Abstract
Aim
An assertive case management intervention program, ACTION‐J, proved effective for preventing suicide attempters from reattempting suicide within 6 months. The ACTION‐J randomized trial was conducted as part of the “National Strategic Research Projects.” The program has been covered by the national medical payment system of Japan since 2016. The aim of the Post‐ACTION‐J Study (PACS) was to examine the current implementation status of assertive case management in a real‐world clinical setting.
Methods
PACS was a prospective, multicenter registry cohort study. The participants were suicide attempters admitted to the emergency departments of 10 participating medical facilities from October 2016 to September 2018. The assertive case management intervention developed by the ACTION‐J Study was offered to all patients, and the primary outcome was the duration and frequency of use of the intervention at 6 months.
Results
A total of 1159 patients were admitted to emergency departments after a suicide attempt during the study period, 144 of whom were included in our analysis. The proportion of participants who received the intervention for 6 months was 72.2% (104/144), and 63.9% (92/144) of the patients completed ≥7 case management interviews within 6 months.
Conclusion
The findings of this study indicate successful implementation of an assertive case management intervention program based on the ACTION‐J Study in a real‐world clinical setting, following its integration with the national medical payment scheme in Japan. The study provided the useful information that could improve the implementation of assertive case management interventions in future.
Keywords: assertive case management, emergency psychiatry, implementation, medical payment scheme, suicide attempt
INTRODUCTION
A suicide attempt is considered one of the most robust predictors of subsequent attempts and, ultimately, death from suicide. 1 , 2 , 3 Suicidal patients who are severely physically impaired are initially admitted to tertiary emergency departments for physical treatment. Emergency department admission for attempted suicide is increasingly being recognized as an opportunity for medical personnel to intervene and prevent future suicide attempts. 3 , 4 , 5 , 6
The assertive case management intervention program developed by the ACTION‐J Study proved effective for preventing suicide reattempts among suicide attempters over 6 months, according to the results of a randomized controlled multicenter trial. 7 , 8 , 9 The study was conducted as a part of the “National Strategic Research Projects” funded by the Ministry of Health, Labour and Welfare, which aimed to formulate policies to tackle pressing health issues in Japan. The intervention program was integrated into the national medical payment scheme in 2016, based on the favorable results of the study. The payment scheme covers medical fees for continuous assertive case management during hospitalization and once per week thereafter for up to 6 months post‐discharge.
The introduction of evidence‐based interventions for suicide prevention could represent a paradigm shift. The present study examined the current implementation status of the assertive case management intervention program developed by the ACTION‐J Study in a real‐world clinical setting. We investigated the duration and frequency of use of the assertive case management intervention at 6 months after registration.
METHODS
Study design and participants
The Post‐ACTION‐J Study (PACS) is a prospective, multicenter cohort study carried out in 10 general hospitals in Japan, involving both psychiatry and emergency departments. These facilities have case managers who implement the assertive case management intervention program, which involves psychiatrists, social workers, clinical psychologists, occupational therapists, and nurses. This study was carried out in accordance with the research protocol, which has been published previously. 9
The participants in this study were patients admitted to the emergency departments of the participating medical facilities after suicide attempts during the period October 2016–September 2018. The inclusion criteria were as follows: (1) individuals likely to have inflicted self‐injury, as assessed by physicians of the emergency department; (2) individuals with self‐injury who are confirmed as having suicidal intent assessed by at least two psychiatrists; and (3) provision of written informed consent for participation in the assertive case management intervention program. The exclusion criteria were as follows: (1) individuals with impaired consciousness at the time of informed consent; (2) individuals who do not understand Japanese; and (3) individuals who are unsuitable for registration in the present study for any other reasons. 9
General study and data collection procedures
The participants in this study were suicide attempters admitted to the emergency departments of participating medical facilities. Trained psychiatrists checked that the participants met the inclusion and exclusion criteria, provided them with a complete description of the study process, and asked them to give informed consent. Basic patient data were collected first, including initials, ID, age, sex, cohabitation status, marital status, education level, employment status, family history, living with partner or family, and medical history. The psychiatric evaluation was concerned with the index suicide attempt and history of psychiatric care. Moreover, a psychiatric diagnosis was made by at least two psychiatrists in accordance with the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Suicide reattempts, self‐harm, number of attempts survived, and suicidal ideation were assessed and recorded, along with information about psychiatric and medical treatments (including adherence thereto). As psychological measures, the Beck Depression Inventory‐II (BDI‐II) and Columbia‐Suicide Severity Rating Scale (C‐SSRS) were completed at baseline and 6 months after registration. The Buss–Perry Aggression Questionnaire (BAQ) and Barratt Impulsiveness Scale (BIS) were also completed 6 months after registration, in accordance with the study protocol. We plan to publish the results for the BAQ and BIS instruments in a separate report. Data for practice and outcome with the assertive case management intervention were extracted from assertive case management records created by the case managers of the participating hospitals. The study protocol was approved by the Internal Review Board of Sapporo Medical University, and by the local ethics committees of all participating hospitals. This study is registered at UMIN‐CTR (000024474).
