Abstract
Over the past three decades, Individual Placement and Support (IPS) has emerged as a robust evidence‐based approach to helping people with severe mental illnesses, such as schizophrenia, bipolar disorder, and major depression, to obtain and succeed in competitive employment. This review addresses the history, principles, research, and future directions of IPS. It covers current evidence on employment outcomes, cost‐effectiveness, and nonvocational outcomes. It also describes current attempts to extend IPS to new populations. The authors provide an overview of numerous systematic reviews and meta‐analyses of randomized controlled trials involving people with serious mental illness. For studies addressing nonvocational outcomes and new populations, the review uses best available evidence. Published reviews agree that IPS enables patients with serious mental illness in high‐income countries to succeed in competitive employment at a higher rate than patients who receive other vocational interventions. Within IPS programs, quality of implementation, measured by standardized fidelity scales, correlates with better outcomes. Employment itself leads to enhanced income, psychosocial outcomes, clinical improvements, and decreased mental health service use. As IPS steadily spreads to new populations and new settings, research is active across high‐income countries and spreading slowly to middle‐income countries. IPS is an evidence‐based practice for people with serious mental illness in high‐income countries. It shows promise to help other disability groups also, and emerging research aims to clarify adaptations and outcomes.
Keywords: cost‐effectiveness analysis, employment, meta‐analysis, supported employment, systematic reviews
INTRODUCTION
Employment is a key social determinant of health and well‐being for working‐age adults, including people with serious mental illnesses, such as schizophrenia, bipolar disorder, and major depression. 1 , 2 However, even though most people with serious mental illness want to work, 3 less than 20% are employed at any given time, 4 , 5 , 6 and many are unemployed for most of their lives. 7
This paper reviews the research on an employment model called Individual Placement and Support (IPS), which is widely regarded as the most effective employment intervention for patients with serious mental illness. Our review addresses the intervention's history, principles, effectiveness, cost‐effectiveness, implementation and fidelity, extensions to new populations, and modifications. To the extent possible, the review relies on existing systematic reviews and meta‐analyses. In areas without such analyses, we rely on the best available data.
IPS HISTORY
In the 1990s, IPS began in a community mental health center in the northeastern region of the United States to help people with serious mental illness achieve their commonly identified goal of employment. 8 (Three criteria define the subgroup of people with serious mental illness: a psychiatric diagnosis of major mental illness, such as schizophrenia, bipolar disorder, or major depression; significant role impairment, in areas such as independent living, relationships, and employment; and extended involvement with mental health services, such as psychiatric hospitals, group homes, and mental health case management. 9 ) Prior to IPS, common approaches to employment included counseling, skills training, sheltered work, transitional employment, work enclaves, and agency‐run businesses. 10 , 11 These approaches, which had little or no rigorous empirical support, 12 shared the assumption that patients with serious mental illness were not ready for employment and needed training and other prevocational experiences before entering competitive jobs. As a contrast, IPS adopted a place‐and‐then‐support approach, consistent with supported employment from the developmental disabilities field. 13 In other words, IPS used a rapid job search and followed employment with training and support as needed. As a further departure from reliance on expert opinion, researchers developed, refined, and implemented IPS with rigorous research from the beginning. Initial pilot studies 14 , 15 , 16 led to a randomized controlled trial (RCT) in rural New Hampshire, 17 followed by a second RCT in inner‐city Washington, DC. 18 The first trial included rural, White participants in a relatively affluent, demographically homogeneous area. The second took place in a poor urban area and included predominantly African American homeless participants who experienced mental illness and co‐occurring substance use disorders. Both studies compared IPS with the leading employment models of the era and found markedly superior employment outcomes for IPS participants.
Following these initial studies, IPS clinicians and researchers in the United States have developed and refined manuals, fidelity measures, implementation procedures, and training programs. The initial IPS manual 8 has evolved, adding greater specificity, including a separate manual for transition‐age youth that emphasizes supported education, 19 and recently enhancing details of job development and services for special populations, such as patients with mental illness and co‐occurring substance use disorders. 20 The basic principles of IPS (described below) have been constant, augmented by the addition of benefits counseling to help clients understand how specific amounts of work and wages may affect their entitlements related to disability and poverty. Researchers incorporated the principles of IPS into an initial fidelity measure, 21 updated to assess practical details of implementation, 22 and have demonstrated that fidelity consistently correlates with employment outcomes. 23 , 24 , 25 , 26 In the early 2000s, IPS began to spread to other high‐income countries. After translation into several languages, the IPS manuals and fidelity scales have guided and assessed implementation quality and technical assistance in hundreds of programs worldwide. Over time, IPS staff have standardized the process of conducting fidelity assessments and providing technical assistance. 20 The current best evidence, coming from the United States, 27 Japan, 28 and the Netherlands, 24 indicates that agencies and jurisdictions that follow standard implementation procedures, compared with those that do not, have better maintenance and expansion of IPS programs; randomized trials are needed.
The IPS Employment Center, now located at the Research Foundation for Mental Hygiene and Columbia University in New York City, provides research information, online and in‐person training, fidelity reviews, technical assistance, data‐sharing, and dissemination information. Over 80% of US states, numerous Veterans Health Administration hospitals and clinics in the United States, and approximately 20 countries use these services regularly. In addition, an International IPS Learning Community has grown steadily over the past two decades. 27 , 29 , 30 , 31 As of 2023, 26 US states and seven countries have joined the Learning Community (https://ipsworks.org). These states and countries participate in regular discussions, data‐sharing, research projects, and an annual meeting.
IPS is currently available in at least 20 countries in North American, Europe, Asia, and Oceania (Australia and New Zealand). 32 Nearly all of the expansion has been in high‐income countries, though several Eastern European countries are in the preliminary stages of implementing IPS, 33 and recent studies of IPS have been launched in Mexico 34 and India. 35
IPS PRINCIPLES
IPS incorporates eight core principles:
Focus on the goal of competitive employment: Agencies providing IPS are committed to regular jobs in the community as an attainable goal for clients seeking employment.
Zero exclusion/eligibility follows client choice: Every client who wants to work is eligible for services without assessments of readiness or requirements regarding work experience, symptoms, or any other issue.
Attention to client preferences: Services align with clients' preferences and choices, rather than practitioners' expertise or judgments. IPS specialists help clients find jobs that fit their preferences and skills.
Rapid job search: IPS programs help clients look for jobs soon after they express interest in working, and eschew lengthy pre‐employment assessment, training, and counseling.
Targeted job development: Based on clients' interests, IPS specialists build relationships with employers through repeated contact, learning about the business needs of employers and introducing employers to qualified job seekers.
Integration of employment services with mental health treatment: IPS programs integrate mental health and vocational services to ensure that clients receive consistent messages and care from a multidisciplinary team of providers.
Personalized benefits counseling: IPS specialists help clients obtain personalized, understandable, and accurate information about how working may impact their disability payments, health insurance, and other government entitlements.
Individualized long‐term support: Follow‐along supports, tailored for the individual, continue for as long as the client wants and needs the support to keep a job or advance career opportunities.
One hallmark of IPS is that researchers have continuously evaluated its effectiveness since it was developed. 36 Researchers also have reviewed the evidence for the effectiveness for each principle periodically since 1998. 37 , 38 , 39 Research shows that cultural adaptations of IPS, though common and necessary, should not violate the core principles. 40
EFFECTIVENESS OF IPS
The IPS literature has expanded geographically and in relation to target populations over the past 30 years. In this section, we summarize the current research on the effectiveness of IPS. Because many research groups have reviewed the IPS literature, another primary review would be duplicative. We therefore provide a narrative review of the recent systematic reviews of IPS, noting similarities and differences, and summarizing the consensus conclusions about the effectiveness of IPS. These recent reviews present new data that have not been previously available. We have added these new findings.
Most early reviews were narrative and covered the limited number of published studies. 38 , 41 , 42 The two earliest meta‐analyses were Cochrane reviews examining a small number of RCTs of supported employment for people with serious mental illness. 43 , 44 More recent reviews have superseded earlier ones based on an increasing number of studies, especially international studies throughout Europe, Canada, Australia, Hong Kong, and Japan. Between 1996 and 2013, nine (60%) of 15 IPS RCTs were published in the United States; since 2013, 10 (77%) of 13 IPS RCTs have been published outside the United States. 45
The number of systematic reviews and meta‐analyses that have examined a broad range of employment interventions and/or populations (not limited to participants with serious mental illness) has also grown steadily. One systematic compilation of 26 empirical reviews of employment interventions for people with a wide range of disabilities concluded that IPS studies comprised most of the available evidence and that, aside from employment programs for people with severe mental health conditions, “we found only very low‐quality to low‐quality evidence on vocational intervention for people with any other health condition.” 46
Inclusion and exclusion criteria
We included reviews that met the following criteria: published after 2015; included studies of IPS; evaluated RCTs comparing IPS to a non‐IPS control group (we excluded reviews of studies comparing standard IPS to IPS plus an augmentation of IPS.); and examined employment outcomes.
Search procedures
We used four methods to identify relevant literature reviews. First, we began with four systematic reviews that we co‐authored. 47 , 48 , 49 , 50 Second, we received notifications from various listservs on newly published articles on IPS (Google Scholar Alert; CSDP Disability Research Consortium). Third, we relied on a network of IPS researchers who informed us of recent research. Fourth, we examined the reviews identified by Levack and Fadyl. 46
Results
In Table 1, we list nine IPS meta‐analyses published between 2016 and 2023. 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 These meta‐analyses have commonalities as well as important differences. In terms of commonalities, all limit their reviews to RCTs and examine differences between competitive employment rates for IPS and control groups. These reviews have examined IPS studies that included different types of control groups, including no vocational services, vocational services as usual, and active vocational interventions considered best practices at the time. With two exceptions, 47 , 54 all limited studies to people with mental health conditions (i.e., any psychiatric disorder, including both severe mental illnesses, such as schizophrenia and bipolar disorder, and common mental disorders, such as anxiety disorders). Three meta‐analyses included RCTs of IPS for any mental health condition, 48 , 49 , 55 while four included only people with serious mental illness or schizophrenia‐spectrum disorders. 50 , 51 , 52 , 53 One review 53 conducted a network analysis examining both direct and indirect comparisons, and we used the direct comparisons only.
Table 1.
