Abstract
Reproductive organs are complex and well-structured tissues essential to perpetuate the species. In mammals, the male and female reproductive organs vary on their organization, morphology and function. Connectivity between cells in such tissues plays pivotal roles in organogenesis and tissue functions through the regulation of cellular proliferation, migration, differentiation and apoptosis. Connexins and pannexins can be seen as major regulators of these physiological processes. In the present review, we assembled several lines of evidence demonstrating that these two families of proteins are essential for male and female reproduction.
Keywords: Connexin, Pannexin, Testis, Ovary, Function
Introduction
Mammalian reproductive systems, essential to perpetuate the species, are different in males and females in terms of organization, morphology and functions. These differences are required to produce the two different male and female gametes, the spermatozoa and the oocyte.
Testes are male gonads having both an endocrine and an exocrine function. The endocrine function is characterized by the synthesis of androgens, which mainly takes place in Leydig cells. On the other hand, the exocrine function occurs in the seminiferous tubules, where spermatogonia proliferate, become spermatocytes by entering meiosis, and, at the end of meiosis, spermatids differentiate into spermatozoa [1]. During this process, termed spermatogenesis, the developing germ cells migrate towards the lumen of the seminiferous tubules and therefore need to cross the blood–testis barrier (BTB), which is formed by adherens, tight and gap junctions between Sertoli cells. Proliferation and differentiation of germ cells are supported by Sertoli cells that provide nutrients to germ cells. Moreover, the dialog between Sertoli cells and germ cells is critical to orchestrate the maturation of the latter, which allows the release of numerous mature spermatozoa in the lumen of seminiferous tubules. Importantly, spermatogenesis is a process highly regulated in space and time through endocrine and paracrine effectors and direct cell-to-cell interactions via gap junctions [2]. Interestingly, numerous connexins (Cxs), the single units that form gap junctions, were identified in the testes. In addition, some studies reported the expression of pannexins (Panxs), the single units of pannexin-based hemichannels. There is now clear evidence that Cxs and Panxs tune several key physiological functions, such as cell proliferation, differentiation and apoptosis that play pivotal role in testes functions.
The ovary is the female homologue of the testis and also acts as an endocrine organ. Cyclically, it releases an ovum that may be fertilized by a spermatozoon. The ovarian follicle is the functional structural unit of the ovaries and is composed of an oocyte surrounded by supporting granulosa and theca cells. In contrast to the male system, the ovary contains a limited number of follicles that have the ability to develop and release a mature egg [3]. This process, called folliculogenesis, is critically regulated by gap junctional intercellular communication (GJIC) between the oocyte and the granulosa cells.
The uterus is a unique organ that allows implantation of the embryo and formation of the first fetal organ, namely the placenta. During implantation and placentation, various Cxs play key roles in regulating cell lineage differentiation, proliferation and invasion in several uterine and placental tissues. It is now clear that gap junctions take over important roles in the development of this complex feto-maternal unit and in establishing a successful pregnancy. Finally, during labor, coordinated contractions of the uterus enable expel of the fetus. For this process, electrical coupling of uterine smooth muscle cells at the end of pregnancy is required, which is undoubtedly achieved by the formation and function of gap junctions [4–9].
Gap junctions are membrane-spanning channels that permit the direct cytosolic exchange of small molecules between two adjacent cells [10]. A large set of molecules, such as short peptides, amino acids, ions and second messengers, like cyclic adenosine monophosphate (cAMP) and inositol 1,4,5-trisphosphate, can be exchanged through this intercellular communication system [11]. The channels are built up by two opposing hemichannels or connexons provided by adjacent cells. A connexon is a hexamer of Cxs. The Cx family consists of 21 isoforms in humans [12]. The structure of Cxs is well-known with 4 transmembrane domains, 2 extracellular loops, a cytoplasmic loop, and both amino- and carboxyl-domains cytosolic. The trafficking of Cxs and connexons from the endoplasmic reticulum to the plasma membrane and their degradation and recycling has been broadly studied [13], and requires the involvement of numerous protein–protein interactions [14, 15]. The trafficking and the interaction with their protein partners are central for the regulation of Cx function [13, 14]. Panxs are a family of vertebrate glycoproteins discovered based on their homology to the invertebrate gap junction proteins named innexins [16]. This family is currently composed of 3 isoforms that predominantly exist as large transmembrane channels, which connect the intracellular and extracellular space and thereby permit the passage of signaling molecules, such as adenosine triphosphate (ATP) and ions [17].
In the present paper, we critically review the current knowledge on the expression of Cxs and Panxs as well as their functions in male and female reproductive organs.
Role of connexins and pannexins in male reproductive organs
Connexin and pannexin expression
The testis is a male organ composed of several cell types interconnected through GJIC, allowing the organization of these cells in a well-structured tissue. Importantly, the isotypes of Cxs, which compose the gap junctions, vary depending on the cell types, the species and the developmental stages. Here, we will focus on the expression pattern of Cxs and Panxs within the testis, the epididymis, the seminal vesicles, the prostate and the corpus cavernosum.
Testis
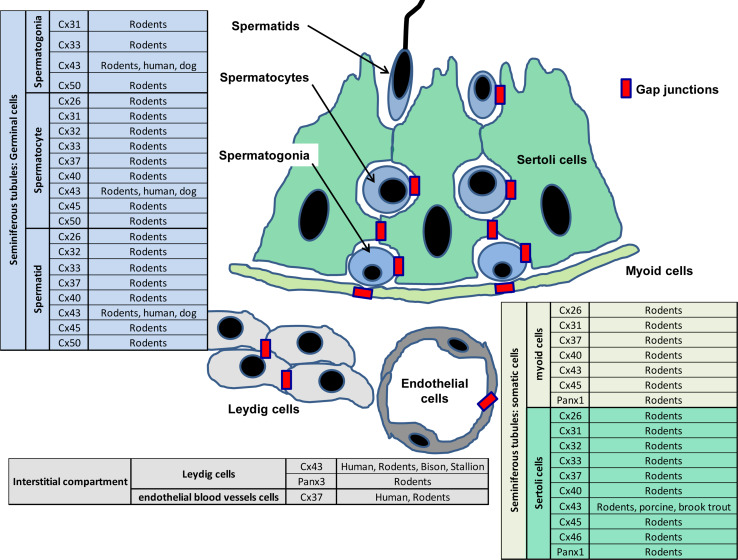
In the testis (Fig. 1), within the interstitial compartment that resides in the space between seminiferous tubules, Leydig cells were found to express exclusively Cx43 in different species, such as human, mouse, rat, guinea pig, European bison, stallion and mink [18–23]. Similarly, in rat Leydig cells, the only Panx isoform detected is Panx3 [24]. The interstitial compartment expresses another Cx isoform, namely Cx37, which was specifically detected in endothelial cells present around blood vessels [18].
Fig. 1.
Connexin and pannexin expression in the testis. The tables summarize the presence of the different Cx and Panx isoforms, which have been identified in the interstitial compartment (gray table), the seminiferous tubules (green table) and the germ cell lineage (blue table) of various species. The red rectangles represent gap junctions
In rodent seminiferous tubules, located at the basis of the tubules, the peritubular myoid (PTM) cells were found to express mRNAs encoding Cx26, Cx31, Cx37, Cx40, Cx43 and Cx45 [18, 25]. However, only Cx43 was so far detected at the protein level in those cells [18, 26]. In rat, PTM cells also express several alternative splicing transcripts of Panx1 [24]. In Sertoli cells, the most important somatic cells in the seminiferous tubules due to their function as nurturing the germ cell lineage, several Cx isoforms were found to be expressed at mRNA and protein levels. Indeed, mRNAs for Cx26, Cx31, Cx32, Cx33, Cx37, Cx40, Cx43 and Cx45 were found in rodents [25, 27, 28], whereas only Cx26, Cx32, Cx33, Cx43 were detected at the protein level [18, 26, 27, 29, 30]. Cx43 was found in Sertoli cells of numerous species, like human, mouse, rat, pork, brook trout and dog [26, 31–34].
In the rodent germ cell lineage, Cx31, Cx33, Cx43 and Cx50 were found in spermatogonia [25, 28, 35, 36]. Cx26, Cx31, Cx32, Cx33, Cx37, Cx40, Cx43, Cx45 and Cx50 have been detected in spermatocytes [25, 35], and Cx26, Cx32, Cx33, Cx37, Cx40, Cx43, Cx45 and Cx50 in spermatids [25, 27, 28, 37]. For other species, however, the knowledge on Cx expression in germ cell lineage is highly limited, since only few studies were performed. Cx43 was detected in human and dog germ cells [33, 34, 38].
During testis development, the expression pattern of Cxs may vary. A single study determined mRNA transcripts for Cxs in 17.5 days postcoitum developing mouse gonads [39]. This study revealed that fetal testes express Cx26, Cx30.3, Cx31, Cx31.1, Cx37, Cx40, Cx45 and Cx46 mRNA. It is noteworthy that Cx32 and Cx50 are undetectable in fetal testis, even if they are present in adult testis [39]. Interestingly, the localization of some Cx isoforms changes during fetal testis development. Indeed, from birth to puberty maturation in rat testes, Cx43 protein expression patterns shift from the apical to the basolateral regions of seminiferous tubules [40]. Similarly, expression patterns of Cxs during the different stages of spermatogenesis, characterized in the seminiferous epithelium by the association of specific germ cells, are also subject to variation in rodents and human [26, 33]. Indeed, the expression of Cx43 decreases in human seminiferous tubules at stages II and III when spermatocytes cross from the basal to the adluminal compartment [33]. In rat seminiferous tubules, the expression of Cx43 strongly drops at stages IX and X [26].
Epididymis
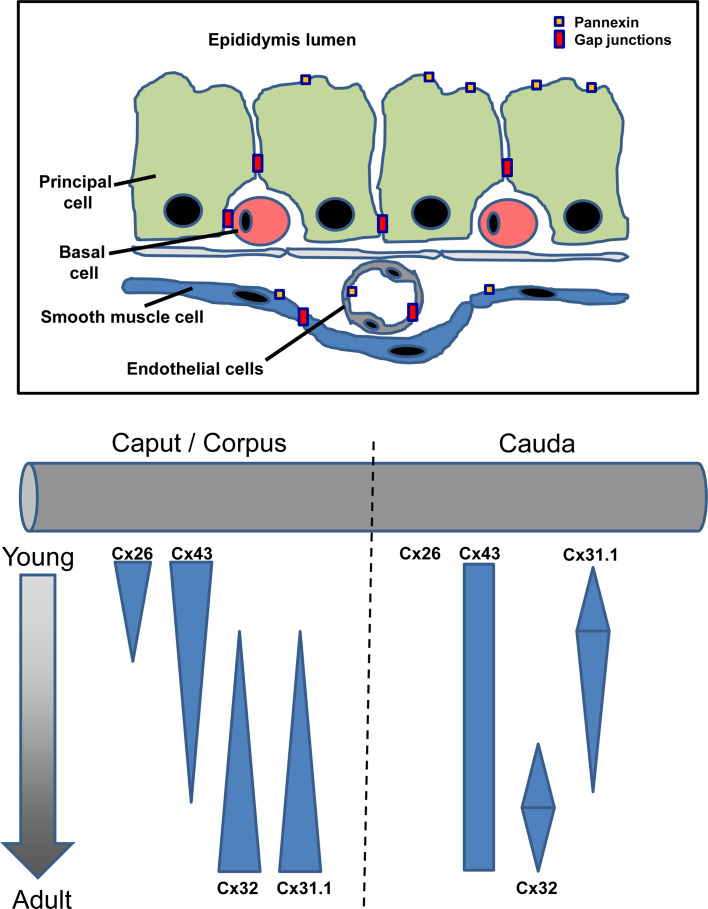
Cx26, Cx30.3, Cx31.1, Cx32 and Cx43 are detectable in the epididymis [41, 42]. This single tightly coiled tube, connecting the efferent ducts from the rear of each testis to the ductus deferens, is composed of 3 segments identified as the caput, the corpus and the cauda. Importantly, the expression of these Cxs within the epididymis is segment-dependent and age-dependent [41]. Indeed, in the proximal region of the epididymis, the expression of both Cx26 and Cx43 is highly elevated in young rats and dramatically decreases during epididymis maturation, whereas both Cx32 and Cx31.1 productions are increasing (Fig. 2). On the other hand, in the cauda, Cx31.1 expression peaks 28 days postnatal and Cx32 amounts culminate 60 days postnatal. Cx43 is stably expressed and Cx26 is barely detectable. Two pannexins, Panx1 and Panx3, are found within the epididymis. As for Cxs, the Panxs are also differentially distributed through the cell types and along the epididymis. Indeed, Panx1 is located in smooth muscle cells all along the epididymis, but its expression in the principal cells is mainly restricted to the caput segment. On the other hand, Panx3 is mostly found in Halo cells and at the apical side of the principal cells [24].
Fig. 2.
Schematic representation of connexin and pannexin expressions along the epididymis during aging. The top panel is a scheme of the localization of gap junctions and Panxs within the epididymis epithelium. The bottom panel is a graphical representation of Cx isoform expression related to age and epididymis position. Two distinct parts of the epididymis, namely the caput/corpus and the cauda, are represented on a gray tube. Maturation from young rodent epididymis to adult and mature epididymis is schematized by an arrow from top to bottom. Expression levels for each connexin isoform are represented by the blue column proportionally varying in thickness
Seminal vesicles
The seminal vesicles are a pair of tubular glands located within the pelvis under the urinary bladder. These seminal vesicles produce a significant amount of fluid for the semen. Only a single study revealed the presence of Cx32 in the epithelial cells of these glands [43]. To date, no study has been performed to analyze the expression pattern of Panxs in seminal vesicles.
Prostate
The prostate is an endocrine gland composed in majority by two cell types, namely epithelial and mesenchymal cells. The epithelial cells participate in the formation of the ducts and the acini, whereas the mesenchymal cells constitute the stroma. In neonatal rat prostate, the yet undifferentiated epithelial cells were found to express Cx43 at the protein level, whereas the mesenchymal cells do not express this Cx isoform. Ten days after birth, the expression of Cx43 has been detected as gradiently changing in developing epithelial ducts. Indeed, when epithelial ducts start to form a lumen around day 15, the expression of Cx43 is restricted to basal epithelial cells. Interestingly, during the reduction of Cx43 production in epithelial ducts, the expression of Cx32 rises. Afterwards, Cx43 decays during maturation of the prostate with concomitant increasing Cx32 expression. Colocalization analyses revealed that Cx32 and Cx43 are not expressed in the same cell types. Thus, Cx43 is expressed in prostatic basal cells, whereas Cx32 is mainly harbored by differentiated luminal cells [44, 45]. In human prostate, the presence of both Cx32 and Cx43 was also reported [46]. Cx43 is detected in smooth muscle interstitial cells of the human prostate [47]. Today, there is no evidence for the presence of Panxs in prostate tissue.
