Abstract
Clinical depression is viewed as a physical and psychic disease process having a neuropathological basis, although a clear understanding of its ethiopathology is still missing. The observation that depressive symptoms are influenced by pharmacological manipulation of monoamines led to the hypothesis that depression results from reduced availability or functional deficiency of monoaminergic transmitters in some cerebral regions. However, there are limitations to current monoamine theories related to mood disorders. Recently, a growing body of experimental data has showed that other classes of endogenous compounds, such as neuropeptides and amino acids, may play a significant role in the pathophysiology of affective disorders. With the development of neuroscience, neuronal networks and intracellular pathways have been identified and characterized, describing the existence of the interaction between monoamines and receptors in turn able to modulate the expression of intracellular proteins and neurotrophic factors, suggesting that depression/antidepressants may be intermingled with neurogenesis/neurodegenerative processes.
Keywords: Depression, Neurotransmitter, Neuropeptide, Brain plasticity, Growth factor
Introduction
Depression is a complex psychiatric disorder affecting approximately 15% of the population with high morbidity and mortality. Major depressive disorder (MDD) is common in the general population; it affects up to one-sixth of the population.
Despite high prevalence and socioeconomic impact, little is known about the etiology of depressive illnesses. The underlying causes of most mood disorders remain unknown. Heritability estimates demonstrate up to a 50% genetic component based on family aggregation and contrasting monozygotic and dizygotic twin studies [1]. This strong heritable component to psychiatric illnesses, when coupled with environmental influences, results in increased susceptibility to develop the illness in response to stressful/adverse environmental conditions. Population genetic studies suggest that there is an increased risk of bipolar illness in the relatives of bipolar patients and an increased risk of unipolar depressive illness in the relatives of both bipolar and unipolar patients. Intensive research efforts have been made to better characterize the genetic underpinnings of mental illness. Technological advances, including the completion of the human genome inventory, chromosome mapping, high throughput DNA sequencing, and others, offer the promise of identifying the genetic basis of mental illnesses. Several linkage and association studies showed that the inheritance for major depressive illness could reside on chromosomes 11 and 18 [2]. In particular, on chromosome 18, two putative candidate genes have been identified: the gene for corticotrophin receptor (CRF1) and for Gs protein-alpha subunit. However, recent genome scan meta-analysis yielded somewhat contrasting conclusions with a relatively low significance for quantitative trait loci on chromosomes 9, 10, 14, and 18 [1]. To date, unfortunately, no gene or genetic risk factor has been convincingly identified yet for depression.
Depression and antidepressants: still matter of neurotransmitters?
Almost 4 decades of intensive research have sought to elucidate the neurobiological bases of depression. However, the study of biological bases of depression is still overdue. The principal aims are to increase the knowledge of the basis of the disease in order to better define its pathogenic process and to identify predictive biomarkers or, at least, markers able to support the diagnosis. Within this context, a great variety of bioumoral parameters have been explored as well as the existence of a genetic component of depression. Epidemiological studies have revealed that both genetic and environmental factors contribute to the risk for depression. Adverse early life experiences influence neurobiological systems, leading to the neurobiological and behavioral manifestations of depression. Several data on biological fluids from patients affected by depression, on brain tissue from suicide subjects, and the evidence of a clinical activity of the antidepressant drugs suggested that depression is associated with an impairment mainly in monoaminergic neurotransmission systems (see below). These observations are mainly indirect and based on the role of the aminergic cerebral circuits on functions, such as attention and alertness, which are altered in depressive illnesses, and on behavioral effects induced by drugs acting on aminergic transmission.
The catecholamine/serotonin theory: a brief view
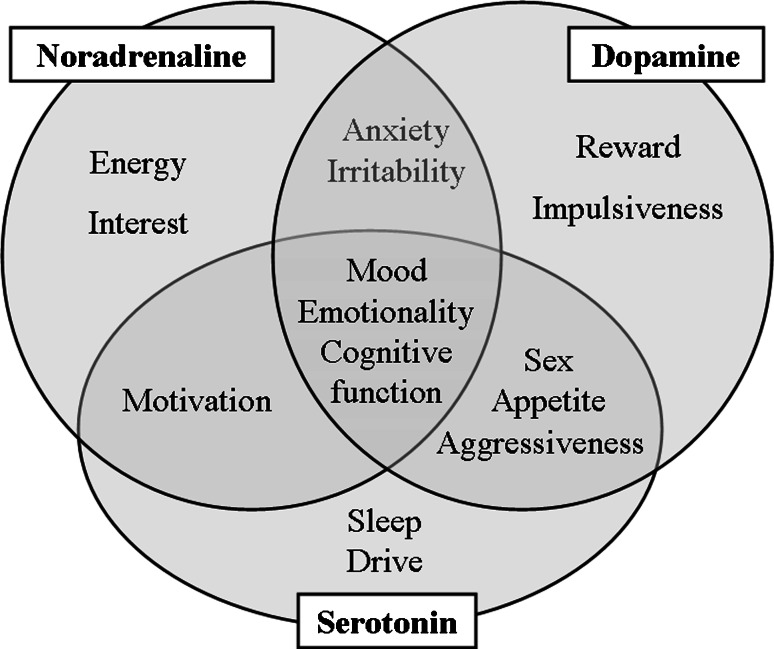
The observation that depressive symptoms were influenced by the pharmacological manipulation of monoaminergic system led to the hypothesis that depression results from reduced availability or functional deficiency of monoaminergic transmitters in some cerebral regions [3–6] (see Table 1 and Fig. 1 for a better comprehension of the role of noradrenaline (NE), serotonin (5-HT), and dopamine (DA) in depression [7–33]). This view was supported by the pharmacological action of both tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs), able to acutely increase synaptic levels of monoamines, and by drugs, such as reserpine, to induce depression [10]. The idea that exposure to chronic stress or cerebral disorders could decrease levels and activity of monoamines, thus leading to depression, took place. On this conceptual basis the commonly used antidepressants were developed. All the antidepressant drugs now in use modulate monoamine neurotransmission, both acutely and chronically, although their therapeutic effects need as long as 6 to 8 weeks to develop, and each drug is efficacious in only 60–70% of patients [34].
Table 1.
The role of noradrenaline, serotonin, and dopamine in depression
| Neurotransmitter | Parameter (brain area, tissue, or biological fluid) | Suggestion | Reference |
|---|---|---|---|
| Noradrenaline (NE) | Decreased levels in 3-methoxy-4-hydroxy-phenylglycol (MHPG) (liquor, plasma, and urine) often with great variability among patients and studies | Inhibition of locus coeruleus (LC) | Maas et al. [7], Roy et al. [8], Potter and Manji [9] |
| Alpha-methylparatyrosine (AMPT) administration | Rapid depletion of brain catecholamines and relapse of depressive symptoms | Ordway et al. [10], Ruhè et al. [11] | |
| Elevated tyrosine hydroxylase (TH) | Noradrenergic dysregulation in depression | Charney [12], Zhu et al. [13] | |
| Increased agonist binding to alpha2-adrenergic receptors | Noradrenergic dysregulation in depression | Ordway et al. [14, 15] | |
| Reduced levels of NE transporters | Noradrenergic dysregulation in depression | Klimek et al. [16] | |
| Serotonin (5-HT) | Reduced 5-hydroxyindoleacetic acid (5-HIAA) concentration (liquor) | Correlation with suicidal and violence-impulsivity behavior than depressive symptoms | Asberg et al. [17, 18] |
| Reduction of 5-HT concentrations (postmortem tissues of whole brain, hypothalamus, and amygdala) | Serotoninergic dysregulation in depression | Csernansky and Sheline [19], Tuinier et al. [20] | |
| Decreased plasma in l-tryptophan | Serotoninergic dysregulation in depression | Quintana 1992 [21], Jans et al. 2007 [22] | |
| Reduction in the activity of the 5-HT reuptake transporter (brain) | Serotoninergic synapse dysregulation in depression | Arango et al. [23], Celada et al. [24] | |
| Increase in the density of 5-HT2 receptors (brain) | Serotoninergic synapse dysregulation in depression | Arango et al. [23], Celada et al. [24] | |
| Increased density of postsynaptic 5-HT2 receptor binding sites (frontal cortex) | Serotoninergic synapse dysregulation in depression | Mann et al. [25], Arora and Meltzer [26], Yates et al. [27] | |
| Reduction of pre- and postsynaptic 5-HT1A receptor binding | Reduced 5-HT1A autoreceptor function and a blunted postsynaptic 5-HT1A receptor signaling in depression | Celada et al. 2004 [24], Drevets et al. [28] | |
| Increase in 5-HT1A autoreceptors in the midbrain areas | Increased 5-HT autoreceptor function and thereby a reduction in 5-HT release | Yates et al. [27] | |
| Dopamine (DA) | Low DA and/or DA metabolite levels (serum, CSF, and urine) | Dopaminergic dysregulation in depression responsible for anhedonia, loss of motivation, and psychomotor slowdown | Hamner and Diamond [29], Engstrom et al. [30] |
| Increased D2/D3-receptor binding in the basal ganglia and striatum | Dopaminergic synapse dysregulation (reactive to low DA levels?) | D’Haenen and Bossuyt [31], Shah et al. [32], Klimek et al. [33] |
Fig. 1.
Relationship among noradrenaline, serotonin, and dopamine and some behaviors
The monoaminergic hypothesis has enjoyed considerable support, since it attempts to provide a pathophysiologic explanation for the actions of antidepressants. However, in its original form it is clearly inadequate, as it does not provide a complete explanation for the actions of antidepressants, and the pathophysiology of depression itself remains unknown. The hypothesis has evolved over the years to include, for example, adaptive changes in receptors to explain why there should be only a gradual clinical response to antidepressant treatment when the increase in availability of monoamines is rapid. Still, the monoamine hypothesis does not address key issues such as the reason why antidepressants are also effective in other disorders, such as panic disorder, obsessive-compulsive disorder, and bulimia, or why all drugs that enhance serotonergic or noradrenergic transmission are not necessarily effective in depression (for example, amphetamine or cocaine). Despite these limitations, however, it is clear that the development of the monoamine hypothesis has been of great importance in understanding depression and in the development of safe and quite effective pharmacologic agents for its treatment.
In the past 2 decades, with the development of neuroscience, a great deal of success has been achieved in our understanding of the neurobiological basis of depressive syndromes and of cerebral systems’ activity, mainly concerning receptor-mediated intracellular mechanisms. Neuronal networks have been identified and characterized. It has been understood that the interaction monoamine-receptor is able to modulate the expression of intracellular proteins, such as CREB (cAMP response element binding protein) and BDNF (brain-derived neurotrophic factor). Through a number of their receptor subtypes, the serotonergic and noradrenergic systems regulate the cyclic adenosine 3′,5′-monophosphate (cAMP)-mediated signal transduction cascade, which activates protein kinases that phosphorylate specific proteins. One of these proteins is the transcription factor CREB, which mediates the cAMP activation of certain genes, such as BDNF [35]. This increased understanding of mechanims at the base of psychopathologies suggests that, beyond receptors, depressive mood is probably characterized by modifications in neurotrophic factors, CREB, and BDNF, which are regulated in turn by a modulation in gene activation.
However, despite the advances in recent years, two critical concepts should be carefully pointed out. It is worth noting that, in spite of an increase in knowledge about the neurobiological basis of depressive syndromes and about cerebral systems’ activity, no valid alternative hypothesis to monoaminergic theory is available to date. This might be due to the nature of clinical studies or the experimental models now available to examine the neuronal state of depressed patients. On the other hand, it should be noticed that animal models can provide crucial information on the whole range of neuronal functions not accessible in humans and potentially allow us to identify novel targets for antidepressant drug development, although they do not predict the clinical outcome and the latency time necessary for the therapeutic response.
Other classical neurotransmitters
Recently, some important advances in a better understanding of the psychopathology of depression have been made. Moving beyond monoamines, a growing body of experimental data indicates that other classes of compounds, such as neuropeptides and amino acids (the glutamatergic and GABA-ergic systems), are likely to play a significant role in the pathophysiology of affective disorders. The compounds currently under investigation are summarized in Table 2.
Table 2.
Classification of antidepressant drugs, approved for use or currently in research and development, on the basis of their mode of action and indication
| Transporter/receptor | Molecule | Pharmacologic action | Indication | Clinical phase |
|---|---|---|---|---|
| 5-HT | Fluoxetine, paroxetine, fluvoxamine, citalopram, escitalopram | Selective serotonin reuptake inhibitor (SSRI) | Depression, anxiety, obsessive-compulsive disorder, and some forms of severe shyness | Approved for use |
| Trazodone | 5-HT2 reuptake and receptor inhibitor; also known as serotonin antagonist reuptake inhibitor (SARI) | Depression; off-label use for panic disorder, insomnia, anxiety, and alcoholism | Approved for use | |
| Vilazodone | 5-HT1A partial agonist, 5-HT reuptake inhibitor | Depression | Phase III | |
| Lu AA21004 | 5-HT3 antagonist, 5-HT1A partial agonist | Depression, anxiety | Phase III | |
| NE | Reboxetine | NE reuptake inhibitor (NRI) | Depression | Approved for use |
| Tricyclic antidepressants (TCA): amoxapine, desipramine, nortriptyline | NE reuptake inhibitor | Depression, panic | Approved for use | |
| 5-HT/NE | Tricyclic antidepressants (TCA): Amitriptyline, clomipramine, doxepine, imipramine, trimipramine | NE and 5-HT reuptake inhibitor | Depression, panic, social anxiety, generalized anxiety, and obsessive-compulsive disorder | Approved for use |
| Noradrenergic and specific serotonergic antidepressant (NaSSA): Mirtazapine, mianserine | Adrenergic alpha2-autoreceptors and alpha2-heteroreceptors antagonist, 5-HT2 and 5-HT3 blocker | Depression | Approved for use | |
| Venlafaxine | 5-HT and NE reuptake inhibitor (SNRI) | Depression, generalized anxiety disorder, social anxiety disorder, and, since November 2005, in adults for panic disorder. Often effective for depression not responding to SSRIs | Approved for use | |
| Duloxetine | 5-HT and NE reuptake inhibitor (SNRI) | Depression, generalized anxiety disorder, pain related to diabetic neuropathy, and fibromyalgia | Approved for use | |
| NE/DA | Bupropion | NE and DA reuptake and receptors inhibitor; about twice as potent inhibitor of DA uptake than NE uptake | Depression and seasonal affective disorder. Also prescribed for smoking cessation | Approved for use |
| 5-HT/NE/DA | GSK 372475 (NS2359) | 5-HT, NE, and DA reuptake inhibitor (SNDR-I) | Depression | Phase II |
| DOV 216,303 | 5-HT, NE, and DA reuptake inhibitor (SNDRI) | Depression, attention deficit hyperactivity disorder | Phase II | |
| DOV 21, 947 | 5-HT, NE, and DA reuptake inhibitor (SNDRI) | Depression, attention deficit hyperactivity disorder, restless leg syndrome | Phase II | |
| Glutamate | TIK-101/D-cycloserine | NMDA partial agonist | Anxiety disorders | Phase II |
| AZD6765 | NMDA receptor antagonist | Depression | Phase II | |
| Delucemine (NPS 1506) | NMDA antagonist | Depression, stroke | Phase I | |
| AFQ056 | mGluR5 receptor antagonist | Anxiety disorders | Phase I | |
| GABA | AZD7325 | GABA receptor partial agonist | Anxiety disorders | Phase II |
| AZD6280 | GABA receptor partial agonist | Anxiety disorders | Phase I |
| Enzyme | Molecule | Pharmacologic action | Indication | Clinical phase |
|---|---|---|---|---|
| Monoamine oxidase | Iproniazide, tranylcypromine, phenelzine | Irreversible monoamine oxidase inhibitor (MAO-I) | Depression, panic, and social phobia | Approved for use |
| Moclobemide | Reversible monoamine oxidase Inhibitor (RIMA) | Depression, anxiety | Approved for use | |
| CX157 (Tyrima™) | Reversible monoamine oxidase A (MAO-A) inhibitor | Depression, anxiety | Phase II | |
| CX2614 | Reversible monoamine oxidase inhibitor (RIMA) | Depression, anxiety | Preclinical |
| Neuropeptide | Molecule | Pharmacologic action | Indication | Clinical phase |
|---|---|---|---|---|
| Tachykinin | Saredutant (SR 48968) | NK2 neurokinin receptor antagonist | Depression, anxiety | Phase III |
| GW823296 (orvepitant) | NK1 antagonist | Depression, anxiety | Phase I | |
| SAR 102279 | NK2 receptor antagonist | Depression, anxiety | Pre-clinical | |
| CRF | Pexacerfont (BMS-562086) | CRF1 antagonist | Depression, anxiety | Phase III |
| SSR 125543 | CRF1 antagonist | Depression, anxiety, hyperphagia | Phase I | |
| -Unnamed- | CRF1 antagonist | Depression, anxiety | Pre-clinical | |
| GSK561679 | CRF1 antagonist | Social anxiety disorder, MDD | Phase II | |
| GW876008 | CRF1 antagonist | Social anxiety disorder | Phase II | |
| Arginine vasopressin | SSR149415 | V1b antagonist | Depression, anxiety disorders | Phase II |
In this table mood stabilizers and natural substances are not mentioned. The table has been built on the basis of available data sheets of the drugs approved for use and on the search on the site ClinicalTrial.gov (consulted 2 February 2009) and/or the site(s) of the producers
Glutamate
Glutamate is the major mediator of excitatory synaptic transmission in the mammalian brain [36]. In the human brain, glutamatergic neurons project within and from the cortex to the subcortical regions, such as the locus coeruleus, raphe nucleus, and substantia nigra, where monoaminergic pathways are modulated. Under normal conditions, the glutamatergic system plays a role in a wide array of physiological functions, including memory and other cognitive tasks, neurotrophic and neurotoxic actions, and the induction of neuronal plasticity. However, in pathological conditions it is known to be a potent neuronal excitotoxin, triggering either rapid or delayed neurotoxicity. To date, an abnormal function of the glutamatergic system is known to be implicated in the pathophysiology of several neurodegenerative disorders, such as Huntington’s chorea, epilepsy, Alzheimer’s disease, schizophrenia, and anxiety disorders. Recent and increasing evidence suggests that abnormal activity of the glutamatergic system is likely to contribute to the impairments in the synaptic and neural plasticity observed in patients with severe mood disorders [37]. Glutamatergic abnormalities have been reported in plasma [38–40], serum [41], cerebrospinal fluid [42, 43], and brain tissue [44] of subjects affected by mood disorders. However, these studies are compromised by problems with potential medication effects, lack of appropriate control for diagnosis, post-mortem effects on metabolism, and the inability to identify the precise source of the glutamate in the peripheral tissue. Brain imaging studies showed the presence of elevated glutamate levels in the occipital cortex of depressed patients and decreased glutamate levels in the anterior cingulate cortex of MDD patients [37]. In addition, an increased glutamate content in several brain regions of individuals with bipolar disorder has also been reported. Several studies showed glutamate receptor alterations, mainly differences related to NMDA (N-methyl-d-aspartate) receptor expression and binding affinities between individuals with and without mood disorders. Decreased NMDA receptor binding and NR1 subunit expression have been reported in the superior temporal cortex of subjects with MDD and bipolar disorder [45]. Interestingly, two polymorphisms of the GRIN1 gene coding for the NR1 subunit and two other polymorphisms in the GRIN2B gene coding for NR2B were also recently reported to be associated with bipolar disorder [46, 47]. On the contrary, fewer postmortem studies have investigated the link between AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid) and kainate receptors and mood disorders. Only a single study reported an increased AMPA binding associated with a decreased glutamate receptor 1 (GLUR1) subunit expression in the striatum in bipolar disorder [48]. Furthermore, decreased levels of GLUR2 and GLUR3 were found in subjects with MDD [49]. Interestingly, the STAR*D (sequenced treatment alternatives to relieve depression) study, the largest prospective treatment trial for MDD, recently demonstrated associations of genetic polymorphisms within kainate and AMPA-glutamate receptors GRIK2 and GRIA3 with treatment-emergent suicidal ideation [50, 51], an uncommon symptom found in some patients following antidepressant treatment initiation. These studies, even if not yet confirmed, suggest the existence of a relationship between antidepressant treatment-emergent suicidal ideation and the glutamate system [52, 53]. In addition, many studies highlighted the importance of glial deficits in mood disorders as they could cause a complex disturbance in glutamatergic regulation. Deficits in glia function, as are found in some types of epilepsy, appear to be associated with dysfunctional accumulations of synaptic glutamate [54]. Postmortem studies [55, 56] have shown cortical glial cell loss and reduced glial density in patients with mood disorders. Glial loss has been well-documented in several brain regions, such as the dorsolateral prefrontal cortex [57], the orbitofrontal cortex [57], and the amygdala [58] from subjects with MDD and bipolar disorder. Altogheter, these data provide a link between the glutamatergic neurotransmitter system and the pathophysiology of mood disorders, thus suggesting that agents acting on the glutamatergic system can be explored as potential treatment in this field. Within this context, in fact, ketamine, an NMDA receptor antagonist, has been recently demonstrated effective in treating antidepressant-resistant patients [59]. Ketamine is of particular interest because it has been shown to yield a rapid and sustained antidepressant effect and has been reported as the only known drug leading to such a dramatic and prolonged response with a single administration [60]. In particular, Maeng and Zarate hypothesized that the rapid onset and the prolonged effects of ketamine are not the consequence of neuroplastic changes from glutamate modulation, rather to an increase in AMPA relative to NMDA glutamatergic throughput, which results in increased synaptic potentiation (for more detailed information, see [60]).
