Abstract
Earthquakes are catastrophic natural disasters that cause extensive damage to infrastructure and disrupt the lives of millions worldwide. Beyond the immediate physical and psychological damage caused by earthquakes, these events can significantly impact respiratory health. The inhalation of dust, smoke, particulates, toxic gases, and asbestos exposure can lead to various respiratory health pathologies. These include respiratory infections, exacerbations of pre-existing respiratory diseases, chest traumas, and pulmonary and venous thromboembolism. Longitudinal studies are necessary to assess the long-term respiratory health effects in affected populations. By addressing these knowledge gaps, future mitigation strategies and preparedness measures can be developed to minimize the respiratory health impacts of earthquakes and improve the well-being of affected communities. Robust building infrastructure and comprehensive earthquake preparedness are emerging as the most important determinants for not only mitigating building collapse but also significantly reducing the potential health impacts that follow. This comprehensive review aims to provide a systematic overview of the lung health impacts of earthquakes. It highlights the need for further research to identify specific pollutants, air contaminants, and environmental factors contributing to respiratory health issues following earthquakes.
Keywords: Earthquake, dust, exacerbation, respiratory diseases, asbestos, respiratory infections, trauma
Main Points
Earthquakes pose significant respiratory health risks due to environmental and occupational exposures like particulates, asbestos, mold, and hazardous chemicals.
Addressing these risks requires: training healthcare professionals, monitoring exposure levels, and constructing resilient buildings.
Longitudinal studies are necessary to assess the long-term respiratory health effects in affected populations.
Interdisciplinary collaboration among public health experts, geologists, engineers, and policymakers is essential for holistic approaches to mitigate immediate and long-term respiratory health impacts.
Introduction
Earthquakes are one of the most devastating natural disasters, causing extensive damage to infrastructure and disrupting the lives of millions worldwide.1,2 Earthquakes are linked to the movement of tectonic plates and can be influenced by several factors, such as plate boundaries, geological structures, and volcanic activity.3,4 These seismic phenomena are often destructive and can result in significant loss of life and property damage. Globally, seismic events surpass 1 million annually, implying a frequency of approximately 2 earthquakes per minute.5,6 According to the U.S. Geological Survey (USGS), on average, around 18 earthquakes with magnitudes between 7.0 and 7.9 on the Richter scale have occurred annually since 1900, while earthquakes with magnitudes of 8.0 and above happen only once a year on average. Recently, a decrease in the frequency of earthquakes with magnitudes of 7.0 and above has been observed.7
On February 6, 2023, the 7.8 and 7.6 magnitude earthquakes hit Southeastern Turkey in about 78 500 km2 and the north-western territories of Syria, causing widespread damage in both countries. The earthquakes have resulted in more than 50 000 deaths and 120 000 injuries, with 448 healthcare providers, including 101 physicians, losing their lives. The affected area had approximately 15 million people, including 2 million Syrian refugees.8
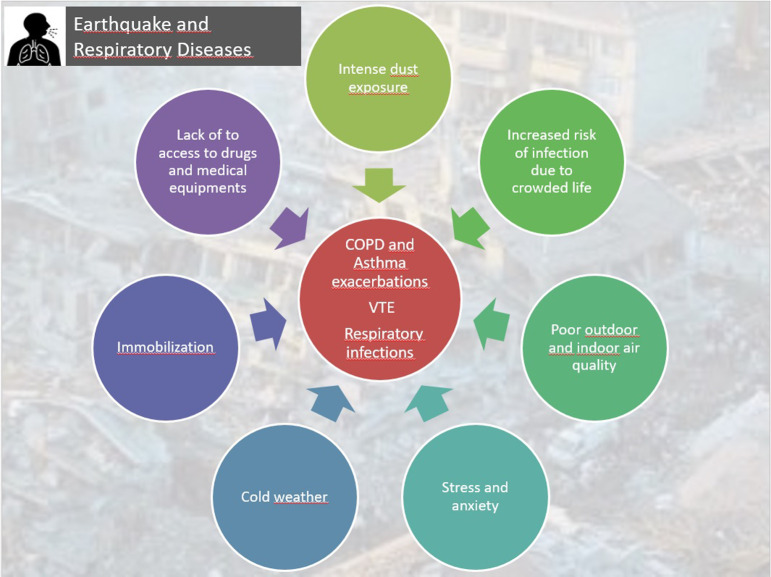
Apart from the immediate physical and psychological harm caused by earthquakes, these events can also significantly impact individuals’ respiratory health. These impacts include the inhalation of dust, smoke, particulates, and other toxic gases; exposure to asbestos; respiratory infections; exacerbation of respiratory diseases; chest traumas; and venous thromboembolism (Table 1, Figure 1).9-12 In nations where the building infrastructure boasts a high standard of quality, a considerable reduction is observed both in the number of individuals affected by the mentioned health effects and in the intensity of their impact. Consequently, it becomes evident that factors such as the quality of the building stock and the level of earthquake preparedness exert a more substantial influence on the emergence of health effects than the sheer magnitude of the seismic event itself. This review aims to provide a comprehensive and systematic overview of the lung health impacts of earthquakes.
Table 1.
Main Impacts of an Earthquake on Lung Health
|
|
|
|
|
|
Figure 1.
Effects of an earthquake on respiratory diseases.
Inhaled Irritants and Respiratory Impacts
Particulate Matters: Dust and Silica Particles
Airborne particulate matter (PM) is a heterogeneous mixture comprising of various chemical components rather than a single pollutant. It encompasses a complex blend of solid particles, liquid-coated solid cores, and minuscule liquid droplets in the form of aerosols. These particles can encompass inorganic ions, metallic compounds, elemental carbon, organic compounds, and substances originating from the Earth’s crust.13 They exhibit significant variations in size, shape, and chemical composition. To regulate air quality, particle diameter is a crucial metric, with particles that measure 10 μm or smaller (PM10) being inhalable and capable of negatively impacting human health. On the other hand, fine PM (PM2.5) refers to particles with a diameter of 2.5 μm or less.