Characteristics of IPS meta‐analyses (2016–2023).
| First author (Reference #) | Year | Intervention | Target population | # of RCTs | Sample size | Publication years for included studies | Review appraisal of quality of RCTs |
|---|---|---|---|---|---|---|---|
| Modini 51 | 2016 | IPS with adequate IPS fidelity | SMI; excluded PTSD and early psychosis | 17 | 4367 | 1996–2015 | Downs & Black: 15 good; 2 fair |
| Carmona 52 | 2017 | Broadly defined supported employment | Schizophrenia spectrum disorders | 13 | 2088 | 1986–2015 | Methodological quality scale adapted from Miller |
| Suijkerbuijk 53 | 2017 | SE, enhanced SE, prevocational, TE, and psychiatric care only | SMI | 22 (follow‐up > 1 year; direct comparisons) | 5233 | 1996–2016 | GRADE (Quality of evidence) SUCRA (for network analysis) |
| Metcalfe 50 | 2018 | IPS with adequate IPS fidelity | SMI; excluded MHTS | 21 (30 sites) | 3000 | 1996–2017 | None |
| Frederick 54 | 2019 | IPS with adequate IPS fidelity | SMI and other disabilities | 25 | 5445 | 1996–2017 | None reported |
| Brinchmann 55 | 2020 | Adequate IPS fidelity; modified IPS or no fidelity excluded | SMI or moderate mental illness | 27 | 6651 | 1996–2019 | Downs & Black; Removed on poor quality study (not identified) |
| First author | Year | Intervention | Target population | # of RCTs | Sample size | Publication years for included studies | Review appraisal of quality of RCTs |
|---|---|---|---|---|---|---|---|
| de Winter 49 | 2022 | IPS with adequate IPS fidelity | Any mental disorder | 32 | 7665 | 1996–2019 | Cochrane Risk of Bias: Overall, “low levels of selection and attrition bias” |
| Special populations | |||||||
| Bond 47 | 2019 | IPS with adequate IPS fidelity | Other conditions not SMI | 9 | 2902 | 1996–2018 | Examined degree of IPS fidelity |
| Bond 48 | 2023 | IPS with adequate IPS fidelity | Young adults with mental health conditions | 7 | 697 | 1996–2022 | Qualitative assessment of individual studies |
Abbreviations: IPS, Individual Placement and Support; MHTS, Mental Health Treatment Study; PTSD, posttraumatic stress disorder; RCT, randomized controlled trial; SE, supported employment; SMD, standard mean difference; SMI, serious mental illness; TE, transitional employment.
All meta‐analyses examined competitive employment rate (sometimes referred to as job acquisition), which is easy to assess, universally measured, and correlates with other employment indices, such as hours of work and wages. One meta‐analysis provided details on a range of employment outcomes (time to first job, job tenure, job length, and income) and nonvocational outcomes (e.g., quality of life and mental health symptoms) in a group of RCTs, not only for people with mental illness but also other conditions. 54
We excluded four systematic reviews published since 2016 for various reasons. One examined study quality and summarized findings from 23 studies without employing meta‐analysis 56 ; a second restricted its search to European studies, identifying a limited number of IPS RCTs 57 ; a third identified 88 studies, but did not screen for duplications (multiple papers reporting findings from the same study) 58 ; and a fourth examined 28 studies assessing non‐RCTs of supported employment for people with mental illness in routine practice. 59 These reviews included low‐quality studies, some of which did not examine IPS.
Competitive employment outcomes
In Table 1, the first seven meta‐analyses examined between 13 and 48 RCTs (or sites, in the case of multisite trials), with the total sample size ranging from 2088 to 8743. The RCTs of IPS included in these meta‐analyses have generally examined outcomes over a period of 6 months to 2 years. One summary of 28 RCTs of IPS found the follow‐up period to be a median duration of 18 months (mean = 18.6 months). 45 The mean sample sizes in these 28 studies were 114 for IPS and 117 for the control group. Most RCTs of IPS have monitored fidelity using a standardized IPS fidelity scale. Five of the seven meta‐analyses limited the studies reviewed to studies of IPS using a standardized IPS fidelity scale and achieving at least good fidelity.
The meta‐analyses differ in the number of included studies (based on the recency of the review), the populations included, the outcome measures examined, the search for moderator variables among external factors, and the assessment of methodological quality. As shown in Table 2, the relative risk ratio assessing the advantage of the competitive employment rate for IPS compared to controls was significant in all seven meta‐analyses, with a median risk ratio of 2.16 (range: 1.63–2.49). We used what we judged to be the most representative risk ratio from one study that reported multiple comparisons. 53
Table 2.
Findings for nine IPS meta‐analyses.
| First author (Reference #) | Relative risk ratio for competitive employment rate | Moderators and other outcome measures |
|---|---|---|
| Modini 51 | 2.40 | ns: unemployment; geographic region; IPS more effective with higher GDP growth |
| Carmona 52 | 2.49 | Hours worked: SMD = 1.33, p = 0.06 |
| Suijkerbuijk 53 | 2.16 9 RCTs of SE versus prevoc; >1 year follow‐up; N = 1569 | Network analysis to compare between different vocational models |
| Metcalfe 50 | 2.31 | IPS impact increased with labor laws favoring employers and less generous disability benefits |
| Frederick 54 | 1.63 | Time to first job: d = ‐0.31; job tenure: d = 0.55; job length: d = 0.46; income: d = 0.48; employment rate at end of trial: d = 0.58. Nonvocational outcomes were ns (quality of life: d = 0.30; global functioning: d = 0.09; mental health: d = 0.03) |
| Brinchmann 55 | 2.07 | IPS efficacy reduced by strong legal protection against dismissals. ns: temporary employment laws, generosity of disability benefits, integration policies, GDP, unemployment. |
| de Winter 49 | 1.80 | Job duration: d = 0.41; wages: d = 0.31; Moderators: Most measures were ns, but IPS more effective for people with SMI, schizophrenia spectrum disorders, and less severe symptoms; IPS less effective in Europe. |
| Special populations | ||
| Bond 47 | 1.54 | Examined other employment outcomes for individual studies but did not synthesize. Most significantly favored IPS. Nonvocational outcomes using different measures had inconsistent results. |
| Bond 48 | 1.69 | Job duration: g = .34; education: RR = 1.33 |
Abbreviations: IPS, Individual Placement and Support; ns, not significant; RR, relative risk; SE, supported employment; SMD, standard mean difference; SMI, serious mental illness.
Another meta‐analysis 54 provided effect sizes for multiple employment outcome measures (time to first job, job tenure, job length, income, and employment rate at the end of the trial). The analyses, which included people with a range of disabilities, found moderate d effect sizes ranging from 0.31 to 0.58, as shown in Table 2. An earlier review, limited to people with serious mental illness, found stronger effects for time to first job and job tenure favoring IPS. 60
Although not comprehensive meta‐analyses, two other studies aggregated data from multiple RCTs to increase statistical power. One study, aggregating data from four RCTs in the United States (N = 681), 61 found that IPS participants gained employment faster, maintained employment four times longer during follow‐up, earned three times the amount from employment, and were three times as likely to work 20 h or more per week, compared with control participants. The second study examined the effectiveness of IPS by combining individual data from six IPS RCTs (N = 1594) (five European studies and one US study). 62 Competitive employment during follow‐up was significantly higher for IPS than controls (odds ratio = 1.92), with a similar significant advantage in time to first job (odds ratio = 1.90); moreover, during follow‐up, IPS participants averaged 1.90 more hours worked (221.5 vs. 116.8) and 1.66 more weeks worked (14.6 vs. 8.8) than controls.
Nonvocational outcomes
Controlled studies, in general, have not shown that IPS has a direct effect on psychosocial outcomes, such as mental health, quality of life, interpersonal functioning, global functioning, or self‐esteem. 54 , 63 Exceptions include one large study that found that IPS had a small but significant effect on mental health symptoms (d = 0.23) and quality of life (d = 0.18) 64 and another that found IPS had a significant impact on a measure of PTSD‐related functioning in interpersonal and lifestyle domains. 65 One other nonvocational area that has been an exception in several studies concerns mental health treatment services, as discussed in the section on cost‐effectiveness.
By contrast, a strong and robust literature shows that employment—specifically, competitive employment, and especially a sustained period of employment—improves mental health outcomes for people with mental health conditions. 1 , 66 , 67 , 68 Many secondary analyses of RCTs of IPS have shown that employment mediates the salutary effects of IPS on the nonvocational outcomes. The findings regarding positive effects of competitive employment align with studies in the general population. 2 , 69 , 70 , 71 , 72
FACTORS MODERATING THE EFFECTS OF IPS
In this section, we review findings from analyses examining participant‐level data and from meta‐regressions that analyze study‐level data. Analysis of study‐level measures is less precise than individual‐level measures and should be interpreted cautiously. We distinguish between different types of analyses below.
Client factors
Many studies have examined client factors (including diagnostic, clinical, and demographic characteristics) as moderators of employment outcomes in IPS. One meta‐analysis found that IPS was relatively more effective in subgroups of people with serious mental illness or schizophrenia spectrum disorder and less effective in those with common mental disorders or major depressive disorder. 49 Similarly, a secondary analysis of a combined dataset from six RCTs (N = 1594) found that IPS had significantly better competitive employment outcomes than services as usual for clients with schizophrenia, bipolar disorder, and drug use disorders, but not for clients with depressive disorders. 62 Another secondary analysis using a combined dataset from four IPS RCTs (N = 671) examined seven sociodemographic, eight clinical, and two work history variables, and concluded that clients benefited more from IPS than alternative employment services regardless of their background characteristics. 73 Another set of analyses found that work history was the only significant predictor for job acquisition among IPS clients, while receipt of disability benefits was associated with fewer total weeks worked. 74 One IPS RCT of 2055 disability beneficiaries found few predictors of employment outcome among 20 background characteristics. 75 Positive work history was a strong predictor of job acquisition within both the IPS and control groups; moreover, patients with a poor work history benefitted from IPS even more than those with recent work experience. A narrative review of six IPS RCTs examining racial and ethnic differences concluded that Black and Hispanic clients have comparable employment outcomes in IPS as non‐Hispanic White clients. 76
Two meta‐analyses examined specific populations: people with health conditions other than serious mental illness 47 and young adults with mental health disorders. 48 The relative risk ratios for the competitive employment rate for these two meta‐analyses were 1.54 and 1.69, respectively, somewhat lower than the risk ratios for the larger meta‐analyses but statistically significant in both studies.