However, NMDA receptor antagonists of this class may have adverse psychiatric effects and may impair memory. Moreover, other than ketamine, also memantine, another NMDA receptor blocker exerting a voltage-dependent reversible block of this ionotropic receptor, which has been approved for the treatment of moderate-severe Alzheimer’s disease, demonstrated early onset efficacy in patients with MDD [61].
Gamma-aminobutyric acid
Gamma-aminobutyric acid (GABA) is the most widely distributed inhibitory transmitter in the mammalian brain [57]. In regions such as the cerebral cortex, hippocampus, thalamus, basal ganglia, cerebellum, and brain stem, it represents about one-third of the synapses [62]. GABA transmission is present in interneurons modulating local neuronal circuitry, such as noradrenergic, dopaminergic, and serotonergic neurons [63]. In the past decades considerable evidence has emerged that, in the brain, GABA acts as a modulator of neuronal function and behavioral processes, such as sleep, feeding, aggression, sexual behavior, pain, cardiovascular regulation, thermoregulation, locomotor activity, and mood [62, 64, 65]. This has been supported by the reduced GABA content in the plasma and cerebrospinal fluid of depressed patients [66–69]. In vivo proton magnetic resonance spectroscopy, a technique for a quantitative analysis of GABAergic systems with the use of brain scan, showed reduced occipital cortex GABA concentrations in a sample of severely depressed subjects [70]. Other studies demonstrated that treatment of depression with electroconvulsive therapy [71] or selective 5-HT reuptake inhibitor agents [72] was able to increase occipital cortex GABA concentrations in MDD patients, thus suggesting that GABA abnormalities may be normalized by antidepressant medication. Glutamate decarboxylase (GAD) and GABA aminotransferase are the enzymes involved in GABA synthesis and degradation [73]. GAD 65 and 67 isoforms were found to be decreased in the cerebellum in samples from both bipolar disorders and schizophrenia [74]. Additional studies indicated a reduction in GABA concentrations and increased GABAA receptor binding in the brain of depressed suicide victims, thus suggesting an impairment in GABAergic neurotransmission [75, 76]. The decreased GABA concentrations found in depression may reflect either decreased rates of synthesis or increased rates of catabolism [77]. However, these studies were not always confirmed, probably because of the rapid postmortem changes in brain GAD activity and GABA content. Furthermore, from a genetic point of view, genes coding for GABAA receptor subunits have been found to be associated with mood disorders. Reports from the literature showed that polymorphisms of the GABAA receptor 1 subunit (GABRA1) can be associated with mood disorders [78, 79], as well as the GABAA receptor α6 subunit variant (Pro385Ser) [79]. However, not all the studies found a significant association of the GABRA1 gene with depression or bipolar disorder [80]. Despite quite consistent findings of GABA deficits in mood disorders, GABAergic drugs, such as benzodiazepines, acting as allosteric agonist of the GABAA receptor, have not proven to be clinically efficacious as a monotherapy in the treatment of MDD [53, 77].
On the other hand, anxiety is frequently a comorbid condition in depressed patients, and some of the disturbances belonging to the anxiety spectrum are better treated with the SSRI antidepressant drugs than with benzodiazepines. Conversely, there are non-benzodiazepine anxiety relievers, such as buspirone, working on serotoninergic terminals. In addition, it should be stressed that presynaptic GABA receptors, both GABAA and GABAB, may regulate monoaminergic terminal activity. These observations do suggest that there is still room to investigate both at the clinical and preclinical level the role of GABAergic transmission in depression and in depression with comorbid anxiety.
Acetylcholine
Cholinergic systems, among other neurotransmitters in the brain, appear to be associated with various altered behaviors, such as psychosis, depression, agitation, and personality changes. One of the most consistent findings in neuropsychiatry is that patients with depression have dysfunctional neuroendocrine systems possibly resulting from prolonged responses to stress [81, 82]. Acetylcholine (ACh) plays a significant role in mediating neuroendocrine, emotional, and physiological responses to stress. For example, central ACh turnover is increased following stress [83], and ACh facilitates the release of several stress-sensitive neurohormones and peptides including corticosterone, adrenocorticotropin (ACTH), and corticotropin-releasing factor (CRF) [84], suggesting a dynamic interaction between cholinergic and monoaminergic systems in the regulation of mood and affect. As proposed by Janowsky et al. [85, 86], depression could be a manifestation of a central cholinergic predominance, whereas mania could be correlated to a relative monoaminergic predominance. The hypothesis that the overactivity of the cholinergic system over the adrenergic one could result in depressive symptoms [85] has been supported by several lines of evidence. The presence of exaggerated responses (behavioral, neurochemical, sleep) to cholinergic agents in patients with affective disorder compared to controls has been reported [87]. The indirect cholinesterase inhibitor ACh agonist, physostigmine, when administered to healthy subjects, produced symptoms of dysphoria, depression, anxiety, and irritability, but increased depressed mood in manic patients [88]; pyridostigmine, another cholinesterase inhibitor, increased growth hormone release to a significantly greater extent in depressed patients than in healthy subjects, suggesting cholinergic receptor supersensitivity in depressed subjects [89]. Furthermore, central acting cholinomimetics decreased rapid eye movement (REM) sleep latency and increased ACTH and cortisol levels, changes observed in depression [90–92]. Based on the “cholinergic-adrenergic hypothesis of mania and depression,” small pilot trials in humans with cholinesterase inhibitors and muscarinic agonists suggested that stimulation of muscarinic receptors may produce an antimanic effect [93]. Within this context, Burt and coworkers [94] demonstrated that the cholinesterase inhibitor, donepezil, when added to existing therapy in treatment-resistant bipolar patients, improved symptoms in over half of the patients. Bymaster and Felder [93] proposed that the antimanic activity could be mediated by activation of muscarinic M4 receptor. The rationale for the potential use of M4 agonists in the treatment of mania is based on the fact that these molecules, similarly to mood stabilizers, decrease cAMP formation and can block DA receptor functions (motor and mood effects) in cortical and limbic areas, which are affected in bipolar disorders [93]. Moreover, consistently with the hypothesis generated by Janowsky et al. [85], also the antidepressant effects of antimuscarinic agents, such as scopolamine, have been reported, thus supporting the link between muscarinic receptor function and mood disorders. Within this context, a rapid and robust antidepressant response to scopolamine in depressed patients with poor prognoses has been observed [95, 96]. Although the specific mechanism through which antimuscarinic effects may positively impact the pathogenesis of depression is still unknown, scopolamine seems to modulate, as other somatic antidepressant drugs, NMDA receptor function. In particular, muscarinic receptor stimulation regulates NMDA receptor gene expression in some brain regions, and scopolamine has been found to decrease messenger RNA concentrations for NMDA receptors 1A and 2A in the rat brain [97].
Furthermore, the role of nicotinic acetylcholine receptors (nAChRs) has also been investigated. Shytle et al. [98] and Silver et al. [99] have discussed the role of antidepressant medications in inhibiting nAChRs and suggested that antagonism of these receptors could contribute to their effectiveness in reducing symptoms of depression and mood instability in patients with comorbid depression and bipolar disorder. Modulation of nAChRs by antidepressants, in fact, plays important roles in neuronal circuits regulating mood, by regulating stress-related effects in hypothalamic pituitary adrenal axis, behavioral reinforcement in mesolimbic DA system and citoplasticity in hippocampus [98]. Based on the evidence supporting the hypothesis that nicotinic receptors inhibition may reduce depression and stabilize mood [100], future research should fully investigate the therapeutic potential of nicotinic receptor antagonists as a novel approach to treat affective disorders. However, much work has to be done. It is still controversial whether the antidepressant-like effect of nAChRs modulation is induced by activation, desensitization, or inhibition of central nAChRs, and to date the specific nAChR subtype/s involved remain unknown.
Furthermore, this hypothesis is also somewhat controversial, as suggested by data showing that acetylcholinesterase inhibitors relieve depressive symptoms, even in demented patients [101, 102]. The putative use of nicotinic antagonists could be based on the fact that nicotinic agonists increase agitation and anxiety, symptoms which can be signs of depression. On the other hand, such an effect in these patients may be linked to the action of cholinesterase inhibition on the cognitive function.
Finally, the potential antidepressant activity of drugs inhibiting cholinergic activity, as outlined before, should be carefully evaluated taking into consideration the possible negative effects on the cognitive function of such agents. A clinical observation supports this warning. Literature data show that in the elderly tricyclic antidepressant and SSRI with muscarinic receptor blocking properties should be avoided, if possible, because of their anticholinergic effect both in the periphery and on cognition [103, 104].
Other non-classical (peptidergic) transmitters
About 30 years ago the observation that neuropeptides serve as signalling molecules in the nervous system generated great expectations for the drug industry. Much progress has been made since then in exploiting neuropeptide systems pharmacologically in the psychiatric field. Nowadays, the health burden of stress-related diseases, including depression and anxiety disorders, is rapidly increasing, whereas the range of available pharmacotherapies to treat these disorders is limited. In affective disorders several neuropeptides seem to be causally involved in mediating the response to stress, thus identifying neuropeptide systems as attractive therapeutic targets for depression and anxiety disorders [105]. Interestingly, repeated administration of antidepressant drugs is able to induce adaptive changes in non-monoaminergic systems, such as orexinergic neurons [106]. Furthermore, other neuropeptides involved in depression-related responses such as tachykinins [substance P (SP) and neurokinin A], CRF, vasopressin, neuropeptide Y, neurotensin, and galanin have received recent attention as candidates for antidepressant drug development.
Corticotropin-releasing factor (CRF)
The 41 amino acid neuropeptide CRF initiates the hypothalamic-pituitary-adrenal (HPA) axis response to stress and has been the subject of intense investigation in the pathophysiology and treatment of depression and anxiety disorders. A large body of evidence correlates stressful life events with an increased vulnerability for affective and anxiety disorders; stressful events often precede the onset of depression, and stress has also been associated with the severity of the illness [107, 108]. Furthermore, stressful life events in childhood have been shown to predispose an individual for development of mood and anxiety disorders in adulthood. In mammalian brain, CRF is heterogeneously distributed throughout the CNS and interacts with two G-protein-coupled CRF receptor subtypes (CRF1 and CRF2 receptors) [109]. One of the molecular mechanisms associated with depression is an abnormal HPA activity [110], driven by CRF-containing neurons, which start to coexpress vasopressin when chronically activated, in turn able to enhance CRF actions. Dysfunction of the HPA system has been extensively studied since various researchers independently reported that plasma cortisol concentrations, following a higher release in ACTH, were elevated in a majority of patients with MDD. Moreover, synthetic glucocorticoid dexamethasone did not suppress plasma ACTH and cortisol concentrations in depressed patients [111]. In depressed patients cortisol levels are increased mainly during the afternoon and the evening, whereas in healthy subjects the peaks of plasma cortisol concentrations are detected during the morning. These abnormal cortisol levels are due to a defect in neurotransmitter regulation of CRF release. CRF is hypersecreted from hypothalamic as well as from extrahypothalamic neurons in depression, resulting in hyperactivity of the HPA axis and increase in CSF concentrations of CRF [112]. Elevated concentrations of CRF in CSF of drug-free patients with MDD and from suicide victims compared with patients with other psychiatric disorders and healthy controls have been reported [113, 114]. The elevations of CRF neuronal activity are also believed to mediate certain behavioral symptoms of depression involving sleep and appetite disturbances, reduced libido, and psychomotor changes. However, other studies have been unable to replicate these observations [115, 116]. Differently from CSF data, cerebral levels of CRF appeared not to be altered. Transgenic CRF overexpressing mice showed an increase in anxiogenic behavior [117] and a different ability to adapt to an environmental stressor, probably related to individual differences in stress reactivity [118]. Interestingly, there is evidence that CRF1 receptors play an important role in mediating the HPA response to stress and the extrahypothalamic mediation of stress-related behaviors [119]. Within this context, some studies, showing that the anxiolytic-like effects of CRF1 receptor antagonists are more pronounced in rats pre-exposed to stressors such as immobilization and forced swimming, allowed to hypothesize that CRF1 receptor antagonists might be capable of blocking pathological CRF-mediated stress responses without producing side effects caused by a general suppression of HPA activity [120].
The potential clinical usefulness of CRF1 receptor antagonists led to synthesizing several CRF1 antagonists for the treatment of anxiety and depression in patients with MDD under investigation as reported in Table 2 [121].
Finally, it is worth highlighting the amount of literature data on ACTH abnormal levels in depression at the expense of a lack of information on its precursor, the proopiomelanocortin (POMC) or big-ACTH. POMC initially is synthesized as an inactive molecule that requires posttranslational modifications to generate bioactive products, among which are ACTH, β-endorphin, and melanocyte stimulating hormone. It should be interesting to evaluate whether an alteration in POMC is also associated with depression and which neuronal structures could be involved.
Arginine vasopressin
Vasopressin (AVP, arginine vasoPressin) seems to be a key regulator of HPA axis, acting synergically with CRF to secrete ACTH and other corticoid hormones in physiological and stress-related conditions [122]. The vasopressinergic system consists of hypothalamic AVP-containing cells located in the paraventricular and supraoptic nucleus and extrahypothalamic AVP-containing neurons (limbic system and amigdala) and may be critically involved in the ethiopathogenesis of depression as supported by postmortem studies on the brains of individuals with a known history of depression [123]. In depressed patients an overproduction of AVP has been detected, measured as increased AVP plasma levels [124, 125], number of AVP expressing cells in paraventricular nucleus [123], or AVP content in the paraventricular nucleus [126]. Furthermore, increased AVP mRNA was detected in supraoptic nuclei of depressed patients [127]. These findings are consistent with experimental studies in rodents showing that paraventricular neurons are able to coexpress both CRH and AVP and tend to increase the relative predominance of AVP production by stressors [128]. Furthermore, in vivo and in vitro studies showed that a single nucleotide polymorphism (SNP) in the AVP locus, specifically the SNP[A(-1276)G], resulted in overexpression of AVP and in increased HPA axis function in a rat selected for high anxiety behavior [129]. In addition in AVP-deficient rodents, such as Brattleboro rats endowed with a single nucleotide deletion (-G326) in the AVP gene, some authors reported low levels of basal ACTH and corticosterone [130], decreased responses to stress in terms of endocrine response such as low ACTH response, decreased adrenal sensitivity to ACTH [131, 132], and behavioral responses such as decreased anxiety in a variety of models of depression (open-field, force swimming, and sucrose preference test) [133, 134]. As other hormones, AVP exerts its effects through interaction with three specific receptors (V1a, V1b, or V3 and V2) [135, 136], and the vasopressin 1b (V1b) receptors seem to be the prominent ones involved in depression and anxiety disorders, although also the role of V1a subtype has been considered [137]. Studies in V1b-receptor KO-mice reported a normal HPA axis function [138] and a reduced aggressive behavior along with again a normal neuroendocrine response and social response to stress [139, 140], with no phenotypic differences in stress-induced models compared to wild-type mice [141]. This might be due to some complementary/compensatory mechanism(s) probably involving other AVP or CRF receptor subtypes, but further studies are necessary to explore this hypothesis.
The involvement of the V1b receptor subtype is supported by experimental evidence using SR149415, a selective V1b antagonist, at this time in phase II clinical trials in patients with anxiety and MDD (Table 2) [142]. Preclinical studies in rodents showed that this compound is endowed with antidepressant-like activity in different models of depression (forced swimming test, olfactory bulbectomized-induced hyperemotionality, DRL-72s schedule test, unpredictable chronic mild stress) [142–146]. Its antidepressant-like effects are also supported by the data obtained administrating SR149415 directly into the lateral septum, the central, basolateral, or medial nuclei of amygadala in the rat forced swimming test [147, 148]. Only one study failed to detect behavioral changes [149]. Furthermore, SR149415 is able to inhibit the enhancement of ACTH levels induced by acute restrain stress with no influence on ACTH basal release, as expected by a V1b receptor antagonist [150]. In addition to the vasopressin V1b selectivity, SR149415 acts also as an oxytocin receptor antagonist, and this may be helpful to its antidepressant-like activity [151].
