Abstract
This review discussed analyzing information dissemination and activities related to mental health conducted by the Centers of Disease Control and Prevention (CDC), considering their application in Japan, and disseminating them to the public is necessary for the Japanese New Center for Health Control. The Japanese government also explores the Japanese New Center For Health Control in addressing children's mental health issues potentially under the Japan health crisis. The findings underscore the urgency of prioritizing children's mental health and implementing effective strategies to mitigate the long‐term effects of the COVID‐19 pandemic.
Keywords: Centers of Disease Control and Prevention (CDC), child, Japan, mental health, pandemic
INTRODUCTION
Coronavirus disease‐2019 (COVID‐19) has raged globally for more than 3 years. Many countries voiced the need for social distance, which caused much disruption to daily life, along with the collapse of medical care in some countries. Schools closed in 188 countries, >90% of the world's population lost access to education, and the United Nations Educational, Scientific and Cultural Organization warned of educational disruption. 1 Schools were closed during the COVID‐19 pandemic and many children suffered from loneliness and fear of the unknown virus, which has become a social problem in many countries.
In Japan, nationwide elementary and junior high schools were asked to temporarily close from March 2, 2020, until the spring vacation in response to the explosive spread of the virus. This response to schools was part of the emergency declaration to slow and prevent the spread of the infection, but the closure of schools and confinement at home could have negatively influenced the physical health and psychological well‐being of the children. 2 However, the situation further worsened, and a state of emergency was declared on April 7, 2020 (The Prime Minister's Office in Japan 2020). 3 The long struggle that followed continues to this day.
The Japanese Society of Neuropsychiatry, the Japanese Society of Child and Adolescent Psychiatry, the Japanese Society of Disaster Medicine, the Japanese Society of General Hospital Psychiatry, and the Japanese Society of Traumatic Stress Medicine jointly published the first edition of the Guidelines for Mental Health Measures during the COVID‐19 epidemic on June 25, 2020. This guideline is based on the first edition of the Guidelines for Mental Health Measures during the COVID‐19 pandemic. This guideline is intended to provide individuals who were engaged in psychiatric care in Japan and those supporting health, education, welfare, and other related fields with basic information, awareness, and issues to be addressed in implementing mental health measures during the COVID‐19 pandemic, and to share ideas based on accumulated opinions to date regarding the direction to be considered. This report aims to share basic information, perceptions, and issues to be addressed in implementing mental health measures, promote mutual collaboration among related organizations and fields, and facilitate the implementation of effective measures. However, this report was not revised after the first edition, which is a crucial problem for Japanese society.
Japan's legal and social structure has demonstrated its vulnerability to this crisis in children's mental health as well as stress‐related issues among healthcare professionals. Faced with this critical situation, the Cabinet approved the new Japanese Center Bill on March 7, 2023. The National Institute of Infectious Diseases and the National Institute for Health Risk Management will be established to conduct research and surveys, provide medical care, international cooperation, and train human resources in terms of infectious and other diseases, as well as strengthen the system to provide scientific knowledge by comprehensively conducting epidemiological surveys to clinical research during infectious disease outbreaks and spread that may seriously affect the lives and health of the public. The National Institute of Infectious Diseases and the National Center for Global Health and Medicine (NCGM) are scheduled to be merged to develop a new Japanese center for all Japanese citizens' health.
Through the COVID‐19 pandemic, the new Japanese national center was needed to conduct clinical, research, and administrative roles related to infectious diseases that did not exist before. When making discussions for the establishment of the new center, governments should not forget that mental health problems can occur in a pandemic. Developing the Japanese psychiatric clinical and research fields, the new center has to discuss the importance of mental health care under the pandemic and add mental health problems to policy‐making about infection control by the government.
CENTERS FOR DISEASE CONTROL AND PREVENTION IN THE UNITED STATES
On July 1, 1946, the Centers of Disease Control and Prevention (CDC) opened on one floor of a small building in Atlanta, United States. 4 Its primary mission was to prevent the spread of malaria throughout the United States. With a budget of only $10 million and <400 employees, the CDC continued to advocate for public health issues and lobbied to expand its responsibilities to other communicable diseases. Now, with its headquarters still in Atlanta, the CDC has expanded its focus to include all communicable diseases, and to provide practical assistance to state health departments upon request. The CDC is the nation's leading science‐based, data‐driven service agency that protects the public's health. It has helped children stay healthy to grow and learn, as well as families, businesses, and communities to fight disease, for over 70 years.
