Continuous treatment with antiepileptic drugs (AEDs) is critical for seizure prevention in patients with epilepsy (PWE). Uncontrolled seizure due to poor adherence to AEDs could affect patients' social lives, including their employment, and is known to be an important predictor of traffic accidents. 1 Although the situation differs depending on the licensing system in each country, continued medication is essential for PWE to be able to drive a car because they must be seizure‐free for a certain period of time. On the other hand, the package inserts for all AEDs in Japan require a prohibition against automobile driving while taking the medication, restricting the patient's social life. Each AED has different pharmacological properties and effects on cognitive function. 2 However, little evidence has been presented regarding the effects of AEDs on driving performance. 3
A large epidemiologic study found an increased risk of traffic accidents in PWE, but independent of AEDs. 4 Experimental studies have reported that carbamazepine (CBZ) impairs driving performance in healthy controls (HCs), 5 , 6 whereas PWE undergoing AED treatment have demonstrated driving performance comparable to that of HCs. 7 Although risk communication between physicians and patients regarding medication and automobile driving is important to prevent traffic accidents, the current evidence for its effectiveness is insufficient. Therefore, we reanalyzed our previous study of PWE 7 from the perspective of antiepileptic monotherapy with the aim of comparing driving performance between AED groups and HCs.
Thirty‐one PWE (12 men, 19 women) aged 19–60 years (mean ± standard deviation [SD], 36.4 ± 10.0 years) and 55 HCs (40 men, 15 women) aged 21–60 years (37.0 ± 9.4 years) were included in this study. All participants had a valid driver's license and drove regularly. All PWE received first‐line antiepileptic monotherapy in the Epilepsy Care Unit of Aichi Medical University and had the following prescriptions: valproate (VPA) (n = 10), CBZ (n = 12), levetiracetam (LEV) (n = 5), and lamotrigine (LMG) (n = 4). PWEs taking first‐generation antiallergic and psychotropic drugs were excluded. This study was approved by the Ethics Committee of Aichi Medical University, and written informed consent was received from all participants. Driving performance was measured using a standardized driving simulator, the details of which have been described previously. 7 , 8 , 9 The road‐tracking task measures the standard deviation of lateral position (SDLP) on a gently winding road at a constant speed of 100 km/h, which indicates weaving and was the primary outcome. The mean and SD of speed (SDSpeed) were also calculated. The car‐following task measures the coefficient of variation of the intervehicle distance from a preceding vehicle (DCV) with varying speeds, which was the exploratory outcome. The mean distance (MCarDistance) and SD (SDCarDistance) were also calculated. We used an independent‐samples t‐test to compare variables in each AED group and HCs in SPSS (version 27; IBM SPSS Japan). Due to the small sample size, the distributions in each AED group and HCs were also compared in dot plots.
No significant difference in age was found between PWE and HCs, but a sex difference was observed (P = 0.785 and P = 0.003, respectively). The clinical data for each AED group are shown in Table S1, and the results of driving performance in Table S2. The SDLPs of each AED group and HCs were not significantly different, with overlapping distributions (Figure 1). SDSpeed was significantly lower in all AED groups (P ≤ 0.005). The DCVs of each AED group and HCs were also not significantly different, with overlapping distributions. MCarDistance was significantly greater in the CBZ and LEV groups (P = 0.042 and P = 0.018, respectively), and SDCarDistance was significantly greater in the CBZ group (P = 0.042). The driving performances of the epilepsy types and HCs were also not significantly different (Table S3).
Figure 1.
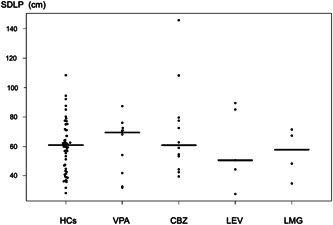
Dot plot of road‐tracking performance in each AED group and HCs. The distributions of SDLP in the AED groups and HCs generally overlapped. Horizontal lines represent the median of SDLP in each AED group and HCs. Abbreviations: SDLP, standard deviation of lateral position; AED, antiepileptic drug; HCs, healthy controls; VPA, valproate; CBZ, carbamazepine: LEV, levetiracetam; LMG, lamotrigine.
These findings demonstrate that PWE undergoing VPA, CBZ, LEV, or LMG monotherapy do not significantly differ from HCs with respect to driving performance. The smaller SDSpeed value indicates a more stable driving speed compared with HCs. The greater MCarDistance and SDCarDistance values, which could be affected by individual differences, may suggest failure to follow the indicated distance, or may mean safer driving behavior that maintains sufficient intervehicle distance. These safety‐oriented driving attitudes were also confirmed in our previous study. 7 The discrepancy between the present and previous 5 , 6 findings in CBZ may be explained by the participants, dosage, and duration of drug administration. Thus, long‐term administration of CBZ might not have a detrimental effect on driving performance in PWE.