To date, conflicting data on the role of V1a receptor subtype in depression have been reported. V1a-KO mice show normal anxiety response to stress, and an overexpression of V1a receptor seems to be associated with an enhanced anxiety behavior [152]. Opposite results, a reduced anxiety-related behavior, have been found by Landgraf et al. [153] in a model of V1a-deficient mice obtained with the infusion of an antisense oligodeoxynucleotide into the septum, suggesting an involvement of this tract in anxiety onset. Recently, an antidepressant-like action has been found in murine models of depression using SRX251 [154], a promising V1a antagonist, at this time, in phase I of development for other therapeutic target. Moreover, a better understanding of the physiological role of V1a receptor subtype will probably help to understand its role in anxiety and depression disorders.
Complexively, the data on CRF and vasopressin point to the existence in depression of a profound dysfunction of the systems participating to the endocrine response to stress, which includes their involvement both in brain and periphery and, obviously, the coparticipation of the monoaminergic stress system. Finally, the traits that appear to be particularly affected by the derangement of these systems include anxiety as a key feature deepening the biological link between depressed mood and anxiety.
Substance P
The isolation of substance P (SP) in 1931 and the later discovery of its preferred neurokinin (NK)1 receptor led to intense research aimed at elucidating the biological role of SP, mainly within the CNS. SP is an 11-amino acid peptide belonging to the tachykinin family, and neurons containing SP are widely distributed in the periphery and CNS [155]. To date, there is a large body of evidence supporting the hypothesis that SP is one of the most important neurotransmitters and neuromodulators in the brain [156, 157]. SP has been suggested to be involved in the etiopathology of psychiatric disorders including affective disorders, anxiety disorders and cognitive disorders [158–160], on the basis of data from animal and human studies. There is some evidence for increased SP levels in the plasma [161] and CSF [162] of depressed patients. Furthermore, increasing evidence suggests that SP and its NK1 receptor might play an important role in the modulation of stress-related affective behaviors [163]. This observation is reinforced by the fact that SP and NK1 receptor are expressed in brain regions involved in stress, fear, and affective response, such as the amygdala, hippocampus, hypothalamus, and frontal cortex and that SP content in these areas is modified by stressful stimuli [163]. In addition, SP is colocalized with other neurotransmitters such as 5-HT [164], NE [163], DA (which are known to be involved in the regulation of stress, mood, and anxiety), and neuropeptides such as CRF. Therefore, it was hypothesized that blockade of the NK1 receptor might have anxiolytic and antidepressant effects, as demonstrated in several animal models frequently used for assessing the activity of antidepressant and/or anxiolytic drugs. In addition, knockout animals for the SP-encoding gene as well as NK1 receptor knockout mice show decreased depression- and anxiety-related behaviors when compared to wild-type animals [163]. The antidepressant efficacy of the first NK1 receptor antagonist to be developed clinically, MK0869 (Aprepitant), was originally demonstrated in patients with MDD and high anxiety [165] and has recently been replicated with a second compound, L759274 [166]. Aprepitant, however, failed to exert antidepressant effects in recent phase III trials [167]. The future of NK1 receptor antagonists as antidepressant drugs will depend on the outcome of clinical trials with other NK1 receptor antagonists. The discovery of a new family of tachykinins, the hemokinins and endokinins, which acts on NK1 receptors and has potent effects on immune cells, has implications for the clinical use of NK1 receptor antagonists [168]. Hence, specific therapeutic strategies may be required to enable NK1 receptor antagonists to be introduced for treatment of neuropsychiatric disorders. Furthermore, it has been reported that several antidepressants (TCAs such as clomipramine and SSRIs such as fluoxetine) did not act as NK1 antagonists, but their action on SP-induced effects seems to be due to their calcium-blocking properties as reported in functional and biochemical studies in humans and rodents [169–172].
Another member of the tachykinin family, neurokinin A, which acts through NK2 receptors, is also under investigation for its potential role in depression and anxiety disorders [173, 174], and clinical trial to assess the antidepressant effects of NK2 receptor antagonists are currently underway [163, 168].
Neuropeptide Y
Neuropeptide Y (NPY), is a 36 amino acid neuropeptide discovered in 1980 by Tatemoto and Mutt [175]. NPY modulates neuronal activity and HPA-axis function, influences circadian rhythms and seizure activity, and is involved in memory processing and cognition, all of which are dysregulated in many psychiatric states [176, 177]. It is abundantly expressed, together with its receptors (Y1–Y5) in numerous brain areas, including the locus coeruleus, hypothalamus, amygdala, hippocampus, nucleus accumbens, and neocortex. Impaired central NPY signaling may therefore be involved in the pathophysiology of depression, anxiety, and schizophrenia [177]. Data from animal and human studies have led to the hypothesis that NPY is involved in the etiology and pathogenesis of affective disorders. In this regard, decreased peptide and mRNA NPY were found in hippocampus of both the genetic and environmental rat models of depression [178]. Reduced NPY content in the caudate nucleus and frontal cortex in brains from suicide victims has also been found [179]. Moreover, NPY was found to be reduced in CSF of depressed patients [177, 178]. Furthermore, antidepressive treatments selectively increased NPY in rat hippocampus and in human CSF. In addition, when injected to rats, NPY showed antidepressive effects that have been antagonized by NPY-Y1 blockers [178].
Neurotensin
Neurotensin (NT) is a neuropeptide consisting of 13 amino acids, involved in locomotion, reward, stress, and the pathophysiology of schizophrenia and depression [180]. NT was reported to be widely distributed in the brain with the greatest concentrations in the hypothalamus and basal forebrain, intermediate levels in the basal ganglia, brainstem and dorsal horn of the spinal cord, and low concentrations in the thalamus and cortex [180]. Locomotor and reward effects depend on stimulation of NT-1 receptors linking NT systems and the mesotelencephalic DA system. There are indications that exogenously administered NT produces pharmacological actions similar to those of antipsychotic drugs, particularly atypical antipsychotics [181]. Moreover, NT alters the firing rate and the metabolic activity of DA neurons, especially in the mesolimbic system. A series of studies showed that antipsychotic drugs increase both NT mRNA expression and NT concentrations in specific DA terminal areas [182–184]. The NT function as an endogenous antipsychotic is based on clinical investigations in which low CSF NT concentrations were found in drug-free schizophrenic patients [185]. While the NT function has been well documented in psychosis [186], the possible role of endogenous NT in depression has essentially not been fully elucidated. Cervo et al. [187] examined locomotor activity and behavior in the forced swim test, a model of depression-like behavior, in rats that had received NT in the ventral tegmental area. The results suggested that activation of the mesolimbic DA system through administration of NT produced antidepressant-like effects, as evaluated by a behavioral hyperactivity characterized by an increase in exploratory behaviors. However, to date the NT hypothesis has not been pursued, and no NT agonists have been developed for depression.
Galanin
Galanin, isolated from the porcine gut by Viktor Mutt and coworkers in 1983, is a 29 (30 in human) amino acid neuropeptide [188], widely distributed in brain regions implicated in the regulation of mood and anxiety, including the ventral forebrain, amygdala, hypothalamus and brainstem, in a number of species [189]. Galanin is of particular interest since it is colocalized with 5-HT in the dorsal raphe nucleus (DRN) and with NE in the LC, nuclei known to play a major role in affective disorders and in the action of antidepressant drugs. The neuropeptide has been shown to act as an inhibitory neuromodulator of these neurotransmitters in the rodent brain [190, 191]. Analyses of the role of galanin in the brain have been based on administration of the peptide via a chronic cannula placed in the lateral ventricle (icv), or directly into relevant brain regions, or on in vitro application to brain slices. Both in vitro and in vivo studies suggest that galanin could mediate its actions via multiple receptors in brain tissue [192]. Three distinct galanin receptor subtypes (GAL-R), GAL-R1, GAL-R2 and GAL-R3, have been identified in the rodent brain, which are coupled to G-protein [193]. Several pharmacological studies suggest a role of galanin in depression-like behavior in rodents. The first pharmacological evidence for involvement of endogenous galanin in depression-like behavior was obtained after galanin icv infusions into the ventral tegmental area, showing a significant increased immobility time in forced swim test in rats [194], which was fully blocked by the galanin receptor antagonist M35. Importantly, the antagonist M35 given icv produced a significant decrease in immobility in the forced swim test, indicative of an antidepressant-like effect [195]. Ogren et al. [196] showed from experimental studies in rodents that in vivo galanin is a potent modulator of brain 5-HT transmission, and in particular 5-HT1A receptor-mediated functions. Once given icv, galanin showed strong inhibitory interactions with 5 HT1A receptor functions, particularly in the dorsal raphe, but also in the hippocampus. Since pre- and postsynaptic 5-HT1A receptors in the dorsal raphe and hippocampus are implicated in the action of antidepressant drugs, it has been hypothesized that galanin receptors may be an important target for the development of novel antidepressant drugs. Within this context, stimulation of GAL-R1 and/or GAL-R3 receptors resulted in depression-like phenotype, while activation of the GAL-R2 receptor attenuated depression-like behavior [192, 197, 198]. At present, there is no information on the role of galanin in humans, with the exception of one short-term study, carried out in depressed patients, which showed an acute and rapid antidepressant-like effect of galanin following intravenous administration as demonstrated by a decrease in Hamilton depression rating scale score and an increase in REM latency [199].
Altogether the data on peptides, with the exclusion of CRF and vasopressin, do not allow to suggest a general working hypothesis and/or a hierarchy of events to establish whether the observed changes of substance P, neurotensin, neuropeptide Y, and galanin are primary events or are driven by the alteration in monoaminergic or other transmission systems. On the other hand, their modulatory roles are appreciated and may be useful pharmacological targets. Within this context, it will be important to establish whether acting upon these targets will allow to control MDD in a large number of patients, as it is with the presently available drugs, or only a subpopulation of patients characterized by a specific neurochemical alteration profile.
Depression: a matter of brain plasticity
Depression and synaptic strength
Long-term potentiation (LTP) and long-term depression (LTD) regulate the strength of synaptic transmission and the formation of new synapses in many neural networks. Currently, a few key aspects of the LTP are well established. A single train of stimuli initially produces an early phase of LTP, which lasts only 1–3 h and does not require new protein synthesis. It involves covalent modifications of pre-existing proteins that lead to the strengthening of pre-existing connections. Repeated trains of electrical stimuli produce a late phase of LTP, which persists for a longer time, up to 24 h, and requires both translation and transcription. Several kinases can participate in this local synaptic regulation, among them the protein kinase A, the protein kinase C, and the mitogen-activated protein kinase, playing dominant roles in activation of the transcription factor cAMP response-element-binding protein (CREB), in turn able to regulate a transcription cascade ultimately involved in a process that yields synapse-specific structural changes [200–204]. It has been proposed that long-term synaptic plasticity or its modulation might be disturbed in depressed patients [205, 206]. This observation is reinforced by the fact that different antidepressants and electroconvulsive therapy have been shown to effectively modulate synaptic plasticity in the dentate gyrus and the CA1 subfield of the hippocampus and in the neostriatum [206, 207].
The relationship between memory and depression is a complex one since brain circuits and neurotransmitters involved in depressed mood are also involved in attention and memory trace formation [208]. This intermingling of the two systems is further strengthened by the novel information on the growth factor changes in the hippocampus, a brain area that is key for memory (see next paragraph). From the clinical point of view, it is well known that, particularly in the elderly, depressed mood negatively influences cognitive functions and that depression may, in some cases, be prodromal to the manifestation of a cognitive disorder [209]. However, at this time, while published data suggest that antidepressants may have favorable effects on attention and memory, no data on drugs affecting memory support an action also on depressed mood, suggesting that the two systems are indeed separate.
Growth factors
While in the past depression research has focused mainly on the regulation of 5-HT, NE, and DA, their synthesizing and metabolizing enzymes, transporters and receptors, more recent studies have identified alterations of intracellular signal transduction pathways and target genes that contribute to the possible cause of depression (Fig. 2). Studies of neurotrophic factors, particularly brain-derived neurotrophic factor (BDNF), have been of particular interest and have led to the “neurotrophic hypothesis” of depression [210]. The “neurotrophic hypothesis” postulates that reduced levels of neurotrophic factors, mainly BDNF, contribute to the hippocampal atrophy, as observed in depressed patients, whereas antidepressant treatments exert their therapeutic effects through increased expression of neurotrophic factors in the hippocampus [211]. BDNF, the most abundant neurotrophic factor, promotes the growth and development of immature neurons and enhances the survival and function of adult neurons [212]. BDNF plays a role in the survival of neurons during hippocampal development, and this may relate to its putative role in depression. Antidepressant drugs increased expression of proteins associated with synaptic plasticity [213]. There is evidence demonstrating a requirement for BDNF in synaptic plasticity for LTP [214] and for persistence of long-term memory storage [215]. As BDNF has a role in synaptic plasticity, alterations in BDNF signaling may well be involved in mood disorders, such as MDD, and in the mechanism of action of antidepressant drugs. Although recent findings suggest a different BDNF action/function depending on the brain area involved [216], BDNF mRNA expression is decreased by stress and glucocorticoids in the hippocampus, whereas several antidepressant drugs are able to enhance it [217]. Compared with normal human subjects, levels of BDNF have been reported to be lower in postmortem brain tissue from depressed patients but higher in those taking antidepressants at the time of death [218]. Moreover, brain imaging studies have documented a reduction in hippocampal volume in depressed subjects, which can be attenuated by antidepressant treatment [219]. Decreased volumes of the prefrontal cortex and the amygdala brain regions have also been linked to altered mood, anxiety, and cognition in depressed patients [210, 219]. In addition, several reports demonstrate that serum BDNF, which likely reflects BDNF levels in the brain, is significantly decreased in depressed patients [220, 221]. This decline in serum BDNF levels is negatively correlated with the severity of depressive symptoms [220]. In murine models of depression infusion of BDNF into the midbrain or hippocampus produces antidepressant-like effects [222]. Moreover, repeated administration of both electroconvulsive shocks as well as antidepressant drugs increase BDNF gene expression in rat brain [223, 224]. Exogenous application of BDNF, which induces a long-term potentiation (BDNF-LTP) [225], required upregulation of the immediate early gene Arc [226] and five other genes regulated with Arc during BDNF-LTP; moreover, an upregulation of these BDNF-LTP-associated genes only after chronic antidepressant administration has been observed [226], thus suggesting that antidepressant treatment can promote gene expression responses linked to BDNF signaling and long-term synaptic plasticity. In order to elucidate BDNF dysfunctions in mood disorders, a single nucleotide polymorphism (SNP) was identified in the coding exon of the BDNF gene resulting in a valine (Val) to methionine (Met) change at amino acid position 66 (Val66Met) [227]. This polymorphism has been demonstrated to be correlated with a decreased hippocampal volume and abnormal hippocampal activation, which may underlie an enhanced vulnerability [228]. In addition, a recent study reported that a highly significant excess of the Met allele is present in geriatric depressed patients [229].
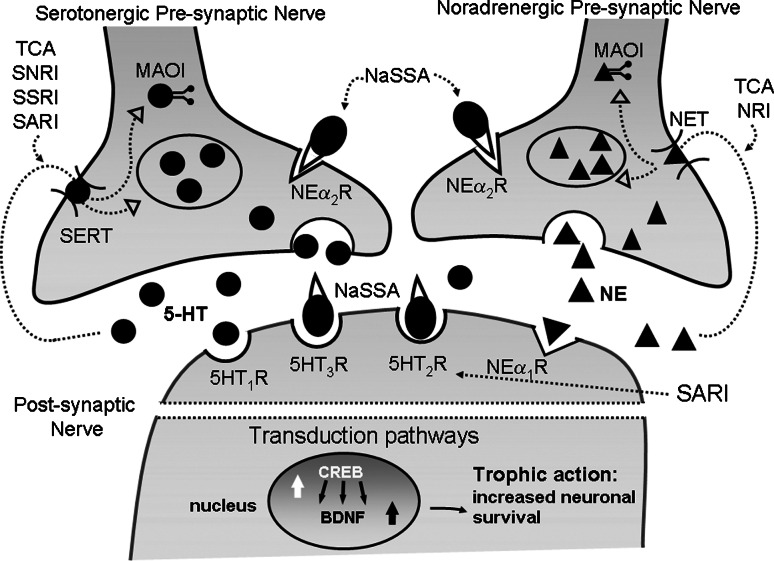
Fig. 2.
An example of some antidepressants’ activity on noradrenergic and serotonergic nerve endings. The figure shows the acute effect of some antidepressants on NE and 5-HT nerve endings. TCAs, NRIs, SSRIs, SNRIs, and SARIs modulate the reuptake of monoamines. NaSSA antidepressants are antagonists of some 5-HT receptor subtypes and also act as adrenergic alpha-2 receptors antagonists, thus controlling the monoaminergic release. This pharmacological action on 5-HT2 and 5-HT3 receptors, together with the effect on reuptake, promotes 5-HT action on other receptor subtypes, mainly 5-HT1A, involved in the cerebral circuits deranged in depression. Chronic effects of antidepressants involve further mechanisms on signal transduction, second messengers formation, and transcriptional control of specific genes, such as BDNF. Not indicated in the figure is the dopaminergic nerve ending. Some antidepressants have a triple action on 5-HT, NE, and DA synapses (see text). Abbreviations: TCA TriCyclic antidepressant, SNRI serotonin and norepinephrine reuptake inhibitor, SSRI selective serotonin reuptake inhibitor, SARI serotonin antagonist reuptake inhibitor, NaSSA noradrenergic and specific serotonergic antidepressant, MAOI monoamine oxidase inhibitor, NET, norepinephrine transporter, SERT serotonin transporter, CREB cAMP response element binding protein, BDNF brain-derived neurotrophic factor
Furthermore, in an animal model of a behavioral antidepressant, referred to as learned safety, a learning process critical for preventing chronic stress, an increased expression of BDNF has been found in the hippocampus, promoting the survival of newborn cells in the dentate gyrus of the hippocampus [230].
On the contrary, the social avoidance induced by chronic social defeat, a novel murine model of depression, seems to be strictly dependent on BDNF signaling in the mesolimbic area. It should be stressed that ventral tegmental area-nucleus accumbens (VTA-NAc) circuits play a critical role in reward-emotion-related behaviors. In detail, VTA-NAc increased BDNF content induced by stress or by direct BDNF infusion may result in neuronal changes that could be maladaptive [231]. A pro-depressant action of BDNF in the mesolimbic circuits was demonstrated, reversed by chronic but not acute administration of antidepressant [232–234]. Furthermore, NAc knock-down of BDNF produced the same effect of antidepressant chronic therapy [232].
This seems to suggest a more complex picture in the BDNF implications in the pathogenesis of depression-related disorders and to probably open new potential strategies for pharmacologic intervention.
The observations on all neuromodulatory peptides and growth factors introduce into the depression field the concept that has emerged in the case of neurodegenerative diseases, that is, that besides the neurotransmitter deficits also growth factors and protein/protein interaction malfunctioning may lead to the disease [235]. This view is also supported by recent observations on the erythropoietin alterations in depression and on the experimental antidepressive effects of erythropoietin [236].
