87.Alexandre MD, Lu Q, Chen YH. Overexpression of claudin-7 decreases the paracellular Cl-conductance and increases the paracellular Na+ conductance in LLC-PK1 cells. J Cell Sci. 2005;118:2683–2693. doi: 10.1242/jcs.02406. [DOI] [PubMed] [Google Scholar]
- 88.Wittchen ES, Haskins J, Stevenson BR. Exogenous expression of the amino-terminal half of the tight junction protein ZO-3 perturbs junctional complex assembly. J Cell Biol. 2000;151:825–836. doi: 10.1083/jcb.151.4.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Balda MS, Matter K. The tight junction protein ZO-1 and an interacting transcription factor regulate ErbB-2 expression. EMBO J. 2000;19:2024–2033. doi: 10.1093/emboj/19.9.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Umeda K, Matsui T, Nakayama M, Furuse K, Sasaki H, Furuse M, Tsukita S. Establishment and characterization of cultured epithelial cells lacking expression of ZO-1. J Biol Chem. 2004;279:44785–44794. doi: 10.1074/jbc.M406563200. [DOI] [PubMed] [Google Scholar]
- 91.Cordenonsi M, D’Atri F, Hammar E, Parry DA, Kendrick-Jones J, Shore D, Citi S. Cingulin contains globular and coiled-coil domains and interacts with ZO-1, ZO-2, ZO-3, and myosin. J Cell Biol. 1999;147:1569–1582. doi: 10.1083/jcb.147.7.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cordenonsi M, Turco F, D’Atri F, Hammar E, Martinucci G, Meggio F, Citi S. Xenopus laevis occludin. Identification of in vitro phosphorylation sites by protein kinase CK2 and association with cingulin. Eur J Biochem. 1999;264:374–384. doi: 10.1046/j.1432-1327.1999.00616.x. [DOI] [PubMed] [Google Scholar]
- 93.Guillemot L, Hammar E, Kaister C, Ritz J, Caille D, Jond L, Bauer C, Meda P, Citi S. Disruption of the cingulin gene does not prevent tight junction formation but alters gene expression. J Cell Sci. 2004;117:5245–5256. doi: 10.1242/jcs.01399. [DOI] [PubMed] [Google Scholar]
- 94.Niessner M, Volk BA. Altered Th1/Th2 cytokine profiles in the intestinal mucosa of patients with inflammatory bowel disease as assessed by quantitative reversed transcribed polymerase chain reaction (RT-PCR) Clin Exp Immunol. 1995;101:428–435. doi: 10.1111/j.1365-2249.1995.tb03130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Stallmach A, Giese T, Schmidt C, Ludwig B, Mueller-Molaian I, Meuer SC. Cytokine/chemokine transcript profiles reflect mucosal inflammation in Crohn’s disease. Int J Colorectal Dis. 2004;19:308–315. doi: 10.1007/s00384-003-0554-4. [DOI] [PubMed] [Google Scholar]
- 96.Bruewer M, Luegering A, Kucharzik T, Parkos CA, Madara JL, Hopkins AM, Nusrat A. Proinflammatory cytokines disrupt epithelial barrier function by apoptosis-independent mechanisms. J Immunol. 2003;171:6164–6172. doi: 10.4049/jimmunol.171.11.6164. [DOI] [PubMed] [Google Scholar]
- 97.Bruewer M, Utech M, Ivanov AI, Hopkins AM, Parkos CA, Nusrat A. Interferon-gamma induces internalization of epithelial tight junction proteins via a macropinocytosis-like process. FASEB J. 2005;19:923–933. doi: 10.1096/fj.04-3260com. [DOI] [PubMed] [Google Scholar]
- 98.Sandborn WJ, Hanauer SB. Antitumor necrosis factor therapy for inflammatory bowel disease: a review of agents, pharmacology, clinical results, and safety. Inflamm Bowel Dis. 1999;5:119–133. doi: 10.1097/00054725-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 99.Ricart E, Panaccione R, Loftus EV, Tremaine WJ, Sandborn WJ. Successful management of Crohn’s disease of the ileoanal pouch with infliximab. Gastroenterology. 1999;117:429–432. doi: 10.1053/gast.1999.0029900429. [DOI] [PubMed] [Google Scholar]
- 100.Murch SH, Braegger CP, Walker-Smith JA, MacDonald TT. Location of tumour necrosis factor alpha by immunohistochemistry in chronic inflammatory bowel disease. Gut. 1993;34:1705–1709. doi: 10.1136/gut.34.12.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Braegger CP, Nicholls S, Murch SH, Stephens S, MacDonald TT. Tumour necrosis factor alpha in stool as a marker of intestinal inflammation. Lancet. 1992;339:89–91. doi: 10.1016/0140-6736(92)90999-J. [DOI] [PubMed] [Google Scholar]
- 102.Schulzke JD, Bojarski C, Zeissig S, Heller F, Gitter AH, Fromm M. Disrupted barrier function through epithelial cell apoptosis. Ann N Y Acad Sci. 2006;1072:288–299. doi: 10.1196/annals.1326.027. [DOI] [PubMed] [Google Scholar]
- 103.Ma TY, Iwamoto GK, Hoa NT, Akotia V, Pedram A, Boivin MA, Said HM. TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol. 2004;286:G367–G376. doi: 10.1152/ajpgi.00173.2003. [DOI] [PubMed] [Google Scholar]
- 104.Ma TY, Boivin MA, Ye D, Pedram A, Said HM. Mechanism of TNF-{alpha} modulation of Caco-2 intestinal epithelial tight junction barrier: role of myosin light-chain kinase protein expression. Am J Physiol Gastrointest Liver Physiol. 2005;288:G422–G430. doi: 10.1152/ajpgi.00412.2004. [DOI] [PubMed] [Google Scholar]
- 105.Graham WV, Wang F, Clayburgh DR, Cheng JX, Yoon B, Wang Y, Lin A, Turner JR. Tumor necrosis factor-induced long myosin light chain kinase transcription is regulated by differentiation-dependent signaling events. Characterization of the human long myosin light chain kinase promoter. J Biol Chem. 2006;281:26205–26215. doi: 10.1074/jbc.M602164200. [DOI] [PubMed] [Google Scholar]
- 106.Ye D, Ma I, Ma TY. Molecular mechanism of tumor necrosis factor-alpha modulation of intestinal epithelial tight junction barrier. Am J Physiol Gastrointest Liver Physiol. 2006;290:G496–G504. doi: 10.1152/ajpgi.00318.2005. [DOI] [PubMed] [Google Scholar]
- 107.Mankertz J, Amasheh M, Krug SM, Fromm A, Amasheh S, Hillenbrand B, Tavalali S, Fromm M, Schulzke JD. TNFalpha up-regulates claudin-2 expression in epithelial HT-29/B6 cells via phosphatidylinositol-3-kinase signaling. Cell Tissue Res. 2009;336:67–77. doi: 10.1007/s00441-009-0751-8. [DOI] [PubMed] [Google Scholar]
- 108.Reinecker HC, Steffen M, Witthoeft T, Pflueger I, Schreiber S, MacDermott RP, Raedler A. Enhanced secretion of tumour necrosis factor-alpha, IL-6, and IL-1 beta by isolated lamina propria mononuclear cells from patients with ulcerative colitis and Crohn’s disease. Clin Exp Immunol. 1993;94:174–181. doi: 10.1111/j.1365-2249.1993.tb05997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang F, Graham WV, Wang Y, Witkowski ED, Schwarz BT, Turner JR. Interferon-gamma and tumor necrosis factor-alpha synergize to induce intestinal epithelial barrier dysfunction by up-regulating myosin light chain kinase expression. Am J Pathol. 2005;166:409–419. doi: 10.1016/S0002-9440(10)62264-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang F, Schwarz BT, Graham WV, Wang Y, Su L, Clayburgh DR, Abraham C, Turner JR. IFN-gamma-induced TNFR2 expression is required for TNF-dependent intestinal epithelial barrier dysfunction. Gastroenterology. 2006;131:1153–1163. doi: 10.1053/j.gastro.2006.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schwarz BT, Wang F, Shen L, Clayburgh DR, Su L, Wang Y, Fu YX, Turner JR. LIGHT signals directly to intestinal epithelia to cause barrier dysfunction via cytoskeletal and endocytic mechanisms. Gastroenterology. 2007;132:2383–2394. doi: 10.1053/j.gastro.2007.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dinarello CA. The interleukin-1 family: 10 years of discovery. FASEB J. 1994;8:1314–1325. [PubMed] [Google Scholar]