Assertive case management intervention
The assertive case management intervention was then offered to participants, on an ongoing basis, by trained case managers. The intervention involved periodic face‐to‐face discussions. The case manager contacted the participants every month during their hospital stay, and after discharge (at least 6 months after registration).
First, the case managers collected information about each participant's treatment status, and any social problems that could impact treatment adherence. Based on that information, they encouraged the participants to adhere to current psychiatric treatment, or to seek treatment again in the event that it had been discontinued. They also scheduled appointments with psychiatrists and primary care physicians, and referred participants to social services and private support organizations as needed. Then they administered semi‐structured psychoeducation developed by the ACTION‐J Study. The interventions include psychoeducation for mental illness in general, but do not provide different psychoeducation for respective psychiatric disorders. After the psychoeducation sessions, participants were provided with information about social resources via a pamphlet. The details of the assertive case management intervention program based on the ACTION‐J Study have been reported previously. 9 , 10
Outcomes
The primary outcome was the duration and frequency of use of the assertive case management intervention at 6 months (24 weeks) after registration. The secondary outcomes were the incidence and proportion of deaths (suicides and death from any cause), recurrence and frequency of suicide attempts and self‐injury, and differences in the C‐SSRS and BDI‐II scores between baseline and 6 months. The assessors were not blinded.
Statistical analysis
We calculated the number, frequency, and percentage data for binary and categorical variables, and mean and standard deviation or median and interquartile range for continuous variables (for patient characteristics and outcome measures postintervention). Odds ratios (ORs) and 95% confidence intervals (CIs) for the primary outcome were calculated via multivariable logistic regression for the following factors: age, sex, cohabitation status, marital status, education, employment status, family history, living with partner or family, BDI‐II score, and psychiatric diagnosis at baseline. We also calculated differences between scores at baseline and 6 months post‐intervention for each outcome when these data were available, such as the C‐SSRS and BDI‐II. One sample T‐test was performed for pre–post difference in additional secondary outcomes. Some of the preplanned analyses could not be performed because of an insufficient number of registered patients or unavailable data. Statistical analysis was performed using SPSS 15.0 J (SPSS Inc.) and JMP 10.0 (SAS Software) software for Windows.
RESULTS
A total of 1159 patients were admitted to the emergency department after a suicide attempt during the study period. Of these patients, 179 (15.4%) died during critical care. The data from one hospital were excluded because of deviations from the study protocol (in terms of auditing and monitoring). Of the 623 patients assessed for eligibility, 228 were excluded because of a short hospital stay, along with 45 who could not be interviewed, 111 who declined to participate in the intervention, and 94 for other reasons, including nonavailability of the necessary study personnel, patients' hope to consult with others and difficulty of management after discharge because of the distance to the patient's home. Among the 198 patients to whom the consent form was distributed, 144 were included in the final analysis (Figure 1).
Figure 1.