During earthquakes, releasing particulate pollution containing dust and silica particles from collapsed buildings into the air severely threatens respiratory health. Inhaling these particles, particularly the PM2.5 particles, can facilitate deep penetration into the respiratory system. General sources of these particles include car exhaust, in particular diesel exhaust, industrial processes, construction activities, and environmental dust and pollen. Prolonged exposure to such particles can exacerbate preexisting lung conditions, cause respiratory disorders, and elevate the risk of respiratory infections.8,9
Among those most exposed to PM following earthquakes are victims and search-and-rescue teams, who are exposed to dust particles in the debris during and immediately after the seismic event. Demolition teams engaged in dismantling buildings are severely affected by the earthquake, and teams involved in rubble removal also face substantial exposure. Furthermore, the concentrated presence of airborne dust particles during debris clearance poses a significant risk of acute and chronic respiratory diseases for individuals residing near the debris and those living in nearby tent cities.14-16
On January 17, 1995, a significant earthquake, known as the Hanshin earthquake, struck the city of Hyogo, Japan. Within a year after the earthquake, the demolition of damaged buildings commenced. An air quality assessment conducted in the earthquake-affected regions revealed high total suspended particulate levels in heavily damaged areas, with a maximum concentration of 150 µg/m3 measured at 5 locations. Additionally, 8 concrete, mortar, and soil dust samples were collected and analyzed using the elemental x-ray fluorescence method. The concrete and mortar samples exhibited calcium (Ca) and sulfur (S) elements. In contrast, the soil samples contained heavy metals such as titanium (Ti), iron (Fe), and zirconium (Zi).17 Another study conducted after the Hanshin earthquake disclosed that the concentration of inhalable dust particles in the demolition area exceeded the recommended threshold limit value of 2 mg/m3 set by the Japan Society for Occupational Health.18 In 2011, a significant earthquake of approximately 9 hit the city of Tohoku, Japan, followed by a subsequent tsunami 6 minutes later, resulting in many casualties and injuries.19 Three weeks after the earthquake, a case of pulmonary alveolar proteinosis was reported due to the intense inhalation of fine dust particles.14 Following an earthquake in central Italy in 2009, the affected region witnessed thousands of construction sites over the course of 10 years. Mastrantonio et al20 determined that workers engaged in manual demolition activities were exposed to inhalable dust particles exceeding the threshold limit value of 10 mg/m3.
In 2002, a 6-magnitude earthquake in Sultandagi, Afyon, Turkey, resulted in 39 deaths and 325 injured individuals. This study showed that one of the leading causes of death was respiratory failure resulting from inhaling dust particles associated with the traditional architecture of rural areas.21 Research on the increased dust density in earthquake-affected areas after seismic events and the specific PM species contributing to this increase is limited. Identifying such data immediately after and in the days following an earthquake, during rescue and demolition activities, would contribute to raising awareness and implementing measures to safeguard the lung health of survivors and aid teams.
Radon, Carbon Dioxide, and Carbon Monoxide Gases
Radon and carbon dioxide (CO2) can be released during and after an earthquake.22 Radon is a naturally occurring radioactive gas produced by the decay of uranium in soil and rocks and can seep into buildings through cracks and other openings.23,24 Carbon dioxide is a colorless and odorless gas that is also naturally occurring but can be released from underground sources during seismic activity.25 These radon offspring are thought to be the primary cause of human exposure to alpha radiation, which damages DNA and causes cellular harm to the respiratory system. Lung cancer and radon-induced lung illnesses eventually develop because of these alterations in the respiratory epithelium.26 Studies show that exposure to radon gas can increase the risk of lung cancer, particularly for those exposed to high gas levels over a long period of time. Exposure to high radon levels can cause symptoms such as headaches, dizziness, and nausea.27 Exposure to CO2 can also be dangerous, particularly in sealed spaces with poor ventilation. High concentrations of CO2 can cause symptoms such as headaches, dizziness, and shortness of breath. In extreme cases, exposure to high levels of CO2 can lead to unconsciousness and even death.
During and after an earthquake, secondary effects can potentially lead to the release of carbon monoxide (CO). For example, if there is damage to gas lines or heating systems, CO can be released. Appliances linked to CO poisoning in disasters are furnaces, boilers, gas stoves, water heaters, portable generators, automobiles, vans and trucks, portable heaters, chainsaws, pressure washers, and petroleum or diesel-powered tools. Taking CO safety seriously is crucial, and ensuring appropriate precautions are in place. Fuel-burning equipment should be checked regularly to minimize the risk of CO leakage. On the other hand, survivors may use enclosed spaces and vehicles for shelter in cold conditions, especially during the winter. Such areas with insufficient ventilation can lead to the accumulation of CO, which can cause CO poisoning.28-31
Respiratory Infections
Bacterial, Viral and Fungal Infections
Victims of earthquakes, volunteers involved in rescue operations, and survivors are exposed to microbiological threats during and after the earthquake. Following the 1999 Marmara earthquake in Turkey, Keven et al32 examined the clinical and laboratory results of 639 patients admitted to 35 hospitals and reported infections in 223 patients. Sepsis was found in more than half of these patients, while wound infections were observed in half of the remaining patients and lung infections in the other half. Furthermore, the analysis revealed that most of these infections were caused by gram-negative aerobic bacteria and Staphylococcus spp.
Wang et al33 conducted a bacteriological evaluation on patients with crush syndrome admitted to Sichuan University, West China Hospital after the Wenchuan earthquake and identified 210 different bacterial isolates from 42 out of 66 earthquake victims. Most of these isolates were gram-negative bacilli, followed by gram-positive bacteria and fungi. The main isolates obtained from the wounds were Acinetobacter baumannii and Pseudomonas aeruginosa.
In another study published in 2012, pathogenic bacteria were investigated in 91 patients rescued alive from under the rubble during the same earthquake. In 43.3% of the patients, infections were detected in the wound areas, and in 37.1%, infections were detected in the airways. The report stated that 62 patients had gram-negative bacilli, 23 had gram-positive rods, 9 had fungi, and 3 had Clostridium perfringens, an anaerobic bacterium. Additionally, these patients had different isolates from the microbiological isolates obtained from non-earthquake trauma patients in the hospital. The most frequently observed pathogenic isolates were Escherichia coli, Acinetobacter baumannii, Staphylococcus aureus, Burkholderia cepacia, and Enterococcus sp.34
Furthermore, Zhang et al35 demonstrated that wound infection, lung infection, and sepsis were common complications in 112 out of 147 crush syndrome patients admitted to the hospital due to infection after the Wenchuan earthquake (75.7% of the patients). Mainly, lung infections were observed in 24 patients, and sputum examinations showed that the bacterial isolates responsible for lung infection were A. baumannii (11/24), Klebsiella pneumonia (5/24), S. aureus (4/24), E. coli (2/24), and P. aeruginosa (2/24).
Another microbial threat from earthquakes is the contamination of water sources with bacteria, viruses, fungi, and parasites due to damage to water distribution systems and sanitation units or direct earthquake-induced soil liquefaction and tsunamis.36,37 These contaminations can lead to various waterborne diseases and respiratory infections. Moreover, this risk is particularly high for survivors pulled from the debris, those involved in rescue operations, and people living in tent cities, making it an issue that requires careful attention. Inadequate sanitation and improper waste disposal can contribute to the spread of infectious microorganisms.38 Urgent measures such as water quality assessment, sanitation promotion, and emergency medical services are necessary to mitigate the impact of these hazards on lung health.
Earthquakes often result in population displacement, with people seeking temporary shelter in crowded spaces such as evacuation centers or makeshift camps. These crowded living conditions can facilitate the spread of viral respiratory infections, particularly those transmitted through respiratory droplets. Earthquakes and their subsequent aftermath can lead to increased stress levels that could lead to post-traumatic stress disorder syndrome among individuals. Stress has been associated with immune system dysfunction, potentially making individuals more susceptible to viral respiratory infections and worsening outcomes.9
The study conducted by Kun et al39 highlights an essential point regarding the increased risk of acute respiratory infections among rescuers and healthcare workers in the aftermath of earthquakes. The study focused on rescue teams living in shelters in Beichuan after the 2008 China earthquake and found that acute upper respiratory tract infections were the most common disease reported among these individuals, accounting for 13.2% of cases.
