September 6, 2023
ABSTRACT | Rapidly rising drug overdose rates in the United States during the past three decades underscore the critical need to prevent overdose deaths and reduce the development of opioid and related substance use disorders (SUDs). Traditional public health models of prevention emphasize the biological and physical risks of SUDs, often neglecting to consider the broader environmental and social factors that influence health and well-being. Taking a socioecological approach, the authors aim to illustrate the complex interplay among individual, interpersonal, societal, and structural factors that contribute to the development of SUD and overdose risk. The authors propose evidence-informed strategies and interventions across primary, secondary, and tertiary levels of prevention. By doing so, the authors hope to encourage policy makers, funders, service providers, and community leaders to broaden their approaches to SUD prevention and consider how they can create and advocate for a health-promoting environment by addressing the social and structural factors that drive rising SUD and overdose trends.
| Glossary of Terms and Concepts | |
|---|---|
| Biomedical Model of Health | Focuses on the biological and physiological factors of disease and illness |
| Harm Reduction | Aims to minimize the negative health, social, and legal impacts associated with drug use |
| Individual Level of Influence | The biological, behavioral, and psychosocial factors within an individual that influence health and disease |
| Interpersonal Level of Influence | The relationships, social dynamics, and ways of interacting between individuals, including family relationships, that influence health and disease |
| Macro Level of Influence | The policies, culture, norms, laws, and systems that exist across groups of people and institutions that influence health and disease |
| Primary Prevention | Approaches that aim to prevent disease conditions from developing |
| Secondary Prevention | Approaches that seek to identify a health condition as early as possible to halt or slow its progression |
| Socioecological Model of Health | Focuses on the interaction among the individual-, interpersonal-, and macro-level (e.g., community, social, and political) factors that influence disease and illness, and improve overall well-being |
| Structural Vulnerabilities | The intersecting structural and social factors (e.g., socioeconomic, political, racial, and cultural) that create and perpetuate inequalities, increase risk of experiencing negative health outcomes, and reduce opportunities for overall well-being |
| Tertiary Prevention | Approaches that strive to minimize acute negative consequences, such as death, among those who have a disease, while promoting recovery and the management of long-term effects to improve overall well-being |
Introduction
Clinical medicine and public health have long held dueling perspectives of illness. Leading public health thinkers have consistently connected socioeconomic factors to illness, while some traditional clinical medicine professionals have held views restricted to the somatic parameters and “the organic elements . . . of human malfunction” (Jones-Eversley and Dean, 2018; Engel, 1977). The biomedical model described in the latter half of the previous sentence forms the basis of classical Western medical training, in which illness can be reduced to a biological or physiological physical element. Rudolf Virchow (1848), considered the father of modern pathology, stated that “medicine is a social science” and understood that disease operates at the cellular level. He also recognized the social conditions that facilitated the spread of disease, yet this acknowledgment had minimal influence in the evolution of the biomedical model.
In many ways, the American health care system still struggles with the same dilemma today: reimbursement structures incentivize delivery of high acuity care and surgical procedures and rarely pay for care coordination, case management, or other services known to impact long-term health outcomes. But there is an increasingly urgent need, made more salient during the co-occurring COVID-19 and overdose epidemics, to resolve the philosophical debate over clinical medicine’s scope of responsibility for identifying, treating, and preventing substance use disorder (SUD). While the importance of understanding the social and economic conditions of patients is a common component of medical training, the application of this notion to people who use drugs (PWUD) is less common (Yoast et al., 2008). Furthermore, training on the importance of patient socioeconomic conditions may not translate to an understanding of how medical professionals can play an active role in addressing them, through prevention, treatment, or policy advocacy.
Effectively addressing SUDs and their associated social determinants of health requires a collaborative, cross-sector approach involving not only health care systems and professionals, but also schools, social service organizations, and local communities. By working together, partners can have a greater impact and yield more significant outcomes. They can realize collective impact by fostering strategic partnerships to invest in and implement prevention programs and by improving both the capacity to treat SUDs and the awareness of available supportive service (Health and Human Services Office of the Surgeon General, 2016).
The urgency of such collaborative strategies has been underscored in an era marked by the COVID-19 pandemic, which has heightened society’s awareness of nonbiomedical influences on health. The pandemic has exacerbated risk factors for increased substance use and SUD, disrupting employment, housing, health care access, and social connection, and heightening fear, anxiety, financial stress, and grief—particularly among those with preexisting structural vulnerabilities (Collins et al., 2022). Pandemic-related stressors have been tied to escalation of the ongoing overdose epidemic and increases in substance use (Ghose, Forati, and Mantsch, 2022). For example, caregiving responsibilities, stress, depression, and anxiety were associated with increased substance use during the pandemic (Schmidt et al., 2021). After a historic 30 percent year-to-year increase in overdose fatalities from 2019 to 2020, estimates suggest that the United States again experienced a 15 percent increase in overdose fatalities in 2021, with a record-breaking 109,179 deaths—75 percent of which were related to opioids (Centers for Disease Control and Prevention, 2021). Overdose fatalities remained steady in 2022, with provisional data indicating 109,680 deaths (Ahmad et al., 2023).
Among those in the United States who died of overdose, the racial inequity that existed before the pandemic was amplified by the heavier economic, social, and health burdens carried by non-Hispanic Black individuals during the pandemic. This group had the greatest annual increase in drug-related overdose deaths in 2020 (Mistler et al., 2021; SAMHSA, 2020a). While rates of drug overdose death have consistently been higher among the White versus Black population, Black people have seen a 3.6-fold increase in overdose deaths since 2015, compared to the 1.7-fold increase among White individuals. In 2021, the age-adjusted drug death rates of Black (44 per 100,000) and American Indian/Alaskan Native (56 per 100,000) people were significantly higher than the rate for White people (36.8 per 100,000; National Center for Health Statistics, n.d.). To mitigate the worsening overdose crisis, the broader health and human services system must consider the structural and social determinants behind these growing disparities.
To make this case, this paper first explores the historical events that have informed the current US biomedical paradigm for SUD prevention, using the example of opioid use disorder (OUD), and the problems that have, in part, resulted from this approach. The authors then discuss how a socioecological framework—which considers the complex interplay among individual, interpersonal, societal, and structural factors—can offer a more comprehensive and effective means of understanding SUD prevention. The paper concludes with an exercise in which the authors apply a socioecological lens to the traditional public health model of OUD prevention, elucidating evidence-informed strategies and interventions across primary, secondary, and tertiary levels of prevention that aim not only to prevent disease but also to promote overall health and well-being.
The authors recognize the pivotal role the socioecological approach has played in shaping responses to various health conditions, including mental health conditions (Akers et al., 2023; National Institute on Minority Health and Health Disparities, 2017). However, despite its proven merits, the socioecological approach remains underused and its integration into the field of SUD prevention has been limited. Therefore, the primary purpose of this paper is to articulate the application of this approach and underscore its significance within the overarching context of SUD prevention. Further, this paper seeks to catalyze the expansion and uptake of this approach, empowering stakeholders to identify strategies that align with their circumstances and available resources.
From Moralization to Medicalization
The United States has a long history of politicizing, moralizing, and racializing drug use, a history that existed for nearly a century before President Richard Nixon formally declared the “war on drugs” in the 1970s (Rosino and Hughey, 2018). Political rhetoric preceding legislation that restricted or criminalized the possession of opium, cocaine, and cannabis featured statements that stoked fears of lost virtues and moral hygiene, and often cited unsubstantiated claims of the victimization of White women at the hands of people of certain races and ethnicities. For example, prior to the enactment of the 1914 Harrison Narcotics Act, proponents of racial prejudice warned Congress, claiming that “[m]ost of the attacks upon [W]hite women of the South are the direct result of a cocaine-crazed Negro brain” (Nunn, 2002). Congress passed the act, which regulated and taxed the production, importation, and distribution of opiates, and spurred federal agencies to prohibit physicians from prescribing opioids to persons with addiction, effectively initiating the criminalization of SUD in the United States at the federal level (Courtwright, 2015; Kleber, 2008).
Contrary to popular belief, the process of “scheduling”—which categorizes drugs based on their potential for abuse— as controlled substances was not informed by a systematic examination of relative drug risk, but rather by geopolitical and commercial interests and xenophobic ideologies that marginalized certain racial and ethnic populations (Daniels et al., 2021). For instance, the Controlled Substance Act of 1970, which laid the foundation for the current US drug scheduling system, emerged amid a broader cultural and political shift during the Nixon administration. Strategically aiming to neutralize the 1960s counterculture, the Nixon administration “knew [they] couldn’t make it illegal to be either against the war or [B]lack, but by getting the public to associate hippies with marijuana and [B]lacks with heroin, and then with criminalizing both heavily, [they] could disrupt those communities” (Baum, 2016).
In the ensuing years, US drug policy has consistently prioritized addressing the perceived moral outrage against drug use through tough-on-crime policies and a seemingly unrestricted cascade of federal dollars invested in drug interdiction (Shepard and Blackley, 2004). However, rather than serving as an effective public health strategy, this punitive approach has only served to perpetuate stigmatizing attitudes by erroneously associating drug use with social deviance and criminality (Dineen and Pendo, 2021). Prevention strategies have often relied on harsh criminal legal actions and fear-based educational campaigns, ostensibly to send a warning to individuals who might sell or use drugs. Nevertheless, research suggests that compulsory detention, other harsh criminal penalties, and youth-focused scare tactics have had little impact on reducing drug supply or curbing demand (Substance Abuse and Mental Health Services Administration, 2015; Global Commission on Drug Policy, 2011; Degenhardt et al., 2010).
To counter the prevailing erroneous theories of addiction as a moral failing, the medical community put forth the brain disease model, which expressed addiction in scientific terms, namely explaining that SUD resulted from a brain system that had been dysregulated by drug use (Heilig et al., 2021; Leshner, 1997). However, the mechanistic view of drugs “hijacking” the brain was not in conflict with the interdiction paradigm that similarly targeted drugs as the source of growing social ills. The mechanistic causal narrative continued to focus on regulating drugs and the drug supply instead of interrogating the social factors that drove the demand for drugs (El-Sabawi, 2019; Office of the Surgeon General, 2016; Institute of Medicine et al., 1994; Hawkins, Catalano, and Miller, 1992). In more recent years, and in response to greater attention to racial disparities in the criminal legal system, advocates within the medical community have called for reform of the criminal legal response to SUD and targeted broader social change, including increased access to housing, education, and health care (AMA, 2022; AMA, 2021; ASAM, 2021a; ASAM, 2021b; AMA, 2020).
From Medicalization to a Socioecological Approach
Prescriptive biomedical views of SUD prevention have led to simplistic problem statements and unidimensional solutions. For example, the United States experienced an excessive focus on increased opioid prescribing as a response to the opioid overdose crisis, often at the expense of supportive strategies (Dasgupta, Beletsky, and Ciccarone, 2018). The increase in prescribing stemmed from a complex interplay between predatory marketing of opioids and the need to address the undertreatment of chronic pain in the 1990s and early 2000s (DeWeerdt, 2019). However, the disproportionate emphasis on pharmaceuticals in the public narrative obscured other important drivers of the crisis, while fostering a defensive dynamic between patients and prescribers.
Key factors—such as the high prevalence of illicitly manufactured opioids, the counterproductive role of prohibition policies in creating an increasingly toxic drug supply, and evolving trends in substance use—have been largely overlooked. This reductionist view diverted attention from the myriad of contextual factors related to the onset and progression of SUD (Herzberg et al., 2016; Wailoo, 2014). A case in point is the rigid misapplication of prescribing limits outlined in the 2016 “CDC [Centers for Disease Control and Prevention] Guideline for Prescribing Opioids for Chronic Pain,” which contributed to many patients with pain who benefited from opioid therapy being nonconsensually tapered or denied further treatment (Kroenke et al., 2019; Dowell, Haegerich, and Chou, 2016). Consequently, some individuals resorted to seeking illicit alternatives for pain relief, paradoxically exacerbating the very issue that the guideline sought to address (Coffin et al., 2020).
The focus on reducing opioid prescriptions may have the veneer of a less punitive and more medical approach to preventing SUD but is still a supply-side narrative (El-Sabawi, 2019). Moreover, a purely biomedical focus for preventing SUD offers limited insight into the structural and systemic factors driving racial and ethnic disparities in overdose deaths.
Service providers and policy makers should consider how they can create a health-promoting environment regardless of whether an individual has ever used drugs, is diagnosed with SUD, or engages in high-risk substance use. Indeed, the health care industry depends on the biomedical model, with a focus on diagnosis, precise and prescriptive treatment, and decision-chart resolutions (Fricton et al., 2015). However, expanding the broader health care system’s understanding of prevention beyond the body’s mechanistic functions is critical to stemming the nation’s ongoing rise in overdoses and future substance use epidemics.
While it is now socially acceptable in many circles to state that addiction is not a moral failing—an advancement that goes against a long history of socially accepted condemnation of PWUD—the debate has now shifted to whether addiction is a brain disease, a chronic disease, or not a disease at all (Volkow and Boyle, 2018; Racine, Sattler, and Escande, 2017; Szalavitz, 2016; ASAM, n.d.). The conversation needs to be elevated beyond individual positions on the matter to include structural and societal factors. Here, the authors seek not to discredit the biomedical view but merely to provide support for more inclusive problem statements and solutions.
A Socioecological Theoretical Framework for SUD Prevention
A socioecological framework for SUD prevention recognizes the complex interactions between people and their environments at the individual, interpersonal, and macro levels (Agency for Toxic Substances and Disease Registry, 2015; Bronfenbrenner, 1979). Social epidemiologists have established causal mechanisms to support the application of a socioecological framework to health broadly and to clarify how structural and social determinants of health create socially patterned distributions of disease (Berkman, Kawachi, and Glymour, 2015; Krieger, Dorling, and McCartney, 2012; Glass and McAtee, 2006; Link and Phelan, 1995). Social epidemiologic research supports the assertion that the context in which individuals make health-related choices serves as a barrier to or facilitates health (Galea, Nandi, and Vlahov, 2004; DuBois, 2003). Race, often treated in biomedical perspectives as biologically defined (Ioannidis, Powe, and Yancy, 2021), is recognized as a socially constructed factor that is not biologically determined but does create differences in biological outcomes (Krieger, Dorling, and McCartney, 2012; Roberts, 2012).
Figure 1 illustrates the nested levels of factors considered in a socioecological framework, which have been highly simplified for the purpose of organizing the current argument. Macro-level factors, such as policies and practices, can have direct impacts on individuals’ health by subjecting them to stigma, trauma, and discrimination stemming from these broader influences. These experiences then physically manifest via stress response mechanisms (Hatzenbuehler et al., 2015; Geller et al., 2014). Additionally, macro-level factors shape the interpersonal structures in communities, influencing individuals’ access to resources and opportunities, and their health-related behaviors and beliefs. Importantly, the interplay among levels is interdependent and multidirectional, with influences at one level often facilitated or inhibited by elements at another level.
FIGURE 1. Examples of Nested Levels of Influence in a Socioecological Approach to Health.
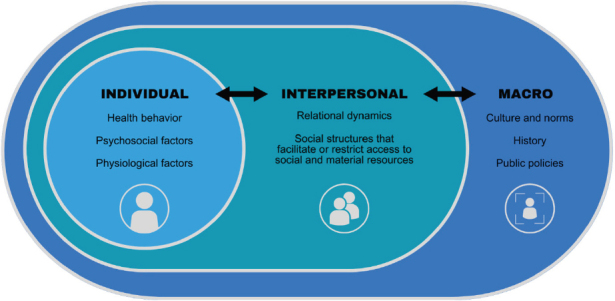
SOURCE: Developed by authors.
Understanding this interplay, social epidemiology recognizes that people make places and places make people (Macintyre and Ellaway, 2003). Due to the complex feedback loops and interactions between people and their environments (e.g., people may not buy healthy foods because stores do not carry healthy foods, and stores may not carry healthy foods because of a perception that people will not buy them), reductionist views of health can be antithetical to the socioecological perspective. While not the focus of this current work, the authors recognize that this complex person-environment interaction can occur across the life course and is intergenerational (Latimore et al., in press).
