Abstract
Objective:
This study aims to assess the efficacy of mindfulness-based cognitive therapy (MBCT) in alleviating depression in older adults.
Methods:
A comprehensive search was conducted in 4 electronic databases and 1 registered database from inception up to July 2021 to identify relevant trials. The meta-analysis employed Hedge’s g, along with its 95% CI, and associated z and P-values for the included studies, utilizing Comprehensive Meta-Analysis software.
Results:
Qualitative synthesis was performed on 5 eligible studies. Evaluation of methodological quality and bias risk across the papers involved scrutiny of key variables due to the heterogeneous research formats. Our findings indicated a significant moderating effect of MBCT against current depressive symptoms in older adults (g = 0.53, 95% Confidence Intervals (CI) = 0.31-0.75) and a similar effect size for anxiety (g = 0.43, 95% CI = 0.20-0.65). However, caution is warranted due to the limited number of studies and potential publication bias. Further extensive research with longer follow-up measures and larger sample sizes is essential.
Conclusion:
This study underscores the effectiveness of MBCT as a treatment for anxiety and despair in older individuals. Mindfulness-based cognitive therapy should be recommended for its positive impact on older adults with depression, and the involvement of authorized psychiatric nurses is crucial for conducting successful MBCT interventions. However, caution is warranted due to the limited number of studies and potential publication bias. Further extensive research with longer follow-up measures and larger sample sizes is essential.
Keywords: Mindfulness-based cognitive therapy (MBCT), late-life depression, older adults
Main Points
Mindfulness-based cognitive therapy (MBCT) treatment of depression in the elderly is beneficial for improving their emotional health.
Mindfulness-based cognitive therapy is effective in improving depressive symptoms in the elderly.
Mindfulness-based cognitive therapy is effective in improving anxiety symptoms in the elderly.
The effect of MBCT in treating depression has some implications for mental health nursing.
The use of MBCT in nurses can improve their abilities to take care of patients with emotional disorders.
Introduction
Depression represents the third leading cause of the global burden of disease, with a prevalence among older adults ranging from 4.6% to 9.3%.1 Over the years, late-life depression (LLD) has become increasingly prevalent, significantly impacting the physical and mental health of older individuals and imposing a substantial economic burden on medical service systems.2 Recognized as a critical global public health issue, LLD is often accompanied by comorbidities, such as hypertension, coronary heart disease, diabetes, and cognitive impairment. Importantly, LLD can hinder the prognosis of primary diseases due to reduced treatment adherence associated with depressive symptoms.3,4 Clinical responses to LLD treatment with medication are often unsatisfactory, with approximately 40%-60% of patients showing responsiveness to pharmacotherapy and a notable recurrence rate. Moreover, antidepressant use during the maintenance period has limitations, including adverse effects and recurring depressive symptoms in a significant percentage of patients over a 2-year period.5-7 Consequently, there is a growing demand for evidence-based, non-pharmacological treatments such as psychotherapy.8,9
Various psychological therapies, including cognitive therapy (CT), interpersonal therapy, behavioral activation therapy, and brief psychodynamic therapy, have demonstrated effectiveness in treating LLD.10,11 Mindfulness-based CT (MBCT), an 8-week group training that combines mindfulness meditation techniques with elements of cognitive-behavioral therapy, has emerged as a promising approach. Mindfulness-based CT aims to help participants recognize and disengage from maladaptive cognitive patterns while fostering a nonjudgmental and compassionate attitude toward their thoughts and feelings.12 As the third wave of CT, MBCT has shown great promise in reducing the relapse and recurrence of depressive episodes among individuals who have recovered from major depression. Notably, MBCT stands out from other mindfulness-based interventions (MBIs), such as mindfulness stress reduction. Theoretically, operating as a manualized therapy, MBCT has the potential to enhance patients’ metacognitive awareness while mitigating cognitive and emotional rumination, thereby contributing to the amelioration of depressive symptoms.8,9
Existing meta-analyses have consistently demonstrated the feasibility of MBIs in mitigating depressive symptoms. A meta-analysis incorporating 31 randomized controlled trials with 2532 participants experiencing acute depressive symptoms revealed a mean effect size of −0.76 (95% Confidence Intervals (CI), −0.95-0.56, P < .01) for MBCT compared to individuals on a waitlist or receiving no treatment. Over time, the mean treatment effect size remained substantial at −0.97 (95% CI, −1.68-0.26, P = .01) based on 4 included studies.13 Thimm et al14 found that the effects of MBCT on depression, assessed using the Hamilton Depression Rating Scale or the Beck Depression Inventory (BDI), were consistently effective, with the effect size showing no moderation based on the time of publication.14 Kishita et al15 reported a significant moderate effect size for depression (g = 0.5, 95% CI, 0.34-0.75) and a significant overall effect size for anxiety in older adults undergoing MBCT and acceptance and commitment therapy (g = 0.58, 95% CI, 0.27-0.88).15
However, previous meta-analyses have predominantly focused on adults, with older adults receiving less attention. Nonetheless, there is evidence supporting the efficacy of MBCBTs, including acceptance and commitment therapy and MBCT, in treating depression in adults.15 Consequently, it is reasonable to infer that MBCT could improve depressive symptoms in older adults. Existing research has demonstrated that MBCT strengthens functional and structural connections between the amygdala and the medial frontal gyrus, and this increase in communication correlates with improvements in clinical symptoms.16 Summarizing research on MBCT aids in ascertaining its effectiveness and exploring further clinical promotion.