Following seismic events, compromised and damp structures can create favorable conditions for the proliferation and dissemination of molds, fungi, and organic PM. Water infiltration into buildings also provides an optimal environment for these microorganisms’ growth; when their spores become airborne, they can lead to respiratory pathologies, including allergies. Additionally, inhalation of high concentrations of organic dust derived from soil, debris, and decaying organic matter poses respiratory risks.
In the aftermath of the 1994 Northridge earthquake in Ventura County, California, a significant outbreak of coccidioidomycosis, a respiratory disease caused by inhaling airborne spores of the dimorphic fungus Coccidiodes immitis, wasexperienced. This fungus primarily grows in the upper layers of grand soil, around 10-30 cm below the surface, in limited semi-arid regions of the western hemisphere, including the southwestern United States, Mexico, and parts of Central and South America. Approximately 60% of infected individuals remain asymptomatic, while others may exhibit symptoms resembling influenza-like respiratory illness or other clinical manifestations.40
The Santa Susana Mountains, located north of Simi Valley, California, experienced landslides triggered by the earthquake and its strong aftershocks. These landslides generated dust clouds dispersed into nearby valleys by north-easterly winds. Consequently, the number of coccidioidomycosis cases in the region dramatically increased 2 weeks after the earthquake. Out of the 203 identified cases, 56% occurred in Simi Valley. Individuals physically present in the dust clouds were 3 times more likely to be diagnosed with acute coccidioidomycosis than those not exposed. The risk of acute coccidioidomycosis diagnosis increased with a longer duration of exposure and a prolonged stay within the dust clouds.41 These reports strongly suggest that the outbreak of coccidioidomycosis in Ventura County was linked to the dissemination of C. immitis arthrospores through dust clouds caused by the landslides triggered by the 1994 Northridge earthquake.
The geographical distribution of respiratory tract infection agents can vary due to a variety of factors, including climate, population density, healthcare infrastructure, and cultural practices. Establishing a robust disease surveillance system is crucial for early detection and effective management of infectious diseases after disasters.5
Conducting prompt assessments and developing remediation and prevention strategies to address these hazards and protect lung health is important. Moreover, it should be noted that no studies have been published regarding cases of coccidioidomycosis or other respiratory fungal infections following earthquakes in Turkey. However, it is plausible to expect that in the aftermath of earthquakes, damaged buildings, debris areas, and moistened rubble provide favorable conditions for mold and fungal growth and dissemination. To mitigate these risks and safeguard lung health, regular and rapid evaluation of disease-causing microorganisms, as well as the implementation of effective cleaning and prevention strategies, is essential.
Tuberculosis
The relationship between earthquakes and tuberculosis (TB) primarily revolves around the potential impact of earthquakes on TB control programs and the living conditions that can facilitate the transmission of TB. Earthquakes can cause damage to healthcare infrastructure, disrupt healthcare services, and lead to the displacement of populations. This can hamper the diagnosis, treatment, and follow-up of individuals with TB and interrupt the supply of medications.
Following an earthquake, displaced populations may be forced to live in crowded temporary shelters or communal areas. Overcrowding and poor ventilation can increase the risk of TB transmission among individuals, particularly in settings with a high TB burden. Earthquakes often result in economic hardships and social disruptions. Poverty and a lack of access to healthcare services can contribute to delays in TB diagnosis and treatment, leading to increased transmission and poorer treatment outcomes.5
The psychological stress caused by earthquakes can weaken individuals’ immune systems and make them more susceptible to TB infection. Stress and trauma can also contribute to the reactivation of latent TB infections.42
In a study assessing the risk of TB after earthquakes, 5746 children in earthquake-affected areas were tested for Mycobacterium tuberculosis in the 2013 Bohol earthquake in the Philippines. Of these, 355 tested positive for the tuberculin skin test, indicating latent TB, and 16 were found to have active TB.43 Tuberculosis incidence increased in individuals in the earthquake-affected region after the 2010 Haiti earthquake.44 Similarly, an increase in TB cases was found during the 2008 Wenchuan earthquake compared to the same period in the previous year.
Balbay et al45 investigated the effects of 2 consecutive earthquakes on TB patients’ sociodemographic and disease-related characteristics in Düzce, a rural area in northwest Turkey. Although the study did not specifically focus on factors influencing patient adherence to TB therapy, no major changes were observed in the socioeconomic parameters that could impact the outcome of TB. In the pre-earthquake period, patients were frequently hospitalized, while in the peri- and post-earthquake periods, patients received ambulatory care. In the peri-earthquake period, patients were significantly monitored every month. Furthermore, patients were mainly followed by the same doctor in the post-earthquake period. Their findings suggested that the earthquakes had a minimal impact on TB incidence and control during and after the earthquakes in Düzce. Another study from Turkey aimed to investigate the adherence to TB treatment. Although the adherence rate for patients who initiated anti-TB therapy before the earthquake tended to be higher than that for those who initiated treatment immediately after the earthquake, this was not significant.46
It is important to note that the relationship between earthquakes and TB is complex, and the specific impact may vary depending on the magnitude of the earthquake, the local TB epidemiology, and the existing healthcare infrastructure. Efforts to mitigate the impact of earthquakes on TB control may include maintaining and strengthening healthcare services, ensuring access to medications, implementing infection control measures in crowded settings, and conducting active case-finding activities in post-disaster situations.
Chest Traumas
Trauma is a significant cause of morbidity and mortality in earthquake situations, and it is often the primary reason for hospital admissions in the immediate aftermath of an earthquake, particularly within the first 24 hours.12 Bulut et al47 conducted a retrospective analysis of the medical records of 645 earthquake victims in Türkiye following the 1999 Marmara earthquake. Most patients (77%) were hospitalized within the first 3 days after the earthquake, and approximately 10% of the individuals who sought medical attention at the hospital during the earthquake had chest traumas. Chest traumas can occur in earthquake situations for various reasons, including collapsing buildings or constructions, falling debris, or being struck by objects.48 The forceful compression or impaction on the chest during an earthquake can lead to rib fractures, which can cause significant pain, difficulty breathing, and an increased risk of lung injury. Pneumothorax may be caused by rib fractures or other trauma to the chest during an earthquake. Crushing injuries to the chest may occur when individuals are trapped under collapsed structures. These injuries can cause severe damage to the chest wall and internal organs and may result in various complications, including respiratory distress.49,50 It is important to note that the severity and prevalence of these chest injuries can vary depending on the earthquake's magnitude, the proximity to the epicenter, and the level of destruction.