The application of a socioecological framework to SUD is not new (American Institutes for Research, 2022; Park et al., 2020; Jalali et al., 2020; Galea, Nandi, and Vlahov, 2004), but the addiction field has been slow to adopt the framework in practice. Macro-level risk factors such as restrictive drug policies and stigma isolate people with SUD from social and economic resources, such as services associated with SUD prevention, treatment, recovery, and harm reduction. These resources influence health at the individual level through physiological, psychosocial, and health behavior pathways. Similarly, racial disparities in SUD result from the experience of race in society and the distribution of economic and social resources that affect health. For the remainder of the paper, the authors focus on OUD, because of its relative contribution to the current overdose epidemic and the availability of resources targeted to OUD. However, the authors recognize the evolving nature of drug trends, the need for attention to other SUDs, and the applicability of this theoretical approach and related strategies to related SUDs.
Applying a Socioecological Framework for a More Nuanced View of OUD and Public Health Prevention
In the biomedical model of health and health care, prevention interventions have traditionally been classified according to three distinct levels: primary, secondary, and tertiary (Leavell and Clark, 1965). Primary prevention strategies aim to mitigate risk factors and prevent health conditions from ever developing. Secondary prevention interventions seek to identify a health condition as early as possible to halt or slow its progression. Tertiary prevention approaches strive to minimize acute negative consequences, like death, among those who have the disease.
In the context of OUD, a primary prevention approach under the traditional biomedical model aims to avoid the onset of OUD by, for example, educating clinicians and patients on alternative modalities and non-opioid medications for effective pain management to reduce exposure to prescribed opioids. Similarly, screening and referring patients to be prescribed medications for OUD constitute one approach to achieving the secondary prevention goal of identifying, diagnosing, and treating OUD as early as possible. Lastly, providing naloxone to those using opioids is an example of tertiary prevention, as naloxone can reduce the risk of opioid overdose and death among individuals with OUD.
While the primary, secondary, and tertiary classification can be useful for partitioning types of responses, its typical application to a biomedical model focuses on a clinical response and does not include efforts to address structural determinants of health and the complex interactions among the human body, the environment, and an individual’s life circumstances included in the socioecological perspective.
For example, negative stereotypes persist about people with OUD that do not exist for people with other chronic conditions; the latter are met with relatively clear pathways to additional testing, treatment, and support. Comparatively, upon discovery of their nonprescribed opioid use, too often individuals face judgement or blame and are left without connections to appropriate, evidence-based care (Tsai et al., 2019). Such counterproductive interactions with health care professionals and the health care system deter individuals from seeking help at critical moments before and after the development of OUD and associated negative health and social consequences. Widespread recognition that OUD is a treatable condition, and that stigmatizing language has negative impacts on people with OUD, is critical for reducing the continuous rise in overdoses.
The primary, secondary, and tertiary prevention classification is somewhat ill fitting for the nonlinear nature of addiction and other chronic health conditions, particularly if the treatment approach does not consider the social and environment factors impacting disease and health. OUD is a medical diagnosis defined by a pattern of opioid use that leads to problems or distress (e.g., physical, mental, interpersonal, and financial; American Psychiatric Association, 2013). Most people who are exposed to opioids do not develop OUD. Of the estimated 10.1 million individuals 12 years or older who reported problematic use of opioids in 2019, 1.6 million met The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, criteria for OUD (SAMHSA, 2020b). Among individuals prescribed opioids long term for chronic pain, between 8 percent and 12 percent will develop an addiction to opioids, although nuance exists in the reported estimates (Dowell, Haegerich, and Chou, 2016; Volkow and McLellan, 2016; Vowles et al., 2015). Individuals can move in and out of the “diagnosed” and “high-risk” categories as they reduce their drug use and no longer meet the criteria for OUD. Among those with an OUD diagnosis, the extent to which they participate in drug use behaviors that place them at high risk for overdose can fluctuate.
The definitions of recovery and remission are hotly debated topics that involve differing schools of thought (Office of the Surgeon General, 2016). While there is general agreement that recovery involves achieving a state of improved well-being, varying perspectives exist on the nature of addiction, the goals of treatment, the necessity of treatment, and the possibility of complete remission. At one end of the spectrum, proponents argue that long-term abstinence is the primary criterion for recovery. Conversely, alternative schools of thought adopt a more inclusive approach to recovery, recognizing that complete abstinence may not be immediately feasible or desirable for everyone. Instead, they emphasize harm reduction approaches and focus on positive behavior changes and improved well-being as indicators of recovery.
Socioecological Levels of Prevention for OUD
To address the limitations of the classical prevention categorizations, the authors have recast OUD prevention with a socioecological framework that recognizes the nonlinear interconnectivity between people and their environments. Hood et al. (2016) estimate that individual health behavior accounts for about one-third of health outcomes; the remaining two-thirds of health factors can be broadly defined as social determinants and include social and economic factors (47 percent), the physical environment (3 percent), and access to quality health care (16 percent). These social determinants can be broken into two categories: risk factors and protective factors. Protective factors—such as community safety, supportive relationships, financial stability, and access to care—are associated with positive health outcomes. Conversely, unsafe living conditions, food insecurity, poverty, and social isolation are associated with negative health outcomes.
Risk and protective factors exist within the contexts in which a person interacts and exists. Combining the socioecological framing of risk and protective factors with the classical framing of prevention (Figures 2, 3, and 4) is a start to identifying individual, interpersonal, and macro-level strategies that can promote or deter health for those at different stages of the prevention continuum.
FIGURE 2. Primary Prevention: Examples of Risk and Protective Factors for Those at Risk for Developing Opioid Use Disorder.
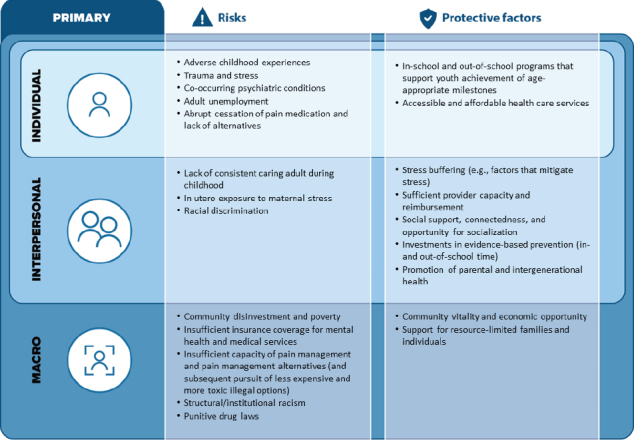
SOURCE: Latimore A. D., E. Salisbury-Afshar, N. Duff, E. Freiling, B. Kellett, R. Sullenger, A. Salman, and the Prevention, Treatment, and Recovery Services Working Group of the National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic. 2023. Primary, Secondary, and Tertiary Prevention of Opioid Use Disorder through Socioecological Strategies. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202309b.
NOTE: Figure created by American Institutes for Research. Copyright 2023. All rights reserved.
FIGURE 3. Secondary Prevention: Examples of Risks and Protective Factors for Those with Opioid Use Disorder.
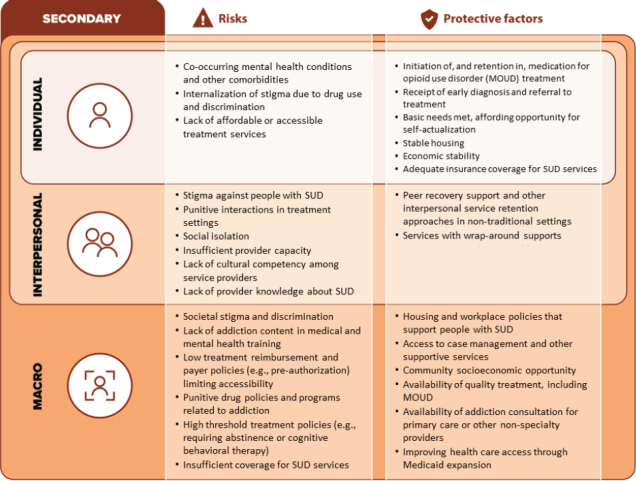
SOURCE: Latimore A. D., E. Salisbury-Afshar, N. Duff, E. Freiling, B. Kellett, R. Sullenger, A. Salman, and the Prevention, Treatment, and Recovery Services Working Group of the National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic. 2023. Primary, Secondary, and Tertiary Prevention of Opioid Use Disorder through Socioecological Strategies. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202309b.
NOTE: Figure created by American Institutes for Research. Copyright 2023. All rights reserved.
FIGURE 4. Tertiary Prevention: Examples of Risks and Protective Factors for Those at Risk for Acute Consequences of Opioid Use Disorder.
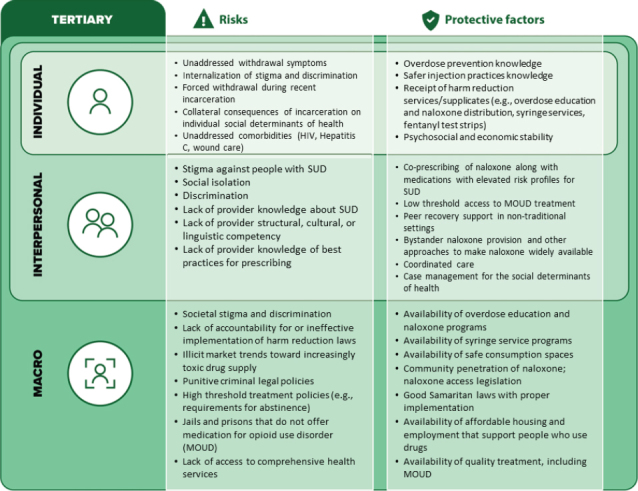
SOURCE: Latimore A. D., E. Salisbury-Afshar, N. Duff, E. Freiling, B. Kellett, R. Sullenger, A. Salman, and the Prevention, Treatment, and Recovery Services Working Group of the National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic. 2023. Primary, Secondary, and Tertiary Prevention of Opioid Use Disorder through Socioecological Strategies. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202309b.
NOTE: Figure created by American Institutes for Research. Copyright 2023. All rights reserved.
Primary Prevention of OUD Using a Socioecological Model
Primary prevention using a socioecological framework seeks to prevent the onset of disease and acknowledges that an individual’s risk of developing OUD is shaped by a combination of intersecting biopsychosocial and environmental risk and protective factors, as outlined in Figure 2. Evidence-based primary prevention interventions address both biopsychosocial and environmental risk and protective factors at the individual, interpersonal, and macro levels to prevent the onset of OUD (Office of the Surgeon General, 2016).
An example could involve adverse childhood experiences (ACEs) and positive childhood experiences (PCEs), which both play crucial roles in shaping a person’s life trajectory. ACEs—which encompass negative, stressful, and traumatizing events that occur before the age of 18—are strongly associated with increased risk of developing OUD over the life span (Guarino et al., 2021). On the other hand, PCEs, such as supportive relationship and safe environments, can act as protective factors against the harmful effects of ACEs (Bethell et al., 2019). Factors that contribute to ACEs include the lack of a consistent caring adult during childhood and/or growing up with food insecurity, while factors that promote PCEs involve creating and sustaining safe, stable, and nurturing relationships and environments in which children and families can thrive (CDC, 2022; CDC, 2019). Recognizing the prevalence of ACEs and their strong association with opioid use and related behavioral health outcomes, it is crucial to prioritize prevention of ACEs. Further research is needed to describe the cultivation of PCEs and impact on incidence of OUD. (National Academies of Science, Engineering, and Medicine, 2019).
Applying the socioecological lens to primary prevention provides targets at the individual, interpersonal, and macro levels for preventing the onset of OUD (Figure 2). Examples of interventions at each of these levels include the following:
Individual: Mentoring and Out-of-School Programs
Research demonstrates that school completion, stable career employment, and quality relationships are associated with reduced high-risk substance use patterns, including opioid use, leading into young adulthood (Merrin et al., 2020). Mentoring and out-of-school programs—such as Big Brothers Big Sisters of America (n.d.), After School Matters (n.d.), and Powerful Voices (n.d.)—support the growth and development of youth and adolescents by addressing the need for positive adult contact and offering skills development opportunities, resources, and platforms. The enhanced support helps to increase confidence and foster professional values, such as leadership, teamwork, and respect, all of which have been shown to reduce problematic drug use among youth (Erdem and Kaufman, 2020; CDC, 2019).
Interpersonal: Family Support Programs
Data support the assertion that close family relationships can ameliorate the impact that trauma, stress, and adversity have on an individual’s physical health over their life span (Chen, Brody, and Miller, 2017; Brody et al., 2016). Culturally relevant and asset-based family support programs, such as the Strong African American Families Program (University of Georgia, Center for Family Research, n.d.), help to foster positive family environments and improve supportive parenting practices, including positive racial socialization, communication, and consistent discipline, thereby enhancing parents’ and caregivers’ efforts to help youth develop positive goals as well as skills to resist involvement in risk behaviors, like early initiation of opioid or other drug use (Brody et al. 2006).
Macro: Federal and State Policies and/or Investments That Support Resource-Limited Families
The harmful effects of economic hardship and financial instability on child health and development are well documented (Sandstrom and Huerta, 2013). Research shows that when families can meet their basic needs—such as food, housing, and health care—parents and caregivers can better provide the critical emotional and material support that children need to grow into healthy, productive adults (Masten, Lombardi, and Fisher, 2021). Policies and investments in social programs—including livable minimum wage requirements, child care subsidies, and federal tax credits—can be important levers to reduce the strain on low-income families to meet their basic needs, thereby reducing socioeconomic risks for parents and their children, which in turn decreases the risk of developing OUD (Cooper, Mokhiber, and Zipperer, 2021; Milligan and Stabile, n.d.).
For additional examples of socioecological primary prevention interventions for OUD, please refer to Table A-1.