Penis
The corpora cavernosa and corpus spongiosum are penis tissues required for erectile function. These expendable sponge-like tissues, positioned along the penis, are filled with blood during penile erection. The smooth muscle cells in the human corpus cavernosa express Cx43 [48, 49]. At present, it is not known whether Panxs are expressed in the corpus cavernosa.
Implications for male reproductive organogenesis
Organogenesis is a multistep process that requires cellular migration, proliferation and polarization. However, these cellular processes need to be highly controlled in space and time allowing the formation of well-structured organs. In the fetus, the primordial germ cells (PGCs) start to migrate from the umbilicus cord towards the genital ridge. To successfully achieve this migration, PGCs exploit an intrinsic motility program and external guidance cues [50]. Because gap junctions were found to play pivotal roles in neural crest cell migration [51], they are likely to participate in PGC migration. Interestingly, PGCs express Cx43 during their migratory stage to the genital ridge [52]. Strengthening a potent role in migration, mice fetuses lacking Cx43 exhibit a decreased number of PGCs in the genital ridges [53]. Although this was not yet confirmed in mammals, a study performed in Drosophila demonstrates that the knockout of an orthologue/paralogue protein of Cx and Panx, namely innexin4, leads to a defect in PGC migration [54].
The development of the testes also requires intensive Sertoli cell proliferation, which will support the interaction with the germ cell line during spermatogenesis. Our group demonstrated that experimental blockage of GJIC through a pharmacological approach using oleamide and alpha glycyrrhetinic acid alters proliferation of a Sertoli cell line [55]. Subsequently, we confirmed that both Cx43 and Cx32 are implicated in the control of Sertoli cell proliferation by using a specific mimetic peptide approach in primary cultures of rat Sertoli cells [36].
An organ is not just a mass of the correct cell number, but relies on a well-defined cell organization. This organization is highly controlled through adherens and tight junctions that shape both the cellular polarization and the interface between the cells. In a transgenic mouse model deficient for Cx43 specifically in Sertoli cells, we reported reduction of zonula occludens 1 (ZO-1) production along with a strong increase in N-cadherin, beta-catenin and occludin protein levels [56]. This effect, recently confirmed for occludin [57], is cell-autonomous, since similar results were obtained in vitro in a Sertoli cell line [56]. Therefore, GJIC can be seen as a hub of signaling events controlling the essential proteins of the BTB. In addition, a study revealed that Cx43 is an essential player for tight junction reassembly at the BTB through its cyclic remodeling that occurs during spermatogenesis [58].
Implications for endocrine functions
Male steroid hormone synthesis, also termed steroidogenesis, which occurs within the testis, plays a pivotal role in the development of the organism. Indeed, the sexual hormones secreted during this process control primary and secondary sexual differentiation and sexual behavior. Under the control of the luteinizing hormone (LH), released by the anterior pituitary, Leydig cells, located between the seminiferous tubules near the blood vessels, synthesize and secrete testosterone. Through the androgen and follicle-stimulating hormone (FSH) receptor, both testosterone and FSH, released by the pituitary gland, act in synergy on Sertoli cells to push the secretion of inhibin. Gap junctions are found in these two cell types and several lines of evidence highlight Cxs and Panxs as goalkeepers in steroidogenesis production [24, 59].
The first evidence for a potential link between gap junctions and Leydig steroidogenesis comes from the fact that LH treatment of the TM3 Leydig cell line decreases GJIC [60]. In accordance, another study demonstrated that both LH and human chorionic gonadotropin (hCG) hormones are modulating this process via cAMP, Cx43 expression and GJIC [61]. This role of LH and hCG in GJIC regulation was further confirmed in vivo [20]. Stronger evidence was revealed by the work of Li and collaborators, who observed a dramatic reduction of testosterone synthesis in Leydig cells treated with carbenoxolone, a general inhibitor of GJIC [62]. Nevertheless, the Cx isoform involved in this process remains to be determined. Grafting testes from Cx43 knock-out mice under the kidney of castrated adult mice have allowed to determine in vivo that Cx43 is not involved in Leydig cell steroidogenesis [63]. However, the observation that dye coupling in that system was maintained between Leydig cells lacking Cx43 suggests a role of Cx isoforms other than Cx43 [63]. In fact, the involvement of other Cxs was recently confirmed in a study showing the presence of Cx36 and Cx45 in Leydig cells in addition to Cx43. Simultaneously, it was found that specific blockage of Cx36-based and Cx45-based GJIC, but not of Cx43-based GJIC, alters Leydig cell steroidogenesis [62]. Interestingly, immunolocalization revealed that Cx36 is present at cell–cell contacts, whereas Cx45 resides in the cytosol. This result suggests that Cx36 is the only Cx isoform that regulates steroidogenesis through gap junction coupling. However, recent reports indicate that Cxs are also able to control cellular functions through mechanisms independent of GJIC [64]. Therefore, the involvement of Cx45 in steroidogenesis, independent of gap junction coupling, still remains to be elucidated.
The role of Panxs in steroidogenesis has not yet been studied. The only Panx isoform present in Leydig cells is Panx3, but its function in these cells is presently undetermined. Interestingly, in the epididymis, the expression of Panxs parallels that of the androgen receptors [24], supporting a possible link between Panxs and steroidogenesis. In Sertoli cells, the membranous expression of the androgen receptors fulfills a key function in synergizing the effects of FSH. Of note, androgen receptor levels are strongly reduced in Sertoli cells isolated from testes of Sertoli cell-specific Cx43 knock-out mice [65], suggesting a role for Cx43 in androgen receptor signaling pathways.
Implications for spermatogenesis
Spermatogenesis is a physiological process that produces spermatozoa from spermatogonia through cellular proliferation and differentiation. This process highly depends on the communication between Sertoli cells and germ cells. Our group demonstrated that GJIC occurs among Sertoli cells, between Sertoli cells and spermatogonia and between Sertoli cells and early and late spermatocytes, but not between Sertoli cells and spermatids [66]. In addition, we found that communication between Sertoli cells and spermatogonia is unidirectional from the somatic cells to the specific germ cells [66].
GJIC among Sertoli cells is essential in the control of the balance between Sertoli cell differentiation, proliferation and apoptosis [37, 55, 64]. After confirming this effect in primary cultures of Sertoli cells, we demonstrated that both Cx43 and Cx32 are involved in the control of Sertoli cell differentiation [36]. This physiological role of Cx43 was further confirmed in a more recent study showing that not only the expression of Cx43 is required, but in addition that phosphorylation of this Cx at serine368 could be a key event to complete Sertoli cell differentiation [67]. Using a Sertoli cell-specific Cx43 knock-out mice model, two independent groups showed in parallel that Cx43 is crucial for Sertoli cell function [68, 69]. In accordance with our studies, proliferation of Sertoli cells lacking Cx43 was strongly increased [68, 69]. More recently, using the same mouse model, it was found that acute proliferation of Sertoli cells lacking Cx43 is due to failure of these somatic cells to differentiate [70].
GJIC between Sertoli cells and spermatogonia could be essential during the neonatal period to precisely control the number of germ cells connected to differentiated Sertoli cells by regulating apoptosis [36]. Importantly, during adulthood, depletion of Cx43 in rat Sertoli cells leads to an increase in germ cell apoptosis [68, 69, 71]. Interestingly, the effect on germ cell apoptosis after specific Cx43 depletion in Sertoli cells is not recovered in mice lacking Cx43 specifically in spermatogonia, which are viable and fertile [72]. This result suggests that the role of Cx43 in the coupling between Sertoli cells and spermatogonia is rate-limiting at the Sertoli cell side, but not mandatory at the germ cell side.
GJIC between Sertoli cells and spermatocytes could be a major determinant of meiotic progression of spermatocytes. This is supported by the observation that meiotic progression of spermatocytes is dependent on direct and close-contacting interactions between Sertoli cells and spermatocytes [37]. The presence of Cx43 at the interface between these two cell types [37] provides some of the molecular components required for GJIC previously observed between these cell populations [66]. In Sertoli cell-specific Cx43 knock-out mice, a negligible number of spermatogonia manage to differentiate to spermatocytes, but no spermatozoa are produced [68], further supporting the notion that Cx43-based GJIC could participate in the germ cell differentiation process during spermatogenesis. However, a specific study on the role of Cx43 in this process seems to be required to irrevocably prove this role.
During spermatogenesis, remodeling of junctional proteins occurs, since differentiating germ cells need to pass through the BTB. This restructuration process, essential for spermatogenesis [73, 74], occurs during stages VIII–IX of the epithelial cycle to facilitate the transit of spermatocytes. At stage VIII, the expression of Cx43 is at its paroxysm just before a dramatic drop occurs at stage IX [26]. It is important to note that regulation of Cx43 expression levels is controlled, in space and time, in a concomitant manner with BTB restructuration. Recent evidence by our and other groups highlighted the role of gap junctions in the control of BTB component expression levels. Indeed, we observed that the expression of occludin, N-cadherin and beta-catenin are increased in the testis of Sertoli cell-specific Cx43 knock-out mice, whereas the expression of ZO-1 is reduced [56]. We further demonstrated that this effect in Sertoli cells is cell-autonomous and GJIC-independent [56]. The effect of Cx43 on the expression of other components of the BTB was recently confirmed by several studies [57, 58, 75].
Implications for semen production and erectile function
During their transport along the epididymis, spermatozoa undergo maturation [76], which depends on the release of proteins, macromolecules and ions into the lumen of the epididymis. The release of ions can be achieved through specific channels present at the plasma membrane surface. Before the formation of gap junctions, connexons reach the plasma membrane through exocytic vesicles [77]. It has been believed for a long time that these hemichannels are closed until docking to another opposing connexon. However, there is an increasing number of reports demonstrating the existence of plasma membrane connexons in an open form in tissues, such as in the eye and in the central nervous system [78, 79]. These hemichannels allow the exchange of specific molecules, like gliotransmitters [80] or classical molecules that pass through gap junctions, such as ATP, nicotinamide dinucleotide, glutamate, glutathione, prostaglandin, sodium and calcium ions [78, 81]. To date, there is no evidence either demonstrating or excluding a role of hemichannels in the epididymis medium maturation process. However, several isotypes of Cxs found to form or suspected to form hemichannels are present in this tissue. Therefore, it could be postulated that, through the formation of functional hemichannels, Cxs could participate in the regulation of intraluminal epididymis medium composition. In support of this hypothesis, it is interesting to note that Cx43-based hemichannels were found to release prostaglandin E2 [82], a prostaglandin synthesized by the epididymis basal cells to act on principal cells [83, 84]. The role of these hemichannels remains to be elucidated in reproductive organs. Overall, the function of Panxs in male reproduction is less clear than that of Cxs, mainly due to the lack of efficient tools to test their functions, but also because of their more recent discovery. Nevertheless, due to their localization either at the surface of the basal cells or at the apical region of the epididymis, it is possible that Panx1 and Panx3, respectively, participate in the release of PGE2 or ATP in the lumen [84, 85].
Another role for Cxs in the male reproductive system relates to their involvement in erectile function. Cx43 present in smooth muscle cells of the corpus cavernosum participates in the propagation of the electrical signals required to ensure the coordination of the smooth muscle relaxation that conduces to penile erection [48, 49, 86]. This role has been discussed in detail in a previous review [87]. This important function was unambiguously demonstrated by the observation of a negative correlation between Cx43 levels in smooth muscle cells and erectile function in patients [88]. This correlation is of importance to explain the effects of diabetes, age or cigarette smoking on erectile function through their impact on Cx43 expression [88–90].
Role of connexins and pannexins in female reproductive organs
Connexin and pannexin expression
The female reproductive system is composed of the inner reproductive organs, including the ovaries and the uterus, and the external reproductive organ, namely the vagina and the vulva. The internal female reproductive organs serve two distinct functions, including the production of female eggs in the ovaries and the support of the developing embryo in the uterus over gestation. Gap junctions show a very specific spatial–temporal expression pattern in female reproductive tissues, which is linked to the presence of a conceptus as well as to species-specific variations in reproductive strategies. In the following part, focus will be put on the expression pattern of Cxs within the ovarian follicle, the uterine endometrium, preimplantation embryos, the placenta and the uterine myometrium in respect to pregnancy. At present, nothing is known about the expression and role of Panxs in the female reproductive system.
Ovarian follicle
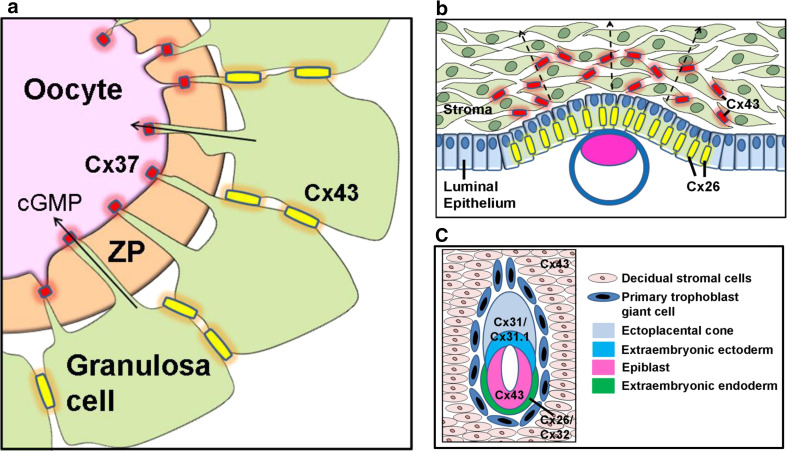
In the ovary of many species, Cx37 and Cx43 are the most abundantly expressed Cxs (Fig. 3a). In the developing mouse follicle, Cx37-based gap junctions connect the oocytes with the surrounding cumulus cells, whereas Cx43-forming channels connect cumulus cells with each other [91, 92]. In human granulosa cells, both Cx37 and Cx43 are expressed, and Cx43 forms channels between granulosa cells [93]. The location of Cx37 expressed by granulosa cells of fertile women remains unknown.