Therefore, this meta-analysis aimed to comprehend the impact of exclusively utilizing MBCT in older adults with current depression. Acknowledging the limitations of inadequate high-quality randomized controlled studies, this study also considered pre-post studies without a control group. The objective of this study was to determine whether the published research supports a call for additional studies to elucidate the effectiveness of MBCT in reducing depressive symptoms in older adults.
Material and Methods
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (a) participants aged ≥60 years old; (b) exclusive use of MBCT as an intervention; (c) inclusion of active or passive control for comparison; (d) examination of the effects of MBCT pre- and post-intervention for LLD; (e) peer-reviewed publication; (f) provision of sufficient information for effect size computation; and (g) publication in English. Exclusion criteria encompassed: (a) recruitment of participants diagnosed with severe physical diseases; (b) lack of examination of treatment outcomes for depression; or (c) comparison with findings from other systematic reviews or meta-analyses.
Search Strategies
A comprehensive search was conducted in electronic databases, including PubMed (title and abstract), EBSCOhost (abstract), Scopus (title, abstracts, and keywords), and Cochrane Central Register of Controlled Trials (title, abstracts, and keywords) in July 2021. The search terms “mindfulness-based cognitive therapy” and “older adult population” were employed in PubMed, and “depression” was added to other databases for precision (Table 1). ClinicalTrials.gov was also searched for ongoing or unpublished articles, and manual searches of references from identified trials and systematic reviews were performed.
Table 1.
Search Strategy
| Name | Search Strategy | Number |
|---|---|---|
| PubMed | (“mindfulness-based cognitive therapy”[Title/Abstract] OR “mindfulness based cognitive therapy”[Title/Abstract] OR “MBCT”[Title/Abstract]) AND (Elder*[Title/Abstract] OR old adults [Title/Abstract] OR aging [Title/Abstract] OR elder [Title/Abstract] OR older [Title/Abstract] OR aged [Title/Abstract] OR geriatric [Title/Abstract] OR senile [Title/Abstract] OR “late life”[Title/Abstract] OR late-life [Title/Abstract]) | 51 |
| Scopus | (TITLE-ABS-KEY ({mindfulness-based cognitive therapy} OR “mindfulness based cognitive therapy” OR MBCT) AND TITLE-ABS-KEY (depression OR depressive OR mood OR depress* OR “depressive disorder” OR “mood disorder” OR “Dysthymic disorder”) AND TITLE-ABS-KEY (elder* OR “old adults” OR aging OR elder OR older OR aged OR geriatric OR senile OR “late life” OR “old* adult* “)) | 246 |
| EBSCOhost | (TITLE-ABS-KEY ({mindfulness-based cognitive therapy} OR “mindfulness based cognitive therapy” OR MBCT) AND TITLE-ABS-KEY (depression OR depressive OR mood OR depress* OR “depressive disorder” OR “mood disorder” OR “Dysthymic disorder”) AND TITLE-ABS-KEY (elder* OR “old adults” OR aging OR elder OR older OR aged OR geriatric OR senile OR “late life”)) | 32 |
| Cochrane Central Register of Controlled Trails | (TITLE-ABS-KEY ({mindfulness-based cognitive therapy} OR “mindfulness based cognitive therapy” OR MBCT) AND TITLE-ABS-KEY (depression OR depressive OR mood OR depress* OR “depressive disorder” OR “mood disorder” OR “Dysthymic disorder”) AND TITLE-ABS-KEY (elder* OR “old adults” OR aging OR elder OR older OR aged OR geriatric OR senile OR “late life” OR “old* adult* “)) | 34 |
| ClinicalTrails.gov | (([Condition or disease] “mindfulness based cognitive therapy”) AND ([Other term] “depression”)) | 31 |
Study Selection
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 guidelines for systematic review reporting, the initial step involved eliminating duplicates from the total number of identified records using EndNote X9. Subsequently, the abstracts of the remaining records underwent screening to identify publications eligible for full-text evaluation. The screening aimed to select research meeting the predefined inclusion criteria. This process was carried out independently by 2 authors. Any uncertainties or discrepancies in the eligibility of specific papers were resolved through a discussion with a third person to reach a consensus. Throughout the screening procedure, all relevant features of studies deemed ineligible for inclusion were comprehensively documented. The systematic review was registered at INPLASY (https://inplasy.com) (Registration No: INPLASY202210121).