The CDC launched an effort to enhance and modernize its structures, systems, and processes for science and program development and deployment in April 2022. It aimed to pivot long‐standing practices, learn how to adapt to pandemics and other public health emergencies, and apply the lessons learned throughout the organization. Further, this effort included a major workflow overhaul, with a particular emphasis on ensuring that CDC science reaches the public as quickly as possible in an understandable, accessible, and actionable way.
PUBLIC ENLIGHTENMENT OF MENTAL HEALTH BY THE CDC
The CDC, which has functioned with the above philosophy and history, has four of its 10 current divisions dealing with children's mental health, including the National Center for Injury Prevention and Control; the National Center for HIV, Viral Hepatitis, STD and TB Prevention; the National Center on Birth Defects and Developmental Disabilities; and the National Center for Chronic Disease Prevention and Health Promotion. Public enlightenment on mental health by the CDC is disseminated on mental health in general, child and teen mental health, and even suicide and disaster psychiatry.
Among the health topics presented by the CDC, public information on children's mental health is extremely vast. 5 The CDC's reports provide a wide range of information on not only healthy child development, sleep hygiene, and school health, but also the latest information on developmental disorders, such as attention deficit hyperactivity disorder and autism spectrum disorder, the association between thimerosal and vaccines, underage drinking, child care, school mental health during disasters, and the effects of child abuse and adverse childhood experiences. The Youth Risk Behavior Surveillance System, which tracks behaviors that may cause poor health outcomes for students in Grades 9–12, also provides the Youth Risk Behavior Survey data set and analysis tools.
The CDC focuses on mental health for many reasons. People with mental disorders had a 1.45 times higher risk of COVID‐19 during the pandemic. 6 The risk of COVID‐19 demonstrated differences by type of mental disorder, with the increasing risk of organic mental, mood, and neurotic/stress‐related disorders. Further, several challenges were noted with age, alcohol intake, body mass index, and social poverty being associated with the risk of COVID‐19 during the pandemic. Worsening mental health, including anxiety and mood symptoms, developmental disorders, stress‐related disorders, and eating disorders in children, adolescents, and young adults, were emphasized during the COVID‐19 pandemic. 7 Similarly, a meta‐analysis of 634,338 patients with COVID‐19 from 16 studies revealed that prior mental disorder diagnosis increased the risk of COVID‐19 fatality and severity. 8 Furthermore, higher fatality rates were reported in patients with schizophrenia, schizotypal, and paranoid disorders compared to patients with mood disorders, indicating that, with the introduction of the COVID‐19 vaccine, patients with mental disorders need to be prioritized for vaccination, along with healthcare professionals and the elderly. Another systematic review and meta‐analysis of the association between COVID‐19 and psychiatric disorders in patients from seven countries revealed that patients with psychiatric disorders demonstrated an increased risk of COVID‐19‐related deaths. 9
These studies indicate that patients with psychiatric disorders are considered at higher risk for COVID‐19 severity and require improved strategies for prevention and disease management. Future studies should more accurately assess the risk for patients with each psychiatric disorder. They warn that patients with mental disorders are at higher risk for COVID‐19 and therefore require more attention. Further, public health guidelines should focus on reducing the risk of COVID‐19 by encouraging healthy lifestyles and preferential policies for patients with mental disorders.
CHILDREN'S MENTAL HEALTH DURING THE COVID‐19 PANDEMIC
The highest prevalence among patients infected with COVID‐19 was post‐traumatic symptoms (94%), followed by behavioral problems in those with a history of mental disorders (77%), fear in healthcare workers (71%), anxiety in caregivers/family members of patients infected with COVID‐19 (42%), general health/social contact in the general population/passive coping styles (38%), depression in people with a history of physical disability (37%), and fear of nonmedical professionals (29%). 10 Additionally, a significant impact was observed on the mental health of the general public and healthcare providers. 11 The most prominent mental disorders are anxiety, sleep disorders, and depression.