Fig. 3.
a Role of gap junctions in the ovarian follicle. Cx37 and Cx43 are the predominantly expressed Cxs in mammalian follicles. Cx43 forms gap junctions (yellow) between the cumulus cells. Granulosa cells are metabolically coupled with oocytes by transzonal projections from the granulosa cell traversing the zona pellucida (ZP) and forming gap junctions at the oocyte plasma membrane (red). Animal models revealed that Cx37 forms gap junctions at the granulose cell–oocyte interface, which are responsible for the exchange of metabolites and signaling molecules, such as cyclic guanosine monophosphate, important for folliculogenesis. b Induction of gap junctions during implantation. During the receptive phase after ovulation, Cx expression and GJIC are completely repressed in the endometrium by ovarian progesterone. Upon blastocyst attachment, Cx26 expression (yellow) is locally induced in the luminal epithelium and, shortly after Cx43 expression (red), is induced in underlying stromal cells corresponding with formation of the implantation chamber. Cx43 expression further increases through the stromal compartment (arrows), characterizing its transformation into a secretory active decidua. c Connexin expression during lineage formation in the early rodent embryo. With formation of the early lineages, the expression of Cxs becomes immediately restricted to specific lineages. Whereas Cx43 is found in gap junctions throughout the epiblasts, the extraembryonic endoderm expresses Cx26 and Cx32. The proliferating diploid cells of the early trophoblast lineage express Cx31 and Cx31.1, which play critical roles in regulating trophoblast stem cell differentiation and development of the placenta
Endometrium
The endometrium is the inner mucosa of the uterus, consisting of a single layered epithelium and an underlying stroma of connective tissue with uterine glands and embedded vasculature [94]. The luminal epithelium is characterized by the expression of Cx26, whereas the stromal compartment expresses Cx43 in rat [95], mouse [96] and sheep [97] (Fig. 3b). In addition to Cx26, Cx32 expression is found in the endometrial glands of pig [98], in the epithelium layer of baboon [99] and rabbit [100] as well as in basal glandular cells in humans [101].
Preimplantation embryo
The first expression of Cx genes can be detected in the two-cell embryo and functional GJIC is present from the late compaction stage of the 8-cell rodent embryo onwards [102]. Overall, for different species, Cx43 and Cx31 are the predominantly expressed Cxs throughout mammalian preimplantation development (Fig. 3c). In the blastocyst, both isoforms can be found in the trophectoderm and in the inner cell mass in mouse and rat [102, 103], pig [104], cattle and sheep [105] as well as in humans [106, 107]. Cx26 and Cx32 have been described as sporadically expressed in human blastocysts [107], which is potentially due to maturity of the blastocysts [106].
Placenta
The placenta shows an enormous variability in anatomy in eutherian mammals and this is reflected by the species-specific expression of Cxs in this fetal organ. In rodents, proliferative postimplantation trophoblasts within the implantation chamber express Cx31 and Cx31.1. In the mature placenta, Cx31 expression is maintained in proliferative cytotrophoblast cell populations [108], whereas the two multinucleated syncytiotrophoblast layers in the labyrinth layer are connected by Cx26-based channels [96] (Fig. 4a–c). In human, the Cx expression pattern in corresponding stages of early postimplantation trophoblast is unknown. However, in mature placenta, Cx expression is different from rodents. The proliferative extravillous cytotrophoblast (EVT) expresses Cx40 [109], whereas the villous cytotrophoblast is characterized by Cx43 production [110] (Fig. 4d–f).
Fig. 4.
Comparative connexin expression in mouse and human placenta. Humans and rodents have a discoid shaped hemochorial placenta (b, e), where maternal blood has direct contact with fetal trophoblasts. In mice, invasive secondary trophoblast giant cells (TGCs) differentiate from the Cx31-expressing spongiotrophoblast (SpT) cells and erode maternal spiral arteries, ensuring continuous blood flow into the placenta. Cx31-expressing and Cx31.1-expressing glycogen cells invade into the decidua (a). In human placenta, Cx40-expressing cytotrophoblast (CytT) cells are the functional homologues of Cx31-expressing SpT cells. Here, Cx40-expressing cells, detaching from the columns, change from a proliferative to an invasive phenotype. Detached cells loose Cx40 expression and differentiate into TGCs or into endovascular EVT cells, which erodes maternal spiral arteries (d). The exchange of metabolites occurs over a continuous layer of syncytiotrophoblast (SynT) cells. In the mouse (c), mononucleated CytT cells fuse into two layers of SynT cells, which are coupled via large gap junction plaques, composed of Cx26 (yellow). In human placenta, CytT cells express Cx43 (red), which mediates the fusion to a single SynT cell layer (f)
Myometrium
The myometrium is the muscular layer of the uterus, consisting predominantly of myocytes or uterine smooth muscle cells, interspersed stromal cells and vasculature. Cx26 [111], Cx43 [112] and Cx45 [113] have been identified in uterine myocytes of rodents and humans. Cx40 has been additionally described in human [113].
Implications for oogenesis
Several Cxs, specifically Cx26, Cx32, Cx37, Cx43 and Cx45, have been detected in ovarian follicles of different species, including rat, mouse, pig, sheep and cattle [114]. Meanwhile, it is well known that Cx37 and Cx43 are the most abundant Cx proteins in the ovary of many species, which have been extensively explored and stated as being important for follicle development and oocyte growth in mammals [114–117].
Each oocyte develops into a primordial follicle, consisting of a single layer of epithelial granulosa cells and a layer of surrounding mesenchymal theca cells. During further development, granulosa cells proliferate, mediated by growth differentiation factor 9, which belongs to the transforming growth factor beta transcription factor family [118]. In the secondary follicle stage, an antrum forms, which contains various proteins and hormones. This stage characterizes the tertiary follicle, which acquires competence to undergo the first meiosis at ovulation and that can be fertilized [3].
GJIC among granulosa cells and between granulosa cells and oocytes starts in the primordial stage of follicle development and remains throughout the later stages of follicle growth [119]. This cell coupling is necessary for the direct transfer of nutrients, such as amino acids and glucose, between the granulosa cells and the oocytes as well as ions for the regulation of the pH level of the oocytes and cyclic guanosine monophosphate to maintain the oocytes in a state of meiotic arrest [120, 121] (Fig. 3a). The mouse has been a popular experimental species for studying the localization of the different Cxs in the ovary. Cx37 is responsible for metabolic cell coupling of the oocyte–granulosa complex, whereas Cx43-based gap junctions link granulosa cells with each other [91, 92, 122].
The generation of knock-out mice lacking Cx37 and Cx43 has shed light onto the roles of the corresponding gap junctions in oogenesis and follicle development, respectively. In Cx37 knock-out mice, folliculogenesis is arrested at the early antral stage. Oocytes in these mice are not fully developed and fail to achieve full meiotic competence [92]. This study further revealed that granulosa cells of Cx37-null ovaries undergo premature luteinization. Thus, Cx37-based gap junctions are needed to maintain the differentiated state of granulosa cells, preventing them from luteinizing before ovulation [92, 123].
Cx43-deficient mice are not viable and die soon after birth as a result of cardiac failure [124]. To overcome this phenotype for studying folliculogenesis, ovaries were removed from prenatal Cx43 knock-out mice and further developed either in vitro, in organ culture, or in vivo, implanted under the kidney capsule of wild type mice. At any time, folliculogenesis in Cx43-deficient ovaries stops at the primary follicle stage and meiotic maturation or fertilization of oocytes does not occur [53, 125].
In a transgenic mouse approach, Cx43 was specifically deleted from oocytes using zona pellucida-3/Cre-LoxP excision of Cx43. Embryos derived from these Cx43-depleted oocytes develop into the blastocyst stage in an apparently normal fashion, but some fail to implant and both parturition rate and litter size are significantly decreased [126]. Thus, complete deletion of Cx43 in oocytes allows normal oogenesis and folliculogenesis, ovulation and early embryonic development, but severely impairs the implantation capacity of the resulting blastocysts. The implantation failure could possibly be attributed to the reduced expression of Cx43 in the granulosa cells that in turn may lead to corpus luteum insufficiency [126].
To scrutinize the function of Cx37 and Cx43 in oogenesis, chimeric ovaries containing either Cx-null mutant oocytes and wild type granulosa cells, or the reverse combination, were implanted into the renal capsules of immune-deficient female mice [91]. These studies clearly confirmed that Cx43 is not necessary for mouse oocytes to develop into meiotically competent fertilizable gametes, but that Cx37 is indispensable for coupling with granulosa cells during oogenesis [91]. In a recent study, Cx mimetic peptides were used to disrupt GJIC within granulosa cell–oocyte complexes and in isolated cultured antral follicles. This study showed that both Cx37 and Cx43 are required for the meiotic arrest [127]. Nevertheless, the question remains if Cx43 could support oogenesis by forming undocked connexons in the granulosa cell plasma membranes. Those Cx43-based hemichannels could transfer ATP [128] to interact with receptors on adjacent cells, thereby establishing a paracrine signaling route to enhance calcium signals in oocytes [129, 130]. The hypothesis that in granulosa cells the function of Cx43-based hemichannels might be more important for folliculogenesis than Cx43-forming gap junctions was investigated by generating mutant granulosa cells, which can form hemichannels, but no functional gap junctions [131]. These cells were reaggregated with wild type oocytes, which were grafted into host kidneys. The results revealed that undocked Cx43-based hemichannels in ovarian granulosa cells are not able to support follicular development in the same way as their full channel counterparts. This observation supports the necessity of Cx43 to form gap junctions to fulfill its role in folliculogenesis [131].
The expression of Cx37 and Cx43 has also been confirmed in human follicles. However, due to obvious ethical limitations, the exact composition of granulosa cell–oocyte gap junctions during oogenesis is yet unknown [93, 132–134]. Also, the participation of additional Cx members in ovary function remains to be revealed, as Cx32 knock-out females are fertile [135] and Cx26-deficient and Cx45-deficient mice die in utero [136, 137].
Implications for endometrium and implantation
The endometrium shows tight spatial–temporal regulation of Cx26 and Cx43 expression patterns that is under the control of ovarian steroid hormones in rodents and humans (Fig. 3b). After ovulation and during the receptive phase of the endometrium, basal expression levels of both Cxs are repressed by changed estrogen and progesterone levels [95, 101, 138]. Whereas high physiological progesterone levels downregulate Cx expression, estrogen administration in rodents can induce expression of Cx26 and Cx43, a process which is mediated specifically by estrogen receptor alpha [139]. Upon blastocyst attachment, Cx26 is locally induced in the luminal epithelium lining the implantation chamber. This specific local induction of Cx26 during implantation is independent of estrogen receptor signaling and can also be achieved by applying a mechanical stimulus or injecting of oil droplets into the uterus, which simulates the presence of blastocysts [138, 139]. Furthermore, in a delayed implantation rat model where ovarian hormones are experimentally depleted by ovarectomy after fertilization followed by progesterone substitution, the implantation reaction does not take place. However, Cx26 expression is still initiated in the luminal epithelium, showing that presence of a stimulus is sufficient for Cx26 induction and precedes the implantation process [139]. A recent study demonstrated the importance of GJIC for embryo implantation. Uteri of mice injected with carbenoxolone before implantation showed features of delayed implantation with failed blastocyst implantation. Cx26 expression was triggered in the luminal epithelium, albeit to a lower extent. However, in carbenoxolone-treated uteri, the decidualization process was delayed, evidenced by persistent progesterone receptor expression, which normally disappears during decidualization [138]. This shows that carbenoxolone application also influences GJIC in the stromal compartment. This study reveals the importance of endometrial GJIC for blastocyst attachment and successful implantation. However, it is not clear whether this effect is exclusively mediated by Cx26-based channels in the luminal epithelium or if it is a combined effect of general GJIC blockage in uterine tissues. The specific role of Cx32, found to be coexpressed with Cx26 in the endometrial luminal or glandular epithelium of several species, also remains to be investigated.
During pregnancy, the endometrium undergoes a transformation into a secretory tissue, called the decidua. In the stromal compartment of the endometrial layer, Cx43 expression is induced, which is strongly promoted around the implantation chamber and further increased with the ongoing decidualization process [140]. Conditional deletion of Cx43 from the endometrial stroma, using a progesterone receptor/Cre-LoxP deletion approach, resulted in an impaired decidualization process and the loss of pregnancies after 7.5 days postcoitum [141]. The absence of Cx43 impairs the differentiation program of stromal cells, which is indicated by downregulation of the decidual markers prolactin-related protein and prolactin-like protein. In addition, the downregulation of the angiogenic regulators vascular endothelial growth factor and angiopoietin leads to a compromised development of the endothelial network in the Cx43-deficient decidua, which further demonstrates a block in the decidualization process [141].
The importance of Cx43-based channels for proper decidual function has been additionally demonstrated by introducing the dominant Cx43G60S point mutation into mice, which results in intracellular accumulation of mutant and wild type Cx43 protein and more than 50 % reduction in GJIC, knowing to cause various tissue-specific phenotypes [142]. The decidua of Cx43G60S mice displays increased vasculogenesis, accompanied by upregulation of the angiogenic factor vascular endothelial growth factor and its receptors. Furthermore, the placenta shows a mislocation in relation to the eroded uterine spiral artery sinusoids, which explains the growth retardation probably due to abnormal placental blood supply to the embryos. This phenotype is a maternal effect, as it affects wild type embryos implanting into Cx43G60S mothers and since it does not influence stage-specific embryonic development [143]. These two studies demonstrate an important role for Cx43 in the development and function of the decidua in establishing a successful pregnancy. However, both mouse models show differences, in particular delayed differentiation of stromal cells in Cx43del/del mice [141], which is not observed in Cx43G60S mice [143], whereas the opposite holds true for vascularization. This is probably due to the complete lack of Cx43 protein from the initiation of decidualization in one mouse model versus the expression of mutated yet still prevailing protein in the other model [141, 143].
Experiments with human primary stromal endometrial cell cultures treated with the gap junction blockers alpha glycyrrhetinic acid or octanol during hormone-induced decidualization also showed an impaired decidualization process [144]. As in the rodent model, this impairment shows reduced prolactin secretion and vascular endothelial growth factor expression. Interestingly, small interference RNA-mediated knock-down of Cx43 leads to the same morphological and biochemical impaired decidualization, suggesting a role for gap junctions in exchanging small molecules that regulate coordinated differentiation of decidual cells after implantation [144]. Interestingly, in the decidua of patients with recurrent early pregnancy loss, Cx43 expression was found to be reduced, suggesting a potential link with human fertility [145]. In bovine embryo transfer experiments, the endometrium shows a different reaction to cloned embryos compared to fertilized embryos, with low endometrial Cx43 expression in transferred cloned conceptuses, which has a negative effect on placentation [146]. This shows that regulation of Cx43 expression patterns and channel function, controlled either by genetic, hormonal factors or the implanting embryo itself, is a critical factor for establishing a successful pregnancy [144–146].