Depression: a body-brain dialogue
Is the female brain depressed? Depression and sex hormones
Dysregulation of hypothalamic-pituitary axes affecting adrenal, thyroid, and gonadal function have also been associated with mood disturbance. In particular, the hypothalamic-pituitary-gonadal (HPG) axis has been the focus of interest concerning the study of gender-based differences in depression at various points across the life cycle [237].
The fact that men and women differ with respect to the prevalence of several psychiatric disorders, certain aspects of cognitive function, and certain personality traits may possibly also reflect an influence of sex steroids on human behavior. In addition on their actions on their classical targets, sex steroids are able to exert important effects on CNS, regulating neuronal structure and synaptic plasticity. Furthermore, at a molecular level, steroids modulate synthesis and release of several transmitters as well as the expression of neuronal growth factors and their receptors [238].
A close functional interaction between the HPA-axis and the HPG-axis has been reported [229], based on the effects of sex hormones on the HPA axis. Such interactions may be a basis for the higher prevalence of mood disorders in women compared to men [239]. The prevalence of MDD increases during the reproductive years, mainly during times when sex hormone levels show rapid fluctuations, as observed in the premenstrual period or post partum or during the transition phase to menopause or the oral contraceptive treatment [240–243]. In addition, women with histories of depression appear to be more vulnerable to recurrent episodes of depression during periods of significant reproductive endocrine change. In depressed women an increased HPA axis and a parallel reduced HPG-axis activity has been observed, which is linked to lower plasma levels of estrogen and higher levels of androgens [244]. Reduced plasma levels of estradiol could be related to the inhibition of the reproductive axis by the HPA axis, which is comparable to the situation during stress or after CRF administration [244]. Sex hormone replacement therapy indeed seems to improve mood in elderly people and may make women with Alzheimer’s disease less vulnerable to depression [245, 246]. However, to date, the exact mechanism for an involvement of sex hormones in mood disorders has not been fully understood yet. Apart from the effects on the HPA axis, an interaction between sex hormones and the serotonergic system has also been proposed [244]. In animal studies, differences in estrogen concentration between the sexes may modulate increased 5-HT activity seen in female rats, including higher 5-HT levels in the brain stem and limbic forebrain [247], 5-HT synthesis, and 5-HT turnover [248]. Human studies showing the ability of estrogens to modulate 5-HT function are relatively sparse. Women have decreased whole brain 5-HT synthesis [249], increased CSF 5-hydroxyindoleacetic acid levels [250], and decreased 5-HT2 receptor binding capacity in specific brain regions [251] compared to men. Estrogen and other gonadal hormones have been reported to facilitate down-regulation of 5-HT2 receptors [252] also when associated with chronic administration of antidepressants, which has been linked to the mechanism of delayed therapeutic action of antidepressants [237]. Interestingly, the possible influence of polymorphisms in sex-steroid-related genes on behavior and psychiatric morbidity has been recently explored, suggesting that estrogen receptor α polymorphisms may influence interindividual differences, at least in women, in anxiety, depression, and schizophrenia [253].
Emerging players involved in depression: new therapeutic avenues?
With the development of neuroscience, a great deal of success has been achieved in a better identification and characterization of the networks involved in depressive syndromes. As an example, searching for the genetic and functional mechanisms underlying the HPA dysfunction in depression, recent research has focused on genes involved in HPA axis regulation, among which FKBP5, a cochaperone of HSP90 regulating glucocorticoid receptor (GR) function, has gained growing interest as an important regulator of GR sensitivity and HPA axis responsivity. FKBP5 is located on chromosome 6p21, a chromosomal region associated with bipolar disorder and psychosis [254] and is mainly expressed in the brain and in a wide range of human cell tissue, including muscle, liver and thymus. The heatshock protein FKBP5 is a part of the mature GR heterocomplex reducing the receptor affinity for cortisol and is thought to diminish the dynein binding and nuclear translocation of the GR complex [255]. The interest in this protein has been recently reinforced by the observation that genetic variants of FKBP5 have been reported to be associated with adapatative changes in HPA regulation and to be related to a different antidepressant response, suggesting FKBP5 as an important target for further studies of depression and treatment response [256].
Furthermore, important new literature has showed that epigenetic mechanisms of gene regulation in neurons could be involved in the regulation of psychiatric disorders such as depression and mediate stable adaptations in brain function [257, 258]. Changes in histone acetylation, histone methylation, and DNA methylation have been documented in specific brain regions both in animal models of stress, depression, and antidepressant treatment and in human brains and have been related to an altered behavior. In particular, changes in histone modifications and DNA methylation have been mainly documented at the promoters of BDNF and GR genes and only on the hippocampus [227, 259, 260]. These data suggest the involvement of a chromatin remodeling in the formation of stable neurobiological adaptations in the hippocampus that could explain some of the long-lasting changes in behavior induced by chronic stress and reversed by chronic antidepressants. Moreover, these studies also suggest the potential use of specific inhibitors for epigenetic regulators (such as histone deacetylases or histone demethylases) as antidepressant treatments. However, the problem of the brain area selective effect of such drugs should be considered.
Depression and antidepressant response: a matter of molecular genetics?
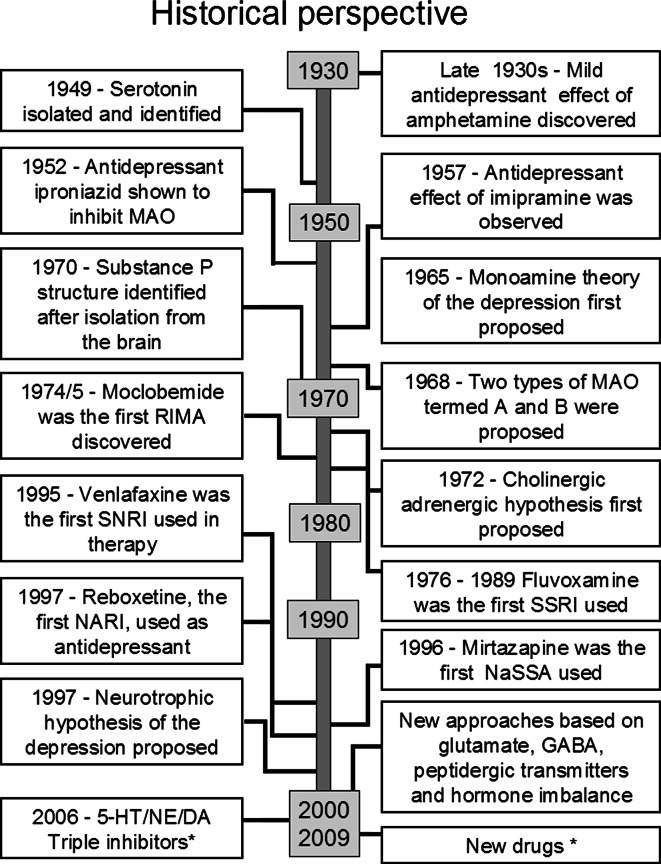
Drugs interfering with the uptake of biogenic amines have been used to treat depression for about 4 decades (see Fig. 3 for an historical view). TCAs and MAOIs have represented important drugs due to their clinical efficacy, even if to date their usefulness is reduced because of many side effects. SSRIs or selective NE reuptake inhibitors (NRIs) were originally designed to find drugs as effective as TCAs, but more selective towards a single monoamine transporter and with fewer side effects. Recently, 5-HT and NE inhibitors (SNRIs) (dual uptake inhibitors) have been successfully introduced into the market. However, also these drugs show a delayed onset of action and side effects altering patients’ compliance. Moreover, the efficacy of all currently used antidepressants has been questioned because of the existence of a significant proportion of drug-resistant patients and a debated drug/placebo effect. A recent development has been obtained with the introduction of the triple uptake inhibitors, designed to inhibit the uptake of all three neurotransmitters, 5-HT, NE, and DA, mainly involved in depression. Triple uptake inhibitors (SNDRIs) are expected to be the next generation of drugs for the treatment of MDD [261] (Table 2). Preclinical studies indicate indeed that they could produce a more rapid onset of action and possess greater efficacy than traditional antidepressants [261]. DOV 216,303 [(±)-1-(3,4-dichlorophenyl)-3-azabicyclo-[3.1.0]hexane hydrochloride], the prototype of the compounds referred to as triple uptake inhibitors, has been demonstrated to be active in tests predictive of antidepressant activity, such as the mouse forced-swim test and locomotor depression [262] (Fig. 3).
Fig. 3.
Historical perspective of the different hypotheses on depression ethiopatology and of related drugs. *See Table 2 for details
To date, because of the less severe side effects than those of other antidepressants, SSRIs represent the class of drugs of choice for treating MDD. However, a substantial number of patients benefit only partially or not at all from treatment. Drug response can be influenced by genetic factors and several physiological and environmental factors, including age, renal and liver function, nutritional status, smoking and alcohol consumption. In particular, genetic polymorphisms may play a major role in determining the response to SSRI treatment [263–266]. At present the main focus of research is to gain greater understanding of the functional polymorphism in the 5-HT transporter (SERT) promoter region. SERT polymorphism (referred as 5-HTTLPR) involves the presence or absence of a 44 base-pair segment, which produces a long (L) or short (S) allele; the short allele results in decreased transporter expression and, hence, in a reduced uptake of 5-HT [267]. 5-HTTLPR has been associated with susceptibility to depression [268], although there is considerable heterogeneity between studies [269]. The S allele has also been associated with lower response to several SSRIs than the L allele in several studies [270–272] and may also increase vulnerability to SSRI side effects [273]. The large-scale study referred as STAR*D confirmed the S variant of 5-HTTLPR to be predictive for the global burden of side effects. Furthermore, Binder and coworkers examined 57 single nucleotide polymorphisms (SNP) in eight candidate genes related to the HPA axis in patients afflicted with depression searching for the SNP associated with antidepressant response. They observed that a polymorphism of FKBP5, the cochaperone of HSP90 regulating glucocorticoid receptor function, was associated with rapid response to antidepressants [256]. Another investigated polymorphic gene is the 5HT2A-receptor gene. All antidepressants induce a down-regulation of this postsynaptic receptor. The C variant at 102T/C was found to be associated with less antidepressant response. Murphy and coworkers observed in elderly depressed subjects that this polymorphism may be associated with sensitivity to the adverse effects of mirtazapine, but was without influence on SSRI adverse effects [273]. Antidepressants can also alter the synthesis and release of CRF; polymorphisms in the CRF gene have been described [274] and may be associated with MDD [275]. For further genes, TPH1 and G-protein β3, initially shown to be implicated in the modulation of antidepressant response, no definite conclusions can be made [276]. Delineating the genes that are correlated to an antidepressant response may be valuable in identifying the best treatment specific for the patient.
References
- 1.Hamet P, Tremblay J. Genetics and genomics of depression. Metabolism. 2005;54(5 Suppl 1):10–15. doi: 10.1016/j.metabol.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Segurado R, Detera-Wadleigh SD, Levinson DF, Lewis CM, Gill M, Nurnberger JI, Jr, Craddock N, DePaulo JR, Baron M, Gershon ES, Ekholm J, Cichon S, Turecki G, Claes S, Kelsoe JR, Schofield PR, Badenhop RF, Morissette J, Coon H, Blackwood D, McInnes LA, Foroud T, Edenberg HJ, Reich T, Rice JP, Goate A, McInnis MG, McMahon FJ, Badner JA, Goldin LR, Bennett P, Willour VL, Zandi PP, Liu J, Gilliam C, Juo SH, Berrettini WH, Yoshikawa T, Peltonen L, Lönnqvist J, Nöthen MM, Schumacher J, Windemuth C, Rietschel M, Propping P, Maier W, Alda M, Grof P, Rouleau GA, Del-Favero J, Van Broeckhoven C, Mendlewicz J, Adolfsson R, Spence MA, Luebbert H, Adams LJ, Donald JA, Mitchell PB, Barden N, Shink E, Byerley W, Muir W, Visscher PM, Macgregor S, Gurling H, Kalsi G, McQuillinm A, Escamilla MA, Reus VI, Leon P, Freimer NB, Ewald H, Kruse TA, Mors O, Radhakrishna U, Blouin JL, Antonarakis SE, Akarsu N. Genome scan meta-analysis of schizophrenia and bipolar disorder, part III: bipolar disorder. Am J Hum Genet. 2003;73(1):49–62. doi: 10.1086/376547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bunney WE, Jr, Davis JM. Norepinephrine in depressive reactions. A review. Arch Gen Psychiatry. 1965;13(6):483–494. doi: 10.1001/archpsyc.1965.01730060001001. [DOI] [PubMed] [Google Scholar]
- 4.Schildkraut JJ. The catecholamine hypothesis of affective disorders: a review of supporting evidence. J Neuropsychiatry Clin Neurosci. 1965;7:524–533. doi: 10.1176/jnp.7.4.524. [DOI] [PubMed] [Google Scholar]
- 5.Coppen A. The biochemistry of affective disorders. Br J Psychiatry. 1967;113:1237–1264. doi: 10.1192/bjp.113.504.1237. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery SA. The under-recognized role of dopamine in the treatment of major depressive disorder. Int Clin Psychopharmacol. 2008;23(2):63–69. doi: 10.1097/YIC.0b013e3282f2b3cb. [DOI] [PubMed] [Google Scholar]
- 7.Maas JW, Fawcett JA, Dekirmenjian H. Catecholamine metabolism, depressive illness, and drug response. Arch Gen Psychiatry. 1972;26(3):252–262. doi: 10.1001/archpsyc.1972.01750210060012. [DOI] [PubMed] [Google Scholar]
- 8.Roy A, Jimerson DC, Pickar D. Plasma MHPG in depressive disorders and relationship to the dexamethasone suppression test. Am J Psychiatry. 1986;143(7):846–851. doi: 10.1176/ajp.143.7.846. [DOI] [PubMed] [Google Scholar]
- 9.Potter WZ, Manji HK. Are monoamine metabolites in cerebrospinal fluid worth measuring? Arch Gen Psychiatry. 1993;50(8):653–656. doi: 10.1001/archpsyc.1993.01820200067007. [DOI] [PubMed] [Google Scholar]
- 10.Ordway GA, Smith KS, Haycock JW. Monoamine dysfunction and the pathophysiology and treatment of depression. J Clin Psychiatry. 1998;59(Suppl 14):11–14. [PubMed] [Google Scholar]
- 11.Ruhé HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12(4):331–359. doi: 10.1038/sj.mp.4001949. [DOI] [PubMed] [Google Scholar]
- 12.Charney DS. Elevated tyrosine hydroxylase in the locus coeruleus of suicide victims. J Neurochem. 1994;62(2):680–685. doi: 10.1046/j.1471-4159.1994.62020680.x. [DOI] [PubMed] [Google Scholar]
- 13.Zhu MY, Klimek V, Dilley GE, Haycock JW, Stockmeier C, Overholser JC, Meltzer HY, Ordway GA. Elevated levels of tyrosine hydroxylase in the locus coeruleus in major depression. Biol Psychiatry. 1999;46(9):1275–1286. doi: 10.1016/s0006-3223(99)00135-3. [DOI] [PubMed] [Google Scholar]
- 14.Ordway GA, Widdowson PS, Smith KS, Halaris A. Agonist binding to alpha 2-adrenoceptors is elevated in the locus coeruleus from victims of suicide. J Neurochem. 1994;63(2):617–624. doi: 10.1046/j.1471-4159.1994.63020617.x. [DOI] [PubMed] [Google Scholar]
- 15.Ordway GA, Schenk J, Stockmeier CA, May W, Klimek V. Elevated agonist binding to alpha2-adrenoceptors in the locus coeruleus in major depression. Biol. Psychiatry. 2003;53(4):315–323. doi: 10.1016/s0006-3223(02)01728-6. [DOI] [PubMed] [Google Scholar]
- 16.Klimek V, Stockmeier C, Overholser J, Meltzer HY, Kalka S, Dilley G, Ordway GA. Reduced levels of norepinephrine transporters in the locus coeruleus in major depression. J Neurosci. 1997;17(21):8451–8458. doi: 10.1523/JNEUROSCI.17-21-08451.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asberg M, Traskman L, Thoren P. 5-HIAA in the cerebrospinal fluid: a biochemical suicide predictor? . Arch Gen Psychiatry. 1976;33:1193–1197. doi: 10.1001/archpsyc.1976.01770100055005. [DOI] [PubMed] [Google Scholar]
- 18.Asberg M, Thoren L, Traskman P. Serotonin depression: a biochemical subgroup within the affective disorders. Science. 1976;191:478–480. doi: 10.1126/science.1246632. [DOI] [PubMed] [Google Scholar]
- 19.Csernansky JG, Sheline YI. Abnormalities of serotonin metabolism and nonpsychotic psychiatric disorders. Ann Clin Psychiatry. 1993;5(4):275–281. doi: 10.3109/10401239309148828. [DOI] [PubMed] [Google Scholar]
- 20.Tuinier S, Verhoeven WM, van Praag HM. Cerebrospinal fluid 5-hydroxyindolacetic acid and aggression: a critical reappraisal of the clinical data. Int Clin Psychopharmacol. 1995;10(3):147–156. doi: 10.1097/00004850-199510030-00003. [DOI] [PubMed] [Google Scholar]