Table A-1. Evidence-Based Interventions at the Primary Level of Prevention.
| I. Targeted Level of Action | II. Risk(s) at the Targeted Level of Action | III. Protective Factor(s) Addressed | IV. Intervention | V. Intervention Description | VI. Examples of Programs/Models |
|---|---|---|---|---|---|
| Individual | Adult unemployment | Social support, connectedness, and opportunity for socialization | Out-of-school programs | School completion, obtaining stable career employment, and quality relationships are associated with reducing high-risk substance use patterns leading into young adulthood. [1] |
1. Powerful Voices:
https://www.powerfulvoices.org/about 2. Big Brothers Big Sisters of America: https://www.bbbs.org/ 3. After School Matters: https://www.sesp.northwestern.edu/docs/publications/1070224029553e7f678c09f.pdf |
| In-school and out-of-school programs that support youth achievement of age-appropriate milestones | Mentoring and out-of-school programs (such as Big Brothers Big Sisters of America, After School Matters, and Powerful Voices) support the growth and development of youth and adolescents by offering skills development opportunities, resources, and platforms that help to increase confidence and foster professional values, such as leadership, teamwork, and respect. These qualities have been shown to reduce the use of drugs and drug-related activity. [2] | ||||
| Interpersonal | Adverse childhood experiences | Promotion of parental and intergenerational health | Family skills training programs | Family skills training programs (such as the Nurse-Family Partnership and Strengthening Families Program) empower and support vulnerable and high-risk families by equipping them with tools and resources that help to reduce risk factors (e.g., substance misuse) and improve protective factors, leading to improved health and life outcomes. [3,4] |
1. Nurse-Family Partnership:
https://www.nursefamilypartnership.org/about/ 2. Strengthening Families Program: https://strengtheningfami-liesprogram.org/ |
| In utero exposure to maternal stress | |||||
| Interpersonal | Adverse childhood experiences | Stress buffering (e.g., factors that mitigate stress) | Support programs focused on strengthening the family environment | Family support programs, such as the Strong African American Families Program, help to foster positive family environments and thus reduce the impact that childhood stressors can have on biological processes and health behaviors over one’s lifetime, including the development of risky behaviors like substance misuse. [5,6] | 1. Strong African American Families Program: https://cfr.uga.edu/saaf-programs/saaf/ |
| Promotion of parental and intergenerational health | |||||
| Interpersonal | Racial discrimination | Prejudice habit-breaking strategies | Intervention strategies can reduce the implicit bias of service providers (e.g., stereotype replacement, perspective taking, individuation). Such interventions include Multi-Faceted Prejudice Habit-Breaking Intervention and also increase bias awareness and concern about discrimination. Thus, they help to decrease social stressors that can impact the biological processes and health behaviors that can lead to substance use and development of a SUD. [7,8] | 1. Long-Term Reduction in Implicit Bias: A Prejudice Habit-Breaking Intervention: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3603687/ | |
| Interpersonal | Adverse childhood experiences | Investment in evidence-based prevention (in- and out-of-school time) | Social-emotional learning programs | Social-emotional learning programs—such as LifeSkills Training, the Good Behavior Game, and Promoting Alternative THinking Strategies (PATHS)—promote positive behavior and help youth and adolescents to develop emotional and social competencies, leading to a range of positive outcomes, including reduced youth alcohol, tobacco, and drug use; depression; anxiety; and suicidal thoughts. [9,10,11,12] |
1. LifeSkills Training:
https://www.lifeskillstraining.com/lst-overview/ 2. Good Behavior Game: https://goodbehavior-game.air.org/about_gbg.html 3. PATHS: https://nationalgangcenter.ojp.gov/spt/Programs/104 |
| Interpersonal |
Adverse childhood events In utero exposure to maternal stress |
Promotion of parental and intergenerational health | Social determinants of health and adverse childhood events screening in primary care settings, with followup and linkage services | The integration of screening for social determinants of health and adverse childhood events in primary care settings helps primary health care professionals address common psychosocial problems, such as parental depression and substance use. This integration also provides early intervention and counsel, which may lead to reduced child maltreatment. [13,14] | 1. Safe Environment for Every Kid: https://seekwellbeing.org/about-seek-2/ |
|
Interpersonal (teacher/student) Macro (state and local school systems) |
Trauma and stress Co-occurring psychiatric conditions |
Investment in evidence-based prevention (in- and out-of-school time) | Wellness and resilience programs | Wellness and resilience programs, such as Project Advancing Wellness and Resiliency in Education (AWARE), focus on building partnerships between state and local school systems to increase awareness of mental illness among school-aged children. The programs also provide school personnel with the skills and training necessary to identify mental health problems and connect students in need of care. Such programs can improve student support at school, which has been shown to help decrease the prevalence of nonmedical use of prescription drugs among school-aged children. [15,16,17] | 1. Project AWARE: https://www.samhsa.gov/grants/grant-announcements/sm-20-016 |
| Macro | Insufficient insurance coverage for mental health and medical services | Accessible and affordable health care services | Medicaid expansion | The Affordable Care Act provided state funds to expand Medicaid to adults with incomes below 138 percent of the federal poverty level. The expansion gave millions of previously uninsured adults coverage and expanded access to services that can reduce the risk of an SUD, such as mental, behavioral, and physical health care for chronic conditions. [18,19] | 1. Status of State Medicaid Expansion Decisions: https://www.kff.org/medicaid/issue-brief/status-of-statemedicaid-expansion-decisions-interactive-map/ |
| Macro | Community disinvestment and poverty | Support for resource-limited families and individuals | Federal and state policies and/or investments that support resource-limited families |
Macro-level policies reduce low-income families’ strain to meet basic needs and decrease socioeconomic risks for parents and their children. They also decrease risk for SUD. [20,21,22] Examples include the following:
|
1. Child Cash Benefits: https://www.nber.org/papers/w21101 |
| Macro | Insufficient capacity of pain management alternatives (and subsequent pursuit of less expensive and more toxic illegal options) | Accessible and affordable health care services | Policies that expand access to pain management | Policies that expand coverage of non-opioid pain management alternatives improve access to high-quality, evidence-based pain care and decrease opioid overuse and exposure. [23] | 1. Medicaid Strategies for Non-Opioid Pharmacologic and Non-Pharmacologic Chronic Pain Management: https://www.medicaid.gov/federal-policy-guidance/downloads/cib022219.pdf |
| Macro | Community disinvestment and poverty | Support for resource-limited families and individuals | Homelessness diversion programs | While social selection and social adaptation explain the relationship between homelessness and substance misuse, research suggests a greater proportion of individuals develop an SUD after experiencing homelessness. [24,25] Programs such as Bridges to Housing Stability aim to prevent homelessness by helping individuals identify immediate alternate housing arrangements and connecting them with services and financial assistance to help them return to permanent housing, if necessary. [26,27] |
1. Michigan’s Shelter Diversion Pilot Program:
https://www.michigan.gov/mshda/homeless/homeless-and-special-housing-needs-programs/shelter-diversion-pilot 2. Bridges to Housing Stability: https://bridges2hs.org/bridges-housing-stability-programs/ |
Sources
Merrin, G. J., M. E. Ames, C. Sturgess, and B. J. Leadbeater. 2020. Disruption of transitions in high-risk substance use from adolescence to young adulthood: school, employment, and romantic relationship factors. Substance Use & Misuse 55(7):1129–1137.https://doi.org/10.1080/10826084.2020.1729200.
CDC (Centers for Disease Control and Prevention). 2019. Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence. Available at: https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf (accessed April 28, 2022).
Nurse-Family Partnership. n.d. Evidence of Effectiveness. Available at: https://www.nursefamilypartnership.org/about/proven-results/evidence-of-effectiveness/ (accessed April 11, 2022).
Center for the Study of Social Policy. n.d. The Research Behind Strengthening Families. Available at: https://cssp.org/our-work/projects/the-research-behind-strengthening-families/ (accessed April 11, 2022).
Brody, G. H., G. E. Miller, T. Yu, S. R. H. Beach, and E. Chen. 2016. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: A replication across two longitudinal cohorts. Psychological Science 27(4):530–541.https://doi.org/10.1177/0956797615626703.
Chen, E., G. H. Brody, and G. E. Miller. 2017. Childhood close family relationships and health. American Psychologist 72(6):555–566. https://doi.org/10.1037/amp0000067.
Amaro, H., M. Sanchez, T. Bautista, and R. Cox. 2021. Social vulnerabilities for substance use: Stressors, socially toxic environments, and discrimination and racism. Neuropharmacology 188:108518. https://doi.org/10.1016/j.neuropharm.2021.108518.
McCabe, S. E., W. B. Bostwick, T. L. Hughes, B. T. West, and C. J. Boyd. 2010. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health 100(10):1946–1952. https://doi.org/10.2105/ajph.2009.163147.
CDC. 2019. Preventing adverse childhood experiences: leveraging the best available evidence. Available at: https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf (accessed April 28, 2022).
Wilcox, H. C., S. G. Kellam, C. H. Brown, J. M. Poduska, N. S. Ialongo, W. Wang, and J. C. Anthony. 2008. The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence 95:S60–S73. https://doi.org/10.1016/j.drugalcdep.2008.01.005.
Kellam, S. G., C. H. Brown, J. M. Poduska, N. S. Ialongo, W. Wang, P. Toyinbo, H. Petras, C. Ford, A. Windham, and H. C. Wilcox. 2008. Effects of a universal classroom behavior management program in first and second grades on young adult behavioral, psychiatric, and social outcomes. Drug and Alcohol Dependence 95:S5–S28. https://doi.org/10.1016/j.drugalcdep.2008.01.004.
Botvin, G. J., K. W. Griffin, and T. D. Nichols. 2006. Preventing youth violence and delinquency through a universal school-based prevention approach. Prevention Science 7(4):403–408. https://doi.org/10.1007/s11121-006-0057-y.
Poleshuck, E., K. Possemato, E. M. Johnson, A. J. Cohen, C. T. Fogarty, and J. S. Funderburk. 2022. Leveraging integrated primary care to address patients’ and families’ unmet social needs: aligning practice with National Academy of Sciences, Engineering and Medicine recommendations. The Journal of the American Board of Family Medicine 35(1):185. https://doi.org/10.3122/jabfm.2022.01.210287.
Eismann, E. A., J. Theuerling, S. Maguire, E. A. Hente, and R. A. Shapiro. 2018. Integration of the Safe Environment for Every Kid (SEEK) model across primary care settings. Clinical Pediatrics 58(2):166–176. https://doi.org/10.1177/0009922818809481.
Project Cal-Well. 2021. Project Cal-Well: 2020-21 Evaluation Highlights. San Francisco, CA: UCSF School Health Evaluation and Research Team. Available at: https://schoolhealthresearch.ucsf.edu/sites/g/files/tkssra8116/f/wysiwyg/Project%20Cal-Well%202020-21%20California%20Evaluation%20Highlights.pdf (accessed August 22, 2023).
Pacific Institute for Research and Evaluation. 2021. State of South Dakota Project AWARE 2021 Annual Evaluation Report. Chapel Hill, NC. Available at: https://doe.sd.gov/publications/documents/SD-AWARE-21.pdf (accessed April 11, 2022).
Georgia Department of Education. n.d. Supporting student wellness and resilience by all means possible. Georgia Project AWARE Digest S2019. Available at: https://cld.gsu.edu/files/2020/11/Georgia-Project-Aware-Digest-Sp19.pdf (accessed August 22, 2023).
Winkelman, T. N. A., and V. W. Chang. 2018. Medicaid expansion, mental health, and access to care among childless adults with and without chronic conditions. Journal of General Internal Medicine 33(3):376–383. https://doi.org/10.1007/s11606-017-4217-5.
Maclean, J. C., and B. Saloner. 2019. The effect of public insurance expansions on substance use disorder treatment: evidence from the Affordable Care Act. Journal of Policy Analysis and Management 38(2):366–393.
Cooper, D., Z. Mokhiber, and B. Zipperer. 2021. Raising the federal minimum wage to $15 by 2025 would lift the pay of 32 million workers. Washington, DC: Economic Policy Institute. Available at: https://www.epi.org/publication/raising-the-federal-minimum-wage-to-15-by-2025-would-lift-the-pay-of-32-million-workers/ (accessed April 11, 2022).
Milligan, K., and M. Stabile. n.d. Do child tax benefits affect the wellbeing of children? Evidence from Canadian child benefit expansions. Vancouver and Toronto, Canada. Available at: https://sticerd.lse.ac.uk/dps/pep/pep01.pdf (accessed April 11, 2022).
National Academies of Sciences, Engineering, and Medicine. 2019. A roadmap to reducing childhood poverty. Washington, DC: The National Academies Press. https://doi.org/10.17226/25246.
Lin, D. H., C. M. Jones, W. M. Compton, J. Heyward, J. L. Losby, I. B. Murimi, G. T. Baldwin, J. M. Ballreich, D. A. Thomas, M. Bicket, L. Porter, J. C. Tierce, and G. C. Alexander. 2018. Prescription drug coverage for treatment of low back pain among US Medicaid, Medicare Advantage, and commercial insurers. JAMA Network Open 1(2):e180235. https://doi.org/10.1001/jamanetworkopen.2018.0235.
Johnson, T. P., S. A. Freels, J. A. Parsons, and J. B. Vangeest. 1997. Substance abuse and homelessness: social selection or social adaptation? Addiction 92(4):437–445.https://doi.org/10.1111/j.1360-0443.1997.tb03375.x.
Johnson, G., and C. Chamberlain. 2008. Homelessness and substance abuse: which comes first? Australian Social Work 61(4):342–356. https://doi.org/10.1080/03124070802428191.
Evans, W. N., J. X. Sullivan, and M. Wallskog. 2016. The impact of homelessness prevention programs on homelessness. Science 353(6300):694–699. https://doi.org/doi:10.1126/science.aag0833.
Connecticut Coalition to End Homelessness. 2015. Early analysis of CAN diversion data. Hartford, CT. Available at: https://cceh.org/early-analysis-of-can-diversion-data/ (accessed April 12, 2022).
NOTES: Some interventions address both risks and protective factors; other interventions may address only one.
The interventions included in the table have been limited to those with promising evidence to reduce the risks associated with precursors of SUD, SUD incidence, SUD morbidity, or SUD-related mortality; however, their inclusion does not suggest, and should not be taken as, an endorsement by the National Academy of Medicine or any of the authors’ organizations. Additionally, it should be noted that this table does not encompass an exhaustive list of all primary level interventions.
The selection process involved a thorough review of existing scientific literature, including published studies, meta-analyses, systematic reviews, and program evaluations. In determining the inclusion of interventions, the authors considered various factors, such as the strength of evidence supporting the program’s effectiveness, the quality of research studies conducted on the intervention, the consistency of positive outcomes across multiple studies, and the intervention’s relevance to the prevention of OUD and its associated risks.
Secondary Prevention of OUD Using a Socioecological Model
Secondary prevention interventions using a socioecological framework focus on biopsychosocial and environmental strategies that target early identification of OUD and support for those with OUD. As illustrated in Figure 3, several risk factors impede and/or challenge the success of screening and treatment referral, including stigma, discrimination, and insufficient provider competency and/or knowledge, all of which can influence an individual’s engagement in their health and human services.
Applying the socioecological lens to secondary prevention provides targets at the individual, interpersonal, and macro levels for supporting those in the early or mild stages of OUD. Examples of interventions at each of these levels include the following:
Individual: Access to Trauma-Informed Care
Based on a large population-based survey, an estimated 50 percent to 60 percent of adults in the United States have experienced some type of traumatic event at least once in their lives (Husarewycz et al., 2014). Given the strong link between exposure to trauma and OUD, receiving trauma-informed care—which includes considering a person’s traumatic experiences when providing care and adopting policies, procedures, and practices that avoid retraumatization and support healing and recovery—can help to improve patient engagement, OUD treatment adherence, and health outcomes (SAMHSA, 2014a).
Interpersonal: Training in Structural and Cultural Competency
Culturally and linguistically diverse populations face greater challenges to accessing OUD treatment (Gainsbury, 2016). Consequently, it is vital that health and treatment providers create a more inclusive care environment by developing a greater awareness and understanding of the cultural, structural, and linguistic factors that may help their patients feel more comfortable in accessing care. Training and education programs for health professionals that focus on developing cultural and structural competencies—such as the National Culturally and Linguistically Appropriate Services Standards (Office of Minority Health, n.d.)—can help to improve patient engagement in services, therapeutic relationships between patients and providers, and treatment retention and outcomes to advance health equity (Jones and Branco, 2021; SAMHSA, 2014b).
Macro: Comprehensive, Interprofessional Addiction Curricula and Training Programs
OUD touches nearly every aspect of the health care system. Individuals who experience a nonfatal opioid overdose are likely to interact with at least one health professional in the six months preceding their overdose (Wagner et al., 2015). Given this context, it is critical that all health professionals have the requisite knowledge, skills, abilities, and attitudes to effectively identify and support those with problematic substance use. Adoption of interprofessional curricula and training programs, such as those outlined in the National Academy of Medicine’s 3Cs Framework for Pain and Unhealthy Substance Use (Holmboe et al., 2022), provide the opportunity to better prepare health professionals across the care continuum to identify and meet the complex and varied needs of patients with unhealthy substance use behaviors. (See Table A-2 for additional examples of secondary prevention interventions using the socioecological framework.)