COVID‐19 wreaked havoc on the mental health of the general infected population, children, and those affected by mental illness. Suicidal behavior increased, especially among young women and men aged over 70 years. Illegal drug use and gambling decreased during the pandemic, but pornography consumption substantially increased, as did compulsive shopping and video game use. Vulnerable groups particularly included adolescents and patients with autism spectrum disorders. 11 The COVID‐19 pandemic and the accompanying infection control measures have caused sudden and significant disruption in the lives of children and adolescents globally. Staying at home and being less active outdoors caused less physical activity, social withdrawal from their usual surroundings, less peer interaction, more screen time, irregular sleep patterns, and less favorable eating habits. 12
One study of the general population revealed not only an increase in both dietary restriction and binge eating behaviors during the COVID‐19 pandemic but also a decrease in physical activity compared to pre‐pandemic levels. 13 A systematic review of 191 studies of 1,389,447 children and adolescents aged 18 years and younger revealed pooled prevalence rates of depressive, anxiety, and sleep disorders of 31%, 31%, and 42%, respectively. 14 Age, grade level, education level, gender, geographic region, and use of electronic devices correlated with the prevalence of mental health symptoms. Additionally, the prevalence rates of anxiety symptoms, depressive symptoms, irritability, and anger were 1.8%–49.5%, 2.2%–63.8%, 16.7%–73.2%, and 30.0%–51.3%, respectively, in 61 articles involving 54,999 children (19 years and younger) and adolescents (mean age = 11.3 years, 49.7% female) exposed to COVID‐19 lockdown. 15 The presence of special needs and mental disorders before lockdown were significant risk factors for anxiety, along with excessive media exposure, considering that parent–child communication was protective against anxiety and depression. Additionally, children with anorexia nervosa demonstrated increased restriction and anxiety about their eating behavior during the COVID‐19 pandemic. 16 , 17 Children with anorexia nervosa are at high risk for death. However, there are few hospitals that treat these children in Japan. NCGM, which is the base of the New Center, is the only national center that has a special ward for child and adolescent psychiatry.
Many studies have revealed that some children sleep longer and have later bedtimes and wake times since the COVID‐19 pandemic. 18 Sleep disturbances and the association between sleep and psychological outcomes in children have also been reported. The extent to which increased sleep duration and changes in sleep behavior have improved sleep quality and changes in sleep disturbances remains unclear. This review indicates the importance of considering children's sleep in other mass trauma situations, particularly natural and man‐made disasters and pandemics.
Moreover, the mental health of children's caregivers is a frequent issue, and the COVID‐19 pandemic affected children and adolescents with neurodevelopmental disorders, which created difficulties and increased the burden on caregivers. A systematic review and meta‐analysis of 20 studies involving 14,743 participants revealed that the main psychological problems among caregivers were anxiety (36.6%), depression (41.1%), and stress (58.9%). 19 Prevalence varied by study year, country economic level, continent, and sample size. The results of this study indicate that caregivers of children and adolescents with neurodevelopmental disorders had a higher prevalence of anxiety, depression, and stress during the COVID‐19 pandemic. Thus, the psychological problems of these caregivers may be caused by COVID‐19 during the pandemic.
JAPAN IS FACING A CHILDREN'S MENTAL HEALTH CRISIS BEFORE AND AFTER THE PANDEMIC
As we have discussed, all individuals, from children to adults, who have not previously had mental health issues, may face challenges with the spread of COVID‐19. Like previous discussions about children's lives in other countries, problems related to depression, anxiety, game addiction, and eating behavior have been noted in Japan. 20 , 21 , 22 , 23 , 24 However, there is no national center like the CDC to oversee and disseminate information on children's mental health during a pandemic. After the COVID‐19 pandemic, the challenges of child and adolescent mental health care and medical policy in Japan did not change to become adequately discussed.