Implications for preimplantation development
The role of gap junctions in developing preimplantation embryos after fertilization is controversial. During preimplantation development, several Cxs are expressed, thereby showing species-specific and strain-specific variations as well as embryo culture-influenced expression patterns [147] (Fig. 3c). In mouse preimplantation embryos, disruption of GJIC by alpha glycyrrhetinic acid leads to complete absence of dye coupling, but does not affect blastocyst formation in vitro [103, 148]. In addition, the generation of gene-deficient mice revealed that none of the individual Cxs are essential for preimplantation development [147]. Moreover, absence of both Cx31 and Cx43, the predominant and continuously expressed Cx isoforms, has no obvious effect on preimplantation development and leads to normal implantation in the Cx31/Cx43 double gene-deficient mice [149]. The absence of any obvious preimplantation embryo phenotype in transgenic mouse models led to the assumption that specific Cx expression patterns accompany the preparation of the embryo for postimplantation development, where a rapid segregation of Cxs can be observed between the embryo, the trophoblast lineage and the visceral yolk sac immediately during the implantation process (Fig. 3c) [150]. It has been discussed that this rapid restriction of Cx expression patterns to the specific embryonic and extraembryonic lineages allows the formation of isolated communication compartments, which might influence developmental processes [150–152]. However, the generation of several knock-in mice revealed that Cx43 can be substituted by Cx26 [153], Cx31 [154] or Cx32 [155], without affecting preimplantation and postimplantation embryonic development. In particular, the Cx43KI31 mouse showed normal postimplantation embryo development and trophoblast lineage formation [154]. Thus, no obvious function for GJIC or specific Cxs in preimplantation embryos could be found when focusing on classic mutant mouse models. However, it is well known that embryo culture conditions used in assisted reproduction in humans and cattle influence gene expression profiles with impact on embryonic development and adult life [156]. Cx43 expression is known to be reduced during in vitro culture of bovine embryos [157, 158] and junctional conductance is lower in in vitro-produced bovine embryos [159]. Vice versa, recent studies show that upregulation of Cx43 in in vitro-cultured bovine embryos promotes their development, suggesting that Cx43 is a positive marker for bovine embryo culture [160]. Thus, GJIC and connexin expression might have more sophisticated metabolic effects on uterine preimplantation or peri-implantation development, or embryonic/fetal growth in farm animals and humans that differ from what is observed in mutant mouse models focusing on classic developmental or anatomical effects.
Implications for placentation and placental function
The placenta is the first fetal organ that connects the embryo with the mother. Although it serves the same function in all mammals, namely the exchange of nutrients, gas and excretion products, the anatomy and the expression of Cxs varies between species. Humans and rodents both have a discoid shaped hemochorial placenta, where the trophoblast has direct contact with maternal blood and invades the maternal uterine spiral arteries [161, 162].
During implantation, the trophectoderm of the blastocytes starts expanding and differentiating into different proliferating trophoblast populations. In mouse, these early postimplantation trophoblasts are characterized by coexpression of Cx31 and Cx31.1 (Fig. 3c) [163, 164]. Several studies showed that Cx31 and Cx31.1 play a critical and coordinated role in trophoblast differentiation in these early stages of mouse placental development (Fig. 4a–c). Inactivation of Cx31 or Cx31.1 gene production leads to loss of conceptuses around midgestation. Specifically, 60 % of Cx31-deficient embryos and 30 % of Cx31.1-deficient embryos die between 10.5 and 13.5 days postcoitum, and surviving embryos and newborns show growth restriction. In both mutant mice, placental sizes are strongly reduced due to a shift in placental trophoblast subpopulations [108, 164]. Cx31 knock-out placentas show strongly reduced size of labyrinth and spongiotrophoblast layers, and an increased number of parietal secondary trophoblast giant cells [108]. Further in vitro analysis of Cx31-deficient trophoblast stem cell lines pointed out that Cx31 supports the stem cell state and maintains the proliferative capacity by delaying terminal trophoblast lineage differentiation [165]. Cx31.1-deficient placentas also display a reduction in labyrinth size and fetal blood spaces, but a reduced number of parietal trophoblast giant cells. In addition, analysis of Cx31.1-deficient trophoblast stem cell lines revealed that Cx31.1, in contrast to Cx31, supports the terminal differentiation of trophoblasts at the expense of proliferation [166]. This clearly shows that both Cxs have opposite effects on stem cell fate and proliferation during early trophoblast differentiation in mouse by balancing the terminal differentiation into the placental trophoblast subpopulations [166]. This suggest that these two coexpressed Cx isoforms coordinately regulate the physiological trophoblast differentiation process, rather than competing for the same function or just having redundant effects [166].
The subpopulations of the placenta are formed when the extraembryonic mesoderm invades the Cx31/Cx31.1-expressing chorion trophoblasts, forming placental mesenchyme and fetal blood vessels. This triggers trophoblast cells to elongate and fuse, and to build the multinucleated syncytiotrophoblast in the labyrinth layer. The syncytiotrophoblast forms the main placental barrier between the maternal blood and the fetal capillaries, which are formed by the invading mesoderm [162]. The rodent placenta, in contrast to the primate placenta, is composed of two layers of syncytiotrophoblasts that are connected by Cx26-based channels [96]. Inactivation of the Cx26 gene leads to strong growth retardation of conceptuses followed by embryonic death at 9.5 days postcoitum due to reduced glucose over the placental barriers [136]. Thus, Cx26-forming gap junctions act as metabolic channels for the exchange of small molecules, like glucose, over this placental barrier. Metabolites are actively transported by specific transporters from the maternal blood into syncytiotrophoblast layer I and can passively diffuse along a gradient through Cx26-based channels into syncytiotrophoblast layer II from where specific transporters translocate them to the fetal side (Fig. 4c) [136].
At the feto-maternal interface, the trophoblasts differentiate into secondary polyploid trophoblast giant cells and glycogen cells. Trophoblast giant cells invade the maternal decidua and are involved in transforming maternal spiral arteries to ensure placental blood circulation [167]. In murine placenta, Cx31 and Cx31.1 expression is maintained in placental glycogen cells, which differentiate at the feto-maternal interface at midgestation and invade into the decidua. The exact role of this cell type and the impact of Cx31 and Cx31.1 on this cell population are unknown [168–170].
The extraembryonic mesoderm forming fetal vasculature in the yolk sac and the placenta expresses Cx45. Cx45 knock-out mice show reduced invasion of mesenchyme into the labyrinth with enlarged fetal blood vessels and less vascular branching compared to control animals. In addition, development of vasculature in the yolk sac of Cx45-deficient conceptuses is severely impaired, probably by a strong reduction of transforming growth factor beta signaling pathways associated with embryonic death between 9.5 and 10.5 days postcoitum [137].
In conclusion, several mutant mouse models clearly show that Cxs are critical for placental development and function covering different cellular functions, namely controlling trophoblast lineage differentiation processes, allowing metabolic coupling or regulating vasculogenesis [136, 137, 166].
The human placenta differs not only morphologically from the rodent placenta, but also in the composition of the different Cx isoforms that are responsible for various functions during development of the placenta [169]. Several studies have identified analogous cell types among the human and rodent trophoblasts, including proliferative and invasive trophoblast cells and trophoblast cells that have the ability to fuse into a syncytium. In human placenta, the chorionic villi are the structural and functional units. The floating villi are composed of fetal vessels, surrounded by trophoblasts and bathing in maternal blood in the intervillous space, and act as a site of nutrient exchange between the mother and the fetus, equivalent to the mouse labyrinth layer. In contrast to rodents, the human placenta contains a single layer of syncytiotrophoblasts, with underlying cytotrophoblast cells that continuously fuse to maintain the syncytiotrophoblast layer. The anchoring villi attach the placenta to the maternal decidua. Here, at the side of the cell columns, EVT cells originate and invade into the maternal decidua. These cells are called interstitial EVT cells. A subpopulation invades the uterine spiral arteries of the myometrium, called endovascular trophoblasts, which leads to transformation of these vessels from small resistance vessels to high-caliber capacitance vessels to support sufficient fetal growth [171]. Analogous to the invasive polyploidy trophoblast giant cells in the mouse placenta, these extravillous mononucleated trophoblast cells erode the endothelium of maternal spiral arteries to establish the utero-placental circulation. The other subpopulation of interstitial invasive EVT cells deeply invades into the decidua and fuses to multinucleated giant cells in the placental bed after completion of invasion [172].
In the human placenta, Cx43 is located in cytotrophoblast cells and mediates cellular fusion of the cytotrophoblasts into multinucleated syncytiotrophoblasts (Fig. 4d–f) [110, 172–175]. A recent study supports a central role for Cx43 in mediating both GJIC and protein–protein interactions via the transcription factor Drosophila glial cell missing gene 1 and its downstream target human endogenous retrovirus envelope protein/syncytin-1 with its receptor neutral amino acid transporter B(0) to stimulate trophoblast cell fusion [176]. Here, the carboxyterminal tail of Cx43 seems to be required for proper cell fusion, since a truncated Cx43 protein, which forms functional gap junctions, did not enable cAMP-mediated fusion [176–178]. Detailed analysis of the Cx43 signaling process involved in cytotrophoblast fusion revealed that a protein kinase A-ezrin-Cx43 signaling complex is necessary for discrete control of Cx43 phosphorylation and hCG-stimulated GJIC that triggers cell fusion [179]. As there is only a single syncytial trophoblast layer in humans compared to two layers in mouse placenta, GJIC is probably not necessary for transplacental transport (Fig. 4f) [169].
Cx40 characterizes the proximal EVT cell population of the cell columns in the anchoring villi (Fig. 4d–e) [109, 180]. During the invasion process of the EVT cells into the decidual tissue, Cx40 expression is repressed. Cx40 is also found in the malignant EVT cell lines BeWo and JAr, two experimental model systems for investigating the role of Cx40 in trophoblast proliferation and invasion, showing that Cx40 positively regulates cell proliferation [180–182]. Moreover, using placental organ explant cultures, proliferation of EVT cells was found to be reduced when placental explants were either treated with GJIC inhibitors or when Cx40 expression was silenced using small interfering RNA duplexes. This confirms that Cx40 supports proliferation of proximal EVT cells, inhibiting them from differentiating into the invasive pathway [182]. Thus, Cx40 in the human placenta has analogous functions to Cx31 in the mouse placenta in maintaining a proliferative phenotype of trophoblasts. Future experiments have to answer the question how Cxs contribute to the development of placental diseases, such as preeclampsia, which are associated with an imbalance between trophoblast proliferation and differentiation, and that have an enormous impact on pregnancy outcomes for both the baby and the mother [169].
Implications for myometrium and labor
The myometrium is the muscular layer of the uterus, consisting predominantly of uterine smooth muscle cells with interspersed stromal cells and vasculature. During pregnancy, it undergoes dramatic changes to acquire physiological properties required for labor [4]. The strong upregulation of gap junctions right before the onset of labor ensures coordinated uterine contractions to deliver the fetus [112]. Three different Cxs have been described in rodent and human uterine myocytes, namely Cx26 [111], Cx43 [112] and Cx45 [5]. Cx26 expression increases from midgestation, peaks at late pregnancy and declines to basal levels before the onset of labor. In contrast to Cx43, this increase in Cx26 is dependent on the presence of progesterone [112]. Cx45 is present in nonpregnant and early pregnant myometrium and decreases before term [5]. Cx40 has been detected in human myometrial myocytes, but no information is available about its regulation during pregnancy [113].
Cx43 is the major gap junction protein responsible for the establishment of electrical coupling of uterine myocytes at the end of pregnancy [6]. Cx43 shows low expression levels in the nonpregnant uterus and during gestation, but displays strongly increased production and associated gap junction formation at the end of pregnancy associated with the onset of labor [7]. Cx43 belongs to a group of contractile-associated proteins, similar to the oxytocin receptor and prostaglandin F receptor, which mark the change from quiescence to the activated state of term labor myometrium [8]. The regulation of Cx43 is under the control of ovarian steroid hormones. High levels of progesterone during gestation repress Cx43 expression, whereas the sudden decline of progesterone at the end of pregnancy leads to an increase in Cx43 amounts [7]. In addition, mechanical stretch by the growing fetus on the myometrium has a positive effect on Cx43 production, but not on Cx26 expression [7]. While the role of the tightly regulated Cx26 expression in the uterus for pregnancy is not yet understood, the importance of Cx43 for labor has been demonstrated using mutant mouse models. The smooth muscle cell-specific Cre-loxP deletion of Cx43 leads to a strong reduction in its expression and decreased coupling of myocytes. Parturition is impaired in these animals with prolonged gestational length and partial death of fetuses in utero [9]. This demonstrates the importance of Cx43 for myometrial function and labor. Experiments with Cx43G60S mutant mice have substantiated these findings. Indeed, this mutation downregulates Cx43 expression and reduces gap junction presence in the laboring myometrium of Cx43G60S mice, which impairs parturition with decreased uterine contractions, prolonged gestational length and partly retained fetuses and placentas [183]. Although labor is strongly impaired in these mice, it is not completely abolished. In both models, dams could still give birth to pups, which could be due to the remaining expression of other Cx isoforms backing up for GJIC either among uterine myocytes or with interstitial stromal cells [183]. The regulation of myometrial Cx43 expression is regulated by transcription factors of the c-jun/c-fos family, which bind to activator protein-1 sites in the Cx43 gene promoter [184]. These transcription factors can form complexes with ligated progesterone receptors and block gene transcription of Cx43 in rodents and humans [185, 186]. The fact that Cx43-based channels play key roles in the onset of contractions during labor makes them potential targets for pharmaceutical interventions in managing complications, such as the development of premature contractions and preterm labor.
Conclusions and perspectives
In this review, the roles of Cxs, Panxs and their channels in male and female reproductive organs have been discussed. The pivotal functions of Cxs and Panxs in various cellular processes, such as proliferation, migration, differentiation and apoptosis, that shape the organs and that drive their overall functionality, have been addressed. As master regulators of these important physiological functions, it is likely that alterations of the production and activity of these crucial proteins may underlie pathogenesis. In this respect, a plethora of reports already demonstrated defective GJIC during reproductive pathologies [187–189]. By contrast, the localization and the function of Panxs in male and female reproductive organs remain largely unknown. Therefore, the impact of Panx-related defects on reproductive functions is impossible to estimate at present. It seems necessary to direct future research in a way that will allow to increase the basic knowledge on these proteins and to exploit our knowledge to address Cxs and Panxs as potential targets in therapeutic approaches.