Table A-2. Evidence-Based Interventions at the Secondary Level of Prevention.
| Secondary Prevention | |||||
|---|---|---|---|---|---|
| I. Targeted Level of Action | II. Risk(s) at the Targeted Level of Action | III. Protective Factor(s) Addressed | IV. Intervention | V. Intervention Description | VI. Examples of Programs/Models |
| Individual | Stigma against people with an SUD | Access to trauma-informed care | Trauma-informed care, an evidence-based approach, encourages health care providers to consider a person’s traumatic experiences when providing care. It also encourages providers to adjust policies, procedures, and practices to minimize perceived threats, avoid retraumatization, and support healing and recovery. Having access to this type of care has been shown to improve an individual’s engagement with care, adherence to SUD treatment, and overall health outcomes. [28] |
1. CA Bridge—Trauma-Informed Care for Opioid Use Disorder:
https://cabridge.org/resource/trauma-informed-care-for-opioid-use-disorder/ 2. The Missouri Model: A Developmental Framework for Trauma-Informed Approaches: https://dmh.mo.gov/media/pdf/missouri-model-developmental-framework-trauma-informed-approaches |
|
| Interpersonal | Services with wraparound supports | Community-based care management | An interpersonal care management approach combines the benefits of clinical care services with the ongoing support of community-based care coordination. Community-based care management can improve health outcomes for those with SUD and enhance efficiency along the care continuum. [29,30] |
1. Camden Core Model:
https://camden-health.org/care-interventions/camden-core-model/ 2. Michigan Medicaid Program’s substance use disorder community-based treatment: https://www.wmcmhs.org/wp-content/uploads/2019/10/Attachment-A-SUD-Community-Based-Treatment.pdf |
|
| Interpersonal | Social isolation | Peer recovery support and other interpersonal retention approaches in nontraditional settings | Peer recovery support services | These services are designed and delivered by people who have experienced both SUD and recovery. Such an approach can help people become and stay engaged in the recovery process and reduce the likelihood of relapse. [31] |
1. Enhancing Permanency in Children and Families:
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10668-1 2. Imani Breakthrough Project: https://www.tandfonline.com/doi/abs/10.1080/15332985.2021.1930329 |
| Interpersonal | Lack of cultural competency among service providers |
Culturally relevant and linguistically appropriate services Training in structural competence |
National Culturally and Linguistically Appropriate Services (CLAS) are respectful of, and responsive to, the health beliefs, practices, and needs of diverse populations. [32] These services help to advance health equity, improve quality, and reduce health care disparities. For behavioral health specifically, CLAS can improve client engagement in services, therapeutic relationships between clients and providers, and treatment retention and outcomes. [33] However, providers should also be trained in structural competency and recognize that different economic and sociopolitical conditions can shape the interpersonal interactions between a provider and patient, thus affecting outcomes. |
1. Incorporating a Race Equity Framework into Opioid Use Disorder Treatment:
https://link.springer.com/chapter/10.1007/978-3-030-80818-1_13 2. Structural Competency in Mental Health and Medicine: https://link.springer.com/book/10.1007/978-3-030-10525-9 |
|
| Macro | Punitive drug policies and programs related to addiction | Community socioeconomic opportunity | Restorative justice reinvestment | Macro-level policies aim to reinvest savings and revenues previously channeled into criminal justice systems into productive, community-based initiatives that aim to tackle the underlying problems that give rise to criminal behaviors, including risky substance use. Examples of initiatives include the following:
|
1. Justice Reinvestment Initiative:
https://csgjusticecenter.org/projects/justice-reinvestment/ 2. California Community Reinvestment Grants Program: https://www.grants.ca.gov/grants/california-communityreinvestment-grants-program/ |
| Macro | Availability of quality treatment, including medications for opioid use disorder (MOUD) | MOUD | Medications for OUD include buprenorphine, methadone, and extended-release naltrexone. Individuals who receive MOUD are more likely to remain in treatment and less likely to use illicit opioids, compared to individuals who receive treatment services without medication. Buprenorphine and methadone have also been shown to reduce opioid-related mortality. Although counseling should not be required to initiate or continue MOUD, case management and counseling services should be offered when available. [34,35] |
1. Medication-Assisted Treatment Models of Care for Opioid Use Disorder in Primary Care Settings:
https://www.ncbi.nlm.nih.gov/books/NBK402343/ 2. Primary Care-Based Models for the Treatment of Opioid Use Disorder: A Scoping Review: https://pubmed.ncbi.nlm.nih.gov/27919103/ 3. Innovations in Methadone Medication for Opioid Use Disorder—A Scoping Review: https://www.nationalacademies.org/documents/embed/link/LF2255DA3DD1C41C0A42D-3BEF0989ACAECE3053A6A9B/file/D5D2AC018C5BED2881735AC4FF36BEA0CF2C89ED2803 4. Medications for Opioid Use Disorder Save Lives: https://nap.nationalacademies.org/catalog/25310/medications-for-opioid-use-disorder-save-lives |
|
| Macro | Societal stigma and discrimination | Housing and workplace policies that support people with SUD | Housing First Model | This homelessness assistance approach is premised on the philosophy that all people deserve housing and that adequate housing is a precondition for recovery from addiction. The model prioritizes providing permanent, stable housing and additional support services without a requirement of abstinence. [36,37] |
1. Pathways to Housing PA:
https://pathwaystohousingpa.org/ 2. Housing First in Canada: https://www.homelesshub.ca/sites/default/files/HousingFirstInCanada.pdf |
| Macro | Societal stigma and discrimination | Housing and workplace policies that support people with SUD | Workplace supported recovery | In this approach, employers use evidence-based policies and programs to prevent exposure to workplace risk factors that could cause or perpetuate SUD. Employers also lower barriers to seeking care, receiving care, and maintaining recovery. |
1. CDC’s Workplace Supported Recovery Program:
https://www.cdc.gov/niosh/topics/opioids/wsrp/default.html 2. Recovery Friendly Workplaces Pennsylvania: https://recoveryfriendlypa.org/ 3. Nevada Recovery Friend Workplace Toolkit: https://www.opioidlibrary.org/wp-content/uploads/2020/12/Nevada-Recovery-Friendly-Workplace-Toolkit.pdf |
| Macro | Low treatment reimbursement and payer policies (e.g., preauthorizations) limiting accessibility | Enforcement of mental health and SUD parity laws | The Mental Health Parity and Addiction Equity Act (MHPAEA) requires most health plans to apply similar rules to mental health and SUD benefits as those applied to medical/surgical benefits, but enforcement of these laws has not been universal. [38,39] The Consolidated Appropriations Act of 2021 requires group health plans to provide to the Departments of Labor and Health and Human Services an evaluation of their compliance with the MHPAEA (e.g., visit limits, pre-authorization requirements, comparative analyses with medical/surgical coverage). [40] Enforcement of MHPAEA is critical to ensuring access to mental health and SUD treatment. |
1. ParityTrack—State parity reports:
https://www.paritytrack.org/reports/#state-disparities 2. Know Your Rights: Parity for Mental Health and Substance Use Disorder Benefits: https://store.samhsa.gov/product/know-your-rights-parityfor-mental-health-substance-use-disorder-benefits/pep21-05-00-003 3. Understanding Parity: A Guide to Resources for Families and Caregivers: https://store.samhsa.gov/product/understanding-parity-guide-to-resources-for-families-caregivers/pep2105-00-002 4. The Essential Aspects of Parity: A Training Tool for Policymakers: https://store.samhsa.gov/product/essential-aspects-of-parity-training-tool-for-policymakers/pep21-05-00-001 |
|
| Macro | Low treatment reimbursement and payer policies (e.g., preauthorizations) limiting accessibility | Section 1115 waiver demonstrations for behavioral health | Section 1115 of the Social Security Act gives the secretary of the Department of Health and Human Services the authority to approve demonstration projects that are likely to assist in promoting the objectives of the Medicaid program. Demonstration projects for behavioral health, such as California’s Whole Person Care pilot program, can improve access to and integration of behavioral health services, including SUD care, for high-risk, high-cost patient populations. [41,42] | 1. Integrating Health and Human Services in California’s Whole Person Care Medicaid 1115 Waiver Demonstration: https://www.healthaffairs.org/doi/10.1377/hlthaff.2019.01617 | |
| Macro | Lack of addiction content in medical and mental health training | Comprehensive, interprofessional addiction curricula and training programs | These curricula and training programs reflect the interdisciplinary nature of effective SUD care and educate health professionals to approach SUD like other chronic conditions. [43] These programs can better prepare health professionals to more proactively identify and address the complex needs of patients with unhealthy substance use. |
1. Coalition on Physician Education in Substance Use Disorder (COPE) Curriculum Innovation Challenge:
https://www.copenow.org/curriculuminnovation-challenge-2-0/ 2. The 3Cs Framework for Pain and Unhealthy Substance Use: Minimum Core Competencies for Interprofessional Education and Practice: https://doi.org/10.31478/202206a |
|
| Macro | Lack of addiction content in medical and mental health training | Availability of addiction consultation for primary care or other nonspecialty providers |
Telementoring Peer-to-peer consultation On-call technical assistance |
Collaborative approaches may be aided by the use of virtual platforms—which allow clinicians to speak to specialists to get input on clinical cases, SUD diagnoses, and management. Such platforms, in effect, extend the reach of specialty care providers. [44,45,46] |
1. Maryland Addiction Consultation Services:
https://www.marylandmacs.org/ 2. Massachusetts Consultation Service for Treatment of Addiction and Pain: https://www.mcstap.com/ 3. UCSF Substance Use Warmline: https://nccc.ucsf.edu/clinical-resources/substance-use-resources/ |
| Macro | Availability of addiction consultation for primary care or other nonspecialty providers | Integrated, collaborative care models | Collaborative care models, such as the Hub and Spoke Model, support the integration of behavioral health services into primary care and other general medical settings through integrated care systems that incorporate specialist collaboration and consultation, expanding access to SUD care. [47,48] |
1. New York State’s Behavioral Health Care Collaborative:
https://omh.ny.gov/omhweb/bho/bh-vbp.html 2. Vermont’s Hub and Spoke Model: https://blueprintforhealth.vermont.gov/about-blueprint/hub-and-spoke |
|
| Macro | Punitive drug policies and programs related to addiction | Housing and workplace policies that support people with SUD | Fair Chance Hiring policies | This approach includes laws and policies designed to improve the ability of those with past criminal convictions, including those related to drug use and possession, to obtain employment by removing criminal history disclosures. Employment is associated with improved treatment adherence and recovery outcomes. [49] |
1. San Francisco’s Fair Chance ordinance:
https://sfgov.org/olse/fair-chance-ordinance-fco 2. New York City’s Fair Chance Act: https://www1.nyc.gov/site/cchr/law/fair-chance-law.page |
| Macro | High threshold treatment policies (e.g., requiring abstinence or cognitive behavioral therapy) | Availability of quality treatment, including MOUD | Emergency department- and hospital-initiated MOUD | Starting buprenorphine treatment in an emergency department and any form of MOUD in hospital settings can serve as an important initiation point and bridge to community-based treatment for patients not actively engaged in SUD care. [50] |
1. CA Bridge Program:
https://bridgetotreatment.org/addiction-treatment/ca-bridge/ 2. Addressing Opioid Use Disorder in Emergency Departments: https://www.thenationalcouncil.org/wp-content/uploads/2021/02/NCBH_TEP_Opioid_Toolkit_v5_021021.pdf?daf=375ateTbd56 3. Inpatient Addiction Consult Service: Expertise for Hospitalized Patients with Complex Addiction Problems: https://pubmed.ncbi.nlm.nih.gov/29933817/ |
| Macro | Housing and workplace policies that support people with SUD | Housing programs that provide access to case management and support services | Housing programs, such as Central City Concern and the Department of Housing and Urban Development’s Recovery Housing Program, combine affordable housing with intensive, coordinated services to help people maintain stable housing and receive appropriate health care, including SUD care. However, exclusionary local housing policies still disproportionately affect people with a drug-related history, despite federal guidance, and should be revised. [51] |
1. Central City Concern:
https://centralcityconcern.org/impact/ 2. U.S. Department of Housing and Urban Development Recovery Housing Program: https://www.hud.gov/program_offices/comm_planning/rhp |
|
| Macro | Punitive drug policies and programs related to addiction | Diversion programs | Diversion programs offer alternatives to incarceration for people who have been arrested for substance use or substance use–related crimes. The programs instead divert them to treatment programs and other social services. |
1. Project EDGE:
https://www.samhsa.gov/criminal-juvenile-justice/grantsgrantees/early-diversion#project-edge-colorado 2. Madison Area Addiction Recovery Initiative: https://www.cityofmadison.com/police/community/maari/ 3. Knoxville Early Diversion Program: https://www.samhsa.gov/criminaljuvenile-justice/grants-grantees/earlydiversion#knoxville-early-diversion-program |
|
| Macro | Community socioeconomic opportunity | Supportive employment programs | These programs assist individuals with mental health and SUD in gaining and maintaining employment by offering individualized and long-term support through integrated vocational and clinical services. [49] |
1. U.S. Department of Veterans Health Administration Compensated Work Therapy:
https://www.va.gov/health/cwt/ 2. Transforming Lives Through Supported Employment Program: https://www.samhsa.gov/criminaljuvenile-justice/grant-grantees/transforming-lives-through-supported-employment-program 3. West Virginia’s Creating Opportunities for Recovery Employment Initiative: https://www.marshallhealth.org/services/addiction-medicine/core/ |
|
Sources
SAMHSA (Substance Abuse and Mental Health Services Administration). 2014. Trauma-informed care in behavioral health services. HHS publication no. (SMA) 13-4801. Available at: https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4816.pdf (accessed April 12, 2022).
Pew Charitable Trusts. 2020. Care coordination strategies for patients can improve substance use disorder outcomes: models that show promise focus on access to lifesaving medications. Philadelphia, PA. Available at: https://www.pewtrusts.org/-/media/assets/2020/04/carecoordinationbrief.pdf (accessed April 12, 2022).
Sevak, P., C. N. Stepanczuk, K. W. V. Bradley, T. Day, G. Peterson, B. Gilman, L. Blue, K. Kranker, K. Stewart, and L. Moreno. 2018. Effects of a community-based care management model for super-utilizers. The American Journal of Managed Care 24(11):e365–e370.
Center for Substance Abuse Treatment. 2009. What are peer recovery support services? HHS publication no. (SMA) 09-4454. Rockville, MD. Available at: https://store.samhsa.gov/product/What-ArePeer-Recovery-Support-Services-/SMA09-4454 (accessed July 27, 2022).
U.S. Department of Health and Human Services. n.d. National CLAS Standards. Washington, DC. Available at: https://thinkculturalhealth.hhs.gov/clas/standards (accessed April 12, 2022).
SAMHSA. 2014. Improving cultural competence. Treatment Improvement Protocol Series No. 59. HHS publication no. (SMA) 14-4849. Rockville, MD. Available at: https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4849.pdf (accessed April 12, 2022).
National Academies of Sciences, Engineering, and Medicine. 2019. Medications for Opioid Use Disorder Save Lives. Washington, DC: The National Academies Press.https://doi.org/10.17226/25310.
SAMHSA. 2021. Medications for opioid use disorder: for healthcare and addiction professionals, policymakers, patients, and families. Rockville, MD. Available at:https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-02-01-002.pdf (accessed April 12, 2022).
Wyant, B. E., S. S. Karon, and S. G. Pfefferle. Housing options for recovery for individuals with opioid use disorder: a literature review. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. Available at: https://aspe.hhs.gov/reports/housing-options-recovery-individuals-opioid-use-disorder-literature-review (accessed April 12, 2022).
Kelleher, K. J., R. Famelia, T. Yilmazer, A. Mallory, J. Ford, L. J. Chavez, and N. Slesnick. 2021. Prevention of opioid use disorder: The HOME (Housing, Opportunities, Motivation and Engagement) feasibility study. Harm Reduction Journal 18(1):112. https://doi.org/10.1186/s12954-021-00560-x.
Centers for Medicare & Medicaid Services. n.d. The Mental Health Parity and Addiction Equity Act (MHPAEA). Available at: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-InsuranceProtections/mhpaea_factsheet (accessed April 12, 2022).
Douglas, M., G. Wrenn, S. Bent-Weber, L. Tonti, G. Carneal, T. Keeton, J. Grillo, S. Rachel, D. Lloyd, E. Byrd, B. Miller, A. Lang, R. Manderscheid, and J. Parks. 2018. Evaluating state mental health and addiction parity statutes: a technical report. The Kennedy Forum. Available at: https://wellbeingtrust.org/wp-content/uploads/2019/06/evaluating-state-mental-health-report-wbt-for-web.pdf (accessed April 12, 2022).