Data Collection Process
Eligible studies underwent coding based on the first author’s name and publication year. The characteristics and findings of the enrolled studies were systematically organized and presented in Table 2. Information extracted from eligible studies included country, treatment target, sample source, participant age range, characteristics of control and intervention groups, format of MBCT, length of follow-up, measurements, outcomes, and therapist training experiences. The data extraction process was independently conducted by the first author and subsequently passed to other authors for thorough evaluation and discussion to mitigate potential errors.
Table 2.
Characteristic of Studies
| Study Code | Country (Design) |
Treatment Target | Sample | Age Range (Years) (Mean) |
Treatment (N)c |
Control (N)c |
Therapy Format | Depression Measurements |
Other Measurements |
|---|---|---|---|---|---|---|---|---|---|
| Torres, 2019 | Canada (a blind, 2-arm RCT) |
LLA/LLD | 5 primary care centers | ≥60 (67.8) |
MBCT (PP-27) |
TAU(26) | Group | PHQ-9 | GAD-7, EQ-5D |
| O’connor, 2014 | Denmark (a non-randomized, controlled pilot design) |
Long-term bereavement-related distress. | The Danish Central Person Register (CPR) |
65-80 (77) |
MBCT (ITT-18); MBCT (PP-12) |
WLC(18) | Group | BDI-II | HTQ, ICG-R; CES |
| Splevins, 2009 | Northwest England (a pre-post within-subjects design) |
Moderate levels of depression, anxiety, and stress |
In response to advertisements or referral by medical staff | 49-79 (65) (4 carers under 65 included reasonably) |
MBCT (PP-22) |
N | Group | DASS-21 | KIMS |
| Meeten, 2015 | UK (a mixed methodology study) |
Older people in recovery from recurrent depression and/or experiencing mild chronic depression | Older People’s Mental Health Services (OPMHS) |
65-78 (71.25) |
MBCT (PP-13) |
N | Group | DASS-21 | Ryff Well-being scale; MBCT Rating Questions |
| Labbé, 2016 | Canada (a retrospective case series) |
Acute anxiety and depression | Outpatient | 66-82 (74.5) | MBCT (PP-4*) |
N | Group | BDI-2 | BAI; MoCA |
BAI, Beck Anxiety Inventory; BDI-2, Beck Depression Inventory 2; BDI-II, The Beck Depression Inventory; CES, The Centrality of Event Scale; DASS-21, The Depression, Anxiety and Stress scales; EQ-5D, EuroQol Five Dimension Scale questionnaire; GAD-7, Generalized Anxiety Disorder-7; HTQ, The Harvard Trauma Questionnaire—Part IV; ICG-R, The Inventory of Complicated Grief—Revised; KIMS, The Kentucky Inventory of Mindfulness Skills; MBCT, mindfulness-based cognitive therapy; RCT, Randomized controlled trial; LLA, Late-life Anxiety; LLD, Late-life Depression; ITT-18, intention-to-treat-18; MoCA, Montreal Cognitive Assessment; PP, per protocol; PHQ-9, Patient Health Questionnaire-9; Ryff, The Ryff Psychological Well-being Inventory; TAU, Treat as usual; WLC, Wait-list control.
*4 means completers who have depression scores.
All controlled studies reporting means, Standard Deviations (SD), and sample sizes at both pretest and posttest stages were compiled. When available, data was retrieved from intent-to-treat (ITT) samples using the last observation carried forward technique. Preference was given to studies utilizing symptom-specific depression scales such as the BDI-II and the Patient Health Questionnaire-9. Additionally, studies employing broader measures of depression symptoms, such as the Depression Anxiety Stress Scales, were considered. In instances where data or other relevant information for analysis were not available, efforts were made to contact study authors for the necessary details, and papers with inaccessible data were excluded.