- 113.Carty E, De Brabander M, Feakins RM, Rampton DS. Measurement of in vivo rectal mucosal cytokine and eicosanoid production in ulcerative colitis using filter paper. Gut. 2000;46:487–492. doi: 10.1136/gut.46.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Barksby HE, Lea SR, Preshaw PM, Taylor JJ. The expanding family of interleukin-1 cytokines and their role in destructive inflammatory disorders. Clin Exp Immunol. 2007;149:217–225. doi: 10.1111/j.1365-2249.2007.03441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dinarello CA. Anti-cytokine therapeutics and infections. Vaccine. 2003;21(Suppl 2):S24–S34. doi: 10.1016/S0264-410X(03)00196-8. [DOI] [PubMed] [Google Scholar]
- 116.Al-Sadi RM, Ma TY. IL-1beta causes an increase in intestinal epithelial tight junction permeability. J Immunol. 2007;178:4641–4649. doi: 10.4049/jimmunol.178.7.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Al-Sadi R, Ye D, Dokladny K, Ma TY. Mechanism of IL-1beta-induced increase in intestinal epithelial tight junction permeability. J Immunol. 2008;180:5653–5661. doi: 10.4049/jimmunol.180.8.5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Al-Sadi R, Ye D, Said HM, Ma TY. IL-1beta-induced increase in intestinal epithelial tight junction permeability is mediated by MEKK-1 activation of canonical NF-kappaB pathway. Am J Pathol. 2010;177:2310–2322. doi: 10.2353/ajpath.2010.100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Oliphant CJ, Barlow JL, McKenzie AN. Insights into the initiation of type 2 immune responses. Immunology. 2011;134:378–385. doi: 10.1111/j.1365-2567.2011.03499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Okoye IS, Wilson MS. CD4+ T helper 2 cells-microbial triggers, differentiation requirements and effector functions. Immunology. 2011;134:368–377. doi: 10.1111/j.1365-2567.2011.03497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wisner DM, Harris LR, 3rd, Green CL, Poritz LS. Opposing regulation of the tight junction protein claudin-2 by interferon-gamma and interleukin-4. J Surg Res. 2008;144:1–7. doi: 10.1016/j.jss.2007.03.059. [DOI] [PubMed] [Google Scholar]
- 122.Colgan SP, Resnick MB, Parkos CA, Delp-Archer C, McGuirk D, Bacarra AE, Weller PF, Madara JL. IL-4 directly modulates function of a model human intestinal epithelium. J Immunol. 1994;153:2122–2129. [PubMed] [Google Scholar]
- 123.Ceponis PJ, Botelho F, Richards CD, McKay DM. Interleukins 4 and 13 increase intestinal epithelial permeability by a phosphatidylinositol 3-kinase pathway. Lack of evidence for STAT 6 involvement. J Biol Chem. 2000;275:29132–29137. doi: 10.1074/jbc.M003516200. [DOI] [PubMed] [Google Scholar]
- 124.Tilg H, Dinarello CA, Mier JW. IL-6 and APPs: anti-inflammatory and immunosuppressive mediators. Immunol Today. 1997;18:428–432. doi: 10.1016/S0167-5699(97)01103-1. [DOI] [PubMed] [Google Scholar]
- 125.Alonzi T, Fattori E, Lazzaro D, Costa P, Probert L, Kollias G, De Benedetti F, Poli V, Ciliberto G. Interleukin 6 is required for the development of collagen-induced arthritis. J Exp Med. 1998;187:461–468. doi: 10.1084/jem.187.4.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Louis E, Belaiche J, van Kemseke C, Franchimont D, de Groote D, Gueenen V, Mary JY. A high serum concentration of interleukin-6 is predictive of relapse in quiescent Crohn’s disease. Eur J Gastroenterol Hepatol. 1997;9:939–944. doi: 10.1097/00042737-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 127.Kusugami K, Fukatsu A, Tanimoto M, Shinoda M, Haruta J, Kuroiwa A, Ina K, Kanayama K, Ando T, Matsuura T, et al. Elevation of interleukin-6 in inflammatory bowel disease is macrophage- and epithelial cell-dependent. Dig Dis Sci. 1995;40:949–959. doi: 10.1007/BF02064182. [DOI] [PubMed] [Google Scholar]
- 128.Suzuki T, Yoshinaga N, Tanabe S. Interleukin-6 (IL-6) regulates claudin-2 expression and tight junction permeability in intestinal epithelium. J Biol Chem. 2011;286:31263–31271. doi: 10.1074/jbc.M111.238147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yang R, Han X, Uchiyama T, Watkins SK, Yaguchi A, Delude RL, Fink MP. IL-6 is essential for development of gut barrier dysfunction after hemorrhagic shock and resuscitation in mice. Am J Physiol Gastrointest Liver Physiol. 2003;285:G621–G629. doi: 10.1152/ajpgi.00177.2003. [DOI] [PubMed] [Google Scholar]
- 130.Ouyang W, Rutz S, Crellin NK, Valdez PA, Hymowitz SG. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu Rev Immunol. 2011;29:71–109. doi: 10.1146/annurev-immunol-031210-101312. [DOI] [PubMed] [Google Scholar]
- 131.Saraiva M, O’Garra A. The regulation of IL-10 production by immune cells. Nat Rev Immunol. 2010;10:170–181. doi: 10.1038/nri2711. [DOI] [PubMed] [Google Scholar]
- 132.Kucharzik T, Lugering N, Pauels HG, Domschke W, Stoll R. IL-4, IL-10 and IL-13 down-regulate monocyte-chemoattracting protein-1 (MCP-1) production in activated intestinal epithelial cells. Clin Exp Immunol. 1998;111:152–157. doi: 10.1046/j.1365-2249.1998.00481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Madsen KL, Malfair D, Gray D, Doyle JS, Jewell LD, Fedorak RN. Interleukin-10 gene-deficient mice develop a primary intestinal permeability defect in response to enteric microflora. Inflamm Bowel Dis. 1999;5:262–270. doi: 10.1097/00054725-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 134.Madsen KL, Lewis SA, Tavernini MM, Hibbard J, Fedorak RN. Interleukin 10 prevents cytokine-induced disruption of T84 monolayer barrier integrity and limits chloride secretion. Gastroenterology. 1997;113:151–159. doi: 10.1016/S0016-5085(97)70090-8. [DOI] [PubMed] [Google Scholar]
- 135.Duran B. The effects of long-term total parenteral nutrition on gut mucosal immunity in children with short bowel syndrome: a systematic review. BMC Nurs. 2005;4:2. doi: 10.1186/1472-6955-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wildhaber BE, Yang H, Spencer AU, Drongowski RA, Teitelbaum DH. Lack of enteral nutrition–effects on the intestinal immune system. J Surg Res. 2005;123:8–16. doi: 10.1016/j.jss.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 137.Kansagra K, Stoll B, Rognerud C, Niinikoski H, Ou CN, Harvey R, Burrin D. Total parenteral nutrition adversely affects gut barrier function in neonatal piglets. Am J Physiol Gastrointest Liver Physiol. 2003;285:G1162–G1170. doi: 10.1152/ajpgi.00243.2003. [DOI] [PubMed] [Google Scholar]
- 138.Sun X, Yang H, Nose K, Nose S, Haxhija EQ, Koga H, Feng Y, Teitelbaum DH. Decline in intestinal mucosal IL-10 expression and decreased intestinal barrier function in a mouse model of total parenteral nutrition. Am J Physiol Gastrointest Liver Physiol. 2008;294:G139–G147. doi: 10.1152/ajpgi.00386.2007. [DOI] [PubMed] [Google Scholar]