U.S. Department of Labor, U.S. Department of Health and Human Services, and U.S. Department of the Treasury. 2021. FAQs about mental health and substance use disorder parity implementation and the Consolidated Appropriations Act, 2021 part 45. Washington, DC. Available at: https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-45.pdf (accessed April 12, 2022).
Kaiser Family Foundation. 2022. Medicaid waiver tracker: approved and pending section 1115 waivers by state. San Francisco, CA. Available at: https://www.kff.org/medicaid/issue-brief/medicaidwaiver-tracker-approved-and-pending-section-1115-waivers-by-state/ (accessed April 12, 2022).
Centers for Medicare & Medicaid Services. n.d. Section 1115 demonstrations: substance use disorders, serious mental illness, and serious emotional disturbance. Available at: https://www.medicaid.gov/medicaid/section-1115-demonstrations/1115-substance-use-disorder-demonstrations/section-1115-demonstrations-substance-use-disorders-serious-mental-illness-and-serious-emotional-disturbance/index.html (accessed April 12, 2022).
Chappell, K., E. Holmboe, L. Poulin, S. Singer, E. Finkelman, and A. Salman, editors. 2021. Educating Together, Improving Together: Harmonizing Interprofessional Approaches to Address the Opioid Epidemic. NAM Special Publication. Washington, DC: National Academy of Medicine.
Sagi, M. R., G. Aurobind, P. Chand, A. Ashfak, C. Karthick, N. Kubenthiran, P. Murthy, M. Komaromy, and S. Arora. 2018. Innovative telementoring for addiction management for remote primary care physicians: a feasibility study. Indian Journal of Psychiatry 60(4):461–466. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_211_18.
Englander, H., A. Patten, R. Lockard, M. Muller, and J. Gregg. 2021. Spreading addictions care across Oregon’s rural and community hospitals: mixed-methods evaluation of an interprofessional telementoring echo program. Journal of General Internal Medicine 36(1):100–107. https://doi.org/10.1007/s11606-020-06175-5.
Puckett, H. M., J. S. Bossaller, and L. R. Sheets. 2021. The impact of project ECHO on physician preparedness to treat opioid use disorder: a systematic review. Addiction Science & Clinical Practice 16(1):6. https://doi.org/10.1186/s13722-021-00215-z.
Watkins, K. E., A. J. Ober, K. Lamp, M. Lind, C. Setodji, K. C. Osilla, S. B. Hunter, C. M. McCullough, K. Becker, P. O. Iyiewuare, A. Diamant, K. Heinzerling, and H. A. Pincus. 2017. Collaborative care for opioid and alcohol use disorders in primary care: the Summit randomized clinical trial. JAMA Internal Medicine 177(10):1480–1488.https://doi.org/10.1001/jamainternmed.2017.3947.
Brooklyn, J. R., and S. C. Sigmon. 2017. Vermont hub-and-spoke model of care for opioid use disorder: development, implementation, and impact. Journal of Addiction Medicine 11(4):286–292. https://doi.org/10.1097/adm.0000000000000310.
SAMHSA. 2021. Substance use disorders recovery with a focus on employment and education. HHS publication no. PEP21-PL-Guide-6. Rockville, MD. Available at: https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/pep21-pl-guide-6.pdf (accessed April 11, 2022).
SAMHSA. 2021. Use of medication-assisted treatment in emergency departments. HHS publication no. PEP21-PL-Guide-5. Rockville, MD. Available at: https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/pep21-pl-guide-5.pdf (accessed April 12, 2022).
Purtle, J., l. T. Gebrekristos, D. Keene, P. Schlesinger, L. Niccolai, and K. M. Blankenship. 2020. Quantifying the restrictiveness of local housing authority policies toward people with criminal justice histories: United States, 2009–2018. American Journal of Public Health 110(S1):S137–S144. https://doi.org/10.2105/ajph.2019.305437.
NOTES: Some interventions address both risks and protective factors; other interventions may address only one.
The interventions included in the table have been limited to those with promising evidence to reduce the risks associated with precursors of SUD, SUD incidence, SUD morbidity, or SUD-related mortality. In some cases the interventions are specific to harms related to opioid use/opioid use disorder, and this is clearly described in the table. However, their inclusion does not suggest, and should not be taken as, an endorsement by the National Academy of Medicine or any of the authors’ organizations. Additionally, it should be noted that this table does not encompass an exhaustive list of all secondary level interventions.
The selection process involved a thorough review of existing scientific literature, including published studies, meta-analyses, systematic reviews, and program evaluations. In determining the inclusion of interventions, the authors considered various factors, such as the strength of evidence supporting the program’s effectiveness, the quality of research studies conducted on the intervention, the consistency of positive outcomes across multiple studies, and the intervention’s relevance to the prevention of OUD and its associated risks.
Tertiary Prevention of OUD Using a Socioecological Model
Tertiary prevention strategies seek to mitigate the negative consequences and worsening of symptoms among those with OUD through a wide range of services and supports. These could include treatment and recovery services, self-help, and mutual aid groups, as well as harm reductions services to support individuals who are active in their substance use. Tertiary prevention strategies do not stop new cases of OUD from emerging, yet they do significantly reduce opioid-related morbidity and mortality and improve overall well-being. Many of the interventions at this stage are typically categorized as harm reduction; however, it is worth noting that harm reduction includes a spectrum of interventions, including strategies across the primary and secondary levels of prevention.
The socioecological model acknowledges that more can be done to address and prevent collateral consequences and comorbidities associated with OUD, including incarceration and spread of infectious diseases (see Figure 4).
Applying the socioecological lens to tertiary prevention provides targets at the individual, interpersonal, and macro levels for preventing severe consequences among those with OUD, such as overdose death and infectious diseases like HIV and hepatitis C (HCV) related to injection drug use. Examples of interventions at each of these levels include the following:
Individual: Low-Barrier Access to Harm Reduction Services and Supplies
Harm reduction services, which include interventions such as the distribution of sterile syringes and naloxone, have been proven to be effective at preventing morbidity and mortality associated with injection drug use. However, a significant number of PWUD do not have access to these services, a gap that frequently stems from geographical limitations (e.g., for those residing in rural areas) and the enduring stigma associated with the receipt of such services (Harm Reduction International, 2020). Innovative, remote harm-reduction platforms like NEXT Distro have emerged to address these obstacles, leveraging the reach and convenience of digital technologies (e.g., internet, text messaging, and e-mail) to mail essential harm reduction supplies directly to those in need (NEXT Distro, n.d.). These platforms not only dismantle geographical and stigma-related access barriers but also provide comprehensive harm reduction resources and support (Barnett et al., 2021; Yang, Favaro, and Meacham, 2021). With an emphasis on anonymity and privacy, these services expand accessibility, offering a practical, transformative solution for PWUD.
Interpersonal: Education on Safer Injection Practices
Higher risk of HIV and HCV infections, abscesses, cellulitis, and other skin infections is associated with certain drug injection practices (CDC, n.d.). Promoting safer injection practices among PWUD through education and training—like that of the National Harm Reduction Coalition’s Getting Off Right: A Safety Manual for Injection Drug Users (National Harm Reduction Coalition, 2020)—empowers individuals to minimize potential harms associated with injection drug use (Roux et al., 2021).
Macro: Syringe Service Programs
Nearly 30 years of research strongly support the conclusion that syringe service programs (SSPs) play an important role in promoting community safety and reducing the transmission of HIV, HCV, and other blood-borne infections commonly associated with injection drug use (Javed et al., 2020). Policies that remove barriers to the development of SSPs are critical to increasing access to this evidence-based prevention practice. (An example is Florida’s Infectious Disease Elimination Act [IDEA] of 2016, which permitted county commissions to authorize SSPs through grants and donations from private resources and funds, enabling the University of Miami to open the state’s first and only SSP: IDEA Exchange [IDEA Exchange, n.d.]). These programs are instrumental in ensuring that high-risk individuals have access to the full range of services made available by SSPs, including access to and disposal of sterile syringes and injection equipment, vaccination, testing, and links to infectious disease care and OUD treatment. (Table A-3 includes additional examples of tertiary prevention interventions.)
Table A-3. Evidence-Based Interventions at the Tertiary Level of Prevention.
| Tertiary Prevention | |||||
|---|---|---|---|---|---|
| I. Targeted Level of Action | II. Risk(s) at the Targeted Level of Action | III. Protective Factor(s) Addressed | IV. Intervention | V. Intervention Description | VI. Examples of Programs/Models |
| Individual |
Internalization of stigma and discrimination Unaddressed comorbidities (HIV, hepatitis C virus [HCV], wound care) |
Receipt of harm reduction services/supplies (e.g., overdose education and naloxone distribution, syringe services, fentanyl test strips) |
Low-barrier access to sterile drug supplies and other harm reduction services Remote harm reduction services |
Despite the efficacy of harm reduction services in mitigating drug use–related risks, including spread of infectious disease and overdose deaths, many people who use drugs (PWUD) cannot access these services because of geographical constraints and/or the prevailing stigma tied to these services. [52] Remote harm reduction services, such as NEXT Distro, overcome these challenges by leveraging digital technologies for mail-based distribution of supplies and information, thus providing low-barrier access to essential and lifesaving resources. [53,54] | 1. NEXT Distro: https://nextdistro.org/ |
| Interpersonal | Internalization of stigma and discrimination |
Knowledge of safer injection practices Overdose prevention knowledge |
Education on safer injection practices and overdose prevention | Education for PWUD on safer drug use and overdose risks empowers individuals to take steps to minimize potential harms associated with drug use. [55,56] |
1. Getting Off Right: A Safety Manual for Injection Drug Users:
https://harmreduction.org/wp-content/uploads/2020/08/ResourceSaferDruguse-GettingOffRightASafetyMan ualforInjectionDrugUsers.pdf 2. Guide to Developing and Managing Overdose Prevention and Take-Home Naloxone Projects: https://harmreduction.org/wp-content/uploads/2020/08/ResourceOverdosePrevention-GuidetoDevelopingandManagingOverdosePreventionandTakeHomeNaloxoneProjects.pdf 3. Overdose training—Chicago Recovery Alliance: https://anypositivechange.org/overdose-training/ |
| Interpersonal |
Stigma against people with SUD Lack of provider knowledge about SUD |
Co-prescribing of naloxone along with medications with elevated risk profiles for SUD | Co-prescribing of naloxone | Prescribing naloxone along with opioids is recommended as a best practice, particularly at higher opioid doses, to increase access to naloxone for individuals at high risk of experiencing an opioid overdose and to reduce overdose deaths. [57] |
1. Prescribe to Prevent—Prescribe Naloxone, Save a Life:
https://prescribetoprevent.org/ 2. Naloxone for Opioid Safety: https://www.dos.pa.gov/ProfessionalLicensing/BoardsCommissions/Documents/SN%20-%20Naloxone%20for%20Opioid%20Safety%20-%20A%20Provider%27s%20Guide%20to%20Prescribing%20to%20Patients%20Who%20Use%20Opioids.pdf |
| Interpersonal | Stigma against people with SUD Social isolation | Peer recovery support in nontraditional settings | Peer support programs | Individuals with lived experience serve as a resource to PWUD. Peer support workers use their own experiences to connect with and assist PWUDs. They may assist in community building, provide education, and link PWUD with resources, such as harm reduction services or treatment. [58,59,60] | 1. New Mexico Peer Education Project: https://f6f10dcd-f59d-42bc-bec9-c2b204cf568a.usrfiles.com/ugd/f6f10d_c9f0f0d817524f2984fecce04afd574d.pdf |
| Interpersonal |
Lack of provider structural, cultural, or linguistic competency Social isolation |
Syringe service programs in culturally relevant settings (e.g., faith-based institutions) | Faith-based settings, particularly in rural areas, often serve as important cultural institutions. Syringe service programs in these settings can reach people who may not otherwise have access to harm reduction measures. | 1. Faith Leaders’ Perceptions of Needle Exchange Programs in the Rural Illinois Delta Region: Religion as a Social Determinant of Health: https://onlinelibrary.wiley.com/doi/10.1111/ajad.13213 | |
| Macro | High threshold treatment policies (e.g., requirements of abstinence) | Availability of quality treatment, including medications for opioid use disorder (MOUD) | Low-threshold MOUD treatment | A treatment approach that emphasizes principles of medication access, engagement, and treatment retention, and minimizes excessive barriers to treatment. In many cases, these programs offer open access or deliver services outside of traditional clinic settings. [61,62] |
1. Begin the Turn: A Mobile Recovery Program for a Targeted Urban Population:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489971/ 2. Street Medicine and Shelter Health, San Francisco Department of Public Health: https://sf.gov/street-medicine |
| Macro |
Unaddressed comorbidities (HIV, HCV, wound care) Stigma against people with SUD |
Receipt of harm reduction services/supplies (e.g., overdose education and naloxone distribution, syringe services, fentanyl test strips) Overdose prevention knowledge Knowledge of safer injection practices |
Syringe services programs | These programs provide access to and disposal of sterile syringes and injection equipment. Syringe service programs are associated with preventing transmission of blood-borne infections (such as HIV and HCV), improving public safety, and increasing linkage to SUD treatment. [63] |
1. Guide to Starting and Managing Needle and Syringe Programmes:
https://www.unodc.org/documents/hivaids/NSP-GUIDE-WHO-UNODC.pdf 2. IDEA Exchange Florida: https://ideaexchangeflorida.org/ 3. Expanding the Circle of Care: Practical Guide to Syringe Services for Tribal and Rural Communities: https://www.rcorp-ta.org/resources/expanding-circle-care-practical-guide-syringe-services-tribal-and-rural-communities 4. Start a Harm Reduction Program: https://harmreduction.org/take-action/start-a-harm-reduction-program/ 5. Connecting—A Guide to Using Harm Reduction Supplies as Engagement Tools: http://ohrn.org/wp-content/uploads/2021/06/Connecting_Full-Guide.pdf |
| Macro | Illicit market trends toward increasingly toxic drug supply | Receipt of harm reduction services/supplies (e.g., overdose education and naloxone distribution, syringe services, fentanyl test strips) Overdose prevention knowledge | Drug checking (e.g., fentanyl test strips and/or more robust drug checking services) | Drug checking services, which can include the use of fentanyl test strips, provide information to PWUD about what substance(s) are in the drug supply they are using. This information allows individuals to adapt and reduce risks. [64,65,66,67] | 1. The Drug Resource and Education Project: https://dredproject.ca/ |
| Macro | Stigma against people with SUD | Bystander naloxone and other approaches to make naloxone widely available | Naloxone distribution programs | These programs distribute naloxone to individuals who may observe an overdose and provide education on how to respond when one occurs. [68] |
1. Preventing Overdose and Naloxone Intervention:
https://poniri.org/ 2. Find Harm Reduction Resources Near You: https://harmreduction.org/resource-center/harm-reduction-near-you/ 3. NEXT Distro: https://nextdistro.org/ 4. “Feeling Confident and Equipped”: Evaluating the Acceptability and Efficacy of an Overdose Response and Naloxone Administration Intervention to Service Industry Employees in New York City: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6237076/ |
| Macro |
Lack of accountability for or ineffective implementation of harm reduction laws Illicit market trends toward increasingly toxic drug supply |
Community penetration of naloxone Naloxone access legislation |