There are many serious issues about children's mental health in Japan during and after the pandemic. In FY2022, the number of elementary and junior high school children who did not attend school increased for the ninth year to 294,000, which is the highest number ever. The Ministry of Education, Culture, Sports, Science, and Technology emphasizes that the environmental changes and various restrictions on school life caused by COVID‐19 have affected friendships and other relationships, thereby making the motivation of the students to attend school difficult. Additionally, more serious issues in Japanese society included suicide in 512 children <18 years of age in 2022. Suicides among children have been increasing in recent years while the birth rate is decreasing. 25 Further, the number of child suicides has increased and the issue is becoming more serious.
The worldwide prevalence of neurodevelopmental disorders is rapidly increasing. 26 The “Administrative Evaluation of Support for Persons with developmental disabilities—Monitoring” of the Ministry of Internal Affairs and Communications recommended that the waiting list for the initial consultation for children suspected of having a developmental disability is getting longer in specialized medical institutions. In particular, the longest waiting time is approximately 10 months for an initial consultation, with a maximum waiting list of 316 patients. Japan's Ministry of Internal Affairs and Communications has issued recommendations to medical institutions for improvement.
Studies revealed increased restriction and anxiety regarding eating behavior in individuals with anorexia nervosa during the COVID‐19 pandemic. 17 Several patients presented with medical instability following restrictive diets and required acute hospitalization to correct malnutrition but frequently had difficulty finding a hospital that has a child and adolescent psychiatric unit.
The development of mental illness begins in adolescence, thus children with such diverse issues are recognized. 27 However, the medical field of child and adolescent psychiatry in Japan faces a shortage of child and adolescent psychiatrists which requires multiprofessional support. One child psychiatrist at the Japanese Council of Child and Adolescent Mental Health Institutions treated an average of 132 outpatients (maximum 360 outpatients) and five inpatients (maximum 19 inpatients), spending ≥60 min for the initial visit and 30–60 min for the follow‐up visit. This significantly exceeded the consultation time of a regular psychiatrist in Japan, thereby causing the depopulation of child psychiatry in terms of overwork and cost‐effectiveness. Additionally, more inpatient hospital beds were required to provide comprehensive treatment for psychiatric difficulties beyond developmental problems, such as depression, suicide, and eating disorders.
Therefore, support and research focused on the mental health of infected children in the community and children with mental disorders are recommended if a Japanese version of the CDC is to be developed to mitigate its long‐term impact.
NEED MORE EVIDENCE OF JAPANESE CHILDREN'S MENTAL
Recently, the Japanese government attempted to enhance evidence‐based policymaking (EBPM). The Cabinet Office defined EBPM as the practice of basing policy planning on evidence, with clear policy objectives, rather than relying on ad hoc episodes. 28
EBPM has several issues, including organizing data into analyzable formats and avoiding a half‐hearted approach to policy formation. This study highlights the importance of systematically reviewing information and sharing information‐based tools for children's mental health. Further, it indicates a dialogue between medical professionals, such as child and adolescent psychiatrists, psychologists, social workers, policy‐makers, policy formation experts, economists, and educators. This discussion would ensure that evidence is rigorously analyzed, translated, and successfully disseminated.
EBPM highlights the importance of transitioning from the “equality for everyone” approach to the “resource allocation based on needs” approach. This transition is crucial to resolve the growing disparity in education among Japanese children. Overall, this study offers a detailed examination of the various issues associated with child poverty and childcare policies in Japan. It emphasizes the need to use EBPM to establish informed decisions, as well as the importance of systematically reviewing and sharing information, the challenges in child and adolescent psychiatry, and the need to transition from the “equality for everyone” approach to the “resource allocation based on needs” approach.
Some studies discuss EBPM for children's mental health. The American Child Welfare System determines this area and discusses the use of decision‐analytic models to advance child welfare policy and practice. 29 Researchers of Canadian child mental health policy hope to utilize the best available research evidence to develop policy to address important public issues. 30 Children are more vulnerable to abuse and neglect and are, thus, more likely to experience negative health and mental health outcomes. Therefore, this study discussed the EBPM that prevents child maltreatment and reduces negative mental health outcomes for young people who are victims. 31
The Child and Adolescent Mental Health Registry of the NCGM continues to collect clinical activities in child psychiatry from normal times. It reports on changes in children's mental health using data before the COVID‐19 pandemic.