Overall, the impact of client factors across studies has been modest compared with the impact of IPS, which has been shown to benefit a wide range of clients with mental health conditions. One exception may be work history, which has a consistent, substantial impact on employment outcome.
External factors
Four meta‐analyses examined the impact of external factors, such as geographic region, unemployment rate, economic growth, disability policy, and labor laws. 49 , 50 , 51 , 55 The findings differed somewhat, but one consistent finding has been lower competitive employment rates overall in European studies. 77 A multisite study of IPS in six European nations found that study sites in northern countries were more affected than southern countries by disability systems that incentivize people to avoid work. 78
The barriers to implementing evidence‐based practices in rural communities might imply that rural IPS programs are more difficult to implement to high fidelity and have poorer outcomes than programs located in more populated areas. 79 , 80 However, several studies have found no differences between rural and urban IPS programs in fidelity 81 or employment rates. 82
Methodological factors
Reviewers have also examined methodological factors, such as IPS fidelity, 49 length of follow‐up, 49 , 54 , 55 and year of publication. 55
Logically, the choice of control group should affect the findings of an RCT. If the control group has a positive impact on outcome, then the effect size for IPS‐control differences should be attenuated. To date, however, researchers have not found any alternative employment model that shows this effect. Two systematic reviews assessed the impact of type of control group on the strength of the experimental findings. One meta‐analysis found that RCTs using active placebo comparison groups (i.e., control groups providing employment services following a recognized vocational model) paradoxically had larger effects favoring IPS than those with passive control groups (e.g., no‐treatment control groups). 49 The mean employment rate at follow‐up was lower for participants in active placebo control groups than passive control groups (26.7% vs. 29.4%, respectively) compared with corresponding IPS groups (50.1% vs. 48.3%). Using network analysis, another review examined direct and indirect comparisons between supported employment and several other employment interventions (prevocational training, transitional employment, and psychiatric care only). 53 Their analyses were compromised by including studies with small samples, serious methodological limitations, and supported employment services that were not based on IPS.
Because of limitations in both the measurement and precision of reporting of IPS fidelity scores, meta‐analyses have not examined direct correlations for the relationship between fidelity and employment outcome. However, differences across studies in fidelity may be a confounding factor in some subgroup analyses. For example, one meta‐analysis reported that 89% of the RCTs of IPS for serious mental illness had good or excellent IPS fidelity compared with only 50% of RCTs of IPS for common mental disorders. 49 Two multisite studies with standardized procedures for measuring fidelity did find small correlations between IPS fidelity and employment outcomes. 78 , 83
Year of publication has also shown a modest effect suggesting decreasing effect sizes over time, with smaller effect sizes for more recent studies, though this finding may be confounded by recent European studies, which have smaller effect sizes than US studies, most of which were conducted earlier. IPS fidelity may have been less robust as well in some recent studies. 55 One meta‐analysis found publication bias such that smaller studies had larger effect sizes (a fairly common meta‐analytic finding). 55 Another meta‐analysis did not find publication bias. 49 One meta‐analysis reported that length of follow‐up was negatively correlated with effect size, 55 but another did not show this. 54
Long‐term outcomes
Most RCTs of IPS have limited their assessment to the period during and shortly after participants have received IPS services, usually 2 years or less. A handful of studies have examined longer‐term outcomes of 5 years or more. An aggregation of three long‐term studies 45 found that 49% of 120 clients enrolled in IPS became steady workers (defined as working in at least 6 months of each year of follow‐up), maintaining competitive employment for 10 years or longer. 84 , 85 , 86 By comparison, only 11% of 54 control clients maintained steady employment for 5 years in one study. 85 A follow‐up study of a large, multisite trial of IPS for disability beneficiaries with serious mental illness found that significantly higher earnings for IPS clients compared to controls persisted over a 5‐year period after the end of the 2‐year follow‐up. 87 Moreover, the IPS participants increased their annual employment earnings by 40% over the 5‐year follow‐up period, whereas control participants changed little.
COST‐EFFECTIVENESS
Direct IPS costs
The direct costs of IPS services refer to costs associated with services provided by the IPS team, including staffing and supervision. Economists typically treat vocational services as a separate cost center and do not include mental health treatment, case management, housing, or other nonvocational services provided to IPS clients. Personnel costs comprise a large percentage of IPS costs, although a complete accounting of costs includes overhead (office space, transportation, computers, etc.). Six US studies 88 , 89 , 90 , 91 , 92 , 93 have reported annual per‐client costs of IPS services in the public mental health system. After converting to 2022 dollars using a federal consumer price index calculator, 94 the annual per‐client costs range from $4000 to $7500. Averaging across these studies, the mean cost of serving one client for 12 months is approximately $6000 in 2022 US dollars.
The length of clients' enrollment in IPS varies widely. The time to first job averages 4–5 months for IPS clients who successfully find a job and start employment, 60 after which IPS services taper off sharply over the next several months. 95 On a typical IPS caseload with most clients gaining employment but others terminating before reaching that goal, IPS clients average 6–8 months receiving IPS services before termination. 92 Assuming that clients receive IPS services on average for 8 months, the mean per‐client cost of IPS is estimated to be $4000 in 2022 US dollars.
In addition to length of services, other factors influence IPS costs, including caseload size and staff salaries. Labor costs reflect geographic differences in cost of living and wages. Thus, the $4000 per‐client cost estimate is an average, and the actual cost of a specific IPS program depends on many factors. 92 , 93 Two European pilot studies suggested that the per‐client costs might be systematically reduced without reducing effectiveness by introducing time limits on duration of enrollment in IPS 96 or amount of IPS specialist time allocated to helping individual clients find employment. 97 Long‐term research could clarify this issue.
Is IPS an expensive intervention? Studies have found annual mean per‐client service costs for IPS to be less than those for rehabilitative day treatment, 98 similar to costs for stepwise approaches providing prevocational preparation prior to competitive employment placement, 89 , 90 and twice as expensive as one using a transitional work program. 91 Of the alternative vocational interventions examined in IPS RCTs, none, including expensive alternatives, have yielded better outcomes than IPS.
Other costs affected by IPS services
Several economic analyses of IPS have examined mental health treatment costs or, less often, health care costs in general. Depending on the study purposes, total costs could include a wide range of costs of interest to specific stakeholder groups. For example, IPS has been hypothesized to reduce applications for and receipt of Social Security disability benefits (especially among young adults). Although minimal research has examined this question, 99 enrolling in IPS does not appear to increase the rate of termination or suspension of Social Security disability benefits among beneficiaries. 64 IPS has also been hypothesized to reduce criminal justice involvement, but the few IPS studies that have examined this question have found little supporting evidence. For example, a small RCT of IPS for people with justice involvement (N = 85) found no differences in rates of arrest or incarceration between IPS and a comparison group during a 1‐year follow‐up period. 100 On the other hand, a much larger program evaluation using administrative data for 7284 mental health clients (including those without justice involvement) found a small but significant reduction in arrest rates between 1 year prior to IPS enrollment and 1 year after enrollment for IPS clients compared with matched controls. 101
IPS cost‐effectiveness analyses
A recent systematic review examined the cost‐effectiveness of IPS in seven RCTs. 102 We updated this review with four additional studies (and excluded one report because it was the earlier of two reports based on the same study). 103
Of the 10 studies shown in Table 3, nine were RCTs assessing the costs and benefits of IPS, 85 , 89 , 90 , 104 , 105 , 106 , 107 , 108 , 109 and one was a pre–post design in which IPS services replaced a day treatment program. 98 Four were conducted in the United States and six outside the United States. Seven studies conducted a cost‐effectiveness analysis, 90 , 104 , 105 , 106 , 107 , 108 , 109 three studies conducted a cost–benefit analysis, 85 , 98 and one study reported the findings in terms of cost offset. 98 Methodological features of these studies varied. Sample sizes ranged from 100 to 720, follow‐up periods ranged from 12 to 60 months, and IPS fidelity scores were rated as good in six studies, fair to good in three studies, and poor in one study. Measurement of effectiveness also varied, although all studies used some measure of employment outcome. The choice of specific employment outcome measures was relatively unimportant for determining direction of effectiveness, because most employment outcomes in these studies significantly favored IPS, regardless of specific measure used as the criterion in the cost‐effectiveness (or related) analysis.
Table 3.
Economic analyses of IPS.
| Primary author (Year) # Reference | Design | Location | Clients served | N | Months of follow‐up | IPS fidelity | Analytic approach | Total costs | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Clark (1998) 98 | Day treatment conversion | US (New Hampshire) | SMI | 184 | 12 | Good | Cost offset | IPS < day treatment | After shifting to IPS, employment rates increased from 33% to 56% at Site 1 and from 9% to 45% at Site 2. Mental health center costs reduced by 29% at the two study sites. |
| Clark (1998) 89 | RCT | US (New Hampshire) | SMI | 143 | 18 | Good | Cost–benefit | IPS = Control | Mean per‐client employment program costs ($5636 for IPS and $5532 for controls) and mental health treatment costs ($14,429 for IPS and $16,712 for controls) were similar. |
| Dixon (2002) 90 | RCT | US (Washington, DC) | SMI | 150 | 18 | Good | CEA | IPS > Control | Overall costs for IPS 16% higher: Mean per‐client costs employment program costs ($6059 for IPS and $5723 for controls) and mental health treatment costs ($23,018 for IPS and $19,396 for controls). |
| Stroupe (2022) 104 | Multisite RCT | US (Veterans Affairs) | Veterans with PTSD | 541 | 18 | Good | CEA | IPS > Control | Mean per‐client annual health care costs $4000 more for IPS than control group |
| Heslin (2011) 105 | RCT | UK | SMI | 219 | 24 | Poor | CEA | IPS < Control | Overall costs for IPS 20% lower: Mean per‐client costs for IPS were £300 and mean per‐client mental health service costs were £9571 for IPS and £11,932 for controls. |
| Shi (2012) 106 | RCT | Canada | SMI | 149 | 12 | Good | CEA | IPS < Control | IPS was cost‐effective compared to usual services, although baseline differences in inpatient days attenuated finding. |
| Knapp (2013) 107 | Six‐nation RCT | Europe | SMI | 312 | 12 | Fair–good | CEA | IPS < Control | IPS had better health outcomes at lower cost (fewer days of hospitalization). |
| Hoffmann (2014) 85 | RCT | Switzerland | SMI | 100 | 60 | Good | Cost–benefit | IPS = Control | Higher return on investment for IPS ($0.54 for IPS vs $0.18 for control). |
| Yamaguchi (2017) 108 | RCT | Japan | SMI | 111 | 12 | Fair | CEA | IPS < Control | IPS intervention was modified IPS and included cognitive remediation |
| Christensen (2021) 109 | Multisite RCT | Denmark | SMI | 720 | 18 | Fair–good | Cost–utility | IPS < Control | Overall costs for IPS 41% lower: Mean per‐client total costs for IPS were €13,582 for IPS and €23,125 for controls. Mean per‐client costs for IPS were €914. |
Abbreviations: CEA, cost‐effectiveness analysis; IPS, Individual Placement and Support; PTSD, posttraumatic stress disorder; RCT, randomized controlled trial; SMI, serious mental illness.