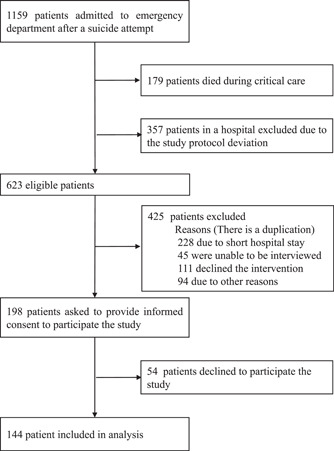
Study flowchart.
Table 1 shows the characteristics of the sample. Of the 144 patients, 89 (61.8%) were female. The mean age was 47.4 ± 20.1 years, and 34 (23.6%) patients were aged >65 years. The primary psychiatric diagnoses were substance‐related disorders (n = 3; 2.1%), schizophrenia or other psychotic disorder (n = 19; 13.2%), mood disorder (n = 82; 56.9%), adjustment disorder (n = 27; 18.8%)and “other” (n = 13; 9%).
Table 1.
Baseline participant characteristics (N = 144).
| N (%) | |
|---|---|
| Sex | |
| Female | 89 (61.8) |
| Male | 55 (38.2) |
| Age (years), mean [SD] | 47.4 [20.1] |
| Aged >65 years | 34 (23.6) |
| Primary psychiatric diagnosis | |
| Substance‐related and addictive disorders | 3 (2.1) |
| Schizophrenia spectrum and other psychotic disorders | 19 (13.2) |
| Depressive disorders and bipolar and related disorders | 82 (56.9) |
| Adjustment disorder | 27 (18.8) |
| Other | 13 (9.0) |
| Timing of appointment with a psychiatrist (before the suicide attempt) | |
| <1 month | 68 (47.2) |
| 1–3 months | 6 (4.2) |
| 4–6 months | 2 (1.4) |
| 7–12 months | 0 (0) |
| >12 months | 6 (4.2) |
| Never | 58 (40.3) |
| Missing data | 4 (2.8) |
| Visited a physician other than a psychiatrist before the suicide attempt | |
| <1 month | 39 (27.1) |
| 1–3 months | 8 (5.6) |
| 4–6 months | 1 (0.7) |
| 7–12 months | 1 (0.7) |
| >12 months | 4 (2.8) |
| Never | 85 (59.0) |
| Missing data | 6 (4.2) |
| Education | |
| <High school | 31 (21.5%) |
| High school | 70 (48.6%) |
| >High school | 40 (27.8%) |
| Missing data | 3 (2.1%) |
| Employment status | |
| Unemployed | 42 (29.2) |
| Employed (full‐time) | 42 (29.2) |
| Employed (part‐time) | 23 (16.0) |
| Retired | 4 (2.8) |
| Student | 12 (8.3) |
| Housewife | 17 (11.8) |
| Sick leave | 3 (2.1) |
| Incapacitated by disability | 1 (1.0) |
| Missing data | 0 |
| Marital status | |
| Married | 50 (34.7) |
| Single | 68 (47.2) |
| Divorced | 19 (13.2) |
| Widowed | 6 (4.2) |
| Missing data | 1 (1.4) |
| Living with partner or family | 110 (76.4) |
| Previous suicide attempts, n | |
| 0 | 82 (56.9) |
| 1–2 | 31 (21.5) |
| ≥3 | 29 (20.1) |
| Missing data | 2 (1.4) |
| Method of the most recent suicide attempt | |
| Drug overdose | 54 (37.5) |
| Laceration | 24 (16.7) |
| Jumping from a height | 20 (13.9) |
| Hanging | 14 (9.7) |
| Poisoning | 13 (9.0) |
| Gas | 8 (5.6) |
| Burning | 3 (2.1) |
| Intentional traffic‐related injury | 1 (0.7) |
| Charcoal burning | 1 (0.7) |
| Drowning | 1 (0.7) |
| Entering a mountainous area with suicidal intent | 1 (0.7) |
| Missing data | 4 (2.8) |
| BDI‐II score, mean [SD] (n = 136) | 26.94 [13.77] |
| C‐SSRS “type” score, mean [SD] (n = 137) | 4.25 [1.1] |
| C‐SSRS “content” score, mean [SD] (n = 136) | 17.46 [5.29] |
Abbreviations: BDI‐II, Beck Depression Inventory‐II; C‐SSRS, Columbia‐Suicide Severity Rating Scale; SD, standard deviation.