The initial hours after an earthquake pose significant challenges for emergency medical services and hospitals, as they must rapidly assess, triage, and treat many trauma patients. The severity of injuries and the immediate need for medical intervention often determine the priorities in such situations. Prompt and effective management of trauma victims, i.e., timely triage, stabilization, and surgical interventions, can substantially reduce morbidity and mortality rates.47
In the 1999 Marmara earthquake, Toker et al51 evaluated 19 patients with chest trauma, and pneumothorax was observed in 37% of the patients. Rib fractures, hemothorax, and hemopneumothorax were present in 26% and 11% of the patients, respectively. Diaphragmatic tears, subcutaneous emphysema, and cervical tracheal damage were observed in 11%, 11%, and 5% of the injuries, respectively. In their study on hospitalized patients in the Düzce and İzmit earthquakes, Ozdoğan et al48 found that pneumothorax was the most frequent pathology, accounting for 50% of the injuries, and rib fractures were the second most common finding, accounting for 33.3% of the injuries. These findings provide valuable insights into the types and frequencies of chest trauma observed in earthquake situations, and pneumothorax and rib fractures appear to be the most common injuries in such conditions.
Healthcare systems and emergency responders must be well-prepared and equipped to handle the surge in trauma cases following an earthquake. This includes having sufficient medical personnel, supplies, and facilities in place and establishing effective communication and coordination systems to ensure a timely and organized response.
Exacerbation of Respiratory Diseases
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) patients can experience exacerbations or worsening of symptoms during and after an earthquake. The environmental conditions and interruptions associated with earthquakes can lead to COPD exacerbations. The damage and collapse of buildings can lead to the release of dust and other airborne particles. These particles can irritate the airways of individuals and induce symptoms such as coughing, wheezing, and shortness of breath.52 The sudden and unexpected nature of earthquakes can also induce stress and anxiety, worsening COPD symptoms and leading to increased breathing difficulties and exacerbating respiratory symptoms.53 Earthquakes can disrupt infrastructure, including power outages, damage to air filtration systems, or contamination of water sources. These factors can deteriorate indoor and outdoor air quality, adversely affecting COPD patients.52
Ma et al54 investigated the major risk factors for acute exacerbations of COPD in patients who survived the Wenchuan earthquake in Sichuan, China. The study utilized a questionnaire survey conducted at multiple time points (1 month, 3 months, and 12 months) after the earthquake. The study included 301 COPD patients from both earthquake-affected and non-earthquake areas. Patients from the earthquake zone had a significantly higher incidence of acute exacerbations of COPD compared to those from the non-earthquake zone at 3 months and 12 months following the earthquake. Furthermore, patients from the earthquake area had a significantly higher prevalence of post-traumatic stress disorder (PTSD) and higher scores on the Self-Rating Anxiety Scale and Self-Rating Depression Scale within 1 month and 3 months after the earthquake. The difference in PTSD prevalence remained significant even 12 months after the earthquake. The identified risk factors, including older age, worse pulmonary functions, psychological disorders, and poor living environment, were associated with an increased risk of acute exacerbations of COPD. The study suggested that COPD patients should receive psychotherapy and better living arrangements as early as possible after such severe disasters to minimize the risk of exacerbations.
A retrospective cohort analysis from Ishinomaki, a region severely affected by the Great East Japan Earthquake in 2011, investigated the impact of the disaster on patients with COPD. The findings of the study revealed several important observations. Firstly, in the immediate aftermath of the disaster, patients who required oxygen therapy at home visited the hospital to receive oxygen. This suggests that the disruption caused by the earthquake led to a lack of access to essential medical equipment and supplies necessary for managing COPD at home. Furthermore, during the subacute phase, which encompassed the third to fifth weeks after the earthquake, there was a significant increase in the number of hospitalizations due to COPD exacerbations compared to the prior period. This suggests that the disaster had a detrimental effect on the respiratory health of COPD patients, potentially due to various factors such as increased stress, exposure to environmental hazards, or limited access to medical care. The incidence of exacerbated COPD cases returned to normal levels 6 weeks after the earthquake, suggesting that although the disaster initially had a significant negative impact on COPD patients, the situation gradually improved over time, possibly due to the restoration of healthcare services and the overall recovery efforts in the region.55
Asthma
Dust particles resulting from the crashed buildings and debris may irritate the airways of individuals with asthma, triggering symptoms such as coughing, wheezing, and shortness of breath.56
The sudden and unexpected nature of earthquakes can also induce stress and anxiety, which are known to be potential triggers for asthma symptoms. Emotional stress can lead to increased sensitivity of the airways and bronchoconstriction, making asthma symptoms more likely to occur.57 Earthquakes may disrupt access to essential medications or medical care, making it challenging for asthma patients to manage their condition effectively. Inadequate access to rescue inhalers or maintenance medications can increase the risk of an asthma attack.
Tomita et al56 conducted a retrospective cohort involving 156 asthmatic outpatients of Tottori University Hospital, aged 18-89. They documented the asthmatic symptoms and monitored patients' peak expiratory flow (PEF) rates for more than 1 year before the Tottori-Ken Seibu earthquake and 1 year after the earthquake. Among the study participants, 17 patients (11%) experienced an exacerbation of asthma within 1 month after the earthquake. The researchers compared the diurnal variability of PEF during the month following the earthquake to values recorded during a matched month 1 year prior to the earthquake. They also reviewed the medical case noted to identify factors associated with the exacerbation and used the multivariate analysis to determine the contribution of these factors. The results indicated that airflow limitation was independently associated with asthma exacerbations after the earthquake.
Furthermore, acute asthma attacks were more likely to occur within the first week following the earthquake, even without diurnal PEF variability. The study highlights the importance of identifying individuals with asthma who have the risk of exacerbations after earthquakes. Factors such as preexisting airflow limitations may increase susceptibility to exacerbations. The early post-earthquake period, particularly the first week, appears to be critical for monitoring and managing asthma symptoms in at-risk individuals.56
Following the major earthquake in Eastern Japan (March 11, 2011), the indoor fungal contamination in prefabricated temporary housing, private residences, and rental apartments during the winter season and rainy days was significantly higher than the recommended indoor fungal contamination level of 1000 colony-forming units (cfu)/m3. The contaminant identified was Aspergillus, a known allergenic species.58,59 In February 2012, a 66-year-old male ex-smoker diagnosed with bronchial asthma since the age of 5 presented to the hospital with symptoms of chest tightness, coughing, and wheezing following the earthquake. A skin prick test on the patient revealed a positive reaction to the reproductive stage form of Aspergillus glaucus, known as Eurotium herbarium (E. herbarium). Air sampling from the patient's home revealed a significantly high count of E. herbarium at 163 200 colony-forming units per cubic meter (CFU/m3). Further clinical evaluations confirmed the patient’s diagnosis of bronchial asthma.60
Individuals with asthma must consult their healthcare provider for personalized guidance on managing asthma during earthquakes.
