Abstract
People living with HIV (PLWH) have a higher prevalence of psychiatric disorders than the general population. We retrospectively examined the medical records of PLWH who underwent the Kessler Psychological Distress Scale‐10, the Patient Health Questionnaire‐9, and the Generalized Anxiety Disorder‐7 at an HIV referral hospital during the COVID‐19 pandemic. Some PLWH who were unemployed with a history of psychiatric visits may remain in poor mental health during the prolonged COVID‐19 pandemic until the Omicron variant occurs, so they may need to pay attention to their mental health.

Keywords: COVID‐19, HIV, mental health, Omicron variant
Stringent responses such as social distancing and restrictions on going out are necessary to prevent the spread of COVID‐19 infection. However, in Europe, the severity of depression and anxiety showed a considerable correlation with Stringency Index (SI) values, 1 which indicates the strength of social infection measures. People living with HIV (PLWH) are known to have a higher prevalence of psychiatric disorders than the general population, even before the COVID‐19 pandemic. 2 , 3
This study surveyed the medical records of PLWH attending an HIV‐referral hospital in Japan to examine their mental health during the COVID‐19 pandemic.
This retrospective and observational study was performed using collected medical records from February 2020 to March 2022 during the COVID‐19 surges. The subjects were 30 male PLWH receiving regular care who were randomly selected and agreed to be interviewed by an HIV clinician at the Research Hospital of the Institute of Medical Science at the University of Tokyo, excluding those who could not agree. Three questionnaires were completed to assess mental health: the Kessler Psychological Distress Scale‐10 (K10), the Patient Health Questionnaire‐9 (PHQ‐9), and the Generalized Anxiety Disorder‐7 (GAD‐7). The questionnaires were filled out by the patients themselves at each interview. We examined the mental states of PLWH over time by referring to the social restrictions defined by the SI.
The baseline characteristics of the 30 PLWH are shown in Table S1. We found that 29.4% of PLWH were highly stressed, 53.3% had depression, and 28.6% had anxiety disorders in the first surge.
The trends in the K10, PHQ‐9, and GAD‐7 results of the 14 PLWH whose progress could be followed up to the time of the Omicron epidemic are shown with SI values in Figure 1. Two PLWH had consistently scored cut‐off or more in all three psychological tests from the beginning of the pandemic until the Omicron variant surge. Five of the other 12 PLWH had scored less than the cut‐off in all psychological tests. The remaining seven PLWH had scored equal to or more than the cut‐off in one of the psychological tests, but these seven PLWH had improved to less than the cut‐off by the Omicron pandemic. The median scores of 12 PLWH for all tests also remained almost the same or decreased regardless of the SI values. The mental health trends for two PLWH fluctuated up and down but they continued to have high scores over 2 years (Figure 1).
Figure 1.
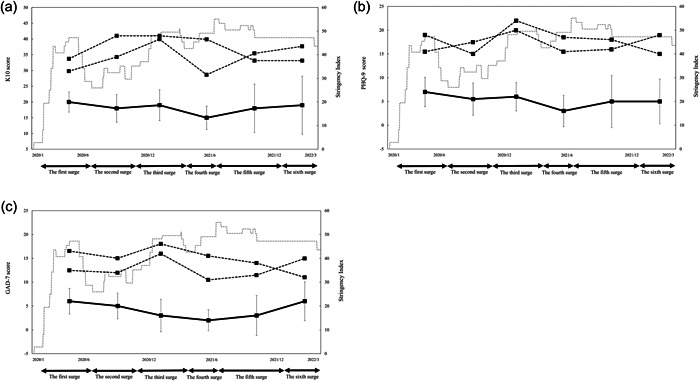
Changes in Psychological test values K10, the Kessler Psychological Distress Scale‐10; PHQ‐9, the Patient Health Questionnaire‐9; GAD‐7, the Generalized Anxiety Disorder‐7. The results of the two high scorers are shown as a thick dotted line, the median of the remaining 12 is shown as a bold line and the IQR is shown as a solid line. The thin dotted line is the Stringency Index of Japan.
The 12 PLWH fell into two or three of the following categories: “Having a partner,” “Having jobs,” and “Having no history of psychiatric visits.” The two PLWH with the higher psychometric test values met neither or only one of the three factors; they were both unemployed and had a history of psychiatric visits in common (Table S2).