Acknowledgments
This work was supported by the “Institut National de la Santé et de la Recherche Medicale” (INSERM-France), by the “Deutsche Forschungsgemeinschaft” (DFG KI1278/1-1) and by the Institute of Anatomy and Molecular Biology (University of Duisburg-Essen).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
Abbreviations
- ATP
Adenosine triphosphate
- BTB
Blood–testis barrier
- cAMP
Cyclic adenosine monophosphate
- Cx(s)
Connexin(s)
- EVT
Extravillous cytotrophoblast
- FSH
Follicle-stimulating hormone
- GJIC
Gap junctional intercellular communication
- hCG
Human chorionic gonadotropin
- LH
Luteinizing hormone
- Panx(s)
Pannexin(s)
- PGCs
Primordial germ cells
- PTM
Peritubular myoid
- ZO-1
Zonula occludens 1
References
- 1.Clermont Y. Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and spermatogonial renewal. Physiol Rev. 1972;52(1):198–236. doi: 10.1152/physrev.1972.52.1.198. [DOI] [PubMed] [Google Scholar]
- 2.Pointis G, Segretain D. Role of connexin-based gap junction channels in testis. Trends Endocrinol Metab. 2005;16(7):300–306. doi: 10.1016/j.tem.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Kidder GM, Vanderhyden BC. Bidirectional communication between oocytes and follicle cells: ensuring oocyte developmental competence. Can J Physiol Pharmacol. 2010;88(4):399–413. doi: 10.1139/y10-009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shynlova O, Tsui P, Jaffer S, Lye SJ. Integration of endocrine and mechanical signals in the regulation of myometrial functions during pregnancy and labour. Eur J Obstet Gynecol Reprod Biol. 2009;144(Suppl 1):S2–S10. doi: 10.1016/j.ejogrb.2009.02.044. [DOI] [PubMed] [Google Scholar]
- 5.Albrecht JL, Atal NS, Tadros PN, Orsino A, Lye SJ, Sadovsky Y, Beyer EC. Rat uterine myometrium contains the gap junction protein connexin45, which has a differing temporal expression pattern from connexin43. Am J Obstet Gynecol. 1996;175(4 Pt 1):853–858. doi: 10.1016/s0002-9378(96)80012-3. [DOI] [PubMed] [Google Scholar]
- 6.Sakai N, Tabb T, Garfield RE. Studies of connexin 43 and cell-to-cell coupling in cultured human uterine smooth muscle. Am J Obstet Gynecol. 1992;167(5):1267–1277. doi: 10.1016/s0002-9378(11)91699-8. [DOI] [PubMed] [Google Scholar]
- 7.Ou CW, Orsino A, Lye SJ. Expression of connexin-43 and connexin-26 in the rat myometrium during pregnancy and labor is differentially regulated by mechanical and hormonal signals. Endocrinology. 1997;138(12):5398–5407. doi: 10.1210/endo.138.12.5624. [DOI] [PubMed] [Google Scholar]
- 8.Carbillon L, Seince N, Uzan M. Myometrial maturation and labour. Ann Med. 2001;33(9):571–578. [PubMed] [Google Scholar]
- 9.Doring B, Shynlova O, Tsui P, Eckardt D, Janssen-Bienhold U, Hofmann F, Feil S, Feil R, Lye SJ, Willecke K. Ablation of connexin43 in uterine smooth muscle cells of the mouse causes delayed parturition. J Cell Sci. 2006;119(Pt 9):1715–1722. doi: 10.1242/jcs.02892. [DOI] [PubMed] [Google Scholar]
- 10.Kumar NM, Gilula NB. The gap junction communication channel. Cell. 1996;84(3):381–388. doi: 10.1016/s0092-8674(00)81282-9. [DOI] [PubMed] [Google Scholar]
- 11.Bruzzone R, White TW, Paul DL. Connections with connexins: the molecular basis of direct intercellular signaling. Eur J Biochem. 1996;238(1):1–27. doi: 10.1111/j.1432-1033.1996.0001q.x. [DOI] [PubMed] [Google Scholar]
- 12.Sohl G, Willecke K. An update on connexin genes and their nomenclature in mouse and man. Cell Commun Adhes. 2003;10(4–6):173–180. doi: 10.1080/cac.10.4-6.173.180. [DOI] [PubMed] [Google Scholar]
- 13.Gilleron J, Carette D, Chevallier D, Segretain D, Pointis G. Molecular connexin partner remodeling orchestrates connexin traffic: from physiology to pathophysiology. Crit Rev Biochem Mol Biol. 2012;47(5):407–423. doi: 10.3109/10409238.2012.683482. [DOI] [PubMed] [Google Scholar]
- 14.Herve JC, Bourmeyster N, Sarrouilhe D, Duffy HS. Gap junctional complexes: from partners to functions. Prog Biophys Mol Biol. 2007;94(1–2):29–65. doi: 10.1016/j.pbiomolbio.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Herve JC, Derangeon M, Sarrouilhe D, Giepmans BN, Bourmeyster N. Gap junctional channels are parts of multiprotein complexes. Biochim Biophys Acta 1818. 2012;8:1844–1865. doi: 10.1016/j.bbamem.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Panchin Y, Kelmanson I, Matz M, Lukyanov K, Usman N, Lukyanov S. A ubiquitous family of putative gap junction molecules. Curr Biol. 2000;10(13):R473–R474. doi: 10.1016/s0960-9822(00)00576-5. [DOI] [PubMed] [Google Scholar]
- 17.Penuela S, Gehi R, Laird DW. The biochemistry and function of pannexin channels. Biochim Biophys Acta 1828. 2013;1:15–22. doi: 10.1016/j.bbamem.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 18.Risley MS, Tan IP, Roy C, Saez JC. Cell-, age- and stage-dependent distribution of connexin43 gap junctions in testes. J Cell Sci. 1992;103(Pt 1):81–96. doi: 10.1242/jcs.103.1.81. [DOI] [PubMed] [Google Scholar]
- 19.Pelletier RM. The distribution of connexin43 is associated with the germ cell differentiation and with the modulation of the Sertoli cell junctional barrier in continual (guinea pig) and seasonal breeders’ (mink) testes. J Androl. 1995;16(5):400–409. [PubMed] [Google Scholar]
- 20.You S, Li W, Lin T. Expression and regulation of connexin43 in rat Leydig cells. J Endocrinol. 2000;166(2):447–453. doi: 10.1677/joe.0.1660447. [DOI] [PubMed] [Google Scholar]
- 21.Kotula-Balak M, Hejmej A, Sadowska J, Bilinska B. Connexin 43 expression in human and mouse testes with impaired spermatogenesis. Eur J Histochem. 2007;51(4):261–268. [PubMed] [Google Scholar]
- 22.Hejmej A, Kopera I, Kotula-Balak M, Gizejewski Z, Bilinska B. Age-dependent pattern of connexin43 expression in testes of European bison (Bison bonasus, L.) J Exp Zool A Ecol Genet Physiol. 2009;311(9):667–675. doi: 10.1002/jez.554. [DOI] [PubMed] [Google Scholar]
- 23.Hejmej A, Kotula-Balak M, Sadowska J, Bilinska B. Expression of connexin 43 protein in testes, epididymides and prostates of stallions. Equine Vet J. 2007;39(2):122–127. doi: 10.2746/042516407x169393. [DOI] [PubMed] [Google Scholar]
- 24.Turmel P, Dufresne J, Hermo L, Smith CE, Penuela S, Laird DW, Cyr DG. Characterization of pannexin1 and pannexin3 and their regulation by androgens in the male reproductive tract of the adult rat. Mol Reprod Dev. 2011;78(2):124–138. doi: 10.1002/mrd.21280. [DOI] [PubMed] [Google Scholar]
- 25.Risley MS. Connexin gene expression in seminiferous tubules of the Sprague-Dawley rat. Biol Reprod. 2000;62(3):748–754. doi: 10.1095/biolreprod62.3.748. [DOI] [PubMed] [Google Scholar]
- 26.Gilleron J, Carette D, Carpentier F, Segretain D, Pointis G. Three-dimensional analysis of connexin43 gap junction in the ex vivo rat seminiferous tubules: short-term effects of hormonal effectors. Microsc Res Tech. 2009;72(11):845–855. doi: 10.1002/jemt.20731. [DOI] [PubMed] [Google Scholar]
- 27.Fischer P, Brehm R, Konrad L, Hartmann S, Kliesch S, Bohle RM, Bergmann M. Connexin 33: a rodent-specific member of the gap junction protein family? J Androl. 2005;26(1):75–84. [PubMed] [Google Scholar]
- 28.Batias C, Siffroi JP, Fenichel P, Pointis G, Segretain D. Connexin43 gene expression and regulation in the rodent seminiferous epithelium. J Histochem Cytochem. 2000;48(6):793–805. doi: 10.1177/002215540004800608. [DOI] [PubMed] [Google Scholar]
- 29.Fiorini C, Mograbi B, Cronier L, Bourget I, Decrouy X, Nebout M, Ferrua B, Malassine A, Samson M, Fenichel P, Segretain D, Pointis G. Dominant negative effect of connexin33 on gap junctional communication is mediated by connexin43 sequestration. J Cell Sci. 2004;117(Pt 20):4665–4672. doi: 10.1242/jcs.01335. [DOI] [PubMed] [Google Scholar]
- 30.Carette D, Gilleron J, Decrouy X, Fiorini C, Diry M, Segretain D, Pointis G. Connexin 33 impairs gap junction functionality by accelerating connexin 43 gap junction plaque endocytosis. Traffic. 2009;10(9):1272–1285. doi: 10.1111/j.1600-0854.2009.00949.x. [DOI] [PubMed] [Google Scholar]
- 31.de Montgolfier B, Audet C, Cyr DG. Regulation of the connexin 43 promoter in the brook trout testis: role of the thyroid hormones and cAMP. Gen Comp Endocrinol. 2011;170(1):110–118. doi: 10.1016/j.ygcen.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 32.Roger C, Mograbi B, Chevallier D, Michiels JF, Tanaka H, Segretain D, Pointis G, Fenichel P. Disrupted traffic of connexin 43 in human testicular seminoma cells: overexpression of Cx43 induces membrane location and cell proliferation decrease. J Pathol. 2004;202(2):241–246. doi: 10.1002/path.1509. [DOI] [PubMed] [Google Scholar]
- 33.Steger K, Tetens F, Bergmann M. Expression of connexin 43 in human testis. Histochem Cell Biol. 1999;112(3):215–220. doi: 10.1007/s004180050409. [DOI] [PubMed] [Google Scholar]
- 34.Ruttinger C, Bergmann M, Fink L, Pesch S, Seitz K, Trautmann A, Steger K, Konrad L, Brehm R. Expression of connexin 43 in normal canine testes and canine testicular tumors. Histochem Cell Biol. 2008;130(3):537–548. doi: 10.1007/s00418-008-0432-9. [DOI] [PubMed] [Google Scholar]
- 35.Mok BW, Yeung WS, Luk JM. Differential expression of gap-junction gene connexin 31 in seminiferous epithelium of rat testes. FEBS Lett. 1999;453(3):243–248. doi: 10.1016/s0014-5793(99)00714-0. [DOI] [PubMed] [Google Scholar]
- 36.Gilleron J, Carette D, Durand P, Pointis G, Segretain D. Connexin 43 a potential regulator of cell proliferation and apoptosis within the seminiferous epithelium. Int J Biochem Cell Biol. 2009;41(6):1381–1390. doi: 10.1016/j.biocel.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Godet M, Sabido O, Gilleron J, Durand P. Meiotic progression of rat spermatocytes requires mitogen-activated protein kinases of Sertoli cells and close contacts between the germ cells and the Sertoli cells. Dev Biol. 2008;315(1):173–188. doi: 10.1016/j.ydbio.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 38.Steiner M, Weipoltshammer K, Viehberger G, Meixner EM, Lunglmayr G, Schofer C. Immunohistochemical expression analysis of Cx43, Cx26, c-KIT and PlAP in contralateral testis biopsies of patients with non-seminomatous testicular germ cell tumor. Histochem Cell Biol. 2011;135(1):73–81. doi: 10.1007/s00418-010-0769-8. [DOI] [PubMed] [Google Scholar]
- 39.Juneja SC. mRNA expression pattern of multiple members of connexin gene family in normal and abnormal fetal gonads in mouse. Indian J Physiol Pharmacol. 2003;47(2):147–156. [PubMed] [Google Scholar]
- 40.Perez-Armendariz EM, Lamoyi E, Mason JI, Cisneros-Armas D, Luu-The V, Bravo Moreno JF. Developmental regulation of connexin 43 expression in fetal mouse testicular cells. Anat Rec. 2001;264(3):237–246. doi: 10.1002/ar.1164. [DOI] [PubMed] [Google Scholar]
- 41.Dufresne J, Finnson KW, Gregory M, Cyr DG. Expression of multiple connexins in the rat epididymis indicates a complex regulation of gap junctional communication. Am J Physiol Cell Physiol. 2003;284(1):C33–C43. doi: 10.1152/ajpcell.00111.2002. [DOI] [PubMed] [Google Scholar]
- 42.Cyr DG, Hermo L, Laird DW. Immunocytochemical localization and regulation of connexin43 in the adult rat epididymis. Endocrinology. 1996;137(4):1474–1484. doi: 10.1210/endo.137.4.8625926. [DOI] [PubMed] [Google Scholar]
- 43.Meda P, Pepper MS, Traub O, Willecke K, Gros D, Beyer E, Nicholson B, Paul D, Orci L. Differential expression of gap junction connexins in endocrine and exocrine glands. Endocrinology. 1993;133(5):2371–2378. doi: 10.1210/endo.133.5.8404689. [DOI] [PubMed] [Google Scholar]
- 44.Habermann H, Chang WY, Birch L, Mehta P, Prins GS. Developmental exposure to estrogens alters epithelial cell adhesion and gap junction proteins in the adult rat prostate. Endocrinology. 2001;142(1):359–369. doi: 10.1210/endo.142.1.7893. [DOI] [PubMed] [Google Scholar]
- 45.Habermann H, Ray V, Habermann W, Prins GS. Alterations in gap junction protein expression in human benign prostatic hyperplasia and prostate cancer. J Urol. 2002;167(2 Pt 1):655–660. doi: 10.1016/S0022-5347(01)69118-3. [DOI] [PubMed] [Google Scholar]
- 46.Mehta PP, Perez-Stable C, Nadji M, Mian M, Asotra K, Roos BA (1999) Suppression of human prostate cancer cell growth by forced expression of connexin genes. Dev Genet 24(1–2):91–110. doi:10.1002/(SICI)1520-6408(1999)24:1/2<91:AID-DVG10>3.0.CO;2-# [DOI] [PubMed]
- 47.Van der Aa F, Roskams T, Blyweert W, De Ridder D. Interstitial cells in the human prostate: a new therapeutic target? Prostate. 2003;56(4):250–255. doi: 10.1002/pros.10264. [DOI] [PubMed] [Google Scholar]
- 48.Moreno AP, Campos de Carvalho AC, Christ G, Melman A, Spray DC. Gap junctions between human corpus cavernosum smooth muscle cells: gating properties and unitary conductance. Am J Physiol. 1993;264(1 Pt 1):C80–C92. doi: 10.1152/ajpcell.1993.264.1.C80. [DOI] [PubMed] [Google Scholar]