- 139.Heller F, Florian P, Bojarski C, Richter J, Christ M, Hillenbrand B, Mankertz J, Gitter AH, Burgel N, Fromm M, Zeitz M, Fuss I, Strober W, Schulzke JD. Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129:550–564. doi: 10.1016/j.gastro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 140.Fuss IJ, Heller F, Boirivant M, Leon F, Yoshida M, Fichtner-Feigl S, Yang Z, Exley M, Kitani A, Blumberg RS, Mannon P, Strober W. Nonclassical CD1d-restricted NK T cells that produce IL-13 characterize an atypical Th2 response in ulcerative colitis. J Clin Invest. 2004;113:1490–1497. doi: 10.1172/JCI19836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Prasad S, Mingrino R, Kaukinen K, Hayes KL, Powell RM, MacDonald TT, Collins JE. Inflammatory processes have differential effects on claudins 2, 3 and 4 in colonic epithelial cells. Lab Invest. 2005;85:1139–1162. doi: 10.1038/labinvest.3700316. [DOI] [PubMed] [Google Scholar]
- 142.Weber CR, Raleigh DR, Su L, Shen L, Sullivan EA, Wang Y, Turner JR. Epithelial myosin light chain kinase activation induces mucosal interleukin-13 expression to alter tight junction ion selectivity. J Biol Chem. 2010;285:12037–12046. doi: 10.1074/jbc.M109.064808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pappu R, Ramirez-Carrozzi V, Sambandam A. The interleukin-17 cytokine family: critical players in host defence and inflammatory diseases. Immunology. 2011;134:8–16. doi: 10.1111/j.1365-2567.2011.03465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chang SH, Dong C. Signaling of interleukin-17 family cytokines in immunity and inflammation. Cell Signal. 2011;23:1069–1075. doi: 10.1016/j.cellsig.2010.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cosmi L, Liotta F, Maggi E, Romagnani S, Annunziato F. Th17 cells: new players in asthma pathogenesis. Allergy. 2011;66:989–998. doi: 10.1111/j.1398-9995.2011.02576.x. [DOI] [PubMed] [Google Scholar]
- 146.Kinugasa T, Sakaguchi T, Gu X, Reinecker HC. Claudins regulate the intestinal barrier in response to immune mediators. Gastroenterology. 2000;118:1001–1011. doi: 10.1016/S0016-5085(00)70351-9. [DOI] [PubMed] [Google Scholar]
- 147.Harris RC, Chung E, Coffey RJ. EGF receptor ligands. Exp Cell Res. 2003;284:2–13. doi: 10.1016/S0014-4827(02)00105-2. [DOI] [PubMed] [Google Scholar]
- 148.Booth BW, Smith GH. Roles of transforming growth factor-alpha in mammary development and disease. Growth Factors. 2007;25:227–235. doi: 10.1080/08977190701750698. [DOI] [PubMed] [Google Scholar]
- 149.Forsyth CB, Banan A, Farhadi A, Fields JZ, Tang Y, Shaikh M, Zhang LJ, Engen PA, Keshavarzian A. Regulation of oxidant-induced intestinal permeability by metalloprotease-dependent epidermal growth factor receptor signaling. J Pharmacol Exp Ther. 2007;321:84–97. doi: 10.1124/jpet.106.113019. [DOI] [PubMed] [Google Scholar]
- 150.Rao R, Baker RD, Baker SS. Inhibition of oxidant-induced barrier disruption and protein tyrosine phosphorylation in Caco-2 cell monolayers by epidermal growth factor. Biochem Pharmacol. 1999;57:685–695. doi: 10.1016/S0006-2952(98)00333-5. [DOI] [PubMed] [Google Scholar]
- 151.Howe KL, Reardon C, Wang A, Nazli A, McKay DM. Transforming growth factor-beta regulation of epithelial tight junction proteins enhances barrier function and blocks enterohemorrhagic Escherichia coli O157:H7-induced increased permeability. Am J Pathol. 2005;167:1587–1597. doi: 10.1016/S0002-9440(10)61243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hering NA, Andres S, Fromm A, van Tol EA, Amasheh M, Mankertz J, Fromm M, Schulzke JD. Transforming growth factor-beta, a whey protein component, strengthens the intestinal barrier by upregulating claudin-4 in HT-29/B6 cells. J Nutr. 2011;141:783–789. doi: 10.3945/jn.110.137588. [DOI] [PubMed] [Google Scholar]
- 153.Roche JK, Martins CA, Cosme R, Fayer R, Guerrant RL. Transforming growth factor beta1 ameliorates intestinal epithelial barrier disruption by Cryptosporidium parvum in vitro in the absence of mucosal T lymphocytes. Infect Immun. 2000;68:5635–5644. doi: 10.1128/IAI.68.10.5635-5644.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rao R. Oxidative stress-induced disruption of epithelial and endothelial tight junctions. Front Biosci. 2008;13:7210–7226. doi: 10.2741/3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Basuroy S, Seth A, Elias B, Naren AP, Rao R. MAPK interacts with occludin and mediates EGF-induced prevention of tight junction disruption by hydrogen peroxide. Biochem J. 2006;393:69–77. doi: 10.1042/BJ20050959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Banan A, Fields JZ, Talmage DA, Zhang L, Keshavarzian A. PKC-zeta is required in EGF protection of microtubules and intestinal barrier integrity against oxidant injury. Am J Physiol Gastrointest Liver Physiol. 2002;282:G794–G808. doi: 10.1152/ajpgi.00284.2001. [DOI] [PubMed] [Google Scholar]
- 157.Banan A, Fields JZ, Talmage DA, Zhang Y, Keshavarzian A. PKC-beta1 mediates EGF protection of microtubules and barrier of intestinal monolayers against oxidants. Am J Physiol Gastrointest Liver Physiol. 2001;281:G833–G847. doi: 10.1152/ajpgi.2001.281.3.G833. [DOI] [PubMed] [Google Scholar]
- 158.Banan A, Keshavarzian A, Zhang L, Shaikh M, Forsyth CB, Tang Y, Fields JZ. NF-kappaB activation as a key mechanism in ethanol-induced disruption of the F-actin cytoskeleton and monolayer barrier integrity in intestinal epithelium. Alcohol. 2007;41:447–460. doi: 10.1016/j.alcohol.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 159.Samak G, Aggarwal S, Rao RK. ERK is involved in EGF-mediated protection of tight junctions, but not adherens junctions, in acetaldehyde-treated Caco-2 cell monolayers. Am J Physiol Gastrointest Liver Physiol. 2011;301:G50–G59. doi: 10.1152/ajpgi.00494.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Baudry B, Fasano A, Ketley J, Kaper JB. Cloning of a gene (zot) encoding a new toxin produced by Vibrio cholerae . Infect Immun. 1992;60:428–434. doi: 10.1128/iai.60.2.428-434.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Fasano A, Baudry B, Pumplin DW, Wasserman SS, Tall BD, Ketley JM, Kaper JB. Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. Proc Natl Acad Sci USA. 1991;88:5242–5246. doi: 10.1073/pnas.88.12.5242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Di Pierro M, Lu R, Uzzau S, Wang W, Margaretten K, Pazzani C, Maimone F, Fasano A. Zonula occludens toxin structure-function analysis. Identification of the fragment biologically active on tight junctions and of the zonulin receptor binding domain. J Biol Chem. 2001;276:19160–19165. doi: 10.1074/jbc.M009674200. [DOI] [PubMed] [Google Scholar]