- 21.Quintana J. Platelet serotonin and plasma tryptophan decreases in endogenous depression: clinical, therapeutic and biological correlations. J Affect Disord. 1992;24:58–62. doi: 10.1016/0165-0327(92)90019-3. [DOI] [PubMed] [Google Scholar]
- 22.Jans LA, Riedel WJ, Markus CR, Blokland A. Serotonergic vulnerability and depression: assumptions, experimental evidence and implications. Mol Psychiatry. 2007;12(6):522–543. doi: 10.1038/sj.mp.4001920. [DOI] [PubMed] [Google Scholar]
- 23.Arango V, Huang YY, Underwood MD, Mann JJ. Genetics of the serotonergic system in suicidal behavior. J Psychiatr Res. 2003;37(5):375–386. doi: 10.1016/s0022-3956(03)00048-7. [DOI] [PubMed] [Google Scholar]
- 24.Celada P, Puig M, Amargós-Bosch M, Adell A, Artigas F. The therapeutic role of 5-HT1A and 5-HT2A receptors in depression. J Psychiatry Neurosci. 2004;29(4):252–265. [PMC free article] [PubMed] [Google Scholar]
- 25.Mann JJ, Stanley M, McBride PA, McEwen BS. Increased serotonin2 and beta-adrenergic receptor binding in the frontal cortices of suicide victims. Arch Gen Psychiatry. 1986;43:945–959. doi: 10.1001/archpsyc.1986.01800100048007. [DOI] [PubMed] [Google Scholar]
- 26.Arora RC, Meltzer HY. Serotonergic measures in the brains of suicide victims: 5-HT2 binding sites in the frontal cortex of suicide victims and control subjects. Am J Psychiatry. 1989;146:730–736. doi: 10.1176/ajp.146.6.730. [DOI] [PubMed] [Google Scholar]
- 27.Yates M, Leake A, Candy JM, Fairbairn AF, McKeith IG, Ferrier IN. 5-HT2 receptor changes in major depression. Biol Psychiatry. 1990;27:489–496. doi: 10.1016/0006-3223(90)90440-d. [DOI] [PubMed] [Google Scholar]
- 28.Drevets WC, Frank E, Price JC, Kupfer DJ, Holt D, Greer PJ, Huang Y, Gautier C, Mathis C. PET imaging of serotonin 1A receptor binding in depression. Biol Psychiatry. 1999;46:1375–1387. doi: 10.1016/s0006-3223(99)00189-4. [DOI] [PubMed] [Google Scholar]
- 29.Hamner MB, Diamond BI. Plasma dopamine and norepinephrine correlations with psychomotor retardation, anxiety, and depression in non-psychotic depressed patients: a pilot study. Psychiatry Res. 1996;64(3):209–211. doi: 10.1016/s0165-1781(96)02879-x. [DOI] [PubMed] [Google Scholar]
- 30.Engstrom G, Alling C, Blennow K, Regnell G, Traskman-Bendz L. Reduced cerebrospinal HVA concentrations and HVA/5-HIAA ratios in suicide attempters. Monoamine metabolites in 120 suicide attempters and 47 controls. Eur Neuropsychopharmacol. 1999;9(5):399–405. doi: 10.1016/s0924-977x(99)00016-4. [DOI] [PubMed] [Google Scholar]
- 31.D’Haenen HA, Bossuyt A. Dopamine D2 receptors in depression measured with single photon emission computed tomography. Biol Psychiatry. 1994;35(2):128–132. doi: 10.1016/0006-3223(94)91202-5. [DOI] [PubMed] [Google Scholar]
- 32.Shah PJ, Ogilvie AD, Goodwin GM, Ebmeier KP. Clinical and psychometric correlates of dopamine D2 binding in depression. Psychol Med. 1997;27(6):1247–1256. doi: 10.1017/s0033291797005382. [DOI] [PubMed] [Google Scholar]
- 33.Klimek V, Schenck JE, Han H, Stockmeier CA, Ordway GA. Dopaminergic abnormalities in amygdaloid nuclei in major depression: a postmortem study. Biol Psychiatry. 2002;52(7):740–748. doi: 10.1016/s0006-3223(02)01383-5. [DOI] [PubMed] [Google Scholar]
- 34.Sonnenberg CM, Deeg DJ, Comijs HC, van Tilburg W, Beekman AT. Trends in antidepressant use in the older population: Results from the LASA-study over a period of 10 years. J Affect Disord. 2008;111(2–3):299–305. doi: 10.1016/j.jad.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 35.Duman RS, Heninger GR, Nestler EJ. A molecular and cellular theory of depression. Arch Gen Psychiatry. 1997;54(7):597–606. doi: 10.1001/archpsyc.1997.01830190015002. [DOI] [PubMed] [Google Scholar]
- 36.Orrego F, Villanueva S. The chemical nature of the main central excitatory transmitter: a critical appraisal based upon release studies and synaptic vesicle localization. Neuroscience. 1993;56:539–555. doi: 10.1016/0306-4522(93)90355-j. [DOI] [PubMed] [Google Scholar]
- 37.Sanacora S, Zarate CA, Krystal JH, Manji HK. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov. 2008;7(5):426–437. doi: 10.1038/nrd2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim JS, Schmid-Burgk W, Claus D, Kornhuber HH. Increased serum glutamate in depressed patients. Arch Psychiatr Nervenkr. 1982;232:299–304. doi: 10.1007/BF00345492. [DOI] [PubMed] [Google Scholar]
- 39.Altamura CA, Mauri MC, Ferrara A, Moro AR, D’Andrea G, Zamberlan F. Plasma and platelet excitatory amino acids in psychiatric disorders. Am J Psychiatry. 1993;150:1731–1733. doi: 10.1176/ajp.150.11.1731. [DOI] [PubMed] [Google Scholar]
- 40.Mauri MC, Ferrara A, Boscati L, Bravin S, Zamberlan F, Alecci M, Invernizzi G. Plasma and platelet amino acid concentrations in patients affected by major depression and under fluvoxamine treatment. Neuropsychobiology. 1998;37:124–129. doi: 10.1159/000026491. [DOI] [PubMed] [Google Scholar]
- 41.Mitani H, Shirayama Y, Yamada T, Maeda K, Ashby CR, Jr, Kawahara R. Correlation between plasma levels of glutamate, alanine and serine with severity of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1155–1158. doi: 10.1016/j.pnpbp.2006.03.036. [DOI] [PubMed] [Google Scholar]
- 42.Levine J, Panchalingam K, Rapoport A, Gershon S, McClure RJ, Pettegrew JW. Increased cerebrospinal fluid glutamine levels in depressed patients. Biol Psychiatry. 2000;47:586–593. doi: 10.1016/s0006-3223(99)00284-x. [DOI] [PubMed] [Google Scholar]
- 43.Frye MA, Tsai GE, Huggins T, Coyle JT, Post RM. Low cerebrospinal fluid glutamate and glycine in refractory affective disorder. Biol Psychiatry. 2006;61:162–166. doi: 10.1016/j.biopsych.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 44.Francis PT, Poynton A, Lowe SL, Najlerahim A, Bridges PK, Bartlett JR, Procter AW, Bruton CJ, Bowen DM. Brain amino acid concentrations and Ca2+-dependent release in intractable depression assessed antemortem. Brain Res. 1989;494:315–324. doi: 10.1016/0006-8993(89)90600-8. [DOI] [PubMed] [Google Scholar]
- 45.Nudmamud-Thanoi S, Reynolds GP. The NR1 subunit of the glutamate/NMDA receptor in the superior temporal cortex in schizophrenia and affective disorders. Neurosci Lett. 2004;372:173–177. doi: 10.1016/j.neulet.2004.09.035. [DOI] [PubMed] [Google Scholar]
- 46.Mundo E, Tharmalingham S, Neves-Pereira M, Dalton EJ, Macciardi F, Parikh SV, Bolonna A, Kerwin RW, Arranz MJ, Makoff AJ, Kennedy JL. Evidence that the N-methyl-d-aspartate subunit 1 receptor gene (GRIN1) confers susceptibility to bipolar disorder. Mol Psychiatry. 2003;8:241–245. doi: 10.1038/sj.mp.4001218. [DOI] [PubMed] [Google Scholar]
- 47.Martucci L, Wong AH, De Luca V, Likhodi O, Wong GW, King N, Kennedy JL. N-methyl-d-aspartate receptor NR2B subunit gene GRIN2B in schizophrenia and bipolar disorder: polymorphisms and mRNA levels. Schizophr Res. 2006;84:214–221. doi: 10.1016/j.schres.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 48.Meador-Woodruff JH, Hogg AJ, Jr, Smith RE. Striatal ionotropic glutamate receptor expression in schizophrenia, bipolar disorder, and major depressive disorder. Brain Res Bull. 2001;55:631–640. doi: 10.1016/s0361-9230(01)00523-8. [DOI] [PubMed] [Google Scholar]
- 49.Beneyto M, Meador-Woodruff JH. Lamina-specific abnormalities of AMPA receptor trafficking and signaling molecule transcripts in the prefrontal cortex in schizophrenia. Synapse. 2006;60:585–598. doi: 10.1002/syn.20329. [DOI] [PubMed] [Google Scholar]
- 50.Laje G, Paddock S, Manji H, Rush AJ, Wilson AF, Charney D, Mc-Mahon FJ. Genetic markers of suicidal ideation emerging during citalopram treatment of major depression. Am J Psychiatry. 2007;164:1530–1538. doi: 10.1176/appi.ajp.2007.06122018. [DOI] [PubMed] [Google Scholar]
- 51.Menke A, Lucae S, Kloiber S, Horstmann S, Bettecken T, Uhr M, Ripke S, Ising M, Müller-Myhsok B, Holsboer F, Binder EB. Genetic markers within glutamate receptors associated with antidepressant treatment-emergent suicidal ideation. Am J Psychiatry. 2008;165(7):917–918. doi: 10.1176/appi.ajp.2008.08020274. [DOI] [PubMed] [Google Scholar]
- 52.Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and gammaaminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64:193–200. doi: 10.1001/archpsyc.64.2.193. [DOI] [PubMed] [Google Scholar]
- 53.Kugaya A, Sanacora G. Beyond monoamines: glutamatergic function in mood disorders. CNS Spectr. 2005;10:808–819. doi: 10.1017/s1092852900010403. [DOI] [PubMed] [Google Scholar]
- 54.During MJ, Spencer DD. Extracellular hippocampal glutamate and spontaneous seizure in the conscious human brain. Lancet. 1993;341:1607–1610. doi: 10.1016/0140-6736(93)90754-5. [DOI] [PubMed] [Google Scholar]
- 55.Ongur D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc Natl Acad Sci USA. 1998;95:13290–13295. doi: 10.1073/pnas.95.22.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cotter D, Mackay D, Landau S, Kerwin R, Everall I. Reduced glial cell density and neuronal size in the anterior cingulate cortex in major depressive disorder. Arch Gen Psychiatry. 2001;58:545–553. doi: 10.1001/archpsyc.58.6.545. [DOI] [PubMed] [Google Scholar]
- 57.Cotter D, Pariante CM, Rajkowska G (2002) Glial pathology and major psychiatric disorders. In: Agam G, Everall I, Belmaker RH (eds) The postmortem brain in psychiatric research. Mass Kluwer Academic Publishers, Boston, pp 49–73
- 58.Bowley MP, Drevets WC, Ongur D, Price JL. Low glial numbers in the amygdala in major depressive disorder. Biol Psychiatry. 2002;52:404–412. doi: 10.1016/s0006-3223(02)01404-x. [DOI] [PubMed] [Google Scholar]
- 59.Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK. A randomized trial of an N-methyl-d-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–864. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]
- 60.Maeng S, Zarate CA., Jr The role of glutamate in mood disorders: results from the ketamine in major depression study and the presumed cellular mechanism underlying its antidepressant effects. Curr Psychiatry Rep. 2007;9(6):467–474. doi: 10.1007/s11920-007-0063-1. [DOI] [PubMed] [Google Scholar]
- 61.Ferguson JM, Shingleton RN. An open-label, flexible-dose study of memantine in major depressive disorder. Clin Neuropharmacol. 2007;30(3):136–144. doi: 10.1097/WNF.0b013e3180314ae7. [DOI] [PubMed] [Google Scholar]
- 62.Paredes RG, Agmo A. GABA and behavior: the role of receptor subtypes. Neurosci Biobehav Rev. 1992;16(2):145–170. doi: 10.1016/s0149-7634(05)80177-0. [DOI] [PubMed] [Google Scholar]
- 63.Petty F. GABA and mood disorders: a brief review and hypothesis. J Affect Disord. 1995;34(4):275–281. doi: 10.1016/0165-0327(95)00025-i. [DOI] [PubMed] [Google Scholar]
- 64.Sanacora G, Mason GF, Krystal JH. Impairment of GABAergic transmission in depression: new insights from neuroimaging studies. Crit Rev Neurobiol. 2000;14:23–45. doi: 10.1615/critrevneurobiol.v14.i1.20. [DOI] [PubMed] [Google Scholar]
- 65.Krystal JH, Sanacora G, Blumberg H, Anand A, Charney DS, Marek G, Epperson CN, Goddard A, Mason GF. Glutamate and GABA systems as targets for novel antidepressant and mood-stabilizing treatments. Mol Psychiatry. 2002;7:S71–S80. doi: 10.1038/sj.mp.4001021. [DOI] [PubMed] [Google Scholar]
- 66.Petty F, Kramer GL, Gullion CM, Rush AJ. Low plasma γ-aminobutyric acid levels in male patients with depression. Biol Psychiatry. 1992;32:354–363. doi: 10.1016/0006-3223(92)90039-3. [DOI] [PubMed] [Google Scholar]
- 67.Gerner R, Hare TA. CSF GABA levels in normal subjects and patients with depression, schizophrenia, mania and anorexia nervosa. Am J Psychiatry. 1981;138:1098–1101. doi: 10.1176/ajp.138.8.1098. [DOI] [PubMed] [Google Scholar]
- 68.Kasa K, Otsuki S, Yamamoto M, Sato M, Kuroda H, Ogawa N. Cerebrospinal fluid γ-aminobutyric acid and homovanillic acid in depressive disorders. Biol Psychiatry. 1982;17:877–883. [PubMed] [Google Scholar]
- 69.Roy A, Dejong J, Ferraro T. CSF GABA in depressed patients and normal controls. Psychol Med. 1991;21:613–618. doi: 10.1017/s0033291700022248. [DOI] [PubMed] [Google Scholar]
- 70.Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, Petroff OA, Berman RM, Charney DS, Krystal JH. Reduced cortical γ-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 1999;56:1043–1047. doi: 10.1001/archpsyc.56.11.1043. [DOI] [PubMed] [Google Scholar]
- 71.Sanacora G, Mason GF, Rothman DL, Krystal JH. Increased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitors. Am J Psychiatry. 2002;159:663–665. doi: 10.1176/appi.ajp.159.4.663. [DOI] [PubMed] [Google Scholar]
- 72.Sanacora G, Mason GF, Rothman DL, Ciarcia JJ, Ostroff RB, Krystal JH. Increased occipital cortex GABA concentrations following electroconvulsive therapy in depressed patients. Am J Psychiatry. 2003;160:577–579. doi: 10.1176/appi.ajp.160.3.577. [DOI] [PubMed] [Google Scholar]
- 73.Tunnicliff G, Ngo TT. Regulation of γ-aminobutyric acid synthesis in the vertebrate nervous system. Neurochem Int. 1986;8:287–297. doi: 10.1016/0197-0186(86)90002-1. [DOI] [PubMed] [Google Scholar]
- 74.Fatemi SH, Stary JM, Earle JA, Araghi-Niknam M, Eagan E. GABAergic dysfunction in schizophrenia and mood disorders as reflected by decreased levels of glutamic acid decarboxylase 65 and 67 kDa and reelin proteins in cerebellum. Schizophr Res. 2005;72:109–122. doi: 10.1016/j.schres.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 75.Benes FM, Todtenkopf MS, Logiotatos P, Williams M. Glutamate decarboxylase(65)-immunoreactive terminals in cingulate and prefrontal cortices of schizophrenic and bipolar brain. J Chem Neuroanat. 2000;20(3–4):259–269. doi: 10.1016/s0891-0618(00)00105-8. [DOI] [PubMed] [Google Scholar]
- 76.Heckers S, Stone D, Walsh J, Shick J, Koul P, Benes FM. Differential hippocampal expression of glutamic acid decarboxylase 65 and 67 messenger RNA in bipolar disorder and schizophrenia. Arch Gen Psychiatry. 2002;59(6):521–529. doi: 10.1001/archpsyc.59.6.521. [DOI] [PubMed] [Google Scholar]
- 77.Sanacora G, Saricicek A. GABAergic contributions to the pathophysiology of depression and the mechanism of antidepressant action. CNS Neurol Disord Drug Targets. 2007;6(2):127–140. doi: 10.2174/187152707780363294. [DOI] [PubMed] [Google Scholar]
- 78.Horiuchi Y, Nakayama J, Ishiguro H, Ohtsuki T, Detera-Wadleigh SD, Toyota T, Yamada K, Nankai M, Shibuya H, Yoshikawa T, Arinami T. Possible association between a haplotype of the GABA-A receptor alpha 1 subunit gene (GABRA1) and mood disorders. Biol Psychiatry. 2004;55(1):40–45. doi: 10.1016/s0006-3223(03)00689-9. [DOI] [PubMed] [Google Scholar]
- 79.Yamada K, Watanabe A, Iwayama-Shigeno Y, Yoshikawa T. Evidence of association between gamma-aminobutyric acid type A receptor genes located on 5q34 and female patients with mood disorders. Neurosci Lett. 2003;349(1):9–12. doi: 10.1016/s0304-3940(03)00611-6. [DOI] [PubMed] [Google Scholar]
- 80.Serretti A, Macciardi F, Cusin C, Lattuada E, Lilli R, Di Bella D, Catalano M, Smeraldi E. GABAA alpha-1 subunit gene not associated with depressive symptomatology in mood disorders. Psychiatr Genet. 1998;8(4):251–254. doi: 10.1097/00041444-199808040-00009. [DOI] [PubMed] [Google Scholar]
- 81.Mitchell AJ. The role of corticotropin releasing factor in depressive illness: a critical review. Neurosci Biobehav Rev. 1998;22:635–651. doi: 10.1016/s0149-7634(97)00059-6. [DOI] [PubMed] [Google Scholar]
- 82.Nemeroff CB. The neurobiology of depression. Sci Am. 1998;278:42–49. doi: 10.1038/scientificamerican0698-42. [DOI] [PubMed] [Google Scholar]
- 83.Gilad GM. The stress-induced response of the septo-hippocampal cholinergic system. A vectorial outcome of psychoneuroendocrinological interactions. Psychoneuroendocrinology. 1987;12:167–184. doi: 10.1016/0306-4530(87)90002-3. [DOI] [PubMed] [Google Scholar]
- 84.Janowsky DS, Risch SC. Cholinomimetic and anticholinergic drugs used to investigate an acetylcholine hypothesis of affective disorders and stress. Drug Devel Res. 1984;4:125–142. [Google Scholar]
- 85.Janowsky DS, El-Yousef MK, Davis JM, Sekerke HJ. A cholinergic-adrenergic hypothesis of mania and depression. Lancet. 1972;2:632–635. doi: 10.1016/s0140-6736(72)93021-8. [DOI] [PubMed] [Google Scholar]
- 86.Janowsky DS, El-Yousef MK, Davis JM, Sekerke HJ. Parasympathetic suppression of mania by physostigmine. Arch Gen Psych. 1973;28:542–547. doi: 10.1001/archpsyc.1973.01750340072012. [DOI] [PubMed] [Google Scholar]