Bystander naloxone legislation | Legislation to increase access to naloxone may provide civil, criminal, or disciplinary immunity for medical professionals who prescribe or dispense naloxone. It may also provide civil and criminal immunity for laypeople who administer naloxone. It may permit organizations, such as nonprofits or syringe service programs, to distribute naloxone. In some cases, such legislation allows naloxone to be prescribed to individuals who are not themselves at risk of overdose, allowing them to intervene if an overdose occurs. [69] | 1. Legal Interventions to Reduce Overdose Mortality: Naloxone Access Laws: https://www.networkforphl.org/resources/legalinterventions-to-reduce-overdose-mortality-naloxone-access-and-goodsamaritan-laws/ |
| Macro |
Societal stigma and discrimination Punitive criminal legal policies |
Good Samaritan law with proper implementation | Good Samaritan laws | These laws provide immunity from criminal charges for individuals who report an overdose to emergency services and to those who experience the overdose. Such laws encourage people to seek medical help for individuals experiencing an overdose. [70,71] | 1. Good Samaritan Fatal Overdose Prevention and Drug-Induced Homicide: Summary of State Laws: https://legislativeanalysis.org/wp-content/uploads/2020/08/GSFOPlaws.8.10.2020-version.FINAL_.pdf |
| Macro | Jails and prisons that do not offer MOUD Forced withdrawal during recent incarceration | Transition from punitive, criminal legal responses toward supportive, person-centered services | MOUD for people in jails and prisons or reentering society | Individuals with OUD who are incarcerated have a significantly increased risk of death in the days and weeks following release. Offering MOUD inside the jail/prison, with linkage to community services for ongoing treatment at the time of release, is considered a best practice and has been shown to reduce mortality. [72,73,74] Not allowing an individual to continue MOUD while incarcerated violates the Americans with Disabilities Act. [75] |
1. Medications for Opioid Use Disorder in Jails and Prisons: Moving toward Universal Access:
https://americanhealth.jhu.edu/sites/default/files/2021-08/JHU-014%20OUD%20in%20Jail%20Report%20FINAL%202.pdf 2. Pennsylvania Department of Corrections Medication Assisted Treatment: https://www.cor.pa.gov/About%20Us/Initiatives/Pages/Medication-Assisted-Treatment.aspx 3. Behavioral Health Leadership Institute Project Connections at Re-Entry: https://www.bhli.org/projectconnections-at-re-entry.html |
| Macro | Punitive criminal legal policies | Transition from punitive, criminal legal responses toward supportive, person-centered services | Diversion programs | Diversion programs, such as Law Enforcement Assisted Diversion (LEAD), allow police officers the option to divert individuals away from arrest and incarceration to a community-based, harm-reduction intervention for legal violations driven by unmet behavioral health needs. [76] While results are encouraging, challenges with low treatment referral rates and racial disparities in program enrollment persistent, and the need for staff training remains. [77,78] | 1. LEAD Support Bureau: https://www.leadbureau.org/ |
| Macro | Punitive criminal legal policies | Transition from punitive, criminal legal responses toward supportive, person-centered services | Outreach to people who survive an opioid overdose | Under the Houston Emergency Opioid Engagement System [HEROES], police officers are trained to conduct outreach and provide referrals for individuals who experienced a law enforcement–reported overdose. Enrollment in HEROES entails MOUD, peer recovery coaching, clinical behavioral counseling, and educational and support group sessions. [79] | 1. HEROES: https://sbmi.uth.edu/heroes/ |
| Macro | Societal stigma and discrimination |
Availability of affordable housing Employment that supports PWUD |
Employment programs that support recovery | These programs support the employment of individuals in recovery by educating employers on hiring and retaining employees in recovery and connecting people in recovery to employers and workplaces that support their recovery. Employment encourages recovery by creating consistency and purpose, while potentially supporting financial independence. |
1. Creating Opportunities for Recovery Employment, Marshall Health:
https://www.marshallhealth.org/services/addiction-medicine/core/ 2. Recovery Friendly Employer Training Modules: https://recoveryohio.gov/resources/all-resources/recovery-friendly-employer-modules |
| Macro | Unaddressed comorbidities (HIV, HCV, wound care) | Availability of quality treatment, including MOUD | Screening and treatment of individuals who inject drugs for HIV, HCV, and sexually transmitted infections (STIs) | These macro-level solutions provide strategies for implementing programs that screen and treat individuals who inject drugs for HIV, HCV, and STIs. People who inject drugs are at an increased risk of HIV, HCV, and STIs. Screening ensures that individuals are aware of any comorbidities and that they can receive appropriate treatment, thus reducing the spread of infectious diseases. [80] |
1. Wound Care:
https://www.health.state.mn.us/people/syringe/woundcare.pdf 2. An introductory guide for assessing and understanding common wounds with people who inject drugs: https://www.rcorp-ta.org/resources/introductory-guide-assessing-and-understanding-common-wounds-people-who-inject-drugs 3. Wound Aware: A Resource for Commissioners and Providers of Drug Services, GOV.UK: https://www.gov.uk/government/publications/wound-aware-a-resource-for-drug-services/wound-aware-a-resource-for-commissioners-and-providers-of-drug-services 4. Implementing Comprehensive HIV and HCV Programmes with People Who Inject Drugs: Practical Guidance for Collaborative Interventions: https://www.unaids.org/sites/default/files/media_asset/2017_HIV-HCV-programmespeople-who-inject-drugs_en.pdf 5. Be in the KNOW: HIV Programming and Best Practice, Prevention: https://www.beintheknow.org/hiv-programming-and-best-practice/prevention |
| Macro |
Societal stigma and discrimination Illicit market trends toward increasingly toxic drug supply |
Availability of safe consumption spaces |
Safe consumption spaces Overdose prevention sites |
These spaces are sites where individuals may consume previously obtained drugs in a hygienic, monitored environment without fear of arrest and where trained personnel can respond in the event of overdose. [81] |
1. Rhode Island Harm Reduction Centers:
https://health.ri.gov/addiction/about/harmreductioncenters/ 2. OnPoint NYC: https://onpointnyc.org/ |
| Macro | Punitive criminal legal policies | Personal drug possession decriminalization policies | These policies remove the criminal penalties for drug possession. Decriminalization can reduce stigma around drug use, encourage people to access treatment and other services, and free up resources that can be redirected to better support PWUD. [82] | 1. Oregon’s Measure 110: https://www.oregon.gov/oha/hsd/amh/pages/measure110.aspx | |
Sources
Harm Reduction International. 2020. The global state of harm reduction: 2020, 7th Edition. London, UK: Harm Reduction International. Available at: https://hri.global/wp-content/uploads/2022/10/Global_State_HRI_2020_BOOK_FA_Web-1.pdf (accessed July 12, 2023).
Torres-Leguizamon, M., J. Favaro, D. Coello, E. G. Reynaud, T. Nefau, and C. Duplessy. 2023. Remote harm reduction services are key solutions to reduce the impact of COVID-19-like crises on people who use drugs: evidence from two independent structures in France and in the USA. Harm Reduction Journal 20:1. https://doi.org/10.1186%2Fs12954-023-00732-x.
Hayes, B. T., J. Favaro, C. N. Behrends, D. Coello, A. Jakubowski, and A. D. Fox. 2022. NEXT: description, rationale, and evaluation of a novel internet-based mail-delivered syringe service program. Journal of Substance Use. https://doi.org/10.1080/14659891.2022.2144500.
Roux, P., C. Donadille, C. Magen, E. Schatz, R. Stranz, A. Curado, T. Tsiakou, L. Verdes, A. Aleksova, P. Carrieri. S. Mezaache. B. Charif Ali, and the Eurosider Study Group. 2021. Implementation and evaluation of an educational intervention for safer injection in people who inject drugs in Europe: a multi-country mixed-methods study. International Journal of Drug Policy 87:102992. https://doi.org/https://doi.org/10.1016/j.drugpo.2020.102992.
Enteen, L., J. Bauer, R. McLean, E. Wheeler, E. Huriaux, A. H. Kral, and J. D. Bamberger. 2010. Overdose prevention and naloxone prescription for opioid users in San Francisco. Journal of Urban Health 87(6):931–941. https://doi.org/10.1007/s11524-010-9495-8.
Behar, E., C. Rowe, G. M. Santos, N. Santos, and P. O. Coffin. 2017. Academic detailing pilot for naloxone prescribing among primary care providers in San Francisco. Family Medicine 49(2):122–126. Available at: https://www.stfm.org/FamilyMedicine/Vol49Issue2/Behar122 (accessed July 12, 2023).
Stack, E., C. Hildebran, G. Leichtling, E. N. Waddell, J. M. Leahy, E. Martin, and P. T. Korthuis. 2022. Peer recovery support services across the continuum: in community, hospital, corrections, and treatment and recovery agency settings—a narrative review. Journal of Addiction Medicine 16(1):93–100. https://doi.org/10.1097/adm.0000000000000810.
Reif, S., L. Braude, Lyman D. R., R. H. Dougherty, A. S. Daniels, S. S. Ghose, O. Salim, and M. E. Delphin-Rittmon. 2014. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatric Services 65(7):853–861.https://doi.org/10.1176/appi.ps.201400047.
Bardwell, G., T. Kerr, J. Boyd, and R. McNeil. 2018. Characterizing peer roles in an overdose crisis: preferences for peer workers in overdose response programs in emergency shelters. Drug and Alcohol Dependence 190:6–8. https://doi.org/10.1016/j.drugalcdep.2018.05.023.
Winograd, R. P., C. A. Wood, E. J. Stringfellow, N. Presnall, A. Duello, P. Horn, and T. Rudder. 2020. Implementation and evaluation of Missouri’s medication first treatment approach for opioid use disorder in publicly-funded substance use treatment programs. Journal of Substance Abuse Treatment 108:55–64. https://doi.org/10.1016/j.jsat.2019.06.015.
Regis, C., J. M. Gaeta, S. Mackin, T. P. Baggett, J. Quinlan, and E. M. Taveras. 2020. Community care in reach: mobilizing harm reduction and addiction treatment services for vulnerable populations. Frontiers in Public Health 8. https://doi.org/10.3389/fpubh.2020.00501.
Javed, Z., K. Burk, S. Facente, L. Pegram, A. Ali, and A. Asher. 2020. Syringe services programs: a technical package of effective strategies and approaches for planning, design, and implementation. Atlanta, GA: Centers for Disease Control and Prevention. Available at: https://stacks.cdc.gov/view/cdc/105304 (accessed April 13, 2022).
Utah Drug Monitoring Initiative. 2021. Fentanyl report. Available at: https://vipp.health.utah.gov/wp-content/uploads/SIAC-2021-134-Utah-DMI-Fentanyl-Report.pdf (accessed August 22, 2023).
Peiper, N. C., S. D. Clarke, L. B. Vincent, D. Ciccarone, A. H. Kral, and J. E. Zibbell. 2019. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. International Journal of Drug Policy 63:122–128. https://doi.org/https://doi.org/10.1016/j.drugpo.2018.08.007.
National Harm Reduction Coalition. 2020. Fentanyl test strip pilot. Available at: https://harmreduction.org/issues/fentanyl/fentanyl-test-strip-pilot/ (accessed April 13, 2022).
Maghsoudi, N., J. Tanguay, K. Scarfone, I. Rammohan, C. Ziegler, D. Werb, and A. I. Scheim. 2022. Drug checking services for people who use drugs: a systematic review. Addiction 117(3):532–544. https://doi.org/10.1111/add.15734.
Lewis, D. A., J. N. Park, L. Vail, M. Sine, C. Welsh, and S. G. Sherman. 2016. Evaluation of the overdose education and naloxone distribution program of the Baltimore Student Harm Reduction Coalition. American Journal of Public Health 106(7):1243–1246.https://doi.org/10.2105/ajph.2016.303141.
Smart, R., B. Pardo, and C. S. Davis. 2021. Systematic review of the emerging literature on the effectiveness of naloxone access Laws in the United States. Addiction 116(1):6–17. https://doi.org/10.1111/add.15163.
Hamilton, L., C. S. Davis, N. Kravitz-Wirtz, W. Ponicki, and M. Cerdá. 2021. Good Samaritan laws and overdose mortality in the United States in the fentanyl era. International Journal of Drug Policy 97:1–7. https://doi.org/10.1016/j.drugpo.2021.103294.
McClellan, C., B. H. Lambdin, M. M. Ali, R. Mutter, C. S. Davis, E. Wheeler, M. Pemberton, and A. H. Kral. 2018. Opioid-overdose laws association with opioid use and overdose mortality. Addictive Behaviors 86:90–95. https://doi.org/10.1016/j.addbeh.2018.03.014.
Mace, S., A. Siegler, K. Wu, A. Latimore, and H. Flynn. 2020. Medication-assisted treatment for opioid use disorder in jails and prisons: a planning and implementation toolkit. New York: National Council for Behavioral Health and Vital Strategies. Available at: https://www.vitalstrategies.org/wp-content/uploads/MAT_in_Jails_Prisons_Toolkit.pdf (accessed April 13, 2022).
Pew Charitable Trusts. 2020. Opioid use disorder treatment in jails and prisons: medication provided to incarcerated populations save lives. Philadelphia, PA: Available at: https://www.pewtrusts.org/-/media/assets/2020/04/caseformedicationassistedtreatmentjailsprisons.pdf (accessed April 13, 2022).
Green, T. C., J. Clarke, L. Brinkley-Rubinstein, B. D. L. Marshall, N. Alexander-Scott, R. Boss, and J. D. Rich. 2018. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry 75(4):405–407. https://doi.org/10.1001/jamapsychiatry.2017.4614.
U.S. Department of Justice. 2022. Justice Department issues guidance on protections for people with opioid use disorder under the Americans with Disabilities Act. Available at: https://www.justice.gov/opa/pr/justice-department-issues-guidance-protections-people-opioid-use-disorder-under-americans (accessed June 13, 2022).
Clifasefi, S., H. Lonczak, and S. Collins. 2017. Seattle’s Law Enforcement Assisted Diversion (LEAD) program: within-subjects changes on housing, employment, and income/benefits outcomes and associations with recidivism. Crime & Delinquency 63(4):429–445.https://doi.org/10.1177/0011128716687550.
Krawczyk, N., C. E. Picher, K. A. Feder, and B. Saloner. 2017. Only one in twenty justice-referred adults in specialty treatment for opioid use receive methadone or buprenorphine. Health Affairs 36(12):2046–2053. https://doi.org/10.1377/hlthaff.2017.0890.
Anderson, E., R. Shefner, R. Koppel, C. Megerian, and R. Frasso. 2022. Experiences with the Philadelphia Police Assisted Diversion Program: a qualitative study. International Journal of Drug Policy 100:103521. https://doi.org/10.1016/j.drugpo.2021.103521.
Yatsco, A. J., R. D. Garza, T. Champagne-Langabeer, and J. R. Langabeer. 2020. Alternatives to arrest for illicit opioid use: a joint criminal justice and healthcare treatment collaboration. Substance Abuse: Research and Treatment 14. https://doi.org/10.1177/1178221820953390.
Ballard, A. M., R. Haardöerfer, N. Prood, C. Mbagwu, H. L. F. Cooper, and A. M. Young. 2021. Willingness to participate in at-home HIV testing among young adults who use opioids in rural Appalachia. AIDS and Behavior 25(3):699–708. https://doi.org/10.1007/s10461-020-03034-6.
Kral, A. H., B. H. Lambdin, L. D. Wenger, and P. J. Davidson. 2020. Evaluation of an unsanctioned safe consumption site in the United States. New England Journal of Medicine 383(6):589–590. https://doi.org/10.1056/NEJMc2015435.
Drug Policy Alliance. 2015. Approaches to decriminalizing drug use & possession. New York. Available at: https://www.unodc.org/documents/ungass2016/Contributions/Civil/DrugPolicyAlliance/DPA_Fact_Sheet_Approaches_to_Decriminalization_Feb2015_1.pdf (accessed April 13, 2022).
NOTES: Some interventions address both risks and protective factors; other interventions may address only one.
The interventions included in the table have been limited to those with promising evidence to reduce the risks associated with precursors of SUD, SUD incidence, SUD morbidity, or SUD-related mortality. In some cases the interventions are specific to harms related to opioid use/opioid use disorder, and this is clearly described in the table. However, their inclusion does not suggest, and should not be taken as, an endorsement by the National Academy of Medicine or any of the authors’ organizations. Additionally, it should be noted that this table does not encompass an exhaustive list of all tertiary level interventions.
The selection process involved a thorough review of existing scientific literature, including published studies, meta-analyses, systematic reviews, and program evaluations. In determining the inclusion of interventions, the authors considered various factors, such as the strength of evidence supporting the program’s effectiveness, the quality of research studies conducted on the intervention, the consistency of positive outcomes across multiple studies, and the intervention’s relevance to the prevention of OUD and its associated risks.