Risk of Bias Within/Across Studies
Methodological quality assessment included the following information extracted from each trial:17 (a) the procedure for tracking treatment adherence; and (b) follow-up outcome assessments. In controlled trials, additional information was collected on (a) the type of data analysis, (b) research design methodology, (c) whether assessors were blinded to group allocations, and (d) whether the duration of treatment was consistent across all groups. While the quality of studies did not determine eligibility, bias potential was evaluated by the first author, reexamined by the other author, and subsequently discussed among all authors.
Statistical Analysis
Comprehensive Meta-Analysis (CMA) software 2.0 was employed for data analysis (National Institutes of Health, Bethesda, MD, USA). Effect sizes were determined using means, SDs, and sample sizes to calculate Hedge’s g, a variant of Cohen’s d, which adjusts for biases resulting from small sample sizes (Hedges & Olkin, 1985).17 For each included study, CMA was utilized to ascertain the corresponding z and P values, along with the 95% CI. When correlations between pretreatment and posttreatment outcomes were unknown, a conservative estimate (r = 0.7) suggested by Rosenthal (1986)18 was utilized.
Heterogeneity analysis employed Q and I 2 indicators, where I 2 denotes the percentage of variance between studies in the population variance (I 2 = 25%, 50%, and 75% representing low, medium, and high heterogeneity, respectively). A random-effects model was selected when the I2 value was ≥75% and Q indicated substantial heterogeneity, and vice versa.19
To evaluate publication bias, Rosenthal’s fail-safe N test was selected. This method involves calculating the number of missing papers that would need to be retrieved and included in the analysis to reduce the overall effect size to a non-significant level. A larger fail-safe N (Nfs) suggests a lower likelihood of bias. However, if Nfs is less than 5k + 10 (where k is the number of original studies), the possibility of publication bias cannot be ignored.
Results
Study Selection
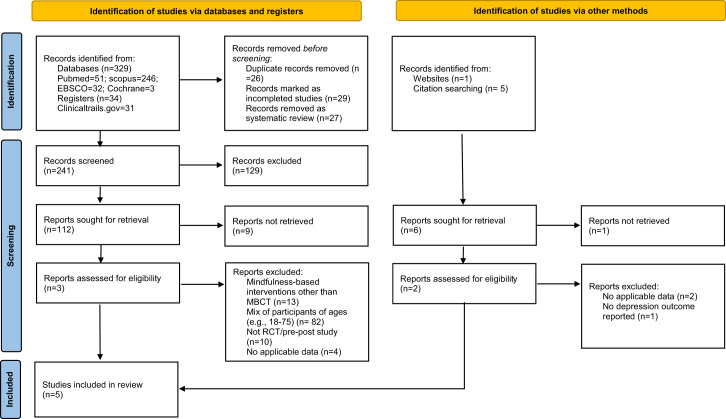
The study’s selection process is illustrated in Figure 1. Our search yielded 315 citations; duplicates (n = 50) were automatically removed, and incomplete articles (n = 29) on clinical trials were excluded. Subsequently, 239 articles were screened based on titles and abstracts, making 118 reports available for full-text screening. However, only 5 studies met the inclusion criteria. Two studies20,21 were excluded due to unavailable data for meta-analysis, and 1 study22 was included despite having participants under 65 years old, as they were caregivers for older adults. Disagreements were resolved through discussion with other authors.
Figure 1.
Flow chart. MBCT, Mindfulness-Based Cognitive Therapy; RCT, Randomized Controlled Trial
Characteristics of Included Studies
Table 2 and Table 3 present the key features of the studies incorporated into this meta-analysis. The study encompassed a cohort of 196 elderly participants engaged in mindfulness-based cognitive studies (treatment, n = 109; control, n= 65). Five studies were identified, comprising 2 controlled studies and 3 pre-post studies. Among the controlled studies, 1 employed a double-blind randomized controlled trial design utilizing treatment as usual as controls during treatment, while the other utilized a waitlist control group for comparative purposes.
Table 3.