- 87.Janowsky DS, Overstreet DH, Nurnberger JI., Jr Is cholinergic sensitivity a genetic marker for the affective disorders? Am J Med Genet. 1994;54:335–344. doi: 10.1002/ajmg.1320540412. [DOI] [PubMed] [Google Scholar]
- 88.Davis KL, Berger PA, Hollister LE, Defraites E. Physostigmine in man. Arch Gen Psychiatry. 1978;35:119–122. doi: 10.1001/archpsyc.1978.01770250121012. [DOI] [PubMed] [Google Scholar]
- 89.O’Keane V, O’Flynn K, Lucey J, Dinan TG. Pyridostigmine-induced growth hormone responses in healthy and depressed subjects: evidence for cholinergic supersensitivity in depression. Psychol Med. 1992;22:55–60. doi: 10.1017/s0033291700032724. [DOI] [PubMed] [Google Scholar]
- 90.Gillin JC, Salin-Pascual R, Velazquez-Moctezuma J, Shiromani P, Zoltoski R. Cholinergic receptor subtypes and REM sleep in animals and normal controls. Prog Brain Res. 1993;98:379–387. doi: 10.1016/s0079-6123(08)62422-x. [DOI] [PubMed] [Google Scholar]
- 91.Janowsky DS, Risch SC, Kennedy B, Ziegler M, Huey LY. Central muscarinic effects of physostigmine on mood, cardiovascular function, pituitary and adrenal neuroendocrine. Psychopharmacology. 1986;89:150–154. doi: 10.1007/BF00310619. [DOI] [PubMed] [Google Scholar]
- 92.Riemann D, Berger M. Sleep, age depression and the cholinergic induction test with RS 86. Prog Neuropsychopharmacol Biol Psychiatry. 1992;16:311–316. doi: 10.1016/0278-5846(92)90082-p. [DOI] [PubMed] [Google Scholar]
- 93.Bymaster FP, Felder CC. Role of the cholinergic muscarinic system in bipolar disorder and related mechanism of action of antipsychotic agents. Mol Psychiatry. 2002;7:S57–S63. doi: 10.1038/sj.mp.4001019. [DOI] [PubMed] [Google Scholar]
- 94.Burt T, Sachs GS, Demopulos C. Donepezil in treatment-resistant bipolar disorder. Biol Psychiatry. 1999;45:959–964. doi: 10.1016/s0006-3223(98)00320-5. [DOI] [PubMed] [Google Scholar]
- 95.Furey ML, Drevets WC. Antidepressant efficacy of the antimuscarinic drug scopolamine: a randomized, placebo-controlled clinical trial. Arch Gen Psychiatry. 2006;63(10):1121–1129. doi: 10.1001/archpsyc.63.10.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Janowsky DS. Scopolamine as an antidepressant agent: theoretical and treatment considerations. Curr Psychiatry Rep. 2007;9(6):447–448. doi: 10.1007/s11920-007-0060-4. [DOI] [PubMed] [Google Scholar]
- 97.Liu HF, Zhou WH, Xie XH, Cao JL, Gu J, Yang GD. Muscarinic receptors modulate the mRNA expression of NMDA receptors in brainstem and the release of glutamate in periaqueductal grey during morphine withdrawal in rats. Sheng Li Xu Bao. 2004;56(1):95–100. [PubMed] [Google Scholar]
- 98.Shytle RD, Silver AA, Lukas RJ, Newman MB, Sheehan DV, Sanberg P. Nicotinic acetylcholine receptors as targets for antidepressants. Mol Psychiatry. 2002;6:525–535. doi: 10.1038/sj.mp.4001035. [DOI] [PubMed] [Google Scholar]
- 99.Silver AA, Shytle RD, Sheehan KH, Sheehan DV, Ramos A, Sanberg P. Multicenter, double-blind, placebo-controlled study of mecamylamine monotherapy for Tourette’s disorder. J Am Acad Child Adolesc Psychiatry. 2001;40:1103–1110. doi: 10.1097/00004583-200109000-00020. [DOI] [PubMed] [Google Scholar]
- 100.Sacco KA, Bannon KL, George TP. Nicotinic receptor mechanisms and cognition in normal states and neuropsychiatric disorders. J Psychopharmacol. 2004;18(4):457–474. doi: 10.1177/0269881104047273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rozzini L, Vicini Chilovi B, Bertoletti E, Trabucchi M, Padovani A. Acetylcholinesterase inhibitors and depressive symptoms in patients with mild to moderate Alzheimer’s disease. Aging Clin Exp Res. 2007;19(3):220–223. doi: 10.1007/BF03324693. [DOI] [PubMed] [Google Scholar]
- 102.Wynn ZJ, Cummings JL. Cholinesterase inhibitor therapies and neuropsychiatric manifestations of Alzheimer’s disease. Dement Geriatr Cogn Disord. 2004;17(1–2):100–108. doi: 10.1159/000074281. [DOI] [PubMed] [Google Scholar]
- 103.Salzman C. Practical considerations for the treatment of depression in elderly and very elderly long-term care patients. J Clin Psychiatry. 1999;60(20):30–33. [PubMed] [Google Scholar]
- 104.Mottram P, Wilson K, Strobl J (2006) Antidepressants for depressed elderly. Cochrane Database Syst Rev (1):CD003491 [DOI] [PMC free article] [PubMed]
- 105.Griebel G. Is there a future for neuropeptide receptor ligands in the treatment of anxiety disorders? Pharmacol Ther. 1999;82:1–61. doi: 10.1016/s0163-7258(98)00041-2. [DOI] [PubMed] [Google Scholar]
- 106.Feng P, Vurbic D, Wu Z, Hu Y, Strohl KP. Changes in brain orexin levels in a rat model of depression induced by neonatal administration of clomipramine. J Psychopharmacol. 2008;22(7):784–791. doi: 10.1177/0269881106082899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brown GW, Bifulco A, Harris TO. Life events, vulnerability and onset of depression. Br J Psychiatry. 1987;150:30–42. doi: 10.1192/bjp.150.1.30. [DOI] [PubMed] [Google Scholar]
- 108.Hammen C, Davila J, Brown G, Ellicott A, Gitlin M. Psychiatric history and stress: predictors of severity of unipolar depression. J Abnorm Psychol. 1992;101:45–52. doi: 10.1037//0021-843x.101.1.45. [DOI] [PubMed] [Google Scholar]
- 109.Owens MJ, Nemeroff CB. Physiology and pharmacology of corticotropin-releasing factor. Pharmacol Rev. 1991;43:425–473. [PubMed] [Google Scholar]
- 110.Pariante CM. Depression, stress and the adrenal axis. J Neuroendocrinol. 2003;15(8):811–812. doi: 10.1046/j.1365-2826.2003.01058.x. [DOI] [PubMed] [Google Scholar]
- 111.Holsboer F, Barden N. Antidepressants and hypothalamic-pituitary-adrenocortical regulation. Endocr Rev. 1996;17:187–205. doi: 10.1210/edrv-17-2-187. [DOI] [PubMed] [Google Scholar]
- 112.Plotsky P, Owens MJ, Nemeroff CB. Neuropeptide alterations in affective disorders. In: Bloom FE, Kupfer DJ, editors. Psychopharmacology: the fourth generation of progress. New York: Raven Press; 1995. pp. 971–981. [Google Scholar]
- 113.Nemeroff CB, Widerlöv E, Bissette G, Walleus H, Karlsson I, Eklund K, Kilts CD, Loosen PT, Vale W. Elevated concentrations of CSF corticotropin-releasing factor-like immunoreactivity in depressed patients. Science. 1984;226:1342–1344. doi: 10.1126/science.6334362. [DOI] [PubMed] [Google Scholar]
- 114.Bánki CM, Karmacsi L, Bissette G, Nemeroff CB. Cerebrospinal fluid neuropeptides in mood disorders and dementia. J Affect Disord. 1992;25:39–46. doi: 10.1016/0165-0327(92)90091-j. [DOI] [PubMed] [Google Scholar]
- 115.Pitts AF, Samuelson SD, Meller WH, Bissette G, Nemeroff CB, Kathol RG. Cerebrospinal fluid corticotropin-releasing hormone, vasopressin, and oxytocin concentrations in treated patients with major depression and controls. Biol Psychiatry. 1995;38:330–335. doi: 10.1016/0006-3223(95)00229-A. [DOI] [PubMed] [Google Scholar]
- 116.Molchan SE, Hill JL, Martinez RA, Lawlor BA, Mellow AM, Rubinow DR, Bissette G, Nemeroff CB, Sunderland T. CSF somatostatin in Alzheimer’s disease and major depression: relationship to hypothalamic-pituitary-adrenal axis and clinical measures. Psychoneuroendocrinology. 1993;19:509–519. doi: 10.1016/0306-4530(93)90044-l. [DOI] [PubMed] [Google Scholar]
- 117.Stenzel-Poore MP, Heinrichs SC, Rivest S, Koob GF, Vale WW. Overproduction of corticotropin-releasing factor in transgenic mice: a genetic model of anxiogenic behavior. J Neurosci. 1994;14(5 Pt 1):2579–2584. doi: 10.1523/JNEUROSCI.14-05-02579.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kasahara M, Groenink L, Breuer M, Olivier B, Sarnyai Z. Altered behavioral adaptation in mice with neural corticotrophin-releasing factor overexpression. Genes Brain Behav. 2007;6(7):598–607. doi: 10.1111/j.1601-183X.2006.00286.x. [DOI] [PubMed] [Google Scholar]
- 119.Holmes A, Heilig M, Rupniak NMJ, Steckler T, Griebel G. Neuropeptides systems as novel therapeutic targets for depression and anxiety disorders. TIPS. 2003;24:580–588. doi: 10.1016/j.tips.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 120.Griebel G, Perrault G, Sanger DJ. Characterization of the behavioral profile of the non-peptide CRF receptor antagonist CP-154, 526 in anxiety models in rodents. Comparison with diazepam and buspirone. Psychopharmacology (Berl) 1998;138:55–66. doi: 10.1007/s002130050645. [DOI] [PubMed] [Google Scholar]
- 121.Holsboer F, Ising M. Central CRH system in depression and anxiety—evidence from clinical studies with CRH1 receptor antagonists. Eur J Pharmacol. 2008;583(2–3):350–357. doi: 10.1016/j.ejphar.2007.12.032. [DOI] [PubMed] [Google Scholar]
- 122.Aguilera G, Rabadan-Diehl C. Vasopressinergic regulation of the hypothalamic-pituitary-adrenal axis: implications for stress adaptation. Regul Pept. 2000;96:23–29. doi: 10.1016/s0167-0115(00)00196-8. [DOI] [PubMed] [Google Scholar]
- 123.Merali Z, Kent P, Du L, Hrdina P, Palkovits M, Faludi G, Poulter MO, Bédard T, Anisman H. Corticotropin-releasing hormone, arginine vasopressin, gastrin-releasing peptide, and neuromedin B alterations in stress-relevant brain regions of suicides and control subjects. Biol Psychiatry. 2006;59:594–602. doi: 10.1016/j.biopsych.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 124.van Londen L, Goekoop JG, van Kempen GM, Frankhuijzen-Sierevogel AC, Wiegant VM, van der Velde EA, De Wied D. Plasma levels of arginine vasopressin elevated in patients with major depression. Neuropsychopharmacology. 1997;17(4):284–292. doi: 10.1016/S0893-133X(97)00054-7. [DOI] [PubMed] [Google Scholar]
- 125.van Londen L, Kerkhof GA, van den Berg F, Goekoop JG, Zwinderman KH, Frankhuijzen-Sierevogel AC, Wiegant VM, de Wied D. Plasma arginine vasopressin and motor activity in major depression. Biol Psychiatry. 1998;43(3):196–204. doi: 10.1016/S0006-3223(97)80433-7. [DOI] [PubMed] [Google Scholar]
- 126.Purba JS, Hoogendijk WJ, Hofman MA, Swaab DF. Increased number of vasopressin- and oxytocin-expressing neurons in the paraventricular nucleus of the hypothalamus in depression. Arch Gen Psychiatry. 1996;53(2):137–143. doi: 10.1001/archpsyc.1996.01830020055007. [DOI] [PubMed] [Google Scholar]
- 127.Meynen G, Unmehopa UA, van Heerikhuize JJ, Hofman MA, Swaab DF, Hoogendijk WJ. Increased arginine vasopressin mRNA expression in the human hypothalamus in depression: a preliminary report. Biol Psychiatry. 2006;60(8):892–895. doi: 10.1016/j.biopsych.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 128.Spinedi E, Hadid R, Gaillard RC. Increased vasopressinergic activity as a possible compensatory mechanism for a normal hypothalamic-pituitary-adrenal axis response to stress in BALB/c nude mice. Neuroendocrinology. 1997;66(4):287–293. doi: 10.1159/000127250. [DOI] [PubMed] [Google Scholar]
- 129.Keck ME, Wigger A, Welt T, Müller MB, Gesing A, Reul JM, Holsboer F, Landgraf R, Neumann ID. Vasopressin mediates the response of the combined dexamethasone/CRH test in hyper-anxious rats: implications for pathogenesis of affective disorders. Neuropsychopharmacology. 2002;26(1):94–105. doi: 10.1016/S0893-133X(01)00351-7. [DOI] [PubMed] [Google Scholar]
- 130.Conte-Devolx B, Oliver C, Giraud P, Castanas E, Boudouresque F, Gillioz P, Millet Y. Adrenocorticotropin, and corticosterone secretion in Brattleboro rats. Endocrinology. 1982;110(6):2097–2100. doi: 10.1210/endo-110-6-2097. [DOI] [PubMed] [Google Scholar]
- 131.Wiley MK, Pearlmutter AF, Miller RE. Decreased adrenal sensitivity to ACTH in the vasopressin-deficient (Brattleboro) rat. Neuroendocrinology. 1974;14(5):257–270. doi: 10.1159/000122269. [DOI] [PubMed] [Google Scholar]
- 132.Fink G, Dow RC, Casley D, Johnston CI, Bennie J, Carroll S, Dick H. Atrial natriuretic peptide is involved in the ACTH response to stress and glucocorticoid negative feedback in the rat. J Endocrinol. 1992;135(1):37–43. doi: 10.1677/joe.0.1350037. [DOI] [PubMed] [Google Scholar]
- 133.Williams AR, Carey RJ, Miller M. Altered emotionality of the vasopressin-deficient Brattleboro rat. Peptides. 1985;6(Suppl 1):69–76. doi: 10.1016/0196-9781(85)90013-0. [DOI] [PubMed] [Google Scholar]
- 134.Mlynarik M, Zelena D, Bagdy G, Makara GB, Jezova D. Signs of attenuated depression-like behavior in vasopressin deficient Brattleboro rats. Horm Behav. 2007;51(3):395–405. doi: 10.1016/j.yhbeh.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 135.Jard S, Barberis C, Audigier S, Tribollet E. Neurohypophyseal hormone receptor systems in brain and periphery. Prog Brain Res. 1987;72:173–187. doi: 10.1016/s0079-6123(08)60206-x. [DOI] [PubMed] [Google Scholar]
- 136.Birnbaumer M. Vasopressin receptors. Trends Endocrinol Metab. 2000;11(10):406–410. doi: 10.1016/s1043-2760(00)00304-0. [DOI] [PubMed] [Google Scholar]
- 137.Thomson F, Craighead M. Innovative approaches for the treatment of depression: targeting the HPA axis. Neurochem Res. 2008;33(4):691–707. doi: 10.1007/s11064-007-9518-3. [DOI] [PubMed] [Google Scholar]
- 138.Lolait SJ, Stewart LQ, Jessop DS, Young WS, 3rd, O’Carroll AM. The hypothalamic-pituitary-adrenal axis response to stress in mice lacking functional vasopressin V1b receptors. Endocrinology. 2007;148(2):849–856. doi: 10.1210/en.2006-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wersinger SR, Ginns EI, O’Carroll AM, Lolait SJ, Young WS., 3rd Vasopressin V1b receptor knockout reduces aggressive behavior in male mice. Mol Psychiatry. 2002;7(9):975–984. doi: 10.1038/sj.mp.4001195. [DOI] [PubMed] [Google Scholar]
- 140.Wersinger SR, Kelliher KR, Zufall F, Lolait SJ, O’Carroll AM, Young WS., 3rd Social motivation is reduced in vasopressin 1b receptor null mice despite normal performance in an olfactory discrimination task. Horm Behav. 2004;46(5):638–645. doi: 10.1016/j.yhbeh.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 141.Egashira N, Tanoue A, Higashihara F, Fuchigami H, Sano K, Mishima K, Fukue Y, Nagai H, Takano Y, Tsujimoto G, Stemmelin J, Griebel G, Iwasaki K, Ikeda T, Nishimura R, Fujiwara M. Disruption of the prepulse inhibition of the startle reflex in vasopressin V1b receptor knockout mice: reversal by antipsychotic drugs. Neuropsychopharmacology. 2005;30(11):1996–2005. doi: 10.1038/sj.npp.1300784. [DOI] [PubMed] [Google Scholar]
- 142.Griebel G, Simiand J, Serradeil-Le Gal C, Wagnon J, Pascal M, Scatton B, Maffrand JP, Soubrie P. Anxiolytic- and antidepressant-like effects of the non-peptide vasopressin V1b receptor antagonist, SSR149415, suggest an innovative approach for the treatment of stress-related disorders. Proc Natl Acad Sci USA. 2002;99(9):6370–6375. doi: 10.1073/pnas.092012099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Overstreet DH, Griebel G. Antidepressant-like effects of the vasopressin V1b receptor antagonist SSR149415 in the Flinders Sensitive Line rat. Pharmacol Biochem Behav. 2005;82(1):223–227. doi: 10.1016/j.pbb.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 144.Iijima M, Chaki S. An arginine vasopressin V1b antagonist, SSR149415 elicits antidepressant-like effects in an olfactory bulbectomy model. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(3):622–627. doi: 10.1016/j.pnpbp.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 145.Alonso R, Griebel G, Pavone G, Stemmelin J, Le Fur G, Soubrié P. Blockade of CRF(1) or V(1b) receptors reverses stress-induced suppression of neurogenesis in a mouse model of depression. Mol Psychiatry. 2004;9(3):278–286. doi: 10.1038/sj.mp.4001464. [DOI] [PubMed] [Google Scholar]
- 146.Louis C, Cohen C, Depoortère R, Griebel G. Antidepressant-like effects of the corticotropin-releasing factor 1 receptor antagonist, SSR125543, and the vasopressin 1b receptor antagonist, SSR149415, in a DRL-72 s schedule in the rat. Neuropsychopharmacology. 2006;31(10):2180–2187. doi: 10.1038/sj.npp.1301036. [DOI] [PubMed] [Google Scholar]
- 147.Stemmelin J, Lukovic L, Salome N, Griebel G. Evidence that the lateral septum is involved in the antidepressant-like effects of the vasopressin V1b receptor antagonist, SSR149415. Neuropsychopharmacology. 2005;30(1):35–42. doi: 10.1038/sj.npp.1300562. [DOI] [PubMed] [Google Scholar]
- 148.Salomé N, Stemmelin J, Cohen C, Griebel G. Differential roles of amygdaloid nuclei in the anxiolytic- and antidepressant-like effects of the V1b receptor antagonist, SSR149415, in rats. Psychopharmacology (Berl). 2006;187(2):237–244. doi: 10.1007/s00213-006-0424-1. [DOI] [PubMed] [Google Scholar]