The total costs for the IPS condition were less than those for the control condition in six studies, equal in two studies, and greater in two studies. Every study showed better employment outcomes for IPS than controls. The 10 economic analyses were mostly short‐term studies; eight had follow‐up periods of 12–18 months in duration. Long‐term studies of IPS suggest that its benefits persist and in some cases increase over time. 87 Therefore, the long‐term benefits from IPS may exceed those found in the published studies.
IPS cost savings: Areas of greatest impact
Historically, day treatment continues to be a core component in many mental health systems throughout the world. For example, in Japan, service agencies provide group services that include work skills training, cognitive rehabilitation, illness management, and recreation and physical activities. 110 A series of studies conducted in the 1990s examined the effectiveness of closing day treatment programs and replacing them with IPS. The studies showed that this organizational change was feasible and led to significant improvement in employment outcomes. 38 One study systematically examining costs to the participating mental health center found that terminating a day treatment program and replacing it with IPS resulted in a 29 percent reduction in overall costs. 98
Several RCTs have found that IPS significantly decreased inpatient treatment costs, 85 , 107 , 108 , 109 , 111 as did one study examining outcomes before and after implementing IPS. 16 IPS studies have not shown reductions in outpatient treatment costs, at least in the short term. However, observational studies suggest that unemployed clients who gain employment and continue to work over time show reduced mental health treatment costs over the long term. 66 , 112
IPS IMPLEMENTATION AND FIDELITY
The IPS Employment Center has accrued extensive experience while helping to implement hundreds of IPS programs. Although specific strategies have not been confirmed by RCTs, US states that follow these strategies maintain and expand high‐fidelity programs at a much higher rate than those that do not follow such procedures. 27 In general, new IPS programs require several months or 1 year of intensive training and supervision to achieve high‐fidelity implementation. Standard implementation procedures include hiring IPS specialists and an IPS supervisor, followed by a kickoff meeting to build consensus among stakeholders. Shortly after the kickoff, an IPS trainer visits the IPS team several times to provide training (e.g., on client engagement, job development, job supports, integrated services, helping individuals who have co‐occurring disorders, and supported education). The trainer also attends mental health treatment team meetings, models engaging mental health practitioners in conversations about employment, and attends IPS vocational unit meetings on a regular basis to emphasize applying IPS principles. Trainers strive to be at the agency at least twice a month for the first 6 months to attend meetings, accompany IPS specialists to meet with employers, and join with IPS specialists to help individual job seekers who are having difficulty reaching their goals. They model effective strategies for the IPS specialists and the supervisor. They also participate in IPS steering committees to help guide agency‐wide decisions that will affect the program. After six or seven months of implementation, the IPS trainer, along with another experienced fidelity reviewer, visit the agency for 1.5 days to complete a fidelity assessment and then provide technical assistance to improve IPS implementation.
In the United States, local program implementations typically depend on administrative supports from state mental health, vocational rehabilitation, and insurance authorities. Optimally, these agencies meet regularly to align policies, regulation, and procedures. The US Office of Disability Employment Policy has sponsored such coordination efforts through the Advancing State Policy for Integrated Recovery and Employment project since 2021 (https://www.dol.gov/agencies/odep/initiatives/aspire). The project provides technical assistance to state leaders to help them coordinate state policies, funding contracts, data sharing, training initiatives, and fidelity reviews for IPS programs in their states. Federal leaders from federal agencies provide advice on new programs. Subject matter experts help the states with whatever technical assistance is needed to start new programs, hire trainers and fidelity reviewers, and oversee their IPS programs. State leaders participate in monthly learning community conferences with other states.
The challenges to implementing IPS outside the United States include many of the same themes as described above, 113 but also other barriers specific to each country's history, economy, mental health and welfare systems, labor laws, culture, and myriad of other factors. A collection of case reports describing IPS implementation in 11 countries on four continents (Europe, Australia/New Zealand, Asia, and North America) illustrates both similarities and differences across countries. 114 Researchers should continue trying to fit the IPS model to different mental health systems, welfare systems, and labor laws that are sometimes country‐specific and sometimes applicable to multiple countries. One limitation of the IPS implementation literature is that the preponderance of this research has been conducted in the United States and Europe.
NEW DIRECTIONS
Extending IPS to new populations
IPS developed initially to help people with serious mental illnesses in the US public mental health system. The term “serious mental illness” encompasses psychotic and mood disorders (usually including schizophrenia, bipolar disorder, and major depression) that are enduring and disabling. 9 People with such conditions generally meet criteria for federal disability programs in the United States because they have significant impairments in social functioning and qualify for services in public community mental health centers. They comprise approximately 5.6% of working‐age adults in the United States. 115 However, approximately half of these individuals do not receive services in community mental health centers 116 and therefore have no access to IPS‐supported employment. Many decline to use or cannot access community mental health services; others are homeless or institutionalized in hospitals, jails, prisons, or nursing homes. IPS programs are beginning to reach out to alternative settings (e.g., Building Evidence for Employment Services [https://www.acf.hhs.gov/opre/project/building-evidence-employment-strategies-project-bees] and NextGen [https://mathematica.org/projects/next-generation-of-enhanced-employment-strategies-project-nextgen]), but related research is just beginning.
In addition to people with serious mental illnesses, many others, approximately 15% of working‐age adults in the United States, experience a mental health disorder that does not qualify as serious mental illness, but many are unemployed and need assistance to secure employment. Disorders affecting people in this category include posttraumatic stress disorders, mild to moderate depression or anxiety disorders, substance use disorders, developmental disorders, personality disorders, and numerous other conditions. Many young people in their late teens or early 20s, often called transition‐age youth, have initial psychoses complicated by substance use and various other mental health conditions. Many other people have disabling physical conditions (e.g., injuries, pain syndromes, and autoimmune disorders) and need vocational assistance. The prevalence of disability in the United States varies according to survey methods, but one research group conservatively estimated that between 40 million and 57 million Americans were living with a disability in 2010. 117 Using the estimate of 18.7% of the population from the Survey of Income and Program Participation, approximately 56 million people in the United States had a disability in 2020. Because evidence‐based vocational interventions for unemployed people with these myriad other conditions are rare, programs are extending IPS‐supported employment to some of these populations, even though the currently available research is sparse.
A meta‐analysis of seven RCTs for young adults with mental health conditions found that 208 (58.3%) of 357 IPS participants and 110 (32.4%) of 340 control participants were competitively employed during follow‐up, with a small effect size (g = 0.34) for job duration favoring IPS and with modest education outcomes favoring IPS. 48 Thus, IPS appears to be effective in helping young adults with serious mental illness or early psychosis gain and keep competitive jobs, but the impact of IPS on education outcomes for this population is unclear.
One study examined the effectiveness of IPS for different diagnostic groups in a data set combining individual data from six IPS RCTs (N = 1594) (five European studies and one US study). 62 For clients with schizophrenia and substance use disorder, IPS had significantly better employment outcomes than controls on measures of employment rate, time to first job, hours worked, and weeks worked. Participants with bipolar disorder receiving IPS also had a significantly higher employment rate than control participants, but hours and weeks worked did not differ. IPS did not differ from controls for people with depression. The authors noted that nonsignificant results may have been due to low statistical power.
The extension of IPS to new populations is a relatively recent development. Figure 1 summarizes 13 RCTs of IPS for working‐age adults with conditions other than serious mental illness. 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 Only three of these RCTs were completed before 2016. 120 , 126 , 127 These RCTs include four completed since the publication of a meta‐analyses of IPS for other populations discussed earlier. 47 The target groups included people with common mental disorders (anxiety and depression), posttraumatic stress disorder, chronic pain, substance use disorders, or spinal cord injuries, and one study of primary care clinic patients. Of the new studies, one found that significantly more primary care patients enrolled in IPS achieved steady work than patients receiving usual services. 121 Two others found significant employment outcomes favoring IPS for young adults with health conditions at risk for long‐term disability 129 and for military veterans with substance use and criminal justice involvement. 124 The small pilot RCT of IPS for pain patients, however, did not find a significant effect for IPS, possibly because it was underpowered. 130
Figure 1.
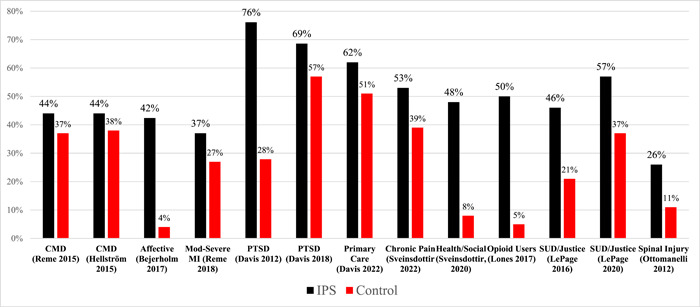
Competitive employment rates in 13 randomized controlled trials (RCTs) of Individual Placement and Support (IPS) in other populations. CMD, common mental disorder; MI, mental illness; PTSD, posttraumatic stress disorder; SUD, substance use disorder.
Research on IPS for new populations ranges across groups from nonexistent to several studies, but many areas obviously need more work. Examples include IPS programs for people in different stages of justice‐system involvement; people with primary substance use disorders 131 , 132 ; refugees 133 ; recently homeless people living in supportive housing; people with common and disabling conditions, such as obsessive‐compulsive disorder and autism spectrum disorder; and indigenous populations in many countries. Another frontier is people who reside in low‐ and middle‐income countries.
Modifications, adaptations, and augmentations
IPS program implementers often modify the intervention, particularly when extending IPS to new populations or in new settings. These modifications fall into three basic categories: adaptations for context that do not compromise basic principles; omissions or changes to one or more of the basic principles of IPS; and augmentations of standard IPS services with addition of a new component. 40 Each type of modification occurs frequently, but rigorous evaluations are rare.