Therapist and Treatment Characteristics for Mindfulness-Based Cognitive Therapy Studies with Older Adults
| Study Code |
Number of Sessions | Training Experiences of Therapist(s) Reported | Training Experiences of Participants | Age-Specific Modifications made to the Standard Manual | Home- Practicing |
Follow-Up | Remission Rate (MBCT Group) |
||
|---|---|---|---|---|---|---|---|---|---|
| MBCT | Gerontology | CBT | Meditation | ||||||
| Torres, 2019 | 2 hours × 8 weeks | YES | NO | N | N | YES, from time to requirementsa | YES, 25 minutes daily | 8 weeks | 16% |
| O’connor, 2014 | 2 hours × 8 weeks | YES | NO | N | N | YES, reduced the practicing time from 2½ to 2 hours per session; | YES, 40 minutes a day | 5 months | 55% |
| Splevins, 2009 | 2 hours × 8 weeks | N | N | YES (18%) | YES (9%) | N | N | NO | 50.0% |
| Meeten, 2015 | 2 hours × 8 weeks | YES | NO | N | N | YES | NO | Y, 6 months | 56.3% |
| Labbé, 2016 | 2 hours × 8 weeks | YES | N | N | N | N | N | N | 66.7% |
aReducing time of body scan meditation; using chairs; allowing patients to remain seated during yoga practices; encouraging patients to modify postures for safety and well-being; providing pillows; slowing down the pace of walking meditation; projecting loudly; and taking more frequent breaks.
MBCT, Mindfulness-Based Cognitive Therapy; CBT, Cognitive Behavior Therapy; Y, Yes; ITT, intent-to-treat; N, not clearly; PP, per protocol.
The mean age of participants across the 5 studies ranged from 65 to 77 years. The primary focus of the included articles was on addressing depressive symptoms, supplemented by consideration of other emotional indices such as anxiety or stress. Three studies measured additional indices correlated with depression, including mindfulness skills, quality of life, and cognition degree. Predominantly, studies opted for per protocol as the preferred statistical analysis, with only 1 study adopting intention-to-treat (ITT) analysis. Notably, the absence of ITT analysis resulted in a high dropout rate, exceeding 50% in 4 studies, while 1 study reported a 16% dropout rate for the depression index.
All studies uniformly employed a group format for the implementation of MBCT. Only 1 study enlisted therapists trained in geriatric psychology, while the remaining studies predominantly featured psychiatrists or other professionals with substantial experience in MBCT. Although 1 article explored participants’ experiences related to cognitive behavior therapy (CBT) or meditation, no significant associations were found between gender, previous related experience, or any outcome variables. Two studies detailed specific adaptations made to the manual’s recommendations to ensure suitability for older adults, such as adjusting session lengths, slowing down walking meditation, and encouraging participants to modify comfort postures for enhanced well-being and safety. Additionally, 2 studies reported the incorporation of home practice after group sessions, and 1 study provided insights into the effect size of MBCT practice among older adults.
Synthesis of Results
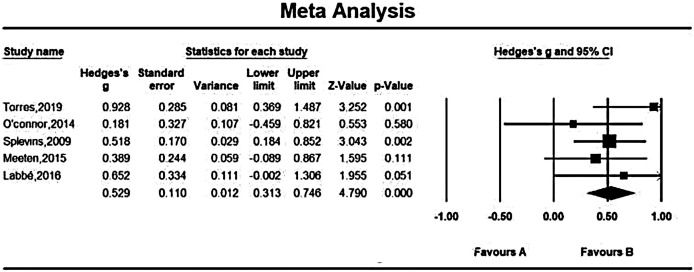
Effects on Late-Life Depression:
Measurements of depressed symptoms across 5 studies yielded effect sizes ranging from “not effective” (g = 0.18) to “large and positive” (g = 0.93) (Figure 2). The fixed-effects model indicated an overall effect size of g = 0.53 (95% CI, 0.31-0.75), suggesting a substantial moderating effect of mindfulness-based cognitive treatment on depression symptoms in older individuals (z = 4.79, P < .01). Low heterogeneity between study effect sizes was observed (Q (4) = 3.56, P > 0.1; I 2 = 0).
Figure 2.
Effect on late-life depression.
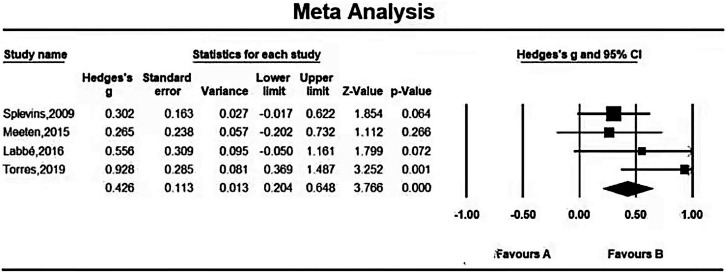
Effects on Late-Life Anxiety:
Four studies assessing anxiety symptoms showed varying effect sizes from ineffective (g = 0.27) to large and positive (g = 0.93) (Figure 3). The fixed-effects model yielded an overall effect size of g = 0.43 (95% CI, 0.20-0.65), signifying a significant moderating effect of MBCT on anxiety symptoms in the elderly (z = 3.77, P < .01). Significant moderate heterogeneity between study effect sizes was identified (Q(3) = 4.30, P> 0.1; I2 = 30.27).