Interconnected and Multidirectional Levels of Influences
The above examples highlight the complex interplay among the three levels of prevention and the socioecological levels of influence, wherein multidirectional interactions among levels means that factors at one level are often facilitated or restricted by factors at another. For example, individual-level factors—such as individual behaviors, psychological state, and physiological mechanisms—are both supported and limited by interpersonal factors like social support, sense of community cohesion, and access to person-centered care. However, these interpersonal factors do not exist in isolation; they are influenced and shaped by macro-level factors, such as drug control policies, fragmented and unaccountable treatment delivery systems, concentrated poverty, and stigmatizing cultural narratives about people with OUD. Thus, each level is not only dependent on but also instrumental in shaping the dynamics of the others, thereby creating a complex web of interconnected influences.
Additional examples of socioecological primary, secondary, and tertiary interventions that further illustrate this dynamic are provided in Tables A-1, A-2, and A-3. The interventions included in the tables have been limited to those with promising evidenceto reduce the risks associated with precursors of OUD, OUD incidence, OUD morbidity, and OUD-related mortality; however, their inclusion does not suggest, and should not be taken as, an endorsement by the National Academy of Medicine or any of the authors’ organizations.
The goal of this exercise is neither to provide an exhaustive list of all possible interventions, nor to grade the available evidence for various interventions. Instead, the focus is specifically to provide a socioecological public health prevention framework to support a holistic vision for OUD policy, research, and service delivery solutions. Additionally, the socioecological foundation of this framework will foster adaptable and effective solutions that are responsive to the underlying needs of those who are most affected by OUD.
The outlined interventions and strategies can serve as a starting point and inspiration for stakeholders interested in addressing OUD and other related SUDs. By offering examples that make a socioecological approach to OUD prevention practical, the authors hope to provide tangible strategies that can be applied to other SUDs more broadly and that will encourage and empower practitioners, policy makers, funders, service providers, and community leaders to take action through relational dynamics, institutional practices, policy, and advocacy. The tables do not prioritize specific interventions, since each advocate operates within a unique context. Therefore, when determining which strategies and interventions to adopt, advocates should consider their target population and sphere of influence, and the resources they have at their disposal.
Conclusion
Given the severity of the impact of overdose deaths on the nation and the dramatically increasing rates of OUD and other related SUDs in the United States over the past 20 years, it is critical that a public health framework is applied when considering policy, research, and service delivery solutions. This approach is particularly important in light of the structural and systemic factors driving the growing racial and ethnic disparities in SUD treatment and care (Center for Behavioral Health Statistics and Quality, 2021). This discussion paper applies principles of social epidemiology to a traditional public health prevention framework and elucidates contextual and structural points of intervention.
The authors hope to expand the purview of action and responsibility beyond the individual, encourage an expanded lens for those who ascribe only to the biomedical approach to health and well-being, and promote an evergreen focus on SUD prevention that elevates the conversation beyond any particular drug. Leveraging a socioecological approach empowers leaders to champion prevention strategies that address health equity and amend the nation’s historically unjust practices, some of which persist today. With health equity in mind, the authors encourage US leaders to sharpen their attention toward macro-level solutions for prevention; these hold the greatest potential for sustainably improving health for all citizens across a broad set of health outcomes.
While there are a variety of evidence-based and promising practices related to SUD and overdose prevention, there remain significant gaps in researchers’ and practitioners’ understanding. Public funds addressing overdose trends should ensure individual-, interpersonal-, and macro-level investments across the primary, secondary, and tertiary prevention spectrum and support continued research on intended and unintended health outcomes of all funded interventions.
The nation can no longer solely target individuals for one of the greatest social ills of modern times (Reinarman and Levine, 1997). Rather, it must embrace a more comprehensive, multitiered approach that also considers the interpersonal, societal, and structural factors in which individuals interact. This view will ensure that the health care system not only treats the symptoms of disease but also concentrates on the underlying drivers that have fueled the unrelenting rise in incidence of SUD and overdose. In turn, this broader focus on prevention and treatment can also contribute significantly to promoting overall health and well-being. Addressing these underlying determinants of health has the potential to enhance not only addiction outcomes but also broader societal health outcomes, fostering healthier, more resilient communities.
Acknowledgments
This paper benefitted from the thoughtful input of David S. Anderson, George Mason University; Cady Berkel, Arizona State University; Richard F. Catalano, Social Development Research Group; and Amy B. Goldstein, National Institute on Drug Abuse.
Funding Statement
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies.
Footnotes
Conflict-of-Interest Disclosures: Ms. Sullenger reports personal fees from National Academy of Medicine.
Contributor Information
Amanda D. Latimore, American Institutes for Research.
Elizabeth Salisbury-Afshar, University of Wisconsin–Madison.
Noah Duff, National Academy of Medicine.
Emma Freiling, National Academy of Medicine.
Brett Kellett, American Institutes for Research.
Rebecca D. Sullenger, Duke University School of Medicine.
Aisha Salman, National Academy of Medicine; and the Prevention, Treatment, and Recovery Services Working Group of the National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic.
References
- 1.After School Matters. After School Matters empowers Chicago’ s teens. [September 7, 2022]. n.d. https://afterschoolmatters.org/ [Google Scholar]
- 2.Agency for Toxic Substances and Disease Registry. Models and frameworks for the practice of community engagement. 2015. [July 11, 2022]. https://www.atsdr.cdc.gov/communityengagement/pce_models.html . [Google Scholar]
- 3.Ahmad FB, Cisweski JA, Roseen LM, Sutton P. Provisional drug overdose death counts. Hyattsville, MD: National Center for Health Statistics; 2023. [June 6, 2023]. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdosedata.htm . [Google Scholar]
- 4.Akers L, Tippins J, Hauan S, Lynch-Smith M. Key findings from an HHS convening on advancing primary prevention in human services (issue brief) Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services; 2023. [June 5, 2023]. https://aspe.hhs.gov/sites/default/files/documents/8228e700f6e369df9382ac8e0d3976c1/primaryprevention-convening-brief.pdf . [Google Scholar]
- 5.American Institutes for Research. AIR CARES webinar series: social determinants of addiction. 2022. [July 11, 2022]. https://www.air.org/webinar-series-social-determinantsaddiction . [Google Scholar]
- 6.AMA (American Medical Association) Racism as a public health threat H-65.952. 2022. [September 12, 2022]. https://policysearch.ama-assn.org/policyfinder/detail/racism?uri=%2FAMADoc%2FHOD.xml-H-65.952.xml . [Google Scholar]
- 7.AMA. PolicingreformH-65.954. 2021. [September 12, 2022]. https://policysearch.ama-assn.org/policyfinder/detail/Policing%20Reform%20H-65.954?uri=%2FAMADoc%2FHOD.xml-H-65.954.xml [Google Scholar]
- 8.AMA. Treatment versus criminalization— physician role in drug addiction during pregnancy H-420.970. 2020. [September 12, 2022]. https://policysearch.ama-assn.org/policyfinder/detail/criminal%20addiction?uri=%2FAMADoc%2FHODxml-0-3713.xml . [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition, text revision. Washington, DC: 2013. [Google Scholar]
- 10.ASAM (American Society of Addiction Medicine) Access to medications for addiction treatment for persons under community correctionalcontrol. 2021a. [September 7, 2022]. https://www.asam.org/advocacy/public-policy-statements/details/public-policy-statements/2021/08/09/accessto-medications-for-addiction-treatment-for-persons-under-community-correctional-control . [Google Scholar]
- 11.ASAM. Public policy statement on advancing racial justice in addiction medicine. 2021b. [April 28, 2022]. https://sitefinitystorage.blob.core.windows.net/sitefinity-productionblobs/docs/default-source/public-policy-statements/asam-policy-statement-on-racial-justiced7a33a9472bc604ca5b7ff000030b21a.pdf?sfvrsn=5a1f5ac2_0 . [Google Scholar]
- 12.ASAM. Definition of addiction. [April 28, 2022]. n.d. https://www.asam.org/quality-care/definition-of-addiction . [Google Scholar]
- 13.Barnett BS, Wakeman SE, Davis CS, Favaro J, Rich JD. Expanding mail-based distribution of drug-related harm reduction supplies amid COVID-19 and beyond. American Journal of Public Health. 2021;111(6):1013–1017. doi: 10.2105/AJPH.2021.306228. https://doi.org/10.2105%2FAJPH.2021.306228 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baum D. Legalize it all. [April 2016]; [May 17, 2023];Harper’s Magazine. 2016 https://harpers.org/archive/2016/04/legalize-it-all/ [Google Scholar]
- 15.Berkman LF, Kawachi I, Glymour MM. Social epidemiology. Oxford, UK: Oxford University Press; 2015. [Google Scholar]
- 16.Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample. JAMA Pediatrics. 2019;173(11):e193007. doi: 10.1001/jamapediatrics.2019.3007. https://doi.org/10.1001%2Fjamapediatrics.2019.3007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Big Brothers Big Sisters of America. Home. [September 7, 2022]. n.d. https://www.bbbs.org/ [Google Scholar]
- 18.Brody GH, Kogan SM, Chen Y-F, Murry VM. Long-term effects of the Strong African American Families Program on youths’ conduct problems. Journal of Adolescent Health. 2006;43(5):474–481. doi: 10.1037/0893-3200.20.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brody GH, Miller GE, Yu T, Beach SRH, Chen E. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: a replication across two longitudinal cohorts. Psychological Science. 2016;27(4):530–541. doi: 10.1177/0956797615626703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brofenbrenner U. The ecology of human development: experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 21.Center for Behavioral Health Statistics and Quality. Racial/ethnic differences in substance use, substance use disorders, and substance use treatment utilization among people aged 12 or older (2015– 2019) Rockville, MD: Substance Abuse and Mental Health Services Administration; 2021. [March 1, 2023]. https://www.samhsa.gov/data/report/racialethnic-differences-substance-use . [Google Scholar]
- 22.CDC (Centers for Disease Control and Prevention) Creating positive childhood experiences. 2022. [May 17, 2023]. https://www.cdc.gov/injury/features/prevent-childabuse/index.html . [Google Scholar]
- 23.CDC. U.S. overdose deaths in 2021 increased half as much as in 2020 – but are still up 15%. 2021. [June 13, 2021]. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm . [Google Scholar]
- 24.CDC. Preventing adverse childhood experiences: leveraging the best available evidence. 2019. [October 7, 2022]. https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf . [Google Scholar]
- 25.CDC. Infectious diseases, opioids and injection drug use. [October 13, 2022]. n.d. https://www.cdc.gov/pwid/opioiduse.html . [Google Scholar]
- 26.Chen E, Brody GH, Miller GE. Childhood close family relationships and health. American Psychologist. 2017;72(6):555–566. doi: 10.1037/amp0000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coffin PO, Rowe C, Oman N, Sinchek K, Santos G-M, Faul M, Bagnulo R, Mohamed D, Vittinghoff E. Illicit opioid use following changes in opioids prescribed for chronic non-cancer pain. PLOS ONE. 2020;15(5):e0232538. doi: 10.1371/journal.pone.0232538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins AB, Edwards S, McNeil R, Goldman J, Hallowell BD, Scagos RP, Marshall BDL. A rapid ethnographic study of risk negotiation during the COVID-19 pandemic among unstably housed people who use drugs in Rhode Island. International Journal of Drug Policy. 2022;103(103626) doi: 10.1016/j.drugpo.2022.103626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooper D, Mokhiber Z, Zipperer B. Raising the federal minimum wage to $15 by 2025 would lift the pay of 32 million workers. Washington, DC: Economic Policy Institute; 2021. [April 11, 2022]. https://www.epi.org/publication/raising-the-federal-minimum-wage-to-15-by-2025-would-liftthe-pay-of-32-million-workers/ [Google Scholar]
- 30.Courtwright DT. Preventing and treating narcotic addiction—a century of federal drug control. New England Journal of Medicine. 2015;373:2095–2097. doi: 10.1056/NEJMp1508818. [DOI] [PubMed] [Google Scholar]
- 31.Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, Cepeda J, Comfort M, Goosby E, Goulão J, Hart C, Kerr T, Lajous AM, Lewis S, Martin N, Mejía D, Camacho A, Mathieson D, Obot I, Ogunrombi A, Sherman S, Stone J, Vallath N, Vickerman P, Zábranský T, Beyrer C. Public health and international drug policy. The Lancet. 2016;387(10026):1427–1480. doi: 10.1016/S0140-6736(16)00619-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daniels C, Aluso A, Burke-Shyne N, Koram K, Rajagopalan S, Robinson I, Shelly S, Shirley-Beavan S, Tandon T. Decolonizing drug policy. Harm Reduction Journal. 2021;18(120) doi: 10.1186/s12954-02100564-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. American Journal of Public Health. 2018;108(2):182–186. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. The Lancet. 2010;376(9737):285–301. doi: 10.1016/S01406736(10)60742-8. [DOI] [PubMed] [Google Scholar]
- 35.DeWeerdt S. Tracing the US opioid crisis to its roots. Nature. 2019;573:S10–S13. doi: 10.1038/d41586-019-02686-2. [DOI] [PubMed] [Google Scholar]
- 36.Dineen KK, Pendo E. Ending the war on people with substance use disorders in health care. The American Journal of Bioethics. 2021;21(4):20–22. doi: 10.1080/15265161.2021.1891353. [DOI] [PubMed] [Google Scholar]
- 37.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. Morbidity and Mortality Weekly Report. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 38.DuBois WEB. The health and physique of the Negro American. American Journal of Public Health. 2003;93(2):272–276. doi: 10.2105/AJPH.93.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.El-Sabawi T. The role of pressure groups and problem definition in crafting legislative solutions to the opioid crisis. Northeastern University Law Review. 2019;11(1):372–400. https://ssrn.com/abstract=3460109 . [Google Scholar]
- 40.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 41.Erdem G, Kaufman MR. Mentoring for preventing and reducing substance use and associated risks among youth. Boston, MA: National Mentoring Resource Center; 2020. [October 11, 2022]. https://nationalmentoringresourcecenter.org/wp-content/uploads/2020/05/Mentoring_for_Preventing_and_Reducing_Substance_Use_and_Associated_Risks_Among_Youth_Outcome_Review.pdf . [Google Scholar]
- 42.Fricton J, Anderson K, Clavel A, Fricton R, Hathaway K, Kang W, Jaeger B, Maixner W, Pesut D, Russell J, Weisberg MB, Whitebird R. Preventing chronic pain: a human systems approach-results from a massive open online course. Global Advances in Health and Medicine. 2015;4(5):23–32. doi: 10.7453/gahmj.2015.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gainsbury S. Cultural competence in the treatment of addictions: theory, practice and evidence. Clinical Psychology & Psychotherapy. 2016;24(4):987–1001. doi: 10.1002/cpp.2062. [DOI] [PubMed] [Google Scholar]