Table 2 shows the implementation status and outcomes of the assertive case management intervention program. The duration of the intervention was ≥6 months for 104 (72.2%) patients, <1 month for three (2.1%) patients, and “first interview only” for six (4.2%) patients. In total, 92 (63.9%) patients were interviewed ≥7 times, while six (4.2%) were only interviewed once (at the beginning of the intervention).
Table 2.
Duration (primary outcome) and frequency of use of the assertive case management intervention (N = 144).
| (a) Duration of enrollment in intervention | n (%) |
|---|---|
| ≥6.0 months (primary outcome) | 104 (72.2) |
| 5.0–5.9 months | 7 (4.9) |
| 4.0–4.9 months | 3 (2.1) |
| 3.0–3.9 months | 3 (2.1) |
| 2.0–2.9 months | 9 (6.3) |
| 1.0–1.9 months | 9 (6.3) |
| <1.0 month | 3 (2.1) |
| First interview only | 6 (4.2) |
| (b) Case management interviews, n | n (%) |
|---|---|
| ≥7 | 92 (63.9) |
| 6 | 17 (11.8) |
| 5 | 4 (2.8) |
| 4 | 9 (6.3) |
| 3 | 8 (5.6) |
| 2 | 8 (5.6) |
| 1 | 6 (4.2) |
Table 3 shows the numbers of suicide deaths, deaths from any cause, recurrent suicide attempts, and recurrent episodes of self‐injury. There was only one (0.7%) suicide death during the study period, and three (2.1%) deaths from any cause. Recurrent suicide attempts were observed in 16 (11.1%) patients, and recurrent episodes of self‐injury in 17 (11.8%) patients. Regarding psychiatric treatment adherence, 128 (88.9%) patients received continuous psychiatric treatment throughout the study period, while seven (4.9%) stopped (or did not receive) psychiatric treatment. Of all participants, 58 (40.3%) had no history of psychiatric visits, as shown in Table 1. They were seen by psychiatrists while in the emergency department, and 51 of them continued to visit psychiatrists during the study period.
Table 3.
Secondary outcomes of the assertive case management intervention program (N = 144).
| Outcomes | n (%) |
|---|---|
| Suicide | 1 (0.7) |
| Death from any cause | 3 (2.1) |
| Recurrent suicide attempts, n | 16 (11.1) |
| 1 | 10 |
| 2 | 5 |
| 3 | 0 |
| 4 | 1 |
| 5 | 0 |
| Recurrent self‐injury episodes, n | 17 (11.8) |
| 1 | 7 |
| 2 | 4 |
| 3 | 2 |
| 4 | 3 |
| 5 | 1 |
| Psychiatric treatment adherence | |
| Continuous | 128 (88.9) |
| Stopped or did not receive treatment | 7 (4.9) |
| Missing data | 9 (6.3) |
As shown in Table 4, there was a statistically significant decrease in depression and suicidal ideation scores at 6 months post‐registration (relative to baseline). The mean BDI‐II score was significantly reduced, by 7.37 ± 16.09, while the mean C‐SSRS “type” score was reduced by 2.90 ± 1.93, and the mean C‐SSRS “content” score by 10.85 ± 8.77.
Table 4.
Additional secondary outcomes of the assertive case management intervention program (psychological measures; N = 144).
| Outcomes | Mean (SD) |
|---|---|
| BDI‐II at 6 months (n = 94) | 19.16 (13.75) |
| Pre–post difference (n = 93) | −7.37 (16.09)* |
| C‐SSRS‐type at 6 months (n = 95) | 1.28 (1.55) |
| Pre–post difference (n = 94) | −2.90 (1.93)* |
| C‐SSRS‐content at 6 months (n = 95) | 6.92 (7.00) |
| Pre–post difference (n = 94) | −10.85 (8.77)* |
Abbreviations: BDI‐II, Beck Depression Inventory‐II; C‐SSRS, Columbia‐Suicide Severity Rating Scale; SD, standard deviation.
p ≤ 0.0001.