Figure 3.
Effect on late-life anxiety.
Publication Bias
Studies on Late-Life Depression:
The observed effect sizes for LLD may lack robustness, as indicated by Rosenthal’s fail-safe N method, estimating that 23 missing studies would be required before the aggregate 2-tailed P-value exceeded .05. This suggests the potential presence of publication bias, emphasizing the need for caution when interpreting findings related to depression.
Studies on Late-Life Anxiety:
In studies on late-life anxiety, Rosenthal’s Fail-safe N approach suggested that 16 missing trials would be necessary before the combined 2-tailed P-value exceeded .05. This implies that the observed effect sizes for anxiety might not be robust, raising concerns about potential publication bias in studies related to anxiety.
Study Quality:
Table 4 provides an assessment of the study’s quality. Notably, while most studies reported reasons for remission to explore feasibility or acceptability, participant adherence during sessions was often overlooked. High attrition bias, linked to the absence of ITT analyses, was identified in 4 out of 5 studies. Various factors, such as inconvenience due to aging or poor health, contributed to elevated attrition rates. Among the 2 studies, Meeten et al23 suggested a promising impact on anxiety at follow-up but not on depression. Depression scores tended to revert to baseline levels. O’Connor et al24 revealed that 29% (5 participants) in the waitlist group, and none in the intervention group, qualified as experiencing exacerbated depressive symptoms at follow-up. All studies demonstrated statistically significant small to large effects in depression from pre- to post-intervention. Torres et al (2019) did not publish their longer-term follow-up measures, but the same group presented these results in Dikaios et al21. Similarly, a main randomized controlled trial paper may not report mindfulness measures, but planned secondary analyses could publish these separately in another paper.
Table 4.
Study Quality Assessment
| Study Code | Method of Treatment Adherence Reporting | Administration of Measures at Follow-Up | Use of Validated Mindfulness Measures | Using Intent-to-Treat Data Analyses | Randomization Method | Assessors were Blind Regarding Allocation to Group | Treatment Time was Equal Across Groups |
|---|---|---|---|---|---|---|---|
| Torres, 2019 | − | − | − | + | + | + | + |
| O’connor, 2014 | − | + | − | + | − | − | + |
| Splevins, 2009 | − | − | + | − | NA | NA | NA |
| Meeten, 2015 | − | + | + | − | NA | NA | NA |
| Labbé, 2016 | ? | − | − | − | NA | NA | NA |
Key: present (+), absent (−), unclear (?), not applicable (NA).
Only 1 study employed an appropriate randomization strategy (e.g., randomization by a third party) and a blinded design (e.g., concealing group allocation from outcome assessors and investigators). The remaining studies measured only the change in scores of emotional well-being pre- and post-interventions, with a few also assessing quality of life or mindfulness ability. Moreover, none of the articles included active control groups.
Discussion
The findings of this study suggest that adopting MBCT for treating depression in older adults holds potential benefits for enhancing their emotional well-being. We found that this approach was effective in alleviating depressive symptoms, with a total reported effect size of g = 0.53 (95% CI, 0.31%-0.75%). Besides, MBCT exhibited a comparable moderating effect size for anxiety (g = 0.43, 95% CI, 0.20-0.65). These outcomes align with findings reported by Kishita et al,15 who documented that mindfulness-based CBTs have a moderately effective overall effect size (g = 0.55; g = 0.58) for depressive or anxiety symptoms in older adults with diverse physical and psychological conditions, such as chronic pain.15 However, studies included in our meta-analysis did not provide detailed information about the physical conditions of the participants. Consequently, the effectiveness of MBCT in depressed older adults with somatic diseases remains unclear. Additionally, the presence of publication bias was more prominent compared to the previous meta-analysis. This discrepancy can be attributed to variations in the design of the included studies and the likelihood that negative results were less likely to be published.