Minor adaptations for context are common. Examples of apparently successful cultural adaptations are abundant. For example, one trial that oversampled Hispanic Americans adjusted IPS by adding outreach to families, recognizing that in this culture families rather than individuals made decisions regarding employment. 134 Another survey of rural IPS providers identified common changes to hiring IPS specialists and conducting job development. 79 Another common adaptation involves changes to job planning and supports for clients with co‐occurring substance use disorders. 135 However, few if any randomized trials have specifically tested cultural adaptations of any evidence‐based practices, including IPS. 136 Cultural adaptations are often commonsensical, and the resources required to test them rigorously may be disproportionately high.
Many programs and a few studies have deleted one or more of the principles of IPS, for example, the integration of vocational and clinical services. These changes generally weaken employment outcomes. For example, studies that have failed to confirm interest in employment, 137 to prioritize client preferences, 138 to provide integrated vocational and clinical services, 139 to offer long‐term supports, 140 or to provide systematic job development and follow‐along support 141 have yielded weak results.
Finally, several augmentations to IPS have been tried, for example, adding motivational interviewing, but most of these additions have not enhanced outcomes. 40 One possible exception involves adding cognitive enhancement interventions to standard IPS. Some RCTS of IPS plus cognitive enhancement have shown improvement of employment outcomes over IPS alone, 142 , 143 but other studies of cognitive enhancement have not improved employment outcomes. 144 , 145
Modifying IPS deserves further study. One obvious target is the group of IPS participants who do not have vocational success and may be helped by something more or something different. In addition, delivering IPS to people in new populations or in new settings will likely require modifications to enhance fit.
DISCUSSION
Numerous RCTs and systematic reviews agree that IPS‐supported employment effectively increases competitive employment among participants with serious mental illnesses. IPS is broadly effective for this population in high‐income countries, although characteristics of participants (e.g., justice system involvement), program quality (e.g., model fidelity), and environments (e.g., disability regulations and payments) have some influence on outcomes. IPS is also cost‐effective compared with active comparison approaches. Several studies indicate that IPS employment outcomes persist for years, which may produce substantial cost savings.
Many other findings are less certain. Current innovations address extending IPS to new populations, new settings, and new countries. Active studies are investigating IPS for people with: substance use disorders; common mental health conditions, such as anxiety and depression; chronic pain syndromes; chronic homelessness; justice system involvement; autism spectrum disorder; experience of human trafficking; and other groups. Attention to historically underserved populations, such as specific ethnic and racial groups, is also spreading. IPS has typically been provided within mental health clinics, but new settings include addiction treatment centers, immigration and refugee centers, supportive housing programs, primary healthcare clinics, and welfare programs. Although most high‐income countries have adopted IPS, spread to low‐ and middle‐income countries is an important new frontier. In many of these new populations and settings, implementers are modifying, adapting, or augmenting IPS, but minimal or no research supports these changes.
Several factors may explain the success and spread of IPS‐supported employment. First and foremost, most people with mental health conditions want meaningful work and consistently report that employment is an essential, often central, part of their recovery process. They therefore advocate for employment services. Second, a strong research base has guided and buttressed the development and spread of IPS. Program leaders, healthcare leaders, and employment policy leaders pay attention to research, perhaps more so in some countries than others. The process proceeds slowly due to resistance to change, difficulty integrating health and vocational services, and difficulties funding IPS, but over time research does influence policy. Third, healthcare providers and policy‐makers in many countries recognize that employment is itself a powerful social determinant of health and that IPS should therefore be a core treatment for people with serious mental illness. The research on IPS has stimulated this critical shift in beliefs. Similar transitions have not yet occurred in relation to other populations but may happen as implementation and research develop. Good research generally leads to good policy.
One critical aspect of scientific evidence is consilience, defined as the unity of knowledge across different scientific disciplines. 146 Numerous scientific approaches undergird the importance of employment for the well‐being of humans, including those with disabilities. The effectiveness of IPS‐supported employment has support from not only RCTs but also qualitative studies, implementation research, economic analyses, and many other fields. For example, studies from animal research, hominid development, cultural anthropology, epidemiology, sociology, psychology, and other disciplines support the central importance of employment for homo sapiens.
Despite many successes, current limitations and challenges are legion. The largest one involves bureaucratic inertia, which limits the availability of IPS services to a small minority of those in need. In the United States, profit‐making industries, rather than patient preferences and effective interventions, dominate health policy. In many countries, the separation between agencies that are designated as health‐related and those that address social determinants is rigid. Stigma continues to limit access, participation, and quality for mental health and substance use disorder services in most countries, and people with these conditions suffer self‐stigma that prevents seeking help. Despite abundant empirical evidence that people with even the most serious mental health conditions can live independently, make their own decisions, and benefit from meaningful activities, including competitive employment, officials in many countries and regions have been slow to adopt and actualize the potentiating philosophy of recovery. Progress for people with disabilities has been painfully slow. However, as Martin Luther King famously stated, “the arc of the moral universe is long, but it bends toward justice.”
CONCLUSIONS
Evidence‐based supported employment (IPS) has fundamentally changed the field of psychiatric rehabilitation by providing the first highly effective employment intervention for people with serious mental illness and documenting that most people who become employed have a significantly better quality of life. As IPS spreads steadily across high‐income countries, innovators are testing the intervention with new populations and in new settings, often using adaptations of uncertain validity. Further research opportunities abound, not just to study IPS in new populations and settings, but also to understand the role of employment and other social determinants on mental health, to examine IPS implementations and modifications scientifically, and to develop economic, training, supervisory, and quality assurance structures that are needed to implement and sustain IPS broadly.
AUTHORS CONTRIBUTIONS
The two authors contributed equally to the preparation of the paper, including drafting and editing the manuscript. Gary R. Bond prepared the tables and the figure.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS APPROVAL STATEMENT
The authors did not conduct any new research with human subjects in the preparation of this review paper and therefore this work did not require review by an institutional review board.
PATIENT CONSENT STATEMENT
N/A.
CLINICAL TRIAL REGISTRATION
N/A.
ACKNOWLEDGMENTS
This was an invited paper for which the authors received an honorarium. The authors received no other financial support for preparing this paper.
Drake RE, Bond GR. Individual placement and support: history, current status, and future directions. Psychiatry Clin Neurosci Rep. 2023;2:e122. 10.1002/pcn5.122
DATA AVAILABILITY STATEMENT
N/A.
REFERENCES
- 1. Drake RE, Wallach MA. Employment is a critical mental health intervention. Epidemiol Psychiat Sci. 2020;29:e178. 10.1017/S2045796020000906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Modini M, Joyce S, Mykletun A, Christensen H, Bryant RA, Mitchell PB, et al. The mental health benefits of employment: results of a systematic meta‐review. Australas Psychiat. 2016;24:331–6. [DOI] [PubMed] [Google Scholar]
- 3. Bond GR, Drake RE. Making the case for IPS supported employment. Adm Policy Ment Health. 2014;41:69–73. [DOI] [PubMed] [Google Scholar]
- 4. Perkins R, Rinaldi M. Unemployment rates among patients with long‐term mental health problems: a decade of rising unemployment. Psychiatr Bull R Coll Psychiat. 2002;26:295–8. [Google Scholar]
- 5. Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, et al. Barriers to employment for people with schizophrenia. Am J Psychiat. 2006;163:411–7. [DOI] [PubMed] [Google Scholar]