- 163.Goldblum SE, Rai U, Tripathi A, Thakar M, De Leo L, Di Toro N, Not T, Ramachandran R, Puche AC, Hollenberg MD, Fasano A. The active Zot domain (aa 288–293) increases ZO-1 and myosin 1C serine/threonine phosphorylation, alters interaction between ZO-1 and its binding partners, and induces tight junction disassembly through proteinase activated receptor 2 activation. FASEB J. 2011;25:144–158. doi: 10.1096/fj.10-158972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Mel SF, Fullner KJ, Wimer-Mackin S, Lencer WI, Mekalanos JJ. Association of protease activity in Vibrio cholerae vaccine strains with decreases in transcellular epithelial resistance of polarized T84 intestinal epithelial cells. Infect Immun. 2000;68:6487–6492. doi: 10.1128/IAI.68.11.6487-6492.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wu Z, Nybom P, Magnusson KE. Distinct effects of Vibrio cholerae haemagglutinin/protease on the structure and localization of the tight junction-associated proteins occludin and ZO-1. Cell Microbiol. 2000;2:11–17. doi: 10.1046/j.1462-5822.2000.00025.x. [DOI] [PubMed] [Google Scholar]
- 166.Muza-Moons MM, Schneeberger EE, Hecht GA. Enteropathogenic Escherichia coli infection leads to appearance of aberrant tight junctions strands in the lateral membrane of intestinal epithelial cells. Cell Microbiol. 2004;6:783–793. doi: 10.1111/j.1462-5822.2004.00404.x. [DOI] [PubMed] [Google Scholar]
- 167.Philpott DJ, McKay DM, Sherman PM, Perdue MH. Infection of T84 cells with enteropathogenic Escherichia coli alters barrier and transport functions. Am J Physiol. 1996;270:G634–G645. doi: 10.1152/ajpgi.1996.270.4.G634. [DOI] [PubMed] [Google Scholar]
- 168.Shifflett DE, Clayburgh DR, Koutsouris A, Turner JR, Hecht GA. Enteropathogenic E. coli disrupts tight junction barrier function and structure in vivo. Lab Invest. 2005;85:1308–1324. doi: 10.1038/labinvest.3700330. [DOI] [PubMed] [Google Scholar]
- 169.Simonovic I, Rosenberg J, Koutsouris A, Hecht G. Enteropathogenic Escherichia coli dephosphorylates and dissociates occludin from intestinal epithelial tight junctions. Cell Microbiol. 2000;2:305–315. doi: 10.1046/j.1462-5822.2000.00055.x. [DOI] [PubMed] [Google Scholar]
- 170.Spitz J, Yuhan R, Koutsouris A, Blatt C, Alverdy J, Hecht G. Enteropathogenic Escherichia coli adherence to intestinal epithelial monolayers diminishes barrier function. Am J Physiol. 1995;268:G374–G379. doi: 10.1152/ajpgi.1995.268.2.G374. [DOI] [PubMed] [Google Scholar]
- 171.Tomson FL, Koutsouris A, Viswanathan VK, Turner JR, Savkovic SD, Hecht G. Differing roles of protein kinase C-zeta in disruption of tight junction barrier by enteropathogenic and enterohemorrhagic Escherichia coli . Gastroenterology. 2004;127:859–869. doi: 10.1053/j.gastro.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 172.Dean P, Kenny B. Intestinal barrier dysfunction by enteropathogenic Escherichia coli is mediated by two effector molecules and a bacterial surface protein. Mol Microbiol. 2004;54:665–675. doi: 10.1111/j.1365-2958.2004.04308.x. [DOI] [PubMed] [Google Scholar]
- 173.Philpott DJ, McKay DM, Mak W, Perdue MH, Sherman PM. Signal transduction pathways involved in enterohemorrhagic Escherichia coli-induced alterations in T84 epithelial permeability. Infect Immun. 1998;66:1680–1687. doi: 10.1128/iai.66.4.1680-1687.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brynestad S, Granum PE. Clostridium perfringens and foodborne infections. Int J Food Microbiol. 2002;74:195–202. doi: 10.1016/S0168-1605(01)00680-8. [DOI] [PubMed] [Google Scholar]
- 175.McClane BA, Wnek AP, Hulkower KI, Hanna PC. Divalent cation involvement in the action of Clostridium perfringens type A enterotoxin. Early events in enterotoxin action are divalent cation-independent. J Biol Chem. 1988;263:2423–2435. [PubMed] [Google Scholar]
- 176.Hanna PC, Mietzner TA, Schoolnik GK, McClane BA. Localization of the receptor-binding region of Clostridium perfringens enterotoxin utilizing cloned toxin fragments and synthetic peptides. The 30 C-terminal amino acids define a functional binding region. J Biol Chem. 1991;266:11037–11043. [PubMed] [Google Scholar]
- 177.Hanna PC, Wieckowski EU, Mietzner TA, McClane BA. Mapping of functional regions of Clostridium perfringens type A enterotoxin. Infect Immun. 1992;60:2110–2114. doi: 10.1128/iai.60.5.2110-2114.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Katahira J, Sugiyama H, Inoue N, Horiguchi Y, Matsuda M, Sugimoto N. Clostridium perfringens enterotoxin utilizes two structurally related membrane proteins as functional receptors in vivo. J Biol Chem. 1997;272:26652–26658. doi: 10.1074/jbc.272.42.26652. [DOI] [PubMed] [Google Scholar]
- 179.Katahira J, Inoue N, Horiguchi Y, Matsuda M, Sugimoto N. Molecular cloning and functional characterization of the receptor for Clostridium perfringens enterotoxin. J Cell Biol. 1997;136:1239–1247. doi: 10.1083/jcb.136.6.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sonoda N, Furuse M, Sasaki H, Yonemura S, Katahira J, Horiguchi Y, Tsukita S. Clostridium perfringens enterotoxin fragment removes specific claudins from tight junction strands: evidence for direct involvement of claudins in tight junction barrier. J Cell Biol. 1999;147:195–204. doi: 10.1083/jcb.147.1.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Takahashi A, Kondoh M, Masuyama A, Fujii M, Mizuguchi H, Horiguchi Y, Watanabe Y. Role of C-terminal regions of the C-terminal fragment of Clostridium perfringens enterotoxin in its interaction with claudin-4. J Controlled Release. 2005;108:56–62. doi: 10.1016/j.jconrel.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 182.Singh U, Van Itallie CM, Mitic LL, Anderson JM, McClane BA. CaCo-2 cells treated with Clostridium perfringens enterotoxin form multiple large complex species, one of which contains the tight junction protein occludin. J Biol Chem. 2000;275:18407–18417. doi: 10.1074/jbc.M001530200. [DOI] [PubMed] [Google Scholar]
- 183.Peng X, Yan H, You Z, Wang P, Wang S. Effects of enteral supplementation with glutamine granules on intestinal mucosal barrier function in severe burned patients. Burns. 2004;30:135–139. doi: 10.1016/j.burns.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 184.Ding LA, Li JS. Effects of glutamine on intestinal permeability and bacterial translocation in TPN-rats with endotoxemia. World J Gastroenterol. 2003;9:1327–1332. doi: 10.3748/wjg.v9.i6.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Li J, Langkamp-Henken B, Suzuki K, Stahlgren LH. Glutamine prevents parenteral nutrition-induced increases in intestinal permeability. JPEN J Parenter Enteral Nutr. 1994;18:303–307. doi: 10.1177/0148607194018004303. [DOI] [PubMed] [Google Scholar]
- 186.Foitzik T, Stufler M, Hotz HG, Klinnert J, Wagner J, Warshaw AL, Schulzke JD, Fromm M, Buhr HJ. Glutamine stabilizes intestinal permeability and reduces pancreatic infection in acute experimental pancreatitis. J Gastrointest Surg. 1997;1:40–46. doi: 10.1007/s11605-006-0008-8. [DOI] [PubMed] [Google Scholar]
- 187.Li N, Lewis P, Samuelson D, Liboni K, Neu J. Glutamine regulates Caco-2 cell tight junction proteins. Am J Physiol Gastrointest Liver Physiol. 2004;287:G726–G733. doi: 10.1152/ajpgi.00012.2004. [DOI] [PubMed] [Google Scholar]