The findings of this study provide insights into mental health nursing, revealing that approximately 4.6% to 9.3% of older adults experience LLD, which may be particularly critical in low- and middle-income countries.1 In recent years, mental health experts have been actively exploring treatments for LLD, while medical policymakers have been diligently working to improve public access to effective LLD treatments. Notably, in Guangdong, one of the largest provinces in China, MBCT has been incorporated into resident medical insurance since 2021.25 Given the shortage of psychotherapists, mental health nurses who obtain national occupational qualifications as psychotherapists and complete MBCT training are now authorized to conduct MBCT. This policy carries 2 significant implications for mental health nursing. From the perspective of nurses, being qualified to conduct MBCT signifies an enrichment of their professionalism. As supplementary professionals, mental health nurses authorized to perform MBCT play a crucial role in the treatment of LLD. Furthermore, MBCT, combining mindfulness training and CT, aims to assist individuals in disengaging from negative thinking by recognizing emotional deterioration without judgment or reactive responses.26 From the standpoint of mental health services, educating nurses in MBCT enhances their post-competency in caring for patients with mood disorders.
Apart from the implications in the nursing field, several recommendations for future research design emerge from this study. First, researchers should be encouraged to conduct randomized controlled trials (RCTs) with ITT analysis to analyze data or explore other types of psychotherapy compared to MBCT in quasi-experimental studies. Second, enhancing study quality could involve researchers incorporating measures of adherence and monitoring adverse events throughout the intervention process, along with including additional relevant outcome measures. Last but not least, future studies should investigate factors that might influence treatment outcomes in older adults, such as the duration of the sessions, the components of the intervention, and other physical health considerations.
A notable strength of the current study is its provision of preliminary support for MBCT in the context of LLD. Despite the majority of participants experiencing depression, with only a few in recovery from recurrent depression and 4 under the age of 65, the study’s findings highlight the immediate positive impact of MBCT on depressive symptoms in older adults. However, it is crucial to acknowledge certain limitations of this study. Firstly, due to the current scarcity of relevant RCTs, this meta-analysis focuses on only 1 RCT, with the included studies primarily employing pre- and post-designs and 1 study being a retrospective case series, potentially introducing recall bias. Secondly, insufficient data were available to assess the long-term effects of the MBCT approach in this meta-analysis, leaving uncertainty about the duration of MBCT effects. Despite these limitations and a relatively small sample size, this study provides valuable insights and suggests adaptations and developments for future research.
Conclusion
Our study demonstrates the efficacy of MBCT as a viable approach for reducing depressive symptoms and improving the well-being of older adults. To our knowledge, this is the first meta-analysis focusing on the impact of MBCT among older adults aged over 65 years with depression. In summary, our findings provide compelling evidence that mindfulness training serves as an effective treatment for a range of issues affecting older adults, including depression, anxiety, chronic pain, loneliness, and caregiver stress.27 Future studies could benefit from exploring the specific role of MBCT and its value in the treatment of depression among older adults.
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Availability of Data and Materials: All data points generated or analyzed during this study are included in this article, and there are no further underlying data necessary to reproduce the results.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – J.Y., Z.H., A.X.; Design – J.Y., A.X.; Supervision – J.G., A.X.; Resources – A.X., J.G.; Materials – J.Y., Y.P., C.W.; Data Collection and/or Processing – C.W., Y.P., S.W., W.W.; Analysis and/or Interpretation – J.Y., J.G.; Literature Search – C.W., Y.P.; Writing – J.Y., Y.P., C.W.; Critical Review – Z.H., S.W., J.G., A.X.
Acknowledgments: We would like to thank all the patients who have contributed to this study.
Declaration of Interests: The authors have no conflict of interest to declare.