- 44.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiologic Review. 2004;26(1):36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 45.Geller A, Fagan J, Tyler T, Link BG. Aggressive policing and the mental health of young urban men. American Journal of Public Health. 2014;104(12):2321–2327. doi: 10.2105/ajph.2014.302046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghose R, Forati AM, Mantsch JR. Impact of the COVID-19 pandemic on opioid overdose deaths: a spatiotemporal analysis. Journal of Urban Health. 2022;99(2):316–327. doi: 10.1007/s11524-022-00610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Social Science & Medicine. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 48.Global Commission on Drug Policy. War on drugs: report of the Global Commission on Drug Policy. Geneva, Switzerland: 2011. [April 28, 2022]. http://www.globalcommissionondrugs.org/wp-content/uploads/2017/10/GCDP_WaronDrugs_EN.pdf . [Google Scholar]
- 49.Guarino H, Mateu-Gelabert P, Quinn K, Sirikantraporn S, Ruggles KV, Syckes C, Goodbody E, Jessell L, Friedman SR. Adverse childhood experiences predict early initiation of opioid use behaviors. Frontiers in Sociology. 2021;6:620395. doi: 10.3389/fsoc.2021.620395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harm Reduction International. The global state of harm reduction: 2020. 7th. London, UK: Harm Reduction International; 2020. [July 12, 2023]. https://hri.global/wpcontent/uploads/2022/10/Global_State_HRI_2020_BOOK_FA_Web-1.pdf . [Google Scholar]
- 51.Hatzenbuehler ML, Keyes K, Hamilton A, Uddin M, Galea S. The collateral damage of mass incarceration: risk of psychiatric morbidity among nonincarcerated residents of high-incarceration neighborhoods. American Journal of Public Health. 2015;105(1):138–143. doi: 10.2105/ajph.2014.302184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 53.Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJMJ. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacology. 2021;46(10):1715–1723. doi: 10.1038/s41386-020-00950-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Herzberg D, Guarino H, Mateu-Gelabert P, Bennett AS. Recurring epidemic of pharmaceutical drug abuse in America: time for an all-drug strategy. American Journal of Public Health. 2016;106(3):408–410. doi: 10.2105/AJPH.2015.302982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holmboe E, Singer S, Chappell K, Assadi K, Salman A The Education and Training Working Group of the National Academy of Medicine’s Action Collaborative on Countering the U.S. Opioid Epidemic. NAM Perspectives. National Academy of Medicine; Washington, DC: 2022. The 3Cs framework for pain and unhealthy substance use: minimum core competencies for interprofessional education and practice. Discussion Paper. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. American Journal of Preventive Medicine. 2016;50(2):129–135. doi: 10.1016/j.amepre.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 57.Husarewycz MN, El-Gabalawy R, Logsetty S, Sareen J. The association between number and type of traumatic life experiences and physical conditions in a nationally representative sample. General Hospital Psychiatry. 2014;36(1):26–32. doi: 10.1016/j.genhosppsych.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 58.IDEA Exchange. The Infectious Disease Elimination Act (IDEA Exchange): Reducing the spread of HIV and hepatitis C through harm reduction. [September 7, 2022]. n.d. https://ideaexchangeflorida.org/ [Google Scholar]
- 59.Mrazek PJ, Haggerty RJ, editors. Institute of Medicine, Committee on Prevention of Mental Disorders. Reducing the risks for mental disorders: frontiers for preventive intervention research. Washington, DC: National Academy Press; 1994. [DOI] [PubMed] [Google Scholar]
- 60.Ioannidis JPA, Powe NR, Yancy C. Recalibrating the use of race in medical research. JAMA. 2021;325(7):623–624. doi: 10.1001/jama.2021.0003. [DOI] [PubMed] [Google Scholar]
- 61.Jalali MS, Botticelli M, Hwang RC, Koh HK, McHugh RK. The opioid crisis: a contextual, social-ecological framework. Health Research Policy and Systems. 2020;18(1):87. doi: 10.1186/s12961-020-005968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Javed Z, Burk K, Facente S, Pegram L, Ali A, Asher A. Syringe services programs: a technical package of effective strategies and approaches for planning, design, and implementation. Atlanta, GA: Centers for Disease Control and Prevention; 2020. [April 13, 2022]. https://stacks.cdc.gov/view/cdc/105304 . [Google Scholar]
- 63.Jones CT, Branco SF. Advances in Addiction & Recovery Winter. 2021. [May 17, 2023]. Cultural considerations in addiction treatment: the application of cultural humility. https://www.naadac.org/assets/2416/aa&r_winter2021_cultural_considerations_in_addiction_treatment.pdf . [Google Scholar]
- 64.Jones-Eversley SD, Dean LT. After 121 years, it’s time to recognize W.E.B. Du Bois as a founding father of social epidemiology. The Journal of Negro Education. 2018;87(3):230–245. doi: 10.7709/jnegroeducation.87.3.0230. [DOI] [Google Scholar]
- 65.Kleber HD. Methadone maintenance 4 decades later. JAMA. 2008;300(19):2303–2305. doi: 10.1001/jama.2008.648. [DOI] [PubMed] [Google Scholar]
- 66.Krieger N, Dorling D, McCartney G. Mapping injustice, visualizing equity: why theory, metaphors and images matter in tackling inequalities. Public Health. 2012;126(3):256–258. doi: 10.1016/j.puhe.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 67.Kroenke K, Alford DP, Argoff C, Canlas B, Covington E, Frank JW, Haake KJ, Hanling S, Hooten WM, Kertesz SG, Kravitz RL, Krebs EE, Stanos SP, Jr, Sullivan M. Challenges with implementing the Centers for Disease Control and Prevention opioid guideline: a consensus panel report. Pain Medicine. 2019;20(4):724–735. doi: 10.1093/pm/pny307. [DOI] [PubMed] [Google Scholar]
- 68.Latimore AD, Schoyer E, Mossburg S, Kellett B, Derrington T, Caglayan K, Lin D. Child Welfare. A public health approach to preventing intergenerational transmission of substance use disorder: applying a social determinants of health framework to child welfare and across systems. In press. [Google Scholar]
- 69.Leavell HR, Clark EG. Preventive medicine for the doctor in his community: an epidemiologic approach. 3rd. New York: McGraw Hill; 1965. [Google Scholar]
- 70.Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278(5335):45–47. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- 71.Link BG, Phelan J. Journal of Health and Social Behavior (extra issue) 1995. Social conditions as fundamental causes of disease; pp. 80–94. [DOI] [PubMed] [Google Scholar]
- 72.Macintyre S, Ellaway A. Neighborhoods and health: an overview. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. 1st. Oxford, UK: Oxford Academic; 2003. pp. 20–42. [DOI] [Google Scholar]
- 73.Masten C, Lombardi J, Fisher P. Helping families meet basic needs enables parents to promote children’s health growth, development. Washington, DC: Center on Budget and Policy Priorities; 2021. [October 7, 2022]. https://www.cbpp.org/research/poverty-and-inequality/helping-families-meet-basic-needs-enables-parents-to-promote . [Google Scholar]
- 74.Merrin GJ, Ames ME, Sturgess C, Leadbeater BJ. Disruption of transitions in high-risk substance use from adolescence to young adulthood: school, employment, and romantic relationship factors. Substance Use & Misuse. 2020;55(7):1129–1137. doi: 10.1080/10826084.2020.1729200. [DOI] [PubMed] [Google Scholar]
- 75.Milligan K, Stabile M. Do child tax benefits affect the wellbeing of children? Evidence from Canadian child benefit expansions. Vancouver and Toronto, Canada. [April 11, 2022]. n.d. https://sticerd.lse.ac.uk/dps/pep/pep01.pdf . [Google Scholar]
- 76.Mistler CB, Sullivan MC, Copenhaver MM, Meyer JP, Roth AM, Shenoi SV, Edelman EJ, Wickersham JA, Shrestha R. Differential impacts of COVID-19 across racial-ethnic identities in persons with opioid use disorder. Journal of Substance Abuse Treatment. 2021;129:108387. doi: 10.1016/j.jsat.2021.108387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.National Academies of Science, Engineering, and Medicine. The promise of adolescence: realizing opportunity for all youth. Washington, DC: The National Academies Press; 2019. [DOI] [PubMed] [Google Scholar]
- 78.National Center for Health Statistics. CDC WONDER, multiple cause of death (detailed mortality) – national drug overdose (OD) deaths, 1999-2021 (data file) [March 24, 2023]. n.d. https://nida.nih.gov/sites/default/files/Overdose_data_1999-2021%201.19.23.xlsx . [Google Scholar]
- 79.National Harm Reduction Coalition. Getting off right: a safety manual for injection drug users. New York: 2020. [September 7, 2022]. https://harmreduction.org/issues/safer-drug-use/injection-safety-manual/ [Google Scholar]
- 80.National Institute on Drug Abuse. Naloxone for opioid overdose: life-saving science. Gaithersburg, MD: 2017. [May 17, 2023]. https://nida.nih.gov/publications/naloxoneopioid-overdose-life-saving-science . [Google Scholar]
- 81.National Institute on Minority Health and Health Disparities. NIMHD research framework. 2017. [June 5, 2023]. https://www.nimhd.nih.gov/about/overview/research-framework/nimhd-framework.html . [Google Scholar]
- 82.NEXT Distro. Home. [July 12, 2023]. n.d. https://nextdistro.org/ [Google Scholar]
- 83.Nunn KB. Race, Crime and the pool of surplus criminality: or why the “war on drugs” was a “war on Blacks”. [May 17, 2023];The Journal of Gender, Race & Justice. 2002 6:381–445. https://scholarship.law.ufl.edu/cgi/viewcontent.cgi?article=1178&context=facultypub . [Google Scholar]
- 84.Nutt DJ, King LA, Phillips LD, on behalf of the Independent Scientific Committee on Drugs Drug harms in the UK: A multicriteria decision analysis. The Lancet. 2010;376(9752):P1558–P1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- 85.Office of Minority Health. National standards for culturally and linguistically appropriate services (CLAS) in health and health care. Rockville, MD: US Department of Health and Human Services; [September 7, 2022]. n.d. https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedNationalCLASStan-dards.pdf . [Google Scholar]
- 86.Office of the Surgeon General. Facing addiction in America: the surgeon general’ s report on alcohol, drugs, and health. Washington, DC: 2016. [May 16, 2023]. https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf . [PubMed] [Google Scholar]
- 87.Olsen Y. What is addiction? History, terminology, and core concepts. Medical Clinics of NorthAmerica. 2022;106(1):1–12. doi: 10.1016/j.mcna.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 88.Park JN, Rouhani S, Beletsky L, Vincent L, Saloner B, Sherman SG. Situating the continuum of overdose risk in the social determinants of health: a new conceptual framework. The Milbank Quarterly. 2020;98(3):700–746. doi: 10.1111/1468-0009.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Powerful Voices. Home. [September 7, 2022]. n.d. https://www.powerfulvoices.org/ [Google Scholar]
- 90.Racine E, Sattler S, Escande A. Free will and the brain disease model of addiction: the not so seductive allure of neuroscience and its modest impact on the attribution of free will to people with an addiction. Frontiers in Psychology. 2017;8:1850. doi: 10.3389/fpsyg.2017.01850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reinarman C, Levine HG. Crack in America: demon drugs and social justice. Berkeley, CA: University of California Press; 1997. [Google Scholar]
- 92.Roberts D. Fatal invention: how science, politics, and big business re-create race in the twenty-first century. New York: The New Press; 2012. [Google Scholar]
- 93.Rosino ML, Hughey MW. The war on drugs, racial meanings, and structural racism: a holistic and reproductive approach. The American Journal of Economics and Sociology. 2018;77(3–4):849–892. doi: 10.1111/ajes.12228. [DOI] [Google Scholar]
- 94.Roux P, Donadille C, Magen C, Schatz E, Stranz R, Curado A, Tsiakou T, Verdes L, Aleksova A, Carrieri P, Mezaache S, Charif Ali B The Eurosider Study Group. Implementation and evaluation of an educational intervention for safer injection in people who inject drugs in Europe: a multi-country mixed-methods study. International Journal of Drug Policy. 2021;87:102992. doi: 10.1016/j.drugpo.2020.102992. [DOI] [PubMed] [Google Scholar]
- 95.Sandstrom H, Huerta S. The negative effects of instability on child development: a research synthesis. Washington, DC: Urban Institute; 2013. [October 7, 2022]. https://www.urban.org/sites/default/files/publication/32706/412899-The-Negative-Effects-of-Instability-on-Child-Development-A-Research-Synthesis.PDF . [Google Scholar]
- 96.Schmidt RA, Genois R, Jin J, Vigo D, Rehm J, Rush B. The early impact of COVID-19 on the incidence, prevalence, and severity of alcohol use and other drugs: a systematic review. Drug and Alcohol Dependence. 2021;228(109065) doi: 10.1016/j.drugalcdep.2021.109065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shepard E, Blackley PR. U.S. drug control policies: federal spending on law enforcement versus treatment in public health outcomes. Journal of Drug Issues. 2004;34(4):771–786. doi: 10.1177/002204260403400403. [DOI] [Google Scholar]
- 98.SAMHSA (Substance Abuse and Mental Health Services Administration) The opioid crisis and the Black/African American population: an urgent issue. Rockville, MD: 2020a. [April 28, 2022]. https://store.samhsa.gov/product/The-Opioid-Crisis-and-the-Black-African-American-Population-An-Urgent-Issue/PEP20-05-02-001 . [Google Scholar]
- 99.SAMHSA. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health. Rockville, MD: 2020b. [March 31, 2021]. https://store.samhsa.gov/product/key-substance-use-and-mental-health-indicators-in-the-united-states-results-from-the-2019-national-survey-on-Drug-Use-and-Health/PEP20-07-01-001?referer=from_search_result . [Google Scholar]
- 100.SAMHSA. Using fear messages and scare tactics in substance abuse prevention efforts. Rockville, MD: 2015. [August 22, 2023]. https://www.riprc.org/wp-content/uploads/2018/04/fear-messages-prevention-efforts.pdf . [Google Scholar]
- 101.SAMHSA. Trauma-informed care in behavioral health services. Rockville, MD: 2014a. [April 12, 2022]. HHS publication no. (SMA) 13-4801. https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4816.pdf . [PubMed] [Google Scholar]
- 102.SAMHSA. Improvingculturalcompetence.Treatment Improvement Protocol Series no. 59. Rockville, MD: 2014b. [April 12, 2022]. HHS publication no. (SMA) 14-4849. https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4849.pdf . [Google Scholar]
- 103.Szalavitz M. Unbroken brain: a revolutionary new way of understanding addiction. New York: St. Martin’s Press; 2016. [Google Scholar]
- 104.Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, Smith LR, Strathdee SA, Wakeman SE, Venkataramani AS. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLOS Medicine. 2019;16(11):e1002969–e1002969. doi: 10.1371/journal.pmed.1002969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.University of Georgia, Center for Family Research. Strong African American Families Program. [September 7, 2022]. n.d. https://cfr.uga.edu/saaf-programs/saaf/ [Google Scholar]
- 106.Virchow R. Der Armenarzt. Medicinische Reform. 1848;18:125–127. [Google Scholar]
- 107.Volkow ND, Boyle M. Neuroscience of addiction: relevance to prevention and treatment. American Journal of Psychiatry. 2018;175(8):729–740. doi: 10.1176/appi.ajp.2018.17101174. [DOI] [PubMed] [Google Scholar]
- 108.Volkow ND, McLellan AT. Opioid abuse in chronic pain—misconceptions and mitigation strategies. New England Journal of Medicine. 2016;374:1253–1263. doi: 10.1056/NEJMra1507771. [DOI] [PubMed] [Google Scholar]
- 109.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569–576. doi: 10.1097/01.j.pain.0000460357.01998.f1. [DOI] [PubMed] [Google Scholar]
- 110.Wagner KD, Liu L, Davidson PJ, Cuevas-Mota J, Armenta RF, Garfein RS. Association between non-fatal opioid overdose and encounters with healthcare and criminal justice systems: identifying opportunities for intervention. Drug and Alcohol Dependence. 2015;153:215–220. doi: 10.1016/j.drugalcdep.2015.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wailoo K. Pain: a political history. Baltimore, MD: Johns Hopkins University Press; 2014. [Google Scholar]
- 112.Weintraub WS, Daniels SR, Burke LE, Franklin BA, Goff DC, Jr, Hayman LL, Lloyd-Jones D, Pandey DK, Sanchez EJ, Schram AP, Whitsel LP. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation. 2011;124(8):967–990. doi: 10.116/CIR.0b013e3182285a8. [DOI] [PubMed] [Google Scholar]
- 113.Yang C, Favaro J, Meacham MC. NEXT Harm Reduction: an online, mail-based naloxone distribution and harm-reduction program. American Journal of Public Health. 2021;111(4):667–671. doi: 10.2105/AJPH.2020.306124. https://doi.org/10.2105%2FAJPH.2020.306124 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yoast RA, Filstead WJ, Wilford BB, Hayashi S, Reenan J, Epstein J. Teaching about substance abuse. VirtualMentor. 2008;10(1):21–29. doi: 10.1001/virtualmentor.2008.10.1.medu1-0801. [DOI] [PubMed] [Google Scholar]