- 149.Hodgson RA, Higgins GA, Guthrie DH, Lu SX, Pond AJ, Mullins DE, Guzzi MF, Parker EM, Varty GB. Comparison of the V1b antagonist, SSR149415, and the CRF1 antagonist, CP-154, 526, in rodent models of anxiety and depression. Pharmacol Biochem Behav. 2007;86(3):431–440. doi: 10.1016/j.pbb.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 150.Serradeil-Le Gal C, Wagnon J, Simiand J, Griebel G, Lacour C, Guillon G, Barberis C, Brossard G, Soubrié P, Nisato D, Pascal M, Pruss R, Scatton B, Maffrand JP, Le Fur G. Characterization of (2S, 4R)-1-[5-chloro-1-[(2, 4-dimethoxyphenyl)sulfonyl]-3-(2-methoxy-phenyl)-2-oxo-2, 3-dihydro-1H-indol-3-yl]-4-hydroxy-N, N-dimethyl-2-pyrrolidine carboxamide (SSR149415), a selective and orally active vasopressin V1b receptor antagonist. J Pharmacol Exp Ther. 2002;300(3):1122–1130. doi: 10.1124/jpet.300.3.1122. [DOI] [PubMed] [Google Scholar]
- 151.Griffante C, Green A, Curcuruto O, Haslam CP, Dickinson BA, Arban R. Selectivity of d[Cha4]AVP and SSR149415 at human vasopressin and oxytocin receptors: evidence that SSR149415 is a mixed vasopressin V1b/oxytocin receptor antagonist. Br J Pharmacol. 2005;146(5):744–751. doi: 10.1038/sj.bjp.0706383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bielsky IF, Hu SB, Ren X, Terwilliger EF, Young LJ. The V1a vasopressin receptor is necessary and sufficient for normal social recognition: a gene replacement study. Neuron. 2005;47(4):503–513. doi: 10.1016/j.neuron.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 153.Landgraf R, Gerstberger R, Montkowski A, Probst JC, Wotjak CT, Holsboer F, Engelmann M. V1 vasopressin receptor antisense oligodeoxynucleotide into septum reduces vasopressin binding, social discrimination abilities, and anxiety-related behavior in rats. J Neurosci. 1995;15(6):4250–4258. doi: 10.1523/JNEUROSCI.15-06-04250.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ferris CF, Lu SF, Messenger T, Guillon CD, Heindel N, Miller M, Koppel G, Robert Bruns F, Simon NG. Orally active vasopressin V1a receptor antagonist, SRX251, selectively blocks aggressive behavior. Pharmacol. Biochem. Behav. 2006;83(2):169–174. doi: 10.1016/j.pbb.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 155.Pioro EP, Mai JK, Cuello AC (1990) Distribution of substance P and enkephalin immunoreactive neurons and fibers. In: Paxinos G (ed) The human nervous system (ed) Academic Press, San Diego, pp 1051–1094
- 156.Otsuka M, Yoshioka K. Neurotransmitter functions of mammalian tachykinins. Physiol Rev. 1993;73:229–308. doi: 10.1152/physrev.1993.73.2.229. [DOI] [PubMed] [Google Scholar]
- 157.Alvaro G, Di Fabio R. Neurokin 1 receptor antagonists—current prospects. Curr Opin Drug Discov Dev. 2007;10(5):613–621. [PubMed] [Google Scholar]
- 158.Herpfer I, Lieb K. Substance P and Substance P receptor antagonists in the pathogenesis and treatment of affective disorders. World J Biol Psychiatry. 2003;4:56–63. doi: 10.3109/15622970309167952. [DOI] [PubMed] [Google Scholar]
- 159.Stout SC, Owens MJ, Nemeroff CB. Neurokinin(1) receptor antagonists as potential antidepressants. Annu Rev Pharmacol Toxicol. 2001;41:877–906. doi: 10.1146/annurev.pharmtox.41.1.877. [DOI] [PubMed] [Google Scholar]
- 160.Herpfer I, Katzev M, Feige B, Fiebich BL, Voderholzer U, Lieb K. Effects of substance P on memory and mood in healthy male subjects. Hum Psychopharmacol Clin Exp. 2007;22:567–573. doi: 10.1002/hup.876. [DOI] [PubMed] [Google Scholar]
- 161.Bondy B, Baghai TC, Minov C, Schüle C, Schwarz MJ, Zwanzger P, Rupprecht R, Möller HJ. Substance P serum levels are increased in major depression: preliminary results. Biol Psychiatry. 2003;53:538–542. doi: 10.1016/s0006-3223(02)01544-5. [DOI] [PubMed] [Google Scholar]
- 162.Rimon R, Le Greves P, Nyberg F, Heikkila L, Salmela L, Terenius L. Elevation of substance P-like peptides in the CSF of psychiatric patients. Biol Psychiatry. 1984;19:509–516. [PubMed] [Google Scholar]
- 163.Herpfer I, Lieb K. Substance P receptor antagonists in psychiatry: rationale for development and therapeutic potential. CNS drug. 2005;19(4):275–293. doi: 10.2165/00023210-200519040-00001. [DOI] [PubMed] [Google Scholar]
- 164.Sergeyev V, Hokfelt T, Hurd Y. Serotonin and substance P coexist in dorsal raphe neurons of the human brain. Neuroreport. 1999;10:3967–3970. doi: 10.1097/00001756-199912160-00044. [DOI] [PubMed] [Google Scholar]
- 165.Kramer MS, Cutler N, Feighner J, Shrivastava R, Carman J, Sramek JJ, Reines SA, Liu G, Snavely D, Wyatt-Knowles E, Hale JJ, Mills SG, MacCoss M, Swain CJ, Harrison T, Hill RG, Hefti F, Scolnick EM, Cascieri MA, Chicchi GG, Sadowski S, Williams AR, Hewson L, Smith D, Carlson EJ, Hargreaves RJ, Rupniak NM. Distinct mechanism for antidepressant activity by blockade of central substance P receptors. Science. 1998;281:1640–1645. doi: 10.1126/science.281.5383.1640. [DOI] [PubMed] [Google Scholar]
- 166.Kramer MS, Winokur A, Kelsey J, Preskorn SH, Rothschild AJ, Snavely D, Ghosh K, Ball WA, Reines SA, Munjack D, Apter JT, Cunningham L, Kling M, Bari M, Getson A, Lee Y. Demonstration of the efficacy and safety of a novel substance P (NK1) receptor antagonist in major depression. Neuropsychopharmacology. 2004;29:385–392. doi: 10.1038/sj.npp.1300260. [DOI] [PubMed] [Google Scholar]
- 167.Keller M, Montgomery S, Ball W, Morrison M, Snavely D, Liu G, Hargreaves R, Hietala J, Lines C, Beebe K, Reines S. Lack of efficacy of the substance P (neurokinin1 receptor) antagonist aprepitant in the treatment of major depressive disorder. Biol Psychiatry. 2006;59(3):216–223. doi: 10.1016/j.biopsych.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 168.Chahl LA. Tachykinins and neuropsychiatric disorders. Curr Drug Targets. 2006;7(8):993–1003. doi: 10.2174/138945006778019309. [DOI] [PubMed] [Google Scholar]
- 169.Boselli C, Santagostino Barbone M, Lucchelli A. Older versus newer antidepressants: substance P or calcium antagonism? Can J Physiol Pharmacol. 2007;85:1004–1011. doi: 10.1139/y07-089. [DOI] [PubMed] [Google Scholar]
- 170.Kim HJ, Choi JS, Lee Y, Shim EY, Hong SH, Kim M, Min DS, Rhie D, Kim M, Jo Y, Hahn SJ, Yoon SH. Fluoxetine inhibits ATP-induced [Ca2+]i increase in PC12 cells by inhibiting both extracellular Ca2+ influx and Ca2+ release from intracellular stores. Neuropharmacology. 2005;49:265–274. doi: 10.1016/j.neuropharm.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 171.Lavoie PA, Beauchamp G, Elie R. Tricyclic antidepressants inhibit voltage-dependent calcium channels and Na(+)-Ca2+ exchange in rat brain cortex synaptosomes. Can J Physiol Pharmacol. 1990;68:1414–1418. doi: 10.1139/y90-215. [DOI] [PubMed] [Google Scholar]
- 172.Traboulsie A, Chemin J, Kupfer E, Nargeot J, Lory P. T-type calcium channels are inhibited by fluoxetine and its metabolite norfluoxetine. Mol Pharmacol. 2006;69:1963–1968. doi: 10.1124/mol.105.020842. [DOI] [PubMed] [Google Scholar]
- 173.Steinberg R, Alonso R, Griebel G, Bert L, Jung M, Oury-Donat F, Poncelet M, Gueudet C, Desvignes C, Le Fur G, Soubrié P. Selective blockade of neurokinin-2 receptors produces antidepressant-like effects associated with reduced corticotropin-releasing factor function. J Pharmacol Exp Ther. 2001;299:449–458. [PubMed] [Google Scholar]
- 174.Louis C, Stemmelin J, Boulay D, Bergis O, Cohen C, Griebel G. Additional evidence for anxiolytic- and antidepressant-like activities of saredutant (SR48968), an antagonist at the neurokinin-2 receptor in various rodent-models. Pharmacol Biochem Behav. 2008;89(1):36–45. doi: 10.1016/j.pbb.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 175.Tatemoto K, Mutt V. Isolation of two novel candidate hormones using a chemical method for finding naturally occurring polypeptides. Nature. 1980;285:417–418. doi: 10.1038/285417a0. [DOI] [PubMed] [Google Scholar]
- 176.Jiménez Vasquez PA, Salmi P, Ahlenius S, Mathé AA. Neuropeptide Y in brains of the Flinders Sensitive Line rat, a model of depression. Effects of electroconvulsive stimuli and d-amphetamine on peptide concentrations and locomotion. Behav Brain Res. 2000;111(1–2):115–123. doi: 10.1016/s0166-4328(00)00142-x. [DOI] [PubMed] [Google Scholar]
- 177.Eaton K, Sallee FR, Sah R. Relevance of neuropeptide Y (NPY) in psychiatry. Curr Top Med Chem. 2007;7(17):1645–1659. doi: 10.2174/156802607782341037. [DOI] [PubMed] [Google Scholar]
- 178.Mathé AA, Husum H, El Khoury A, Jiménez-Vasquez P, Gruber SH, Wörtwein G, Nikisch G, Baumann P, Agren H, Andersson W, Södergren A, Angelucci F. Search for biological correlates of depression and mechanisms of action of antidepressant treatment modalities. Do neuropeptides play a role? Physiol Behav. 2007;92(1–2):226–231. doi: 10.1016/j.physbeh.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 179.Widdowson PS, Ordway GA, Halaris AE. Reduced neuropeptide Y concentrations in suicide brain. J Neurochem. 1992;59:73–80. doi: 10.1111/j.1471-4159.1992.tb08877.x. [DOI] [PubMed] [Google Scholar]
- 180.Geisler S, Bérod A, Zahm DS, Rostène W. Brain neurotensin, psychostimulants, and stress—emphasis on neuroanatomical substrates. Peptides. 2006;27(10):2364–2384. doi: 10.1016/j.peptides.2006.03.037. [DOI] [PubMed] [Google Scholar]
- 181.Nemeroff CB. Neurotensin: perchance an endogenous neuroleptic. Biol Psychiatry. 1980;15:283–302. [PubMed] [Google Scholar]
- 182.Govoni S, Hong JS, Yang HYT, Costa E. Increase of neurotensin content elicited by neuroleptics in nucleus accumbens. J Pharmacol Exp Ther. 1980;215:413–417. [PubMed] [Google Scholar]
- 183.Merchant KM, Dobner PR, Dorsa DM. Differential effects of haloperidol and clozapine on neurotensin gene transcription in rat neostriatum. J Neurosci. 1992;12:652–663. doi: 10.1523/JNEUROSCI.12-02-00652.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Battaini F, Govoni S, Di Giovine S, Trabucchi M. Neurotensin effect on dopamine release and calcium transport in rat striatum: interactions with diphenylalkylamine calcium antagonists. Naunyn Schmiedebergs Arch Pharmacol. 1986;332(3):267–270. doi: 10.1007/BF00504865. [DOI] [PubMed] [Google Scholar]
- 185.Sharma RP, Janicak PJ, Bissette G, Nemeroff CB. CSF neurotensin concentrations and antipsychotic treatment in schizophrenia and schizoaffective disorder. Am J Psychiatry. 1997;154:1019–1021. doi: 10.1176/ajp.154.7.1019. [DOI] [PubMed] [Google Scholar]
- 186.Boules M, Fredrickson P, Richelson E. Neurotensin agonists as an alternative to antipsychotics. Expert Opin Investig Drugs. 2005;14(4):359–369. doi: 10.1517/13543784.14.4.359. [DOI] [PubMed] [Google Scholar]
- 187.Cervo L, Rossi C, Tatarczynska E, Samanin R. Antidepressant-like effect of neurotensin administered in the ventral tegmental area in the forced swimming test. Psychopharmacology (Berl) 1992;109(3):369–372. doi: 10.1007/BF02245885. [DOI] [PubMed] [Google Scholar]
- 188.Tatemoto K, Rökaeus A, Jörnvall H, McDonald TJ, Mutt V. Galanin—a novel biologically active peptide from porcine intestine. FEBS Lett. 1983;164:124–128. doi: 10.1016/0014-5793(83)80033-7. [DOI] [PubMed] [Google Scholar]
- 189.Kordower JH, Le HK, Mufson EJ. Galanin immunoreactivity in the primate central nervous system. J Comp Neurol. 1992;319:479–500. doi: 10.1002/cne.903190403. [DOI] [PubMed] [Google Scholar]
- 190.Pieribone VA, Burazin TC. Electrophysiologic effects of galanin on neurons of the central nervous system. Ann NY Acad Sci. 1998;863:264–273. doi: 10.1111/j.1749-6632.1998.tb10701.x. [DOI] [PubMed] [Google Scholar]
- 191.Kehr J, Yoshitake T, Wang FH, Razani H, Gimenez-Llort L, Jansson A, Yamaguchi M, Ogren SO. Galanin is a potent in vivo modulator of mesencephalic serotonergic neurotransmission. Neuropsychopharmacology. 2002;27:341–356. doi: 10.1016/S0893-133X(02)00309-3. [DOI] [PubMed] [Google Scholar]
- 192.Lu X, Sharkey L, Bartfai T. The brain galanin receptors: targets for novel antidepressant drugs. CNS Neurolog Dis Drug Targets. 2007;6:183–192. doi: 10.2174/187152707780619335. [DOI] [PubMed] [Google Scholar]
- 193.Branchek T, Smith KE, Walker MW. Molecular biology and pharmacology of galanin receptors. Ann NY Acad Sci. 1998;863:94–107. doi: 10.1111/j.1749-6632.1998.tb10687.x. [DOI] [PubMed] [Google Scholar]
- 194.Weiss JM, Bonsall RW, Demetrikopoulos MK, Emery MS, West CH. Galanin: a significant role in depression? Ann NY Acad Sci. 1998;863:364–382. doi: 10.1111/j.1749-6632.1998.tb10707.x. [DOI] [PubMed] [Google Scholar]
- 195.Kuteeva E, Wardi T, Hökfelt T, Ögren SO. Galanin enhances and a galanin antagonist attenuates depression-like behavior in the rat. Eur Neuropsychopharmacol. 2007;17:64–69. doi: 10.1016/j.euroneuro.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 196.Ogren SO, Razani H, Elvander-Tottie E, Kehr J. The neuropeptide galanin as an in vivo modulator of brain 5-HT1A receptors: possible relevance for affective disorders. Physiol Behav. 2007;92(1–2):172–179. doi: 10.1016/j.physbeh.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 197.Ogren SO, Kuteeva E, Hökfelt T, Kehr J. Galanin receptor antagonists : a potential novel pharmacological treatment for mood disorders. CNS Drugs. 2006;20(8):633–654. doi: 10.2165/00023210-200620080-00003. [DOI] [PubMed] [Google Scholar]
- 198.Kuteeva E, Hökfelt T, Wardi T, Ogren SO. Galanin—25 years with a multitalented neuropeptide: Galanin, galanin receptor subtypes and depression-like behavior. Cell Mol Life Sci. 2008;65(12):1854–1863. doi: 10.1007/s00018-008-8160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Murck H, Held K, Ziegenbein M, Kunzel H, Holsboer F, Steiger A. Intravenous administration of the neuropeptide galanin has fast antidepressant efficacy and affects the sleep EEG. Psychoneuroendocrinology. 2004;29:1205–1211. doi: 10.1016/j.psyneuen.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 200.Amadio M, Govoni S, Alkon DL, Pascale A. Emerging targets for the pharmacology of learning and memory. Pharmacol Res. 2004;50(2):111–122. doi: 10.1016/j.phrs.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 201.Squire LR. Memory and the hippocampus: A synthesis from findings with rats, monkeys and humans. Psychological Rev. 1992;99:195–231. doi: 10.1037/0033-295x.99.2.195. [DOI] [PubMed] [Google Scholar]
- 202.Fenn KM, Nusbaum HC, Margoliash D. Consolidation during sleep of perceptual learning of spoken language. Nature. 2003;425:614–616. doi: 10.1038/nature01951. [DOI] [PubMed] [Google Scholar]
- 203.Foster DJ, Wilson MA. Reverse replay of behavioral sequences in hippocampal place cells during the awake state. Nature. 2006;440:680–683. doi: 10.1038/nature04587. [DOI] [PubMed] [Google Scholar]
- 204.Kandel ER. The Molecular biology of memory storage: a dialog between genes and synapses. Biosci Rep. 2004;24(4/5):477–522. doi: 10.1007/s10540-005-2742-7. [DOI] [PubMed] [Google Scholar]
- 205.Spedding M, Neau I, Harsing L. Brain plasticity and pathology in psychiatric disease: sites of action for potential therapy. Curr Opin Pharmacol. 2003;3:33–40. doi: 10.1016/s1471-4892(02)00008-5. [DOI] [PubMed] [Google Scholar]
- 206.De Murtas M, Tatarelli R, Girardi P, Vicini S. Repeated electroconvulsive stimulation impairs long-term depression in the neostriatum. Biol Psychiatry. 2004;55:472–476. doi: 10.1016/j.biopsych.2003.11.022. [DOI] [PubMed] [Google Scholar]
- 207.Shakesby AC, Anwyl R, Rowan MJ. Overcoming the effects of stress on synaptic plasticity in the intact hippocampus: rapid actions of serotonergic and antidepressant agents. J Neurosci. 2002;22:3638–3644. doi: 10.1523/JNEUROSCI.22-09-03638.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Han JH, Kushner SA, Yiu AP, Hsiang HL, Buch T, Waisman A, Bontempi B, Neve RL, Frankland PW, Josselyn SA. Selective erasure of a fear memory. Science. 2009;323(5920):1492–1496. doi: 10.1126/science.1164139. [DOI] [PubMed] [Google Scholar]
- 209.Potter GG, Steffens DC. Contribution of depression to cognitive impairment and dementia in older adults. Neurologist. 2007;13(3):105–117. doi: 10.1097/01.nrl.0000252947.15389.a9. [DOI] [PubMed] [Google Scholar]
- 210.Duman RS. Role of neurotrophic factors in the etiology and treatment of mood disorders. Neuromolecular Med. 2004;5:11–25. doi: 10.1385/NMM:5:1:011. [DOI] [PubMed] [Google Scholar]