- 49.Campos de Carvalho AC, Roy C, Moreno AP, Melman A, Hertzberg EL, Christ GJ, Spray DC. Gap junctions formed of connexin 43 are found between smooth muscle cells of human corpus cavernosum. J Urol. 1993;149(6):1568–1575. doi: 10.1016/s0022-5347(17)36455-8. [DOI] [PubMed] [Google Scholar]
- 50.Richardson BE, Lehmann R. Mechanisms guiding primordial germ cell migration: strategies from different organisms. Nat Rev Mol Cell Biol. 2010;11(1):37–49. doi: 10.1038/nrm2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu X, Li WE, Huang GY, Meyer R, Chen T, Luo Y, Thomas MP, Radice GL, Lo CW. Modulation of mouse neural crest cell motility by N-cadherin and connexin 43 gap junctions. J Cell Biol. 2001;154(1):217–230. doi: 10.1083/jcb.200105047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Molyneaux KA, Wang Y, Schaible K, Wylie C. Transcriptional profiling identifies genes differentially expressed during and after migration in murine primordial germ cells. Gene Expr Patterns. 2004;4(2):167–181. doi: 10.1016/j.modgep.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 53.Juneja SC, Barr KJ, Enders GC, Kidder GM. Defects in the germ line and gonads of mice lacking connexin43. Biol Reprod. 1999;60(5):1263–1270. doi: 10.1095/biolreprod60.5.1263. [DOI] [PubMed] [Google Scholar]
- 54.Tazuke SI, Schulz C, Gilboa L, Fogarty M, Mahowald AP, Guichet A, Ephrussi A, Wood CG, Lehmann R, Fuller MT. A germline-specific gap junction protein required for survival of differentiating early germ cells. Development. 2002;129(10):2529–2539. doi: 10.1242/dev.129.10.2529. [DOI] [PubMed] [Google Scholar]
- 55.Gilleron J, Nebout M, Scarabelli L, Senegas-Balas F, Palmero S, Segretain D, Pointis G. A potential novel mechanism involving connexin 43 gap junction for control of sertoli cell proliferation by thyroid hormones. J Cell Physiol. 2006;209(1):153–161. doi: 10.1002/jcp.20716. [DOI] [PubMed] [Google Scholar]
- 56.Carette D, Weider K, Gilleron J, Giese S, Dompierre J, Bergmann M, Brehm R, Denizot JP, Segretain D, Pointis G. Major involvement of connexin 43 in seminiferous epithelial junction dynamics and male fertility. Dev Biol. 2010;346(1):54–67. doi: 10.1016/j.ydbio.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 57.Gerber J, Weider K, Hambruch N, Brehm R. Loss of connexin 43 (Cx43) in Sertoli cells leads to spatio-temporal alterations in occludin expression. Histol Histopathol. 2014;29(7):935–948. doi: 10.14670/HH-29.935. [DOI] [PubMed] [Google Scholar]
- 58.Li MW, Mruk DD, Lee WM, Cheng CY. Connexin 43 is critical to maintain the homeostasis of the blood-testis barrier via its effects on tight junction reassembly. Proc Natl Acad Sci USA. 2010;107(42):17998–18003. doi: 10.1073/pnas.1007047107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pointis G, Gilleron J, Carette D, Segretain D. Physiological and physiopathological aspects of connexins and communicating gap junctions in spermatogenesis. Philos Trans R Soc Lond B Biol Sci. 2010;365(1546):1607–1620. doi: 10.1098/rstb.2009.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goldenberg RC, Fortes FS, Cristancho JM, Morales MM, Franci CR, Varanda WA, Campos de Carvalho AC. Modulation of gap junction mediated intercellular communication in TM3 Leydig cells. J Endocrinol. 2003;177(2):327–335. doi: 10.1677/joe.0.1770327. [DOI] [PubMed] [Google Scholar]
- 61.Perez-Armendariz EM, Luna J, Miranda C, Talavera D, Romano MC. Luteinizing and human chorionic gonadotropin hormones increase intercellular communication and gap junctions in cultured mouse leydig cells. Endocrine. 1996;4(2):141–157. doi: 10.1007/BF02782759. [DOI] [PubMed] [Google Scholar]
- 62.Li D, Sekhon P, Barr KJ, Marquez-Rosado L, Lampe PD, Kidder GM. Connexins and steroidogenesis in mouse Leydig cells. Can J Physiol Pharmacol. 2013;91(2):157–164. doi: 10.1139/cjpp-2012-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kahiri CN, Khalil MW, Tekpetey F, Kidder GM. Leydig cell function in mice lacking connexin43. Reproduction. 2006;132(4):607–616. doi: 10.1530/rep.1.01234. [DOI] [PubMed] [Google Scholar]
- 64.Carette D, Gilleron J, Chevallier D, Segretain D, Pointis G. Connexin a check-point component of cell apoptosis in normal and physiopathological conditions. Biochimie. 2014;101:1–9. doi: 10.1016/j.biochi.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 65.Chojnacka K, Brehm R, Weider K, Hejmej A, Lydka M, Kopera-Sobota I, Bilinska B. Expression of the androgen receptor in the testis of mice with a Sertoli cell specific knock-out of the connexin 43 gene (SCCx43KO(−/−)) Reprod Biol. 2012;12(4):341–346. doi: 10.1016/j.repbio.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 66.Decrouy X, Gasc JM, Pointis G, Segretain D. Functional characterization of Cx43 based gap junctions during spermatogenesis. J Cell Physiol. 2004;200(1):146–154. doi: 10.1002/jcp.10473. [DOI] [PubMed] [Google Scholar]
- 67.Pelletier RM, Akpovi CD, Chen L, Day R, Vitale ML. CX43 expression, phosphorylation, and distribution in the normal and autoimmune orchitic testis with a look at gap junctions joining germ cell to germ cell. Am J Physiol Regul Integr Comp Physiol. 2011;300(1):R121–R139. doi: 10.1152/ajpregu.00500.2010. [DOI] [PubMed] [Google Scholar]
- 68.Brehm R, Zeiler M, Ruttinger C, Herde K, Kibschull M, Winterhager E, Willecke K, Guillou F, Lecureuil C, Steger K, Konrad L, Biermann K, Failing K, Bergmann M. A sertoli cell-specific knockout of connexin 43 prevents initiation of spermatogenesis. Am J Pathol. 2007;171(1):19–31. doi: 10.2353/ajpath.2007.061171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sridharan S, Simon L, Meling DD, Cyr DG, Gutstein DE, Fishman GI, Guillou F, Cooke PS. Proliferation of adult sertoli cells following conditional knockout of the Gap junctional protein GJA1 (connexin 43) in mice. Biol Reprod. 2007;76(5):804–812. doi: 10.1095/biolreprod.106.059212. [DOI] [PubMed] [Google Scholar]
- 70.Weider K, Bergmann M, Giese S, Guillou F, Failing K, Brehm R. Altered differentiation and clustering of Sertoli cells in transgenic mice showing a Sertoli cell specific knockout of the connexin 43 gene. Differentiation. 2011;82(1):38–49. doi: 10.1016/j.diff.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 71.Lee NP, Leung KW, Wo JY, Tam PC, Yeung WS, Luk JM. Blockage of testicular connexins induced apoptosis in rat seminiferous epithelium. Apoptosis. 2006;11(7):1215–1229. doi: 10.1007/s10495-006-6981-2. [DOI] [PubMed] [Google Scholar]
- 72.Gunther S, Fietz D, Weider K, Bergmann M, Brehm R. Effects of a murine germ cell-specific knockout of Connexin 43 on Connexin expression in testis and fertility. Transgenic Res. 2013;22(3):631–641. doi: 10.1007/s11248-012-9668-1. [DOI] [PubMed] [Google Scholar]
- 73.Li MW, Mruk DD, Lee WM, Cheng CY. Cytokines and junction restructuring events during spermatogenesis in the testis: an emerging concept of regulation. Cytokine Growth Factor Rev. 2009;20(4):329–338. doi: 10.1016/j.cytogfr.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lui WY, Mruk D, Lee WM, Cheng CY. Sertoli cell tight junction dynamics: their regulation during spermatogenesis. Biol Reprod. 2003;68(4):1087–1097. doi: 10.1095/biolreprod.102.010371. [DOI] [PubMed] [Google Scholar]
- 75.Mok KW, Mruk DD, Lee WM, Cheng CY. Rictor/mTORC2 regulates blood-testis barrier dynamics via its effects on gap junction communications and actin filament network. Faseb J. 2013;27(3):1137–1152. doi: 10.1096/fj.12-212977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Orgebin-Crist MC. Maturation of spermatozoa in the rabbit epididymis: delayed fertilization in does inseminated with epididymal spermatozoa. J Reprod Fertil. 1968;16(1):29–33. doi: 10.1530/jrf.0.0160029. [DOI] [PubMed] [Google Scholar]
- 77.Segretain D, Falk MM. Regulation of connexin biosynthesis, assembly, gap junction formation, and removal. Biochim Biophys Acta. 2004;1662(1–2):3–21. doi: 10.1016/j.bbamem.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 78.Mandal A, Shahidullah M, Delamere NA. Calcium entry via connexin hemichannels in lens epithelium. Exp Eye Res. 2015;132C:52–58. doi: 10.1016/j.exer.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Abudara V, Roux L, Dallerac G, Matias I, Dulong J, Mothet JP, Rouach N, Giaume C. Activated microglia impairs neuroglial interaction by opening Cx43 hemichannels in hippocampal astrocytes. Glia. 2015 doi: 10.1002/glia.22785. [DOI] [PubMed] [Google Scholar]
- 80.Montero TD, Orellana JA. Hemichannels: new pathways for gliotransmitter release. Neuroscience. 2015;286C:45–59. doi: 10.1016/j.neuroscience.2014.11.048. [DOI] [PubMed] [Google Scholar]
- 81.Vinken M. Connexin hemichannels: novel mediators of toxicity. Arch Toxicol. 2015;89(1):143–145. doi: 10.1007/s00204-014-1422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang J, Zhang HY, Zhang M, Qiu ZY, Wu YP, Callaway DA, Jiang JX, Lu L, Jing L, Yang T, Wang MQ. Connexin 43 hemichannels mediate small molecule exchange between chondrocytes and matrix in biomechanically-stimulated temporomandibular joint cartilage. Osteoarthritis Cartilage. 2014;22(6):822–830. doi: 10.1016/j.joca.2014.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leung PS, Chan HC, Chung YW, Wong TP, Wong PY. The role of local angiotensins and prostaglandins in the control of anion secretion by the rat epididymis. J Reprod Fertil Suppl. 1998;53:15–22. [PubMed] [Google Scholar]
- 84.Leung GP, Cheung KH, Leung CT, Tsang MW, Wong PY. Regulation of epididymal principal cell functions by basal cells: role of transient receptor potential (Trp) proteins and cyclooxygenase-1 (COX-1) Mol Cell Endocrinol. 2004;216(1–2):5–13. doi: 10.1016/j.mce.2003.10.077. [DOI] [PubMed] [Google Scholar]
- 85.Zhou WL, Zuo WL, Ruan YC, Wang Z, Du JY, Xiong Y, Chan HC. The role of extracellular ATP in the male reproductive tract. Sheng Li Xue Bao. 2007;59(4):487–494. [PubMed] [Google Scholar]
- 86.Christ GJ, Moreno AP, Parker ME, Gondre CM, Valcic M, Melman A, Spray DC. Intercellular communication through gap junctions: a potential role in pharmacomechanical coupling and syncytial tissue contraction in vascular smooth muscle isolated from the human corpus cavernosum. Life Sci. 1991;49(24):PL195–PL200. doi: 10.1016/0024-3205(91)90489-x. [DOI] [PubMed] [Google Scholar]
- 87.Pointis G. Connexin43: emerging role in erectile function. Int J Biochem Cell Biol. 2006;38(10):1642–1646. doi: 10.1016/j.biocel.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 88.Traish AM, Stottrup C, van Renterghem K, Achten R, Roy S. Density and distribution of connexin 43 in corpus cavernosum tissue from diabetic and hypogonadal patients with erectile dysfunction. Horm Mol Biol Clin Investig. 2013;13(1):7–12. doi: 10.1515/hmbci-2013-0001. [DOI] [PubMed] [Google Scholar]
- 89.Karicheti V, Christ GJ. Physiological roles for K+ channels and gap junctions in urogenital smooth muscle: implications for improved understanding of urogenital function, disease and therapy. Curr Drug Targets. 2001;2(1):1–20. doi: 10.2174/1389450013348894. [DOI] [PubMed] [Google Scholar]
- 90.Liu XB, Wu TP, Zhan YY, Wang ZY. Cigarette smoke extract reduces NOS activity and CX43 expression in the corporal cavernosum. Zhonghua Nan Ke Xue. 2011;17(4):351–355. [PubMed] [Google Scholar]
- 91.Gittens JE, Kidder GM. Differential contributions of connexin 37 and connexin43 to oogenesis revealed in chimeric reaggregated mouse ovaries. J Cell Sci. 2005;118(Pt 21):5071–5078. doi: 10.1242/jcs.02624. [DOI] [PubMed] [Google Scholar]
- 92.Simon AM, Goodenough DA, Li E, Paul DL. Female infertility in mice lacking connexin 37. Nature. 1997;385(6616):525–529. doi: 10.1038/385525a0. [DOI] [PubMed] [Google Scholar]
- 93.Cepni I, Kahraman N, Ocal P, Idil M, Uludag S. Expression and comparison of gap junction protein connexin 37 in granulosa cells aspirates from follicles of poor responder and nonpoor responder patients. Fertil Steril. 2008;89(2):417–420. doi: 10.1016/j.fertnstert.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 94.Ferenczy A, Bergeron C. Histology of the human endometrium: from birth to senescence. Ann N Y Acad Sci. 1991;622:6–27. doi: 10.1111/j.1749-6632.1991.tb37847.x. [DOI] [PubMed] [Google Scholar]
- 95.Winterhager E, Grummer R, Jahn E, Willecke K, Traub O. Spatial and temporal expression of connexin 26 and connexin 43 in rat endometrium during trophoblast invasion. Dev Biol. 1993;157(2):399–409. doi: 10.1006/dbio.1993.1144. [DOI] [PubMed] [Google Scholar]
- 96.Pauken CM, Lo CW. Nonoverlapping expression of Cx43 and Cx26 in the mouse placenta and decidua: a pattern of gap junction gene expression differing from that in the rat. Mol Reprod Dev. 1995;41(2):195–203. doi: 10.1002/mrd.1080410210. [DOI] [PubMed] [Google Scholar]