Several cohort studies focused on the general pediatric population but collected information from limited geographic areas and with inconsistent data collected. Hence, the evidence base for EBPM practices in child mental health in Japan is poor. Training medical specialists and establishing a system to support local people with developmental disabilities who wish to be examined are crucial to solving the problem of children with developmental disabilities waiting to be examined, which was an issue before the pandemic. Further, expanding the number of specialized hospitals that can provide inpatient treatment for problems other than developmental disabilities, such as suicide, depression, and anorexia, is essential. Evidence is lacking on how many of the limited number of child psychiatric facilities should be established in which areas to address these issues, as well as how they should respond to emergencies.
Childhood adversity experiences have a significant impact on a child's life, as the CDC in the United States has recognized. Establishing a continuous support system that includes maternal and child healthcare as well as adolescent mental health care is necessary. Field surveys should be conducted to collect evidence on children's mental health in the field of child and adolescent psychiatry in Japan, and a statistical maintenance system needs to be established. Thus, developing an implementation system that does not increase the burden of actual clinical practice and the need to bridge the gap between the treatment of mental disorders and the fields of maternal and child health and child welfare is important. 30 , 31 , 32 Furthermore, the need for statistical systems and the promotion of their use must ensure ease of access, protection of personal information, promotion of their use in health care, welfare, and education, and budgetary incentives.
THE JAPANESE NEW CENTER OF HEALTH CONTROL SHOULD TREAT CHILDREN'S MENTAL HEALTH
Analyzing information dissemination and activities related to mental health conducted by the CDC, considering their application in Japan, and disseminating them to the public is necessary for the Japanese New Center for Health Control. This center needs to disseminate evidence‐based information and EBPM available to protect children's mental health pre‐pandemic, during a pandemic, and post‐pandemic (Figure 1).
Figure 1.
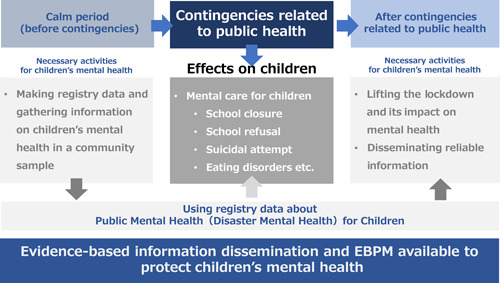
The Japanese new center needs to disseminate evidence‐based information and evidence‐based policy‐making (EBPM) available to protect the children's mental health pre‐pandemic, during a pandemic, and post‐pandemic.
New mental health recommendations that consider Japanese culture and lifestyle (mental health of healthcare professionals, mental health of children, etc.) are needed, and the Japanese new health control center must disseminate information that can be used for EBPM about children's mental health to the Child and Family Agency and the Ministry of Health, Labour, and Welfare. Leveraging NCGM's child and adolescent psychiatry services, early intervention in children's mental health is considered useful from a cost–benefit perspective. Further, appropriate information dissemination, including socioeconomic impact, is essential.
Therefore, psychiatric clinical and research functions that can manage children's mental health, such as suicide, school refusal, eating disorders, internet addiction, and neurodevelopmental disorders, during a new infectious disease outbreak are essential functions of infection controls for a new Japanese national center for health risk control.
AUTHOR CONTRIBUTIONS
All authors are members of the new center's project team and conducted discussions on the content of this review. Usami Masahide wrote this manuscript. Yanai Hidekatsu, Katsuyama Hisayuki, Satake Naoko, and Hayakawa Tatsuro revised this manuscript.
CONFLICT OF INTERESTS STATEMENT
The authors declare no conflicts of interest.
ETHICS APPROVAL STATEMENT
None. This manuscript is only reviewing previous studies and domestic policy for the Japanese new center.
PATIENT CONSENT STATEMENT
N/A.
CLINICAL TRIAL REGISTRATION
N/A.