- 211.Duman RS, Monteggia LM. A neurotrophic model for stressrelated mood disorders. Biol Psychiatry. 2006;59:1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 212.Lindsay RM, Wiegand SJ, Altar CA, DiStefano PS. Neurotrophic factors: from molecule to man. Trends Neurosci. 1994;17:182–190. doi: 10.1016/0166-2236(94)90099-x. [DOI] [PubMed] [Google Scholar]
- 213.Sairanen M, O’Leary OF, Knuuttila JE, Castren E. Chronic antidepressant treatment selectively increases expression of plasticity related proteins in the hippocampus and medial prefrontal cortex of the rat. Neuroscience. 2007;144:368–374. doi: 10.1016/j.neuroscience.2006.08.069. [DOI] [PubMed] [Google Scholar]
- 214.Pang PT, Teng HK, Zaitsev E, Woo NT, Sakata K, Zhen S, Teng KK, Yung WH, Hempstead BL, Lu B. Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science. 2004;306:487–491. doi: 10.1126/science.1100135. [DOI] [PubMed] [Google Scholar]
- 215.Bekinschtein P, Cammarota M, Igaz LM, Bevilaqua LR, Izquierdo I, Medina JH. Persistence of long-term memory storage requires a late protein synthesis- and BDNF- dependent phase in the hippocampus. Neuron. 2007;53:261–277. doi: 10.1016/j.neuron.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 216.Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455(7215):894–902. doi: 10.1038/nature07455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and TrkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci. 1995;15:7539–7547. doi: 10.1523/JNEUROSCI.15-11-07539.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Chen B, Dowlatshahi D, MacQueen GM, Wang JF, Young LT. Increased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medication. Biol Psychiatry. 2001;50:260–265. doi: 10.1016/s0006-3223(01)01083-6. [DOI] [PubMed] [Google Scholar]
- 219.Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160:1516–1518. doi: 10.1176/appi.ajp.160.8.1516. [DOI] [PubMed] [Google Scholar]
- 220.Karege F, Schwald M, Cisse M. Postnatal developmental profile of brain-derived neurotrophic factor in rat brain and platelets. Neurosci Lett. 2002;328:261–264. doi: 10.1016/s0304-3940(02)00529-3. [DOI] [PubMed] [Google Scholar]
- 221.Shimizu E, Hashimoto K, Okamura N, Koike K, Komatsu N, Kumakiri C, Nakazato M, Watanabe H, Shinoda N, Okada S, Iyo M. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry. 2003;54:70–75. doi: 10.1016/s0006-3223(03)00181-1. [DOI] [PubMed] [Google Scholar]
- 222.Shirayama Y, Chen AC, Nakagawa S, Russell DS, Duman RS. Brain-derived neurotrophic factor produces antidepressant effects in behavioral models of depression. J Neurosci. 2002;22(8):3251–3261. doi: 10.1523/JNEUROSCI.22-08-03251.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Coppell AL, Pei Q, Zetterström TS. Bi-phasic change in BDNF gene expression following antidepressant drug treatment. Neuropharmacology. 2003;44(7):903–910. doi: 10.1016/s0028-3908(03)00077-7. [DOI] [PubMed] [Google Scholar]
- 224.De Foubert G, Carney SL, Robinson CS, Destexhe EJ, Tomlinson R, Hicks CA, Murray TK, Gaillard JP, Deville C, Xhenseval V, Thomas CE, O’Neill MJ, Zetterström TS. Fluoxetine-induced change in rat brain expression of brain-derived neurotrophic factor varies depending on length of treatment. Neuroscience. 2004;128(3):597–604. doi: 10.1016/j.neuroscience.2004.06.054. [DOI] [PubMed] [Google Scholar]
- 225.Messaoudi E, Ying SW, Kanhema T, Croll SD, Bramham CR. Brain-derived neurotrophic factor triggers transcription-dependent, late phase long-term potentiation in vivo. J Neurosci. 2002;22(17):7453–7461. doi: 10.1523/JNEUROSCI.22-17-07453.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Alme MN, Wibrand K, Dagestad G, Bramham CR. Chronic fluoxetine treatment induces brain region-specific upregulation of genes associated with BDNF-induced long-term potentiation. Neural Plast. 2007;2007:26496. doi: 10.1155/2007/26496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10(9):1089–1093. doi: 10.1038/nn1971. [DOI] [PubMed] [Google Scholar]
- 228.Bueller JA, Aftab M, Sen S, Gomez-Hassan D, Burmeister M, Zubieta JK. BDNF Val66Met allele is associated with reduced hippocampal volume in healthy subjects. Biol Psychiatry. 2006;59:812–815. doi: 10.1016/j.biopsych.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 229.Hwang JP, Tsai SJ, Hong CJ, Yang CH, Lirng JF, Yang YM. The Val66Met polymorphism of the brain-derived neurotrophic factor gene is associated with geriatric depression. Neurobiol Aging. 2006;27:1834–1837. doi: 10.1016/j.neurobiolaging.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 230.Pollak DD, Monje FJ, Zuckerman L, Denny CA, Drew MR, Kandel ER. An animal model of a behavioral intervention for depression. Neuron. 2008;60(1):149–161. doi: 10.1016/j.neuron.2008.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Krishnan V, Han MH, Graham DL, Berton O, Renthal W, Russo SJ, Laplant Q, Graham A, Lutter M, Lagace DC, Ghose S, Reister R, Tannous P, Green TA, Neve RL, Chakravarty S, Kumar A, Eisch AJ, Self DW, Lee FS, Tamminga CA, Cooper DC, Gershenfeld HK, Nestler EJ. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131(2):391–404. doi: 10.1016/j.cell.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 232.Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, Graham D, Tsankova NM, Bolanos CA, Rios M, Monteggia LM, Self DW, Nestler EJ. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science. 2006;311(5762):864–868. doi: 10.1126/science.1120972. [DOI] [PubMed] [Google Scholar]
- 233.Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9(4):519–525. doi: 10.1038/nn1659. [DOI] [PubMed] [Google Scholar]
- 234.Nestler EJ, Carlezon WA., Jr The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59(12):1151–1159. doi: 10.1016/j.biopsych.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 235.Cummings JL. Toward a molecular neuropsychiatry of neurodegenerative diseases. Ann Neurol. 2003;54(2):147–154. doi: 10.1002/ana.10616. [DOI] [PubMed] [Google Scholar]
- 236.Girgenti MJ, Hunsberger J, Duman CH, Sathyanesan M, Terwilliger R, Newton SS (2009) Erythropoietin induction by electroconvulsive seizure, gene regulation, and antidepressant-like behavioral effects. Biol Psychiatry. doi: 10.1016/j.biopsych.2008.12.005 [DOI] [PubMed]
- 237.Joffe H, Cohen LS. Estrogen, serotonin, and mood disturbance: where is the therapeutic bridge? Biol Psychiatry. 1998;44:798–811. doi: 10.1016/s0006-3223(98)00169-3. [DOI] [PubMed] [Google Scholar]
- 238.Sohrabji F, Greene LA, Miranda RC, Toran-Allerand CD. Reciprocal regulation of estrogen and NGF receptors by their ligands in PC12 cells. J Neurobiol. 1994;25:974–988. doi: 10.1002/neu.480250807. [DOI] [PubMed] [Google Scholar]
- 239.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- 240.Parry BL, Newton RP. Chronobiological basis of female-specific mood disorders. Neuropsycopharmacology. 2001;25(5):S102–S108. doi: 10.1016/S0893-133X(01)00340-2. [DOI] [PubMed] [Google Scholar]
- 241.Young EA, Korszun A. The hypothalamic-pituitary-gonadal axis in mood disorders. Endocrinol Metab Clin North Am. 2002;31(1):63–78. doi: 10.1016/s0889-8529(01)00002-0. [DOI] [PubMed] [Google Scholar]
- 242.Gallicchio L, Schilling C, Miller SR, Zacur H, Flaws JA. Correlates of depressive symptoms among women undergoing the menopausal transition. J Psychosom Res. 2007;63:263–268. doi: 10.1016/j.jpsychores.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 243.Morsink LF, Vogelzangs N, Nicklas BJ, Beekman AT, Satterfield S, Rubin SM, Yaffe K, Simonsick E, Newman AB, Kritchevsky SB, Penninx BW, for the Health ABC study Associations between sex steroid hormone levels and depressive symptoms in elderly men and women: results from the Health ABC study. Psychoneuroendocrinology. 2007;32:874–883. doi: 10.1016/j.psyneuen.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 244.Young EA, Midgley AR, Carlson NE, Brown MB. Alteration in the hypothalamic-pituitary-ovarian axis in depressed women. Arch Gen Psychiatry. 2000;57(12):1157–1162. doi: 10.1001/archpsyc.57.12.1157. [DOI] [PubMed] [Google Scholar]
- 245.Carlson LE, Sherwin BB, Chertkow HM. Relationships between mood and estradiol (E2) levels in Alzheimer’s disease (AD) patients. J Gerontol. 2000;B55:47–53. doi: 10.1093/geronb/55.1.p47. [DOI] [PubMed] [Google Scholar]
- 246.Bloch M, Schmidt PJ, Su TP, Tobin MB, Rubinow DR. Pituitary-adrenal hormones and testosterone across the menstrual cycle in women with premenstrual syndrome and controls. Biol Psychiatry. 1998;43:897–903. doi: 10.1016/s0006-3223(98)00403-x. [DOI] [PubMed] [Google Scholar]
- 247.Carlsson M, Carlsson A. A regional study of sex differences in rat brain serotonin. Prog Neuropsychopharmacol Biol Psychiatry. 1988;12:53–61. doi: 10.1016/0278-5846(88)90061-9. [DOI] [PubMed] [Google Scholar]
- 248.Haleem DJ, Kennett GA, Curzon G. Hippocampal 5-hydroxy-tryptamine synthesis is greater in female rats than in males and more decreased by the 5-HT1A agonist 8-OHDPAT. J Neural Transm Gen Sect. 1990;79:93–101. doi: 10.1007/BF01251004. [DOI] [PubMed] [Google Scholar]
- 249.Nishizawa S, Benkelfat C, Young SN, Leyton M, Mzengeza S, deMontignuy C, Blier P, Diksic M. Differences between males and females in rates of serotonin synthesis in human brain. Proc Natl Acad Sci USA. 1997;94:5308–5313. doi: 10.1073/pnas.94.10.5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Agren H, Mefford IN, Rudorfer MV, Linnoila M, Potter WZ. Interacting neurotransmitter systems: a non-experimental approach to the 5-HIAA-HVA correlation in human CSF. J Psychiatr Res. 1986;20:175–193. doi: 10.1016/0022-3956(86)90002-6. [DOI] [PubMed] [Google Scholar]
- 251.Biver F, Lotstra F, Monclus M, Wikler D, Damhaut P, Mendlewicz J, Goldman S. Sex difference in 5HT2 receptor in the living human brain. Neurosci Lett. 1996;204:25–28. doi: 10.1016/0304-3940(96)12307-7. [DOI] [PubMed] [Google Scholar]
- 252.Kendall DA, Stancel GM, Enna SJ. Imipramine: effect of ovarian steroids on modifications in serotonin receptor binding. Science. 1981;211:1183–1185. doi: 10.1126/science.6258229. [DOI] [PubMed] [Google Scholar]
- 253.Westberg L, Eriksson E. Sex steroid-related candidate genes in psychiatric disorders. J Psychiatry Neurosci. 2008;33(4):319–330. [PMC free article] [PubMed] [Google Scholar]
- 254.Cheng R, Juo SH, Loth JE, Nee J, Iossifov I, Blumenthal R, Sharpe L, Kanyas K, Lerer B, Lilliston B, Smith M, Trautman K, Gilliam TC, Endicott J, Baron M. Genome-wide linkage scan in a large bipolar disorder sample from the National Institute of Mental Health genetics initiative suggests putative loci for bipolar disorder, psychosis, suicide, and panic disorder. Mol Psychiatry. 2006;11:252–260. doi: 10.1038/sj.mp.4001778. [DOI] [PubMed] [Google Scholar]
- 255.Wochnik GM, Ruegg J, Abel GA, Schmidt U, Holsboer F, Rein T. FK506-binding Proteins 51 and 52 differentially regulate dynein interaction and nuclear translocation of the glucocorticoid receptor in mammalian cells. J Biol Chem. 2005;28:4609–4616. doi: 10.1074/jbc.M407498200. [DOI] [PubMed] [Google Scholar]
- 256.Binder EB, Salyakina D, Lichtner P, Wochnik GM, Ising M, Pütz B, Papiol S, Seaman S, Lucae S, Kohli MA, Nickel T, Künzel HE, Fuchs B, Majer M, Pfennig A, Kern N, Brunner J, Modell S, Baghai T, Deiml T, Zill P, Bondy B, Rupprecht R, Messer T, Köhnlein O, Dabitz H, Brückl T, Müller N, Pfister H, Lieb R, Mueller JC, Lõhmussaar E, Strom TM, Bettecken T, Meitinger T, Uhr M, Rein T, Holsboer F, Muller-Myhsok B. Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment. Nat Genet. 2004;36:1319–1325. doi: 10.1038/ng1479. [DOI] [PubMed] [Google Scholar]
- 257.Tsankova N, Renthal W, Kumar A, Nestler EJ. Epigenetic regulation in psychiatric disorders. Nat Rev Neurosci. 2007;8:355–367. doi: 10.1038/nrn2132. [DOI] [PubMed] [Google Scholar]
- 258.McGowan PO, Sasaki A, D’Alessio AC, Dymov S, Labonté B, Szyf M, Turecki G, Meaney MJ. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. 2009;12(3):342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Weaver IC, Cervoni N, Champagne FA, D’Alessio AC, Sharma S, Seckl JR, Dymov S, Szyf M, Meaney MJ. Epigenetic programming by maternal behavior. Nat Neurosci. 2004;7(8):847–854. doi: 10.1038/nn1276. [DOI] [PubMed] [Google Scholar]
- 260.Levenson JM, Roth TL, Lubin FD, Miller CA, Huang IC, Desai P, Malone LM, Sweatt JD. Evidence that DNA (cytosine-5) methyltransferase regulates synaptic plasticity in the hippocampus. J Biol Chem. 2006;281(23):15763–15773. doi: 10.1074/jbc.M511767200. [DOI] [PubMed] [Google Scholar]
- 261.Chen Z, Skolnick P. Triple uptake inhibitors: therapeutic potential in depression and beyond. Expert Opin Investig Drugs. 2007;16:1365–1377. doi: 10.1517/13543784.16.9.1365. [DOI] [PubMed] [Google Scholar]
- 262.Skolnick P, Krieter P, Tizzano J, Basile A, Popik P, Czobor P, Lippa A. Preclinical and clinical pharmacology of DOV216, 303, a “triple” reuptake inhibitor. CNS Drug Rev. 2006;12:123–134. doi: 10.1111/j.1527-3458.2006.00123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Lotrich FE, Pollock BG. Candidate genes for antidepressant response to selective serotonin reuptake inhibitors. Neuropsychiatr Dis Treat. 2005;1(1):17–35. doi: 10.2147/nedt.1.1.17.52301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kato T. Molecular genetics of bipolar disorder and depression. Psychiatry Clin Neurosci. 2007;61(1):3–19. doi: 10.1111/j.1440-1819.2007.01604.x. [DOI] [PubMed] [Google Scholar]
- 265.Maier W, Zobel A. Contribution of allelic variations to the phenotype of response to antidepressants and antipsychotics. Eur Arch Psychiatry Clin Neurosci. 2008;258(1):12–20. doi: 10.1007/s00406-007-1004-z. [DOI] [PubMed] [Google Scholar]
- 266.Camilleri M. Pharmacogenomics and serotonergic agents: research observations and potential clinical practice implications. Neurogastroenterol Motil. 2007;19(2):40–45. doi: 10.1111/j.1365-2982.2007.00961.x. [DOI] [PubMed] [Google Scholar]
- 267.Lesch KP. Serotonin transporter and psychiatric disorders: listening to the gene. Neuroscientist. 1998;4:25–34. [Google Scholar]
- 268.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:368–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 269.Lotrich FE, Pollock BG. Meta-analysis of serotonin transporter polymorphisms and affective disorder. Psychiatr Genet. 2004;14(3):121–129. doi: 10.1097/00041444-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 270.Yu YW, Tsai SJ, Chen TJ, Lin CH, Hong CJ. Association study of the serotonin transporter promoter polymorphism and symptomatology and antidepressant response in major depressive disorders. Mol Psychiatry. 2002;7(10):1115–1119. doi: 10.1038/sj.mp.4001141. [DOI] [PubMed] [Google Scholar]
- 271.Arias B, Catalán R, Gastó C, Gutiérrez B, Fañanás L. 5-HTTLPR polymorphism of the serotonin transporter gene predicts non-remission in major depression patients treated with citalopram in a 12-weeks follow up study. J Clin Psychopharmacol. 2003;23(6):563–567. doi: 10.1097/01.jcp.0000095350.32154.73. [DOI] [PubMed] [Google Scholar]
- 272.Serretti A, Cusin C, Rossini D, Artioli P, Dotoli D, Zanardi R. Further evidence of a combined effect of SERTPR and TPH on SSRIs response in mood disorders. Am J Med Genet B Neuropsychiatr Genet. 2004;129:36–40. doi: 10.1002/ajmg.b.30027. [DOI] [PubMed] [Google Scholar]
- 273.Murphy GM, Jr, Kremer C, Rodrigues HE, Schatzberg AF. Pharmacogenetics of antidepressant medication intolerance. Am J Psychiatry. 2003;160(10):1830–1835. doi: 10.1176/appi.ajp.160.10.1830. [DOI] [PubMed] [Google Scholar]
- 274.Gonzalez-Gay MA, Hajeer AH, Garcia-Porrua C, Dababneh A, Amoli MM, Botana MA, Thomson W, Llorca J, Ollier WE. Corticotropin-releasing hormone promoter polymorphisms in patients with rheumatoid arthritis from northwest Spain. J Rheumatol. 2003;30(5):913–917. [PubMed] [Google Scholar]
- 275.Claes S, Villafuerte S, Forsgren T, Sluijs S, Del-Favero J, Adolfsson R, Van Broeckhoven C. The corticotropin-releasing hormone binding protein is associated with major depression in a population from Northern Sweden. Biol Psychiatry. 2003;54(9):867–872. doi: 10.1016/s0006-3223(03)00425-6. [DOI] [PubMed] [Google Scholar]
- 276.Binder EB, Holsboer F. Pharmacogenomics and antidepressant drugs. Ann Med. 2006;38:82–94. doi: 10.1080/07853890600551045. [DOI] [PubMed] [Google Scholar]