Finally, we performed multivariate analysis to examine the associations between use of the assertive case management intervention for 6 months (primary outcome) and patient characteristics (Table 5). Schizophrenia spectrum and other psychotic disorders (OR = 0.04, 95% CI: 0.002–0.42), depressive disorders and bipolar and related disorders (OR = 0.01, 95% CI: 0.002–0.58), visiting a physician other than a psychiatrist within 1 month before the suicide attempt (OR = 3.85, 95% CI: 1.24–12.92), and BDI‐II score at baseline (OR = 1.05, 95% CI: 1.01–1.09) were significantly associated with intervention use for 6 months (i.e., “successful implementation”).
Table 5.
Multivariate analysis of the primary outcome measure (duration and frequency of use of the assertive case management intervention) (n = 128).
| Odds ratio | 95% CI | p‐value | ||
|---|---|---|---|---|
| Sex | ||||
| Female | 0.62 | 0.17 | 2.24 | 0.4634 |
| Male | Reference | |||
| Age (10‐year increment) | 0.95 | 0.69 | 1.31 | 0.7493 |
| Primary psychiatric diagnosis | ||||
| Schizophrenia spectrum and other psychotic disorders | 0.04 | 0.002 | 0.42 | 0.0127 |
| Depressive disorders and bipolar and related disorders | 0.09 | 0.01 | 0.58 | 0.0156 |
| Adjustment disorder | 0.14 | 0.02 | 1.03 | 0.0628 |
| Other | Reference | |||
| Visited a psychiatrist within 1 month before the suicide attempt | 1.47 | 0.41 | 5.57 | 0.5574 |
| Visited a physician other than a psychiatrist within 1 month before the suicide attempt | 3.85 | 1.24 | 12.92 | 0.0225 |
| Education | ||||
| <High school | 1.87 | 0.53 | 6.75 | 0.3284 |
| High school | Reference | |||
| >High school | 0.80 | 0.19 | 2.98 | 0.7384 |
| Employment status | ||||
| Unemployed | Reference | |||
| Employed | 1.16 | 0.33 | 4.26 | 0.8197 |
| Other | 0.70 | 0.15 | 2.97 | 0.6284 |
| Marital status | ||||
| Married | 0.74 | 0.18 | 2.97 | 0.6747 |
| Other | Reference | |||
| Living with partner or family | 0.37 | 0.11 | 1.19 | 0.0974 |
| Previous suicide attempts, n | ||||
| 0 | Reference | |||
| 1–2 | 0.23 | 0.04 | 0.94 | 0.0541 |
| ≥3 | 0.28 | 0.06 | 1.23 | 0.1028 |
| Method of suicide attempt at baseline | ||||
| Drug overdose | 0.92 | 0.31 | 2.59 | 0.8705 |
| Other | Reference | |||
| BDI‐II score at baseline (1‐point increment) | 1.05 | 1.01 | 1.09 | 0.0346 |
| C‐SSRS “type” score at baseline (1 point increment) | 1.69 | 0.93 | 3.31 | 0.1013 |
| C‐SSRS “content” score at baseline (1‐point increment) | 0.90 | 0.78 | 1.02 | 0.1076 |
Note: Bold text emphasize statistically significant values.
Abbreviations: BDI‐II, Beck Depression Inventory‐II; CI, confidence interval; C‐SSRS, Columbia‐Suicide Severity Rating Scale.