- 188.Li N, Neu J. Glutamine deprivation alters intestinal tight junctions via a PI3-K/Akt mediated pathway in Caco-2 cells. J Nutr. 2009;139:710–714. doi: 10.3945/jn.108.101485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Seth A, Basuroy S, Sheth P, Rao RK. l-Glutamine ameliorates acetaldehyde-induced increase in paracellular permeability in Caco-2 cell monolayer. Am J Physiol Gastrointest Liver Physiol. 2004;287:G510–G517. doi: 10.1152/ajpgi.00058.2004. [DOI] [PubMed] [Google Scholar]
- 190.Basuroy S, Sheth P, Mansbach CM, Rao RK. Acetaldehyde disrupts tight junctions and adherens junctions in human colonic mucosa: protection by EGF and l-glutamine. Am J Physiol Gastrointest Liver Physiol. 2005;289:G367–G375. doi: 10.1152/ajpgi.00464.2004. [DOI] [PubMed] [Google Scholar]
- 191.Watanabe J, Fukumoto K, Fukushi E, Sonoyama K, Kawabata J. Isolation of tryptophan as an inhibitor of ovalbumin permeation and analysis of its suppressive effect on oral sensitization. Biosci Biotechnol Biochem. 2004;68:59–65. doi: 10.1271/bbb.68.59. [DOI] [PubMed] [Google Scholar]
- 192.Isobe N, Suzuki M, Oda M, Tanabe S. Enzyme-modified cheese exerts inhibitory effects on allergen permeation in rats suffering from indomethacin-induced intestinal inflammation. Biosci Biotechnol Biochem. 2008;72:1740–1745. doi: 10.1271/bbb.80042. [DOI] [PubMed] [Google Scholar]
- 193.Tanabe S. Short peptide modules for enhancing intestinal barrier function. Curr Pharm Des. 2012;18:776–781. doi: 10.2174/138161212799277653. [DOI] [PubMed] [Google Scholar]
- 194.Yasumatsu H, Tanabe S. The casein peptide Asn-Pro-Trp-Asp-Gln enforces the intestinal tight junction partly by increasing occludin expression in Caco-2 cells. Br J Nutr. 2010;104:951–956. doi: 10.1017/S0007114510001698. [DOI] [PubMed] [Google Scholar]
- 195.Usami M, Muraki K, Iwamoto M, Ohata A, Matsushita E, Miki A. Effect of eicosapentaenoic acid (EPA) on tight junction permeability in intestinal monolayer cells. Clin Nutr. 2001;20:351–359. doi: 10.1054/clnu.2001.0430. [DOI] [PubMed] [Google Scholar]
- 196.Usami M, Komurasaki T, Hanada A, Kinoshita K, Ohata A. Effect of gamma-linolenic acid or docosahexaenoic acid on tight junction permeability in intestinal monolayer cells and their mechanism by protein kinase C activation and/or eicosanoid formation. Nutrition. 2003;19:150–156. doi: 10.1016/S0899-9007(02)00927-9. [DOI] [PubMed] [Google Scholar]
- 197.Willemsen LE, Koetsier MA, Balvers M, Beermann C, Stahl B, van Tol EA. Polyunsaturated fatty acids support epithelial barrier integrity and reduce IL-4 mediated permeability in vitro. Eur J Nutr. 2008;47:183–191. doi: 10.1007/s00394-008-0712-0. [DOI] [PubMed] [Google Scholar]
- 198.Anderberg EK, Lindmark T, Artursson P. Sodium caprate elicits dilatations in human intestinal tight junctions and enhances drug absorption by the paracellular route. Pharm Res. 1993;10:857–864. doi: 10.1023/A:1018909210879. [DOI] [PubMed] [Google Scholar]
- 199.Lindmark T, Nikkila T, Artursson P. Mechanisms of absorption enhancement by medium chain fatty acids in intestinal epithelial Caco-2 cell monolayers. J Pharmacol Exp Ther. 1995;275:958–964. [PubMed] [Google Scholar]
- 200.Soderholm JD, Oman H, Blomquist L, Veen J, Lindmark T, Olaison G. Reversible increase in tight junction permeability to macromolecules in rat ileal mucosa in vitro by sodium caprate, a constituent of milk fat. Dig Dis Sci. 1998;43:1547–1552. doi: 10.1023/A:1018823100761. [DOI] [PubMed] [Google Scholar]
- 201.Mortensen PB, Clausen MR. Short-chain fatty acids in the human colon: relation to gastrointestinal health and disease. Scand J Gastroenterol Suppl. 1996;216:132–148. doi: 10.3109/00365529609094568. [DOI] [PubMed] [Google Scholar]
- 202.Topping DL, Clifton PM. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev. 2001;81:1031–1064. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 203.Mariadason JM, Barkla DH, Gibson PR. Effect of short-chain fatty acids on paracellular permeability in Caco-2 intestinal epithelium model. Am J Physiol. 1997;272:G705–G712. doi: 10.1152/ajpgi.1997.272.4.G705. [DOI] [PubMed] [Google Scholar]
- 204.Kinoshita M, Suzuki Y, Saito Y. Butyrate reduces colonic paracellular permeability by enhancing PPARgamma activation. Biochem Biophys Res Commun. 2002;293:827–831. doi: 10.1016/S0006-291X(02)00294-2. [DOI] [PubMed] [Google Scholar]
- 205.Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr. 2009;139:1619–1625. doi: 10.3945/jn.109.104638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Suzuki T, Yoshida S, Hara H. Physiological concentrations of short-chain fatty acids immediately suppress colonic epithelial permeability. Br J Nutr. 2008;100:297–305. doi: 10.1017/S0007114508888733. [DOI] [PubMed] [Google Scholar]
- 207.Le Poul E, Loison C, Struyf S, Springael JY, Lannoy V, Decobecq ME, Brezillon S, Dupriez V, Vassart G, Van Damme J, Parmentier M, Detheux M. Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J Biol Chem. 2003;278:25481–25489. doi: 10.1074/jbc.M301403200. [DOI] [PubMed] [Google Scholar]
- 208.Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ. The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem. 2003;278:11312–11319. doi: 10.1074/jbc.M211609200. [DOI] [PubMed] [Google Scholar]
- 209.Karaki S, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A. Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res. 2006;324:353–360. doi: 10.1007/s00441-005-0140-x. [DOI] [PubMed] [Google Scholar]
- 210.Karaki S, Tazoe H, Hayashi H, Kashiwabara H, Tooyama K, Suzuki Y, Kuwahara A. Expression of the short-chain fatty acid receptor, GPR43, in the human colon. J Mol Histol. 2008;39:135–142. doi: 10.1007/s10735-007-9145-y. [DOI] [PubMed] [Google Scholar]
- 211.Rowe A. Retinoid X receptors. Int J Biochem Cell Biol. 1997;29:275–278. doi: 10.1016/S1357-2725(96)00101-X. [DOI] [PubMed] [Google Scholar]
- 212.Dusso AS, Brown AJ. Mechanism of vitamin D action and its regulation. Am J Kidney Dis. 1998;32:S13–S24. doi: 10.1053/ajkd.1998.v32.pm9808140. [DOI] [PubMed] [Google Scholar]
- 213.Maciel AA, Oria RB, Braga-Neto MB, Braga AB, Carvalho EB, Lucena HB, Brito GA, Guerrant RL, Lima AA. Role of retinol in protecting epithelial cell damage induced by Clostridium difficile toxin A. Toxicon. 2007;50:1027–1040. doi: 10.1016/j.toxicon.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kong J, Zhang Z, Musch MW, Ning G, Sun J, Hart J, Bissonnette M, Li YC. Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier. Am J Physiol Gastrointest Liver Physiol. 2008;294:G208–G216. doi: 10.1152/ajpgi.00398.2007. [DOI] [PubMed] [Google Scholar]
- 215.Kandaswami C, Middleton E., Jr Free radical scavenging and antioxidant activity of plant flavonoids. Adv Exp Med Biol. 1994;366:351–376. doi: 10.1007/978-1-4615-1833-4_25. [DOI] [PubMed] [Google Scholar]
- 216.Hamalainen M, Nieminen R, Vuorela P, Heinonen M, Moilanen E. Anti-inflammatory effects of flavonoids: genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-kappaB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-kappaB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediat Inflamm. 2007;2007:45673. doi: 10.1155/2007/45673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Suzuki T, Hara H. Quercetin enhances intestinal barrier function through the assembly of zonula occludens-2, occludin, and claudin-1 and the expression of claudin-4 in Caco-2 cells. J Nutr. 2009;139:965–974. doi: 10.3945/jn.108.100867. [DOI] [PubMed] [Google Scholar]