References
- 1. Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life--systematic review and meta-analysis. J Affect Disord. 2012;136(3):212 221. ( 10.1016/j.jad.2010.11.033) [DOI] [PubMed] [Google Scholar]
- 2. McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London, UK: King’s Fund; 2008. [Google Scholar]
- 3. Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961 1970. ( 10.1016/S0140-6736(05)66665-2) [DOI] [PubMed] [Google Scholar]
- 4. Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harv Rev Psychiatry. 2018;26(4):175 184. ( 10.1097/HRP.0000000000000162) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Almeida OP. Prevention of depression in older age. Maturitas. 2014;79(2):136 141. ( 10.1016/j.maturitas.2014.03.005) [DOI] [PubMed] [Google Scholar]
- 6. Reynolds CF, 3RD, Dew MA, Pollock BG, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354(11):1130 1138. ( 10.1056/NEJMoa052619) [DOI] [PubMed] [Google Scholar]
- 7. Macqueen G, Santaguida P, Keshavarz H, et al. Systematic review of clinical practice guidelines for failed antidepressant treatment response in major depressive disorder, Dysthymia, and subthreshold depression in adults. Can J Psychiatry Rev Canadienne Psychiatr. 2017;62(1):11 23. ( 10.1177/0706743716664885) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kok RM, Reynolds CF, 3RD. Management of depression in older adults: a review. JAMA. 2017;317(20):2114 2122. ( 10.1001/jama.2017.5706) [DOI] [PubMed] [Google Scholar]
- 9. Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1 12. ( 10.1016/j.cpr.2015.01.006) [DOI] [PubMed] [Google Scholar]
- 10. Orgeta V, Brede J, Livingston G. Behavioural activation for depression in older people: systematic review and meta-analysis. Br J Psychiatry. 2017;211(5):274 279. ( 10.1192/bjp.bp.117.205021) [DOI] [PubMed] [Google Scholar]
- 11. Cuijpers P, Karyotaki E, Eckshtain D, et al. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiatry. 2020;77(7):694 702. ( 10.1001/jamapsychiatry.2020.0164) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cladder-Micus MB, Speckens AEM, Vrijsen JN, T Donders AR, Becker ES, Spijker J. Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depress Anxiety. 2018;35(10):914 924. ( 10.1002/da.22788) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lenz AS, Hall J, Bailey Smith L. Meta-analysis of group mindfulness-based cognitive therapy for decreasing symptoms of acute depression. J Spec Group Work. 2016;41(1):44 70. ( 10.1080/01933922.2015.1111488) [DOI] [Google Scholar]
- 14. Thimm JC, Johnsen TJ. Time trends in the effects of mindfulness-based cognitive therapy for depression: A meta-analysis. Scand J Psychol. 2020;61(4):582 591. ( 10.1111/sjop.12642) [DOI] [PubMed] [Google Scholar]
- 15. Kishita N, Takei Y, Stewart I. A meta-analysis of third wave mindfulness-based cognitive behavioral therapies for older people. Int J Geriatr Psychiatry. 2017;32(12):1352 1361. ( 10.1002/gps.4621) [DOI] [PubMed] [Google Scholar]
- 16. Li H, Yan W, Wang Q, et al. Mindfulness-based cognitive therapy regulates brain connectivity in patients with late-life depression. Front Psychiatry. 2022;13:841461. ( 10.3389/fpsyt.2022.841461) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vøllestad J, Nielsen MB, Nielsen GH. Mindfulness- and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. Br J Clin Psychol. 2012;51(3):239 260. ( 10.1111/j.2044-8260.2011.02024.x) [DOI] [PubMed] [Google Scholar]
- 18. Rosenthal R. Meta-analytic procedures for social science research. Educ Res. 1986;15:18. [Google Scholar]
- 19. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed). 2003;327(7414):557 560. ( 10.1136/bmj.327.7414.557) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Foulk MA, Ingersoll-Dayton B, Kavanagh J, Robinson E, Kales HC. Mindfulness-based cognitive therapy with older adults: an exploratory study. J Gerontol Soc Work. 2014;57(5):498 520. ( 10.1080/01634372.2013.869787) [DOI] [PubMed] [Google Scholar]
- 21. Dikaios E, Escobar S, Nassim M, Su CL, Torres-Platas SG, Rej S. Continuation Sessions of Mindfulness-Based Cognitive Therapy (MBCT-C) vs. Treatment as usual in late-life depression and anxiety: an open-label extension study. Int J Geriatr Psychiatry Continuation Sessions of Mindfulness-Based Cognitive Therapy (MBCT-C) vs. 2020;35(10):1228 1232. ( 10.1002/gps.5360) [DOI] [PubMed] [Google Scholar]
- 22. Splevins K, Smith A, Simpson J. Do improvements in emotional distress correlate with becoming more mindful? A study of older adults. Aging Ment Health. 2009;13(3):328 335. ( 10.1080/13607860802459807) [DOI] [PubMed] [Google Scholar]
- 23. Meeten F, Whiting S, Williams CM. An exploratory study of group mindfulness-based cognitive therapy for older people with depression. Mindfulness. 2015;6(3):467 474. ( 10.1007/s12671-014-0279-1) [DOI] [PubMed] [Google Scholar]
- 24. O’Connor T. How to set up, run and evaluate a training program based on behavior modeling principles. Training. 1979;16(1):64 67. [PubMed] [Google Scholar]
- 25. Bureau GMS. Basic Medical Insurance, Industrial Injury Insurance and Maternity Insurance in Guangdong Province Catalogue of Diagnosis and Treatment Projects (in Chinese); 2021. [Google Scholar]
- 26. Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression. Psychiatr Clin North Am. 2017;40(4):739 749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jeanne M, Sorrell PRN FAAN. Meditation for older adult- a new look at an ancient intervention for mental health. J Psychosoc Nurs. 2015;53(5):15 19. [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a