DISCUSSION
The ACTION‐J Study showed that a 6‐month assertive case management intervention effectively prevented suicide reattempts over 6 months by those with a history of attempts. 7 , 8 , 9 Subsequent secondary analyses of ACTION‐J data also revealed that assertive case management helped prevent suicide reattempts among patients with comorbid DSM‐IV‐TR Axis I and II disorders 11 and those with a history of self‐poisoning, 12 and reduced the overall incidence of self‐harm. 13 The secondary analysis also elucidated the importance of visits to a psychiatrist a short time before the first suicide attempt in men and in women with substance‐related disorder, previous suicide attempts, and drug overdose in the first suicide attempt as predictive factors for future suicide reattempts. 14
The results of the present study indicated successful implementation of the assertive case management intervention program in a real‐world clinical setting. The proportion of suicide attempters in this study who completed the 6‐month assertive case management intervention was 72.2%. Moreover, 63.9% of the participants completed ≥7 case management interviews.
Several studies implemented interventions involving active contact and follow‐up to prevent suicide attempts among patients admitted to emergency departments for suicidal behavior (i.e., during a high‐risk period). 6 , 15 A previous randomized controlled trial (Assertive Intervention for Deliberate Self‐harm [AID]) conducted at one location (Copenhagen University Hospital, Denmark) assessed whether an assertive outreach intervention could reduce the frequency of subsequent suicide attempts relative to standard treatment. 16 In that study, five of 123 participants in the intervention group did not actually receive the intervention, because they withdrew from the study (even though the intervention schedule was flexible). In a recent randomized controlled study (Attempted Suicide Short Intervention Program [ASSIP]) that provided brief therapy based on a patient‐centered model of suicidal behavior, the drop rates for the intervention and control group were 5% and 22% at 12 months, and 7% and 22% at 24 months, respectively. However, the sample size was small. 17 Although the duration of the assertive case management intervention in our study was shorter, it benefited from the use of real‐world data and an intervention model supported by the national medical payment system of Japan.
With respect to the secondary outcomes, recurrent suicide attempts were seen in 11.1% of patients, and recurrent episodes of self‐injury in 11.8%. Recurrent suicidal behavior (attempted or completed suicide) was seen in 25 (6%) of the 417 participants in the ACTION‐J Study at 6 months. The difference in outcomes between our study and ACTION‐J may be attributable to differences in the enrollment criteria. The ACTION‐J Study was limited to suicidal patients aged <20 years; and patients without an Axis I DSM‐IV‐TR disorder as their primary diagnosis were excluded. In this study, almost all suicidal patients admitted to emergency departments were eligible for participation. We also observed a significant reduction in the mean BDI‐II and C‐SSRS scores compared with baseline. These findings suggest that assertive case management interventions could help prevent suicide reattempts. This study also showed that the intervention was able to connect many patients who had no history of psychiatric visits to psychiatric care, which may explain the post‐intervention results of reduced depression and suicidal ideation in addition to the direct effect of the intervention.
As shown in Table 5, “visiting a physician other than a psychiatrist within 1 month before the suicide attempt” was significantly associated with successful implementation. The study by Luoma et al. 18 indicated that approximately 45% of suicide victims have contact with primary care providers within 1 month of suicide. The reason why suicide attempters visited a physician 1 month before the suicide attempt is unknown, but it is possible that they originally had a physical illness and went to the hospital, or that they had somatization symptoms due to a mental illness, such as depression, that they were suffering from and visited a physician. The results suggest that participants who have been treated by a physician may be more careful of their own health or may be more likely to seek help. Therefore, primary care physicians need to be involved as gatekeepers for suicide prevention.
Since the effectiveness of the assertive case management intervention has already been confirmed in a multicenter, randomized controlled trial, 8 the ongoing issue is to disseminate it in clinical practice as much as possible. In this study, only 15% of suicide attempters seen at emergency departments consented to case management, similar to the ACTION‐J Study. It is understandable that the proportions of suicide attempters who eventually die, do not recover consciousness, or are transferred to other hospitals without physical recovery are relatively high in tertiary emergency centers; for such patients, assertive case management is obviously unsuitable.