Asbestos-Related Lung Diseases
Among other particles that affect the respiratory system following earthquakes are asbestos fibers. Asbestos is a well-established carcinogen known to cause pulmonary fibrosis (asbestosis), lung cancer, and mesothelioma. The International Agency for Research on Cancer has classified asbestos as a group 1 carcinogen, indicating that there is sufficient evidence to support its carcinogenicity in humans. Also, studies have demonstrated a causal relationship between asbestos exposure and various cancers, including larynx carcinoma, nasopharynx carcinoma, gastrointestinal system cancers, and ovarian cancers.61
The extensive collapse of buildings during earthquakes is believed to disperse asbestos fibers into the air, thereby exposing rescue workers and disaster victims to inhalation risks. The adverse health effects of asbestos fibers have been observed in low-dose ambient exposure and high-dose occupational exposure cases. Asbestos has been strictly prohibited since 2006 in Japan and 2010 in Turkey. However, major natural disasters like earthquakes and tsunamis can lead to the release of asbestos due to damage to numerous buildings and homes constructed before the implementation of the asbestos ban. In Turkey, it was reported that 1.2 million tons of asbestos were used as a construction material between 1900 and 2003, before the ban.62-64
Van Orden et al65 analyzed the air samples from buildings following the 1989 earthquake in central coastal California. Their results showed that, in general, asbestos levels in the sampled buildings did not significantly differ from outdoor levels, even immediately after the earthquake. However, there were exceptions to this finding, and samples collected near debris clean-up areas and in buildings undergoing asbestos abatement showed slightly higher concentrations than indoor and outdoor samples. These findings suggest that while there were some localized areas with higher asbestos levels due to debris clean-up and ongoing abatement, the overall risk of asbestos exposure in the sampled buildings was relatively low and within regulatory limits.
Following 2 major earthquakes that occurred on February 6 in Southeastern Turkey, there is an ongoing potential risk of asbestos dissemination in areas characterized by extensive pre-2010 construction. Therefore, it is crucial to analyze ambient PM and surrounding debris from buildings for the presence of asbestos and to compile reports addressing the consequences of such exposure in earthquake-prone areas. Additionally, taking precautions to minimize asbestos exposure during demolition activities is paramount. It is essential to inform and educate the public, including residents and workers in affected areas, about the risks of asbestos exposure and the proper precautions to take during post-earthquake activities. Also, the implementation of a specific surveillance program focusing on the incidence of cancer among people exposed to asbestos or workers engaged in post-earthquake activities in earthquake-affected areas is of great importance.
Venous Thromboembolism
There is no direct relationship between earthquakes and venous thromboembolism (VTE). However, it is important to note that in the aftermath of a major earthquake, secondary effects may be indirectly contributing to an increased risk of VTE. In areas affected by earthquakes, medical infrastructure may be damaged or overwhelmed, leading to delays in accessing appropriate medical care. This delay in treatment or lack of access to anticoagulant medications could potentially increase the risk of VTE in individuals who are already susceptible. Earthquakes can cause structural damage, requiring individuals to remain confined to shelters or temporary accommodations for extended periods. Prolonged immobility can be a risk factor for VTE, especially if people cannot move around.66
Earthquakes can cause injuries that require immobilization, such as fractures or crush injuries. Immobilization of a limb due to trauma can increase the risk of developing blood clots in the veins of the affected limb.67 Sakuma et al68 investigated the occurrence of acute pulmonary embolism (APE) following the 2004 Mid-Niigata Prefecture earthquake in Japan and assessed the associated risk factors. The study found a higher relative risk of APE in the high evacuee rate area compared to the low evacuee rate area. Additionally, the risk of APE was higher in women. All patients in the high evacuee rate area had stayed in their automobiles for long periods, whereas none of the patients in the low evacuee rate area had done so. This suggests a potential link between prolonged immobilization in automobiles and the occurrence of APE. Staying in automobiles for extended periods was identified as a potential risk factor for APE in the high evacuee rate area. Also, Watanabe et al69 investigated the impact of the earthquake in Niigata, Japan, on the occurrence of pulmonary embolism (PE) and sudden death. The researchers observed an increase in PE cases following the earthquake compared to pre-earthquake periods and previous years. The first case of PE occurred 2 days after the initial earthquake, and new cases continued to be reported for 27 days after that. Six out of the 9 patients (67%) with PE had taken refuge in their automobiles before experiencing symptoms, suggesting a potential association between prolonged immobilization in automobiles and the risk of PE. The study also observed an increase in sudden death cases after the earthquake. Of the 22 cases, 7 (32%) had spent 1 or more nights in automobiles. Based on these findings, the study suggests that PE should be considered and attended to after disasters. It also highlights the potential risk of prolonged immobilization in automobiles as a contributing factor to the increased occurrence of PE and sudden death following earthquakes.
Maintaining mobility, staying hydrated, and seeking medical attention are crucial steps to reduce the risk of VTE, especially in situations where movement might be restricted due to the aftermath of an earthquake. In addition to these measures, individuals in earthquake-affected areas should also be mindful of other risk factors that might exacerbate the risk of VTE, such as preexisting medical conditions, certain medications, and genetic predisposition. Following medical advice and guidance is paramount, as healthcare professionals can provide tailored recommendations based on individual health status and the specific circumstances of the earthquake aftermath. Emergency response and medical personnel play a critical role in providing appropriate care and support to those in earthquake-affected areas.
Conclusion
Earthquakes cause various environmental and occupational exposures that can significantly impact lung health. Understanding and addressing the risks associated with PM, asbestos, mineral fibers, metallic particles, molds, fungi, organic dust, and microbiological hazards are crucial for protecting individuals and implementing effective mitigation strategies. By prioritizing appropriate measures and ensuring proper handling and protective measures, the adverse effects of earthquakes on lung health can be minimized, and this can also facilitate a healthier recovery. Training healthcare professionals in disaster management and implementing disaster response plans can further enhance the readiness and effectiveness of healthcare systems in managing earthquake-related trauma.
Measuring occupational and environmental exposure levels to factors such as dust, particulates, toxic gases, and hazardous chemicals requires a combination of technical methods and strategic planning. Monitoring changes in these exposure levels over time involves a systematic approach to data collection, analysis, and interpretation.
It is clear that robust building infrastructure and effective earthquake preparedness play a pivotal role in minimizing the cascading effects of earthquakes, including their impact on respiratory health. By focusing on constructing resilient buildings and bolstering preparedness efforts, communities can not only mitigate building collapses but also significantly reduce the potential health consequences that follow. Such measures should be seen as integral parts of overall disaster management strategies.
As a result, this comprehensive review underscores the urgent need for further research into the specific pollutants, air contaminants, and environmental factors that contribute to respiratory health issues following earthquakes. Identifying these factors will enable more targeted interventions and policies that can safeguard respiratory health during and after seismic events. Furthermore, collaboration among interdisciplinary teams, including public health professionals, geologists, engineers, and policymakers, is crucial to developing holistic approaches that account for both immediate- and long-term health impacts.
Future Research
Although the existing literature suggests an association between earthquakes and increased threats to respiratory health, gaps and unmet needs still require further investigation. To address these gaps, future research should concentrate on the following areas.
Identifying Specific Pollutants and Environmental Factors
Earthquakes can release various pollutants into the air, such as PM, gases, and toxic substances. Determining the specific pollutants, toxicants, and irritants responsible for the respiratory health impacts observed during and after earthquakes is important. This knowledge can help in developing targeted mitigation strategies and interventions.