This study had several limitations in addition to the small sample size, including the limited AEDs and the lack of sex‐matching and randomization. Future studies are needed to evaluate the effects of various AEDs on driving performance in HCs and PWE.
AUTHOR CONTRIBUTIONS
M.S. and K.K. developed the study concept. All authors contributed to the accumulation of the data. All authors contributed to the analysis and interpretation of the data. K.I. and M.S. wrote the first draft of the manuscript. E.M. and K.K. made critical revisions to the manuscript. All authors contributed to and have approved the final manuscript for submission.
FUNDING
This work was supported by Research on Regulatory Science of Pharmaceuticals and Medical Devices from the Japan Agency for Medical Research and Development (JP21mk0101137h0003 and JP22mk0101227h0001).
CONFLICT OF INTEREST STATEMENT
K.I. has received speakers' honoraria from Eisai, Kyowa, Meiji Seika Pharma, MSD, Otsuka, Sumitomo Pharma, Taisho, Takeda, Towa, and Viatris, outside the submitted work. M.S. and E.M. have no conflicts of interest to declare. K.K. has received speakers' fees from Eisai, Daiichi‐Sankyo, and UCB.
ETHICS APPROVAL STATEMENT
This study was approved by the Ethics Committee of Aichi Medical University. This study was conducted in accordance with the Declaration of Helsinki.
PATIENT CONSENT STATEMENT
Written informed consent was obtained from all participants.
CLINICAL TRIAL REGISTRATION
N/A.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
We sincerely thank all volunteers for participating in this study.
Kunihiro Iwamoto and Momoe Saji contributed equally to this study.
DATA AVAILABILITY STATEMENT
The entirety of the participants' data cannot be made publicity available as data sharing was not included in the consent form.
REFERENCES
- 1. Hovinga CA, Asato MR, Manjunath R, Wheless JW, Phelps SJ, Sheth RD, et al. Association of non‐adherence to antiepileptic drugs and seizures, quality of life, and productivity: survey of patients with epilepsy and physicians. Epilepsy Behav. 2008;13:316–22. [DOI] [PubMed] [Google Scholar]
- 2. Brunbech L, Sabers A. Effect of antiepileptic drugs on cognitive function in individuals with epilepsy: a comparative review of newer versus older agents. Drugs. 2002;62:593–604. [DOI] [PubMed] [Google Scholar]
- 3. Iwata M, Iwamoto K, Kawano N, Kawaue T, Ozaki N. Evaluation method regarding the effect of psychotropic drugs on driving performance: a literature review. Psychiatry Clin Neurosci. 2018;72:747–73. [DOI] [PubMed] [Google Scholar]
- 4. Sundelin HEK, Chang Z, Larsson H, Lichtenstein P, Almqvist C, Tomson T, et al. Epilepsy, antiepileptic drugs, and serious transport accidents: a nationwide cohort study. Neurology. 2018;90:e1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ramaekers J, Lamers C, Verhey F, Muntjewerff N, Mobbs E, Sanders N, et al. A comparative study of the effects of carbamazepine and the NMDA receptor antagonist remacemide on road tracking and car‐following performance in actual traffic. Psychopharmacology. 2002;159:203–10. [DOI] [PubMed] [Google Scholar]
- 6. Kaussner Y, Kenntner‐Mabiala R, Hoffmann S, Klatt J, Tracik F, Krüger HP. Effects of oxcarbazepine and carbamazepine on driving ability: a double‐blind, randomized crossover trial with healthy volunteers. Psychopharmacology. 2010;210:53–63. [DOI] [PubMed] [Google Scholar]
- 7. Saji M, Kanemoto K, Matsuoka E, Iwamoto K. Impact of antiepileptic drugs on simulated driving in patients with epilepsy. Seizure. 2021;92:195–9. [DOI] [PubMed] [Google Scholar]
- 8. Iwata M, Iwamoto K, Kitajima I, Nogi T, Onishi K, Kajiyama Y, et al. Validity and reliability of a driving simulator for evaluating the influence of medicinal drugs on driving performance. Psychopharmacology. 2021;238:775–86. [DOI] [PubMed] [Google Scholar]
- 9. Iwamoto K, Iwata M, Kambe D, Imadera Y, Tachibana N, Kajiyama Y, et al. Residual effects of zopiclone on driving performance using a standardized driving simulator among healthy volunteers. Psychopharmacology. 2022;239:841–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The entirety of the participants' data cannot be made publicity available as data sharing was not included in the consent form.