The short hospitalization period was another commonly cited reason for non‐enrollment in both studies. Tertiary emergency departments have always been important places for contact with suicide attempters and for performing intensive intervention, but at the same time, developing a system in order to implement care for suicide attempters has been also an important task. The intervention would require strong collaborations between case managers, psychiatrists and emergency medical physicians; and the interventions may be difficult to implement without adequate medical staff resources. In general, patients are transferred as soon as they are out of a life‐threatening condition in the emergency department, therefore sufficient time may not be available for the case management intervention. In order to be able to provide the assertive case management with more patients, it is necessary for emergency department staff and case managers to cooperate to fully understand the details and effects of the intervention to patients with suicide attempts and their families, and to increase the number of consents, even during the short period of stay in the emergency department.
Also, it is important that there are strong collaborations between the hospital where the intervention is delivered and the supporters as medical and welfare services in the community for the implementation. The reason is that the intervention aims to connect patients to the supporters in the community and to enable the patients to obtain help from the supporters continuously. 10
The main limitation of this study was that the sample size was relatively small, which reduced the statistical power. Furthermore, we could not register additional participants (relative to the number stipulated in the original protocol). Future studies involving more facilities and patients are needed to monitor the implementation status of assertive case management interventions aimed at preventing suicide reattempts in Japan. In addition, this study may not reflect the accurate implementation status because of excluding the patients who do not agree to participate in the study although we investigated the current implementation status of the assertive case management in a real‐world clinical setting. Especially in the emergency department, it may not be possible to take enough time to obtain informed consent to the study. The assertive case management reimbursement was increased in April 2021; further research is needed to determine the impact of this change. Finally, differences in the quality of case management among facilities may have affected the results; we plan to report data pertaining to the quality of case management in a future study.
This study assessed the implementation status of an assertive case management intervention based on the ACTION‐J Study and national medical payment system. The present study demonstrated the potential utility of such interventions in real clinical settings and provided useful information that could improve the implementation of assertive case management interventions in future.
AUTHOR CONTRIBUTION
Takao Ishii, Naohiro Yonemoto, and Chiaki Kawanishi designed the study and wrote the protocol. Mitsuhiko Yamada, Hirokazu Tachikawa, and Chiaki Kawanishi were involved in the conceptualization of the study. Yasushi Otaka, Kazuya Okamura, Noa Tsujii, Kotaro Otsuka, Reiji Yoshimura, Toshihiko Kinoshita, Daisuke Fujisawa, and Satoshi Hashimoto collected the data. Naohiro Yonemoto and Yusuke Tsuyama undertook the statistical analysis. Takao Ishii and Naohiro Yonemoto wrote the first draft of the manuscript. All of the authors contributed to and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS APPROVAL STATEMENT
The study protocol was approved by the Internal Review Board of Sapporo Medical University, and by the local ethics committees of all participating hospitals.
PATIENT CONSENT STATEMENT
Written informed consent has been obtained from all individuals included in this study.
CLINICAL TRIAL REGISTRATION
This study is registered at UMIN‐CTR (000024474).
ACKNOWLEDGMENTS
We thank Michael Irvine, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript. This study was supported by AMED under Grant Number JP18dk0307057.