Assessing Exposure Levels and Patterns
Understanding the exposure levels and patterns of affected populations is crucial for evaluating respiratory health impacts and implementing effective protective measures. Future research should focus on assessing the duration, frequency, and intensity of exposure to various pollutants and environmental factors resulting from earthquakes. This information can also provide insights into the potential mechanisms through which earthquakes affect respiratory health.
Longitudinal Studies for Long-Term Impacts
While the immediate respiratory health effects of earthquakes are well documented, there is a need for more longitudinal studies to assess the middle- and long-term impacts. These studies should follow the cohorts and individuals over an extended period, allowing researchers to investigate the persistence or development of respiratory conditions such as asthma, pulmonary fibrosis, COPD, malign mesothelioma, and other respiratory diseases associated with earthquakes.
Vulnerable Populations and Susceptibility Factors
Research should focus on identifying vulnerable populations and factors that increase susceptibility to the respiratory health impacts of earthquakes. Factors such as age, preexisting respiratory conditions, socioeconomic status, and access to healthcare can influence the severity and duration of respiratory pathologies. Understanding these factors can help target interventions and support services for those most in need.
Mitigation Strategies and Preparedness
Future research should also explore effective mitigation strategies and preparedness measures to reduce the respiratory health impacts of earthquakes. This could involve studying the effectiveness of engineering solutions, building codes, urban planning approaches, and early warning systems in minimizing exposure to harmful pollutants and improving respiratory health outcomes.
By addressing these research areas, we can enhance our understanding of the relationship between earthquakes and respiratory health and develop evidence-based strategies to mitigate the impacts on affected populations.
Funding Statement
This study received no funding.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – E.G.B., Ö.K., Ö.B., Ö.D., P.A., H.B.; Design – E.G.B., Ö.K., Ö.B., H.B; Supervision – H.B., P.A., Ö.D., Ö.B.; Resources – E.G.B., Ö.K., Ö.B., Ö.D, P.A., H.B.; Materials – E.G.B., Ö.K., Ö.B., Ö.D., P.A., H.B.; Data Collection and/or Processing E.G.B., Ö.K., Ö.B., Ö.D., P.A., H.B.; Analysis and/or Interpretation – E.G.B, Ö.K., Ö.B., Ö.D., P.A., H.B.; Literature Search – E.G.B., Ö.K., Ö.B., Ö.D., P.A., H.B.; Writing – E.G.B, Ö.K, Ö.B., Ö.D., P.A., H.B.; Critical Review – E.G.B., Ö.K., Ö.B., Ö.D., P.A., H.B.
Declaration of Interests: The authors have no conflict of interest to declare.
References
- 1. El Saghir NS, Soto Pérez de Celis E, Fares JE, Sullivan R. Cancer care for refugees and displaced populations: Middle East conflicts and global natural disasters. Am Soc Clin Oncol Educ Book. 2018;38:433 440. ( 10.1200/EDBK_201365) [DOI] [PubMed] [Google Scholar]
- 2. Ersoy Ş, Koçak A. Disasters and earthquake preparedness of children and schools in Istanbul, Turkey. Geom Nat Hazards Risk. 2016;7(4):1307 1336. ( 10.1080/19475705.2015.1060637) [DOI] [Google Scholar]
- 3. Vikulin AV, Akmanova DR, Vikulina SA, Dolgaya AA. Migration of seismic and volcanic activity as a display of wave geodynamic process. Geodyn Tectonophys. 2012;3(1):1 18. ( 10.5800/GT-2012-3-1-0058) [DOI] [Google Scholar]
- 4. Sucuoğlu H, Akkar S. Nature of earthquakes. Basic Earthquake Eng Seismol Anal Des. 2014:1 39. [Google Scholar]
- 5. Mavrouli M, Mavroulis S, Lekkas E, Tsakris A. The impact of earthquakes on public health: A narrative review of infectious diseases in the post-disaster period aiming at disaster risk reduction. Microorganisms. 2023;11(2):419. ( 10.3390/microorganisms11020419) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ramírez-Rojas A, Sigalotti LG, Márquez ELF, Rendón O. Tsallis theory. In: Non-extensive statistcs in time series. Time Series Analysis in Seismology: Practical Applications. Ramírez-Rojas A, Sigalotti LG, Márquez ELF, Rendón O, eds. Amsterdam, The Netherlands: Elsevier; 2019:147 164. [Google Scholar]
- 7. United States Geological Survey (USGS). Common myths about earthquakes. Available at: https://www.usgs.gov/programs/earthquake-hazards/myths-and-misconceptions-about-induced-earthquakes. Accessed June 5, 2023. [Google Scholar]
- 8. Bayram H, Rastgeldi Dogan TR, Şahin ÜA, Akdis CA. Environmental and health hazards by massive earthquakes. Allergy. 2023. 7;78(8):2081 2084. ( 10.1111/all.15736) [DOI] [PubMed] [Google Scholar]
- 9. Robinson B, Alatas MF, Robertson A, Steer H. Natural disasters and the lung. Respirology. 2011;16(3):386 395. ( 10.1111/j.1440-1843.2011.01923.x) [DOI] [PubMed] [Google Scholar]
- 10. Bartels SA, VanRooyen MJ. Medical complications associated with earthquakes. Lancet. 2012;379(9817):748 757. ( 10.1016/S0140-6736(11)60887-8) [DOI] [PubMed] [Google Scholar]
- 11. Balbay EG. Inhalation damage in flood and earthquake. In: Control and Treatment of Acute Occupational and Environmental Inhalation Injuries. Akgün M, Akkurt İ, Arbak P, eds. 11th ed. Istanbul, Türkiye: Logos Publishing; 2019:119 126. [Google Scholar]
- 12. Güleç Balbay E. Earthquake and the lung. Duzce Med J. 2023;25(1):1 5. ( 10.18678/dtfd.1256261) [DOI] [Google Scholar]
- 13. Bell ML, Dominici F, Ebisu K, Zeger SL, Samet JM. Spatial and temporal variation in PM2.5 chemical composition in the United States for health effects studies. Environ Health Perspect. 2007;115(7):989 995. ( 10.1289/ehp.9621) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hisata S, Moriyama H, Tazawa R, Ohkouchi S, Ichinose M, Ebina M. Development of pulmonary alveolar proteinosis following exposure to dust after the Great East Japan Earthquake. Respir Investig. 2013;51(4):212 216. ( 10.1016/j.resinv.2013.04.005) [DOI] [PubMed] [Google Scholar]
- 15. Fang GC, Chang CN, Wu YS, et al. Concentration of atmospheric particulates during a dust storm period in central Taiwan, Taichung. Sci Total Environ. 2002;287(1-2):141 145. ( 10.1016/S0048-9697(01)00996-2) [DOI] [PubMed] [Google Scholar]