- 6. Salkever DS, Karakus MC, Slade EP, Harding CM, Hough RL, Rosenheck RA, et al. Measures and predictors of community‐based employment and earnings of persons with schizophrenia in a multisite study. Psychiat Serv. 2007;58:315–24. [DOI] [PubMed] [Google Scholar]
- 7. Hakulinen C, Elovainio M, Arffman M, Lumme S, Suokas K, Pirkola S, et al. Employment status and personal income before and after onset of a severe mental disorder: a case‐control study. Psychiat Serv. 2020;71:250–5. [DOI] [PubMed] [Google Scholar]
- 8. Becker DR, Drake RE. A working life: the Individual Placement and Support (IPS) Program. Concord, NH: New Hampshire‐Dartmouth Psychiatric Research Center; 1993. [Google Scholar]
- 9. Goldman HH. Epidemiology. In: Talbott JA (ed.). The chronic mental patient: Five years later. Orlando, FL: Grune & Stratton; 1984. p.15–31. [Google Scholar]
- 10. Anthony WA. The principles of psychiatric rehabilitation. Baltimore: University Park Press; 1979. [Google Scholar]
- 11. Black BJ. Work and mental illness: Transitions to employment. Baltimore: Johns Hopkins Press; 1988. [Google Scholar]
- 12. Bond GR. Vocational rehabilitation. In: Liberman RP (ed.). Handbook of psychiatric rehabilitation. New York: Macmillan; 1992. p.244–275. [Google Scholar]
- 13. Wehman P, Moon MS. (eds.). Vocational rehabilitation and supported employment. Baltimore: Paul Brookes; 1988. [Google Scholar]
- 14. Bailey EL, Ricketts SK, Becker DR, Xie H, Drake RE. Do long‐term day treatment clients benefit from supported employment? Psychiat Rehabil J. 1998;22(1):24–9. [Google Scholar]
- 15. Drake RE, Becker DR, Biesanz JC, Torrey WC, McHugo GJ, Wyzik PF. Rehabilitative day treatment vs. supported employment: I. Vocational outcomes. Community Ment Health J. 1994;30:519–32. [DOI] [PubMed] [Google Scholar]
- 16. Drake RE, Becker DR, Biesanz JC, Wyzik PF, Torrey WC. Day treatment versus supported employment for persons with severe mental illness: a replication study. Psychiat Serv. 1996;47:1125–7. [DOI] [PubMed] [Google Scholar]
- 17. Drake RE, McHugo GJ, Becker DR, Anthony WA, Clark RE. The New Hampshire study of supported employment for people with severe mental illness. J Consult Clin Psychol. 1996;64:391–9. [DOI] [PubMed] [Google Scholar]
- 18. Drake RE, McHugo GJ, Bebout RR, Becker DR, Harris M, Bond GR, et al. A randomized clinical trial of supported employment for inner‐city patients with severe mental disorders. Arch Gen Psychiat. 1999;56:627–3. [DOI] [PubMed] [Google Scholar]
- 19. Swanson SJ, Becker DR, Bond GR, Drake RE. The IPS supported employment approach to help young people with work and school: a practitioner's guide. Rockville, MD: IPS Employment Center, Westat; 2017. [Google Scholar]
- 20. Swanson SJ, Becker DR. IPS supported employment: 2022 update to The Practical Guide. New York, NY: IPS Employment Center, Research Foundation for Mental Hygiene; 2022. [Google Scholar]
- 21. Bond GR, Becker DR, Drake RE, Vogler KM. A fidelity scale for the Individual Placement and Support model of supported employment. Rehabil Couns Bull. 1997;40:265–84. [Google Scholar]
- 22. Becker DR, Swanson S, Reese SL, Bond GR, McLeman BM. Supported employment fidelity review manual. 4th ed. Lebanon, NH: IPS Employment Center; 2019. [Google Scholar]
- 23. Bond GR, Peterson AE, Becker DR, Drake RE. Validation of the revised Individual Placement and Support Fidelity Scale (IPS‐25). Psychiatr Serv. 2012;63:758–63. [DOI] [PubMed] [Google Scholar]
- 24. de Winter L, Couwenbergh C, van Weeghel J, Bergmans C, Bond GR. Fidelity and IPS: does quality of implementation predict vocational outcomes over time for organizations treating persons with severe mental illness in the Netherlands? Soc Psychiat Epidemiol. 2020;55:1607–17. [DOI] [PubMed] [Google Scholar]
- 25. Kim SJ, Bond GR, Becker DR, Swanson SJ, Langfitt‐Reese S. Predictive validity of the Individual Placement and Support Fidelity Scale (IPS‐25): a replication study. J Vocat Rehab. 2015;43:209–16. [Google Scholar]
- 26. Yamaguchi S, Sato S, Shiozawa T, Matsunaga A, Ojio Y, Fujii C. Predictive association of low‐ and high‐fidelity supported employment programs with multiple outcomes in a real‐world setting: a prospective longitudinal multi‐site study. Adm Policy Ment Health. 2022;49:255–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pogue JA, Bond GR, Drake RE, Becker DR, Logsdon SM. Growth of IPS supported employment programs in the United States: an update. Psychiat Serv. 2022;73:533–8. [DOI] [PubMed] [Google Scholar]
- 28. Yamaguchi S, Sato S, Ojio Y, Shiozawa T, Matsunaga A, Taneda A, et al. Assessing stable validity and reliability of the Japanese version of the individualized supported employment fidelity scale: a replication. Neuropsychopharmacol Rep. 2021;41:248–54. 10.1002/npr2.12172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Becker DR, Drake RE, Bond GR. The IPS supported employment learning collaborative. Psychiatr Rehabil J. 2014;37:79–85. [DOI] [PubMed] [Google Scholar]
- 30. Becker DR, Drake RE, Bond GR, Nawaz S, Haslett WR, Martinez RA. Best practices: a national mental health learning collaborative on supported employment. Psychiat Serv. 2011;62:704–6. [DOI] [PubMed] [Google Scholar]
- 31. Johnson‐Kwochka A, Bond GR, Becker DR, Drake RE, Greene MA. Prevalence and quality of Individual Placement and Support (IPS) supported employment in the United States. Adm Policy Ment Health Serv Res. 2017;44:311–9. [DOI] [PubMed] [Google Scholar]
- 32. Drake RE, Becker DR, Bond GR. Growth and sustainment of individual placement and support. Psychiatr Serv. 2020;71:1075–7. [DOI] [PubMed] [Google Scholar]
- 33. Jónasson H, van Weeghel J, Koatz D, Johnston G, Bejerholm U, Fioritti A. Boosting the development of individual placement and support in Europe. Epidemiol Psychiat Sci. 2022;31:e29. [Google Scholar]
- 34. Saracco R. Individual Placement and Support (IPS) for serious mental illness in Jalisco, Mexico. NIMH Grant 1R34MH131240‐01.2023.
- 35. Mueser KT, McGurk SR, Khare C, Spencer R, Abhivant N. Adapting the Individual Placement and Support (IPS) model of supported employment for people with severe mental illnesses for the cultural context of India. 2023.
- 36. Drake RE, Bond GR, Becker DR. Individual Placement and Support: an evidence‐based approach to supported employment. New York: Oxford University Press; 2012. [Google Scholar]
- 37. Bond GR. Principles of the Individual Placement and Support model: empirical support. Psychiat Rehabil J. 1998;22(1):11–23. [Google Scholar]
- 38. Bond GR. Supported employment: evidence for an evidence‐based practice. Psychiat Rehabil J. 2004;27:345–359. [DOI] [PubMed] [Google Scholar]
- 39. Bond GR, Mueser KT. Supported employment. In: Sowers WE, McQuistion HL, Ranz JM, Feldman JM, Runnels PS, (eds.). Textbook of community psychiatry. 2nd ed. New York: Springer; 2022. pp.513–24. [Google Scholar]
- 40. Drake RE, Bond GR, Mascayano F. Modification of the Individual Placement and Support model of supported employment. Psychiat Serv. 2023;74:656–8. 10.1176/appi.ps.20220484 [DOI] [PubMed] [Google Scholar]
- 41. Bond GR, Drake RE, Mueser KT, Becker DR. An update on supported employment for people with severe mental illness. Psychiat Serv. 1997;48:335–46. [DOI] [PubMed] [Google Scholar]
- 42. Marshall T, Goldberg RW, Braude L, Dougherty RH, Daniels AS, Ghose SS, et al. Supported employment: assessing the evidence. Psychiat Serv. 2014;65:16–23. [DOI] [PubMed] [Google Scholar]
- 43. Crowther RE. Helping people with severe mental illness to obtain work: systematic review. BMJ. 2001;322:204–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kinoshita Y, Furukawa TA, Omori IM, Marshall M, Bond GR, Huxley P, et al. Supported employment for adults with severe mental illness. Cochrane Database Syst Rev. 2010;2013(9):CD008297. 10.1002/14651858.CD008297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bond GR. “Evidence for IPS” powerpoint: Reference list. https://ipsworks.org/index.php/evidence-for-ips/. 2023.
- 46. Levack WMM, Fadyl JK. Vocational interventions to help adults with long‐term health conditions or disabilities gain and maintain paid work: an overview of systematic reviews. BMJ Open. 2021;11(12):e049522. [Google Scholar]
- 47. Bond GR, Drake RE, Pogue JA. Expanding Individual Placement and Support to populations with conditions and disorders other than serious mental illness. Psychiat Serv. 2019;70:488–98. [DOI] [PubMed] [Google Scholar]
- 48. Bond GR, Al‐Abdulmunem M, Marbacher J, Christensen TN, Sveinsdottir V, Drake RE. A systematic review and meta‐analysis of IPS supported employment for young adults with mental health conditions. Adm Policy Ment Health. 2023;50:160–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. de Winter L, Couwenbergh C, van Weeghel J, Sanches S, Michon H, Bond GR. Who benefits from Individual Placement and Support? A meta‐analysis. Epidemiol Psychiat Sci. 2022;31:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Metcalfe JD, Drake RE, Bond GR. Economic, labor, and regulatory moderators of the effect of Individual Placement and Support among people with severe mental illness: a systematic review and meta‐analysis. Schizophr Bull. 2018;44:22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Modini M, Tan L, Brinchmann B, Wang MJ, Killackey E, Glozier N, et al. Supported employment for people with severe mental illness: systematic review and meta‐analysis of the internationalevidence. Br J Psychiat. 2016;209:14–22. [DOI] [PubMed] [Google Scholar]