ACKNOWLEDGMENTS
The authors deeply acknowledge all staff of Kohnodai Hospital, National Center for Global Health and Medicine. This work was supported by grants from the National Center for Global Health and Medicine (21A1012). The funder had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Usami M, Satake N, Katsuyama H, Okudera K, Uchiyama Y, Imamura M, et al. Is Children's Mental Health an Important Function of Newly National Organization for health Crisis Management in Japan? Psychiatry Clin Neurosci Rep. 2024;3:e175. 10.1002/pcn5.175
DATA AVAILABILITY STATEMENT
None.
REFERENCES
- 1. Lee J. Mental health effects of school closures during COVID‐19. Lancet Child Adolesc Health. 2020;4(6):421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bahn GH. Coronavirus disease 2019, school closures, and children's mental health. J Korean Acad Child Adolesc Psychiatry. 2020;31(2):74–79. 10.5765/jkacap.200010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The Prime Minister's Office in Japan . Task Force on New Coronavirus Infections (27th Meeting) , Tokyo. 2020. https://www.kantei.go.jp/jp/98_abe/actions/202004/07corona.htm
- 4. Centers for Disease Control and Prevention . [cited 2023 Nov 21]. Available from: https://www.cdc.gov/
- 5. Fox S. Health topics. Pew Online Research. 2011. [cited 2023 Dec 4]. Available from: https://www.cdc.gov/health-topics.html
- 6. Dai X, Shao Y, Ren L, Tao W, Wang Y. Risk factors of COVID‐19 in subjects with and without mental disorders. J Affective Disord. 2022;297:102–111. 10.1016/j.jad.2021.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stavridou A, Stergiopoulou AA, Panagouli E, Mesiris G, Thirios A, Mougiakos T, et al. Psychosocial consequences of COVID‐19 in children, adolescents and young adults: a systematic review. Psychiatry Clin Neurosci. 2020;74(11):615–616. 10.1111/pcn.13134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS. A meta‐analysis: The mortality and severity of COVID‐19 among patients with mental disorders. Psychiatry Res. 2021;299(January):113856. 10.1016/j.psychres.2021.113856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fond G, Nemani K, Etchecopar‐Etchart D, Loundou A, Goff DC, Lee SW, et al. Association between mental health disorders and mortality among patients with COVID‐19 in 7 countries: A systematic review and meta‐analysis. JAMA Psychiatry. 2021;78(11):1208–1217. 10.1001/jamapsychiatry.2021.2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dragioti E, Li H, Tsitsas G, Lee KH, Choi J, Kim J, et al. A large‐scale meta‐analytic atlas of mental health problems prevalence during the COVID‐19 early pandemic. J Med Virol. 2022;94(5):1935–1949. 10.1002/JMV.27549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bouza E, Arango C, Moreno C, Gracia D, Martín M, Pérez V, et al. Impact of the COVID‐19 pandemic on the mental health of the general population and health care workers. Rev Esp Quimioter. 2023;36(2):125–143. 10.37201/REQ/018.2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID‐19 outbreak. Lancet. 2020;395(10228):945–947. 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Phillipou A, Meyer D, Neill E, Tan EJ, Toh WL, van Rheenen TE, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. 2020;53(7):1158–1165. 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Deng J, Zhou F, Hou W, Heybati K, Lohit S, Abbas U, et al. Prevalence of mental health symptoms in children and adolescents during the COVID‐19 pandemic: a meta‐analysis. Ann NY Acad Sci. 2023;1520(1):53–73. 10.1111/nyas.14947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Panchal U, Salazar de Pablo G, Franco M, Moreno C, Parellada M, Arango C, et al. The impact of COVID‐19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151–1177. 10.1007/s00787-021-01856-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Termorshuizen JD, Watson HJ, Thornton LM, Borg S, Flatt RE, MacDermod CM, et al. Early impact of COVID‐19 on individuals with self‐reported eating disorders: a survey of ~1,000 individuals in the United States and the Netherlands. Int J Eat Disord. 2020;53(11):1780–1790. 10.1002/eat.23353 [DOI] [PubMed] [Google Scholar]