- 16. Pearson AL, Kingham S, Mitchell P, Apparicio P. Exploring hotspots of pneumococcal pneumonia and potential impact of ejecta dust exposure following the Christchurch earthquakes. Spat Spatio-Temporal Epidemiol. 2013;7:1 9. ( 10.1016/j.sste.2013.08.001) [DOI] [PubMed] [Google Scholar]
- 17. Gotoh T, Nishimura T, Nakata M, Nakaguchi Y, Hiraki K. Air pollution by concrete dust from the Great Hanshin Earthquake. J Environ Qual. 2002;31(3):718 723. ( 10.2134/jeq2002.7180) [DOI] [PubMed] [Google Scholar]
- 18. Yamamoto R, Nagai N, Koizumi N, Ninomiya R. Dust concentration around the sites of demolition work after the Great Hanshin-Awaji Earthquake. Environ Health Prev Med. 1999;3(4):207 214. ( 10.1007/BF02932260) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. World Health Organization (WHO). Great East Japan earthquake 2011. Available at: https://www.who.int/westernpacific/emergencies/great-east-japan-earthquake. Accessed May 5, 2023. [Google Scholar]
- 20. Mastrantonio R, Civisca A, Siciliano E, et al. Exposure assessment to inhalable and respirable dust in the post-earthquake construction sites in the city of l’aquila. J Occup Health. 2021;63(1):e12296. ( 10.1002/1348-9585.12296) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akbulut G, Yilmaz S, Polat C, Sözen M, Leblebicioğlu M, Dilek ON. Afyon sultandagi earthquake. Ulus Travma Acil Cerrahi Derg. 2003;9(3):189 193. [PubMed] [Google Scholar]
- 22. Cicerone RD, Ebel JE, Britton J. A systematic compilation of earthquake precursors. Tectonophysics. 2009;476(3-4):371 396. ( 10.1016/j.tecto.2009.06.008) [DOI] [Google Scholar]
- 23. D’Incecco S, Petraki E, Priniotakis G, Papoutsidakis M, Yannakopoulos P, Nikolopoulos D. CO2 and radon emissions as precursors of seismic activity. Earth Syst Environ. 2021;5(3):655 666. ( 10.1007/s41748-021-00229-2) [DOI] [Google Scholar]
- 24. Freund F. Pre-earthquake signals Underlying physical processes. J Asian Earth Sci. 2011;41(4-5):383 400. ( 10.1016/j.jseaes.2010.03.009) [DOI] [Google Scholar]
- 25. Frondini F, Chiodini G, Caliro S, Cardellini C, Granieri D, Ventura G. Diffuse CO2 degassing at Vesuvio, Italy. Bull Volcanol. 2004;66(7):642 651. ( 10.1007/s00445-004-0346-x) [DOI] [Google Scholar]
- 26. Bowie C, Bowie SH. Radon and health. Lancet. 1991;337(8738):409 413. ( 10.1016/0140-6736(91)91177-v) [DOI] [PubMed] [Google Scholar]
- 27. Ruano-Ravina A, Pereyra MF, Castro MT, Pérez-Ríos M, Abal-Arca J, Barros-Dios JM. Genetic susceptibility, residential radon, and lung cancer in a radon-prone area. J Thorac Oncol. 2014;9(8):1073 1080. ( 10.1097/JTO.0000000000000205) [DOI] [PubMed] [Google Scholar]
- 28. Waite T, Murray V, Baker D. Carbon monoxide poisoning and flooding: changes in risk before, during and after flooding require appropriate public health interventions. PLoS Curr. 2014:;6:ecurrents.dis.2b2eb9e15f9b982784938803584487f1. ( 10.1371/currents.dis.2b2eb9e15f9b982784938803584487f1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Singh RP, Senthil Kumar JS, Zlotnicki J, Kafatos M. Satellite detection of carbon monoxide emission prior to the Gujarat earthquake of January 26, 2001. Appl Geochem. 2010;25(4):580 585. ( 10.1016/j.apgeochem.2010.01.014) [DOI] [Google Scholar]
- 30. Fischer T, Matyska C, Heinicke J. Earthquake-enhanced permeability–evidence from carbon dioxide release following the ML 3.5 earthquake in West Bohemia. Earth Planet Sci Lett. 2017;460:60 67. ( 10.1016/j.epsl.2016.12.001) [DOI] [Google Scholar]
- 31. Famin V, Nakashima S, Boullier AM, Fujimoto K, Hirono T. Earthquakes produce carbon dioxide in crustal faults. Earth Planet Sci Lett. 2008;265(3-4):487 497. ( 10.1016/j.epsl.2007.10.041) [DOI] [Google Scholar]
- 32. Keven K, Ates K, Sever MS, et al. Infectious complications after mass disasters: the Marmara earthquake experience. Scand J Infect Dis. 2003;35(2):110 113. ( 10.1080/0036554021000027013) [DOI] [PubMed] [Google Scholar]
- 33. Wang T, Li D, Xie Y, et al. The microbiological characteristics of patients with crush syndrome after the Wenchuan earthquake. Scand J Infect Dis. 2010;42(6-7):479 483. ( 10.3109/00365541003671226) [DOI] [PubMed] [Google Scholar]
- 34. Zhang B, Liu Z, Lin Z, Zhang X, Fu W. Microbiologic characteristics of pathogenic bacteria from hospitalized trauma patients who survived Wenchuan earthquake. Eur J Clin Microbiol Infect Dis. 2012;31(10):2529 2535. ( 10.1007/s10096-012-1591-0) [DOI] [PubMed] [Google Scholar]
- 35. Zhang H, Zeng JW, Wang GL, Tu CQ, Huang FG, Pei FX. Infectious complications in patients with crush syndrome following the Wenchuan earthquake. Chin J Traumatol. 2013;16(1):10 15. [PubMed] [Google Scholar]
- 36. Chao YT, Lai SH, Chang MH, et al. A potential microbiological approach to the evaluation of earthquake-induced soil liquefaction. iScience. 2021;24(9):102984. ( 10.1016/j.isci.2021.102984) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Okumura Y, Kaneko K, Ota H, Nagasaka H, Hara M. Analysis of environmental and microbiological changes in Onagawa Bay immediately after the tsunami of the Great East Japan Earthquake based on sediment cores. Mar Pollut Bull. 2020;157:111235. ( 10.1016/j.marpolbul.2020.111235) [DOI] [PubMed] [Google Scholar]
- 38. Yang X, Liu Q, Zhang R. Epidemiology of pulmonary tuberculosis in Wenchuan earthquake-stricken area: a population-based study. J Evid Based Med. 2013;6(3):149 156. ( 10.1111/jebm.12054) [DOI] [PubMed] [Google Scholar]
- 39. Kun P, Wang Z, Chen X, et al. Public health status and influence factors after 2008 Wenchuan earthquake among survivors in Sichuan Province, China: cross-sectional trial. Public Health. 2010;124(10):573 580. ( 10.1016/j.puhe.2010.06.001) [DOI] [PubMed] [Google Scholar]
- 40. Schneider E, Hajjeh RA, Spiegel RA, et al. A coccidioidomycosis outbreak following the Northridge, Calif, earthquake. JAMA. 1997;277(11):904 908. [PubMed] [Google Scholar]
- 41. Jibson RW, Public A. Health issue related to collateral seismic hazards: the valley fever outbreak triggered by the 1994 Northridge, California earthquake. Surv Geophys. 2002;23:511528. [Google Scholar]