Ishii T, Yonemoto N, Otaka Y, Okamura K, Tsujii N, Otsuka K, et al. Implementations of an evidence‐based assertive case management intervention for suicide attempters: Post‐ACTION‐J Study (PACS). Psychiatry Clin Neurosci Rep. 2023;2:e106. 10.1002/pcn5.106
DATA AVAILABILITY STATEMENT
The datasets generated during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Da Cruz D, Pearson A, Saini P, Miles C, While D, Swinson N, et al. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011;28(6):467–71. [DOI] [PubMed] [Google Scholar]
- 2. Nordentoft M. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68(10):1058–64. [DOI] [PubMed] [Google Scholar]
- 3. Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: even more lethal than we knew. Am J Psychiatry. 2016; 173(11):1094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. D'Onofrio G, Jauch E, Jagoda A, Allen MH, Anglin D, Barsan WG, et al. NIH roundtable on opportunities to advance research on neurologic and psychiatric emergencies. Ann Emerg Med. 2010;56(5):551–64. [DOI] [PubMed] [Google Scholar]
- 5. Miller IW, Camargo, Jr. CA , Arias SA, Sullivan AF, Allen MH, Goldstein AB, et al. Suicide prevention in an emergency department population: the ED‐SAFE study. JAMA Psychiatry. 2017;74(6):563–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Inagaki M, Kawashima Y, Yonemoto N, Yamada M. Active contact and follow‐up interventions to prevent repeat suicide attempts during high‐risk periods among patients admitted to emergency departments for suicidal behavior: a systematic review and meta‐analysis. BMC Psychiatry. 2019;19(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hirayasu Y, Kawanishi C, Yonemoto N, Ishizuka N, Okubo Y, Sakai A, et al. A randomized controlled multicenter trial of post‐suicide attempt case management for the prevention of further attempts in Japan (ACTION‐J). BMC Public Health. 2009;9:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kawanishi C, Aruga T, Ishizuka N, Yonemoto N, Otsuka K, Kamijo Y, et al. Assertive case management versus enhanced usual care for people with mental health problems who had attempted suicide and were admitted to hospital emergency departments in Japan (ACTION‐J): a multicentre, randomised controlled trial. Lancet Psychiatry. 2014;1(3):193–201. [DOI] [PubMed] [Google Scholar]
- 9. Kawanishi C, Ishii T, Yonemoto N, Yamada M, Tachikawa H, Kishimoto T, et al. Protocol for a prospective multicentre registry cohort study on suicide attempters given the assertive case management intervention after admission to an emergency department in Japan: post‐ACTION‐J Study (PACS). BMJ Open. 2018;8(9):e020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okamura K, Komori T, Sugimoto M, Kawashima Y, Yamada M, Kishimoto T. Implementation of evidence‐based intervention for suicidal patients admitted to the emergency department: implications from our real‐world experience of assertive case management. Psychiatry Clin Neurosci. 2021;75(3):108–9. [DOI] [PubMed] [Google Scholar]
- 11. Norimoto K, Ikeshita K, Kishimoto T, Okuchi K, Yonemoto N, Sugimoto T, et al. Effect of assertive case management intervention on suicide attempters with comorbid Axis I and II psychiatric diagnoses: secondary analysis of a randomised controlled trial. BMC Psychiatry. 2020;20(1):311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Inui‐Yukawa M, Miyaoka H, Yamamoto K, Kamijo Y, Takai M, Yonemoto N, et al. Effectiveness of assertive case management for patients with suicidal intent. Psychiatry Res. 2021;304:114125. [DOI] [PubMed] [Google Scholar]
- 13. Furuno T, Nakagawa M, Hino K, Yamada T, Kawashima Y, Matsuoka Y, et al. Effectiveness of assertive case management on repeat self‐harm in patients admitted for suicide attempt: findings from ACTION‐J study. J Affect Disord. 2018;225:460–5. [DOI] [PubMed] [Google Scholar]
- 14. Tachikawa H, Takahashi S, Nemoto K, Yonemoto N, Oda H, Miyake Y, et al. Predictive factors for recurrent suicide attempts: evidence from the ACTION‐J study. Psychiatry Clin Neuroscie Rep. 2022;1(2):e7. [Google Scholar]
- 15. Hawton K, Witt KG, Salisbury TLT, Arensman E, Gunnell D, Hazell P, et al. Psychosocial interventions following self‐harm in adults: a systematic review and meta‐analysis. Lancet Psychiatry. 2016;3(8):740–50. [DOI] [PubMed] [Google Scholar]
- 16. Morthorst B, Krogh J, Erlangsen A, Alberdi F, Nordentoft M. Effect of assertive outreach after suicide attempt in the AID (assertive intervention for deliberate self harm) trial: randomised controlled trial. BMJ. 2012;345:e4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gysin‐Maillart A, Schwab S, Soravia L, Megert M, Michel K. A novel brief therapy for patients who attempt suicide: a 24‐months follow‐up randomized controlled study of the Attempted Suicide Short Intervention Program (ASSIP). PLoS Med. 2016;13(3):e1001968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Luoma JB, Martin CE, Pearson JL Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 2002;159(6):909–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.