- 97.Gabriel S, Winterhager E, Pfarrer C, Traub O, Leiser R. Modulation of connexin expression in sheep endometrium in response to pregnancy. Placenta. 2004;25(4):287–296. doi: 10.1016/j.placenta.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 98.Lenhart JA, Ryan PL, Ohleth KM, Bagnell CA. Expression of connexin-26, -32, and -43 gap junction proteins in the porcine cervix and uterus during pregnancy and relaxin-induced growth. Biol Reprod. 1999;61(6):1452–1459. doi: 10.1095/biolreprod61.6.1452. [DOI] [PubMed] [Google Scholar]
- 99.Winterhager E, Fazleabas A, Hillier S. Endometriosis: science and sense. Mol Hum Reprod. 2009;15(10):575. doi: 10.1093/molehr/gap074. [DOI] [PubMed] [Google Scholar]
- 100.Winterhager E, Brummer F, Dermietzel R, Hulser DF, Denker HW. Gap junction formation in rabbit uterine epithelium in response to embryo recognition. Dev Biol. 1988;126(1):203–211. doi: 10.1016/0012-1606(88)90254-0. [DOI] [PubMed] [Google Scholar]
- 101.Jahn E, Classen-Linke I, Kusche M, Beier HM, Traub O, Grummer R, Winterhager E. Expression of gap junction connexins in the human endometrium throughout the menstrual cycle. Hum Reprod. 1995;10(10):2666–2670. doi: 10.1093/oxfordjournals.humrep.a135764. [DOI] [PubMed] [Google Scholar]
- 102.Davies TC, Barr KJ, Jones DH, Zhu D, Kidder GM. Multiple members of the connexin gene family participate in preimplantation development of the mouse. Dev Genet. 1996;18(3):234–243. doi: 10.1002/(SICI)1520-6408(1996)18:3<234::AID-DVG4>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 103.Houghton FD, Barr KJ, Walter G, Gabriel HD, Grummer R, Traub O, Leese HJ, Winterhager E, Kidder GM. Functional significance of gap junctional coupling in preimplantation development. Biol Reprod. 2002;66(5):1403–1412. doi: 10.1095/biolreprod66.5.1403. [DOI] [PubMed] [Google Scholar]
- 104.Flechon JE, Degrouard J, Flechon B, Lefevre F, Traub O. Gap junction formation and connexin distribution in pig trophoblast before implantation. Placenta. 2004;25(1):85–94. doi: 10.1016/j.placenta.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 105.Rizos D, Gutierrez-Adan A, Moreira P, O’Meara C, Fair T, Evans AC, Boland MP, Lonergan P. Species-related differences in blastocyst quality are associated with differences in relative mRNA transcription. Mol Reprod Dev. 2004;69(4):381–386. doi: 10.1002/mrd.20133. [DOI] [PubMed] [Google Scholar]
- 106.Bloor DJ, Wilson Y, Kibschull M, Traub O, Leese HJ, Winterhager E, Kimber SJ. Expression of connexins in human preimplantation embryos in vitro. Reprod Biology Endocrinol RB&E. 2004;2:25. doi: 10.1186/1477-7827-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hardy K, Warner A, Winston RM, Becker DL. Expression of intercellular junctions during preimplantation development of the human embryo. Mol Hum Reprod. 1996;2(8):621–632. doi: 10.1093/molehr/2.8.621. [DOI] [PubMed] [Google Scholar]
- 108.Plum A, Winterhager E, Pesch J, Lautermann J, Hallas G, Rosentreter B, Traub O, Herberhold C, Willecke K. Connexin31-deficiency in mice causes transient placental dysmorphogenesis but does not impair hearing and skin differentiation. Developmental biology. 2001;231(2):334–347. doi: 10.1006/dbio.2000.0148. [DOI] [PubMed] [Google Scholar]
- 109.Winterhager E, Von Ostau C, Gerke M, Gruemmer R, Traub O, Kaufmann P. Connexin expression patterns in human trophoblast cells during placental development. Placenta. 1999;20(8):627–638. doi: 10.1053/plac.1999.0434. [DOI] [PubMed] [Google Scholar]
- 110.Cronier L, Defamie N, Dupays L, Theveniau-Ruissy M, Goffin F, Pointis G, Malassine A. Connexin expression and gap junctional intercellular communication in human first trimester trophoblast. Mol Hum Reprod. 2002;8(11):1005–1013. doi: 10.1093/molehr/8.11.1005. [DOI] [PubMed] [Google Scholar]
- 111.Lyall F, Lye S, Teoh T, Cousins F, Milligan G, Robson S. Expression of Gsalpha, connexin-43, connexin-26, and EP1, 3, and 4 receptors in myometrium of prelabor singleton versus multiple gestations and the effects of mechanical stretch and steroids on Gsalpha. J Soc Gynecol Investig. 2002;9(5):299–307. doi: 10.1016/s1071-5576(02)00175-2. [DOI] [PubMed] [Google Scholar]
- 112.Orsino A, Taylor CV, Lye SJ. Connexin-26 and connexin-43 are differentially expressed and regulated in the rat myometrium throughout late pregnancy and with the onset of labor. Endocrinology. 1996;137(5):1545–1553. doi: 10.1210/endo.137.5.8612484. [DOI] [PubMed] [Google Scholar]
- 113.Kilarski WM, Dupont E, Coppen S, Yeh HI, Vozzi C, Gourdie RG, Rezapour M, Ulmsten U, Roomans GM, Severs NJ. Identification of two further gap-junctional proteins, connexin40 and connexin45, in human myometrial smooth muscle cells at term. Eur J Cell Biol. 1998;75(1):1–8. doi: 10.1016/S0171-9335(98)80040-X. [DOI] [PubMed] [Google Scholar]
- 114.Gershon E, Plaks V, Dekel N. Gap junctions in the ovary: expression, localization and function. Mol Cell Endocrinol. 2008;282(1–2):18–25. doi: 10.1016/j.mce.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 115.Goodenough DA, Simon AM, Paul DL (1999) Gap junctional intercellular communication in the mouse ovarian follicle. Novartis Foundation Symposium 219:226–235 (discussion 235–240) [DOI] [PubMed]
- 116.Granot I, Dekel N. The ovarian gap junction protein connexin43: regulation by gonadotropins. Trends Endocrinol Metab TEM. 2002;13(7):310–313. doi: 10.1016/s1043-2760(02)00623-9. [DOI] [PubMed] [Google Scholar]
- 117.Kidder GM, Mhawi AA. Gap junctions and ovarian folliculogenesis. Reproduction. 2002;123(5):613–620. doi: 10.1530/rep.0.1230613. [DOI] [PubMed] [Google Scholar]
- 118.Dong J, Albertini DF, Nishimori K, Kumar TR, Lu N, Matzuk MM. Growth differentiation factor-9 is required during early ovarian folliculogenesis. Nature. 1996;383(6600):531–535. doi: 10.1038/383531a0. [DOI] [PubMed] [Google Scholar]
- 119.Mitchell PA, Burghardt RC. The ontogeny of nexuses (gap junctions) in the ovary of the fetal mouse. Anat Rec. 1986;214(3):283–288. doi: 10.1002/ar.1092140307. [DOI] [PubMed] [Google Scholar]
- 120.Eppig JJ. Maintenance of meiotic arrest and the induction of oocyte maturation in mouse oocyte-granulosa cell complexes developed in vitro from preantral follicles. Biol Reprod. 1991;45(6):824–830. doi: 10.1095/biolreprod45.6.824. [DOI] [PubMed] [Google Scholar]
- 121.Eppig JJ, O’Brien MJ. Development in vitro of mouse oocytes from primordial follicles. Biol Reprod. 1996;54(1):197–207. doi: 10.1095/biolreprod54.1.197. [DOI] [PubMed] [Google Scholar]
- 122.Veitch GI, Gittens JE, Shao Q, Laird DW, Kidder GM. Selective assembly of connexin37 into heterocellular gap junctions at the oocyte/granulosa cell interface. J Cell Sci. 2004;117(Pt 13):2699–2707. doi: 10.1242/jcs.01124. [DOI] [PubMed] [Google Scholar]
- 123.Carabatsos MJ, Sellitto C, Goodenough DA, Albertini DF. Oocyte-granulosa cell heterologous gap junctions are required for the coordination of nuclear and cytoplasmic meiotic competence. Dev Biol. 2000;226(2):167–179. doi: 10.1006/dbio.2000.9863. [DOI] [PubMed] [Google Scholar]
- 124.Reaume AG, de Sousa PA, Kulkarni S, Langille BL, Zhu D, Davies TC, Juneja SC, Kidder GM, Rossant J. Cardiac malformation in neonatal mice lacking connexin43. Science. 1995;267(5205):1831–1834. doi: 10.1126/science.7892609. [DOI] [PubMed] [Google Scholar]
- 125.Ackert CL, Gittens JE, O’Brien MJ, Eppig JJ, Kidder GM. Intercellular communication via connexin43 gap junctions is required for ovarian folliculogenesis in the mouse. Dev Biol. 2001;233(2):258–270. doi: 10.1006/dbio.2001.0216. [DOI] [PubMed] [Google Scholar]
- 126.Gershon E, Plaks V, Aharon I, Galiani D, Reizel Y, Sela-Abramovich S, Granot I, Winterhager E, Dekel N. Oocyte-directed depletion of connexin43 using the Cre-LoxP system leads to subfertility in female mice. Dev Biol. 2008;313(1):1–12. doi: 10.1016/j.ydbio.2007.08.041. [DOI] [PubMed] [Google Scholar]
- 127.Richard S, Baltz JM. Prophase I arrest of mouse oocytes mediated by natriuretic peptide precursor C requires GJA1 (connexin-43) and GJA4 (connexin-37) gap junctions in the antral follicle and cumulus-oocyte complex. Biol Reprod. 2014;90(6):137. doi: 10.1095/biolreprod.114.118505. [DOI] [PubMed] [Google Scholar]
- 128.Leybaert L, Braet K, Vandamme W, Cabooter L, Martin PE, Evans WH. Connexin channels, connexin mimetic peptides and ATP release. Cell Commun Adhesion. 2003;10(4–6):251–257. doi: 10.1080/cac.10.4-6.251.257. [DOI] [PubMed] [Google Scholar]
- 129.Tai CJ, Kang SK, Cheng KW, Choi KC, Nathwani PS, Leung PC. Expression and regulation of P2U-purinergic receptor in human granulosa-luteal cells. J Clin Endocrinol Metab. 2000;85(4):1591–1597. doi: 10.1210/jcem.85.4.6558. [DOI] [PubMed] [Google Scholar]
- 130.Webb RJ, Bains H, Cruttwell C, Carroll J. Gap-junctional communication in mouse cumulus-oocyte complexes: implications for the mechanism of meiotic maturation. Reproduction. 2002;123(1):41–52. doi: 10.1530/rep.0.1230041. [DOI] [PubMed] [Google Scholar]
- 131.Tong D, Li TY, Naus KE, Bai D, Kidder GM. In vivo analysis of undocked connexin43 gap junction hemichannels in ovarian granulosa cells. J Cell Sci. 2007;120(Pt 22):4016–4024. doi: 10.1242/jcs.011775. [DOI] [PubMed] [Google Scholar]
- 132.Furger C, Cronier L, Poirot C, Pouchelet M. Human granulosa cells in culture exhibit functional cyclic AMP-regulated gap junctions. Mol Hum Reprod. 1996;2(8):541–548. doi: 10.1093/molehr/2.8.541. [DOI] [PubMed] [Google Scholar]
- 133.Ratchford AM, Esguerra CR, Moley KH. Decreased oocyte-granulosa cell gap junction communication and connexin expression in a type 1 diabetic mouse model. Mol Endocrinol. 2008;22(12):2643–2654. doi: 10.1210/me.2007-0495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wang HX, Tong D, El-Gehani F, Tekpetey FR, Kidder GM. Connexin expression and gap junctional coupling in human cumulus cells: contribution to embryo quality. J Cell Mol Med. 2009;13(5):972–984. doi: 10.1111/j.1582-4934.2008.00373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nelles E, Butzler C, Jung D, Temme A, Gabriel HD, Dahl U, Traub O, Stumpel F, Jungermann K, Zielasek J, Toyka KV, Dermietzel R, Willecke K. Defective propagation of signals generated by sympathetic nerve stimulation in the liver of connexin32-deficient mice. Proc Natl Acad Sci USA. 1996;93(18):9565–9570. doi: 10.1073/pnas.93.18.9565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gabriel HD, Jung D, Butzler C, Temme A, Traub O, Winterhager E, Willecke K. Transplacental uptake of glucose is decreased in embryonic lethal connexin26-deficient mice. J Cell Biol. 1998;140(6):1453–1461. doi: 10.1083/jcb.140.6.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kruger O, Plum A, Kim JS, Winterhager E, Maxeiner S, Hallas G, Kirchhoff S, Traub O, Lamers WH, Willecke K. Defective vascular development in connexin 45-deficient mice. Development. 2000;127(19):4179–4193. doi: 10.1242/dev.127.19.4179. [DOI] [PubMed] [Google Scholar]
- 138.Diao H, Xiao S, Howerth EW, Zhao F, Li R, Ard MB, Ye X. Broad gap junction blocker carbenoxolone disrupts uterine preparation for embryo implantation in mice. Biol Reprod. 2013;89(2):31. doi: 10.1095/biolreprod.113.110106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Grummer R, Hewitt SW, Traub O, Korach KS, Winterhager E. Different regulatory pathways of endometrial connexin expression: preimplantation hormonal-mediated pathway versus embryo implantation-initiated pathway. Biol Reprod. 2004;71(1):273–281. doi: 10.1095/biolreprod.103.024067. [DOI] [PubMed] [Google Scholar]
- 140.Grummer R, Traub O, Winterhager E. Gap junction connexin genes cx26 and cx43 are differentially regulated by ovarian steroid hormones in rat endometrium. Endocrinology. 1999;140(6):2509–2516. doi: 10.1210/endo.140.6.6640. [DOI] [PubMed] [Google Scholar]
- 141.Laws MJ, Taylor RN, Sidell N, DeMayo FJ, Lydon JP, Gutstein DE, Bagchi MK, Bagchi IC. Gap junction communication between uterine stromal cells plays a critical role in pregnancy-associated neovascularization and embryo survival. Development. 2008;135(15):2659–2668. doi: 10.1242/dev.019810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Flenniken AM, Osborne LR, Anderson N, Ciliberti N, Fleming C, Gittens JE, Gong XQ, Kelsey LB, Lounsbury C, Moreno L, Nieman BJ, Peterson K, Qu D, Roscoe W, Shao Q, Tong D, Veitch GI, Voronina I, Vukobradovic I, Wood GA, Zhu Y, Zirngibl RA, Aubin JE, Bai D, Bruneau BG, Grynpas M, Henderson JE, Henkelman RM, McKerlie C, Sled JG, Stanford WL, Laird DW, Kidder GM, Adamson SL, Rossant J. A Gja1 missense mutation in a mouse model of oculodentodigital dysplasia. Development. 2005;132(19):4375–4386. doi: 10.1242/dev.02011. [DOI] [PubMed] [Google Scholar]
- 143.Winterhager E, Gellhaus A, Blois SM, Hill LA, Barr KJ, Kidder GM. Decidual angiogenesis and placental orientation are altered in mice heterozygous for a dominant loss-of-function Gja1 (connexin43) mutation. Biol Reprod. 2013;89(5):111. doi: 10.1095/biolreprod.113.111690. [DOI] [PubMed] [Google Scholar]