- 42. Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601 630. ( 10.1037/0033-2909.130.4.601) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Murray KO, Castillo-Carandang NT, Mandalakas AM, et al. Prevalence of tuberculosis in children after natural disasters, Bohol, Philippines. Emerg Infect Dis. 2019;25(10):1884 1892. ( 10.3201/eid2510.190619) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Koenig SP, Rouzier V, Vilbrun SC, et al. Tuberculosis in the aftermath of the 2010 earthquake in Haiti. Bull World Health Organ. 2015;93(7):498 502. ( 10.2471/BLT.14.145649) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Balbay O, Balbay EG, Arbak P, Annakkaya AN, Bilgin C. The effects of two sequential earthquakes on tuberculosis patients: an experience from Duzce earthquake. Healthmed. 2011;5(3):589 595. [Google Scholar]
- 46. Balbay O, Annakkaya AN, Arbak P, Bilgin C, Erbas M. Which patients are able to adhere to tuberculosis treatment? A study in a rural area in the northwest part of Turkey. Jpn J Infect Dis. 2005;58(3):152 158. [PubMed] [Google Scholar]
- 47. Bulut M, Fedakar R, Akkose S, Akgoz S, Ozguc H, Tokyay R. Medical experience of a university hospital in Turkey after the 1999 Marmara earthquake. Emerg Med J. 2005;22(7):494 498. ( 10.1136/emj.2004.016295) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ozdoğan S, Hocaoğlu A, Cağlayan B, Imamoğlu OU, Aydin D. Thorax and lung injuries arising from the two earthquakes in Turkey in 1999. Chest. 2001;120(4):1163 1166. ( 10.1378/chest.120.4.1163) [DOI] [PubMed] [Google Scholar]
- 49. Karmacharya RM, Devbhandari M, Tuladhar S, Shrestha B, Acharya P. Chest trauma requiring admission: differences in earthquake victims and other modes of injury. Kathmandu Univ Med J (KUMJ). 2018;16(63):237 239. [PubMed] [Google Scholar]
- 50. Kim M, Moore JE. Chest trauma: current recommendations for rib fractures, pneumothorax, and other injuries. Curr Anesthesiol Rep. 2020;10(1):61 68. ( 10.1007/s40140-020-00374-w) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Toker A, Isitmangil T, Erdik O, Sancakli I, Sebit S. Analysis of chest injuries sustained during the 1999 Marmara earthquake. Surg Today. 2002;32(9):769 771. ( 10.1007/s005950200147) [DOI] [PubMed] [Google Scholar]
- 52. Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front Public Health. 2020;8:14. ( 10.3389/fpubh.2020.00014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Strang S, Ekberg-Jansson A, Henoch I. Experience of anxiety among patients with severe COPD: A qualitative, in-depth interview study. Palliat Support Care. 2014;12(6):465 472. ( 10.1017/S1478951513000369) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ma CL, Xiao J, Wang K, et al. Risk factors for acute exacerbation of chronic obstructive pulmonary disease in patients who survived the Wenchuan earthquake. Sichuan Da Xue Xue Bao Yi Xue Ban. 2012;43(4):566 572. [PubMed] [Google Scholar]
- 55. Kobayashi S, Hanagama M, Yamanda S,et al. Impact of a large-scale natural disaster on patients with chronic obstructive pulmonary disease: the aftermath of the 2011 Great East Japan Earthquake. Respir Investig. 2013;51(1):17 23. ( 10.1016/j.resinv.2012.10.004) [DOI] [PubMed] [Google Scholar]
- 56. Tomita K, Hasegawa Y, Watanabe M, Sano H, Hitsuda Y, Shimizu E. The Totton-Ken Seibu earthquake and exacerbation of asthma in adults. J Med Invest. 2005;52(1-2):80 84. ( 10.2152/jmi.52.80) [DOI] [PubMed] [Google Scholar]
- 57. Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21(8):993 999. ( 10.1016/j.bbi.2007.03.009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Watanabe M, Konuma R, Kobayashi N, et al. Indoor fungal contamination in temporary housing after the East Japan great earthquake disaster. Int J Environ Res Public Health. 2021;18(6):3296. ( 10.3390/ijerph18063296) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Watanabe M. Indoor fungal contamination in different housing types after the great East Japan earthquake and flood disaster. Yakugaku Zasshi. 2022;142(1):17 25. ( 10.1248/yakushi.21-00161-2) [DOI] [PubMed] [Google Scholar]
- 60. Oshikata C, Watanabe M, Saito A, et al. Allergic Bronchopulmonary Mycosis due to Exposure to eurotium herbarium after the Great East Japan Earthquake. Prehosp Disaster Med. 2017;32(6):688 690. ( 10.1017/S1049023X17006914) [DOI] [PubMed] [Google Scholar]
- 61. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Arsenic, metals, fibres, and dusts. IARC Monogr Eval Carcinog Risks Hum. 2012;100(C):11 465. [PMC free article] [PubMed] [Google Scholar]
- 62. Virta RL. Worldwide asbestos supply and consumption trends from 1900 through 2003. 2006. Available at: https://pubs.usgs.gov/circ/2006/1298/c1298.pdf; Accessed June 05, 2023. [Google Scholar]
- 63. Bayram M, Özkan D, Hayat E, et al. Asbestos-related diseases in Turkey: caused not only by naturally occurring fibers but also by industrial exposures. Am J Respir Crit Care Med. 2019;199(5):656 659. ( 10.1164/rccm.201810-1922LE) [DOI] [PubMed] [Google Scholar]
- 64. Nakano T, Otsuki T. Environmental air pollutants and the risk of cancer. Gan To Kagaku Ryoho. 2013;40(11):1441 1445. [PubMed] [Google Scholar]
- 65. Van Orden DR, Lee RJ, Bishop KM, Kahane D, Morse R. Evaluation of ambient asbestos concentrations in buildings following the Loma Prieta earthquake. Regul Toxicol Pharmacol. 1995;21(1):117 122. ( 10.1006/rtph.1995.1016) [DOI] [PubMed] [Google Scholar]
- 66. Sahebi A, Nejati-Zarnaqi B, Vasei N, Jahangiri K. Deep vein thrombosis after earthquake: A systematic review and meta-analysis. Disaster Med Public Health Prep. 2023;17:e304. ( 10.1017/dmp.2022.268) [DOI] [PubMed] [Google Scholar]
- 67. Sato K, Sakamoto K, Hashimoto Y, et al. Risk factors and prevalence of deep vein thrombosis after the 2016 Kumamoto earthquakes. Circ J. 2019;83(6):1342 1348. ( 10.1253/circj.CJ-18-1369) [DOI] [PubMed] [Google Scholar]
- 68. Sakuma M, Nakamura M, Hanzawa K, et al. Acute pulmonary embolism after an earthquake in Japan. Semin Thromb Hemost. 2006;32(8):856 860. ( 10.1055/s-2006-955468) [DOI] [PubMed] [Google Scholar]
- 69. Watanabe H, Kodama M, Tanabe N, et al. Impact of earthquakes on risk for pulmonary embolism. Int J Cardiol. 2008;129(1):152 154. ( 10.1016/j.ijcard.2007.06.039) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a