Before the COVID‐19 pandemic, 12.5% of PLWH were highly stressed, 25.7% had depression, and 29.3% had anxiety disorders. 2 , 4 This study suggests that the stress and depression of PLWH worsened during the COVID‐19 first surge. It is crucial that two PLWH without improvement had psychiatric histories, were unemployed, and were in a group that suggested loneliness or social isolation. This indicates that loneliness or social isolation may aggravate the mental health of PLWH, even during the COVID‐19 pandemic in Japan. Furthermore, this study found that PLWH who fell into two or more categories (having a partner, having no history of psychiatric visits, or having jobs) kept depression and anxiety at a mild level below the cut‐off in the prolonged COVID‐19 pandemic (Figure 1). Having a partner, jobs, and no history of psychiatric visits might be protective factors for mental health problems in the COVID‐19 pandemic. 5 , 6
Regardless of the stringency of social infection measures, some PLWH with high anxiety and depression in the early COVID‐19 period remained in poor mental health during the prolonged COVID‐19 pandemic. In particular, unemployed PLWH with a history of psychiatric visits may need to pay attention to their mental health. Cognitive behavior therapy and 15–30 min of exercise per day have been shown in previous studies to reduce high levels of stress, depression, and anxiety. 7 , 8 It is considered necessary to make such an intervention for them at an early stage. The lack of control data on non‐HIV‐infected people is a critical limitation, but it is important findings for HIV‐infected patients with stigma, not only in the field of infectious diseases but also in the field of Liaison Psychiatry. 9 This study was a retrospective observational study and showed that there are differences in mental health due to COVID‐19 among HIV‐infected people.
AUTHOR CONTRIBUTIONS
Takahiro Tanaka, Michiko Koga, and Takashi Hosaka conceived the concept of this study, were responsible for the study design and collected the data. All authors interpreted the collected data, drafted the manuscript, and provided feedback. All authors critically read the drafted manuscript and approved the final version.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
FUNDING
This study was supported in part by research grants from a Health Labor Sciences research grant (grant number R3‐AIDS‐ general‐21HB2005).
ETHICS APPROVAL STATEMENT
This study was approved by the Ethics Review Committee at the University of Tokyo (approval No.: 30‐110‐B20190404) and conformed to the provisions of the Declaration of Helsinki.
PATIENT CONSENT STATEMENT
We applied Opt‐out method to obtain consent on this study.This is a retrospective observational study in which the psychological tests had been collected transiently, and the opt‐out method has been approved by the Ethics Committee of Research Hospital of the Institute of Medical Science at the University of Tokyo (approval No.: 30‐110‐B20190404). A study summary was published on the Internet and guaranteed the opportunity to ask questions or refuse to conduct or continue the study. The absence of a refusal was deemed to be consent.
CLINICAL TRIAL REGISTRATION
N/A
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGMENTS
We are grateful for all the participants of the Hospital of the Institute of Medical Science, University of Tokyo.
Contributor Information
Michiko Koga, Email: michiko@ims.u-tokyo.ac.jp.
Takashi Hosaka, Email: hosaka1952@gmail.com.
Hiroshi Yotsuyanagi, Email: yotsudid@ims.u-tokyo.ac.jp.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the supplementary material of this article.
REFERENCES
- 1.Organization for Economic Co‐operation and Development (OECD): TRACKING CORONAVIRUS (COVID‐19) CONTRIBUTING TO A GLOBAL EFFORT, Tackling the mental health impact of the COVID‐19 crisis: An integrated, whole‐of‐society response. Available from: https://read.oecd-ilibrary.org/view/?ref=1094_1094455-bukuf1f0cm%26title=Tackling-the-mental-health-impact-of-the-COVID-19-crisis-An-integrated-whole-of-society-response%26_ga=2.41681378.1581547161.1630208047-696326152.1572945659
- 2.HIV Futures Japan Project: 2nd Web‐based survey for HIV‐positive people. Available from: https://survey.futures-japan.jp/doc/summary_2nd_all.pdf
- 3. Komatsu K, Kojima K. Treatment of psychiatric disorders and psychological problems among people living with HIV/AIDS. J AIDS Res. 2016;18(3):183–96. [Google Scholar]
- 4. Hayashi K, Wakabayashi C, Ikushima Y, Tarui M. High prevalence of quasi‐legal psychoactive substance use among male patients in HIV care in Japan: a cross‐sectional study. Subst Abuse Treat Prev Policy. 2017;12(11):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Herrman H, Patel V, Kieling C, Berk M, Buchweitz C, Cuijpers P, et al. Time for united action on depression: a Lancet‐World Psychiatric Association Commission. Lancet. 2022;399(10328):957–1022. [DOI] [PubMed] [Google Scholar]
- 6. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID‐19 in the United Kingdom. Psychiatry Res. 2020;291:113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ottisova L, Gillard JA, Wood M, Langford S, John‐Baptiste Bastien R, Madinah Haris A, et al. Effectiveness of psychosocial interventions in mitigating adverse mental health outcomes among disaster‐exposed health care workers: a systematic review. J Trauma Stress. 2022;35(2):746–58. [DOI] [PubMed] [Google Scholar]
- 8. Schuch FB, Bulzing RA, Meyer J, Vancampfort D, Firth J, Stubbs B, et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self‐isolating people during the COVID‐19 pandemic: a cross‐sectional survey in Brazil. Psychiatry Res. 2020;292:113339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shapiro PA, Brahmbhatt K, Caravella R, Erickson J, Everly G, Giles K, et al. Report of the Academy of Consultation‐Liaison Psychiatry Task Force on lessons learned from the Covid‐19 pandemic: executive summary. J Acad Consult Liaison Psychiatry. 2021;62(4):377–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available in the supplementary material of this article.