- 52. Carmona V, Gómez‐Benito J, Huedo‐Medina T, Rojo J. Employment outcomes for people with schizophrenia spectrum disorder: a meta‐analysis of randomized controlled trials. Int J Occup Med Environ Health. 2017;30:345–66. [DOI] [PubMed] [Google Scholar]
- 53. Suijkerbuijk YB, Schaafsma FG, van Mechelen JC, Ojajärvi A, Corbière M, Anema JR. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta‐analysis. Cochrane Database Syst Rev. 2017;2017(Issue 9):CD011867. 10.1002/14651858.CD011867.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Frederick DE, VanderWeele TJ. Supported employment: meta‐analysis and review of randomized controlled trials of individual placement and support. PLoS One. 2019;14(2):e0212208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Brinchmann B, Widding‐Havneraas T, Modini M, Rinaldi M, Moe CF, McDaid D, et al. A meta‐regression of the impact of policy on the efficacy of Individual Placement and Support. Acta Psychiat Scand. 2020;141:206–20. [DOI] [PubMed] [Google Scholar]
- 56. Weld‐Blundell I, Shields M, Devine A, Dickinson H, Kavanagh A, Marck C. Vocational interventions to improve employment participation of people with psychosocial disability, autism and/or intellectual disability: a systematic review. Int J Environ Res Public Health. 2021;18(22):12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Muñoz‐Murillo A, Esteban E, Ávila C, Fheodoroff K, Haro J, Leonardi M, et al. Furthering the evidence of the effectiveness of employment strategies for people with mental disorders in Europe: a systematic review. Int J Environ Res Public Health. 2018;15:838. 10.3390/ijerph15050838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pinto AD, Hassen N, Craig‐Neil A. Employment interventions in health settings: a systematic review and synthesis. Ann Fam Med. 2018;16:447–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Richter D, Hoffmann H. Effectiveness of supported employment in non‐trial routine implementation: systematic review and meta‐analysis. Soc Psychiatry Psychiat Epidemiol. 2019;54:525–31. [DOI] [PubMed] [Google Scholar]
- 60. Bond GR, Drake RE, Becker DR. Generalizability of the Individual Placement and Support (IPS) model of supported employment outside the US. World Psychiat. 2012;11:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Bond GR, Campbell K, Drake RE. Standardizing measures in four domains of employment outcomes for individual placement and support. Psychiat Serv. 2012;63:751–7. [DOI] [PubMed] [Google Scholar]
- 62. Hellström L, Pedersen P, Christensen TN, Wallstroem IG, Bojesen AB, Stenager E, et al. Vocational outcomes of the Individual Placement and Support model in subgroups of diagnoses, substance abuse, and forensic conditions: a systematic review and analysis of pooled original data. J Occup Rehabil. 2021;31:699–710. [DOI] [PubMed] [Google Scholar]
- 63. Kukla M, Bond GR. A randomized controlled trial of evidence‐based supported employment: nonvocational outcomes. J Vocat Rehab. 2013;38:91–98. [Google Scholar]
- 64. Drake RE, Frey W, Bond GR, Goldman HH, Salkever D, Miller A, et al. Assisting Social Security Disability Insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. Am J Psychiat. 2013;170:1433–41. [DOI] [PubMed] [Google Scholar]
- 65. Mueller L, Wolfe WR, Neylan TC, McCaslin SE, Yehuda R, Flory JD, et al. Positive impact of IPS supported employment on PTSD‐related occupational‐psychosocial functional outcomes: results from a VA randomized‐controlled trial. Psychiat Rehabil J. 2019;42:246–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gibbons BJ, Salkever DS. Working with a severe mental illness: estimating the causal effects of employment on mental health status and total mental health costs. Adm Policy Ment Health Serv Res. 2019;46:474–87. [DOI] [PubMed] [Google Scholar]
- 67. Luciano A, Bond GR, Drake RE. Does employment alter the course and outcome of schizophrenia and other severe mental illnesses? A systematic review of longitudinal research. Schizophrenia Res. 2014;159:312–21. [DOI] [PubMed] [Google Scholar]
- 68. Wallstroem IG, Pedersen P, Christensen TN, Hellström L, Bojesen AB, Stenager E, et al. A systematic review of Individual Placement and Support, employment, and personal and clinical recovery. Psychiat Serv. 2021;72:1040–7. [DOI] [PubMed] [Google Scholar]
- 69. Blustein DL. The role of work in psychological health and well‐being: a conceptual, historical, and public policy perspective. Am Psychol. 2008;63:228–40. [DOI] [PubMed] [Google Scholar]
- 70. Butterworth P, Leach LS, Strazdins L, Olesen SC, Rodgers B, Broom DH. The psychosocial quality of work determines whether employment has benefits for mental health: results from a longitudinal national household panel survey. Occup Environ Med. 2011;68:806–12. [DOI] [PubMed] [Google Scholar]
- 71. Pohrt A, Fodor D, Burr H, Kendel F. Appreciation and job control predict depressive symptoms: results from the Study on Mental Health at Work. Int Arch Occup Environ Health. 2021;95:377–387. 10.1007/s00420-021-01735-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Waddell G, Burton AK. Is work good for your health and well‐being? London: The Stationery Office; 2006. [Google Scholar]
- 73. Campbell K, Bond GR, Drake RE. Who benefits from supported employment: a meta‐analytic study. Schizophr Bull. 2011;37:370–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Campbell K, Bond GR, Drake RE, McHugo GJ, Xie H. Client predictors of employment outcomes in high‐fidelity supported employment: a regression analysis. J Nerv Ment Dis. 2010;198:556–63. [DOI] [PubMed] [Google Scholar]
- 75. Metcalfe JD, Drake RE, Bond GR. Predicting employment in the Mental Health Treatment Study: do client factors matter? Adm Policy Ment Health Serv Res. 2017;44:345–53. [DOI] [PubMed] [Google Scholar]
- 76. Bond GR, Mascayano F, Metcalfe JD, Riley J, Drake RE. Access, retention, and effectiveness of Individual Placement and Support in the U.S.: are there racial or ethnic differences? J Vocat Rehab. 2023, 58. 175–185 [Google Scholar]
- 77. Drake RE, Becker DR, Bond GR. Introducing Individual Placement and Support (IPS) supported employment in Japan. Psychiatry Clin Neurosci. 2019;73:47–49. [DOI] [PubMed] [Google Scholar]
- 78. Burns T, Catty J, Becker T, Drake RE, Fioritti A, Knapp M, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370:1146–52. [DOI] [PubMed] [Google Scholar]
- 79. Al‐Abdulmunem M, Drake RE, Carpenter‐Song E. Evidence‐based supported employment in the rural United States: challenges and adaptations. Psychiat Serv. 2021;72:712–5. [DOI] [PubMed] [Google Scholar]
- 80. Bond GR, Al‐Abdulmunem M, Becker DR, Drake RE. Implementing Individual Placement and Support in rural communities: barriers and strategies. ASPIRE Issue Brief. 2022. https://ipsworksorg/wp-content/uploads/2023/03/22-ASPIRE-rural-Issue-Briefpdf
- 81. Luciano A, Bond GR, Drake RE, Becker DR. Is high fidelity to supported employment equally attainable in small and large communities? Community Ment Health J. 2014;50:46–50. [DOI] [PubMed] [Google Scholar]
- 82. Haslett WR, Drake RE, Bond GR, Becker DR, McHugo GJ. Individual Placement and Support: does rurality matter? Am J Psychiat Rehab. 2011;14:237–44. [Google Scholar]
- 83. Metcalfe JD, Riley J, McGurk S, Hale T, Drake RE, Bond GR. Comparing predictors of employment in Individual Placement and Support: a longitudinal analysis. Psychiat Res. 2018;264:85–90. [DOI] [PubMed] [Google Scholar]
- 84. Becker D, Whitley R, Bailey EL, Drake RE. Long‐term employment trajectories among participants with severe mental illness in supported employment. Psychiat Serv. 2007;58:922–928. [DOI] [PubMed] [Google Scholar]
- 85. Hoffmann H, Jäckel D, Glauser S, Mueser KT, Kupper Z. Long‐term effectiveness of supported employment: 5‐year follow‐up of a randomized controlled trial. Am J Psychiat. 2014;171:1183–90. [DOI] [PubMed] [Google Scholar]
- 86. Salyers MP, Becker DR, Drake RE, Torrey WC, Wyzik PF. A ten‐year follow‐up of a supported employment program. Psychiat Serv. 2004;55:302–8. [DOI] [PubMed] [Google Scholar]
- 87. Baller JB, Blyler CR, Bronnikov S, Xie H, Bond GR, Filion K, et al. Long‐term follow‐up of a randomized trial of supported employment for SSDI beneficiaries with mental illness. Psychiatr Serv. 2020;71:243–9. [DOI] [PubMed] [Google Scholar]
- 88. Clark RE, Bush PW, Becker DR, Drake RE. A cost‐effectiveness comparison of supported employment and rehabilitative day treatment. Adm Policy Ment Health. 1996;24:63–77. [Google Scholar]
- 89. Clark RE, Xie H, Becker DR, Drake RE. Benefits and costs of supported employment from three perspectives. J Behav Health Serv Res. 1998;25:22–34. [DOI] [PubMed] [Google Scholar]
- 90. Dixon L, Hoch JS, Clark R, Bebout R, Drake R, McHugo G, et al. Cost‐effectiveness of two vocational rehabilitation programs for persons with severe mental illness. Psychiat Serv. 2002;53:1118–24. [DOI] [PubMed] [Google Scholar]
- 91. Jordan N, Stroupe KT, Richman J, Pogoda TK, Cao L, Kertesz S, et al. Comparing service use and costs of Individual Placement and Support with usual vocational services for Veterans With PTSD. Psychiat Serv. 2022;73:1109–16. [DOI] [PubMed] [Google Scholar]
- 92. Latimer EA, Bush PW, Becker DR, Drake RE, Bond GR. The cost of high‐fidelity supported employment programs for people with severe mental illness. Psychiat Serv. 2004;55:401–6. [DOI] [PubMed] [Google Scholar]
- 93. Salkever D. Social costs of expanding access to evidence‐based supported employment: concepts and interpretive review of evidence. Psychiat Serv. 2013;64:111–9. [DOI] [PubMed] [Google Scholar]
- 94. U.S. Bureau of Labor Statistics . CPI inflation calculator. https://www.bls.gov/data/inflation_calculator.htm2022.