- 218.Suzuki T, Tanabe S, Hara H. Kaempferol enhances intestinal barrier function through the cytoskeletal association and expression of tight junction proteins in Caco-2 cells. J Nutr. 2011;141:87–94. doi: 10.3945/jn.110.125633. [DOI] [PubMed] [Google Scholar]
- 219.Amasheh M, Schlichter S, Amasheh S, Mankertz J, Zeitz M, Fromm M, Schulzke JD. Quercetin enhances epithelial barrier function and increases claudin-4 expression in Caco-2 cells. J Nutr. 2008;138:1067–1073. doi: 10.1093/jn/138.6.1067. [DOI] [PubMed] [Google Scholar]
- 220.Sheth P, Seth A, Atkinson KJ, Gheyi T, Kale G, Giorgianni F, Desiderio DM, Li C, Naren A, Rao R. Acetaldehyde dissociates the PTP1B-E-cadherin-beta-catenin complex in Caco-2 cell monolayers by a phosphorylation-dependent mechanism. Biochem J. 2007;402:291–300. doi: 10.1042/BJ20060665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Watson JL, Ansari S, Cameron H, Wang A, Akhtar M, McKay DM. Green tea polyphenol (−)-epigallocatechin gallate blocks epithelial barrier dysfunction provoked by IFN-gamma but not by IL-4. Am J Physiol Gastrointest Liver Physiol. 2004;287:G954–G961. doi: 10.1152/ajpgi.00302.2003. [DOI] [PubMed] [Google Scholar]
- 222.Sanders ME. Probiotics: considerations for human health. Nutr Rev. 2003;61:91–99. doi: 10.1301/nr.2003.marr.91-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ukena SN, Singh A, Dringenberg U, Engelhardt R, Seidler U, Hansen W, Bleich A, Bruder D, Franzke A, Rogler G, Suerbaum S, Buer J, Gunzer F, Westendorf AM. Probiotic Escherichia coli Nissle 1917 inhibits leaky gut by enhancing mucosal integrity. PLoS One. 2007;2:e1308. doi: 10.1371/journal.pone.0001308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Garrido-Mesa N, Utrilla P, Comalada M, Zorrilla P, Garrido-Mesa J, Zarzuelo A, Rodriguez-Cabezas ME, Galvez J. The association of minocycline and the probiotic Escherichia coli Nissle 1917 results in an additive beneficial effect in a DSS model of reactivated colitis in mice. Biochem Pharmacol. 2011;82:1891–1900. doi: 10.1016/j.bcp.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 225.Zyrek AA, Cichon C, Helms S, Enders C, Sonnenborn U, Schmidt MA. Molecular mechanisms underlying the probiotic effects of Escherichia coli Nissle 1917 involve ZO-2 and PKCzeta redistribution resulting in tight junction and epithelial barrier repair. Cell Microbiol. 2007;9:804–816. doi: 10.1111/j.1462-5822.2006.00836.x. [DOI] [PubMed] [Google Scholar]
- 226.Resta-Lenert S, Barrett KE. Live probiotics protect intestinal epithelial cells from the effects of infection with enteroinvasive Escherichia coli (EIEC) Gut. 2003;52:988–997. doi: 10.1136/gut.52.7.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Resta-Lenert S, Barrett KE. Probiotics and commensals reverse TNF-alpha- and IFN-gamma-induced dysfunction in human intestinal epithelial cells. Gastroenterology. 2006;130:731–746. doi: 10.1053/j.gastro.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 228.Mennigen R, Nolte K, Rijcken E, Utech M, Loeffler B, Senninger N, Bruewer M. Probiotic mixture VSL#3 protects the epithelial barrier by maintaining tight junction protein expression and preventing apoptosis in a murine model of colitis. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1140–G1149. doi: 10.1152/ajpgi.90534.2008. [DOI] [PubMed] [Google Scholar]
- 229.Dai C, Zhao DH, Jiang M. VSL#3 probiotics regulate the intestinal epithelial barrier in vivo and in vitro via the p38 and ERK signaling pathways. Int J Mol Med. 2012;29:202–208. doi: 10.3892/ijmm.2011.839. [DOI] [PubMed] [Google Scholar]
- 230.Chen HQ, Yang J, Zhang M, Zhou YK, Shen TY, Chu ZX, Hang XM, Jiang YQ, Qin HL. Lactobacillus plantarum ameliorates colonic epithelial barrier dysfunction by modulating the apical junctional complex and PepT1 in IL-10 knockout mice. Am J Physiol Gastrointest Liver Physiol. 2010;299:G1287–G1297. doi: 10.1152/ajpgi.00196.2010. [DOI] [PubMed] [Google Scholar]
- 231.Ko JS, Yang HR, Chang JY, Seo JK. Lactobacillus plantarum inhibits epithelial barrier dysfunction and interleukin-8 secretion induced by tumor necrosis factor-alpha. World J Gastroenterol. 2007;13:1962–1965. doi: 10.3748/wjg.v13.i13.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Karczewski J, Troost FJ, Konings I, Dekker J, Kleerebezem M, Brummer RJ, Wells JM. Regulation of human epithelial tight junction proteins by Lactobacillus plantarum in vivo and protective effects on the epithelial barrier. Am J Physiol Gastrointest Liver Physiol. 2010;298:G851–G859. doi: 10.1152/ajpgi.00327.2009. [DOI] [PubMed] [Google Scholar]
- 233.Cario E, Gerken G, Podolsky DK. Toll-like receptor 2 enhances ZO-1-associated intestinal epithelial barrier integrity via protein kinase C. Gastroenterology. 2004;127:224–238. doi: 10.1053/j.gastro.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 234.Miyauchi E, Morita H, Tanabe S. Lactobacillus rhamnosus alleviates intestinal barrier dysfunction in part by increasing expression of zonula occludens-1 and myosin light-chain kinase in vivo. J Dairy Res. 2009;92:2400–2408. doi: 10.3168/jds.2008-1698. [DOI] [PubMed] [Google Scholar]
- 235.Donato KA, Gareau MG, Wang YJ, Sherman PM. Lactobacillus rhamnosus GG attenuates interferon-{gamma} and tumour necrosis factor-alpha-induced barrier dysfunction and pro-inflammatory signalling. Microbiology. 2010;156:3288–3297. doi: 10.1099/mic.0.040139-0. [DOI] [PubMed] [Google Scholar]
- 236.Johnson-Henry KC, Donato KA, Shen-Tu G, Gordanpour M, Sherman PM. Lactobacillus rhamnosus strain GG prevents enterohemorrhagic Escherichia coli O157:H7-induced changes in epithelial barrier function. Infect Immun. 2008;76:1340–1348. doi: 10.1128/IAI.00778-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Yan F, Cao H, Cover TL, Whitehead R, Washington MK, Polk DB. Soluble proteins produced by probiotic bacteria regulate intestinal epithelial cell survival and growth. Gastroenterology. 2007;132:562–575. doi: 10.1053/j.gastro.2006.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Seth A, Yan F, Polk DB, Rao RK. Probiotics ameliorate the hydrogen peroxide-induced epithelial barrier disruption by a PKC- and MAP kinase-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1060–G1069. doi: 10.1152/ajpgi.00202.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Yan F, Cao H, Cover TL, Washington MK, Shi Y, Liu L, Chaturvedi R, Peek RM, Jr, Wilson KT, Polk DB. Colon-specific delivery of a probiotic-derived soluble protein ameliorates intestinal inflammation in mice through an EGFR-dependent mechanism. J Clin Invest. 2011;121:2242–2253. doi: 10.1172/JCI44031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Ewaschuk JB, Diaz H, Meddings L, Diederichs B, Dmytrash A, Backer J, Looijer-van Langen M, Madsen KL. Secreted bioactive factors from Bifidobacterium infantis enhance epithelial cell barrier function. Am J Physiol Gastrointest Liver Physiol. 2008;295:G1025–G1034. doi: 10.1152/ajpgi.90227.2008. [DOI] [PubMed] [Google Scholar]