- 144.Yu J, Wu J, Bagchi IC, Bagchi MK, Sidell N, Taylor RN. Disruption of gap junctions reduces biomarkers of decidualization and angiogenesis and increases inflammatory mediators in human endometrial stromal cell cultures. Mol Cell Endocrinol. 2011;344(1–2):25–34. doi: 10.1016/j.mce.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nair RR, Jain M, Singh K. Reduced expression of gap junction gene connexin 43 in recurrent early pregnancy loss patients. Placenta. 2011;32(8):619–621. doi: 10.1016/j.placenta.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 146.Bauersachs S, Ulbrich SE, Zakhartchenko V, Minten M, Reichenbach M, Reichenbach HD, Blum H, Spencer TE, Wolf E. The endometrium responds differently to cloned versus fertilized embryos. Proc Natl Acad Sci USA. 2009;106(14):5681–5686. doi: 10.1073/pnas.0811841106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Houghton FD. Role of gap junctions during early embryo development. Reproduction. 2005;129(2):129–135. doi: 10.1530/rep.1.00277. [DOI] [PubMed] [Google Scholar]
- 148.Vance MM, Wiley LM. Gap junction intercellular communication mediates the competitive cell proliferation disadvantage of irradiated mouse preimplantation embryos in aggregation chimeras. Radiat Res. 1999;152(5):544–551. [PubMed] [Google Scholar]
- 149.Kibschull M, Magin TM, Traub O, Winterhager E. Cx31 and Cx43 double-deficient mice reveal independent functions in murine placental and skin development. Dev Dyn Off Publ Am Assoc Anat. 2005;233(3):853–863. doi: 10.1002/dvdy.20424. [DOI] [PubMed] [Google Scholar]
- 150.Kidder GM, Winterhager E. Intercellular communication in preimplantation development: the role of gap junctions. Front Biosci J Virtual Library. 2001;6:D731–D736. doi: 10.2741/kidder. [DOI] [PubMed] [Google Scholar]
- 151.Kalimi GH, Lo CW. Gap junctional communication in the extraembryonic tissues of the gastrulating mouse embryo. J Cell Biology. 1989;109(6 Pt 1):3015–3026. doi: 10.1083/jcb.109.6.3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Reuss B, Hellmann P, Traub O, Butterweck A, Winterhager E. Expression of connexin31 and connexin43 genes in early rat embryos. Dev Genet. 1997;21(1):82–90. doi: 10.1002/(SICI)1520-6408(1997)21:1<82::AID-DVG10>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 153.Winterhager E, Pielensticker N, Freyer J, Ghanem A, Schrickel JW, Kim JS, Behr R, Grummer R, Maass K, Urschel S, Lewalter T, Tiemann K, Simoni M, Willecke K. Replacement of connexin43 by connexin26 in transgenic mice leads to dysfunctional reproductive organs and slowed ventricular conduction in the heart. BMC Dev Biol. 2007;7:26. doi: 10.1186/1471-213X-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zheng-Fischhofer Q, Ghanem A, Kim JS, Kibschull M, Schwarz G, Schwab JO, Nagy J, Winterhager E, Tiemann K, Willecke K. Connexin31 cannot functionally replace connexin43 during cardiac morphogenesis in mice. J Cell Sci. 2006;119(Pt 4):693–701. doi: 10.1242/jcs.02800. [DOI] [PubMed] [Google Scholar]
- 155.Lopez D, Rodriguez-Sinovas A, Agullo E, Garcia A, Sanchez JA, Garcia-Dorado D. Replacement of connexin 43 by connexin 32 in a knock-in mice model attenuates aortic endothelium-derived hyperpolarizing factor-mediated relaxation. Exp Physiol. 2009;94(10):1088–1097. doi: 10.1113/expphysiol.2009.048413. [DOI] [PubMed] [Google Scholar]
- 156.Feuer S, Rinaudo P. Preimplantation stress and development. Birth Defects Res Part C Embryo Today Rev. 2012;96(4):299–314. doi: 10.1002/bdrc.21022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gutierrez-Adan A, Rizos D, Fair T, Moreira PN, Pintado B, de la Fuente J, Boland MP, Lonergan P. Effect of speed of development on mRNA expression pattern in early bovine embryos cultured in vivo or in vitro. Mol Reprod Dev. 2004;68(4):441–448. doi: 10.1002/mrd.20113. [DOI] [PubMed] [Google Scholar]
- 158.Rizos D, Gutierrez-Adan A, Perez-Garnelo S, De La Fuente J, Boland MP, Lonergan P. Bovine embryo culture in the presence or absence of serum: implications for blastocyst development, cryotolerance, and messenger RNA expression. Biol Reprod. 2003;68(1):236–243. doi: 10.1095/biolreprod.102.007799. [DOI] [PubMed] [Google Scholar]
- 159.Boni R, Tosti E, Roviello S, Dale B. Intercellular communication in in vivo- and in vitro-produced bovine embryos. Biol Reprod. 1999;61(4):1050–1055. doi: 10.1095/biolreprod61.4.1050. [DOI] [PubMed] [Google Scholar]
- 160.Bao ZJ, Zhao S, Haq IU, Zeng SM. Recombinant bovine interferon-tau enhances in vitro development of bovine embryos by upregulating expression of connexin 43 and E-cadherin. J Dairy Sci. 2014;97(11):6917–6925. doi: 10.3168/jds.2014-8106. [DOI] [PubMed] [Google Scholar]
- 161.Enders AC, Carter AM. Review: the evolving placenta: different developmental paths to a hemochorial relationship. Placenta. 2012;33(Suppl):S92–S98. doi: 10.1016/j.placenta.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 162.Rossant J, Cross JC. Placental development: lessons from mouse mutants. Nat Rev Genet. 2001;2(7):538–548. doi: 10.1038/35080570. [DOI] [PubMed] [Google Scholar]
- 163.Dahl E, Winterhager E, Reuss B, Traub O, Butterweck A, Willecke K. Expression of the gap junction proteins connexin31 and connexin43 correlates with communication compartments in extraembryonic tissues and in the gastrulating mouse embryo, respectively. J Cell Sci. 1996;109(Pt 1):191–197. doi: 10.1242/jcs.109.1.191. [DOI] [PubMed] [Google Scholar]
- 164.Zheng-Fischhofer Q, Kibschull M, Schnichels M, Kretz M, Petrasch-Parwez E, Strotmann J, Reucher H, Lynn BD, Nagy JI, Lye SJ, Winterhager E, Willecke K. Characterization of connexin31.1-deficient mice reveals impaired placental development. Dev Biol. 2007;312(1):258–271. doi: 10.1016/j.ydbio.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 165.Kibschull M, Nassiry M, Dunk C, Gellhaus A, Quinn JA, Rossant J, Lye SJ, Winterhager E. Connexin31-deficient trophoblast stem cells: a model to analyze the role of gap junction communication in mouse placental development. Dev Biol. 2004;273(1):63–75. doi: 10.1016/j.ydbio.2004.04.037. [DOI] [PubMed] [Google Scholar]
- 166.Kibschull M, Colaco K, Matysiak-Zablocki E, Winterhager E, Lye SJ. Connexin31.1 (Gjb5) deficiency blocks trophoblast stem cell differentiation and delays placental development. Stem Cells Dev. 2014;23(21):2649–2660. doi: 10.1089/scd.2014.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Soares MJ. The prolactin and growth hormone families: pregnancy-specific hormones/cytokines at the maternal-fetal interface. Reprod Biol Endocrinol RB&E. 2004;2:51. doi: 10.1186/1477-7827-2-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Coan PM, Conroy N, Burton GJ, Ferguson-Smith AC. Origin and characteristics of glycogen cells in the developing murine placenta. Dev Dyn Off Publ Am Assoc Anat. 2006;235(12):3280–3294. doi: 10.1002/dvdy.20981. [DOI] [PubMed] [Google Scholar]
- 169.Kibschull M, Gellhaus A, Winterhager E. Analogous and unique functions of connexins in mouse and human placental development. Placenta. 2008;29(10):848–854. doi: 10.1016/j.placenta.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 170.Lefebvre L. The placental imprintome and imprinted gene function in the trophoblast glycogen cell lineage. Reprod Biomed Online. 2012;25(1):44–57. doi: 10.1016/j.rbmo.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.De Wolf F, De Wolf-Peeters C, Brosens I, Robertson WB. The human placental bed: electron microscopic study of trophoblastic invasion of spiral arteries. Am J Obstet Gynecol. 1980;137(1):58–70. doi: 10.1016/0002-9378(80)90387-7. [DOI] [PubMed] [Google Scholar]
- 172.Cronier L, Frendo JL, Defamie N, Pidoux G, Bertin G, Guibourdenche J, Pointis G, Malassine A. Requirement of gap junctional intercellular communication for human villous trophoblast differentiation. Biol Reprod. 2003;69(5):1472–1480. doi: 10.1095/biolreprod.103.016360. [DOI] [PubMed] [Google Scholar]
- 173.Cronier L, Bastide B, Defamie N, Niger C, Pointis G, Gasc JM, Malassine A. Involvement of gap junctional communication and connexin expression in trophoblast differentiation of the human placenta. Histol Histopathol. 2001;16(1):285–295. doi: 10.14670/HH-16.285. [DOI] [PubMed] [Google Scholar]
- 174.Cronier L, Bastide B, Herve JC, Deleze J, Malassine A. Gap junctional communication during human trophoblast differentiation: influence of human chorionic gonadotropin. Endocrinology. 1994;135(1):402–408. doi: 10.1210/endo.135.1.8013377. [DOI] [PubMed] [Google Scholar]
- 175.Frendo JL, Cronier L, Bertin G, Guibourdenche J, Vidaud M, Evain-Brion D, Malassine A. Involvement of connexin 43 in human trophoblast cell fusion and differentiation. J Cell Sci. 2003;116(Pt 16):3413–3421. doi: 10.1242/jcs.00648. [DOI] [PubMed] [Google Scholar]
- 176.Dunk CE, Gellhaus A, Drewlo S, Baczyk D, Potgens AJ, Winterhager E, Kingdom JC, Lye SJ. The molecular role of connexin 43 in human trophoblast cell fusion. Biol Reprod. 2012;86(4):115. doi: 10.1095/biolreprod.111.096925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gellhaus A, Dong X, Propson S, Maass K, Klein-Hitpass L, Kibschull M, Traub O, Willecke K, Perbal B, Lye SJ, Winterhager E. Connexin43 interacts with NOV: a possible mechanism for negative regulation of cell growth in choriocarcinoma cells. J Biol Chem. 2004;279(35):36931–36942. doi: 10.1074/jbc.M404073200. [DOI] [PubMed] [Google Scholar]
- 178.Maass K, Ghanem A, Kim JS, Saathoff M, Urschel S, Kirfel G, Grummer R, Kretz M, Lewalter T, Tiemann K, Winterhager E, Herzog V, Willecke K. Defective epidermal barrier in neonatal mice lacking the C-terminal region of connexin43. Mol Biol Cell. 2004;15(10):4597–4608. doi: 10.1091/mbc.E04-04-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Pidoux G, Gerbaud P, Dompierre J, Lygren B, Solstad T, Evain-Brion D, Tasken K. A PKA-ezrin-Cx43 signaling complex controls gap junction communication and thereby trophoblast cell fusion. J Cell Sci. 2014;127(Pt 19):4172–4185. doi: 10.1242/jcs.149609. [DOI] [PubMed] [Google Scholar]
- 180.Winterhager E, Kaufmann P, Gruemmer R. Cell-cell-communication during placental development and possible implications for trophoblast proliferation and differentiation. Placenta. 2000;21(Suppl A):S61–S68. doi: 10.1053/plac.1999.0516. [DOI] [PubMed] [Google Scholar]
- 181.Hellmann P, Winterhager E, Spray DC. Properties of connexin40 gap junction channels endogenously expressed and exogenously overexpressed in human choriocarcinoma cell lines. Pflugers Arch. 1996;432(3):501–509. doi: 10.1007/s004240050162. [DOI] [PubMed] [Google Scholar]
- 182.Nishimura T, Dunk C, Lu Y, Feng X, Gellhaus A, Winterhager E, Rossant J, Lye SJ. Gap junctions are required for trophoblast proliferation in early human placental development. Placenta. 2004;25(7):595–607. doi: 10.1016/j.placenta.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 183.Tong D, Lu X, Wang HX, Plante I, Lui E, Laird DW, Bai D, Kidder GM. A dominant loss-of-function GJA1 (Cx43) mutant impairs parturition in the mouse. Biol Reprod. 2009;80(6):1099–1106. doi: 10.1095/biolreprod.108.071969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Mitchell JA, Lye SJ. Differential activation of the connexin 43 promoter by dimers of activator protein-1 transcription factors in myometrial cells. Endocrinology. 2005;146(4):2048–2054. doi: 10.1210/en.2004-1066. [DOI] [PubMed] [Google Scholar]
- 185.Dong X, Yu C, Shynlova O, Challis JR, Rennie PS, Lye SJ. p54nrb is a transcriptional corepressor of the progesterone receptor that modulates transcription of the labor-associated gene, connexin 43 (Gja1) Mol Endocrinol. 2009;23(8):1147–1160. doi: 10.1210/me.2008-0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Xie N, Liu L, Li Y, Yu C, Lam S, Shynlova O, Gleave M, Challis JR, Lye S, Dong X. Expression and function of myometrial PSF suggest a role in progesterone withdrawal and the initiation of labor. Mol Endocrinol. 2012;26(8):1370–1379. doi: 10.1210/me.2012-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chevallier D, Carette D, Segretain D, Gilleron J, Pointis G. Connexin 43 a check-point component of cell proliferation implicated in a wide range of human testis diseases. Cell Mol Life Sci. 2012 doi: 10.1007/s00018-012-1121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chevallier D, Carette D, Gilleron J, Segretain D, Pointis G. The emerging role of connexin 43 in testis pathogenesis. Curr Mol Med. 2013;13(8):1331–1344. doi: 10.2174/15665240113139990066. [DOI] [PubMed] [Google Scholar]
- 189.Winterhager E, Kidder GM. Gap junction connexins in female reproductive organs: implications for women’s reproductive health. Hum Reprod Update. 2015 doi: 10.1093/humupd/dmv007. [DOI] [PubMed] [Google Scholar]