- 17. Usami M, Sasaki S, Sunakawa H, Toguchi Y, Tanese S, Saito K, et al. Care for children's mental health during the COVID‐19 pandemic in Japan. Glob Health Med. 2021;3(2):119–121. 10.35772/ghm.2020.01081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pfefferbaum B, Tucker P, Ekambaram V, Van Horn RL. Children's sleep and mental health during the COVID‐19 pandemic. Curr Psychiatry Rep. 2023;25:847–856. 10.1007/s11920-023-01475-z [DOI] [PubMed] [Google Scholar]
- 19. Gu X, Shan X, Wang L, Gao WY, Liu XQ. Prevalence of psychological problems among caregivers of children and adolescents with neurodevelopmental disorders during the COVID‐19 pandemic: a meta‐analysis and systematic review. Res Dev Disabil. 2023;143:104632. 10.1016/J.RIDD.2023.104632 [DOI] [PubMed] [Google Scholar]
- 20. Hosozawa M, Ando S, Yamaguchi S, Yamasaki S, DeVylder J, Miyashita M, et al. Sex differences in adolescent depression trajectory before and into the second year of COVID‐19 pandemic. J Am Acad Child Adolesc Psychiatry. 2023. In press. 10.1016/j.jaac.2023.08.016 [DOI] [PubMed] [Google Scholar]
- 21. Hyunshik K, Jiameng M, Sunkyoung L, Ying G. Change in Japanese children's 24‐hour movement guidelines and mental health during the COVID‐19 pandemic. Sci Rep. 2021;11(1):22972. 10.1038/s41598-021-01803-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kishida K, Tsuda M, Waite P, Creswell C, Ishikawa S. Relationships between local school closures due to the COVID‐19 and mental health problems of children, adolescents, and parents in Japan. Psychiatry Res. 2021;306:114276. 10.1016/j.psychres.2021.114276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mizumoto Y, Sasaki Y, Sunakawa H, Tanese S, Shinohara R, Kurokouchi T, et al. Current situation and clinical burden of pediatricians for children with eating disorders during the COVID‐19 pandemic. Glob Health Med. 2023;5(2):122–124. 10.35772/ghm.2022.01034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Usami M. Psychiatric care for children under the COVID‐19 pandemic. JPN J Child Adol Psy. 2022;63(4):465–472. http://export.jamas.or.jp/dl.php?doc=8e2b1ff1f2020ed2ee8dbeb25b22339a154dec3ed8cf0fbd53dc961ca99c77b6_bibtex.bib [Google Scholar]
- 25. National Police Agency . Number of suicides. 2024. [cited 2023 Mar 26]. Available from: https://www.npa.go.jp/publications/statistics/safetylife/jisatsu.html
- 26. Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, et al. Global prevalence of autism: a systematic review update. Autism Res. 2022;15(5):778–790. 10.1002/AUR.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large‐scale meta‐analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–295. 10.1038/s41380-021-01161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cabinet Office . EBPM initiatives in the Cabinet Office. Tokyo: Cabinet Office. 2024. [cited 2023 Mar 26]. Available from: https://www.cao.go.jp/others/kichou/ebpm/ebpm.html
- 29. Goldhaber‐Fiebert JD, Snowden LR, Wulczyn F, Landsverk J, Horwitz SM. Economic evaluation research in the context of child welfare policy: a structured literature review and recommendations. Child Abuse Negl. 2011;35(9):722–740. 10.1016/j.chiabu.2011.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Waddell C, Lavis JN, Abelson J, Lomas J, Shepherd CA, Bird‐Gayson T, et al. Research use in children's mental health policy in Canada: maintaining vigilance amid ambiguity. Soc Sci Med. 2005;61(8):1649–1657. 10.1016/j.socscimed.2005.03.032 [DOI] [PubMed] [Google Scholar]
- 31. Hanson RF, Self‐Brown S, Rostad WL, Jackson MC. The what, when, and why of implementation frameworks for evidence‐based practices in child welfare and child mental health service systems. Child Abuse Negl. 2016;53:51–63. 10.1016/j.chiabu.2015.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Long J, Bhad R, Potenza MN, Orsolini L, Phan V, Kanabar M, et al. Public health approaches and policy changes after the inclusion of gaming disorder in ICD‐11: global needs. BJPsych Int. 2022;19(3):63–66. 10.1192/bji.2021.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.