- 241.Keshavarzian A, Farhadi A, Forsyth CB, Rangan J, Jakate S, Shaikh M, Banan A, Fields JZ. Evidence that chronic alcohol exposure promotes intestinal oxidative stress, intestinal hyperpermeability and endotoxemia prior to development of alcoholic steatohepatitis in rats. J Hepatol. 2009;50:538–547. doi: 10.1016/j.jhep.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Ferrier L, Berard F, Debrauwer L, Chabo C, Langella P, Bueno L, Fioramonti J. Impairment of the intestinal barrier by ethanol involves enteric microflora and mast cell activation in rodents. Am J Pathol. 2006;168:1148–1154. doi: 10.2353/ajpath.2006.050617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Tamai H, Kato S, Horie Y, Ohki E, Yokoyama H, Ishii H. Effect of acute ethanol administration on the intestinal absorption of endotoxin in rats. Alcohol Clin Exp Res. 2000;24:390–394. doi: 10.1111/j.1530-0277.2000.tb04629.x. [DOI] [PubMed] [Google Scholar]
- 244.Ma TY, Nguyen D, Bui V, Nguyen H, Hoa N. Ethanol modulation of intestinal epithelial tight junction barrier. Am J Physiol. 1999;276:G965–G974. doi: 10.1152/ajpgi.1999.276.4.G965. [DOI] [PubMed] [Google Scholar]
- 245.Visapaa JP, Jokelainen K, Nosova T, Salaspuro M. Inhibition of intracolonic acetaldehyde production and alcoholic fermentation in rats by ciprofloxacin. Alcohol Clin Exp Res. 1998;22:1161–1164. doi: 10.1111/j.1530-0277.1998.tb03716.x. [DOI] [PubMed] [Google Scholar]
- 246.Rao RK. Acetaldehyde-induced increase in paracellular permeability in Caco-2 cell monolayer. Alcohol Clin Exp Res. 1998;22:1724–1730. doi: 10.1111/j.1530-0277.1998.tb03972.x. [DOI] [PubMed] [Google Scholar]
- 247.Soderholm JD, Peterson KH, Olaison G, Franzen LE, Westrom B, Magnusson KE, Sjodahl R. Epithelial permeability to proteins in the noninflamed ileum of Crohn’s disease? Gastroenterology. 1999;117:65–72. doi: 10.1016/S0016-5085(99)70551-2. [DOI] [PubMed] [Google Scholar]
- 248.Hollander D, Vadheim CM, Brettholz E, Petersen GM, Delahunty T, Rotter JI. Increased intestinal permeability in patients with Crohn’s disease and their relatives. A possible etiologic factor. Ann Intern Med. 1986;105:883–885. doi: 10.7326/0003-4819-105-6-883. [DOI] [PubMed] [Google Scholar]
- 249.Suenaert P, Bulteel V, Lemmens L, Noman M, Geypens B, Van Assche G, Geboes K, Ceuppens JL, Rutgeerts P. Anti-tumor necrosis factor treatment restores the gut barrier in Crohn’s disease. Am J Gastroenterol. 2002;97:2000–2004. doi: 10.1111/j.1572-0241.2002.05914.x. [DOI] [PubMed] [Google Scholar]
- 250.Zeissig S, Burgel N, Gunzel D, Richter J, Mankertz J, Wahnschaffe U, Kroesen AJ, Zeitz M, Fromm M, Schulzke JD. Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn’s disease. Gut. 2007;56:61–72. doi: 10.1136/gut.2006.094375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Vetrano S, Rescigno M, Cera MR, Correale C, Rumio C, Doni A, Fantini M, Sturm A, Borroni E, Repici A, Locati M, Malesci A, Dejana E, Danese S. Unique role of junctional adhesion molecule-a in maintaining mucosal homeostasis in inflammatory bowel disease. Gastroenterology. 2008;135:173–184. doi: 10.1053/j.gastro.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 252.Blair SA, Kane SV, Clayburgh DR, Turner JR. Epithelial myosin light chain kinase expression and activity are upregulated in inflammatory bowel disease. Lab Invest. 2006;86:191–201. doi: 10.1038/labinvest.3700373. [DOI] [PubMed] [Google Scholar]
- 253.Smecuol E, Bai JC, Vazquez H, Kogan Z, Cabanne A, Niveloni S, Pedreira S, Boerr L, Maurino E, Meddings JB. Gastrointestinal permeability in celiac disease. Gastroenterology. 1997;112:1129–1136. doi: 10.1016/S0016-5085(97)70123-9. [DOI] [PubMed] [Google Scholar]
- 254.Schulzke JD, Bentzel CJ, Schulzke I, Riecken EO, Fromm M. Epithelial tight junction structure in the jejunum of children with acute and treated celiac sprue. Pediatr Res. 1998;43:435–441. doi: 10.1203/00006450-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 255.van Elburg RM, Uil JJ, Mulder CJ, Heymans HS. Intestinal permeability in patients with coeliac disease and relatives of patients with coeliac disease. Gut. 1993;34:354–357. doi: 10.1136/gut.34.3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Lammers KM, Lu R, Brownley J, Lu B, Gerard C, Thomas K, Rallabhandi P, Shea-Donohue T, Tamiz A, Alkan S, Netzel-Arnett S, Antalis T, Vogel SN, Fasano A. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology. 2008;135(194–204):e193. doi: 10.1053/j.gastro.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Lu R, Wang W, Uzzau S, Vigorito R, Zielke HR, Fasano A. Affinity purification and partial characterization of the zonulin/zonula occludens toxin (Zot) receptor from human brain. J Neurochem. 2000;74:320–326. doi: 10.1046/j.1471-4159.2000.0740320.x. [DOI] [PubMed] [Google Scholar]
- 258.Wang W, Uzzau S, Goldblum SE, Fasano A. Human zonulin, a potential modulator of intestinal tight junctions. J Cell Sci. 2000;113(Pt 24):4435–4440. doi: 10.1242/jcs.113.24.4435. [DOI] [PubMed] [Google Scholar]
- 259.Drago S, El Asmar R, Di Pierro M, Grazia Clemente M, Tripathi A, Sapone A, Thakar M, Iacono G, Carroccio A, D’Agate C, Not T, Zampini L, Catassi C, Fasano A. Gliadin, zonulin and gut permeability: effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006;41:408–419. doi: 10.1080/00365520500235334. [DOI] [PubMed] [Google Scholar]
- 260.Szakal DN, Gyorffy H, Arato A, Cseh A, Molnar K, Papp M, Dezsofi A, Veres G. Mucosal expression of claudins 2, 3 and 4 in proximal and distal part of duodenum in children with coeliac disease. Virchows Arch. 2010;456:245–250. doi: 10.1007/s00428-009-0879-7. [DOI] [PubMed] [Google Scholar]
- 261.Louka AS, Sollid LM. HLA in coeliac disease: unravelling the complex genetics of a complex disorder. Tissue Antigens. 2003;61:105–117. doi: 10.1034/j.1399-0039.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- 262.Mooradian AD, Morley JE, Levine AS, Prigge WF, Gebhard RL. Abnormal intestinal permeability to sugars in diabetes mellitus. Diabetologia. 1986;29:221–224. doi: 10.1007/BF00454879. [DOI] [PubMed] [Google Scholar]
- 263.Bosi E, Molteni L, Radaelli MG, Folini L, Fermo I, Bazzigaluppi E, Piemonti L, Pastore MR, Paroni R. Increased intestinal permeability precedes clinical onset of type 1 diabetes. Diabetologia. 2006;49:2824–2827. doi: 10.1007/s00125-006-0465-3. [DOI] [PubMed] [Google Scholar]
- 264.Vaarala O. Leaking gut in type 1 diabetes. Curr Opin Gastroenterol. 2008;24:701–706. doi: 10.1097/MOG.0b013e32830e6d98. [DOI] [PubMed] [Google Scholar]
- 265.Westerholm-Ormio M, Vaarala O, Pihkala P, Ilonen J, Savilahti E. Immunologic activity in the small intestinal mucosa of pediatric patients with type 1 diabetes. Diabetes. 2003;52:2287–2295. doi: 10.2337/diabetes.52.9.2287. [DOI] [PubMed] [Google Scholar]