- 95. Bond GR, Kukla M. Impact of follow‐along support on job tenure in the Individual Placement and Support model. J Nerv Ment Dis. 2011;199:150–5. [DOI] [PubMed] [Google Scholar]
- 96. Burns T, Yeeles K, Langford O, Montes MV, Burgess J, Anderson C. A randomised controlled trial of time‐limited individual placement and support: IPS‐LITE trial. Br J Psychiat. 2015;207:351–6. [DOI] [PubMed] [Google Scholar]
- 97. Rössler W, Kawohl W, Nordt C, Haker H, Rüsch N, Hengartner MP. ‘Placement budgets’ for supported employment: impact on employment rates in a multicentre randomised controlled trial. Br J Psychiat. 2020;216:308–13. [DOI] [PubMed] [Google Scholar]
- 98. Clark RE. Supported employment and managed care: can they coexist? Psychiatr Rehabil J. 1998;22(1):62–68. [Google Scholar]
- 99. Rosenheck RA, Estroff SE, Sint K, Lin H, Mueser KT, Robinson DG, et al. Incomes and outcomes: Social Security disability benefits in first‐episode psychosis. Am J Psychiat. 2017;174:886–894. [DOI] [PubMed] [Google Scholar]
- 100. Bond GR, Kim SJ, Becker DR, Swanson SJ, Drake RE, Krzos IM, et al. A controlled trial of supported employment for people with severe mental illness and justice involvement. Psychiat Serv. 2015;66:1027–34. [DOI] [PubMed] [Google Scholar]
- 101. Fan ZJ, Lucenko BA, Estee S, Felver BE, Black C, Mancuso D, et al. Improving employment outcomes for people with mental health disorders in Washington state. Salem, OR: Washington State Department of Social and Health Services; 2016. https://wwwdshswagov/sites/default/files/rda/reports/research-11-230pdf [Google Scholar]
- 102. Zheng K, Stern BZ, Wafford QE, Kohli‐Lynch CN. Trial‐based economic evaluations of supported employment for adults with severe mental illness: a systematic review. Adm Policy Ment Health. 2022;49:440–52. [DOI] [PubMed] [Google Scholar]
- 103. Howard LM, Heslin M, Leese M, McCrone P, Rice C, Jarrett M, et al. Supported employment: randomised controlled trial. British J Psychiat J Ment Sci. 2010;196:404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Stroupe KT, Jordan N, Richman J, Bond GR, Pogoda TK, Cao L, et al. Cost‐effectiveness of Individual Placement and Support compared to Transitional Work Program for veterans with post‐traumatic stress disorder. Adm Policy Ment Health Serv Res. 2022;49:429–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Heslin M, Howard L, Leese M, McCrone P, Rice C, Jarrett M, et al. Randomized controlled trial of supported employment in England: 2 year follow‐up of the Supported Work and Needs. World Psychiat. 2011;10:132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Shi Y. Cost‐effectiveness of the individual placement and support model of supported employment for people with severe mental illness: results from a Canadian randomized trial. Montreal, CA: McGill University; 2012. [Google Scholar]
- 107. Knapp M, Patel A, Curran C, Latimer E, Catty J, Becker T, et al. Supported employment: cost‐effectiveness across six European sites. World Psychiat. 2013;12:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Yamaguchi S, Sato S, Horio N, Yoshida K, Shimodaira M, Taneda A, et al. Cost‐effectiveness of cognitive remediation and supported employment for people with mental illness: a randomized controlled trial. Psychol Med. 2017;47:53–65. [DOI] [PubMed] [Google Scholar]
- 109. Christensen TN, Kruse M, Hellström L, Eplov LF. Cost‐utility and cost‐effectiveness of Individual Placement Support and cognitive remediation in people with severe mental illness: results from a randomised clinical trial. Eur Psychiat. 2021;64:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Yamaguchi S, Mizuno M, Sato S, Matsunaga A, Sasaki N, Shimodaira M, et al. Contents and intensity of services in low‐ and high‐fidelity programs for supported employment: results of a longitudinal survey. Psychiat Serv. 2020;71:472–9. [DOI] [PubMed] [Google Scholar]
- 111. Salkever D, Gibbons B, Ran X. Do comprehensive, coordinated, recovery‐oriented services alter the pattern of use of treatment services? Mental Health Treatment Study impacts on SSDI beneficiaries' use of inpatient, emergency, and crisis services. J Behav Health Serv Res. 2014;41:434–46. [DOI] [PubMed] [Google Scholar]
- 112. Bush PW, Drake RE, Xie H, McHugo GJ, Haslett WR. The long‐term impact of employment on mental health service use and costs for persons with severe mental illness. Psychiat Serv. 2009;60:1024–1031. [DOI] [PubMed] [Google Scholar]
- 113. Bond GR, Lockett H, van Weeghel J. International growth of Individual Placement and Support. Epidemiol Psychiat Sci. 2020;29:e183. 10.1017/S2045796020000955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Becker DR, Bond GR. Commentary on special issue on individual placement and support (IPS) international. Psychiat Rehabil J. 2020;43:79–82. [DOI] [PubMed] [Google Scholar]
- 115. SAMHSA . NSDUH detailed tables: Table 8.5B – Serious mental illness in past year among persons aged 18 or older, by age group and demographic characteristics: percentages, 2018 and 2019. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2019. [Google Scholar]
- 116. Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am J Public Health. 2002;92:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Brucker DL, Houtenville AJ. People with disabilities in the United States. Arch Phys Med Rehabil. 2015;96:771–4. [DOI] [PubMed] [Google Scholar]
- 118. Bejerholm U, Larsson ME, Johanson S. Supported employment adapted for people with affective disorders: a randomized controlled trial. J Affect Disord. 2017;207:212–20. [DOI] [PubMed] [Google Scholar]
- 119. Davis LL, Kyriakides TC, Suris AM, Ottomanelli LA, Mueller L, Parker PE, et al. Effect of evidence‐based supported employment vs transitional work on achieving steady work among veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatr. 2018;75:316–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Davis LL, Leon AC, Toscano R, Drebing CE, Ward LC, Parker PE, et al. A randomized controlled trial of supported employment among veterans with posttraumatic stress disorder. Psychiat Serv. 2012;63:464–70. [DOI] [PubMed] [Google Scholar]
- 121. Davis LL, Mumba MN, Toscano R, Pilkinton P, Blansett CM, McCall K, et al. A randomized controlled trial evaluating the effectiveness of supported employment integrated in primary care. Psychiat Serv. 2022;73:620–7. [DOI] [PubMed] [Google Scholar]
- 122. Hellström L, Bech P, Hjorthøj C, Nordentoft M, Lindschou J, Eplov LF. Effect on return to work or education of Individual Placement and Support modified for people with mood and anxiety disorders: results of a randomised clinical trial. Occup Environ Med. 2017;74:717–25. [DOI] [PubMed] [Google Scholar]
- 123. LePage JP, Lewis AA, Crawford AM, Parish JA, Ottomanelli L, Washington EL, et al. Incorporating Individualized Placement and Support principles into vocational rehabilitation for formerly incarcerated veterans. Psychiat Serv. 2016;67:735–42. [DOI] [PubMed] [Google Scholar]
- 124. LePage JP, Crawford AM, Cipher DJ, Anderson K, Rock A, Johnson JAP, et al. Blending traditional vocational services and Individualized Placement and Support for formerly incarcerated veterans. Psychiat Serv. 2020;71:816–23. [DOI] [PubMed] [Google Scholar]
- 125. Lones CE, Bond GR, McGovern MP, Carr K, Leckron‐Myers T, Hartnett T, et al. Individual Placement and Support (IPS) for methadone maintenance therapy patients: a pilot randomized controlled trial. Adm Policy Ment Health Serv Res. 2017;44:359–64. [DOI] [PubMed] [Google Scholar]
- 126. Ottomanelli L, Barnett SD, Goetz LL. Effectiveness of supported employment for veterans With spinal cord injury: 2‐year results. Arch Phys Med Rehabil. 2014;95:784–90. [DOI] [PubMed] [Google Scholar]
- 127. Reme SE, Grasdal AL, Løvvik C, Lie SA, Øverland S. Work‐focused cognitive–behavioural therapy and individual job support to increase work participation in common mental disorders: a randomised controlled multicentre trial. Occup Environ Med. 2015;72:745–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Reme SE, Monstad K, Fyhn T, Sveinsdottir V, Løvvik C, Lie SA, et al. A randomized controlled multicenter trial of individual placement and support for patients with moderate to severe mental illness. Scand J Work Environ Health. 2019;45:33–41. [DOI] [PubMed] [Google Scholar]
- 129. Sveinsdottir V, Lie SA, Bond GR, Eriksen HR, Tveito TH, Grasdal AL, et al. Individual placement and support for young adults at risk of early work disability (the SEED trial). A randomized controlled trial. Scand J Work Environ Health. 2020;46:50–59. [DOI] [PubMed] [Google Scholar]
- 130. Sveinsdottir V, Jacobsen HB, Ljosaa TM, Linnemørken LTB, Knutzen T, Ghiasvand R, et al. The Individual Placement and Support (IPS) in pain trial: a randomized controlled trial of IPS for patients with chronic pain conditions. Pain Med. 2022;23:1757–66. 10.1093/pm/pnac032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Marsden J, Anders P, Clark H, Colocassis K, Eastwood B, Knight J, et al. Protocol for a multi‐centre, definitive randomised controlled trial of the effectiveness of Individual Placement and Support for employment support among people with alcohol and drug dependence. Trials. 2020;21:167. 10.1186/s13063-020-4099-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Rognli EB, Aas EM, Drake RE, Marsden J, Anders P, Bond GR, et al. The effect evaluation of Individual Placement and Support (IPS) for patients with substance use disorders: study protocol for a randomized controlled trial of IPS versus enhanced self‐help. Trials. 2021;22:705. 10.1186/s13063-021-05673-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Sveinsdottir V, Flynn T. Supported Employment for Refugees (SER). Bergen, Norway: Uni Research, Norwegian Labour and Welfare Administration; 2018. https://ClinicalTrials.gov/show/NCT03629366 [Google Scholar]
- 134. Alverson H, Carpenter E, Drake RE. An ethnographic study of job seeking among people with severe mental illness. Psychiat Rehabil J. 2006;30:15–22. [DOI] [PubMed] [Google Scholar]
- 135. Becker DR, Drake RE, Naughton WJ. Supported employment for people with co‐occurring disorders. Psychiat Rehabil J. 2005;28:332–338. [DOI] [PubMed] [Google Scholar]
- 136. SAMHSA . Adapting evidence‐based practices for under‐resourced populations. Publication ID: PEP22‐06‐02‐004. Rockville, MD: National Mental Health and Substance Use Policy Laboratory, Substance Abuse and Mental Health Services Administration; 2022. https://store.samhsa.gov/product/evidence-based-practices-under-resourced-populations/pep22-06-02-004 [Google Scholar]
- 137. Lehman AF, Goldberg R, Dixon LB, McNary S, Postrado L, Hackman A, et al. Improving employment outcomes for persons with severe mental illness. Arch Gen Psychiat. 2002;59:165–72. [DOI] [PubMed] [Google Scholar]
- 138. Gewurtz RE, Cott C, Rush B, Kirsh B. How does outcome‐based funding affect service delivery? An analysis of consequences within employment services for people living with serious mental illness. Adm Policy Ment Health Serv Res. 2015;42:19–28. [DOI] [PubMed] [Google Scholar]
- 139. Freedman L, Elkin S, Millenky M. Breaking barriers: implementing Individual Placement and Support in a workforce setting. New York, NY: MDRC; 2019. https://www.mdrc.org/sites/default/files/BBSD_Final_508.pdf [Google Scholar]
- 140. Killackey E, Allott K, Jackson HJ, Scutella R, Tseng YP, Borland J, et al. Individual placement and support for vocational recovery in first‐episode psychosis: randomised controlled trial. Br J Psychiat. 2019;214:76–82. [DOI] [PubMed] [Google Scholar]
- 141. Latimer E. An effective intervention delivered at sub‐therapeutic dose becomes an ineffective intervention. Br J Psychiat. 2010;196:341–2. [DOI] [PubMed] [Google Scholar]
- 142. Burns AM, Erickson DH. Adding cognitive remediation to employment support services: a randomized controlled trial. Psychiatr Serv. 2022; Online ahead of press. [DOI] [PubMed] [Google Scholar]
- 143. McGurk SR, Mueser KT, Xie H, Welsh J, Kaiser S, Drake RE, et al. Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172:852–61. [DOI] [PubMed] [Google Scholar]
- 144. Christensen TN, Wallstrøm IG, Stenager E, Bojesen AB, Gluud C, Nordentoft M, et al. Effects of Individual Placement and Support supplemented with cognitive remediation and work‐focused social skills training for people with severe mental illness: a randomized clinical trial. JAMA Psychiat. 2019;76:1232–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Twamley EW, Thomas KR, Burton CZ, Vella L, Jeste DV, Heaton RK, et al. Compensatory cognitive training for people with severe mental illnesses in supported employment: a randomized controlled trial. Schizophrenia Res. 2019;203:41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Wilson EO. Consilience: The unity of knowledge. Vintage Books; 1998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A.