- 266.Watts T, Berti I, Sapone A, Gerarduzzi T, Not T, Zielke R, Fasano A. Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc Natl Acad Sci USA. 2005;102:2916–2921. doi: 10.1073/pnas.0500178102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Meddings JB, Jarand J, Urbanski SJ, Hardin J, Gall DG. Increased gastrointestinal permeability is an early lesion in the spontaneously diabetic BB rat. Am J Physiol. 1999;276:G951–G957. doi: 10.1152/ajpgi.1999.276.4.G951. [DOI] [PubMed] [Google Scholar]
- 268.Sapone A, de Magistris L, Pietzak M, Clemente MG, Tripathi A, Cucca F, Lampis R, Kryszak D, Carteni M, Generoso M, Iafusco D, Prisco F, Laghi F, Riegler G, Carratu R, Counts D, Fasano A. Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes. 2006;55:1443–1449. doi: 10.2337/db05-1593. [DOI] [PubMed] [Google Scholar]
- 269.Rao RK, Seth A, Sheth P. Recent Advances in Alcoholic Liver Disease I. Role of intestinal permeability and endotoxemia in alcoholic liver disease. Am J Physiol Gastrointest Liver Physiol. 2004;286:G881–G884. doi: 10.1152/ajpgi.00006.2004. [DOI] [PubMed] [Google Scholar]
- 270.Keshavarzian A, Holmes EW, Patel M, Iber F, Fields JZ, Pethkar S. Leaky gut in alcoholic cirrhosis: a possible mechanism for alcohol-induced liver damage. Am J Gastroenterol. 1999;94:200–207. doi: 10.1111/j.1572-0241.1999.00797.x. [DOI] [PubMed] [Google Scholar]
- 271.Fujimoto M, Uemura M, Nakatani Y, Tsujita S, Hoppo K, Tamagawa T, Kitano H, Kikukawa M, Ann T, Ishii Y, Kojima H, Sakurai S, Tanaka R, Namisaki T, Noguchi R, Higashino T, Kikuchi E, Nishimura K, Takaya A, Fukui H. Plasma endotoxin and serum cytokine levels in patients with alcoholic hepatitis: relation to severity of liver disturbance. Alcohol Clin Exp Res. 2000;24:48S–54S. doi: 10.1111/j.1530-0277.2000.tb04552.x. [DOI] [PubMed] [Google Scholar]
- 272.Nanji AA, Jokelainen K, Fotouhinia M, Rahemtulla A, Thomas P, Tipoe GL, Su GL, Dannenberg AJ. Increased severity of alcoholic liver injury in female rats: role of oxidative stress, endotoxin, and chemokines. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1348–G1356. doi: 10.1152/ajpgi.2001.281.6.G1348. [DOI] [PubMed] [Google Scholar]
- 273.Mathurin P, Deng QG, Keshavarzian A, Choudhary S, Holmes EW, Tsukamoto H. Exacerbation of alcoholic liver injury by enteral endotoxin in rats. Hepatology. 2000;32:1008–1017. doi: 10.1053/jhep.2000.19621. [DOI] [PubMed] [Google Scholar]
- 274.Nanji AA, Khettry U, Sadrzadeh SM. Lactobacillus feeding reduces endotoxemia and severity of experimental alcoholic liver (disease) Proc Soc Exp Biol Med. 1994;205:243–247. doi: 10.3181/00379727-205-43703. [DOI] [PubMed] [Google Scholar]
- 275.Adachi Y, Moore LE, Bradford BU, Gao W, Thurman RG. Antibiotics prevent liver injury in rats following long-term exposure to ethanol. Gastroenterology. 1995;108:218–224. doi: 10.1016/0016-5085(95)90027-6. [DOI] [PubMed] [Google Scholar]
- 276.Bode C, Bode JC. Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol. 2003;17:575–592. doi: 10.1016/S1521-6918(03)00034-9. [DOI] [PubMed] [Google Scholar]
- 277.Parlesak A, Schafer C, Schutz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000;32:742–747. doi: 10.1016/S0168-8278(00)80242-1. [DOI] [PubMed] [Google Scholar]
- 278.Keshavarzian A, Fields JZ, Vaeth J, Holmes EW. The differing effects of acute and chronic alcohol on gastric and intestinal permeability. Am J Gastroenterol. 1994;89:2205–2211. [PubMed] [Google Scholar]
- 279.Camilleri M, Gorman H. Intestinal permeability and irritable bowel syndrome. Neurogastroenterol Motil. 2007;19:545–552. doi: 10.1111/j.1365-2982.2007.00925.x. [DOI] [PubMed] [Google Scholar]
- 280.Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702. doi: 10.1053/j.gastro.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 281.Collins SM. Dysregulation of peripheral cytokine production in irritable bowel syndrome. Am J Gastroenterol. 2005;100:2517–2518. doi: 10.1111/j.1572-0241.2005.00246.x. [DOI] [PubMed] [Google Scholar]
- 282.Piche T, Barbara G, Aubert P, Bruley des Varannes S, Dainese R, Nano JL, Cremon C, Stanghellini V, Giorgio R, Galmiche JP, Neunlist M. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009;58:196–201. doi: 10.1136/gut.2007.140806. [DOI] [PubMed] [Google Scholar]
- 283.Alonso C, Guilarte M, Vicario M, Ramos L, Ramadan Z, Antolin M, Martinez C, Rezzi S, Saperas E, Kochhar S, Santos J, Malagelada JR. Maladaptive intestinal epithelial responses to life stress may predispose healthy women to gut mucosal inflammation. Gastroenterology. 2008;135(163–172):e161. doi: 10.1053/j.gastro.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 284.Mazzon E, Crisafulli C, Galuppo M, Cuzzocrea S. Role of peroxisome proliferator-activated receptor-alpha in ileum tight junction alteration in mouse model of restraint stress. Am J Physiol Gastrointest Liver Physiol. 2009;297:G488–G505. doi: 10.1152/ajpgi.00023.2009. [DOI] [PubMed] [Google Scholar]
- 285.Estienne M, Claustre J, Clain-Gardechaux G, Paquet A, Tache Y, Fioramonti J, Plaisancie P. Maternal deprivation alters epithelial secretory cell lineages in rat duodenum: role of CRF-related peptides. Gut. 2010;59:744–751. doi: 10.1136/gut.2009.190728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Soderholm JD, Yang PC, Ceponis P, Vohra A, Riddell R, Sherman PM, Perdue MH. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- 287.Berin MC, Sicherer S. Food allergy: mechanisms and therapeutics. Curr Opin Immunol. 2011;23:794–800. doi: 10.1016/j.coi.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 288.Ventura MT, Polimeno L, Amoruso AC, Gatti F, Annoscia E, Marinaro M, Di Leo E, Matino MG, Buquicchio R, Bonini S, Tursi A, Francavilla A. Intestinal permeability in patients with adverse reactions to food. Dig Liver Dis. 2006;38:732–736. doi: 10.1016/j.dld.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 289.Andre C, Andre F, Colin L, Cavagna S. Measurement of intestinal permeability to mannitol and lactulose as a means of diagnosing food allergy and evaluating therapeutic effectiveness of disodium cromoglycate. Ann Allergy. 1987;59:127–130. [PubMed] [Google Scholar]
- 290.Brandt EB, Strait RT, Hershko D, Wang Q, Muntel EE, Scribner TA, Zimmermann N, Finkelman FD, Rothenberg ME. Mast cells are required for experimental oral allergen-induced diarrhea. J Clin Invest. 2003;112:1666–1677. doi: 10.1172/JCI19785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Moneret-Vautrin DA, de Korwin JD, Tisserant J, Grignon M, Claudot N. Ultrastructural study of the mast cells of the human duodenal mucosa. Clin Allergy. 1984;14:471–481. doi: 10.1111/j.1365-2222.1984.tb02231.x. [DOI] [PubMed] [Google Scholar]
- 292.Banan A, Zhang LJ, Farhadi A, Fields JZ, Shaikh M, Keshavarzian A. PKC-beta1 isoform activation is required for EGF-induced NF-kappaB inactivation and IkappaBalpha stabilization and protection of F-actin assembly and barrier function in enterocyte monolayers. Am J Physiol Cell Physiol. 2004;286:C723–C738. doi: 10.1152/ajpcell.00329.2003. [DOI] [PubMed] [Google Scholar]